A Comprehensive Guide to Organ Bath Experiments: From Foundational Principles to Advanced Applications in Drug Discovery
This article provides a complete guide to the organ bath technique, a cornerstone method in pharmacology and physiology for over a century.
A Comprehensive Guide to Organ Bath Experiments: From Foundational Principles to Advanced Applications in Drug Discovery
Abstract
This article provides a complete guide to the organ bath technique, a cornerstone method in pharmacology and physiology for over a century. Tailored for researchers, scientists, and drug development professionals, it covers the foundational principles of isolated tissue bath systems, detailed methodological protocols for assessing contractile tissue function, advanced troubleshooting and data normalization strategies, and validation approaches for translational research. The content synthesizes current best practices to enable robust experimental design, accurate data interpretation, and effective application in therapeutic development, from basic research to clinical diagnostics like the caffeine-halothane contracture test for malignant hyperthermia.
The Legacy and Principles of Organ Bath Technology: From Historical Discoveries to Modern Setup
The isolated organ bath stands as one of the most historically significant and enduring tools in pharmacological research. For nearly a century, this system has provided the fundamental platform for studying the effects of chemical substances on living tissues, forming the cornerstone of our understanding of drug-receptor interactions and concentration-response relationships. Despite the advent of high-throughput molecular screening and in silico platforms, organ bath assays remain a vital tool for lead optimization and mechanistic studies, bridging the gap between cellular models and whole-animal experiments [1] [2]. These systems are the classical pharmacological screening tool for assessing concentration-response relationships in contractile tissue and are still considered valuable for elucidating the mechanism of action of new therapeutic compounds [3].
Organ bath assays are widely used in preclinical safety studies and basic research. Their most common applications span cardiovascular research (using aortic rings, heart tissue), gastrointestinal studies (using ileum and colon preparations), respiratory research (using tracheal rings), and investigations of urinary bladder, penile muscle, and prostate function [3]. The rebirth of interest in these systems is driven by the need for model systems that more accurately predict in vivo drug effects, as hits generated through target-based screening programs often prove invalid in more complex biological contexts [2].
Modern Applications and Quantitative Data
Modern organ bath systems have evolved into highly sophisticated instruments that maintain the core principles of classical pharmacology while incorporating contemporary technological advances. The data generated from these systems provides crucial quantitative parameters that are fundamental to pharmacology.
Table 1: Key Quantitative Parameters from Organ Bath Experiments
| Parameter | Description | Pharmacological Significance |
|---|---|---|
| Potency (ECâ‚…â‚€) | Concentration producing 50% of maximal effect | Indicates drug affinity for receptor |
| Maximal Effect (Eₘâ‚â‚“) | Greatest possible response produced by a drug | Measures intrinsic efficacy |
| Slope Parameter (nâ‚•) | Steepness of the concentration-response curve | Suggests cooperativity in receptor binding |
| pAâ‚‚ Value | Measure of antagonist affinity | Quantifies antagonist potency |
Table 2: Tissue Preparations and Their Research Applications
| Tissue Type | Common Research Applications | Example Measurements |
|---|---|---|
| Aortic Rings | Cardiovascular drug screening, endothelial function | Vasoconstriction/vasodilation |
| Tracheal Rings | Respiratory drug discovery, asthma research | Bronchoconstriction/bronchodilation |
| Ileum/Colon | Gastrointestinal motility, spasmolytic drugs | Peristaltic contractions, relaxation |
| Heart Tissue | Cardiac inotropy, chronotropy | Contractile force, rate changes |
The information that conventional organ baths produce remains highly valuable, with systems like the Multi Myograph System 620M enabling in-vitro studies of vascular structure and function, while the Organ Bath System 820MO is ideal for measuring mechanical properties of isolated muscle tissue [3]. These systems continue to provide irreplaceable data for pharmacological characterization.
Advanced Protocols: Multi-Well Organ Bath (MuWOB) Technology
A significant innovation in the field is the development of the Multi-Well Organ Bath (MuWOB) system, which adapts isolated organ studies to standard 96-well plates, enabling simultaneous quantification of 96 preparations while using small volumes (≈100 µl/well) [2]. This technology represents a bridge between classical pharmacology and modern high-throughput screening.
MuWOB Protocol for Vascular Studies
Protocol Title: Assessment of Vasoactive Compounds Using Rat Aortic Rings in MuWOB System
Materials:
- Multi-well organ bath system with bi-telecentric optics
- Standard 96-well plates
- Krebs-HEPES buffer solution
- Adult rat thoracic aorta
- Test compounds and reference agonists/antagonists
Methodology:
- Tissue Preparation: Sacrifice rat humanely and rapidly excise thoracic aorta. Carefully remove adhering fat and connective tissue. Cut aorta into 1 mm rings using sharp surgical scissors.
- Plate Loading: Place one aortic ring into each well of a 96-well plate filled with 100 µl of standard saline buffer (Krebs-HEPES).
- Stabilization: Position plate on black surface centered under optics. Allow tissues to stabilize for approximately 30 minutes.
- Drug Addition: Add drug solutions (typically 10 µl volume) after removing equivalent volume from each well to maintain constant total volume.
- Image Acquisition: Capture frames at frequency of 0.1 Hz throughout experiment to precisely track time-course of contractile activity.
- Data Analysis: Use dedicated software to quantify changes in luminal area of vessel rings. Calculate percentage contraction/relaxation relative to baseline.
Technical Considerations: The MuWOB system enables the elaboration of dose-response curves for both agonists and antagonists with high reproducibility. The optical measurement of luminal area reduction correlates well with traditional force transduction methods [2]. This system offers substantial advantages in throughput, reagent consumption, and space efficiency compared to traditional organ baths.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful organ bath experimentation requires specific reagents and equipment designed to maintain tissue viability and enable precise measurement of pharmacological responses.
Table 3: Essential Research Reagent Solutions for Organ Bath Experiments
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Krebs-Henseleit Buffer | Physiological salt solution | Maintains ionic balance, pH, and tissue viability |
| Carbogen Gas (95% Oâ‚‚, 5% COâ‚‚) | Tissue oxygenation | Essential for aerobic metabolism in isolated tissues |
| Force Transducers | Measures tissue contraction | Converts mechanical force to electrical signals |
| Temperature-Controlled Bath | Maintains physiological temperature | Typically 37°C for mammalian tissues |
| Tissue Holders | Secures tissue in bath | Allows optimal length-tension relationship |
| Agonist/Antagonist Solutions | Receptor activation/blockade | Prepared fresh daily in appropriate buffer |
| Cariprazine D6 | Cariprazine D6, MF:C21H32Cl2N4O, MW:433.4 g/mol | Chemical Reagent |
| Norfloxacin-d5 | Norfloxacin-d5, CAS:1015856-57-1, MF:C16H18FN3O3, MW:324.36 g/mol | Chemical Reagent |
Experimental Workflow and Signaling Pathways
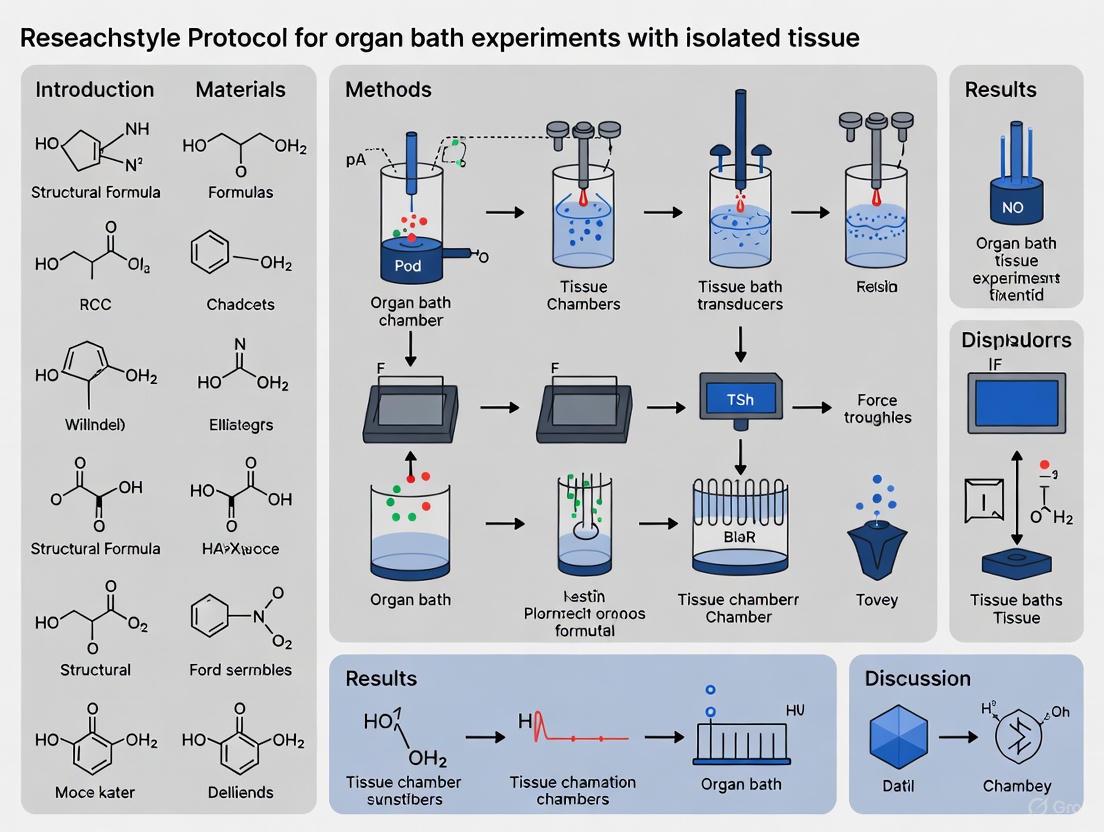
The following diagram illustrates the complete experimental workflow for a standard organ bath experiment, from tissue preparation to data analysis:
The pharmacological effects measured in organ bath systems are mediated through complex signaling pathways that translate receptor activation into tissue responses:
For nitrergic neurons studied in gastrointestinal organ bath preparations, a specific signaling pathway mediates smooth muscle relaxation:
The organ bath preparation has maintained its relevance through a century of pharmacological discovery by adapting to modern research needs while preserving its fundamental capacity to reveal drug actions in living tissues. The development of technologies like the MuWOB system demonstrates how this classical approach can be integrated with contemporary high-throughput screening paradigms [2]. For researchers investigating complex physiological systems, particularly in areas like cardiovascular pharmacology, gastrointestinal motility, and respiratory medicine, organ baths continue to provide critical insights that complement molecular and cellular approaches. As drug discovery faces ongoing challenges in translating target-based hits to effective therapies, the organ bath remains an essential tool for validating compound efficacy and safety in functionally intact tissues.
The isolated tissue bath, commonly referred to as an organ bath, represents a classic yet continually evolving experimental setup that has been instrumental in pharmacology and physiology research for over a century. First developed by Rudolf Magnus in 1904, this system allows researchers to investigate the contractile and functional properties of isolated tissues under controlled ex vivo conditions [4]. The fundamental principle involves suspending an isolated tissue specimen within a fluid-filled chamber that maintains physiological conditions, enabling precise measurement of tissue responses to pharmacological agents or electrical stimulation [5] [6]. Modern iterations, such as the DMT Organ Bath – 820MO, integrate decades of knowledge from myography and conventional organ bath setups into robust, compact designs with built-in features including oxygenation, buffer drainage, calibration procedures, and heating capabilities [7].
The versatility of organ bath systems extends to a wide range of tissue types, including blood vessels, airways, gastrointestinal tissues, genitourinary tissues, and cardiac muscle [8]. These systems remain indispensable in contemporary research and drug development because they allow tissues to function as integrated systems, providing a synthesis of drug-receptor interactions, signal transduction, second messenger generation, changes in smooth muscle excitability, and ultimately, alterations in tissue function [6]. This holistic approach offers significant advantages over reductionist cellular assays by preserving the complex cellular architecture and intercellular communication present in intact tissues.
Core System Components and Their Functions
A modern organ bath system consists of several integrated components that work in concert to maintain tissue viability and enable precise measurement of physiological responses. Understanding these core elements is essential for proper experimental setup and execution.
Table 1: Core Components of a Modern Organ Bath System
| Component | Material & Specifications | Primary Function |
|---|---|---|
| Tissue Bath Chamber | Borosilicate glass; 5, 10, 20 mL volumes (custom sizes available) [5] | Houses tissue specimen and bathing solution in a controlled environment |
| Tissue Mounting System | Teflon holders; stainless steel jaws/wires [8] [5] | Secures tissue between fixed points and force transducer |
| Force Transducer | Compact design with selectable force ranges [7] [5] | Measures isometric contraction/relaxation forces from tissue |
| Temperature Control | Water-jacketed chamber connected to recirculating heated water bath [6] | Maintains physiological temperature (typically 37°C) |
| Oxygenation System | Ultrafine bubbling frits; 95% Oâ‚‚/5% COâ‚‚ medical grade gas [5] [6] | Oxygenates buffer and maintains proper pH |
| Data Acquisition | Computer-based system with analog-to-digital converter and bridge amplifier [6] | Captures, visualizes, and records force measurements |
| Buffer Reservoir/Drainage | Built-in system for solution replacement [7] | Allows for changing bathing solution during experiments |
The tissue bath chamber itself is typically constructed from borosilicate glass for durability and chemical resistance, with available volumes ranging from 5 mL to 20 mL to accommodate different tissue sizes [5]. The chamber is water-jacketed and connected to a recirculating heated water bath that maintains the physiological temperature of 37°C [6]. Modern systems feature easy-to-remove Teflon tissue holders that allow researchers to mount samples outside the chamber, saving time and effort during experimental setup [5].
The oxygenation system employs ultrafine bubbling frits that provide superior oxygenation compared to simple needle valves, with medical-grade carbogen (95% Oâ‚‚/5% COâ‚‚) typically used to oxygenate the physiological salt solution and maintain proper pH [5] [6]. The force transduction system includes compact, sensitive isometric force transducers capable of detecting micro-Newton forces, with some systems offering selectable force ranges optimized for different tissue types [7] [8]. These transducers connect to computer-based data acquisition systems that capture, visualize, and record force measurements using specialized software [6].
Physiological Solutions and Research Reagents
The physiological environment within the organ bath is maintained using carefully formulated salt solutions and research-grade reagents. These solutions provide the ionic composition, nutrients, and buffering capacity necessary to sustain tissue viability throughout experiments.
Table 2: Research Reagent Solutions for Organ Bath Experiments
| Reagent/Solution | Composition | Function |
|---|---|---|
| Krebs-Henseleit Solution | NaCl, KCl, CaCl₂, KH₂PO₄, MgSO₄, NaHCO₃, Glucose [6] | Standard physiological salt solution for maintaining mammalian tissues |
| Tyrode's Solution | NaCl, KCl, CaCl₂, MgCl₂, NaH₂PO₄, NaHCO₃, Glucose [9] | Physiological solution for maintaining ionic balance and tissue viability |
| Carbogen Gas | 95% Oâ‚‚, 5% COâ‚‚ [6] | Oxygenates tissue and maintains physiological pH (7.4) |
| Pharmacological Agents | Acetylcholine, catecholamines, specific receptor agonists/antagonists [10] | Investigate concentration-response relationships and receptor characterization |
| Trypsin Inhibitor | Soybean-derived protease inhibitor [9] | Prevents autodigestion in pancreatic tissue studies |
| Caffeine/Halothane | 0.5-32 mM caffeine; 3% halothane [4] | Diagnostic agents for malignant hyperthermia susceptibility testing |
The composition of physiological salt solutions is critical for maintaining tissue function. A standard Krebs-Henseleit solution typically contains NaCl (118 mM), KCl (4.7 mM), CaCl₂ (2.5 mM), KH₂PO₄ (1.2 mM), MgSO₄ (1.2 mM), NaHCO₃ (25 mM), and glucose (11 mM) [6]. Modified Tyrode's solution used in pancreatic studies contains NaCl (136.9 mM), KCl (2.7 mM), CaCl₂ (1.8 mM), MgCl₂ (1.05 mM), NaH₂PO₄ (0.42 mM), EDTA (3 mM), NaHCO₃ (11.9 mM), and glucose (5.56 mM) [9]. These solutions provide the necessary ions for action potential generation, muscle contraction, and cellular signaling, while glucose serves as an energy substrate.
Pharmacological agents including acetylcholine, catecholamines, and specific receptor agonists/antagonists are applied to tissues to investigate concentration-response relationships and receptor characterization [10]. Specialized reagents such as trypsin inhibitor are employed in pancreatic studies to prevent autodigestion of tissue [9], while caffeine and halothane serve as diagnostic agents for malignant hyperthermia susceptibility testing in skeletal muscle preparations [4].
Experimental Protocols and Methodologies
General Tissue Preparation and Mounting
The following protocol outlines the standard procedure for preparing and mounting tissues in an organ bath system, with specific examples from vascular and gastrointestinal research:
Solution Preparation: Prepare 5 L of physiological salt solution (PSS), such as Krebs-Henseleit or Tyrode's solution, following established recipes [6]. Dissolve salts in HPLC-grade water, add calcium chloride solution last to prevent precipitation, and quantum sufficit to final volume.
System Setup: Preheat the tissue bath system to 37°C by turning on the recirculating heated water bath, ensuring components are connected in series with water flowing into each component at the lowest barbed connection and out at the highest [6]. Turn on the data acquisition system and force transducers at least 15 minutes prior to experimentation to equilibrate temperature and minimize thermal drift [6].
Calibration and Oxygenation: Launch data acquisition software and calibrate force transducers according to manufacturer instructions [6]. Connect the tissue bath system to a carbogen (95% Oâ‚‚/5% COâ‚‚) medical-grade gas cylinder, pressurize the system, and check for gas leaks. Fill tissue bath reservoirs with PSS, prime the system to remove air bubbles, and adjust aeration to ensure consistent solution oxygenation without causing tissue movement that disrupts recordings [6].
Tissue Dissection: Dissect tissues immediately after animal euthanasia and place directly into oxygenated PSS [6]. For vascular tissues like rat thoracic aorta, carefully sever all connections to the aorta, dissect it from the spine, and place it in a dissection dish containing PSS with a black silastic foundation for contrast [6].
Tissue Preparation: Clean the aorta of perivascular adipose tissue and extraneous material until it appears white and fibrous [6]. Cut the cleaned aorta into rings approximately 3-5 mm in width using small vannas scissors. Mount aortic rings on tissue hooks, ensuring one hook has a small knotted loop of silk for attachment to a fixed rod, while the other has a 10-4 cm long suture for tying to the force transducer [6].
Tissue Mounting: With tissue baths filled with warmed, aerated PSS, tie one hook on the tissue preparation to the peg on a stainless steel rod and place this end into the tissue bath chamber [6]. Connect the rod to a ring stand and tie the other suture to the force transducer, leaving slack in the suture between the tissue and transducer [6].
Tissue Equilibration: Adjust the micrometer on the force transducer to remove slack and apply a predetermined pre-tension to the tissue [6]. Allow tissues to equilibrate for 60-120 minutes with periodic washing every 15-20 minutes until a stable baseline is achieved [6].
Diagram 1: Tissue Preparation and Setup Workflow
Viability Testing and Experimental Execution
Before proceeding with experimental protocols, tissue viability must be confirmed:
Viability Assessment: Following the equilibration period, test tissue viability by administering a known contractile agent. For vascular tissues, potassium chloride (KCl) at 60-80 mM is commonly used to elicit a sustained contraction [6]. A viable preparation should generate a robust, sustained contraction that plateaus within minutes.
Experimental Execution: Once viability is confirmed, proceed with the specific experimental protocol. This may involve generating dose-response curves by cumulative addition of increasing concentrations of pharmacological agents, with each concentration allowed to reach a steady-state response before adding the next [6]. Alternatively, tissues may be exposed to single concentrations with washing and recovery between applications.
Electrical Field Stimulation: For studies of nerve-mediated responses, tissues may be subjected to electrical field stimulation (EFS) using parallel electrodes embedded in the tissue bath [10]. EFS parameters typically include pulse durations of 0.5-1 ms, supramaximal voltage, and frequencies ranging from 1-50 Hz, delivered in trains of several seconds duration [10].
Data Collection and Analysis: Record all contractile responses using data acquisition software. For dose-response curves, normalize responses as a percentage of the maximum contractile response to a reference agonist [6]. Analyze EFS responses in the presence and absence of neural blockers such as tetrodotoxin (TTX) to confirm neurogenic origins [10].
Specialized Applications and Protocols
Malignant Hyperthermia Diagnostic Testing
Organ bath systems play a critical role in the clinical diagnosis of malignant hyperthermia (MH) susceptibility using the caffeine-halothane contracture test:
Muscle Biopsy: Obtain a fresh muscle sample (3-5 cm long, 1-1.5 cm diameter) from the vastus lateralis or vastus medialis under non-triggering anesthesia [4].
Bundle Preparation: Using a dissecting microscope, prepare a minimum of six small muscle bundles (approximately 2 mm diameter, 3-5 cm length) [4].
Mounting and Viability: Mount muscle bundles in experimental chambers where they contract via electrical stimulation with supramaximal stimulation (1 ms pulse width). A viable bundle must elicit a minimum of 1 g of twitch force [4].
Halothane Challenge: Introduce 3% halothane into the experimental chamber. MH-susceptible muscle will contract more rigorously (twitch potentiation) and elicit a contracture (sustained force generation >0.7 g) [4].
Caffeine Challenge: Expose additional muscle bundles to increasing bolus doses of caffeine to obtain concentrations of 0.5, 1, 2, 4, 8, and 32 mM. MH-susceptible tissue will elicit twitch potentiation and contractures (≥0.2 g contracture at ≤2 mM caffeine) [4].
This protocol is recognized as the gold standard for clinical diagnosis of MH susceptibility, with reported sensitivity of 97% and specificity of 78% according to the North American Malignant Hyperthermia Registry [4].
Pancreatic Insulin Secretion Studies
Organ bath techniques have been adapted for studying endocrine function in pancreatic tissues:
Pancreas Preparation: Remove the whole pancreas from rats and immerse in modified Tyrode's solution [9]. Divide the pancreas into three parts: the right lobe (duodenal side), left lobe (splenic side), and residual pancreas.
Mounting and Equilibration: Wrap each lobe in nylon mesh and suspend in a 5-mL organ bath with modified Tyrode's solution at 37°C under 95% O₂/5% CO₂ atmosphere [9]. Equilibrate for 120 minutes with fresh replacement of solution every 20 minutes.
Sample Collection: After equilibration, collect incubation medium (2.3 mL) every 20 minutes for 60-80 minutes [9]. To prevent autodigestion, add trypsin inhibitor (0.1 mg/mL) to the solution for some preparations.
Hormone Measurement: Determine insulin concentrations in collected solutions using ELISA kits [9]. Measure amylase activity as an indicator of exocrine pancreas function using dry-chemistry analyzers.
Data Analysis: Express insulin outflow values relative to the weight of the intact pancreas preparation. Compare secretion patterns between different pancreatic lobes and experimental conditions [9].
Diagram 2: Signal Transduction to Tissue Response Pathway
Data Acquisition, Analysis, and Interpretation
Modern organ bath systems employ sophisticated data acquisition and analysis methodologies to extract meaningful pharmacological parameters from experimental data:
Data Acquisition: Computer-based systems with analog-to-digital converters and bridge amplifiers capture force measurements at appropriate sampling rates (typically 10-40 Hz) [6]. Specialized software such as LabChart provides platforms for integrating recordings from multiple devices simultaneously [11].
Dose-Response Analysis: Data from cumulative addition of pharmacological agents are used to construct dose-response curves, typically graphed on a semilog plot yielding sigmoidal curves [4]. These curves are often fitted to mathematical models such as the Hill model to derive pharmacological parameters including ECâ‚…â‚€ (concentration producing 50% of maximal response) and E_max (maximal response) [4].
Signal Processing: Software modules enable real-time signal processing, including baseline adjustment, noise filtering, and integration of contractile responses [11]. The Dose-Response Module in LabChart can automate the derivation of dose-response curves and calculation of ECâ‚…â‚€ values [11].
Statistical Analysis: Experimental results are analyzed using appropriate statistical tests with significance typically set at p<0.05. Data are often normalized to control responses or tissue weight to enable comparisons across preparations [9] [10].
Table 3: Quantitative Parameters in Organ Bath Research
| Parameter | Typical Values/Ranges | Experimental Context |
|---|---|---|
| Tissue Pre-tension | 1-2 g (vascular); 0.5-1 g (other smooth muscle) | Optimal resting force for contractile studies |
| Equilibration Time | 60-120 minutes | Tissue stabilization before experimental protocol |
| Caffeine Threshold | ≥0.2 g contracture at ≤2 mM [4] | Diagnostic for malignant hyperthermia susceptibility |
| Halothane Threshold | >0.7 g contracture at 3% [4] | Diagnostic for malignant hyperthermia susceptibility |
| Electrical Stimulation | 1 ms pulse width, supramaximal voltage [4] | Standard for viability testing in muscle bundles |
| Twitch Force Minimum | 1 g [4] | Viability threshold for muscle bundles |
The organ bath technique continues to evolve with technological advancements while maintaining its fundamental principles. Modern systems offer enhanced precision, automation, and integration capabilities that expand the applications of this classic methodology in both basic research and clinical diagnostics [7] [11]. By providing a bridge between cellular studies and whole-animal experiments, organ bath systems remain an essential tool for understanding tissue function and developing novel therapeutic approaches.
Maintaining the viability and physiological function of tissues ex vivo is a cornerstone of pharmacological and physiological research. Isolated tissue bath experiments, a methodology developed over a century ago, remain the gold standard for investigating drug effects, disease mechanisms, and tissue function outside the living organism [4]. The critical factor determining the success of these experiments is the ability to replicate a physiological environment that sustains tissue health for the duration of the study. This involves precise physiological solutions to maintain osmotic balance and provide nutrients, coupled with stringent environmental controls for temperature and oxygenation [4] [12]. Failures in these fundamental aspects can lead to rapid tissue degradation, compromising data integrity and leading to erroneous conclusions. This application note provides detailed protocols and evidence-based guidance for optimizing these conditions to ensure the reliability and reproducibility of ex vivo research outcomes.
The Scientist's Toolkit: Essential Reagents and Materials
Successful ex vivo tissue experimentation requires a foundational set of reagents and materials designed to preserve tissue integrity and function.
Table 1: Key Research Reagent Solutions and Essential Materials
| Item Name | Function/Explanation | Example/Composition |
|---|---|---|
| Physiological Salt Solutions | Maintains osmotic pressure, pH, and provides essential ions (e.g., Naâº, Kâº, Ca²âº) for normal cellular function and electrophysiology. | Krebs-Henseleit solution, Ringer's solution. |
| Energy Substrates | Provides metabolic fuel (e.g., glucose, pyruvate) to support tissue viability and contractile work during extended experiments. | Typically included in physiological salt solutions. |
| Oxygen-Carbon Dioxide Mixture | Oxygenates the solution for aerobic respiration; COâ‚‚ is used in conjunction with a bicarbonate buffer to maintain physiological pH (typically 7.4). | Carbogen (95% Oâ‚‚, 5% COâ‚‚). |
| p38 Inhibitor | A chemical additive that reduces detrimental cellular stress responses in culture, helping to preserve the long-term functionality of sensitive cells like hematopoietic stem and progenitor cells [13]. | Specific p38 pathway inhibitors. |
| Prebiotics & Specialized Media | Used in complex ex vivo systems to support the host's natural microbiome, which is crucial for modeling the physiology of tissues like the gut [12]. | Media with specific prebiotic components. |
| Microfluidic Chamber System | An advanced tool that provides continuous flow of fresh media, controls shear stress, and can integrate sensors for real-time monitoring of tissue health (e.g., Transepithelial Electrical Resistance - TEER) [12]. | Custom-designed chambers with integrated electrodes. |
| Atovaquone D4 | Atovaquone D4, MF:C22H19ClO3, MW:370.9 g/mol | Chemical Reagent |
| Lignoceric acid-d47 | Lignoceric acid-d47, MF:C24H48O2, MW:415.9 g/mol | Chemical Reagent |
Core Quantitative Data for Experimental Design
The tables below consolidate critical quantitative data for designing and executing ex vivo experiments, from solution preparation to viability assessment.
Table 2: Standard Calculations for Solution and Drug Preparation
| Calculation Type | Formula/Example | Application Note |
|---|---|---|
| Final Bath Concentration | (Volume of Stock Added / Bath Volume) × Stock Concentration.Example: Adding 30 μL of 1 mM d-TC to a 25 mL bath: (0.03 mL / 25 mL) × 1 mM = 1.2 μM [14]. | Ensures accurate and reproducible drug dosing in organ baths. Using molar units throughout is recommended to prevent errors [14]. |
| Solution Percentage to Molarity | (Percentage × 10) / Molecular Weight.Example: 0.9% NaCl: (0.9 × 10) / 58.44 = 0.154 M [14]. | Critical for preparing physiological saline solutions with correct osmolarity. |
| Serial Dilution for Stock Solutions | Prepare a concentrated stock first, then dilute. Example: For 10 mL of 50 μM ACh (MW 181.7), first make 10 mL of 5 mM (weigh 9 mg), then dilute 0.1 mL of this stock in 9.9 mL [14]. | Necessary when the required mass of compound is too small to weigh accurately on standard balances. |
Table 3: Key Parameters for Maintaining Tissue Viability
| Parameter | Target/Threshold | Significance |
|---|---|---|
| Tissue Viability Duration | Up to 72 hours in advanced microphysiological systems [12]. | Enables longer-term studies on chronic effects and slow-acting compounds. |
| Diagnostic Force Threshold | >0.7 g contracture from 3% halothane; ⩾0.2 g contracture at ⩽2 mM caffeine [4]. | Diagnostic thresholds for Malignant Hyperthermia susceptibility in fresh muscle biopsies. |
| Tissue Sample Dimensions (Muscle Biopsy) | 1–3 mm diameter; >3 cm length [4]. | Standardized size ensures viability and uniform experimental responses. |
| Transepithelial Electrical Resistance (TEER) | Real-time, continuous measurement. | A quantitative, real-time measure of barrier tissue integrity (e.g., in gut models) [12]. |
Detailed Experimental Protocols
Protocol 1: Setting Up a Basic Isolated Tissue Bath System
This protocol outlines the fundamental steps for preparing an isolated tissue bath, a workhorse for functional contractility studies.
Materials:
- Physiological salt solution (e.g., Krebs-Henseleit)
- Organ bath with temperature control and oxygenation
- Force transducer and data acquisition system
- Surgical tools for dissection
Method:
- Solution Preparation: Prepare the physiological salt solution, bubble continuously with carbogen (95% O₂ / 5% CO₂), and warm to 37°C.
- Tissue Dissection: Excise the target tissue (e.g., ileum, vas deferens, muscle bundle) from the animal. Handle the tissue gently to minimize trauma.
- Mounting: Suspend the tissue in the organ bath between an anchor point and an isometric force transducer. Apply a resting tension appropriate for the tissue type.
- Equilibration: Allow the tissue to equilibrate for 30-60 minutes, with periodic washing, until a stable baseline is achieved.
- Experimental Intervention: Begin the experimental protocol, such as cumulative addition of agonists or electrical field stimulation, while recording contractile responses.
The workflow for this core protocol is summarized in the following diagram:
Protocol 2: Caffeine-Halothane Contracture Test for Malignant Hyperthermia (MH) Diagnosis
This protocol details the specific steps for the clinical diagnosis of MH susceptibility, demonstrating a highly specialized application of tissue bath methodology [4].
Materials:
- Fresh muscle biopsy (vastus lateralis or medialis)
- Multiple tissue baths running in parallel
- Halothane (3% vol/vol) and caffeine stock solutions (0.5, 1, 2, 4, 8, 32 mM)
- Electrical stimulation apparatus
Method:
- Biopsy Collection: Obtain a fresh muscle biopsy (1–3 mm diameter, >3 cm length) under non-triggering anesthesia.
- Bundle Preparation: Under a dissecting microscope, prepare a minimum of six muscle bundles.
- Viability Check: Mount bundles in tissue baths and apply electrical stimulation. A viable bundle must elicit a minimum of 1 g of twitch force.
- Halothane Challenge: Expose bundles to 3% halothane for 10 minutes. A contracture >0.7 g indicates MH susceptibility.
- Caffeine Challenge: Expose separate bundles to incrementally increasing caffeine concentrations (0.5 to 32 mM). A contracture ≥0.2 g at ≤2 mM caffeine indicates MH susceptibility.
- Diagnosis: A positive result in either test confirms a diagnosis of MH susceptibility.
The logic of this diagnostic protocol is illustrated below:
Protocol 3: Real-Time TEER Measurement in an Ex Vivo Microphysiological System
This protocol describes an advanced setup for monitoring barrier tissue health in real-time over extended durations [12].
Materials:
- Microfluidic chamber system with integrated electrodes
- Peristaltic or syringe pumps for continuous flow
- Bicarbonate-buffered media with prebiotics
- Data acquisition system for continuous TEER recording
Method:
- Chamber Priming: Sterilize the microfluidic chamber and prime both the luminal and serosal sides with pre-warmed, oxygenated media.
- Tissue Mounting: Position the tissue explant (e.g., mouse colon) within the chamber, ensuring a leak-proof seal that separates the two fluidic compartments.
- Flow Initiation: Initiate continuous, low-flow media circulation on both sides of the tissue to deliver nutrients and create physiological oxygen gradients.
- Baseline TEER: Begin continuous TEER measurements to establish a stable baseline barrier integrity.
- Experimental Perturbation: Introduce the experimental stimulus (e.g., collagenase, low pH media, drug candidate).
- Continuous Monitoring: Record TEER values at user-defined intervals throughout the experiment (up to 72 hours) to track dynamic changes in barrier function.
Advanced Considerations for Environmental Control
Beyond the basic setup, several advanced factors are critical for maintaining viability. The shift from static culture to continuous flow in microphysiological systems is a key advancement. It prevents the buildup of metabolic waste, ensures consistent nutrient delivery, and can introduce physiologically relevant shear stress, significantly extending tissue viability to 72 hours or more [12]. Furthermore, the composition of the media is vital. For intestinal models, including prebiotics helps maintain the natural microbiome, which is essential for an accurate physiological model [12]. Finally, integrating real-time monitoring like TEER provides a quantitative measure of tissue health and barrier function without the need to terminate the experiment, offering powerful insights into the kinetics of tissue response [12].
The isolated tissue bath technique has been a cornerstone of pharmacological and physiological research for over a century, remaining an indispensable tool for evaluating concentration-response relationships in contractile tissues [6] [4]. This methodology allows living tissues to function as integrated systems, providing physiologically relevant data on contraction and relaxation that closely mirrors in vivo function [15]. The technique's versatility enables researchers to study a wide array of tissues, from vascular rings and tracheal smooth muscle to gastrointestinal strips and skeletal muscle preparations [3] [16]. These applications facilitate critical research in drug development, disease pathophysiology, and receptor characterization, forming the basis of therapies for hypertension, asthma, gastrointestinal disorders, and numerous other conditions [15]. This article provides detailed application notes and protocols for utilizing diverse tissues in organ bath experiments, framed within the broader context of isolated tissue research methodology.
Fundamental Principles and Historical Significance
Core Methodology and Advantages
The isolated tissue bath system maintains living tissues in an oxygenated physiological salt solution at controlled temperatures, allowing measurement of isometric contraction and relaxation in response to pharmacological agents or electrical stimulation [6] [15]. The primary advantage of this technique is its preservation of integrated tissue function, incorporating the complete sequence from drug-receptor interaction and signal transduction to second messenger generation and ultimate physiological response [15]. This systems-level approach provides pharmacological data on efficacy and potency that are more meaningful than isolated cellular assays, bridging the gap between molecular pharmacology and whole-animal physiology [2].
Historical Research Contributions
The tissue bath technique has facilitated numerous landmark discoveries in pharmacology and physiology. Otto Loewi's famous 1921 experiment demonstrating chemical neurotransmission used frog hearts in tissue baths to identify "vagusstoff" (later identified as acetylcholine), for which he shared the 1936 Nobel Prize [4] [16]. More recently, Robert Furchgott's work with aortic strips in organ baths led to the discovery of endothelium-derived relaxing factor (EDRF), subsequently identified as nitric oxide [4] [16]. These historical contributions underscore the technique's enduring value in basic research and drug discovery.
Tissue-Specific Applications and Protocols
Vascular Tissue Applications
Protocol: Rat Thoracic Aorta Ring Preparation
- Tissue Source: Thoracic aorta from Sprague-Dawley or Wistar rats (250-400g) [6] [15]
- Dissection Procedure:
- Anesthetize rat according to institutional IACUC guidelines (e.g., 70 mg/kg pentobarbital intraperitoneal) [6] [15]
- Create pneumothorax by incision along diaphragm, then bisect sternum to expose thoracic cavity
- Locate aorta along spinal column, sever connections to surrounding tissues
- Cut aorta perpendicular to spine at diaphragm level, gently dissect toward heart
- Immediately place aorta in oxygenated physiological salt solution (PSS) at 4°C
- Tissue Preparation:
- Cannulate aorta with guide wire fastened in silastic dissection dish
- Carefully remove perivascular adipose and connective tissue using fine scissors and forceps
- Cut cleaned aorta into rings 3-5mm in width using sharp scissors
- Mount rings on paired tissue hooks with silk sutatures
- Mounting and Equilibration:
- Attach one suture to stationary rod and immerse in tissue bath containing oxygenated PSS at 37°C
- Connect other suture to force transducer with slack
- Gradually increase passive tension to optimal level (4g for rat aorta) using micrometer
- Equilibrate for 60-90 minutes with periodic PSS changes until stable baseline achieved
- Viability Assessment: Validate tissue responsiveness with high-potassium solution or receptor agonist (e.g., phenylephrine for α1-adrenoceptors) [2]
Table 1: Vascular Tissue Applications in Organ Bath Systems
| Tissue Type | Common Applications | Optimal Tension | Key Agonists/Antagonists | Research Applications |
|---|---|---|---|---|
| Rat Thoracic Aorta | Vascular reactivity studies | 4g [15] | Phenylephrine (α1-agonist), Acetylcholine (endothelium-dependent relaxation) [2] | Hypertension research, endothelial function |
| Murine Mesenteric Arteries | Small vessel pharmacology | Tissue-dependent [6] | Norepinephrine, Serotonin | Microvascular disorders, metabolic syndrome |
| Porcine Coronary Arteries | Coronary heart disease research | Tissue-dependent | Bradykinin, Substance P | Atherosclerosis, vasospasm |
| Human Epigastric Arteries | Translational vascular research | Tissue-dependent | Various receptor-specific agents | Patient-specific pharmacology |
Gastrointestinal Smooth Muscle Applications
Protocol: Rat Colon Smooth Muscle Strip Preparation
- Tissue Source: Colon from Wistar rats (250-350g) [17]
- Dissection Procedure:
- Euthanize rats according to ethical guidelines, open abdominal cavity
- Identify colon, carefully dissect from mesenteric attachments
- Remove fecal contents by gentle flushing with oxygenated PSS
- Pin tissue in silastic-lined dissection dish containing oxygenated PSS
- Strip Preparation:
- For longitudinal strips: Carefully separate longitudinal muscle layer along natural orientation
- For circular strips: Cut parallel to circular muscle fibers
- Prepare strips approximately 2-3mm wide and 10-15mm long
- Attach silk sutures to both ends of each strip
- Mounting and Experimental Setup:
- Mount strips vertically in tissue baths with oxygenated PSS at 37°C
- Apply optimal resting tension (typically 1-2g for colonic strips)
- Equilibrate for 60 minutes with buffer changes every 15 minutes
- Validate tissue viability with acetylcholine (10^-9-10^-5 M) or electrical field stimulation [17]
Table 2: Gastrointestinal Tissue Applications in Organ Bath Systems
| Tissue Type | Common Applications | Stimulation Methods | Key Agonists/Antagonists | Research Applications |
|---|---|---|---|---|
| Rat Colon Strips | GI motility disorders | Electrical Field Stimulation (0.1-20 Hz), Acetylcholine [17] | Atropine (muscarinic antagonist) | Chemotherapy-induced dysmotility, IBS |
| Guinea Pig Ileum | Enteric nervous system function | EFS, Receptor-specific agonists | Histamine, Serotonin, Opioids | Enteric neuropathy, drug absorption |
| Rat Trachea | Respiratory pharmacology | EFS, Potassium depolarization | Methacholine, Histamine [2] | Asthma, COPD therapeutic development |
| Porcine Ileum | Comparative pharmacology | Receptor-specific activation | Various spasmogens | Translational GI research |
Specialized Applications
Malignant Hyperthermia Diagnostic Testing
The caffeine-halothane contracture test represents a critical clinical application of tissue bath methodology for diagnosing susceptibility to malignant hyperthermia (MH) [4]. This standardized protocol requires fresh human skeletal muscle biopsies (1-3mm diameter, >3cm length) from vastus lateralis or medialis muscles. Muscle bundles are mounted in tissue baths and exposed to caffeine (0.5, 1, 2, 4, 8, 32mM) and halothane (3%) following North American MH Group protocols. Diagnostic thresholds include >0.7g contracture with halothane and ≥0.2g contracture at ≤2mM caffeine, with reported 97% sensitivity and 78% specificity [4].
Chemotherapy-Induced Neuropathy Assessment
Organ bath studies using colon strips from rats treated with chemotherapeutic agents have revealed differential effects on enteric neuromuscular function. Research demonstrates that cisplatin significantly decreases responses of both longitudinal and circular smooth muscle to electrical field stimulation, while vincristine tends to increase them non-significantly [17]. These findings illustrate how tissue bath methodology can elucidate mechanisms underlying chemotherapy-induced gastrointestinal disorders.
Experimental Design and Technical Considerations
Solution Preparation and System Setup
- Physiological Salt Solution (PSS): Prepare 5L of standardized PSS containing (in mM): NaCl 118, KCl 4.7, CaCl₂ 1.6, MgSO₄ 1.2, KH₂PO₄ 1.2, NaHCO₃ 25, Glucose 11 [6] [15]
- System Preparation:
- Preheat recirculating water bath to 37°C with serial connection to water-jacketed components
- Power force transducers 15 minutes pre-experiment for thermal equilibration
- Calibrate transducers according to manufacturer specifications
- Connect to 95% Oâ‚‚/5% COâ‚‚ medical gas with proper pressurization
- Fill tissue baths with oxygenated PSS, remove air bubbles from system
- Verify consistent aeration without disruptive tissue movement [6] [15]
Data Acquisition and Analysis
Modern tissue bath systems incorporate computer-based data acquisition with specialized software for real-time visualization and analysis [6]. Key pharmacological parameters including ECâ‚…â‚€, ICâ‚…â‚€, maximum effect (E_max), and Hill coefficient can be calculated from concentration-response curves [4] [16]. Data is typically acquired at 1-10Hz sampling frequency, with appropriate filtering to reduce noise while preserving contractile signal integrity.
Technological Innovations and Future Directions
Multi-Well Organ Bath (MuWOB) Technology
Recent innovations include the development of multi-well organ bath systems that adapt traditional organ bath methodology to standard 96-well plates [2]. This technology uses optical methods to monitor contractile responses in small volumes (≈100µl/well), dramatically reducing drug requirements and enabling high-throughput screening. MuWOB systems incorporate bi-telecentric optics for zenith observation and automated liquid handling, bringing organ bath technology into the realm of modern drug discovery platforms [2].
Video Spatiotemporal Mapping
Advanced video spatiotemporal mapping techniques provide enhanced resolution of contractile activity through D-maps (diameter change), L-maps (longitudinal strain rate), and A-maps (area strain rate) [18]. These methods allow precise quantification of contraction frequency, propagation speed, and spatial patterns without physical contact with tissues, offering advantages for studying complex motility patterns in gastrointestinal and other hollow organs [18].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Organ Bath Studies
| Reagent/Material | Composition/Type | Function | Application Notes |
|---|---|---|---|
| Physiological Salt Solution (PSS) | NaCl, KCl, CaCl₂, MgSO₄, KH₂PO₄, NaHCO₃, Glucose [6] [15] | Maintain physiological ionic environment | Bubble with 95% O₂/5% CO₂; maintain at 37°C |
| Receptor Agonists | Phenylephrine, Acetylcholine, Histamine, Serotonin [2] [17] | Activate specific receptors to elicit contraction/relaxation | Prepare fresh stock solutions; serial dilution for concentration-response |
| Receptor Antagonists | Prazosin, Atropine, Various selective blockers [2] [17] | Inhibit specific receptor responses | Pre-incubate for 15-30 minutes to establish blockade |
| Calcium Modulators | Isradipine, Nifedipine, Caffeine [4] [2] | Modify calcium influx or intracellular release | Useful for characterizing contraction mechanisms |
| Electrical Field Stimulation Electrodes | Platinum or stainless steel electrodes | Direct neural stimulation | Typically 0.1-20 Hz, 1ms pulse width [17] |
| Force Transducers | Isometric force transducers with bridge amplifiers [6] [15] | Measure contractile force | Calibrate before each experiment; allow thermal equilibration |
| D-erythro-sphinganine-d7 | D-erythro-sphinganine-d7, MF:C18H39NO2, MW:308.6 g/mol | Chemical Reagent | Bench Chemicals |
| Canagliflozin D4 | Canagliflozin D4, MF:C24H25FO5S, MW:448.5 g/mol | Chemical Reagent | Bench Chemicals |
Troubleshooting and Methodological Considerations
Common Technical Issues and Solutions
- Poor Tissue Viability: Ensure rapid tissue dissection with minimal stretching or trauma; maintain proper oxygenation and temperature during preparation [6] [15]
- Unstable Baselines: Verify consistent temperature control; check for gas bubble interference; ensure proper tissue oxygenation [6]
- Inconsistent Responses: Validate drug solution preparation and delivery; confirm adequate equilibration time between interventions [15]
- Signal Artifacts: Check transducer calibration; minimize mechanical vibration; ensure secure tissue mounting [6]
Optimal Experimental Design Practices
- Include appropriate positive and negative controls in each experimental series
- Utilize paired tissue samples from same animal when possible to reduce variability
- Employ randomized drug addition sequences to minimize order effects
- Conduct power analysis preliminary to determine appropriate sample sizes
- Adhere to 3R principles (Replacement, Reduction, Refinement) in animal use [17]
The diverse applications of isolated tissue bath methodology, from vascular rings to gastrointestinal smooth muscle, continue to make this century-old technique indispensable in modern pharmacological research and drug development. While molecular approaches provide target-specific information, organ bath studies offer integrated physiological responses that more accurately predict in vivo drug effects. Recent technological innovations, including multi-well organ baths and advanced imaging techniques, are enhancing the throughput and analytical capabilities of this classic methodology. As drug discovery increasingly recognizes the value of physiological systems in lead optimization, tissue bath applications remain essential for evaluating therapeutic efficacy and safety across diverse tissue types.
Executing a Successful Organ Bath Experiment: A Step-by-Step Protocol from Tissue Dissection to Data Acquisition
Successful organ bath experiments with isolated tissues hinge on the quality of the initial dissection and preparation. Minimizing trauma during these stages is paramount to preserving the innate physiological properties of the tissue, thereby ensuring the validity and reliability of subsequent experimental data. Trauma during dissection can induce cellular damage, alter receptor integrity, and provoke inflammatory responses that fundamentally skew pharmacological and physiological assessments. This application note details established protocols designed to safeguard tissue viability and function from the moment of excision through to mounting in the organ bath, framed within the context of preparing tissues for contractile studies.
Fundamental Principles of Trauma-Minimizing Dissection
The overarching goal during dissection is to isolate the target tissue with minimal mechanical, chemical, and ischemic stress. Adherence to the following core principles is critical:
- Maintain Tissue Hydration: Tissues must never be allowed to dry out. Continuous immersion or frequent irrigation with an appropriate, oxygenated physiological salt solution (PSS) is essential to prevent desiccation, which rapidly compromises cellular integrity [4].
- Utilize Sharp, Precision Instruments: The use of sharp scalpels and fine scissors is non-negotiable. Sharp instruments create clean cuts with minimal crush injury and tissue dragging, which is a significant source of trauma. Blunt instruments exert excessive force, tearing and crushing cells at the incision site [19].
- Employ Blunt Dissection for Separation: Where feasible, a blunt dissection technique should be used to separate the target tissue from surrounding connective tissue and fascia. This technique, which involves using a pliable, blunt metal device or forceps to gently separate tissue planes along natural cleavage lines, reduces the risk of accidental cutting of nerves and blood vessels and minimizes trauma to the tissue of interest [19].
- Minimize Direct Handling: Direct manipulation of the tissue specimen with forceps should be avoided. When handling is necessary, grasp only the connective tissue ends or use soft, rubber-tipped forceps. A preferable method is to use a small brush to support the tissue during transfer.
- Ensure Rapid Transfer to Oxygenated PSS: Immediately upon excision, the tissue should be transferred to a beaker containing ice-cold, oxygenated (typically with 95% Oâ‚‚ / 5% COâ‚‚) PSS. The cold temperature reduces the metabolic rate of the tissue, protecting it from ischemic damage during the dissection and preparation phase [4].
Detailed Experimental Protocols
General Workflow for Isolation of Muscular Tissue
The following workflow outlines the key stages for preparing a viable tissue specimen, such as skeletal or smooth muscle, for organ bath studies.
Protocol 1: Preparation of Skeletal Muscle Bundles for Contracture Testing
This protocol, adapted from the standardized North American Malignant Hyperthermia Group protocol, is the gold standard for preparing viable human skeletal muscle for caffeine-halothane contracture tests [4].
Objective: To obtain viable skeletal muscle bundles for the diagnosis of Malignant Hyperthermia (MH) susceptibility. Tissue Source: Vastus lateralis or vastus medialis muscle biopsy. Reagents & Equipment:
- Physiological Salt Solution (PSS, e.g., Krebs-Ringer solution), ice-cold and oxygenated with Carbogen.
- Dissecting microscope.
- Sharp scalpels, fine forceps, and iris scissors.
- Aeration tubing with fine pores.
Methodology:
- Biopsy Handling: The fresh muscle sample, obtained under non-triggering anesthesia, must be processed immediately. The minimum sample size is 3–5 cm in length and 1–1.5 cm in diameter [4].
- Gross Dissection: Transfer the biopsy to a dissection dish containing ice-cold, oxygenated PSS. Using fine forceps and a sharp scalpel, carefully remove any obvious fat or connective tissue.
- Bundle Preparation: Under a dissecting microscope, meticulously dissect a minimum of six small muscle bundles. Each bundle should measure approximately 1–3 mm in diameter and 3–5 cm in length [4].
- Trauma Minimization:
- Do not grasp the contractile body of the bundle with forceps.
- Make clean, single-stroke cuts with sharp instruments.
- Ensure the bundles remain submerged and oxygenated throughout the dissection process.
- Viability Check: Mount the bundles vertically in the tissue baths. A viable muscle bundle must elicit a minimum of 1 g of twitch force in response to electrical stimulation (e.g., supramaximal stimulation, 1 ms pulse width) to be deemed suitable for diagnostic testing [4].
Protocol 2: Blunt Dissection for Tissue Expander Placement (Adapted for Organ Bath)
While developed for surgical insertion of tissue expanders in curved anatomical regions, the principles of this blunt dissection technique are highly applicable to isolating delicate tissues from surrounding fascia [19].
Objective: To create a tissue plane and separate a target tissue with minimal sharp dissection. Application: Useful for isolating tissues like blood vessels, nerves, or thin muscle sheets where sharp dissection poses a high risk of transection. Reagents & Equipment:
- Pliable, blunt metal dissection device (e.g., Krauze forceps).
- Tumescent solution (e.g., saline with adrenaline and tranexamic acid) or PSS for hydrodissection.
Methodology:
- Hydrodissection: Inject a small volume of ice-cold PSS into the tissue plane surrounding the target structure. This helps to physically separate the tissues and create space for the blunt instrument [19].
- Incision: Make a small initial incision to access the tissue plane.
- Blunt Tunneling: Insert the pliable, blunt device through the incision. Gently advance it within the hydrodissected tissue layer, creating a closed tunnel. As the dissection progresses, the device can be flexed externally to navigate curved anatomy, facilitating the separation of tissue layers and creating a suitable pocket [19].
- Final Isolation: Once the target tissue is freed from its attachments, it can be cleanly transected at its ends with sharp scissors with minimal collateral damage.
Key Parameters and Reagent Solutions
Adherence to precise parameters and the use of defined reagent solutions are critical for success. The tables below summarize essential quantitative data and materials.
Table 1: Key Quantitative Parameters for Tissue Preparation
| Parameter | Specification | Rationale & Context |
|---|---|---|
| Muscle Bundle Dimensions | 1–3 mm diameter; 3–5 cm length [4] | Ensures optimal diffusion of oxygen and nutrients; standard for contracture testing. |
| Dissection Solution Temperature | 0–4 °C (Ice-cold) [4] | Slows metabolic rate, reducing ischemic damage during preparation. |
| Solution Osmolarity | ~290-310 mOsm (Iso-osmotic) | Prevents osmotic shock and associated cell swelling or shrinkage. |
| Viability Threshold (Twitch Force) | >1 g [4] | Minimum contractile response indicating viable skeletal muscle for MH diagnostic testing. |
| Prestretch Tension | Tissue-dependent (e.g., 1-2 g for rodent ileum) | Applies optimal preload to achieve the peak of the length-tension relationship. |
| Equilibration Time | 60-90 minutes | Allows tissue to stabilize metabolically and mechanically in the bath environment. |
Table 2: Essential Research Reagent Solutions for Tissue Dissection & Bath Studies
| Reagent / Material | Function / Explanation |
|---|---|
| Physiological Salt Solution (PSS) | Mimics extracellular fluid; provides ions for electrophysiological stability and nutrients (e.g., glucose) [4]. |
| Carbogen (95% Oâ‚‚ / 5% COâ‚‚) | Standard gas for oxygenation and pH maintenance (via bicarbonate buffer) in mammalian tissue baths [4]. |
| Low Concentration Formaldehyde (e.g., 4%) with Glycerol/Ethanol | Preservation solution for long-term specimen storage; formaldehyde cross-links proteins, while glycerol maintains tissue pliability [20]. |
| Caffeine & Halothane | Diagnostic agents used in contracture testing to identify Malignant Hyperthermia susceptibility by challenging skeletal muscle calcium regulation [4]. |
| Colored Silicone (Red/Blue) | Perfusion material for injecting arterial and venous systems in anatomical specimens to enhance visual identification of vasculature during dissection [20]. |
Troubleshooting and Quality Control
A systematic approach to quality control is necessary to identify and mitigate issues arising from tissue trauma.
The most reliable indicator of successful trauma-minimized preparation is a stable, robust baseline and a reproducible response to known agonists. Tissues that fail to meet predefined viability criteria, such as the >1 g twitch force for skeletal muscle, should be excluded from experimental analysis [4].
Mounting Techniques and Setting Optimal Passive Tension
Within the framework of a comprehensive thesis on organ bath experimentation, the precise mounting of isolated tissues and the subsequent application of optimal passive tension are critical foundational steps. These procedures are paramount for maintaining tissue viability and ensuring the physiological relevance of collected data. Proper technique ensures that the tissue is responsive and that contractile forces are accurately measured, forming the bedrock of reliable pharmacological and physiological research [6]. This document details established protocols and application notes for these essential processes, serving as a practical guide for researchers in drug development and basic science.
Fundamental Principles of Passive Tension
The Role of Passive Tension in Tissue Function
In skeletal muscle, passive tension arises when the tissue is stretched beyond its slack length and is borne by both intracellular proteins, such as titin, and the collagenous structures of the extracellular matrix (ECM) [21] [22]. The relative contribution of these components is scale-dependent; while titin dominates at the single-fiber level, the ECM becomes the dominant contributor to passive tension at the whole-muscle level [22]. The passive mechanical properties of a tissue are not merely structural; they have significant functional relevance, influencing factors such as joint mobility and the range of motion, and they adapt in response to various conditions including training, aging, and disease [21].
Quantitative Benchmarks for Different Tissues
Passive mechanical properties, including stress at a given strain and Young's modulus, vary significantly between different muscle types and adipose tissues. These differences reflect their unique structural compositions and functional roles in vivo [21]. The table below summarizes measured passive properties from murine tissues, providing a reference for the expected mechanical behavior of various sample types.
Table 1: Passive Mechanical Properties of Murine Tissues (Mean Values Reported)
| Tissue Type | Stress at 30% Strain (kPa) | Young's Modulus (kPa) | Hysteresis (%) |
|---|---|---|---|
| Soleus Muscle (SOL) | ~10 | ~45 | ~35 |
| Extensor Digitorum Longus (EDL) | ~8 | ~35 | ~30 |
| Diaphragm Muscle (DIA) | ~12 | ~40 | ~25 |
| Brown Adipose Tissue (BAT) | ~4 | ~20 | ~30 |
| Visceral Adipose Tissue (VAT) | ~2.5 | ~12 | ~25 |
| Subcutaneous Adipose Tissue (SAT) | ~1.5 | ~8 | ~20 |
Data adapted from Cesanelli et al. [21]
Experimental Protocols
Protocol 1: Standardized Tissue Mounting and Equilibration
This protocol describes the mounting and equilibration of a blood vessel ring, a common preparation in pharmacological research. The principles are applicable to a variety of tubular and strip-like tissues.
3.1.1 Tissue Preparation and Hooking
- Dissection and Immersion: Anesthetize the animal according to institutional guidelines. Following dissection, immediately place the isolated tissue, such as the thoracic aorta, into a dissection dish containing oxygenated Physiological Salt Solution (PSS) to maintain viability [6].
- Cleaning and Sectioning: Using fine forceps and scissors under a dissecting microscope, carefully remove extraneous adipose and connective tissue. For a vessel, cut the cleaned tissue into rings of 3-5 mm in width [6].
- Mounting on Hooks: Carefully slide a tissue ring onto a pair of dedicated tissue hooks. One hook should have a small knotted loop for attachment to a fixed rod in the bath, while the other is connected via a silk suture to the isometric force transducer [6]. Take care not to damage the endothelial or mucosal layer during this process.
3.1.2 Equilibration in the Organ Bath
- Placement and Connection: Transfer the hooked tissue to the organ bath containing warmed (e.g., 37°C), aerated (e.g., 95% O₂ / 5% CO₂) PSS. Secure the fixed hook to the rod and attach the suture from the other hook to the force transducer, ensuring the tissue is fully immersed [6].
- Setting Resting Tension: Gradually adjust the micrometer attached to the transducer to remove slack from the suture. Apply a preload (e.g., 1-2 g for rodent aorta) to stretch the tissue to its in vivo approximate length. This initial preload represents the starting point for the equilibration process [6].
- Equilibration and Viability Testing: Allow the tissue to equilibrate for a period of 60-90 minutes, replenishing the PSS every 15-20 minutes. During this period, periodically stimulate the tissue with a known agonist (e.g., high-K⺠solution for smooth muscle) to assess viability. A stable, reproducible response indicates the tissue is ready for experimentation [6].
Protocol 2: Determination of Optimal Passive Tension
This protocol outlines a systematic method to determine the optimal preload, or passive tension, for a specific tissue preparation, which is crucial for achieving maximal contractile response.
3.2.1 Length-Tension Relationship Characterization
- Incremental Stretching: After the initial equilibration, subject the tissue to a series of gradual, incremental stretches (e.g., 0.1-0.2 mm steps). Allow the tissue to stabilize for several minutes after each stretch to let the passive force settle [22].
- Active Force Probing: At each new length, elicit a brief, submaximal contraction using a reference agonist (e.g., 10â»â¶ M phenylephrine for vascular tissue or electrical stimulation for skeletal muscle) [6].
- Data Recording: Record the magnitude of the developed active force at each length.
3.2.2 Identification of Optimal Preload (Lâ‚€)
- Plot the active force generated against the respective passive tension (or muscle length). The optimal preload (Lâ‚€) is identified as the point on the graph that yields the maximum active contractile response [23]. Once identified, set the tissue to this length and allow it to equilibrate for a further 15-20 minutes before commencing the main experimental protocol.
Table 2: Research Reagent Solutions for Organ Bath Experiments
| Reagent / Solution | Function / Purpose | Example Composition / Notes |
|---|---|---|
| Physiological Salt Solution (PSS) | Maintains ionic balance, pH, and tissue viability; serves as the experimental buffer. | Typically contains NaCl, KCl, CaCl₂, MgCl₂, NaHCO₃, KH₂PO₄, Glucose; aerated with 95% O₂/5% CO₂ [6]. |
| High-K⺠Solution | Depolarizes cell membranes; used to test tissue viability and contractile function. | PSS with NaCl partially or fully replaced by equimolar KCl [6]. |
| Reference Agonists | Used to elicit a standard contractile response for tension optimization and tissue validation. | e.g., Phenylephrine (αâ‚-adrenergic agonist), Carbachol (muscarinic agonist), specific to the tissue under study. |
| Caffeine / Halothane | Diagnostic agents used specifically for in vitro contracture testing of Malignant Hyperthermia susceptibility. | Used on fresh human muscle bundles to diagnose hypermetabolic responses [4]. |
| Basement Membrane Extract (BME) | A 3D matrix for embedding and cultivating specialized organoids, such as thymic epithelial cells. | Used in advanced 3D culture systems, not in standard organ baths, for complex tissue modeling [24]. |
The following workflow diagram summarizes the key steps from tissue preparation to the final experiment.
Troubleshooting and Technical Notes
Common Artifacts and Mitigation Strategies
- Excessive Baseline Drift: This can be caused by temperature fluctuations, insufficient equilibration time, or a compromised tissue preparation. Ensure the water jacket maintains a constant temperature (e.g., 37°C) and verify the integrity of all connections. Allow for a full equilibration period until the baseline is stable [6].
- Absence of Response to Agonists: This typically indicates non-viable tissue. Potential causes include damage during dissection or mounting, bacterial contamination of solutions, or an incorrect PSS composition. Practice meticulous dissection techniques, use sterile solutions where possible, and double-check the PSS recipe [4].
- Unstable or Noisy Force Signal: This is often due to air bubbles in the bath or excessive aeration causing vibrations at the tissue-transducer connection. Ensure all tubing is primed and bubble-free, and adjust the gas flow rate to provide sufficient oxygenation without causing physical disturbance to the tissue [6].
Advanced Considerations for Specific Tissues
- Skeletal Muscle Bundles: For human skeletal muscle biopsies used in diagnostic contracture tests, specific viability criteria apply. A muscle bundle must elicit a minimum of 1 g of twitch force upon supramaximal electrical stimulation to be considered viable for the Caffeine-Halothane Contracture Test [4].
- Small and Delicate Tissues: When working with small murine blood vessels (e.g., mesenteric arteries), special care must be taken to avoid damaging the endothelium, which can profoundly affect the tissue's pharmacological response. The use of fine wires for cannulation is recommended [6].
- Validation with Modern Techniques: The use of Supersonic Shear Wave Elastography (SSWE) has been validated as a non-invasive method to quantify passive muscle tension. Studies show a strong linear relationship between shear elastic modulus and passive tension, offering a modern tool for validating and refining tension application protocols ex vivo and in vivo [25].
Designing Dose-Response Curves and Electrical Stimulation Protocols
The isolated tissue bath methodology, first developed in 1904, remains a cornerstone in pharmacology and physiology research for assessing contractile tissue function [4]. This approach provides a direct means to investigate the effects of pharmacological agents or electrical stimulation on tissue contractility, serving as a critical tool for both basic research and clinical diagnostics, such as the caffeine-halothane contracture test for malignant hyperthermia susceptibility [4]. Organ baths enable researchers to generate precise dose-response curves and design specific electrical stimulation protocols to elucidate mechanisms of drug action and tissue physiology.
Experimental Protocols
Tissue Preparation and Viability Assessment
Proper tissue preparation is fundamental to obtaining reliable data in organ bath experiments:
Tissue Collection and Dissection: Fresh tissue samples should be obtained and immediately placed in oxygenated physiological solution. Using a dissecting microscope, prepare muscle bundles with dimensions of approximately 1-3 mm in diameter and 3-5 cm in length [4]. For human ventricular trabeculae studies, exclude macroscopically diseased or necrotic tissue [26].
Viability Qualification: Mount tissue specimens in experimental chambers containing oxygenated physiological solution maintained at 37°C. Apply electrical field stimulation (EFS) with supramaximal stimulation (typically 1 ms pulse width) to assess tissue viability. A viable muscle bundle should elicit a minimum of 1 g of twitch force [4]. Tissues that do not respond to standard pharmacological checks should be excluded from studies [26].
Standardization Procedure: Process muscle preparations through standardization procedures to reduce signal variability prior to EFS and pharmacological intervention. This ensures tissues are maintained under appropriate physiological tension throughout experiments [26].
Dose-Response Curve Generation
Dose-response relationships are essential for determining drug efficacy and potency:
Cumulative Concentration-Response Curves (CCRC): Prepare stock solutions of test articles in appropriate vehicles. For each test article, run 6-point cumulative concentration response curves upon a steady baseline EFS response [26]. Include positive control compounds and vehicle controls to allow direct comparison.
Agonist Studies: To study receptor-mediated responses, generate cumulative concentration-response curves for specific agonists. For adrenergic responses, use agonists like phenylephrine or noradrenaline (0.1-100 µM); for cholinergic responses, use carbachol or methacholine (0.1-1000 µM) [27].
Antagonist Studies: To investigate inhibitory effects, pre-incubate tissues with potential antagonists or test compounds before generating agonist concentration-response curves. For example, plant extracts like Acridocarpus smeathmannii at concentrations of 0.25 and 0.50 mg/mL have demonstrated 50% or greater reduction in prostate tissue contractions induced by α1-adrenergic agonists [27].
Data Analysis: Express responses as percentage change from baseline EFS response. Fit data to appropriate mathematical models such as the Hill model for calculation of EC50/IC50 values [4]. Perform statistical analysis using appropriate software such as GraphPad Prism [26].
Electrical Stimulation Protocols
Electrical field stimulation allows investigation of neurogenic responses:
Parameter Optimization: Subject muscle preparations to an EFS voltage curve to determine optimal stimulation settings. This process identifies the appropriate voltage, frequency, and pulse duration for subsequent experimental protocols [26].
Frequency-Response Relationships: Apply EFS across a frequency range (e.g., 2-32 Hz) to characterize neurogenic contractions. Document the inhibition of neurogenic contractions; for example, A. smeathmannii extract has shown up to 90% inhibition of EFS-induced contractions in both prostate and bladder tissues [27].
Experimental Setup: Use tissue bath systems with parallel experimentation capabilities; advanced laboratories may run up to 24 tissue baths in parallel for rapid data collection [4]. Maintain bath volumes at consistent levels (e.g., 25 mL) across experiments [26].
Data Presentation and Analysis
Quantitative Data Tables
Table 1: Characterization of Adrenergic Agonist Effects in Prostate Tissue
| Agonist | Concentration Range (µM) | Maximum Contraction (% of Baseline) | EC50 Value | Inhibition by A. smeathmannii (0.5 mg/mL) |
|---|---|---|---|---|
| Phenylephrine | 0.1 - 100 | 215% ± 15% | 53.5 nM | >50% reduction |
| Noradrenaline | 0.1 - 100 | 228% ± 12% | 42.3 nM | >50% reduction |
Table 2: Electrical Field Stimulation Parameters and Responses
| Tissue Type | Optimal Frequency Range | Stimulation Parameters | Neurogenic Contraction Inhibition |
|---|---|---|---|
| Human Ventricular Trabeculae | 0.5 - 2.0 Hz | 1 ms pulse width, supramaximal voltage | Not applicable |
| Prostate Tissue | 2 - 32 Hz | 1 ms pulse width, 80V | Up to 90% with A. smeathmannii |
| Bladder Tissue | 2 - 32 Hz | 1 ms pulse width, 80V | Up to 90% with A. smeathmannii |
Table 3: Diagnostic Contracture Thresholds for Malignant Hyperthermia Susceptibility
| Triggering Agent | Concentration | Contracture Threshold Indicating MHS | Test Duration |
|---|---|---|---|
| Halothane | 3% | >0.7 g contracture | 10 minutes |
| Caffeine | 0.5, 1, 2, 4, 8, 32 mM | ≥0.2 g contracture at ≤2 mM caffeine | Cumulative dosing |
Data Interpretation Guidelines
Dose-Response Analysis: Plot dose-response curves on a semilog scale, typically resulting in sigmoidal curves. The Hill model remains a common mathematical framework for analyzing these relationships despite its simplifications [4].
Contracture Analysis: For diagnostic tests like the caffeine-halothane contracture test, abnormal responses are defined as specific contracture thresholds: >0.7 g contracture from 10 min exposure to 3% halothane and ≥0.2 g contracture at ≤2 mM caffeine [4].
Statistical Considerations: Run experiments in duplicate or multiple preparations to account for biological variability. Express data as mean ± standard error of the mean (S.E.M.) where appropriate [26].
Visualization of Experimental Workflows
Organ Bath Experimental Setup
Dose-Response Curve Generation Protocol
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Organ Bath Experiments
| Reagent/Chemical | Function/Application | Example Usage |
|---|---|---|
| Phenylephrine | Selective α1-adrenergic receptor agonist | Adrenergic contraction studies (0.1-100 µM) [27] |
| Noradrenaline | Endogenous adrenergic receptor agonist | Adrenergic contraction studies (0.1-100 µM) [27] |
| Carbachol | Cholinergic receptor agonist | Cholinergic contraction studies (0.1-1000 µM) [27] |
| Methacholine | Muscarinic receptor agonist | Cholinergic contraction studies (0.1-1000 µM) [27] |
| Isoprenaline | β-adrenergic receptor agonist | Positive control in ventricular trabeculae studies [26] |
| Halothane | Volatile anesthetic | Diagnostic testing for MH susceptibility (3% concentration) [4] |
| Caffeine | Ryanodine receptor agonist | Diagnostic testing for MH susceptibility (0.5-32 mM) [4] |
| A. smeathmannii extract | Natural product with inhibitory effects | Inhibition of smooth muscle contraction (0.25-0.50 mg/mL) [27] |
| KCl | Depolarizing agent | Reference contractions for tissue viability |
| Schisanwilsonin H | Schisanwilsonin H, MF:C30H32O9, MW:536.6 g/mol | Chemical Reagent |
| XL-784 | XL-784, MF:C21H22ClF2N3O8S, MW:549.9 g/mol | Chemical Reagent |
Troubleshooting and Technical Considerations
Common Experimental Challenges
Tissue Viability: Maintain fresh tissue in oxygenated physiological solution and complete experiments promptly after collection. For malignant hyperthermia diagnostic testing, fresh tissue is required and testing must be initiated within minutes of biopsy [4].
Solution Composition: Use appropriate physiological salt solutions (e.g., Krebs-Henseleit solution) maintained at proper pH (7.4) and temperature (37°C) with continuous oxygenation (95% O2, 5% CO2).
Stimulation Artifacts: Position stimulating electrodes appropriately to minimize direct stimulation artifacts in force measurements. Use optimal EFS settings determined during qualification procedures [26].
Negative Control Inclusion: Always include vehicle control experiments to account for potential solvent effects on tissue contractility [26].
Data Quality Assurance
Parallel Experimentation: Utilize multiple tissue baths run in parallel to increase throughput and account for biological variability. Advanced setups can run up to 24 tissue baths simultaneously [4].
Blinded Assessment: When testing unknown compounds, implement blinded protocols to reduce experimental bias.
Reference Compounds: Include standard reference compounds in each experimental session to validate system performance and enable cross-experiment comparisons [26].
These application notes and protocols provide a framework for designing robust dose-response and electrical stimulation studies in organ bath experiments, enabling researchers to generate reliable, reproducible data for pharmacological and physiological investigations.
Assessing Tissue Viability and Contractile Function
The isolated tissue bath technique is a classical pharmacological tool that has been utilized for over a century to evaluate concentration-response relationships in a wide array of contractile tissues [15]. This methodology remains an indispensable tool for pharmacologists and physiologists due to its versatility, simplicity, and reproducibility [15]. The fundamental principle involves maintaining living tissue in a controlled, physiologically relevant environment, allowing researchers to study integrated tissue function, including drug-receptor interactions, signal transduction, second messenger generation, changes in smooth muscle excitability, and ultimately, alterations in tissue contractile function [15]. This protocol details the application of isolated tissue bath systems for the critical assessment of tissue viability and contractile function, providing a framework for research in pharmacology, physiology, and drug development.
The Scientist's Toolkit: Essential Materials and Equipment
Successful assessment of tissue viability and contractile function requires specific instrumentation and reagents. The following table catalogs the essential components of a functional tissue bath system.
Table 1: Key Research Reagent Solutions and Essential Materials
| Item | Function/Description |
|---|---|
| Organ Bath System (e.g., DMT 820MO) | Core platform housing tissue chambers; maintains perfusate temperature (typically 37°C) and provides oxygenation [28]. |
| Physiological Salt Solution (PSS) | Mimics the ionic composition of extracellular fluid (e.g., Krebs-Henseleit solution) to maintain tissue viability [15]. |
| Isometric Force Transducer | Measures changes in tension (force) generated by the tissue, connected to a data acquisition system [15] [28]. |
| Data Acquisition System & Software | Captures, visualizes, and records force data in real-time (e.g., systems using LabChart) [15] [28]. |
| Gas Mixture (95% Oâ‚‚ / 5% COâ‚‚) | Oxygenates the PSS and maintains physiological pH [15] [29]. |
| Micrometer / Precision Micrometer | Allows fine adjustment of resting tension (preload) on the tissue to achieve optimal length for contraction [15] [28]. |
| Dissection Tools (forceps, scissors, dissection microscope) | For careful isolation and preparation of the tissue specimen without causing damage [15]. |
| Mounting Hooks & Sutures | Used to secure the tissue between the fixed rod and the force transducer within the bath [15]. |
| NorA-IN-1 | 2,4,6-Trimethoxy-4'-hydroxychalcone|Research Grade |
Experimental Workflow for Tissue Viability and Function Assessment
The following diagram outlines the core procedural workflow for preparing a tissue and assessing its viability and contractile function within an organ bath system.
Detailed Methodologies
System Preparation and Tissue Mounting
4.1.1 Physiological Salt Solution (PSS) Preparation A standard PSS recipe is required to sustain tissue viability. A common formulation is a modified Krebs-Henseleit solution. A 5 L volume is typically prepared for experiments using multiple baths [15]. The solution should be prepared with high-purity water (e.g., HPLC-Type I), and the final pH should be 7.4 when bubbled with 95% Oâ‚‚ / 5% COâ‚‚ [15].
4.1.2 Tissue Bath Setup The tissue bath system must be prepared before tissue dissection. Critical steps include preheating the recirculating water bath to 37°C and ensuring all water-jacketed components are connected in series with correct water flow direction [15] [29]. The data acquisition system and force transducers should be powered on at least 15 minutes prior to the experiment to minimize thermal drift [15]. The system is then pressurized with the 95% O₂ / 5% CO₂ gas mixture, filled with pre-warmed PSS, and primed to remove any air bubbles from the tubing [15] [29].
4.1.3 Tissue Dissection and Mounting For a rat thoracic aorta, the animal is anesthetized according to institutional guidelines. The aorta is located along the spinal column, and all connections are severed. The vessel is gently dissected free, taking care not to pull or tug on the tissue, and immediately placed in a dissection dish containing ice-cold, oxygenated PSS [15] [29]. Under a dissection microscope, the aorta is cleaned of perivascular adipose and connective tissue and cut into rings of 3-5 mm in width [15]. Each ring is carefully mounted on a pair of tissue hooks; one hook is attached via a suture to a fixed rod in the bath, and the other is tied to the force transducer, ensuring slack is left for subsequent tension adjustment [15] [29].
Establishing Tissue Viability and Basal Function
4.2.1 Setting Optimal Passive Tension Each tissue type has an optimal length (Lâ‚€) at which it generates maximal force in response to stimulation. This is achieved by applying a specific passive tension, or preload. For the rat thoracic aorta, the optimal passive tension is 4 g [15]. This is typically applied in incremental steps (e.g., 2 g followed by another 2 g after the tissue relaxes and plateaus) using a micrometer [15]. After the final tension is set, the tissue is allowed to equilibrate for approximately 60 minutes, with the PSS being replaced every 15 minutes [15] [29].
4.2.2 Viability Testing Following the equilibration period, tissue viability is confirmed by challenging the tissue with a known contractile agonist. A common test uses a high-potassium (e.g., 60-80 mM Kâº) PSS, which depolarizes the smooth muscle membrane and causes a robust, sustained contraction [15]. A healthy, viable tissue should produce a strong and reproducible contractile response. Failure to do so indicates compromised tissue integrity, and the preparation should be discarded.
Assessing Contractile Function: Generating a Concentration-Response Curve
A primary application of the tissue bath is quantifying tissue responsiveness to pharmacological agents by generating concentration-response curves. The following diagram and protocol detail the process of creating a cumulative concentration-response curve to an agonist, which allows for the determination of drug potency (pDâ‚‚ or ECâ‚…â‚€) and efficacy (E_max).
4.3.1 Protocol for Cumulative Concentration-Response Curve
- Initial Challenge (Optional): A sub-maximal concentration of the agonist may be applied and then washed out to prime the tissue [29].
- Tissue Incubation: If studying an antagonist, the tissue is incubated with the antagonist for a specified period (e.g., one hour) prior to agonist addition [29].
- Cumulative Agonist Addition: Starting from the lowest concentration, the agonist is added directly to the tissue bath. The addition volume should be small (e.g., <1% of bath volume) to avoid significant dilution.
- Response Plateau: The system is allowed to reach a stable plateau force before the next, higher concentration is added. This process is repeated, cumulatively increasing the bath concentration, until no further increase in contraction is observed, defining the maximum response (E_max) [29].
- Data Analysis: The force generated at each plateau is recorded. Responses are normalized as a percentage of the maximum contraction. A semi-log plot of response (%) versus agonist concentration [M] is generated, producing a sigmoidal curve from which the ECâ‚…â‚€ (concentration producing 50% of maximal response) and pDâ‚‚ (-log ECâ‚…â‚€) can be derived [14] [4].
Data Presentation and Analysis
Quantitative Data from Tissue Bath Experiments
Table 2: Key Pharmacological Parameters Derived from Concentration-Response Curves
| Parameter | Description | Interpretation | Example Calculation |
|---|---|---|---|
| ECâ‚…â‚€ | Concentration of an agonist that produces 50% of its maximal effect. | Measure of potency; a lower ECâ‚…â‚€ indicates a more potent agonist. | For an ECâ‚…â‚€ of 10â»â· M, the pDâ‚‚ is 7. |
| pDâ‚‚ | The negative logarithm of the ECâ‚…â‚€ (pDâ‚‚ = -log ECâ‚…â‚€). | A convenient measure of potency; a higher pDâ‚‚ indicates a more potent agonist. | A drug with ECâ‚…â‚€ = 10â»â¸ M has a pDâ‚‚ of 8. |
| E_max | The maximum possible effect achievable with an agonist. | Measure of efficacy; an agonist with higher E_max has greater intrinsic activity. | Expressed as a percentage of a reference agonist or as absolute force (g or mN). |
| pAâ‚‚ | The negative logarithm of the molar concentration of an antagonist that requires a twofold increase in agonist concentration to produce the same effect. | Measure of antagonist affinity; a higher pAâ‚‚ indicates a more potent antagonist. | Determined by analyzing agonist curves in the absence and presence of multiple antagonist concentrations. |
Statistical Analysis of Contractile Data
Data from tissue bath experiments are typically continuous and should be presented as mean ± SEM or SD from multiple tissue preparations (n), where n represents the number of animals or the number of tissues from separate experiments [14]. For normally distributed data, comparisons between two groups can be made using a Student's t-test (paired or unpaired as appropriate), while comparisons between multiple groups require analysis of variance (ANOVA) followed by post-hoc tests [14]. A P-value of < 0.05 is generally considered statistically significant.
Advanced Application: In Vitro Contracture Testing for Malignant Hyperthermia
A critical clinical diagnostic application of tissue bath methodology is the Caffeine-Halothane Contracture Test (CHCT) for Malignant Hyperthermia (MH) susceptibility. Fresh human skeletal muscle biopsies are mounted in tissue baths and exposed to caffeine and halothane [4]. MH-susceptible muscle exhibits an abnormal hypersensitivity, characterized by sustained contractures (involuntary muscle contractions) at significantly lower threshold concentrations than normal muscle. For example, a contracture >0.7 g upon exposure to 3% halothane or ≥0.2 g at ≤2 mM caffeine is diagnostic of MH susceptibility in the North American protocol [4]. This application underscores the translational power of the isolated tissue bath technique from basic research to clinical diagnostics.
The following tables summarize key quantitative findings and experimental parameters relevant to organ bath experiments and advanced in vitro models.
Table 1: Key Performance Metrics in Modern In Vitro Models
| Model/Parameter | Barrier Integrity Measurement | Apical/Basal Access | Cellular Diversity | Key Application |
|---|---|---|---|---|
| Organ-on-Chip (Intestinal) [30] | Permeability Assays | Independent Sampling & Stimulation [30] | Preserved [30] | Drug Transport Studies |
| Organ Bath (Isolated Tissue) [1] | Functional Response | N/A | Native Tissue Context [1] | Efficacy & Safety Pharmacology [1] |
Table 2: Analysis Modalities for Ex Vivo and Advanced Models
| Analysis Type | Specific Method | Data Output | Application Context |
|---|---|---|---|
| Functional Assay | Permeability Assay [30] | Quantitative Integrity Measure | Barrier Function (Organ-on-Chip) [30] |
| Transcriptome Analysis | RNA Isolation [30] | Gene Expression Profile | Mechanistic Studies [30] |
| Secretome Analysis | Protein Assays [30] | Cytokine/Protein Secretion | Immune & Inflammatory Response [30] |
| Microscopy | Staining & Imaging [30] | Structural & Morphological Data | General Model Validation [30] |
Experimental Protocols
Protocol: Organ Bath Experimentation for Drug Efficacy & Safety
This protocol outlines the core methodology for utilizing isolated tissue in an organ bath to assess compound effects, a foundational technique in drug discovery [1].
Key Applications:
- Drug Screening: Determine the pharmacological activity (agonism, antagonism) of new chemical entities on specific tissue types (e.g., vascular, intestinal smooth muscle) [1].
- Safety Pharmacology: Identify potential adverse effects of compounds on organ function, such as contractile responses [1].
Materials:
- Organ bath apparatus with temperature control and aeration (carbogen: 95% Oâ‚‚, 5% COâ‚‚).
- Physiological salt solution (e.g., Krebs-Henseleit solution).
- Force-displacement transducer or isometric force transducer.
- Data acquisition system.
- Isolated tissue sample (e.g., jejunum, trachea).
Methodology:
- Tissue Preparation & Mounting:
- Surgically isolate the target tissue and carefully dissect it to an appropriate size.
- Mount the tissue in the organ bath containing pre-warmed (37°C) and oxygenated physiological salt solution.
- Attach the tissue to a force transducer to measure isometric tension.
System Equilibration:
- Apply a resting tension of 1-2 grams to the tissue.
- Allow the tissue to equilibrate for 60-90 minutes, replacing the bath solution every 15-20 minutes until a stable baseline is achieved.
Experimental Intervention:
- Drug Addition: Add cumulative concentrations of the test compound directly to the organ bath.
- Response Measurement: Record the tissue's contractile or relaxant response following each addition.
- Control & Validation: Include positive control compounds (e.g., known agonists) to validate tissue responsiveness.
Data Analysis:
- Quantify the amplitude of the tissue response for each concentration of the test compound.
- Generate concentration-response curves and calculate pharmacological parameters (e.g., ECâ‚…â‚€, Emax).
Protocol: Generating Organ-on-Chip for Intestinal Studies
This protocol details the generation of a human intestinal organ-on-chip model, which overcomes the lumen inaccessibility of traditional organoids and allows for independent access to apical and basal compartments [30].
Key Applications:
- Disease Modeling: Study chronic inflammatory diseases (e.g., Crohn's disease) and host-pathogen interactions.
- Clinical Diagnostics & Drug Screening: Model patient-specific conditions and test drug efficacy and absorption [30].
Materials:
- Organ-on-chip device (e.g., microfluidic chip with porous membrane).
- Established human or murine intestinal organoid lines [30].
- Dissociation reagent (e.g., TrypLE Express).
- Appropriate cell culture media.
Methodology:
- Organoid Line Establishment: Culture and expand human or murine intestinal organoids using standard 3D culture techniques [30].
- Single-Cell Dissociation: Dissociate the organoids into a single-cell suspension using a enzymatic reagent [30].
- Chip Preparation & Seeding:
- Prepare the organ-on-chip device according to manufacturer instructions.
- Seed the dissociated intestinal cells onto the coated membrane of the chip [30].
- Culture & Differentiation:
- Culture the chip under flow conditions to promote cell differentiation and formation of a polarized, functional epithelium.
- Stimulation & Sampling:
- Independent Sampling: Collect samples from the apical and basal chambers independently for transcriptome (RNA) and secretome (protein) analysis [30].
- Permeability Assay: Apply a marker molecule (e.g., FITC-dextran) to the apical side and measure its appearance in the basal chamber over time to assess barrier integrity [30].
Experimental Workflow and Signaling Visualization
Research Reagent Solutions
Table 3: Essential Materials for Organ Bath and Organ-on-Chip Experiments
| Item | Function/Application |
|---|---|
| Physiological Salt Solution | Maintains ionic balance, pH, and provides nutrients to sustain isolated tissue viability in the organ bath. |
| Organoid Culture Media | Supports the growth and maintenance of 3D intestinal organoids, which serve as a cell source for organ-on-chip models [30]. |
| Dissociation Reagent | Enzymatically breaks down organoids into single-cell suspensions for seeding onto organ-on-chip devices [30]. |
| Force Transducer | Measures isometric tension changes (contraction/relaxation) in real-time from isolated tissues in the organ bath. |
| Microfluidic Organ-on-Chip | Provides a biomimetic microenvironment with a porous membrane, allowing for cell culture under flow and independent apical/basal access [30]. |
Solving Common Challenges and Optimizing Data Quality in Organ Bath Studies
The isolated tissue bath system is a foundational tool in pharmacology and physiology research, enabling the study of contractile responses in tissues like vascular smooth muscle and bladder tissue [4]. A persistent challenge in these experiments is the inherent variability in the size of tissue specimens. Despite efforts to standardize during dissection, variations exist, making data normalization not just common practice but a scientific necessity. The core dilemma for researchers is selecting the most appropriate denominator—weight, length, or cross-sectional area—to normalize force measurements, a decision that significantly impacts data interpretation and reproducibility [31]. This document outlines the evidence-based considerations for this critical choice.
Quantitative Comparison of Normalization Denominators
A pre-planned analysis of organ bath data provides direct comparative evidence on the effectiveness of different normalization parameters. The following table summarizes key findings from a systematic investigation comparing weight, length, and cross-sectional area as denominators in two different tissues [31].
Table 1: Comparison of Normalization Denominators Based on Correlation Strength (R² Values)
| Tissue Type | Stimulus | Normalization Denominator | Correlation (R²) with Force |
|---|---|---|---|
| Urinary Bladder | Carbachol | Weight | 0.3582 |
| Urinary Bladder | Carbachol | Length | Weaker |
| Urinary Bladder | Carbachol | Cross-Sectional Area | Weaker |
| Aorta | Phenylephrine | Weight | 0.0511 |
| Aorta | Phenylephrine | Length | Weaker |
| Aorta | Phenylephrine | Cross-Sectional Area | Weaker |
The data leads to two critical conclusions. First, no single normalization parameter is universally superior. Second, the optimal choice is highly tissue-dependent. For urinary bladder strips, normalization for strip weight yielded the tightest, albeit only moderate, correlation with the generated force. In contrast, for aortic rings, all correlations were markedly weaker, with weight showing a very low correlation (R² = 0.0511) [31]. This implies that normalization for tissue size is less effective at reducing data variability in aortic tissues than previously assumed.
Experimental Protocol for Assessing Normalization Parameters
To empirically determine the best normalization denominator for a new tissue preparation, the following detailed protocol is recommended.
Table 2: Essential Research Reagent Solutions for Organ Bath Experiments
| Item | Function/Description |
|---|---|
| Physiological Salt Solution (PSS) | Provides a physiological environment to maintain tissue viability. Typical composition includes NaCl, KCl, CaCl₂, MgSO₄, KH₂PO₄, NaHCO₃, and Glucose [6]. |
| Contractile Agonists | Substances like Acetylcholine (ACh) or Phenylephrine used to stimulate muscle contraction [31] [10]. |
| Dissection Tools | Fine scissors, forceps, and a dissecting microscope for precise tissue preparation [6]. |
| Tissue Bath System | Water-jacketed chambers maintained at 37°C, connected to a 95% O₂ / 5% CO₂ gas supply for oxygenation [6]. |
| Force Transducers | Instruments that measure isometric force generated by the tissue, connected to a data acquisition system [6]. |
Step-by-Step Workflow
- Tissue Dissection and Preparation: Dissect the target tissue (e.g., thoracic aorta, urinary bladder) and prepare multiple specimens of varying, but meticulously recorded, dimensions [6]. Immediately place tissues in oxygenated PSS.
- Mounting and Equilibration: Mount each tissue specimen in an individual organ bath chamber filled with oxygenated PSS at 37°C. Connect the tissue to a force transducer and apply a resting tension appropriate for the tissue type. Allow the tissue to equilibrate for a stable baseline period (e.g., 60-90 minutes) [6].
- Viability Testing: Apply a known concentration of a contractile agonist (e.g., a high-potassium solution or a standard dose of ACh) to verify tissue responsiveness.
- Experimental Stimulation: Expose each tissue specimen to a standardized, maximally effective concentration of a contractile agonist (e.g., Carbachol for bladder, Phenylephrine for aorta). Record the peak force generated.
- Post-Experiment Measurement: Following the experiment, carefully blot each tissue specimen dry and measure its wet weight. If using cross-sectional area, the area can be calculated from the weight and length of the specimen, assuming a cylindrical shape and a density of 1.0 g/cm³ [31].
- Data Analysis: Plot the raw force generated by each specimen against each potential denominator (weight, length, calculated cross-sectional area). Perform linear regression analysis to determine which parameter yields the strongest correlation (highest R² value). The denominator producing the tightest correlation is the most appropriate for reducing variability in that specific tissue preparation [31].
The following workflow diagram visualizes the key decision points in this protocol.
The Scientist's Toolkit: Decision Framework and Best Practices
No single normalization approach fits all experimental contexts [31]. The choice of denominator must be tailored to the specific tissue type and research question. The following decision diagram provides a framework for selecting the most appropriate normalization strategy.
Based on the evidence, the primary recommendation is to empirically determine the optimal denominator for each new tissue preparation by conducting a correlation analysis as outlined in the protocol above [31]. Relying on assumptions or practices from different tissues can introduce unnecessary variability. Furthermore, it is critical to transparently report the normalization method in all publications, including a justification for its choice to enhance reproducibility and scientific rigor.
Troubleshooting Poor Viability and Lack of Contractile Response
Isolated tissue bath assays are a classical pharmacological tool for evaluating concentration-response relationships in a myriad of contractile tissues, with a history of use spanning over a century [15] [4]. This technique remains indispensable for pharmacologists and physiologists investigating mechanisms of disease, drug efficacy, and receptor characterization. The system allows a living tissue to function as an integrated unit, synthesizing steps from drug-receptor interaction and signal transduction to the final physiological outcome of contraction or relaxation [15]. A primary advantage is the ability to calculate important pharmacological variables, such as drug efficacy and potency, in a context that more closely resembles how drugs work in the body as a whole [15]. However, the technique is prone to specific challenges, chief among them being poor tissue viability and an absent or diminished contractile response. This application note provides a structured framework for diagnosing and resolving these critical issues, ensuring the generation of robust and reproducible functional data.
Troubleshooting Poor Tissue Viability
Tissue viability is the cornerstone of any successful organ bath experiment. The following table summarizes common causes and solutions for poor tissue viability.
Table 1: Troubleshooting Guide for Poor Tissue Viability
| Observed Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| No response to standard viability checks (e.g., KCl) | Non-viable tissue due to improper dissection, hypoxia, or mechanical damage [15]. | Ensure rapid dissection and immediate placement in oxygenated Physiological Salt Solution (PSS) [15]. Handle tissue with extreme care to avoid stretching, pinching, or crushing. |
| Gradual decline in baseline tension or response | Incorrect buffer composition, temperature fluctuations, or bacterial contamination [15]. | Prepare fresh PSS daily and confirm pH (7.4) and osmolarity. Maintain a constant bath temperature (e.g., 37°C). Use sterile techniques where possible. |
| Inconsistent responses between tissue replicates | Variations in tissue dissection, size, or mounting tension [4]. | Standardize dissection protocols. Use templates to create uniform tissue strips. Determine and apply the optimal passive tension (e.g., 4 g for rat aorta) for your tissue type [15]. |
Core Viability Assessment Protocol
A key step in any organ bath experiment is to validate tissue responsiveness and contractile integrity. This is typically done by assessing the contractile response to a known, non-receptor-mediated agonist.
- Principle: High concentrations of potassium chloride (KCl) depolarize smooth muscle cells, opening voltage-gated calcium channels and inducing a robust, reversible contraction. A strong response indicates healthy, viable tissue [32] [15].
- Method:
- After the initial equilibration period under passive tension, administer a single bolus of KCl to the tissue bath to achieve a final concentration of 20-80 mM.
- Allow the contraction to reach a plateau, then wash the tissue with fresh PSS several times until the baseline tension is restored.
- A viable tissue should produce a sustained contraction. Tissues that are unresponsive to this challenge should be excluded from the study [32] [15].
- Troubleshooting: If the KCl response is absent or weak, revisit dissection speed, tissue handling, and PSS oxygenation. This test should be performed both before and after an experimental protocol to confirm tissue viability throughout [32].
Resolving Lack of Contractile Response
When a tissue is viable but fails to respond to a specific agonist, the issue lies with the experimental parameters or the agent itself.
Table 2: Troubleshooting Guide for Lack of Contractile Response
| Observed Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| No response to a receptor-specific agonist | Incorrect drug preparation, degradation of agonist, or presence of an unintended antagonist. | Prepare fresh stock solutions and dilutions using the correct solvent. Verify drug stability and storage conditions. Ensure the tissue bath system is thoroughly cleaned between experiments. |
| Absence of spontaneous contractions | Tissue-type dependency or sub-optimal bath conditions. | Confirm that the specific tissue exhibits spontaneous activity under control conditions. Ensure proper ionic composition of PSS (especially Ca²âº), temperature, and oxygenation [32]. |
| Unexpected receptor pharmacology | Use of an inappropriate animal model or tissue state (e.g., obesity). | Account for pathophysiological state. For instance, oxytocin-induced bladder contractions are significantly heightened in tissues from obese rats, a effect absent in non-obese rats [32]. |
Experimental Protocol for Investigating a Novel Contractile Pathway
The following detailed methodology is adapted from recent research investigating the impact of the oxytocin receptor antagonist atosiban on bladder and prostate contractility [32].
- Tissue Collection & Dissection:
- Sacrifice animals according to approved ethical guidelines (e.g., COâ‚‚ inhalation) [32].
- Rapidly dissect the target organ (e.g., bladder, prostate ventral lobe, or thoracic aorta) and place it in ice-cold, oxygenated PSS [32] [15].
- Carefully remove extraneous fat and connective tissue. Cut the tissue into uniform strips (e.g., 3-5 mm in width) using a sharp blade or scissors [15].
- Tissue Mounting & Equilibration:
- Mount each tissue strip on a pair of tissue hooks or wires in the organ bath. One hook is fixed, while the other is connected to an isometric force transducer [15].
- Submerge the tissue in the bath containing PSS, maintained at 37°C and continuously aerated with 95% O₂ / 5% CO₂ [15].
- Gradually apply the optimal passive tension (determined empirically for each tissue type) and allow the tissue to equilibrate for at least 60 minutes, with periodic washing [32] [15].
- Assessing Contractile Responses:
- Viability Check: Confirm tissue viability by administering 20 mM KCl. Exclude non-responsive tissues [32].
- Recording Spontaneous Activity: Record baseline spontaneous contractions for a set period (e.g., 10-20 minutes) to establish a control level of activity [32].
- Agonist Concentration-Response Curves: Cumulatively add increasing concentrations of the agonist (e.g., oxytocin, 1 nM to 100 µM) at regular intervals (e.g., 10 minutes). Record the contractile response (amplitude, frequency, integral) at each concentration [32].
- Antagonist Studies: To test an inhibitor, pre-incubate the tissue with the antagonist (e.g., 1 µM and 10 µM atosiban) for a specified period before repeating the agonist challenge or assessing its effect on spontaneous contractions [32].
- Data Acquisition & Analysis:
- Record contractile activity using software such as Chart Pro. Normalize contractile integrals against the peak KCl-induced response [32].
- Analyze parameters including frequency, amplitude, and the area under the curve (AUC). Generate concentration-response curves and calculate ECâ‚…â‚€ values using statistical software like GraphPad Prism [32].
The following workflow diagram summarizes the key stages of a standard organ bath experiment.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Organ Bath Experiments
| Item | Function / Application |
|---|---|
| Physiological Salt Solution (PSS) | Provides a buffered, isotonic environment that mimics extracellular fluid, sustaining tissue viability. Typical components: NaCl, KCl, CaCl₂, MgSO₄, NaHCO₃, KH₂PO₄, and glucose [15]. |
| Potassium Chloride (KCl) | Used at high concentrations (e.g., 20-80 mM) as a non-receptor-mediated contractile agent to validate tissue viability and contractile integrity [32] [15]. |
| Oxytocin | A receptor-specific agonist (OXTR) used to induce contractions in sensitive tissues like bladder and prostate; useful for studying receptor-mediated contractility [32]. |
| Atosiban | A competitive oxytocin receptor antagonist; used as a pharmacological tool to probe OXTR function and inhibit oxytocin-induced contractions [32]. |
| Drug Stock Solutions | Agonists and antagonists prepared in appropriate solvents (e.g., distilled water, DMSO) at high-concentration stocks (e.g., 10â»Â² M) for subsequent dilution in PSS [32]. |
Success in isolated tissue bath experiments hinges on meticulous attention to detail at every stage, from tissue acquisition to data analysis. By systematically applying the troubleshooting guidelines and standardized protocols outlined in this document, researchers can effectively diagnose and overcome common obstacles related to tissue viability and contractile responses. This rigorous approach ensures the reliability of data and strengthens the validity of conclusions drawn from this classic, yet powerful, pharmacological technique.
The isolated organ bath technique, a cornerstone of pharmacological and physiological research for over a century, remains an indispensable tool for evaluating concentration-response relationships in contractile tissues [4]. This ex vivo system allows researchers to study tissue function independently of systemic influences, providing crucial data on drug efficacy, potency, and mechanism of action [33]. Despite the advent of high-throughput screening and molecular approaches, organ bath assays continue to offer unique advantages for lead optimization and preclinical safety assessment, bridging the gap between single-cell studies and in vivo models [3] [2]. The versatility of this methodology extends across multiple research domains, including cardiovascular pharmacology, gastrointestinal physiology, respiratory studies, and urological research, making it a fundamental technique in biomedical science [3] [33].
Central to the success of any organ bath experiment is the meticulous optimization of critical physiological parameters: stimulation protocols, temperature control, and aeration management. These factors collectively maintain tissue viability, physiological relevance, and experimental reproducibility. This application note provides a comprehensive framework for researchers to systematically optimize these parameters, ensuring robust and reliable data generation in isolated tissue research. By adhering to these evidence-based protocols, scientists can enhance the predictive validity of their findings and accelerate the drug discovery process.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful organ bath experimentation requires precise selection of physiological solutions, equipment, and pharmacological tools. The following table catalogues essential components for establishing a robust organ bath system.
Table 1: Essential Research Reagents and Solutions for Organ Bath Experiments
| Item | Function | Examples/Specifications |
|---|---|---|
| Physiological Salt Solution (PSS) | Maintains osmotic balance, pH, and provides essential ions for tissue viability [15]. | Krebs-HEPES or Krebs-bicarbonate buffer; contains NaCl, KCl, CaCl₂, MgSO₄, KH₂PO₄, NaHCO₃, glucose [2] [15]. |
| Aeration Gas Mixture | Oxygenates tissue and maintains pH of bicarbonate-buffered solutions [15]. | 95% Oâ‚‚ / 5% COâ‚‚ for bicarbonate buffers; 100% Oâ‚‚ for HEPES buffers [15]. |
| Contractile Agonists | Induce tissue contraction to assess viability and receptor function [29]. | Acetylcholine, Phenylephrine, High Potassium (Kâº) solutions [29] [15]. |
| Receptor Antagonists | Inhibit specific receptor responses to study drug mechanisms [29]. | Atropine (muscarinic), Prazosin (α1-adrenergic) [29]. |
| Tissue Holders & Hooks | Secure tissue specimens within the bath without causing damage [15]. | Stainless steel or glass rods; miniature hooks for smaller vessels [15]. |
| Force Transducers | Measure isometric tension generated by tissue contraction [29] [15]. | High-sensitivity transducers connected to bridge amplifiers [29] [15]. |
Parameter Optimization: Stimulation Protocols
Electrical Field Stimulation (EFS) Parameters
Electrical field stimulation enables the study of neurally-mediated responses in isolated tissues. Optimal EFS parameters vary significantly by tissue type and experimental goals.
Table 2: Optimization Parameters for Electrical Field Stimulation
| Parameter | Typical Range | Application Notes | Experimental Example |
|---|---|---|---|
| Frequency | 0.1 - 20 Hz [17] [10] | Lower frequencies (0.1-5 Hz) often favor cholinergic responses; higher frequencies (10-20 Hz) may recruit additional neurotransmitter release [17]. | Rat colon strips: Frequencies from 0.1 to 20 Hz used to evaluate enteric neuropathy after chemotherapy [17]. |
| Pulse Duration | 0.5 - 1.0 ms [4] | Shorter pulses selectively stimulate nerves; longer pulses may directly depolarize smooth muscle. | Malignant Hyperthermia diagnostic testing: 1 ms pulse width for supramaximal stimulation of skeletal muscle bundles [4]. |
| Voltage | Supramaximal (Typically 10-20% above maximal response) | Must be determined empirically for each tissue type to ensure consistent, reproducible stimulation. | A standard protocol uses voltages sufficient to elicit 80-90% of maximal twitch force [4]. |
| Stimulation Pattern | Continuous trains (5-10 sec) or pulse trains | Duration should be sufficient to achieve peak response without inducing fatigue. | Trains of electrical stimulation applied to colonic strips to evoke neurotransmitter release [17]. |
Experimental Protocol: EFS Setup and Execution
- Electrode Placement: Ensure parallel platinum electrodes are properly positioned on opposite sides of the tissue chamber to create a uniform electrical field [17].
- Stimulator Calibration: Connect to a constant-current or constant-voltage stimulator. Verify output parameters with an oscilloscope before tissue placement.
- Preliminary Frequency-Response Curve: After tissue equilibration, apply EFS across a range of frequencies (e.g., 0.1, 0.5, 1, 5, 10, 20 Hz) using a fixed pulse duration and supramaximal voltage. Allow sufficient recovery time (3-5 minutes) between stimulations.
- Pharmacological Validation: To confirm neural involvement, administer tetrodotoxin (TTX, 1 µM) to block voltage-gated sodium channels in neurons. Alternatively, use atropine (1 µM) to specifically block cholinergic components [17] [10].
- Data Normalization: Express EFS responses as a percentage of a reference contraction (e.g., response to high K⺠solution or maximal receptor agonist).
Diagram 1: Electrical Field Stimulation Workflow
Parameter Optimization: Temperature Control
Temperature Ranges by Tissue Type
Temperature significantly influences metabolic rate, ion channel function, and receptor kinetics in isolated tissues. The following table outlines optimal temperature settings.
Table 3: Temperature Optimization Guidelines for Various Tissues
| Tissue Type | Standard Temperature | Physiological Rationale | Impact of Deviation |
|---|---|---|---|
| Vascular Smooth Muscle | 37°C [15] | Maintains physiological metabolic and contractile function matching core body temperature. | Reduced temperature decreases metabolic rate and can attenuate contractile responses. |
| Skeletal Muscle | 37°C [4] | Optimal for excitation-contraction coupling and enzymatic activity. | Hypothermia prolongs contraction-relaxation cycles; hyperthermia can induce fatigue. |
| Gastrointestinal Tissue | 37°C [17] [10] | Preserves intrinsic neural network (ENS) activity and pacemaker function (ICCs). | Lower temperatures slow rhythmical contractions and neural transmission. |
| Tracheal/Bronchial Tissue | 37°C [2] | Maintains ciliary function and airway smooth muscle responsiveness. | Altered temperature affects mucociliary clearance and bronchoconstrictor responses. |
Experimental Protocol: Temperature Calibration and Maintenance
- System Preparation: Turn on the recirculating heated water bath at least 30-60 minutes before experiments to preheat the entire system [15]. Ensure water jackets are connected in series, with inflow at the lowest barbed connection and outflow at the highest point to prevent air locks.
- Temperature Verification: Use a calibrated thermometer to verify bath temperature directly in multiple tissue chambers, not just the circulating water reservoir. Account for evaporative cooling effects.
- Buffer Pre-warming: Pre-warm physiological salt solution to 37°C before adding to tissue chambers to prevent thermal shock to delicate tissues [15].
- Stability Monitoring: Monitor temperature continuously throughout the experiment. For prolonged experiments (>4 hours), consider using a temperature probe in a control chamber not containing tissue.
- Special Considerations: For temperature-dependence studies, allow at least 30 minutes for tissue acclimation at each new temperature before data collection.
Parameter Optimization: Aeration Management
Aeration Parameters and Standards
Proper aeration serves two critical functions: oxygenating the tissue and maintaining physiological pH in bicarbonate-buffered solutions.
Table 4: Aeration Parameters for Physiological Salt Solutions
| Parameter | Standard Condition | Alternative Conditions | Technical Considerations |
|---|---|---|---|
| Gas Mixture | 95% Oâ‚‚ / 5% COâ‚‚ [15] | 100% Oâ‚‚ for HEPES-buffered solutions; Carbogen (95% Oâ‚‚/5% COâ‚‚) | 5% COâ‚‚ maintains bicarbonate-based buffers at pH ~7.4 [15]. |
| Flow Rate | 1-2 bubbles per second [29] | Adjusted to prevent tissue vibration | Excessive bubbling creates turbulence that destabilizes baseline tension [29]. |
| Aeration Device | Fine-porosity stone or ceramic diffuser | Direct tubing for larger volumes | Fine bubbles increase surface area for efficient gas exchange. |
| Buffer System | Bicarbonate-based (requires COâ‚‚) | HEPES-based (COâ‚‚-independent) | HEPES buffers (10-25 mM) useful when precise COâ‚‚ control is challenging [2]. |
Experimental Protocol: Aeration System Setup
- Gas Supply Connection: Connect medical-grade gas cylinders to the manifold system using appropriate pressure-reducing regulators. Check all connections for leaks using soap solution before pressurizing the system [15].
- Diffuser Inspection: Ensure aeration stones are clean and producing fine bubbles. Clogged stones should be cleaned or replaced to maintain consistent oxygenation.
- Flow Rate Adjustment: Initially set flow to produce a steady stream of fine bubbles (approximately 1-2 bubbles per second). Observe tissue movement under a microscope and reduce flow if baseline tension shows rhythmic oscillations [29].
- pH Verification: Periodically check buffer pH using a calibrated pH meter. For bicarbonate buffers with 95% Oâ‚‚/5% COâ‚‚, pH should stabilize at approximately 7.4.
- Solution Evaporation Management: For extended experiments, use water-jacketed chambers with closed systems or cover chambers with transparent covers to minimize evaporation that concentrates drugs and alters osmolarity [2].
Diagram 2: Aeration Setup and Quality Control Workflow
Integrated Experimental Protocol: Organ Bath Setup and Tissue Equilibration
This comprehensive protocol integrates all three critical parameters for successful organ bath experimentation, from initial setup to tissue equilibration.
System Preparation
- Physiological Salt Solution: Prepare 5L of fresh Krebs-bicarbonate buffer (composition: 118 mM NaCl, 4.7 mM KCl, 1.2 mM MgSO₄, 1.2 mM KH₂PO₄, 25 mM NaHCO₃, 11 mM glucose, 1.6 mM CaCl₂) [15]. Filter through a 0.2 µm filter to remove particulates.
- Temperature System Activation: Turn on recirculating water bath set to 37°C. Verify water is flowing through all jacketed components (chambers, reservoirs) in series [15].
- Transducer Preparation: Power force transducers at least 15 minutes before experiments to minimize thermal drift. Calibrate according to manufacturer specifications using standard weights [15].
- Aeration System: Fill reservoirs with PSS and begin gassing with 95% Oâ‚‚/5% COâ‚‚. Check that all aeration stones are producing fine, consistent bubbles across all chambers.
Tissue Dissection and Mounting
- Tissue Harvest: Dissect tissue humanely according to institutional animal care guidelines. Immediately place tissue in ice-cold, oxygenated PSS [15]. For vascular tissues, carefully remove adherent fat and connective tissue while preserving endothelial integrity [29] [15].
- Tissue Preparation: Prepare appropriate tissue segments (3-5 mm rings for vessels; 2-3 cm strips for intestinal or tracheal smooth muscle) [15]. Avoid over-stretching or crushing tissue during preparation.
- Mounting Procedure: Thread tissue onto two miniature hooks [15]. Attach one hook to a fixed rod and the other to the force transducer with sutures, ensuring tissue is fully immersed in oxygenated PSS.
Tissue Equilibration and Viability Testing
- Passive Tension Setting: Gradually stretch tissue to its optimal resting tension (e.g., 4g for rat aorta [15]; 1g for smaller vessels). Allow tension to stabilize between increments (10-15 minutes).
- Equilibration Period: Equilibrate tissues for 60-90 minutes with buffer changes every 15 minutes [15]. This stabilizes basal tone and metabolic state.
- Viability Assessment: Test tissue viability with a contractile agonist (e.g., 60 mM KCl for vascular smooth muscle [15] or 10 µM acetylcholine for intestinal strips [17] [10]). A reproducible contraction >0.5g indicates viable tissue.
- Experimental Readiness: After viability confirmation, wash tissue thoroughly and allow return to baseline tension before commencing experimental protocols.
The meticulous optimization of stimulation parameters, temperature control, and aeration management represents a fundamental prerequisite for generating physiologically relevant and reproducible data in isolated organ bath experiments. By systematically implementing the protocols and guidelines presented in this application note, researchers can maintain tissue viability and function throughout extended experimental durations, thereby enhancing the predictive validity of their pharmacological and physiological investigations. As the organ bath technique continues to evolve with technological advancements such as multi-well organ bath systems [2], these core principles of parameter optimization remain essential for bridging the gap between molecular screening approaches and whole-animal physiology, ultimately accelerating the drug discovery process and advancing our understanding of tissue function in health and disease.
Advanced Considerations for Transgenic and Disease Model Tissues
The isolated tissue bath technique stands as a classical pillar in pharmacology and physiology, providing critical insights into receptor characterization and tissue function for over a century [15]. This enduring value persists in modern drug discovery, where organ baths continue to play a vital role in ensuring the efficacy and safety of new therapies by allowing investigators to study living tissues in a controlled environment [1]. When applied to the study of transgenic and disease model tissues, the technique offers unparalleled ability to evaluate physiological outcomes—such as contraction or relaxation—that are directly relevant to whole-body function [15]. However, working with these sophisticated biological tools necessitates advanced methodological considerations to maintain tissue viability, minimize experimental artifacts, and generate pharmacologically relevant data. This application note provides a structured framework for optimizing organ bath protocols specifically for transgenic and disease model tissues, addressing key challenges through quantitative experimental design and rigorous methodology.
Technical Challenges and Optimization Strategies
Genetically modified tissues and disease models present unique challenges in organ bath experimentation due to their frequently altered physiology, increased susceptibility to damage during isolation, and potential for exhibiting non-standard pharmacological responses. The table below summarizes major technical considerations and evidence-based optimization approaches.
Table 1: Key Technical Challenges and Optimization Strategies for Transgenic and Disease Model Tissues
| Challenge | Impact on Experiment | Optimization Strategy | Evidence of Efficacy |
|---|---|---|---|
| Tissue Vulnerability | Reduced viability; declining response over time; increased biomarker release (e.g., LDH, GOT) [9]. | Use of protease inhibitors (e.g., Soybean Trypsin Inhibitor (TI) at 0.1 mg/ml) [9]. | Significantly higher maintained insulin outflow (endocrine) and reduced tissue damage markers in pancreas preparations [9]. |
| Ligand Depletion | Substantial underestimation of compound affinity; inaccurate potency (Kd/Ki) calculations [34]. | Ensure compound concentration >> target concentration; use simulation tools to evaluate and manage depletion artifacts [34]. | Critical for high-affinity compounds; ensures accurate data for lead optimization and human dosing prediction [34]. |
| Altered Baseline Physiology | Non-standard resting tension; suboptimal length-tension relationship; inconsistent viability [15]. | Conduct preliminary experiments to determine tissue-specific optimal passive tension (e.g., 4g for rat thoracic aorta) [15]. | Achieves optimal smooth muscle cell response (Lo); ensures consistent and robust contraction/relaxation responses [15]. |
| Equilibration Artifacts | Non-equilibrium binding conditions; inaccurate assessment of antagonist affinity [34]. | Validate that compounds are at equilibrium with the receptor; extend equilibration times if needed [34]. | Particularly critical for modern high-affinity compounds with slow binding kinetics; prevents data misinterpretation [34]. |
Detailed Experimental Protocol
Tissue Dissection and Preparation
The initial tissue handling phase is critical for preserving the viability and functionality of transgenic and disease models, which may be more susceptible to ischemic or mechanical damage.
- Dissection Buffer and Environment: Perform dissections in a physiological salt solution (PSS) such as modified Tyrode's solution (136.9 mM NaCl, 2.7 mM KCl, 1.8 mM CaCl₂, 1.05 mM MgCl₂, 0.42 mM NaH₂PO₄, 3 mM EDTA, 11.9 mM NaHCO₃, and 5.56 mM glucose) maintained at 4°C to reduce metabolic activity [9]. For tissues prone to self-digestion (e.g., pancreas), include soybean trypsin inhibitor (TI) at 0.1 mg/ml in the dissection buffer to protect against proteolytic damage [9].
- Microdissection Technique: Use a dissecting dish with a silastic foundation to stabilize tissue. Employ fine forceps and vannas scissors to meticulously remove perivascular adipose and connective tissues with minimal traction on the tissue of interest [15]. For tubular structures like aorta, gently thread a guide wire into the lumen to provide stability during cleaning without damaging the endothelial lining [15].
- Tissue Sectioning: Cut cleaned tissues into appropriate segments (e.g., 3-5 mm rings for vascular tissues) using sharp scissors or blades. Place tissues in oxygenated, warmed PSS until mounting [15].
Tissue Mounting and Equilibration
Proper mounting and equilibration establish the foundation for reproducible and physiologically relevant responses.
- Hook Placement and Orientation: For tubular tissues, carefully thread two stainless steel hooks through the lumen of the tissue segment. Ensure one hook has a silk suture with a small knotted loop for attachment to a fixed rod, and the other has a longer suture (10-14 cm) for connection to the force transducer [15].
- Bath Immersion: Mount the tissue in the organ bath containing oxygenated (95% O₂ / 5% CO₂) PSS at 37°C. Ensure the tissue is fully immersed and not touching the sides or bottom of the bath chamber [15].
- Passive Tension Optimization: Gradually increase tension to the predetermined optimal level for the specific tissue type (e.g., 4g for rat thoracic aorta) using a micrometer. Apply tension in increments (e.g., 2g steps), allowing the tissue to plateau between adjustments. Equilibrate tissues for a minimum of 120 minutes with periodic buffer changes (every 20 minutes) until a stable baseline is achieved [15].
Viability Assessment and Experimental Execution
Before proceeding with experimental protocols, validate tissue responsiveness and integrity.
- Viability Testing: Expose tissues to a known contractile agonist (e.g., high-potassium solution or receptor-specific agonist) to confirm robust contractile capacity. Tissues should generate reproducible responses of appropriate magnitude before experimental interventions [15].
- Experimental Design Considerations:
- Cumulative Concentration-Response Curves: Add compounds sequentially in increasing concentrations, allowing the response to plateau at each concentration before adding the next. Include appropriate vehicle controls to account for solvent effects.
- Antagonist Studies: Pre-incubate tissues with antagonists for a sufficient duration to reach equilibrium binding before assessing agonist responses. The required time may vary based on the kinetics of the drug-receptor interaction [34].
- Paired Design: When comparing transgenic versus wild-type tissues, use a paired experimental design where tissues from both genotypes are run simultaneously under identical conditions to minimize inter-experimental variability.
Data Quantification and Pharmacological Analysis
Accurate data interpretation from transgenic and disease model tissues requires careful attention to potential artifacts that may disproportionately affect these specialized preparations.
- Response Normalization: Express contractile responses as a percentage of a reference agonist's maximum effect (e.g., 60 mM KCl) or as active tension developed per tissue cross-sectional area. For relaxation studies, normalize responses as a percentage of pre-contraction induced by a submaximal agonist concentration.
- Affinity Calculation Considerations: Be aware that modern high-affinity compounds and assay systems with target overexpression may violate classical pharmacological assumptions. Use appropriate correction methods and simulation tools when ligand depletion or non-equilibrium conditions are suspected [34].
- Tissue-Specific Biomarkers: For disease models involving specific pathological processes, monitor relevant biomarkers in the bath effluent (e.g., amylase for exocrine pancreas function, LDH/GOT for general tissue damage) to correlate functional responses with tissue integrity [9].
Visualization of Experimental Workflow
The following diagram illustrates the complete experimental workflow for organ bath studies with transgenic and disease model tissues, highlighting critical optimization points.
Figure 1: Experimental workflow for organ bath studies with transgenic and disease model tissues, highlighting critical optimization points for tissue protection and data quality assurance.
Signaling Pathways in Tissue Contraction
Understanding the fundamental signaling mechanisms is essential for interpreting data from transgenic tissues where these pathways may be genetically altered. The diagram below outlines key pathways regulating smooth muscle contraction.
Figure 2: Key signaling pathways mediating agonist-induced smooth muscle contraction in organ bath preparations, showing calcium-dependent and calcium-sensitization mechanisms.
Essential Research Reagent Solutions
The table below catalogues critical reagents and their applications for successful organ bath experimentation with transgenic and disease model tissues.
Table 2: Essential Research Reagents for Organ Bath Experiments with Transgenic Tissues
| Reagent | Specification/Concentration | Primary Function | Application Notes |
|---|---|---|---|
| Physiological Salt Solution (PSS) | Modified Tyrode's solution with 5.56 mM glucose [9]. | Maintains physiological ionic environment and tissue viability. | Must be oxygenated with 95% Oâ‚‚ / 5% COâ‚‚; pH 7.4 [15]. |
| Soybean Trypsin Inhibitor (TI) | 0.1 mg/ml in PSS [9]. | Protects vulnerable tissues from proteolytic degradation. | Critical for pancreas preparations; consider for other enzyme-rich tissues [9]. |
| Kanamycin Selection | Concentration varies by system [35]. | Identifies successfully transfected/transformed cells. | Useful for selecting transgenic tissues with antibiotic resistance markers [35]. |
| Contractile Agonists | e.g., KCl (60 mM), phenylephrine, carbachol. | Validates tissue viability and functionality. | Use for initial viability testing and reference standard for normalization [15]. |
| Target-Specific Agonists/Antagonists | Varies by experimental target. | Characterizes specific receptor pathways. | Pre-validate potency and specificity in the specific transgenic model. |
| Biomarker Assay Kits | ELISA for insulin, amylase, LDH, GOT [9]. | Assesses tissue-specific function and damage. | Monitor bath effluent for real-time assessment of tissue health [9]. |
Organ bath experimentation with transgenic and disease model tissues represents a powerful approach for evaluating physiological function in a controlled ex vivo environment. The successful application of this technique requires meticulous attention to tissue-specific vulnerabilities, particularly through the implementation of protective agents like protease inhibitors and the careful determination of optimal resting tensions. Furthermore, researchers must remain vigilant of potential pharmacological artifacts—especially ligand depletion and non-equilibrium binding—that may disproportionately affect high-affinity compound testing in these valuable and often irreplaceable tissues. By adhering to the optimized protocols and quality control measures outlined in this application note, researchers can maximize the scientific return from transgenic and disease model tissues, generating robust, reproducible data that effectively bridges molecular genetic manipulations with tissue-level physiological function.
Ensuring Reliability and Translational Relevance: Validation, Comparative Analysis, and Beyond
The Caffeine-Halothane Contracture Test (CHCT), also known as the In Vitro Contracture Test (IVCT), remains the gold standard functional assay for diagnosing Malignant Hyperthermia (MH) susceptibility [36] [37]. MH is a potentially fatal pharmacogenetic disorder of skeletal muscle calcium signalling, triggered by volatile anaesthetics and depolarizing muscle relaxants [36]. The CHCT directly measures the exaggerated contracture response of freshly biopsied muscle tissue upon exposure to the triggering agents caffeine and halothane, providing critical diagnostic information where genetic testing is inconclusive [38] [39]. This protocol details the application of organ bath methodology to conduct CHCT, establishing a benchmark for isolated tissue research in pharmacological safety assessment.
Background and Principles
Pathophysiological Basis
Malignant Hyperthermia susceptibility is fundamentally a disorder of calcium signalling, often termed a "couplonopathy" [36]. Underlying alterations in Ca²⺠transients disrupt the normal excitation-contraction (EC) coupling in skeletal muscle. The condition is frequently associated with mutations in RYR1, encoding the calcium release channel of the sarcoplasmic reticulum, though mutations in CACNA1S and STAC3 genes are also implicated [36]. These genetic defects predispose individuals to uncontrolled calcium release from the sarcoplasmic reticulum when exposed to triggering agents, leading to sustained muscle contractures, hypermetabolism, and life-threatening hyperthermia.
Diagnostic Rationale
The CHCT capitalizes on this pathophysiology by quantitatively measuring the abnormal contractile response of viable muscle tissue to caffeine, which directly promotes calcium release from the sarcoplasmic reticulum, and halothane, which potentiates calcium-induced calcium release [36] [38]. The test demonstrates high diagnostic sensitivity (97%) and specificity (78%) when performed according to standardized protocols [40]. Research has identified distinct patient subgroups, including those reacting solely to halothane ("HH" group), who exhibit unique cellular features including elevated resting cytosolic calcium and increased frequency of spontaneous calcium events [36].
Materials and Reagents
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 1: Core Reagents and Solutions for CHCT
| Item | Composition/Specifications | Function |
|---|---|---|
| Krebs-Ringer Solution | NaCl 118.1 mM, KCl 3.4 mM, MgSO₄ 0.8 mM, KH₂PO₄ 1.2 mM, Glucose 11.1 mM, NaHCO₃ 25.0 mM, CaCl₂ 2.5 mM; pH 7.35-7.45 [37] | Physiological buffer for muscle specimen maintenance and testing |
| Caffeine Solutions | 0.5, 1.0, 1.5, 2.0, 3.0, 4.0, and 32 mmol·Lâ»Â¹ (free base, analytical grade) [37] | Direct agonist of ryanodine receptors to trigger calcium release |
| Halothane | 0.5%, 1.0%, 2.0% (0.11, 0.22, 0.44 mmol·Lâ»Â¹) delivered via calibrated vaporizer [37] [41] | Volatile anesthetic potentiating calcium-induced calcium release |
| Muscle Biopsy | Quadriceps (vastus medialis/lateralis), 20-25 mm length, 2-3 mm thickness [37] | Source of viable skeletal muscle for contracture response assessment |
| Organ Bath System | Multi-myograph system (e.g., DMT 620M/820MO) with force transducers, temperature control (37°C), and carboxygenation [37] [3] | Maintains tissue viability and measures isometric contracture forces |
Equipment Specifications
- Organ Bath System: Temperature-controlled tissue baths with continuous carboxygenation (95% Oâ‚‚, 5% COâ‚‚) [3]
- Force Transduction: High-sensitivity transducers capable of detecting contractures ≥0.2 g [37]
- Electrical Stimulation: Field stimulation apparatus delivering supramaximal stimuli (1-2 ms duration, 0.2 Hz) [37]
- Halothane Delivery: Calibrated vaporizer with gas concentration verification via gas chromatography [37] [41]
Experimental Protocol
Pre-test Procedures
Muscle Biopsy and Specimen Preparation
- Biopsy Collection: Obtain muscle biopsy (≥10 years old, minimum body weight considerations) from quadriceps under trigger-free anaesthesia [37]
- Specimen Transport: Immediately place tissue in pre-carboxygenated Krebs-Ringer solution at ambient temperature; maximum transport time 15 minutes from biopsy to laboratory dissection [37]
- Specimen Preparation: Dissect muscle into specimens measuring 20-25 mm length × 2-3 mm thickness (100-200 mg weight) with sutures at both ends [37]
- Time Constraint: Complete all testing within 5 hours post-biopsy to maintain tissue viability [37]
Organ Bath Setup
- Mounting: Secure specimens between fixed electrode and force transducer in tissue baths containing Krebs-Ringer solution at 37°C [37]
- Optimal Length Determination: Stretch muscle to initial force of 2 mN (0.2 g), then apply electrical stimulation (0.2 Hz, 1-2 ms supramaximal stimulus) while adjusting length until optimal twitch response is achieved (typically 120-150% initial length) [37]
- Stabilization: Allow specimens to stabilize at optimal length until baseline force variation is <2.0 mN over 10 minutes [37]
Contracture Testing Protocol
Caffeine Contracture Test (Static Cumulative)
- Concentration Series: Expose muscle specimens to progressively increasing caffeine concentrations: 0.5, 1.0, 1.5, 2.0, 3.0, 4.0, and 32 mmol·Lâ»Â¹ [37]
- Exposure Protocol: Administer each successive concentration once maximum contracture plateau is reached or after 3-minute exposure if no contracture occurs [37]
- Threshold Determination: Record the caffeine threshold as the lowest concentration producing sustained contracture ≥2 mN (0.2 g) from the lowest force reached [37]
- Viability Confirmation: Verify response to 32 mmol·Lâ»Â¹ caffeine ≥50 mN (5 g) at test completion [37]
Halothane Contracture Test (Static)
- Concentration Series: Expose separate muscle specimens to halothane concentrations: 0.5%, 1.0%, 2.0% (0.11, 0.22, 0.44 mmol·Lâ»Â¹) with optional 3.0% (0.66 mmol·Lâ»Â¹) [37]
- Vaporizer Calibration: Use serviced, calibrated vaporizer with regular concentration verification via gas chromatography [37] [41]
- Exposure Protocol: Maintain each concentration for at least 3 minutes or until maximum contracture is achieved [37]
- Threshold Determination: Record the halothane threshold as the lowest concentration producing contracture ≥2 mN (0.2 g) [37]
Quality Assurance Measures
- Concentration Validation: Quantitatively verify halothane and caffeine concentrations in tissue baths every 6 months (±10% deviation acceptable) [37] [41]
- Control Specimens: Test 30 control muscle samples before commencing diagnostic program [37]
- Viability Criteria: Initial twitch response ≥10 mN (1 g) and response to 32 mmol·Lâ»Â¹ caffeine ≥50 mN (5 g) [37]
Data Analysis and Interpretation
Diagnostic Thresholds and Classification
Table 2: CHCT Diagnostic Criteria and Classification [37] [40]
| Diagnostic Category | Caffeine Threshold | Halothane Threshold | Clinical Interpretation |
|---|---|---|---|
| MHN (MH Negative) | ≥3.0 mmol·Lâ»Â¹ in all tests | >0.44 mmol·Lâ»Â¹ in all tests | Not susceptible to MH |
| MHSh (Halothane Only) | ≥3.0 mmol·Lâ»Â¹ in all tests | ≤0.44 mmol·Lâ»Â¹ in ≥1 test | MH susceptible, distinct pathophysiology [36] |
| MHSc (Caffeine Only) | ≤2.0 mmol·Lâ»Â¹ in ≥1 test | >0.44 mmol·Lâ»Â¹ in all tests | MH susceptible |
| MHShc (Both) | ≤2.0 mmol·Lâ»Â¹ in ≥1 test | ≤0.44 mmol·Lâ»Â¹ in ≥1 test | MH susceptible |
The North American protocol defines positive CHCT as contracture ≥0.7 g with 3% halothane or ≥0.3 g with 2 mM caffeine [36] [40]. Patients testing positive to halothane only (HH subgroup) demonstrate unique cellular characteristics including elevated resting cytosolic calcium and increased spontaneous calcium event frequency, suggesting pathophysiology rooted in excess calcium leak through sarcoplasmic reticulum channels [36].
Performance Characteristics
- Sensitivity: 97% (95% CI: 84-100%) when using thresholds of ≤0.5 g contracture at 3% halothane or ≤0.3 g at 2 mM caffeine [40]
- Specificity: 78% (95% CI: 69-85%) with the above thresholds [40]
- Predictive Factors: Male sex, normal muscle strength, and personal MH history correlate with positive IVCT results [39]
Troubleshooting and Technical Considerations
Common Technical Challenges
- Halothane Concentration Variability: Tissue bath concentrations often measure lower than nominal vaporizer settings; require regular monitoring via gas chromatography [41]
- Specimen Viability: Strict adherence to time constraints (≤5 hours biopsy-to-test completion) and viability criteria (twitch ≥10 mN) is essential [37]
- Alternative Anaesthetics: Halothane remains the strongest discriminator for MH; sevoflurane is ineffective while enflurane, isoflurane, and desflurane show intermediate efficacy [38]
Methodological Variations
- European vs. North American Protocols: EMHG IVCT uses threshold concentration approach while North American CHCT employs fixed concentration with force measurement [37] [40]
- Dynamic Halothane Testing: Optional methodology incorporating stretching/relaxation cycles for additional assessment [37]
Applications in Research and Development
The CHCT protocol exemplifies rigorous organ bath methodology with direct applications in:
- Pharmacological Safety Screening: Assessing potential MH-triggering properties of novel compounds [3]
- Pathophysiological Investigation: Elucidating calcium signalling abnormalities in MH and related myopathies [36]
- Genotype-Phenotype Correlation: Linking RYR1/CACNA1S variants with functional contracture responses [36] [39]
The comprehensive standardization of the CHCT, from precise reagent concentration verification to strict diagnostic thresholds, establishes a benchmark protocol for organ bath experiments requiring high sensitivity and specificity in assessing pharmacological responses in isolated tissue.
Isolated tissue bath methodologies, first developed in 1904, remain fundamental tools in pharmacology, physiology, and drug discovery research [4]. These ex vivo systems allow investigators to study the contractile and relaxant properties of various tissues under controlled conditions, providing crucial insights into mechanisms of drug action, receptor function, and disease pathophysiology. The two principal systems for these investigations—organ baths and wire myographs—share common physiological principles but differ significantly in their technical applications and experimental capabilities. Understanding their distinct strengths and limitations is essential for designing rigorous, reproducible experiments that yield physiologically relevant data.
The historical significance of these methodologies cannot be overstated. Nobel Prize-winning research by Otto Loewi that identified acetylcholine as a neurotransmitter utilized tissue bath techniques, as did Robert Furchgott's discovery of endothelium-derived relaxing factor (EDRF), later identified as nitric oxide [8] [4]. These foundational discoveries established isolated tissue research as a "gold standard" for investigating nerve-muscle interactions and vascular function, a status it maintains in modern drug development pipelines and clinical diagnostics, including the caffeine-halothane contracture test for malignant hyperthermia susceptibility [4].
Technical Comparison: System Specifications and Applications
Key Differences Between Organ Baths and Wire Myographs
Organ baths and wire myographs serve complementary roles in the isolated tissue research laboratory. Their selection depends primarily on tissue dimensions, the physiological parameters of interest, and the required measurement sensitivity.
Table 1: System Comparison - Organ Baths vs. Wire Myographs
| Parameter | Organ Bath System | Wire Myograph System |
|---|---|---|
| Typical Vessel/Tissue Size | Larger vessels and tissue strips (≥2 mm diameter) [8] | Small resistance arteries and arterioles (∼150-250 μm) [8] [42] |
| Mounting Method | Pins, hooks, or clamps for longitudinal or circular orientation [43] [8] | Horizontal mounting between two stainless steel jaws or wires [43] [8] |
| Chamber Volume | Larger bath volume (typically 10-50 mL) [43] | Low-volume chamber for high sensitivity [43] |
| Force Transduction | Standard isometric force transducers [8] | High-sensitivity transducers capable of detecting micro-Newton forces [8] |
| Primary Applications | Vasoconstriction, bronchodilatation, GI motility, bladder activity, cardiac muscle contractility [8] | Vascular reactivity of resistance arteries, pharmacological studies of microvessels [8] [42] |
| Physiological Relevance | Suitable for various muscle types; less physiological for small resistance vessels | More accurate for resistance vessels controlling organ-specific blood flow [8] |
| Experimental Throughput | Multiple tissues can be run in parallel [4] | Typically fewer simultaneous experiments |
| Operator Skill Required | Moderate technical expertise | High level of operator skill; months of practice often needed [8] |
Quantitative Considerations for Experimental Design
Proper experimental design requires understanding the biophysical principles underlying each method. In wire myography, the "normalization" procedure establishes optimal baseline tension for measuring contractile responses. This process determines the internal circumference of the vessel that corresponds to a transmural pressure of 100 mmHg (IC100), after which tension is typically reduced to 0.9×IC100 to achieve optimal contractility [44]. However, this standard may vary by vessel type—porcine retinal arterioles perform better at 0.9×IC70, while pulmonary arteries require IC20 to reflect their low-pressure physiological environment [44].
Table 2: Normalization Parameters for Different Rat Artery Types in Wire Myography
| Artery Type | Inner Diameter at 0.9×IC100 (μm) | Passive Tension (mN/mm) | Calculated Transmural Pressure (mmHg) |
|---|---|---|---|
| Mesenteric Resistance Artery | 273 | 2.93 | 53 |
| Saphenous Artery | 280 | 3.10 | 55 |
| Cerebral Artery | 201 | 1.60 | 39 |
For organ bath studies, the key consideration is tissue viability. Muscle bundles typically require minimal dimensions (1-3 mm diameter, >3 cm length) and must generate sufficient baseline force (e.g., >1 g twitch force for skeletal muscle) to ensure physiological relevance [4].
Experimental Protocols and Methodologies
Standardized Protocol for Wire Myography
Wire myography requires meticulous technique to study small resistance arteries without damaging these delicate structures. The following protocol outlines critical steps for reproducible experiments:
Tissue Dissection and Mounting: Isolate vessels in cold, oxygenated physiological saline solution (PSS). Under a dissection microscope, carefully remove connective and adipose tissue. Mount the vessel segment between two parallel wires in the myograph chamber, ensuring the wires pass through the lumen without stretching or tearing the tissue [44] [8].
Normalization Procedure: Begin by determining the internal circumference of the vessel under a passive transmural pressure of 100 mmHg (IC100) using the Laplace relationship. Subsequently, set the internal circumference to 0.9×IC100, which establishes optimal resting tension for most arterial preparations. Confirm passive conditions by performing this step in calcium-free PSS to avoid stretch-induced active tone development [44].
Viability Testing and Maximum Contraction Assessment: Challenge the vessel with a high-potassium solution (e.g., 60-120 mM K⺠PSS) to depolarize smooth muscle cells and elicit a reference contraction. Then, expose the vessel to a known contractile agonist (e.g., phenylephrine, norepinephrine, U46619) at a concentration that produces maximum contraction (e.g., 10â»âµ M). This step establishes the vessel's maximum contractile capacity and serves as a reference for normalizing subsequent responses [44] [42].
Endothelial Integrity Verification: Pre-contract the vessel to approximately 50-80% of its maximum capacity with a contractile agonist. Once a stable plateau is achieved, add an endothelium-dependent vasodilator (e.g., acetylcholine 10â»âµ M for arteries; substance P for veins). A relaxation ≥80% indicates a functionally intact endothelium [44] [42].
Experimental Protocol Execution: Conduct cumulative concentration-response curves or single-concentration challenges according to the experimental design. Include appropriate controls (vehicle, positive controls) and maintain consistent washing and equilibration periods between interventions.
Wire Myography Experimental Workflow
Standardized Protocol for Organ Bath Studies
Organ bath methodologies adapt to various tissue types, including vascular rings, airway smooth muscle, gastrointestinal strips, and cardiac muscle. This protocol outlines a generalized approach:
Tissue Preparation and Mounting: Dissect the target tissue in oxygenated, cold PSS. For vascular rings, carefully clean adherent tissue and mount between two parallel hooks—one fixed and one connected to an isometric force transducer. Maintain optimal resting tension specific to the tissue type (e.g., 2-4 g for rat aortic rings, 1-2 g for smaller arteries) [8] [4].
Equilibration and Viability Assessment: Allow tissues to equilibrate for 60-90 minutes in oxygenated PSS at physiological temperature (typically 37°C), with buffer changes every 15-20 minutes. Assess tissue viability using a reference contractile agent appropriate for the tissue type (e.g., potassium chloride for vascular smooth muscle, carbachol for airway smooth muscle) [4].
Experimental Protocol Execution: Conduct cumulative concentration-response curves with thorough washing and re-equilibration between agonist applications. For complex protocols investigating nerve-mediated responses, include electrical field stimulation parameters specific to the tissue and innervation pattern.
Data Normalization and Analysis: Express contractile responses as a percentage of the maximum response to a reference agonist or as absolute force development (e.g., mN/mm for vascular tissues). For tissues with variable dimensions, normalize responses to tissue cross-sectional area, wet weight, or protein content [4].
Research Reagent Solutions and Essential Materials
Successful isolated tissue research requires specific pharmacological tools and physiological solutions. The following table details essential reagents and their applications:
Table 3: Essential Research Reagents for Isolated Tissue Studies
| Reagent Category | Specific Examples | Primary Function | Experimental Application |
|---|---|---|---|
| Physiological Salt Solutions | Krebs-Henseleit, Physiological Salt Solution (PSS), Tyrode's | Maintain physiological ion concentrations and osmolarity | Provides basal maintenance environment for all isolated tissues |
| Contractile Agonists | Phenylephrine (α1-adrenergic), Norepinephrine (α-adrenergic), U46619 (thromboxane mimetic), Endothelin-1, Potassium Chloride | Induce vascular smooth muscle contraction | Assessing contractile function; pre-contracting vessels for relaxation studies |
| Endothelium-Dependent Vasodilators | Acetylcholine, Substance P, Bradykinin, ATP | Stimulate endothelial-dependent relaxation pathways | Assessing endothelial function via NO, prostaglandin, and EDHF pathways |
| Endothelium-Independent Vasodilators | Sodium Nitroprusside (NO donor), Nitroglycerin, Forskolin (adenylyl cyclase activator), Isoproterenol (β-adrenergic) | Directly relax vascular smooth muscle | Assessing smooth muscle function independent of endothelium |
| Signaling Pathway Inhibitors | L-NAME (NOS inhibitor), Indomethacin (cyclooxygenase inhibitor), ODQ (sGC inhibitor), Iberiotoxin (BKCa channel blocker) | Inhibit specific signaling pathways | Mechanistic studies to dissect contribution of specific pathways |
| Ion Channel Modulators | Nifedipine (L-type Ca2+ channel blocker), Tetraethylammonium (K+ channel blocker), Ouabain (Na+/K+ ATPase inhibitor) | Modulate membrane potential and ion flux | Investigating role of specific ion channels in vascular tone |
Signaling Pathways in Vascular Tone Regulation
Vascular tone regulation involves complex interactions between multiple cell types and signaling systems. The following diagram illustrates key pathways modulating contraction and relaxation in vascular smooth muscle, particularly relevant to interpreting organ bath and myography data:
Signaling Pathways in Vascular Tone Regulation
Selecting between organ baths and wire myographs requires careful consideration of research objectives, tissue availability, and technical expertise. Organ baths offer versatility for diverse tissue types and are ideal for studying larger vessels, cardiac muscle, and pharmacological mechanisms across multiple parallel preparations. Wire myographs provide superior sensitivity for resistance arteries that dictate peripheral vascular resistance and are essential for translational research on hypertension, diabetes, and other microvascular disorders.
The enduring value of both methodologies lies in their ability to bridge molecular mechanisms with integrated tissue function, preserving critical cell-cell interactions and mechanical environments that are lost in isolated cell systems [44]. By applying the standardized protocols and analytical frameworks presented herein, researchers can maximize the rigor, reproducibility, and physiological relevance of their investigations, continuing the legacy of these classic physiological techniques in contemporary biomedical discovery.
The isolated tissue bath technique, first developed in 1904, remains a cornerstone in pharmacology and physiology research for evaluating contractile tissue function [4]. This ex vivo approach allows researchers to investigate physiological responses and pharmacological effects in a controlled environment. However, the ultimate translational value of this method depends on effectively correlating these isolated findings with in vivo outcomes. This application note details standardized protocols and analytical frameworks to bridge this critical gap, enhancing the predictive power of organ bath experiments in drug development and basic research.
The Scientific Basis of Organ Bath Experiments
Organ baths provide a simple yet powerful solution to assess contractile tissue function by maintaining isolated tissues in a physiologically supportive environment [4]. The fundamental principle involves measuring isometric contraction of tissue samples in response to various pharmacological agents or electrical stimulation, allowing for the characterization of concentration-response relationships and receptor pharmacology [15].
The continued relevance of this technique stems from several key advantages:
- Tissue Integrity: The tissue functions as an integrated system, synthesizing drug-receptor interactions, signal transduction, second messenger generation, and changes in tissue contractility [15].
- Pharmacological Characterization: Enables determination of critical pharmacological parameters (efficacy, potency) in a tissue context that more closely resembles in vivo conditions than cellular assays [15].
- Versatility: Applicable to various tissue types, from blood vessels [15] and skeletal muscle [4] to gastrointestinal [10] and urinary tract smooth muscle [45].
Experimental Protocols
System Setup and Tissue Preparation
Materials and Reagents
- Physiological Salt Solution (PSS) or Krebs-Ringer bicarbonate (KRB) solution
- 95% Oâ‚‚ / 5% COâ‚‚ medical grade gas mixture
- Dissection tools (forceps, scissors, dissection microscope)
- Silk sutures and tissue hooks
Protocol
Solution Preparation: Prepare 5L of PSS containing (in mM): NaCl (119), KCl (4.7), MgSO₄ (1.2), KH₂PO₄ (1.2), NaHCO₃ (25), CaCl₂ (1.6), and glucose (11) [15]. Bubble continuously with 95% O₂ / 5% CO₂ to maintain pH at 7.4.
System Configuration:
- Preheat the water-jacketed tissue bath system to 37°C using a recirculating heated water bath [15].
- Connect the system to the gas mixture and check for consistent aeration without excessive tissue movement [15].
- Calibrate force transducers at least 15 minutes before experimentation to minimize thermal drift [15].
Tissue Dissection and Mounting:
- Dissect fresh tissue samples (e.g., thoracic aorta, colon, bladder) and place immediately in oxygenated PSS [15].
- For aortic rings: Clean perivascular adipose tissue and cut into 3-5 mm wide rings [15].
- Mount tissue between two hooks: one attached to a stable mount and the other to a force transducer using silk sutures [15].
- For skeletal muscle: Prepare bundles measuring 1-3 mm in diameter and >3 cm in length [4].
Tissue Equilibration and Viability Testing
Protocol
Passive Tension Setting:
- Gradually increase tension to the predetermined optimal level for the specific tissue type (e.g., 4g for rat thoracic aorta) [15].
- Allow tissue to plateau between tension increments until stable baseline is achieved.
Viability Assessment:
- For skeletal muscle: Verify tissue viability by confirming elicitation of minimum 1g twitch force with supramaximal electrical stimulation (1ms pulse width) [4].
- For smooth muscle: Test tissue responsiveness to standard agonists (e.g., high-potassium solution) to confirm contractile capability.
Experimental Execution and Data Acquisition
Protocol
Pharmacological Challenges:
Electrical Field Stimulation (EFS):
- Apply EFS parameters appropriate for the tissue type (typically 0.5-20Hz, 1ms pulse width) to stimulate intrinsic nerves [10].
- Use neural blockers (e.g., tetrodotoxin) to confirm neurogenic responses.
Data Recording:
- Continuously record isometric force using computer-based data acquisition systems [15].
- Mark all drug additions and experimental manipulations in the recording software for accurate data analysis.
Correlation Framework: Connecting Ex Vivo and In Vivo Data
The following diagram illustrates the strategic workflow for correlating ex vivo findings with in vivo outcomes:
Quantitative Correlation Strategies
Table: Framework for Correlating Ex Vivo and In Vivo Data
| Ex Vivo Parameter | Corresponding In Vivo Measure | Correlation Strategy | Interpretation Considerations |
|---|---|---|---|
| ECâ‚…â‚€ / ICâ‚…â‚€ values | Therapeutic dose range | Compare potency rankings across compound series | Account for pharmacokinetics and metabolism |
| Maximum efficacy (Eₘâ‚â‚“) | Magnitude of physiological effect | Normalize responses to internal standards | Consider compensatory mechanisms in vivo |
| Receptor specificity profile | Side effect incidence | Map tissue distribution of target receptors | Evaluate target engagement biomarkers |
| Signal transduction mechanisms | Molecular imaging data | Validate pathway activation through tissue analysis | Assess redundant pathways in intact systems |
| Tissue-specific responses | Organ-level functional measures | Compare response patterns across tissues | Consider neural and hormonal influences |
Case Study: Lower Urinary Tract Function
The differential innervation of bladder and urethral smooth muscle provides an excellent example of successful ex vivo-in vivo correlation:
Ex vivo studies demonstrate that bladder detrusor muscle contracts in response to cholinergic stimulation via muscarinic receptors, while urethral smooth muscle contracts primarily to adrenergic agonists via α1-adrenoceptors [45]. This differential pharmacology accurately predicts the reciprocal bladder-urethral relationship observed in vivo, where sympathetic activation promotes urine storage while parasympathetic activation enables voiding [45]. This correlation has direct therapeutic applications for urinary incontinence treatment.
Research Reagent Solutions
Table: Essential Reagents for Organ Bath Experiments
| Reagent/Category | Function/Application | Example Compounds | Considerations |
|---|---|---|---|
| Physiological Solutions | Maintain tissue viability and ionic balance | Krebs-Ringer bicarbonate, Physiological Salt Solution | Must be oxygenated, pH 7.4, 37°C |
| Receptor Agonists | Activate specific receptors to elicit tissue response | Acetylcholine (cholinergic), Phenylephrine (α-adrenergic) | Use cumulative concentrations for CRC |
| Receptor Antagonists | Block specific receptors to study mechanism | Atropine (muscarinic), Phentolamine (α-adrenergic) | Pre-incubation typically required |
| Neuromodulators | Study neural components of tissue response | Substance P, Neuromodulators affecting NO neurons [46] | Electrical field stimulation often combined |
| Signal Transduction Modifiers | Investigate intracellular pathways | Various kinase inhibitors, calcium channel blockers | Specificity and concentration critical |
| Diagnostic Agents | Clinical correlation and disease modeling | Caffeine, Halothane for MH susceptibility testing [4] | Follow standardized clinical protocols |
Advanced Applications and Techniques
Clinical Diagnostic Applications
The caffeine-halothane contracture test for malignant hyperthermia (MH) susceptibility demonstrates successful translation of organ bath methodology to clinical diagnostics. This standardized protocol uses fresh human skeletal muscle biopsies to assess exaggerated contracture responses to caffeine and halothane, identifying individuals at risk for life-threatening hypermetabolic reactions to anesthesia [4]. The test exhibits 97% sensitivity and 78% specificity in diagnosing MH susceptibility [4].
Integration with Modern Technologies
Contemporary organ bath research increasingly incorporates advanced analytical approaches:
- Stem Cell-Derived Neurons: hPSC-derived nitrergic neurons can be engrafted to improve gut dysmotility in model systems, creating novel platforms for therapeutic development [46].
- Functional Assessment Combinations: Organ bath data can be correlated with molecular analyses (e.g., immunohistochemistry for neuronal markers like substance P or nNOS) to provide comprehensive mechanistic insights [10].
- High-Throughput Adaptation: Modern systems enable parallel operation of multiple tissue baths (e.g., 24 baths simultaneously), significantly accelerating data collection [4].
The isolated tissue bath remains an indispensable tool in pharmacological and physiological research when properly correlated with in vivo outcomes. By implementing standardized protocols, systematic correlation frameworks, and integrative analytical approaches, researchers can significantly enhance the translational predictive value of ex vivo findings. This bridge between isolated tissue responses and whole-organism physiology continues to drive therapeutic innovation across multiple disease domains, from cardiovascular disorders to gastrointestinal and urinary tract conditions.
The Role of Organ Baths in Modern Drug Discovery and Development Pipelines
Organ bath systems remain a cornerstone in pharmacological research, bridging the gap between high-throughput in silico screening and complex whole-animal models. This application note details the experimental protocols for conducting organ bath experiments with isolated tissues, highlighting their enduring value in assessing drug efficacy and safety within modern drug development pipelines. We provide comprehensive methodologies for tissue preparation, system setup, and data interpretation, specifically framed for researchers, scientists, and drug development professionals engaged in lead compound validation and mechanism-of-action studies.
Despite the proliferation of high-throughput screening (HTS) and in silico platforms in early drug discovery, these approaches often produce hits that prove invalid in more complex biological systems [2]. Organ bath techniques maintain critical relevance by enabling functional assessment of drug effects on intact tissues, preserving native cellular architecture, receptor distributions, and signaling pathways [1]. The technology has evolved from traditional single-bath setups to modern multi-well systems that enhance throughput while conserving valuable compounds [2]. This document outlines standardized protocols for organ bath experimentation, focusing on practical implementation for drug discovery applications.
Key Applications in Drug Discovery
Organ bath systems provide critical functional data across multiple stages of drug development:
Table 1: Key Applications of Organ Bath Systems in Drug Discovery
| Application Area | Specific Uses | Common Tissue Models |
|---|---|---|
| Cardiovascular Pharmacology | Vasoconstrictor/vasodilator screening, mechanism studies | Rat aorta, mesenteric arteries, human saphenous arteries [47] [2] |
| Metabolic Disease Research | Insulin secretion studies, pancreatic function | Isolated rat pancreas preparations [9] |
| Respiratory Drug Development | Bronchodilator screening, airway reactivity | Rat trachea, guinea pig airways, swine bronchial rings [2] |
| Safety Pharmacology | Off-target effects on smooth/ cardiac muscle | Various isolated tissue preparations [1] |
| Lead Optimization | Potency (ECâ‚…â‚€) and efficacy (Eₘâ‚â‚“) determination | Tissue-specific target organs [2] |
Material and Methods
Research Reagent Solutions
Table 2: Essential Reagents and Materials for Organ Bath Experiments
| Item Name | Function/Application | Example Specifications |
|---|---|---|
| Modified Tyrode's Solution | Physiological salt solution for tissue maintenance | 136.9 mM NaCl, 2.7 mM KCl, 1.8 mM CaCl₂, 1.05 mM MgCl₂, 0.42 mM NaH₂PO₄, 3 mM EDTA, 11.9 mM NaHCO₃, 5.56 mM glucose [9] |
| Krebs-HEPES Buffer | Alternative physiological buffer for multi-well systems | Standard saline buffer for MuWOB technology [2] |
| Soybean Trypsin Inhibitor (TI) | Prevents tissue autodigestion in pancreatic studies | 0.1 mg/ml in modified Tyrode's solution [9] |
| Enzyme Inhibitors | Protect tissue integrity during experimentation | Various concentrations based on tissue type and experiment duration |
| Pharmacological Agonists/Antagonists | Receptor characterization, pathway modulation | Phenylephrine (α1-adrenergic agonist), prazosin (α1-adrenergic antagonist) [2] |
Experimental Workflow
The following diagram illustrates the standard workflow for conducting organ bath experiments in drug discovery applications:
Tissue Preparation and Mounting Protocol
Tissue Isolation
- Animal Models: Use male Wistar rats (225-300 g) for vascular studies; humane euthanasia following approved institutional guidelines [9] [47].
- Organ Harvesting: Excise target tissue (e.g., thoracic aorta, pancreas, trachea) and immediately immerse in ice-cold, oxygenated physiological buffer [9] [47].
- Tissue Preparation: For aortic rings, clean connective tissue and cut into 1-1.5 mm wide rings [47] [2]. For pancreatic studies, divide into lobes (right lobe has higher β-cell area) [9].
Mounting Techniques
- Traditional Baths: Mount tissues between fixed hooks and isometric force transducers (IFT) in 4-50 ml organ baths [2] [48].
- Multi-Well Systems: For MuWOB technology, place individual tissue rings in 96-well plates with ~100 µl buffer [2].
- Optimal Resting Tension: Apply passive tension appropriate to tissue type (e.g., 1-2 g for rat aorta) to approximate in vivo conditions.
System Configuration and Experimental Setup
Environmental Control
- Temperature Maintenance: Circulate heated water through jacketed baths or use incubators for multi-well plates (37°C for mammalian tissues) [2].
- Oxygenation: Continuously bubble with carbogen (95% Oâ‚‚/5% COâ‚‚) to maintain pH ~7.4 [9].
- Buffer Exchange: Implement regular buffer replacement (every 20 min during equilibration) to maintain tissue viability [9].
Data Acquisition Systems
- Force Transducers: Connect to data acquisition systems (e.g., PowerLab-16) for continuous tension recording [2].
- Optical Monitoring: For MuWOB systems, use charged-coupled device (CCD) cameras with bi-telecentric optics to track luminal area changes [2].
- Sampling Frequency: Capture data at 0.1 Hz for sufficient temporal resolution of contractile responses [2].
Advanced Methodological Applications
Protocol: Investigating Insulin Secretion from Isolated Pancreas
Objective: Quantify compound effects on insulin secretion using rat pancreas preparations.
Step-by-Step Procedure:
- Tissue Preparation: Remove whole pancreas and immerse in modified Tyrode's solution with 5.56 mM glucose [9].
- Trypsin Inhibition: Add soybean trypsin inhibitor (0.1 mg/ml) to prevent autodigestive injury [9].
- Experimental Timeline:
- Equilibration: 120 min with buffer changes every 20 min
- Baseline collection: -20 to 0 min
- Compound application: 0-40 min with sampling every 20 min
- Sample Analysis: Measure insulin concentration using Ultra Sensitive Rat Insulin ELISA Kit [9].
- Tissue Viability Assessment: Quantify amylase outflow and measure GOT/LDH activities as tissue damage markers [9].
Protocol: Vascular Reactivity Studies Using Aortic Rings
Objective: Characterize vasoactive properties of novel compounds.
Step-by-Step Procedure:
- Tissue Mounting: Suspend aortic rings between two hooks in organ baths containing Krebs-HEPES buffer [2].
- Viability Testing: Apply high potassium solution or receptor agonist (e.g., phenylephrine) to confirm tissue responsiveness.
- Experimental Design:
- Generate cumulative concentration-response curves for test compounds
- Include appropriate reference agonists/antagonists
- For antagonist studies, pre-incubate tissue before agonist challenge
- Data Normalization: Express responses as percentage of maximal reference agonist effect or as absolute tension changes.
- Mechanistic Studies: Use pathway-specific inhibitors to elucidate mechanisms of action (e.g., L-type Ca²⺠channel blockers) [2].
Technology Comparison
Table 3: Comparison of Organ Bath Technologies
| Parameter | Traditional Organ Bath | Multi-Well Organ Bath (MuWOB) |
|---|---|---|
| Throughput | 4-16 channels typically [2] | 96 wells simultaneously [2] |
| Buffer Volume | 4-50 ml per tissue [2] | ~100 µl per well [2] |
| Drug Consumption | High (mg range) [2] | Low (µg range) [2] |
| Detection Method | Isometric force transducers [48] | Optical measurement (CCD camera) [2] |
| Automation Potential | Low, manual operations [2] | High, compatible with liquid handlers [2] |
| Primary Applications | Detailed mechanistic studies [1] | Medium-throughput compound screening [2] |
Technical Considerations and Troubleshooting
Optimization Strategies
- Tissue Viability: Monitor enzyme release (amylase, LDH) as tissue damage indicators; implement trypsin inhibition for pancreatic tissues [9].
- Experimental Duration: Control for time-dependent declines in insulin secretion (pancreas) or contractile responses through appropriate experimental design [9].
- Segment Selection: Consider functional differences between tissue regions (e.g., higher β-cell area in duodenal pancreatic segment) [9].
Data Interpretation
Organ bath systems provide rich pharmacological data including:
- Potency Measures: ECâ‚…â‚€ values from concentration-response curves [2]
- Efficacy Assessment: Maximal response (Eₘâ‚â‚“) compared to reference compounds [2]
- Mechanistic Insights: Receptor identification through selective antagonists [2]
- Safety Profiling: Off-target effects on various tissue types [1]
Organ bath methodologies continue to provide indispensable functional data in drug discovery pipelines, complementing target-based screening approaches. The adaptation of these classical techniques to modern platforms like MuWOB technology enables medium-throughput compound assessment while preserving physiological relevance. The protocols detailed in this application note provide researchers with robust methodologies for evaluating novel therapeutic agents across multiple tissue systems, facilitating informed decisions in lead optimization and candidate selection.
Conclusion
Organ bath experimentation remains an indispensable and highly versatile tool in biomedical research, successfully bridging the gap between cellular assays and complex whole-organism studies. Its enduring value, demonstrated by over a century of contributions from seminal neurotransmitter discovery to modern clinical diagnostics and drug development, is secured by a robust methodological framework. Mastering foundational principles, meticulous protocol execution, and strategic data normalization is paramount for generating reliable, reproducible results. As research evolves with more complex disease models and sophisticated therapeutic candidates, the organ bath continues to adapt, proving critical for validating target engagement and physiological efficacy. Future directions will likely see deeper integration with molecular biology techniques and advanced biosensing, further solidifying its role in accelerating the translation of promising discoveries from the bench to the bedside.
References
- 1. The Enduring Value of Organ Baths in Modern Drug ... [https://www.reprocell.com/blog/biopta/the-enduring-value-of-organ-baths-in-modern-drug-discovery]
- 2. The rebirth of isolated organ contraction studies for drug ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644621004979]
- 3. Tissue Organ Bath - DMT [https://www.dmt.dk/tissue.html]
- 4. In vitro contractile studies within isolated tissue baths [https://pmc.ncbi.nlm.nih.gov/articles/PMC9014520/]
- 5. Isolated Tissue Bath Setups [https://mdegmbh.eu/isolated-tissue-bath-setups/]
- 6. Measurement of Smooth Muscle Function in the Isolated ... [https://www.jove.com/t/52324/measurement-smooth-muscle-function-isolated-tissue-bath-applications]
- 7. Introducing the DMT Organ Bath System [https://www.dmt.dk/blog/introducing-the-dmt-organ-bath-system]
- 8. Isolated Organ / Tissue Baths & Wire Myographs [https://www.reprocell.com/drug-efficacy-safety-adme/platform-technologies/organ-baths-wire-myographs]
- 9. Development of an organ bath technique for isolated rat ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7220716/]
- 10. Ex Vivo Study of Colon Health, Contractility and Innervation ... [https://www.mdpi.com/2304-8158/13/16/2474]
- 11. Three benefits of Isolated Organ Research [https://www.adinstruments.com/blog/three-benefits-isolated-organ-research?srsltid=AfmBOor0UQqa_sdWTdIqKJMrwrpjxMAuE17craFfqWLjCRp6q7Yrxb3v]
- 12. A microphysiological system for studying barrier health of ... [https://www.nature.com/articles/s44172-024-00285-2]
- 13. Protocol for optimizing culture conditions for ex vivo ... [https://www.sciencedirect.com/science/article/pii/S2666166725001285]
- 14. Before Entering the Pharmacology Laboratory [https://basicmedicalkey.com/before-entering-the-pharmacology-laboratory/]
- 15. Measurement of Smooth Muscle Function in the Isolated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354551/]
- 16. Organ bath [https://en.wikipedia.org/wiki/Organ_bath]
- 17. Contractility of isolated colonic smooth muscle strips from ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1304609/full]
- 18. Quantifying Patterns of Smooth Muscle Motility in the Gut and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5900429/]
- 19. Blunt dissection for tissue expander placement in curved ... [https://link.springer.com/article/10.1007/s00238-025-02348-9]
- 20. Long-Term Preservation of Human Head and Neck ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469029/]
- 21. Passive mechanical properties of adipose tissue and ... [https://www.sciencedirect.com/science/article/abs/pii/S175161612400208X]
- 22. Non-linear Scaling of Passive Mechanical Properties in ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2020.00211/full]
- 23. Whole Muscle Length-Tension Relationships are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3003754/]
- 24. Protocol for the generation and differentiation of thymic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182356/]
- 25. Quantifying the passive stretching response of human ... [https://www.sciencedirect.com/science/article/abs/pii/S0268003313002763]
- 26. Contractile force in electrically stimulated human ... [https://www.reprocell.com/drug-efficacy-safety-adme/assay-catalog/contractile-force-electrically-stimulated-human-ventricular-trabeculae-muscle-adrenoceptor-research]
- 27. Acridocarpus smeathmannii root extracts inhibit human ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1621346/full]
- 28. Organ Bath System - 820MO - DMT [https://www.dmt.dk/organ-bath-820mo.html]
- 29. Measurement of Smooth Muscle Function in the Isolated ... [https://www.jove.com/v/52324/measurement-smooth-muscle-function-isolated-tissue-bath-applications]
- 30. Protocol for generating and analyzing organ-on-chip using ... [https://www.sciencedirect.com/science/article/pii/S2666166724002028]
- 31. Normalization of organ bath contraction data for tissue ... [https://pubmed.ncbi.nlm.nih.gov/31511953/]
- 32. Investigating the Pharmacological Impact of Atosiban, an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467195/]
- 33. Isolated organ/tissue test – organ bath [https://www.panlab.com/en/tests-solutions/isolated-organ-tissue-test-organ-bath]
- 34. The Problems of Applying Classical Pharmacology ... [https://www.sciencedirect.com/science/article/pii/S2472555222067351]
- 35. New Method Makes Transgene-Free Gene Editing Even More ... [https://today.uconn.edu/2025/11/new-method-makes-transgene-free-gene-editing-even-more-promising/]
- 36. Abnormal calcium signalling and the caffeine–halothane ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6334558/]
- 37. In vitro contracture testing (IVCT) [https://www.emhg.org/testing-for-mh/2017/12/28/in-vitro-contracture-testing-ivct]
- 38. In-vitro contracture testing for susceptibility to malignant ... [https://pubmed.ncbi.nlm.nih.gov/20827211/]
- 39. Predictive factors of the contracture test for diagnosing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10068564/]
- 40. The sensitivity and specificity of the caffeine-halothane ... [https://pure.psu.edu/en/publications/the-sensitivity-and-specificity-of-the-caffeine-halothane-contrac/]
- 41. Update of the quality assurance (QA) results of halothane and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4139678/]
- 42. Guidelines for the measurement of vascular function and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8321813/]
- 43. Wire Myograph vs Organ Bath - BLOG - DMT [https://www.dmt.dk/blog/wire-myograph-vs-organ-bath]
- 44. Myography of isolated blood vessels: Considerations for ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2023.1176748/full]
- 45. Laboratory practical to study the differential innervation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7474251/]
- 46. Engrafted nitrergic neurons derived from hPSCs improve ... [https://www.nature.com/articles/s41586-025-09208-3]
- 47. Pharmacological evidence for a key role of voltage-gated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1575342/]
- 48. Pharmacology organ bath setup equipment Illustration and ... [https://mindthegraph.com/illustrations/pharmacology-organ-bath-setup-equipment/]