A Comprehensive Guide to Validating Receptor Occupancy Assays for Robust Target Engagement Measurement
This article provides a detailed framework for the development, optimization, and validation of receptor occupancy (RO) assays, critical pharmacodynamic biomarkers in biopharmaceutical development.
A Comprehensive Guide to Validating Receptor Occupancy Assays for Robust Target Engagement Measurement
Abstract
This article provides a detailed framework for the development, optimization, and validation of receptor occupancy (RO) assays, critical pharmacodynamic biomarkers in biopharmaceutical development. Tailored for researchers and drug development professionals, it covers foundational RO concepts, core methodological approaches, and strategies for troubleshooting complex challenges like receptor modulation and low antigen expression. A strong emphasis is placed on fit-for-purpose validation practices per clinical guidelines to ensure reliable data generation. By synthesizing best practices from recent scientific literature and industry case studies, this guide aims to equip scientists with the knowledge to deploy robust RO assays that effectively inform dose selection, establish PK/PD relationships, and de-risk clinical development.
Understanding Receptor Occupancy: The Cornerstone of Target Engagement and PK/PD Modeling
Receptor occupancy (RO) assays have emerged as indispensable tools in preclinical and clinical drug development, providing a direct measure of target engagement for protein-based therapies and small molecules. These assays quantify the binding of a therapeutic compound to its specific cellular target, offering crucial insights into the pharmacokinetic-pharmacodynamic (PK/PD) relationships that determine drug efficacy [1] [2]. In the context of first-in-human clinical studies, RO data contribute significantly to PK/PD modeling, enabling the selection of a safe starting dose and rational dose escalation schemes [2]. The fundamental value of RO measurements lies in their ability to demonstrate whether administered doses and their schedules achieve predicted levels of target engagement and whether the receptor undergoes modulation upon therapeutic engagement [2].
The application of RO assays extends beyond dose selection to include comparing clinical efficacy between new modalities and existing therapies targeting the same cell surface antigen, as well as evaluating additional clinical indications [2]. Flow and mass cytometry have proven ideal platforms for these assays because they enable advanced phenotyping of the cellular subsets expressing the drug target receptors [2]. However, the interpretation of RO data requires careful consideration of assay methodology and biological context, as different assay formats can yield substantially different results despite measuring the same underlying phenomenon [3].
Fundamental Concepts and Methodological Approaches
Core Principles of Receptor Occupancy
At its essence, receptor occupancy represents the proportion of total surface receptors occupied by a drug at a given time [3]. This measurement serves as an initial step toward initiating pharmacodynamic effects, though target engagement does not necessarily guarantee functional outcomes due to numerous factors affecting clinical response, including anti-drug antibodies, immune cell infiltration, exhaustion, and tumor mutational burden [3]. The concept applies equally to both large molecule therapeutics (such as monoclonal antibodies) and small molecules (such as clopidogrel), though the technical approaches for measuring engagement differ substantially based on the compound's characteristics [4] [3].
The biological complexity of receptor dynamics presents significant challenges for accurate RO measurement. Receptor internalization, degradation, shedding, and modulation can all complicate interpretation of RO data [1] [3]. Furthermore, the timing of measurement relative to drug administration critically influences the results, as peak occupancy immediately after infusion often differs substantially from trough levels measured just before the next dose [3]. Understanding these dynamics requires not only robust assay methodology but also appropriate mathematical modeling to interpret the results in the context of the underlying biology [3].
Key Methodologies for Measuring Receptor Occupancy
Table 1: Comparison of Major Receptor Occupancy Assay Formats
| Assay Type | Key Reagents | Measurement Principle | Optimal Applications | Technical Limitations |
|---|---|---|---|---|
| Competitive Flow Cytometry | Competitive and non-competitive antibodies [1] | Competitive antibody binds only unoccupied receptors; non-competitive antibody measures total receptors [1] | Protein therapeutics, cell surface targets, when specific antibodies are available [1] | Requires specific antibody pairs; affected by receptor internalization/modulation [1] |
| Saturation Flow Cytometry | Drug product and detection antibody [1] | Half of sample saturated with drug (100% RO); ratio of drug-binding between saturated/unsaturated samples reveals RO [1] | When competitive/non-competitive antibodies are unavailable [1] | May overestimate occupancy if saturation incomplete; requires careful controls [1] |
| LC-MS/MS for Small Molecules | MS tag, surfactants, reducing agents [4] | Labels unoccupied receptors with MS tag; conditional release of tag and drug for quantification [4] | Small molecule drugs, covalent inhibitors, when real-time assessment needed [4] | Technically challenging; requires specialized expertise and equipment [4] |
| Radiotracer Methods | Radioactive ligands (e.g., ³³P-2MeS-ADP) [4] | Competitive binding of radioactive tracer to unoccupied receptors [4] | Historical approach for small molecules | Specificity concerns; radioactive handling requirements; limited temporal resolution [4] |
Experimental Protocols for Key RO Assays
Flow Cytometry-Based Competitive RO Assay Protocol
The flow cytometry competitive assay represents one of the most widely implemented approaches for protein therapeutics. The protocol begins with sample preparation, where fresh whole blood or PBMCs are typically preferred to preserve native receptor expression and binding characteristics [5]. For the staining procedure, two parallel tubes are prepared: one containing a competitive antibody that binds exclusively to unoccupied receptors, and another containing a non-competitive antibody that binds to a different epitope regardless of drug occupancy [1]. The competitive antibody can be substituted with an anti-drug antibody in some configurations [1].
The panel design incorporates phenotypic markers to gate on specific cell populations of interest, enabling RO measurement only in relevant cellular subsets [1]. Acquisition and analysis proceed with flow cytometry data collection, followed by calculation of RO using the formula: RO (%) = [1 - (MFI competitive antibody / MFI non-competitive antibody)] × 100 [1]. This approach normalizes for potential changes in receptor expression levels during treatment. The assay requires rigorous validation including assessment of sample stability, precision, accuracy, and robustness, with particular attention to potential interference from biological matrices [1].
LC-MS/MS-Based RO Assay for Small Molecules
For small molecule therapeutics like clopidogrel, LC-MS/MS offers an alternative approach with real-time assessment capabilities. The protocol for platelet P2Y12 receptor occupancy begins with platelet isolation from blood samples followed by targeted labeling of unoccupied P2Y12 receptors with a mass spectrometry tag [4]. The key innovation in this methodology involves leveraging the chemical properties of the disulfide bond that forms between clopidogrel's active metabolite and the cysteine residue of the P2Y12 receptor [4].
The sample processing phase includes conditional release of both the active metabolite and the MS tag from the P2Y12 complexes through careful manipulation of disulfide bonds [4]. These released compounds serve as small molecular surrogate analytes for occupied and unoccupied platelet P2Y12 receptors, respectively [4]. LC-MS/MS analysis then precisely quantifies the proportion of occupied versus unoccupied target receptors, enabled by the exceptional sensitivity, selectivity, and efficiency of modern mass spectrometry systems [4]. This approach has demonstrated direct correlation between receptor occupancy and antiaggregant activity in animal models, supporting its use as a pharmacodynamic biomarker [4].
Signaling Pathways and Experimental Workflows
PD-1 Signaling Pathway and Nivolumab Mechanism
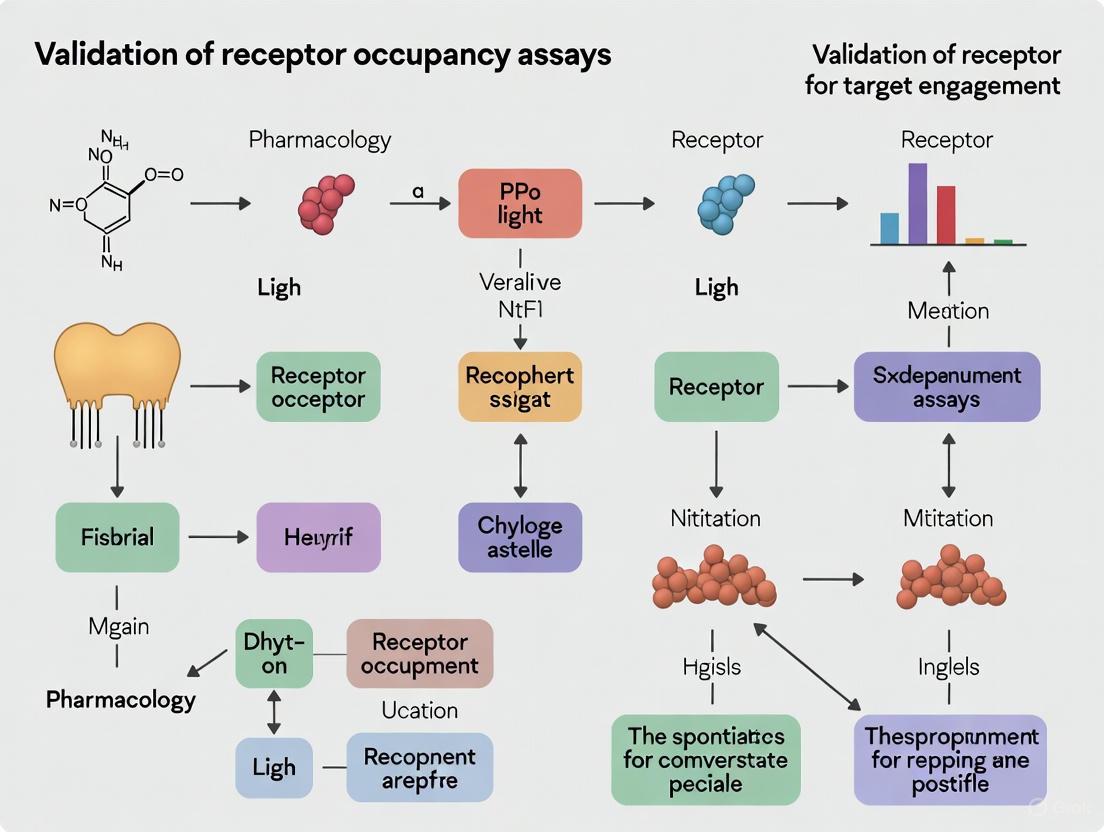
Figure 1: PD-1 Immune Checkpoint Signaling and Therapeutic Blockade
The programmed cell death 1 (PD-1) pathway represents a clinically validated target for receptor occupancy assessment. As illustrated in Figure 1, PD-1 is predominantly expressed on activated T cells and functions as an immune checkpoint receptor that maintains self-tolerance by suppressing T-cell activity [3]. The binding of PD-1 to its natural ligands PD-L1 and PD-L2 initiates a signaling cascade that recruits SHP2 phosphatase, ultimately attenuating T-cell receptor (TCR) signaling and diminishing T-cell effector functions [3]. Therapeutic antibodies like nivolumab (Opdivo) bind to PD-1 and prevent interaction with its ligands, thereby restoring T-cell-mediated immune responses against cancer cells [3]. The occupancy measurement of PD-1 by nivolumab has proven crucial for understanding its pharmacokinetic-pharmacodynamic relationships, though different assay methodologies have produced apparently discordant results in clinical studies [3].
Integrated Workflow for Receptor Occupancy Assessment
Figure 2: Integrated Receptor Occupancy Assessment Workflow
The comprehensive workflow for receptor occupancy assessment (Figure 2) begins with appropriate sample collection and processing, where sample matrix selection profoundly impacts assay quality [1]. Fresh whole blood is often preferred for RO assays because receptor binding can be disrupted by cell isolation or cryopreservation procedures [5]. The choice of assay methodology depends on the therapeutic modality (large vs. small molecule) and reagent availability [1] [4]. Data analysis must account for the specific calculation method employed, as different normalization approaches (e.g., to baseline vs. total receptors at each timepoint) can yield substantially different occupancy values [3]. Finally, integration of RO data with pharmacokinetic parameters and pharmacodynamic outcomes enables sophisticated modeling to inform dose selection and optimization strategies [1] [2].
Critical Research Reagents and Materials
Table 2: Essential Research Reagent Solutions for RO Assays
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Competitive Antibodies | Bind specifically to unoccupied target receptors; quantify free receptor pool [1] | Must recognize same epitope as drug; specificity validation critical [1] |
| Non-competitive Antibodies | Bind to different epitope than drug; quantify total receptor population [1] | Epitope mapping essential to ensure no interference with drug binding [1] |
| Viability Dyes | Distinguish live/dead cells in flow cytometry; improve accuracy [1] | Must be compatible with other fluorophores; minimal spillover [1] |
| Phenotypic Markers | Identify specific cell populations of interest; enable gating strategies [1] | Panel design must account for spectral overlap; titration required [1] |
| MS Tag Compounds | Label unoccupied receptors for LC-MS/MS detection (small molecules) [4] | Reactivity must be specific; should not disrupt native interactions [4] |
| Stabilization Buffers | Preserve receptor expression and binding during processing/storage [5] | Matrix effects must be evaluated; vacutainer selection important [1] |
| Surfactants | Solubilize membrane proteins for LC-MS/MS (e.g., P2Y12) [4] | Concentration optimization critical; can impair MS response [4] |
| Reducing Agents | Conditionally release drugs/tags from receptor complexes [4] | Must not disrupt native disulfide bonds; specificity challenging [4] |
Interpretation Challenges and Normalization Strategies
The interpretation of receptor occupancy data requires careful consideration of the mathematical approaches used for calculation, as different normalization strategies can produce substantially different results. Research has identified four primary equations used for RO assessment, each with distinct implications for data interpretation [3]:
Table 3: Receptor Occupancy Normalization Strategies and Implications
| Normalization Strategy | Calculation Method | Typical Output Range | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Free Receptor to Baseline | RO = 1 - (FreeR / FreeR_baseline) [3] | Higher reported occupancy [3] | Direct measurement of available receptors; intuitive | Requires reliable baseline measurement; affected by receptor dynamics |
| Free Receptor to Timepoint | RO = BoundR / (BoundR + FreeR) [3] | High reported occupancy [3] | Self-contained at each timepoint; no baseline needed | May miss receptor downregulation effects |
| Bound Receptor to Baseline | RO = BoundR / TotalR_baseline [3] | Lower reported occupancy [3] | Accounts for receptor modulation; clinically relevant | Highly dependent on accurate baseline |
| Bound Receptor to Timepoint | RO = BoundR / (BoundR + FreeR) [3] | Moderate to high occupancy [3] | Internally consistent; less variable | May overestimate functional engagement |
The choice between these normalization strategies explains apparently discordant clinical results, such as those observed with nivolumab where different assays reported trough RO values of approximately 70% versus ≥90% despite similar dosing regimens [3]. This discrepancy arises particularly when the internalization rate of bound receptors exceeds the degradation rate of free receptors, creating differential dynamics in the receptor pools being measured [3]. Understanding these subtleties is essential for appropriate interpretation of RO data across studies and for making valid comparisons between different therapeutic approaches targeting the same receptor.
Emerging Trends and Advanced Applications
The field of receptor occupancy assessment continues to evolve with emerging technologies and methodologies enhancing the accuracy and reliability of these assays. Advanced technologies like single-cell RNA sequencing and high-dimensional flow cytometry promise even deeper insights into drug-receptor interactions by enabling more detailed cellular phenotyping and identification of rare cell populations [1]. Complex RO assays now provide additional insights into receptor internalization and shedding, contributing to a more comprehensive understanding of drug-target interactions [1].
The application of quantitative systems pharmacology (QSP) modeling to RO data represents another significant advancement, enabling more sophisticated interpretation of the relationship between target engagement and functional outcomes [3]. These models incorporate specific features of RO assays, including whether they measure free or bound receptors and whether normalization occurs to baseline or at each timepoint, to provide mechanistic explanations for observed clinical results [3]. The integration of real-time assessment capabilities, particularly for small molecule drugs like clopidogrel, addresses previous limitations in temporal resolution and provides more dynamic understanding of target engagement [4]. As these technologies mature, they hold potential to further revolutionize drug development by providing more precise and detailed pharmacodynamic data to inform decision-making.
The Crucial Role of RO Data in Dose Selection and Optimization for Clinical Trials
Receptor occupancy (RO) assays are flow cytometry-based pharmacodynamic biomarkers designed to quantify the binding of a therapeutic agent to its specific target on the cell surface [6] [5]. These assays provide critical data on target engagement, establishing a direct link between pharmacokinetics (PK) and pharmacodynamics (PD) that informs dose-response relationships [6]. In the development of biopharmaceuticals, particularly monoclonal antibodies and other immuno-modulatory therapies, RO measurements have become indispensable for rational dose selection, helping to bridge findings from nonclinical safety studies to first-in-human (FIH) clinical trials [6] [3]. By measuring the percentage of target receptors occupied by a drug, researchers can optimize dosing regimens to achieve sufficient therapeutic effect while minimizing potential risks, thereby addressing the pharmaceutical industry's challenges of rising development costs and decreasing approval rates [6].
The clinical significance of RO was starkly demonstrated by the TGN1412 incident, where a starting dose calculated based on no adverse effect level (NOAEL) in nonhuman primates led to life-threatening cytokine release syndrome in healthy volunteers [6]. Retrospective analysis showed that the administered dose resulted in approximately 90% RO of CD28, whereas a MABEL approach targeting only 10% RO would have recommended a starting dose 30,000 times lower [6]. This case underscores the critical importance of incorporating RO assessments into dose selection strategies, particularly for high-risk therapeutics where toxicity arises from exaggerated pharmacology [6].
RO Assay Formats and Methodologies
Fundamental Assay Formats
There are three primary formats for RO assays, each with distinct applications and limitations based on the drug's mechanism of action and reagent availability [6] [7]:
Free Receptor Assays: These measure the proportion of receptors not bound by drug using a fluorescence-labeled detection reagent that competes with the drug for the same epitope [6]. This format is preferred for antagonistic drugs whose primary mode of action is to block ligand binding [6].
Drug-Occupied Receptor Assays: These quantify the proportion of receptors bound by drug using a non-competitive fluorescence-labeled anti-drug antibody [6]. This approach is particularly valuable when free receptor assays are not feasible [6].
Total Receptor Assays: These measure both free and drug-occupied receptors, typically using an anti-receptor antibody that binds to an epitope distinct from the drug's binding site [6]. This format is ideal when the drug affects receptor regulation or when target-expressing cells are ablated [6].
Experimental Protocols and Workflows
The development of a robust RO assay requires careful planning and validation. Below is a generalized workflow for RO assay development and implementation:
Figure 1: RO Assay Development and Implementation Workflow
For reliable RO assessment, fresh whole blood specimens are typically preferred because receptor binding can be disrupted by cell isolation or cryopreservation [6] [5]. The assay must be customized to the specific drug and receptor biology, accounting for factors such as receptor internalization, downregulation, or cell trafficking that could complicate data interpretation [5]. A critical component of assay development involves creating a calibration curve showing saturating conditions of the drug, which will be used to quantify RO in clinical samples [7].
Research Reagent Solutions
The following table details essential materials and reagents required for implementing RO assays in clinical trials:
Table 1: Essential Research Reagents for RO Assays
| Reagent Type | Function | Application Considerations |
|---|---|---|
| Fluorescence-labeled detection antibodies | Quantify free, occupied, or total receptors | Must not compete with drug binding; requires testing of different clones and fluorochromes [7] |
| Anti-drug antibodies (ADA) | Detect drug-occupied receptors | Should be non-neutralizing and non-competitive with drug binding [6] |
| Cell surface staining antibodies | Identify target cell populations | Dependent on target abundance and receptor density [6] |
| Compensation beads | Adjust for fluorochrome spectral overlap | Critical for multicolor flow cytometry panels [7] |
| Viability dyes | Exclude dead cells from analysis | Improves assay accuracy by reducing non-specific binding [8] |
| Stabilization reagents | Preserve receptor expression | Essential for maintaining sample integrity during transportation [5] |
RO Data Interpretation and PK/PD Modeling
Calculation Methods and Normalization Approaches
The interpretation of RO data requires careful consideration of the calculation method employed, as different approaches can yield substantially different results [3]. RO is fundamentally defined as the proportion of total surface receptors occupied by a drug, but flow cytometry-based assays vary in their normalization strategies:
- Normalization to Baseline: This approach calculates RO using baseline receptor levels as the denominator, which can be problematic if receptor expression changes during the study [3].
- Normalization at Each Time Point: This method uses contemporaneous total receptor measurements, potentially providing more accurate occupancy estimates when receptor dynamics are in flux [3].
The impact of normalization strategy was clearly demonstrated in studies of nivolumab, an anti-PD-1 antibody, where different calculation methods explained discrepant RO results (70% vs. ≥90%) reported in separate clinical trials [3]. When the internalization rate of bound receptors exceeds the degradation rate of free receptors, RO values generated by different normalization approaches can diverge significantly [3].
Integration with PK/PD Modeling
Mechanism-based PK/PD models are frequently constructed to describe quantitative relationships between drug concentrations and RO [6]. These models become particularly powerful when incorporating RO data from animal studies to predict human receptor occupancy for dose selection [6]. The integration of RO measurements into PK/PD modeling enables researchers to:
- Establish exposure-response relationships early in clinical development
- Identify optimal biological dosing regimens
- Support dose justification to regulatory agencies
- Facilitate translation from nonclinical to clinical studies
For therapeutics with nonlinear pharmacokinetics, RO can sometimes be theoretically derived through mechanistic PK/PD modeling, though direct measurement is generally preferred when feasible [6].
Comparative Analysis of RO Assay Performance
Case Studies in Drug Development
RO assays have been successfully applied across various therapeutic areas, providing critical insights for dose optimization:
Table 2: Comparative RO Assay Applications in Clinical Development
| Therapeutic Agent | Target | Assay Format | Key Finding | Impact on Dose Selection |
|---|---|---|---|---|
| Nivolumab [3] | PD-1 | Bound receptor with different normalization methods | Explained discrepant RO results (70% vs ≥90%) between studies | Supported flat dosing regimens (240 mg Q2W or 480 mg Q4W) |
| Leronlimab [8] | CCR5 | Two independent calculation methods | Full RO achieved with weekly 700 mg dosing; increased CCR5+CD4+ T cells | Established dosing for HIV and other indications |
| TGN1412 [6] | CD28 | Not specified (retrospective analysis) | 90% RO associated with cytokine release syndrome | MABEL approach with 10% RO would have recommended 30,000x lower dose |
| Immuno-modulatory therapy [5] | CD6 | Not specified | Enabled batched flow cytometry testing on stabilized blood | Facilitated dose optimization for autoimmune diseases |
Methodological Comparisons
The selection of appropriate RO assay format depends heavily on the drug's mechanism of action and biological context:
Figure 2: RO Assay Format Selection Based on Mechanism of Action
Each assay format presents distinct advantages and limitations. Free receptor assays directly measure the pharmacologically relevant target available for drug binding but may be affected by changes in total receptor levels [6]. Drug-occupied receptor assays provide direct evidence of target engagement but require specific anti-drug reagents [6]. Total receptor assays are essential when the drug modulates receptor expression levels or when target-expressing cells are depleted [6].
Implementation Challenges and Solutions
Technical and Logistical Considerations
Implementing RO assays in clinical trials presents numerous technical and logistical challenges that must be addressed to ensure data quality:
- Sample Stability: RO is commonly measured by flow cytometry on fresh blood specimens due to potential receptor instability [6]. Careful stability assessments are needed to define acceptable sample processing windows [5].
- Assay Reproducibility: Standardization is crucial for global trials where multiple laboratories may be involved [7]. This includes harmonized sample preparation, instrument setup, and operator training [7].
- Receptor Dynamics: Biological factors such as receptor internalization, downregulation, or cellular trafficking can complicate RO interpretation [6] [5].
- Specimen Logistics: For time-sensitive assays, laboratories in close proximity to clinical sites are often necessary unless signal stabilization methods are established [7].
Strategies for Robust RO Assessment
To overcome these challenges, several strategic approaches have been developed:
- Comprehensive Validation: RO assays should undergo rigorous validation tailored to the study phase and endpoint [7]. For secondary endpoints reported to regulatory agencies, validation should include linearity and sensitivity assessments [7].
- Assay Transfer Protocols: Successful transfer to multiple laboratories requires standardized instruments, reference values, and detailed standard operating procedures [7].
- Control Strategies: Appropriate controls including isotype controls, fluorescence minus one controls, and experimental controls ensure assay performance matches clinical sample characteristics [7].
- Data Normalization: When receptor levels change during treatment, normalization strategies must be carefully considered to avoid misinterpretation [6].
Receptor occupancy data have emerged as a critical tool in clinical development, providing a direct measure of target engagement that bridges pharmacokinetic exposure to pharmacodynamic response. The strategic implementation of RO assays enables more rational dose selection and optimization, potentially reducing the risk of adverse events while ensuring therapeutic efficacy. As demonstrated across multiple therapeutic areas, including immuno-oncology, HIV, and autoimmune diseases, RO measurements provide invaluable insights for dose justification and regimen optimization.
The successful application of RO data requires careful assay design, appropriate format selection, and thoughtful interpretation within the context of the drug's mechanism of action. By addressing technical challenges through standardized methodologies and comprehensive validation, RO assays can generate high-quality data to support drug development decisions. As targeted therapies continue to evolve, the role of RO assessment in clinical trials will likely expand, further solidifying its position as a cornerstone of pharmacodynamic biomarker science.
The 2006 phase I clinical trial of TGN1412, a CD28 superagonist monoclonal antibody, resulted in a catastrophic cytokine storm and multiorgan failure in six healthy volunteers, representing a pivotal failure in preclinical risk prediction [9] [10]. This review examines how receptor occupancy (RO) assessment could have prevented this tragedy by providing critical pharmacodynamic data for safer dose selection. We compare different RO assay methodologies, present experimental protocols for target engagement research, and analyze quantitative data from the TGN1412 case study. Incorporating RO assessment into development workflows now represents a standard approach for de-risking first-in-human trials of potent immunomodulators, particularly those with species-specific biological differences.
TGN1412 was a humanized monoclonal antibody developed as an immunotherapeutic for B-cell chronic lymphocytic leukemia and rheumatoid arthritis [11]. As a CD28 "superagonist," it could activate T-cells without the need for prior T-cell receptor engagement, potentially expanding regulatory T-cells to suppress autoimmune responses [9] [12]. Preclinical studies in rodents using the analogous antibody JJ316 showed therapeutic benefits in autoimmune disease models, while toxicology studies in cynomolgus monkeys demonstrated excellent tolerance at doses up to 50 mg/kg [9] [11].
Despite these promising preclinical results, the first-in-human trial in March 2006 resulted in a life-threatening "cytokine storm" in all six healthy volunteers within 90 minutes of administration [9] [10]. Patients developed systemic inflammatory responses characterized by rapid induction of proinflammatory cytokines, leading to headache, myalgia, nausea, diarrhea, erythema, vasodilation, and hypotension [9]. All volunteers subsequently developed critical illness with pulmonary infiltrates, renal failure, and disseminated intravascular coagulation, requiring intensive care support including mechanical ventilation and dialysis [9] [10].
Post-trial investigation revealed that the formulated product contained no contaminants and matched material used in preclinical testing [10]. The disaster was attributed to unforeseen biological effects in humans not predicted by standard preclinical models, highlighting critical limitations in existing approaches to dose extrapolation and risk assessment for novel therapeutic mechanisms [9] [12].
The Role of Receptor Occupancy in Dose Selection
What is Receptor Occupancy?
Receptor occupancy (RO) is a pharmacodynamic biomarker that quantifies the binding of a biotherapeutic to its cellular target [6] [13]. RO assays measure the percentage of target receptors occupied by a therapeutic agent, providing a direct assessment of target engagement that can be correlated with pharmacokinetic profiles to establish PK/PD relationships [6] [14]. These relationships are crucial for informing dose decisions throughout drug development [6].
RO Assay Formats
Three primary RO assay formats exist, each with distinct applications and limitations:
Table 1: Comparison of Receptor Occupancy Assay Formats
| Assay Format | Measurement Target | Detection Method | Best Applications | Limitations |
|---|---|---|---|---|
| Free Receptor | Receptors not bound by drug | Fluorescence-labeled competitive antibody or drug itself | Antagonistic drugs that block ligand binding | May not detect internalized receptors |
| Drug-Occupied Receptor | Receptors bound by drug | Anti-drug antibody that doesn't compete with binding | When monoclonal antibodies to receptor are unavailable | Requires specific anti-drug antibodies |
| Total Receptor | Both free and drug-occupied receptors | Non-competing antibody to different epitope | When receptor levels change during treatment | Doesn't distinguish between free and occupied states |
Each format employs different detection strategies. Free receptor assays use competitive binding approaches, where a labeled detection reagent binds only to unoccupied receptors [6] [13]. Drug-occupied receptor formats utilize anti-drug antibodies to detect bound therapeutic [6]. Total receptor assays employ non-competing antibodies that bind to epitopes distinct from the drug binding site [6] [1].
TGN1412: A Retrospective RO Analysis
The TGN1412 case exemplifies the critical importance of RO assessment in dose selection. Subsequent analysis revealed that the starting dose of 0.1 mg/kg resulted in >90% receptor occupancy, essentially achieving maximum pharmacological effect [11]. This represented an inappropriate starting point for a potent immunostimulatory agent with a novel mechanism.
Table 2: Quantitative Dose Analysis of TGN1412
| Parameter | Actual 2006 Trial | Recommended Safe Approach | Difference Factor |
|---|---|---|---|
| Starting Dose | 0.1 mg/kg | 0.001 mg/kg (1 μg/kg) | 100-fold |
| Receptor Occupancy | >90% | <10% | >9-fold |
| Dose Calculation Basis | NOAEL from monkeys | MABEL with RO assessment | Inappropriate model |
| Monkey-Human Correlation | Poor (biological differences) | Species-specific RO assessment | Critical limitation |
Post-hoc calculations based on the Minimal Anticipated Biological Effect Level (MABEL) approach and RO modeling suggested a safe starting dose of 1 μg/kg would have achieved approximately 10% receptor occupancy, while 5 μg/kg would have yielded about 33% occupancy [11]. This alternative approach would have been 100-fold more conservative than the actual starting dose. Notably, TGN1412 (now TAB08) has subsequently been administered safely to healthy volunteers at doses of 0.1-7 μg/kg, confirming the viability of this lower dosing strategy [11].
Experimental Approaches for RO Assessment
Flow Cytometry-Based RO Protocols
Flow cytometry represents the primary methodology for RO assessment due to its ability to simultaneously measure receptor binding and characterize specific cell populations [6] [13]. The basic workflow involves:
Sample Preparation: RO assays are typically performed on fresh whole blood specimens collected in anticoagulant-containing tubes [6]. Peripheral blood mononuclear cells (PBMCs) may be isolated via density gradient centrifugation, though some assays perform direct staining in whole blood followed by red blood cell lysis [15]. Sample stability is critical, with considerations for shipment time, temperature, and potential use of stabilizing reagents [14].
Detection Strategies: The specific staining protocol varies by assay format. For free receptor detection, samples are incubated with fluorescently-labeled competitive antibodies that bind unoccupied receptors [6] [1]. For drug-occupied receptor detection, anti-drug antibodies are employed [6]. Multi-parameter flow cytometry panels typically include phenotypic markers to identify specific cell populations alongside RO measurements [1].
Data Analysis: RO is calculated by comparing pre-dose and post-dose measurements. For free receptor assays, RO % = (1 - [free receptor post-dose]/[free receptor pre-dose]) × 100 [6]. Normalization to pre-dose baseline accounts for inter-subject variability in receptor expression [13].
Advanced RO Methodologies
Saturation Assays: When competitive or non-competitive antibodies are unavailable, saturation assays provide an alternative approach [1]. This method involves splitting samples into two aliquots—one saturated with excess drug to mimic 100% RO, and another untreated. The ratio of drug binding between saturated and unsaturated samples determines RO [1].
Total Drug-Bound Format: For therapeutics with engineered Fc regions (e.g., IgG1 P329GLALA), specialized detection antibodies can be developed that specifically recognize the modified Fc portion, enabling precise quantification of cell-bound therapeutic [15].
Research Reagent Solutions for RO Assays
Successful RO assay implementation requires carefully selected reagents and controls:
Table 3: Essential Research Reagents for RO Assay Development
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Detection Antibodies | Competitive antibodies, non-competitive antibodies, anti-drug antibodies | Quantify free, total, or drug-occupied receptors | Specificity, affinity, fluorochrome brightness |
| Sample Collection | Sodium heparin tubes, stabilizing fixative tubes (Smart Tube, Transfix) | Maintain sample integrity during processing | Compatibility with target antigen, stability requirements |
| Cell Identification | CD45, CD3, CD4, CD8, lineage-specific markers | Identify target cell populations | Panel design to avoid spectral overlap |
| Reference Controls | Isotype controls, biological controls (pre-dose samples) | Establish background signal and baseline | Critical for assay normalization |
| Therapeutic Analog | Labeled drug product | Direct detection of drug binding | May require specialized conjugation approaches |
Biological Mechanisms: Why Preclinical Models Failed
Species-Specific Differences in CD28 Biology
Investigations following the TGN1412 incident identified crucial species-specific differences in CD28 expression patterns that explained the failure of preclinical models to predict human toxicity:
Research demonstrated that CD4+ effector memory T-cells were the primary source of proinflammatory cytokines in the TGN1412 response [12]. These cells rapidly produced IL-2 and IFN-γ when stimulated by superagonistic anti-CD28 antibodies [12]. Crucially, unlike humans, cynomolgus monkeys lack CD28 expression on their CD4+ effector memory T-cell population [12]. This fundamental immunological difference meant that monkey models were biologically incapable of reproducing the massive cytokine release observed in humans.
In Vitro Model Limitations
Standard in vitro assays also failed to predict TGN1412's effects because the antibody required specific presentation conditions to stimulate maximal T-cell activation [10] [12]. While soluble TGN1412 produced minimal response in human peripheral blood mononuclear cell cultures, immobilizing the antibody onto plastic surfaces (mimicking cell surface presentation) unleashed potent T-cell activation and cytokine production [10]. This presentation requirement was not apparent in standard preclinical testing.
Regulatory Evolution and Current Best Practices
The TGN1412 incident prompted significant regulatory changes aimed at improving safety assessment for high-risk investigational drugs:
MABEL Approach: Regulatory guidance now emphasizes the Minimal Anticipated Biological Effect Level approach for calculating starting doses, particularly for drugs with novel mechanisms or potential for exaggerated pharmacology [11]. This approach considers in vitro potency data and receptor occupancy profiles rather than relying solely on no-observed-adverse-effect-level (NOAEL) from animal studies [6] [11].
Staggered Dosing: Recommendations now specify longer intervals between dosing of individual subjects (typically several weeks) to observe for potential adverse effects before exposing additional participants [9].
Improved Preclinical Models: Enhanced in vitro assays using human cells under appropriate stimulation conditions are now recommended for assessing immunomodulatory agents [10] [12].
The TGN1412 tragedy fundamentally transformed approach to first-in-human trials of high-risk biotherapeutics. Receptor occupancy assessment has emerged as a critical tool for de-risking clinical development by providing quantitative pharmacodynamic data that complements traditional pharmacokinetic and toxicological assessments. The case demonstrates that rigorous RO analysis during preclinical development could have prevented the catastrophic cytokine storm by revealing the inappropriately high level of target engagement at the selected starting dose. Modern drug development programs for immunomodulators now routinely incorporate RO assessment to establish PK/PD relationships, validate species relevance, and guide safe starting dose selection—direct lessons from the TGN1412 experience that continue to protect human trial participants today.
Integrating RO with Pharmacokinetics (PK) to Establish Robust PK/PD Relationships
In the landscape of biotherapeutic development, Receptor Occupancy (RO) assays have emerged as indispensable tools for quantifying the pharmacodynamic (PD) response of a drug, specifically measuring the extent to which a biotherapeutic engages its cellular target [2]. The integration of RO data with pharmacokinetic (PK) profiles establishes a robust PK/PD relationship, creating a foundational framework for understanding the temporal connection between drug concentration in the body and its biological effect [1]. This integration is not merely a technical exercise; it is a strategic necessity that informs critical decisions throughout the drug development pipeline, from lead candidate selection and dose regimen optimization to clinical trial design and regulatory submission [16]. For researchers and drug development professionals, mastering this integration is pivotal for validating target engagement, demonstrating mechanistic proof-of-concept, and ultimately accelerating the development of safer, more effective therapies.
Quantitative PK/PD Integration: Preclinical and Clinical Evidence
The power of integrating RO measurements with PK data is demonstrated by its application across diverse therapeutic areas, from oncology to rare diseases. The following case studies and data summaries illustrate how this approach provides quantitative, data-driven insights for drug development.
Preclinical Application: Enhancing Antibody Delivery to Tumors
A linked PK/PD model was developed to understand how a Smoothened inhibitor (LDE225) primes pancreatic tumors to enhance the delivery of Cetuximab (CTX), an anti-EGFR antibody [17]. The model integrated the plasma and tumor PK of the priming agent with its effects on downstream stromal biomarkers and, crucially, with the in-situ tumor concentrations and receptor occupancy of CTX [17]. This model identified critical physiological parameters for antibody distribution and provided insight into dosing regimens that maximize tumor disposition of therapeutic antibodies under conditions of transient tumor permeability [17].
Clinical Translation and Dose Selection for a Novel Hemophilia Therapy
The regulatory assessment of ALTUVIIIO, a novel recombinant Factor VIII therapy, included a minimal PBPK model to support dose selection for pediatric patients [18]. The model related drug exposure (PK) to a critical PD endpoint: maintaining FVIII activity above a threshold (e.g., >20 IU/dL) to reduce bleeding risk [18]. The PBPK model, which incorporated FcRn recycling pathways, successfully predicted exposure in both adults and children, enabling precise dosing recommendations for a vulnerable population [18].
Table 1: PBPK Model Performance for FVIII Therapy Prediction
| Population | Drug | Dose (IU/kg) | Cmax Prediction Error | AUC Prediction Error |
|---|---|---|---|---|
| Adult | ELOCTATE | 25 | -25% | -11% |
| Adult | ELOCTATE | 65 | -21% | -11% |
| Adult | ALTUVIIIO | 25 | +2% | -8% |
| Adult | ALTUVIIIO | 65 | +2% | -18% |
Table 2: RO Assay Utility Across Clinical Development Phases
| Development Phase | Primary Application of RO Data | Impact on Decision-Making |
|---|---|---|
| Preclinical & Discovery | Guide selection of lead compounds; verify mechanism of action (MOA) [14]. | Prioritizes candidates with optimal binding characteristics. |
| Phase 1 | Identify Minimal Anticipated Biological Effect Level (MABEL) and Pharmacologically Active Doses (PAD) [14]. | Guides safe starting dose and escalation schemes for first-in-human trials [2]. |
| Phase 2 | Assess efficacy of dosing and administration protocols [14]. | Predicts levels of RO and whether the receptor is modulated (up or down) [2]. |
| Phase 3 | Define population PD characteristics for long-term safety and efficacy [14]. | Supports final dosing recommendations and label specifications. |
Methodologies and Experimental Protocols for RO Assessment
A variety of assay formats exist to measure RO, each with distinct advantages and appropriate contexts for use. The choice of methodology depends on reagent availability, the biological question, and the required sensitivity.
Core RO Assay Formats and Workflows
The two principal methodologies for RO assessment are the Competitive Assay and the Saturation Assay [1].
Competitive Assay: This strategy requires two antibodies: a competitive antibody that binds to the same epitope as the drug, and a non-competitive antibody that binds to a different epitope on the same target [1]. The competitive antibody identifies free receptors, while the non-competitive antibody identifies the total receptor pool. RO is calculated based on the difference between total and free receptors.
Saturation Assay: This approach is used when competitive or non-competitive antibodies are unavailable. It involves splitting a sample into two halves. One half is saturated with an excess of the drug, mimicking 100% RO. The other half is left unsaturated, reflecting the in-vivo drug binding. A secondary anti-drug antibody is used to detect the bound drug, and the ratio of signal from the unsaturated to saturated samples reveals the RO level [1].
The following diagram illustrates the logical workflow for selecting and implementing an RO assay strategy, from foundational method selection to data integration.
Advanced and Emerging Methodologies
Beyond flow cytometry, mass spectrometry (MS)-based methods are gaining traction for their precision in measuring target engagement, particularly for covalent drugs. A recent study detailed an intact protein LC-MS assay to quantify the percentage of target engagement (%TE) in biological matrices [19]. This MS-based workflow can directly measure drug-target conjugation, providing a quantitative PD readout that feeds into a specialized intact protein PK/PD (iPK/PD) model. This model outputs critical parameters like drug-target complex half-life and effectively supports a decision tree for covalent drug development from early screening to in-vivo studies [19].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful development and validation of RO assays depend on a suite of critical reagents and tools. The following table details these essential components and their functions in the experimental process.
Table 3: Key Research Reagent Solutions for RO Assays
| Tool / Reagent | Function & Application | Technical Considerations |
|---|---|---|
| Competitive Antibody | Binds the same epitope as the drug; quantifies free, unoccupied receptors [1]. | Must have high specificity and affinity for the target epitope. |
| Non-Competitive Antibody | Binds a different epitope on the target receptor; quantifies total receptor population [1]. | Critical for normalizing data and accounting for receptor modulation. |
| Anti-Drug Antibody | Used in saturation assays to detect the bound therapeutic drug [1]. | Should not interfere with the drug's binding to its receptor. |
| Phenotypic Marker Antibodies | Identify specific cell populations of interest within a complex sample (e.g., PBMCs) [1]. | Enables RO measurement exclusively on relevant cells, improving data accuracy. |
| Stabilizing Sample Tubes | (e.g., Smart Tube, Transfix, CytoChex) preserve cell surface epitopes during shipment [14]. | Mitigates sample degradation, a major challenge for accurate RO measurement. |
| Quantitative Cytometry Standards | Beads or reference cells for instrument calibration and data normalization [2]. | Increases rigor, accuracy, and inter-lab reproducibility of flow cytometry data. |
| MK-0608 | MK-0608, CAS:1001913-41-2, MF:C12H16N4O4, MW:280.28 g/mol | Chemical Reagent |
| GW9662-d5 | GW9662-d5, MF:C13H9ClN2O3, MW:281.70 g/mol | Chemical Reagent |
The systematic integration of Receptor Occupancy assays with Pharmacokinetic profiling represents a paradigm shift in biotherapeutic development, moving beyond empirical dosing to a model-informed, mechanistic approach. As evidenced by the quantitative data and case studies presented, this robust PK/PD relationship is instrumental in de-risking development, optimizing dosing regimens across populations, and providing compelling evidence of target engagement for regulators. With advancements in flow cytometry, mass spectrometry, and sophisticated PBPK modeling, the toolkit available to researchers is more powerful than ever. Embracing this integrated framework is no longer optional but is a critical determinant of success in bringing novel, effective, and safe biologics to patients.
Receptor occupancy (RO) assays are sophisticated analytical methods designed to quantify the precise binding relationship between a therapeutic compound and its specific target on the cell surface. These assays generate crucial pharmacodynamic biomarker data that informs decision-making throughout the drug development pipeline. In an era of rising research costs and declining approval rates, RO data provides a quantitative foundation for establishing pharmacokinetic-pharmacodynamic relationships, enabling more rational dose selection and improving the overall efficiency of clinical trials [6]. By measuring the direct interaction between a drug and its target, RO assays bridge the gap between pharmacokinetic profiles and biological effects, offering a mechanism-based approach to drug development.
The strategic importance of RO was tragically highlighted by the TGN1412 clinical trial incident. In this first-in-human study, a starting dose calculated based on no adverse effect level led to life-threatening cytokine release syndrome in healthy volunteers. Subsequent analysis revealed that this dose resulted in approximately 90% receptor occupancy. A minimum anticipated biological effect level approach based on targeting only 10% RO would have recommended a starting dose 30,000 times lower, potentially averting the adverse outcomes [6]. This case underscores how RO assessment can provide critical safety guidance when traditional toxicology studies may not accurately predict human responses.
RO Assay Formats and Comparative Analysis
Fundamental RO Assay Formats
RO assays are typically implemented in three primary formats, each with distinct advantages and applications in drug development [6]:
Free Receptor Assays: These measure receptors not bound by drug using fluorescent-labeled detection reagents that may include the drug itself, a competitive antibody, or the receptor ligand. This format is particularly valuable for antagonistic drugs whose primary mechanism involves blocking natural ligand binding.
Drug-Occupied Receptor Assays: These quantify receptors bound by therapeutic compounds using anti-drug antibodies that do not compete with target binding. Detection typically employs non-neutralizing anti-idiotypic antibodies or antibodies specific to the drug's Fc region.
Total Receptor Assays: These measure both free and drug-occupied receptors using anti-receptor antibodies binding to non-competing epitopes. This format is essential when drugs modulate receptor expression levels or when receptor-expressing cells are mobilized or ablated.
Table 1: Comparison of RO Assay Formats and Their Applications
| Assay Format | Detection Method | Primary Applications | Technical Considerations |
|---|---|---|---|
| Free Receptor | Labeled drug, competitive antibody, or ligand | Antagonist drugs, target blocking | Most physiologically relevant for antagonists |
| Drug-Occupied Receptor | Non-competitive anti-drug antibody | Direct measurement of drug-target engagement | Requires specialized anti-idiotypic reagents |
| Total Receptor | Non-competing anti-receptor antibody | Receptor modulation, cell ablation, normalization | Essential when receptor levels change during treatment |
Comparative Performance of RO Assay Formats
The selection of an appropriate RO assay format depends on multiple factors including the drug's mechanism of action, reagent availability, and target receptor dynamics. Free receptor assays are generally preferred for antagonistic drugs as they directly measure receptors available for ligand binding. When free receptor assays are not feasible, drug-occupied receptor assays provide a valuable alternative, though free receptor levels must then be derived through PKPD modeling [6].
Total receptor assays offer distinct advantages in scenarios where therapeutic intervention alters receptor expression patterns. For drugs that cause receptor internalization following binding or trigger positive feedback mechanisms that upregulate receptor expression, total receptor measurements enable accurate normalization of free receptor data. This normalization is critical for avoiding misinterpretation of drug effects when receptor levels fluctuate during treatment [6].
Table 2: RO Assay Performance Characteristics Across Therapeutic Areas
| Therapeutic Area | Optimal Assay Format | Key Metrics | Clinical Utility |
|---|---|---|---|
| Immuno-oncology (e.g., anti-PD-1/PD-L1) | Free receptor or drug-occupied | RO percentage on circulating T-cells | Dose optimization for immune activation |
| Inflammatory Diseases | Free receptor with total receptor normalization | RO percentage on target immune cells | PKPD relationship establishment |
| Cell-Ablating Therapies | Total receptor | Receptor-positive cell counts | Assessment of target cell depletion |
| Receptor-Modulating Therapies | Total receptor with free receptor | Absolute receptor numbers | Monitoring receptor up/down-regulation |
Experimental Protocols for RO Assessment
Flow Cytometry-Based RO Assay Methodology
Flow cytometry represents the predominant technological platform for RO assessment due to its ability to perform multiparameter analysis on specific cell populations in complex biological samples like whole blood. The standard protocol involves several critical steps [6]:
Sample Collection and Processing: Fresh whole blood specimens are preferred for RO assays, with minimal processing delays to maintain cell viability and receptor integrity. Blood collection represents a minimally invasive procedure amenable to repeated sampling in longitudinal studies.
Staining Procedure: Cells are incubated with specific detection reagents based on the selected assay format. For free receptor assays, samples are stained with fluorescent-labeled detection antibodies that compete with the therapeutic drug for receptor binding. Critical parameters include antibody concentration, incubation time (typically 20-60 minutes), and temperature control to prevent receptor internalization.
Detection Reagent Selection: The choice of detection reagents significantly impacts assay performance. Bright fluorophores with high quantum yield are essential for targets with low receptor density. For drug-occupied assays, non-neutralizing anti-idiotypic antibodies specific to the therapeutic agent provide the most accurate measurements.
Data Acquisition and Analysis: Flow cytometry data acquisition should capture sufficient event counts for statistical robustness, particularly for rare cell populations. Analysis gates are set based on viability markers and cell lineage markers to ensure accurate RO measurement on the relevant target cells.
Key Research Reagent Solutions
Table 3: Essential Research Reagents for RO Assay Development
| Reagent Category | Specific Examples | Function in RO Assays | Technical Considerations |
|---|---|---|---|
| Viability Dyes | Fixable viability stains | Exclusion of dead cells | Prevents non-specific antibody binding |
| Cell Tracing Dyes | CellTrace Yellow [20] | Cell proliferation tracking | Enables division history monitoring |
| Detection Antibodies | Anti-receptor antibodies with different epitopes | Target receptor quantification | Requires extensive characterization |
| Anti-Drug Antibodies | Non-neutralizing anti-idiotypic antibodies | Detection of drug-bound receptors | Must not compete with receptor binding |
| Reference Standards | Certified cell lines with known receptor density | Assay calibration and normalization | Enables inter-study comparisons |
Methodological Considerations for Robust RO Assays
Several technical challenges must be addressed during RO assay development and implementation. For targets with inherently low receptor expression on circulating cells, signal amplification strategies may be necessary to achieve adequate dynamic range. This can include using secondary detection reagents or selecting exceptionally bright fluorophore conjugates [6].
Sample handling represents another critical consideration. While ex vivo stimulation of whole blood specimens can enhance receptor expression for low-abundance targets, this approach is generally discouraged as it may alter the physiological relevance of RO measurements. Similarly, assay temperature and time from collection to processing must be carefully controlled to prevent artifacts in RO quantification [6].
For cellular targets that undergo rapid modulation in response to drug binding, such as receptor internalization following therapeutic engagement, specialized protocols may be required to stabilize receptor expression patterns during sample processing. These stabilization strategies ensure that measured RO values accurately reflect in vivo conditions at the time of sample collection.
RO Applications Across the Drug Development Continuum
Preclinical Lead Selection and Optimization
In preclinical development, RO assays provide critical data for lead candidate selection by quantifying target engagement potency across different chemical entities. The relationship between drug concentration and RO enables calculation of half-maximal effective concentration values, which can be correlated with functional responses in cellular assays. This quantitative approach facilitates rank-ordering of lead compounds based on their target engagement efficiency rather than relying solely on functional readouts [6].
RO data from animal models supports species relevance assessment for safety evaluations. By comparing RO levels between toxicology species and human cells or tissues, researchers can determine whether animal models adequately predict human target engagement. This comparison is particularly important for therapeutics with significant interspecies differences in target biology or binding affinity [6].
Preclinical RO Workflow
Clinical Translation and Dose Selection
The transition from preclinical to clinical development represents a critical juncture where RO data assumes particular importance for first-in-human dose selection. The minimum anticipated biological effect level approach leverages RO data from in vitro human systems and in vivo animal studies to project human pharmacologically active doses [6]. This strategy is especially valuable for therapeutics with high-risk mechanisms or non-linear PKPD relationships.
During early clinical development, longitudinal RO assessment establishes exposure-response relationships that inform dose escalation decisions and therapeutic regimen optimization. The integration of RO data with pharmacokinetic profiles enables construction of mechanism-based PKPD models that predict optimal dosing strategies for later-stage trials [6]. These models can account for complex phenomena such as target-mediated drug disposition and receptor turnover dynamics.
Clinical RO Implementation
RO as a Clinical Endpoint and Biomarker
In later-stage clinical development, RO measurements can serve as pharmacodynamic endpoints that demonstrate biological activity even when clinical efficacy outcomes may require extended follow-up. This application is particularly relevant for proof-of-concept trials where establishing target engagement provides critical validation of the therapeutic mechanism. RO data can also support patient stratification strategies by identifying individuals with adequate target engagement who are more likely to respond to treatment [6].
For therapeutics directed against targets with substantial interindividual variability in expression levels, RO assessment may guide personalized dosing approaches to ensure adequate target coverage across diverse patient populations. This approach represents a shift from traditional fixed-dosing paradigms toward precision medicine strategies that optimize drug exposure based on individual patient characteristics [6].
Receptor occupancy assays have evolved into indispensable tools that inform critical decisions throughout the drug development continuum. From initial lead selection to final dose justification, RO data provides a quantitative framework for understanding the relationship between drug exposure, target engagement, and biological effect. The integration of RO assessment into drug development programs enhances decision-making confidence, reduces clinical attrition, and ultimately contributes to more efficient delivery of innovative therapies to patients. As drug modalities continue to diversify and targets become more challenging, the strategic application of RO assays will remain essential for successful drug development.
Core Methodologies and Strategic Application of RO Assay Formats
Receptor occupancy (RO) assays are critical pharmacodynamic tools in biopharmaceutical development, designed to quantitatively measure the binding of a therapeutic drug to its specific target receptor on the cell surface [6] [21]. These assays provide indispensable data for establishing pharmacokinetic/pharmacodynamic relationships, guiding optimal dose selection, and predicting clinical efficacy [22]. The direct measurement of target engagement helps confirm the mechanism of action, identify potential safety concerns, and rationalize dosing strategies from first-in-human trials through late-phase clinical studies [14] [21].
Within this context, three primary RO assay formats have been standardized for flow cytometry-based applications: free receptor, drug-occupied receptor, and total receptor assays [6] [22]. Each format offers distinct advantages and limitations while providing complementary perspectives on drug-receptor interactions. This guide provides an objective comparison of these foundational formats, supported by experimental data and methodological details, to inform their appropriate application in target engagement research.
The selection of an appropriate RO assay format is driven largely by the drug's mechanism of action and the availability of specific reagents [6] [21]. The table below summarizes the key characteristics, advantages, and limitations of the three primary formats.
Table 1: Comparative Analysis of Primary RO Assay Formats
| Assay Format | Measurement Focus | Detection Reagent | Primary Applications | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Free Receptor Assay [6] [14] | Unoccupied receptors available for drug binding | Labeled drug, competitive antibody, or receptor ligand [6] | Antagonistic drugs that block ligand binding [6]; Determining therapeutic window and target saturation [22] | Directly measures receptors available for therapeutic engagement [6]; Preferred for blocking agents [6] | Does not directly confirm drug binding; May underestimate engagement if receptor internalization occurs [6] |
| Drug-Occupied Receptor Assay [6] [21] | Receptors currently bound by the drug | Anti-drug antibody that does not compete with receptor binding [6] | Direct assessment of drug-target engagement [22]; Cases where anti-receptor antibodies are unavailable [14] | Directly confirms drug-receptor binding [22]; Useful with low receptor expression when bright fluorophores are used [21] | Requires specific non-neutralizing anti-idiotypic antibodies [6]; May not distinguish between functionally engaged and non-specifically bound drug |
| Total Receptor Assay [6] [14] | Sum of free and drug-occupied receptors | Anti-receptor antibody binding to non-competing epitope [6] | Monitoring receptor expression changes during treatment [6]; Drugs causing receptor up/down-regulation or cell ablation [6] [21] | Controls for variations in receptor expression [22]; Essential when receptor levels change during study [6] | Does not directly distinguish between free and occupied states; Requires antibodies to non-competing epitopes [6] |
Methodological Approaches and Experimental Protocols
Core Methodological Principles
The three RO assay formats share fundamental methodological principles despite their different measurement focuses. All formats typically utilize fresh whole blood specimens due to the minimally invasive nature of blood collection and suitability for repeat sampling [6]. The assays employ fluorescence-labeled detection reagents quantified by flow cytometry, with careful attention to antibody clone selection, fluorochrome combinations, and sample processing protocols to ensure reproducibility [21].
A critical consideration across all formats is the potential for receptor modulation (shedding or internalization) after drug binding, which can profoundly impact RO measurements [6] [21]. Mitigation strategies include shipping samples on ice packs, pre-treating cells with sodium azide or protease inhibitor cocktails, and performing RO assays at 4°C to minimize these effects [21].
Experimental Workflows
The following diagrams illustrate the fundamental workflows and detection strategies for each primary RO assay format.
Figure 1: Detection Strategies for Primary RO Assay Formats
Data Interpretation and Normalization Methods
The interpretation of RO data requires careful consideration of the calculation method, as different normalization approaches can yield substantially different results [3]. RO is typically calculated as the percentage of receptors occupied by the drug, expressed as:
RO = [Antibody-Receptor Complex] / [Total Receptor] × 100% [21]
However, studies have demonstrated that normalization approach significantly impacts RO values, particularly when the internalization rate of drug-bound receptors exceeds the degradation rate of free receptors [3]. Research on nivolumab (anti-PD-1) revealed that normalization to baseline receptor levels versus normalization to total receptors at each time point can produce dramatically different RO profiles—explaining why different studies reported 70% versus ≥90% RO for similar dosing regimens [3].
Table 2: Key Technical Considerations for RO Assay Implementation
| Parameter | Impact on RO Assessment | Recommended Mitigation Strategies |
|---|---|---|
| Sample Matrix [1] [21] | PBMC processing can disrupt drug-receptor binding, causing RO underestimation [1] | Test different anticoagulants and stabilizing reagents; Use consistent sample processing protocols [21] |
| Receptor Expression Level [6] | Low expression reduces dynamic range and assay sensitivity [6] | Use high-affinity detection antibodies with bright fluorophores; Consider signal amplification [6] |
| Receptor Internalization [6] [3] | Drug binding may accelerate internalization, complicating RO interpretation [6] | Perform assays at 4°C; Use protease inhibitors; Employ total receptor assays for normalization [6] [21] |
| Cryopreservation Effects [3] | Freezing/thawing may alter receptor detection and RO values [3] | Validate RO assays against fresh samples; Standardize cryopreservation protocols [3] |
| Temporal Receptor Changes [6] | Receptor levels may increase or decrease during treatment [6] | Combine free and total receptor measurements; Use baseline normalization with caution [6] [3] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of RO assays requires carefully characterized reagents and standardized materials. The following table details essential components for RO assay development and validation.
Table 3: Essential Research Reagents for RO Assay Development
| Reagent/Material | Function | Critical Characterization Parameters |
|---|---|---|
| Therapeutic Agent [22] | Drug candidate for which RO is being assessed | Purity, concentration, binding affinity, specificity [22] |
| Competitive Antibodies [6] [1] | Bind same epitope as drug to detect free receptors | Specificity, affinity, fluorochrome conjugation efficiency [6] |
| Non-Competing Antibodies [6] [1] | Bind different epitope to detect total receptors | Epitope mapping, lack of interference with drug binding [6] |
| Anti-Drug Antibodies [6] | Detect drug-occupied receptors without competition | Non-neutralizing characteristics, specificity for bound drug [6] |
| Cell Lines/Tissues [22] | Express target receptor for assay development | Receptor expression level, physiological relevance, stability [22] |
| Stabilizing Reagents [14] [21] | Preserve receptor expression and drug binding during processing | Compatibility with target receptor, stabilization duration [21] |
| RS 8359 | RS 8359, CAS:119670-32-5, MF:C14H12N4O, MW:252.27 g/mol | Chemical Reagent |
| Aeroplysinin | Aeroplysinin, CAS:55057-73-3, MF:C9H9Br2NO3, MW:338.98 g/mol | Chemical Reagent |
Integrated Data Interpretation and Normalization Framework
The following diagram illustrates how data from different assay formats integrate to provide a comprehensive understanding of drug-receptor interactions, particularly when receptor dynamics change during treatment.
Figure 2: Integrated Framework for RO Data Interpretation
The comparative analysis of primary RO assay formats reveals that each approach provides distinct yet complementary information about drug-target engagement. The free receptor assay is ideally suited for antagonistic therapeutics where measuring available binding sites is critical. The drug-occupied receptor assay directly confirms target engagement and is particularly valuable when specific anti-receptor antibodies are unavailable. The total receptor assay provides essential contextual data when receptor expression levels change during treatment, enabling proper normalization and interpretation of RO results.
The selection of an appropriate RO assay format must be guided by the drug's mechanism of action, reagent availability, and the biological context of the target receptor. Furthermore, researchers must carefully consider normalization methods and sample processing protocols, as these technical factors can significantly impact RO measurements and interpretation. When developed and validated with these considerations in mind, RO assays serve as powerful pharmacodynamic biomarkers that strengthen the rational development of biopharmaceuticals from preclinical studies through clinical trials.
Selecting the Optimal Assay Format Based on Drug Mechanism of Action (MOA)
In target engagement research, demonstrating that a biotherapeutic effectively binds to its intended cellular target is a critical milestone. Receptor occupancy (RO) assays provide this direct evidence, measuring the pharmacodynamic (PD) effect of a drug by quantifying the percentage of receptors occupied by the therapeutic agent [14]. The selection of an appropriate RO assay format is not one-size-fits-all; it is profoundly influenced by the drug's Mechanism of Action (MOA). An assay that is optimal for an antagonistic monoclonal antibody (mAb) may be unsuitable for a receptor-internalizing drug or an agonist. This guide objectively compares the performance of various flow cytometry-based RO assay formats, providing the experimental data and methodologies necessary to align your assay selection with your drug's unique biological mechanism.
Comparative Analysis of RO Assay Formats
The table below summarizes the core characteristics, applications, and performance considerations of the primary RO assay formats, providing a foundation for selection based on MOA.
Table 1: Comparison of Flow Cytometry-Based Receptor Occupancy Assay Formats
| Assay Format | Primary Function | Optimal Drug MOA | Key Clinical Significance | Technical Considerations & Limitations |
|---|---|---|---|---|
| Free Receptor Assay [14] | Measures unbound/unoccupied receptors using a competing antibody. | Antagonistic drugs that block ligand binding. | Measures the extent of receptor blockade. | Requires a non-competing antibody that binds to a different epitope than the therapeutic. |
| Direct Assessment of Bound Receptor [14] | Directly measures therapeutic antibodies bound to the receptor. | Any mAb therapeutic; useful when conjugation of the drug is problematic. | Applied when mAbs to the receptor are not readily available. | Relies on a high-quality anti-therapeutic antibody detection reagent. |
| Total Receptor Assay [14] | Measures total receptor levels (occupied + unoccupied). | Scenarios where receptor density or cell numbers change over time. | Useful for monitoring receptor modulation (shedding or internalization). | Requires two antibodies binding to distinct, non-competing epitopes on the receptor. |
| Receptor Modulation Assay [14] | Measures the functional effect of drug binding on the target receptor. | Drugs designed to cause receptor shedding, inhibition, or activation. | Critical for understanding the downstream consequences of drug binding. | May require specialized readouts beyond simple antibody binding (e.g., phosphorylation). |
| Functional Receptor Occupancy Assay [14] | Measures biological effects (e.g., cell proliferation, cytokine production). | Therapies where binding leads to a measurable functional outcome. | Has direct implications for predicting drug safety and efficacy. | More complex, multi-parameter assays; can be lower throughput. |
Experimental Protocols for Key Assay Formats
Free Receptor Assay Protocol
The Free Receptor Assay is the most commonly employed format for quantifying the PD effect of antagonistic therapeutic drugs [14].
- Principle: This method uses a fluorescently-labeled, non-competing antibody to stain the population of receptors that remain unoccupied by the administered therapeutic. The resulting fluorescence intensity is inversely proportional to the level of receptor occupancy.
- Detailed Workflow:
- Sample Collection & Stabilization: Collect whole blood or peripheral blood mononuclear cells (PBMCs) from subjects. Sample stability is a critical factor; the shipment time from the clinical site to the lab and the age of the blood significantly impact result quality [14]. The use of stabilizing fixative collection tubes (e.g., Smart Tube, Transfix) should be validated for compatibility with the target receptor.
- Staining: Aliquot samples and stain with a titrated volume of the fluorescently-labeled anti-receptor antibody. The antibody must be carefully selected to bind to an epitope distinct from the one bound by the therapeutic drug to avoid competition.
- Lysis & Fixation: Red blood cells are lysed using a commercial lysing solution, and the remaining cells are fixed to preserve staining for analysis.
- Flow Cytometry Acquisition: Acquire data on a flow cytometer, gating on the specific cell population of interest (e.g., T cells, monocytes).
- Data Analysis: The Median Fluorescence Intensity (MFI) of the stained sample is compared to a pre-dose baseline sample to calculate the percentage of free receptors. The RO is then calculated as:
RO (%) = [1 - (MFI_post-dose / MFI_pre-dose)] × 100.
Direct Assessment of Bound Receptor Protocol
This format is ideal for directly detecting the presence of the biotherapeutic on the cell surface.
- Principle: A fluorescently-labeled antibody specific to the therapeutic drug (e.g., an anti-human IgG Fc antibody for a human mAb) is used to stain cells, directly revealing the amount of drug bound to its target.
- Detailed Workflow:
- Sample Preparation: Follow the same sample collection and stabilization procedures as the Free Receptor Assay.
- Staining: Stain the cells with the fluorescent anti-therapeutic antibody.
- Washing & Acquisition: Wash cells to remove unbound antibody and acquire data via flow cytometry.
- Data Analysis: The MFI of the stained sample is directly proportional to the amount of bound drug. This can be reported as MFI or converted to a quantitative measure using a calibrated standard.
Visualizing Assay Workflows and Signaling Context
The following diagrams, created using the specified color palette, illustrate the logical relationships and experimental workflows for the key assay formats.
GPCR Signaling & RO Impact
RO Assay Selection Logic
The Scientist's Toolkit: Essential Research Reagent Solutions
The table below details key reagents and materials required for the successful development and execution of RO assays.
Table 2: Essential Reagents and Materials for Receptor Occupancy Assays
| Item | Function / Description | Critical Considerations |
|---|---|---|
| Anti-Receptor Antibodies [14] | Non-competing antibodies used in Free and Total Receptor assays to detect unoccupied receptor populations. | Must bind to an epitope distinct from the therapeutic drug. Specificity and affinity must be extensively characterized. |
| Anti-Therapeutic Antibodies [14] | Detection reagents for Direct Bound Receptor assays, specific to the biotherapeutic's framework. | Conjugation to a bright fluorochrome is essential for high sensitivity. |
| Stabilizing Fixative Tubes [14] | Sample collection tubes (e.g., Smart Tube, CytoChex) that preserve cell surface epitopes for shipping. | Must be validated for compatibility with the target receptor, as some fixatives can destroy epitopes. |
| Viability Stain | Fluorescent dye to exclude dead cells from analysis, improving data accuracy. | Critical for samples that have undergone shipment or prolonged storage. |
| Flow Cytometry Panels | Pre-configured antibody panels for immunophenotyping the cell population of interest. | Panels are validated under a fit-for-purpose approach, depending on the assay's intended use [14]. |
| Surrogate Positive Control [23] | A reagent (monoclonal or polyclonal) that mimics ADA or drug binding for assessing and monitoring assay parameters. | Must have sufficient volume or high reproducibility for long-term assay support. Generation can be challenging for some therapeutics like peptides. |
| PPQ-102 | PPQ-102, MF:C22H21N5O3, MW:403.4 g/mol | Chemical Reagent |
| AG1557 | AG1557, MF:C19H16BrNO2, MW:370.2 g/mol | Chemical Reagent |
Selecting the optimal receptor occupancy assay is a strategic decision directly dictated by the drug's Mechanism of Action. As evidenced by the comparative data and protocols, the Free Receptor assay is the workhorse for antagonistic drugs, while the Direct Bound Receptor assay provides unambiguous proof of target engagement. For more complex MOAs involving receptor internalization or functional change, Modulation or Functional RO assays are necessary. Adhering to rigorous validation practices, including careful selection of controls and cut-points, is paramount for generating reliable, reproducible data that can guide dosing from early-phase trials through late-phase population studies [23] [14]. A well-chosen and validated RO assay not only confirms target engagement but also serves as a critical pharmacodynamic bridge connecting drug exposure to clinical efficacy and safety.
Receptor occupancy (RO) assays are sophisticated flow cytometry-based methods designed to quantitatively measure the binding of a protein-based therapeutic to its specific cellular target. These assays have become a critical element in the preclinical and clinical development of biopharmaceuticals, providing essential pharmacodynamic (PD) data that contributes to pharmacokinetic (PK)/pharmacodynamic modeling. The primary strength of flow cytometry for RO analysis lies in its ability to simultaneously evaluate receptor expression and drug occupancy on specific cell subsets within complex populations, all while enabling advanced phenotyping of the cellular subsets expressing the drug target receptors [2] [7].
The fundamental application of RO data lies in informing dose selection, particularly for first-in-human clinical studies. By establishing PK/PD relationships, RO assays help bridge preclinical study data and enable the selection of a safe starting dose and a dose escalation scheme [2] [6]. The clinical importance of these assays was starkly illustrated by the case of TGN1412, where a starting dose calculated based on NOAEL (No Observed Adverse Effect Level) led to life-threatening cytokine release syndrome in healthy volunteers. Subsequent analysis showed that if a MABEL (Minimum Anticipated Biological Effect Level) approach based on targeting a 10% RO level had been used, the recommended starting dose would have been approximately 30,000 times lower [6].
RO Assay Formats and Their Applications
Comparative Analysis of RO Assay Formats
The development of a flow cytometry-based RO assay requires careful selection of the most appropriate format based on the drug's mechanism of action, biological context, and reagent availability. The three primary formats each possess distinct characteristics and applications [6] [14].
Table 1: Comparison of Receptor Occupancy Assay Formats
| Assay Format | Detection Method | Primary Applications | Advantages | Limitations |
|---|---|---|---|---|
| Free Receptor | Fluorescence-labeled detection reagent (drug, competitive antibody, or receptor ligand) | Antagonistic drugs that block ligand binding; Dose determination [7] [6] | Measures receptors available for ligand binding; Direct assessment of target engagement | Affected by changes in total receptor levels; Requires competing antibody |
| Drug-Occupied Receptor | Fluorescence-labeled anti-drug antibody (non-competing) | When monoclonal antibodies to receptor are scarce; Low receptor expression scenarios [6] [14] | Enhanced sensitivity for low-expression receptors; Does not require competing anti-receptor antibody | Cannot distinguish between specific and non-specific drug binding |
| Total Receptor | Anti-receptor antibody binding to non-competing epitope | When receptor modulation is expected; Normalization for changing receptor levels [7] [6] | Accounts for drug-induced receptor up/down-regulation; Provides contextual data for interpretation | Does not directly measure occupancy; Requires antibody to non-competing epitope |
The free receptor assay format is particularly valuable for antagonistic drugs whose primary mechanism involves blocking natural ligand binding. This format quantifies the proportion of receptors not bound by the therapeutic agent, typically using a fluorescence-labeled detection reagent that competes with the drug for the same epitope [6]. The drug-occupied receptor format offers an alternative approach that directly detects bound drug using non-competitive anti-idiotypic antibodies or antibodies specific to the drug's Fc region. This format proves especially useful when target receptor expression is low or when competing antibodies are unavailable [6] [14].
For scenarios where the drug is expected to cause receptor modulation (upregulation or downregulation), the total receptor assay provides crucial contextual information. By measuring both occupied and unoccupied receptors using an antibody that recognizes a different epitope than the therapeutic, this approach enables normalization of free receptor data and prevents misinterpretation of drug effects when receptor levels change during treatment [6].
Strategic Workflow for RO Assay Format Selection
The decision-making process for selecting the appropriate RO assay format involves multiple considerations related to the drug's mechanism, biological context, and practical experimental constraints.
Flow Cytometry Platform Selection for RO Assays
Technical Requirements for RO Flow Cytometry
The selection of an appropriate flow cytometry platform for RO assays requires careful consideration of multiple technical parameters to ensure accurate, reproducible data. Different instrument configurations offer varying capabilities that must be matched to the specific requirements of the RO assay being developed [24].
Table 2: Flow Cytometry Platform Selection Criteria for RO Assays
| Parameter | Basic Instrument | Advanced System | High-End Configuration |
|---|---|---|---|
| Laser Configuration | 1-2 lasers (typically 488nm blue, 633nm red) | 3-4 lasers (adding 405nm violet, 561nm yellow-green) | 5+ lasers (including UV and specialized wavelengths) |
| Detection Channels | 6-8 fluorescence detectors | 12-16 fluorescence detectors | 18+ fluorescence detectors |
| Fluorophore Compatibility | FITC, PE, PerCP, APC | Adds Pacific Blue, PE-Cy7, APC-Cy7, Alexa Fluor dyes | Extensive tandem dye support, quantum dots |
| Sensitivity | Standard sensitivity suitable for abundant targets | Enhanced sensitivity for low-expression receptors | Optimal sensitivity for rare cell populations |
| Application Scope | Basic RO assays with limited phenotyping | Multicolor RO with intermediate phenotyping capacity | Comprehensive RO and deep immunophenotyping |
| Reproducibility Assurance | Single-site studies with standardized protocol | Multi-site compatibility with bead normalization | Full validation with CS&T beads and MFI tracking [7] |
When designing panels for RO assays, understanding the instrument configuration is paramount. Researchers must determine the number and type of lasers, the number of detectors, and the specific filter configurations available on their flow cytometer [24]. This knowledge enables optimal matching of fluorophore excitation characteristics to available laser lines and ensures that emission wavelengths align with appropriate detection filters. Substantial variation can exist between different flow cytometers, necessitating careful tailoring of panel design to the specific instrument being used [24].
Strategic Approach to Platform Selection
The process of selecting and validating a flow cytometry platform for RO assays extends beyond technical specifications to encompass practical implementation considerations, particularly for clinical trials.
For global clinical trials where multiple laboratories may be involved in sample analysis, standardization becomes particularly critical. Assay transfer is most seamless when all laboratories use the same flow cytometry instrumentation with identical configurations, allowing direct transfer of reference values, MFI measurements, and standard operating procedures [7]. When this isn't feasible, bridging studies must be conducted to minimize lot-to-lot variability and ensure consistency across sites [7].
Multicolor Panel Design for RO Assays
Fundamental Principles of Fluorophore Selection
The design of multicolor panels for RO assays represents one of the most challenging aspects of experimental setup, requiring systematic optimization to ensure accurate results and reproducibility [24]. Successful panel design hinges on strategic fluorophore selection based on both antigen expression levels and spectral characteristics.
The brightness of fluorophores must be carefully matched to the expression level of target antigens. For low-expression targets or rare cell populations, brighter fluorophores such as PE or APC provide the necessary signal-to-background ratio to adequately separate positive cells from unstained controls [24]. Conversely, highly expressed antigens can typically be detected with dimmer fluorophores, preserving the brighter channels for more challenging targets. The relative brightness of fluorophores can be quantified using the Stain Index, which incorporates both the intensity difference between stained and unstained populations and the distribution spread of the unstained population [25].
Spectral overlap represents another critical consideration in multicolor panel design. Even with careful fluorophore selection, most experiments require compensation to correct for spillover between channels [24]. This process involves using single-stained controls to mathematically subtract the contribution of each fluorophore from other detection channels. Certain fluorophore combinations with extensive spectral overlap (such as APC and PE-Cy5) should be avoided when possible, as excessive compensation can compromise data quality and sensitivity [24].
Practical Panel Design Framework
Implementing a systematic workflow for multicolor flow cytometry panel design is essential for managing the complexity of RO assays. This process involves sequential steps that build upon the fundamental principles of fluorophore selection and instrument configuration.
Table 3: Step-by-Step Multicolor Panel Design Protocol
| Step | Action | Key Considerations | Quality Control Measures |
|---|---|---|---|
| 1. Instrument Assessment | Document laser configuration, detectors, and filter sets [24] | Review manufacturer specifications; Consult core facility managers | Verify with reference beads; Ensure proper laser alignment |
| 2. Antigen Prioritization | Rank markers by abundance and importance | Identify rare populations; Note expected expression levels | Use literature validation; Confirm with preliminary experiments |
| 3. Fluorophore Assignment | Match fluorophore brightness to antigen density [24] [25] | Assign bright fluorophores (PE, APC) to low-expression targets; Use dim fluorophores for abundant antigens | Calculate Stain Index; Compare signal-to-noise ratios |
| 4. Spectral Overlap Management | Analyze emission spectra for potential spillover [24] | Utilize spectral viewing tools; Avoid problematic combinations | Create spillover spreadsheet; Plan compensation controls |
| 5. Panel Validation | Test panel performance with biological samples | Include FMO controls; Verify population resolution | Assess compensation accuracy; Confirm gating strategy |
Experimental Protocols for RO Assay Development
Comprehensive RO Assay Workflow
The development of a robust, reproducible RO assay requires meticulous attention to experimental details throughout a multi-stage process. The following workflow outlines the key stages from initial design through validation and implementation.
The initial assay design phase requires determining whether the target receptor is abundant or expressed at low levels, testing different antibody clones and fluorochromes to ensure they don't compete with the drug, and verifying the absence of interference between the detection antibody and the therapeutic agent [7]. A critical component of this phase is creating a calibration curve showing saturating conditions of the drug, which will be used to quantify RO in clinical samples [7].
The validation phase must be customized based on the study phase, endpoint significance, and data reporting requirements. For exploratory endpoints, general validation guidelines may suffice, while assays serving as secondary endpoints require more rigorous validation, potentially including linearity and sensitivity assessments [7]. For real-time assays, training at least three operators ensures consistent performance over the study duration [7].
Essential Research Reagent Solutions
Successful implementation of RO assays depends on the availability and quality of specific reagents and materials. The following table outlines key solutions required for developing and executing flow cytometry-based RO assays.
Table 4: Essential Research Reagent Solutions for RO Assays
| Reagent Category | Specific Examples | Function in RO Assays | Selection Criteria |
|---|---|---|---|
| Detection Antibodies | Competitive anti-receptor antibodies; Non-competing anti-receptor antibodies; Anti-drug antibodies [6] | Detect free receptors, total receptors, or drug-bound receptors | Specificity, affinity, compatibility with drug binding, availability of non-competing pairs |
| Fluorophore Conjugates | PE, APC, Alexa Fluor dyes, tandem dyes [24] [25] | Enable multiplex detection of multiple parameters | Brightness, spectral overlap, instrument compatibility, stability |
| Viability Dyes | LIVE/DEAD Fixable Stains; 7-AAD [25] | Exclude dead cells from analysis to improve data accuracy | Compatibility with fixation, emission spectrum, staining protocol |
| Compensation Controls | UltraComp beads; Antibody capture beads [24] | Establish compensation matrix for spectral overlap correction | Consistency with sample staining, stability, lot-to-lot reproducibility |
| Reference Standards | CS&T beads; MFI reference beads [7] | Instrument performance tracking and standardization across sites | Stability, reproducibility, compatibility with instrument QC protocols |
| Sample Stabilization | Transfix tubes; Cyto-Chex tubes [14] | Preserve receptor occupancy state during shipment and storage | Compatibility with target receptor, stabilization duration, impact on epitope recognition |
Validation and Implementation in Clinical Development
Strategic Validation Approach
The validation of flow cytometry-based RO assays should follow a fit-for-purpose approach, with the extent of validation tailored to the assay's role in clinical development. For early-phase trials and exploratory endpoints, focused validation may be appropriate, while assays supporting primary or key secondary endpoints require comprehensive validation [7] [14].
Critical validation parameters include specificity, sensitivity, precision, accuracy, and robustness. Specificity confirmation ensures that the detection antibody specifically recognizes the intended target without cross-reactivity. Sensitivity validation establishes the lowest level of receptor occupancy that can be reliably detected, which is particularly important for targets with low expression levels. Precision assessments evaluate both intra-assay and inter-assay variability, while robustness testing examines the assay's resilience to small but deliberate changes in experimental conditions [7].
For RO assays that will be deployed across multiple clinical sites, additional validation elements are necessary. Sample stability studies must establish acceptable timeframes between sample collection and analysis, especially critical for RO assays typically performed on fresh whole blood where receptor stability may be limited [7] [14]. Inter-operator and inter-instrument variability should be quantified, with acceptance criteria defined based on the assay's intended purpose [7].
Clinical Implementation Considerations
Successful implementation of RO assays in clinical trials requires careful logistical planning. The real-time nature of many RO assays necessitates close proximity between clinical sites and testing laboratories or the development of validated sample stabilization methods [7]. The use of stabilizing fixative collection tubes (such as Smart Tube, Transfix, or CytoChex) can extend sample stability but requires verification that the stabilization method is compatible with the target receptor and doesn't affect epitope recognition [14].
For global clinical trials, assay transfer between laboratories demands meticulous standardization. The use of the same flow cytometry instruments with identical configurations across sites facilitates direct transfer of reference values and standard operating procedures [7]. When this isn't feasible, bridging studies must be performed to establish equivalence between different instrument platforms or reagent lots [7].
The clinical significance of RO assays spans all phases of drug development. In preclinical stages, RO data guide compound selection and mechanism of action studies. In Phase 1 trials, RO assessments help identify minimal anticipated biological effect levels (MABEL) or pharmacologically active doses (PAD), critical for potent biotherapeutics where improper dosing can cause severe side effects [6] [14]. During Phase 2 and 3 trials, RO data inform dose optimization and administration schedules, ultimately contributing to population pharmacodynamic characterization for long-term safety and efficacy studies [14].
The Saturating vs. Non-Saturating Approach for Complex Scenarios
Receptor occupancy (RO) assays are indispensable tools in modern biopharmaceutical development, designed to quantitatively measure the binding of a therapeutic drug to its specific target on the cell surface [2] [21]. These assays have become a critical element in preclinical and clinical development of protein-based therapies, providing essential pharmacodynamic (PD) biomarker data that contributes to pharmacokinetic (PK)/pharmacodynamic (PD) modeling [2] [6]. The primary application of RO data lies in its ability to bridge preclinical study findings to human trials, enabling the selection of a safe starting dose and dose escalation scheme for first-in-human clinical studies [2]. Furthermore, data generated from RO assays can model whether given doses of an experimental therapeutic agent and their administration schedules lead to predicted levels of target engagement and whether the receptor is modulated on cells engaged by the therapeutic agent [2].
Flow cytometry has emerged as an ideal platform for RO assays due to its ability to perform advanced phenotyping of cellular subsets expressing drug target receptors [2] [6]. This technology enables researchers to monitor receptor occupancy specifically in cell populations of interest by combining target-specific reagents into a flow cytometry panel of phenotypic markers [1]. When combined with pharmacokinetic profiling, RO assays provide valuable information on dose selection and frequency of drug administration, and can be validated to support secondary endpoints in clinical trials [1].
Comparative Analysis of RO Assay Formats
Three primary formats exist for receptor occupancy assays, each with distinct applications and limitations. Understanding these fundamental approaches is crucial before examining the specific saturating versus non-saturating methodology.
Fundamental Receptor Occupancy Assay Formats
The Saturating vs. Non-Saturating Approach: A Direct Comparison
The saturating versus non-saturating approach represents a specialized methodology within RO assays, particularly valuable when traditional reagents are unavailable or when studying complex drug-receptor interactions. This side-by-side comparison highlights the key differences and applications of each methodology.
Table 1: Comparison of Saturating vs. Non-Saturating RO Approaches
| Parameter | Saturating Approach | Non-Saturating Approach |
|---|---|---|
| Core Principle | One sample portion saturated with excess drug to mimic 100% RO conditions | Untreated sample portion reflecting actual in vivo drug binding |
| Detection Method | Secondary antibody detects bound drug in both portions | Secondary antibody detects bound drug in untreated sample |
| RO Calculation | Ratio of drug-binding between non-saturated and saturated portions | Direct measurement complemented by saturated portion |
| Primary Application | When competitive/non-competitive antibodies are unavailable | Standard measurement combined with saturated control |
| Reagent Requirements | Drug product + detection antibody (anti-drug or anti-Ig) | Same sample matrix without saturation |
| Data Interpretation | Direct comparison within same sample minimizes inter-sample variability | Requires normalization to saturated control for accurate RO % |
| Advantages | Circumvents need for specialized competing antibodies; internal control | Reflects actual physiological binding state |
| Limitations | Requires careful optimization of saturation conditions | Alone, cannot differentiate between low binding and low receptor expression |
Experimental Protocol for Saturating vs. Non-Saturating RO Assays
The following workflow outlines the standardized experimental procedure for implementing the saturating versus non-saturating approach, as employed in clinical trial settings.
Saturating vs. Non-Saturating Workflow
Step-by-Step Protocol:
Sample Collection and Preparation: Collect fresh whole blood samples in appropriate anticoagulants (e.g., EDTA, heparin). Test different vacutainers to maximize stability and precision of RO measurement [1] [21]. Process samples immediately or use stabilizing reagents to maintain receptor integrity.
Sample Splitting and Saturation: Aliquot the sample into two equal portions. For the saturation portion, incubate with a high concentration of the therapeutic drug (typically 10-100 times the expected KD) to ensure complete receptor saturation [1]. The non-saturated portion remains untreated or receives vehicle control.
Staining and Detection: Add fluorophore-conjugated anti-drug antibody to both sample portions. This secondary detection antibody binds to the therapeutic drug occupying the receptors [1]. Include appropriate controls: isotype controls, fluorescence minus one (FMO) controls, and compensation controls for multicolor panels [21] [7].
Flow Cytometry Acquisition: Acquire samples on a standardized flow cytometer with daily quality controls using reference beads [21] [7]. Maintain consistent instrument settings across all samples and timepoints. Gate on live, target cell populations using phenotypic markers.
Data Analysis and RO Calculation: Measure Mean Fluorescence Intensity (MFI) of drug binding in both saturated and non-saturated portions. Calculate percentage RO using the formula: % RO = (MFInon-saturated / MFIsaturated) × 100 [1].
Applications in Complex Scenarios
Challenging Research Contexts
The saturating versus non-saturating approach proves particularly valuable in specific challenging research scenarios where traditional assay formats face limitations:
Low Receptor Expression or Rare Cell Populations: When target receptors are expressed at low levels or on rare cell types, the direct detection of bound drug using anti-drug antibodies provides enhanced sensitivity compared to competitive assays [6] [7]. The use of bright fluorophores such as Brilliant Violet conjugated to the secondary detection antibody further increases the dynamic signal range [21].
Receptor Modulation and Internalization: For therapeutics that cause receptor internalization or downregulation upon binding, the saturating approach helps distinguish between true occupancy and receptor loss [6] [21]. By comparing total potential binding sites (saturated portion) to actual in vivo binding (non-saturated portion), researchers can quantify both occupancy and modulation simultaneously.
Bispecific Therapeutics: For bi-specific molecules binding multiple targets, the saturating approach provides a straightforward method to assess engagement without requiring multiple competing antibodies for different epitopes [1]. The same anti-drug antibody can detect binding regardless of the specific target engaged.
Absence of Suitable Competing Antibodies: When antibodies that compete with the drug for receptor binding are unavailable or cannot be identified, the saturating approach offers a viable alternative [1] [7]. This eliminates the need for extensive reagent development and validation.
Integration with PK/PD Modeling
RO data generated through saturating versus non-saturating approaches contribute significantly to pharmacokinetic/pharmacodynamic modeling:
Table 2: RO Data Applications in Drug Development Phases
| Development Phase | RO Application | Impact on Development |
|---|---|---|
| Preclinical | Target verification & mechanism of action | Informs lead compound selection based on binding characteristics [21] |
| Phase I | MABEL/PAD model starting doses | Guides safe starting dose selection; prevents overdosing [6] [21] |
| Phase II | Efficacy of dosing regimens | Predicts RO levels and receptor modulation patterns [21] |
| Phase III | Population PK for long-term safety | Supports safety and efficacy across diverse populations [21] |
Data from saturating versus non-saturating assays help establish critical PK/PD relationships, informing dose selection and frequency of administration [1]. Maintaining drug concentrations above the critical concentration (Ccrit) ensures continuous target engagement, a key consideration in dosing regimen design [26].
Technical Considerations and Validation
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of saturating versus non-saturating RO assays requires careful selection of research reagents and materials:
Table 3: Essential Research Reagent Solutions for RO Assays
| Reagent/Material | Function | Considerations |
|---|---|---|
| Therapeutic Drug | Sample saturation | High purity; same lot as clinical material [7] |
| Anti-Drug Antibody | Detection of bound drug | Non-neutralizing; specific to drug idiotype or Fc region [6] |
| Fluorophore Conjugates | Signal generation | Bright fluorophores (e.g., Brilliant Violet) for low expression targets [21] |
| Whole Blood Samples | Experimental matrix | Anticoagulant selection affects cell stability and receptor expression [21] |
| Stabilizing Reagents | Sample preservation | Transfix or Cyto-Chex for extended sample stability [21] |
| Reference Beads | Instrument standardization | CS&T beads for daily quality control and standardization [7] |
| Phenotypic Markers | Cell population identification | Antibody panel for gating target cell populations [1] |
| Cefprozil | (Z)-Cefprozil | |
| D(+)-Raffinose pentahydrate | D-(+)-Raffinose Pentahydrate|Research Grade|[Your Company] |
Method Validation Parameters
For regulatory compliance and data reliability, saturating versus non-saturating RO assays require rigorous validation:
Precision and Accuracy: Inter- and intra-assay precision should demonstrate ≤20% CV (≤25% for LLOQ) [7]. Accuracy should be within ±20% of nominal values (±25% at LLOQ).
Linearity and Range: Establish a calibration curve using serial dilutions showing saturating conditions of the drug [7]. The assay range should cover expected clinical RO values.
Sample Stability: Validate stability under various conditions including storage temperature, freeze-thaw cycles, and post-staining stability [21] [7]. For RO assays, receptor stability is particularly crucial as binding can be disrupted by cell isolation or cryopreservation [5].
Robustness: Test assay performance with multiple operators, instruments, and reagent lots [7]. For global trials, transfer the assay to multiple labs using the same flow cytometry configuration [7].
Specificity and Selectivity: Demonstrate that the anti-drug antibody specifically detects the drug-receptor complex without cross-reacting with similar receptors or free drug in solution [6].
The saturating versus non-saturating approach represents a robust methodology for assessing receptor occupancy in complex scenarios where traditional assay formats face limitations. This approach excels particularly when studying therapeutics that cause receptor modulation, when target expression is low, or when suitable competing antibodies are unavailable. While requiring careful optimization of saturation conditions, it provides a direct measurement of target engagement with internal controls that enhance data reliability.
When integrated with pharmacokinetic profiling and PD biomarkers, RO data from this approach informs critical decisions throughout drug development—from initial dose selection based on MABEL considerations to late-stage optimization of dosing regimens. The methodology's relative simplicity and reduced reagent requirements make it particularly valuable for accelerating biopharmaceutical development while maintaining scientific rigor.
As drug modalities continue to evolve toward more complex multi-specific molecules and targeted therapies, the saturating versus non-saturating approach will remain an essential tool in the target engagement assessment arsenal, providing critical insights that bridge preclinical findings to clinical success.
Cluster of Differentiation 6 (CD6) is a transmembrane glycoprotein expressed predominantly on T cells and a subset of B and NK cells, playing a pivotal role in immune synapse formation, T cell activation, and differentiation [27] [28]. Its position at the center of the immunological synapse and physical association with the T cell receptor (TCR) complex makes it a promising target for immunomodulatory therapies aimed at treating autoimmune diseases and cancer [28] [29]. The CD6 pathway interacts with multiple ligands, including CD166/ALCAM, CD318/CDCP1, and CD44, which are widely expressed on antigen-presenting cells, epithelial cells, and various cancer cells [27]. The development of Receptor Occupancy (RO) assays for CD6-targeting therapeutics is therefore critical for establishing pharmacokinetic/pharmacodynamic (PK/PD) relationships and guiding dose selection in clinical trials [6] [7].
CD6 Biology and Therapeutic Relevance
Key Ligands and Signaling Pathways
CD6 modulates T-cell responses through interactions with its ligands and downstream signaling effectors. The diagram below illustrates the core CD6 signaling pathway and the points of therapeutic intervention.
CD6's immunomodulatory function is context-dependent, exhibiting both co-stimulatory and inhibitory roles in T cell activation [28] [29]. Itolizumab, a humanized anti-CD6 monoclonal antibody binding to the membrane-distal domain 1, demonstrates therapeutic efficacy without depleting lymphocytes, instead modulating T cell activation and differentiation [30] [29]. It reduces pathogenic Th17 cell differentiation and production of IL-17, a key cytokine driving autoimmune pathology [29].
CD6 Ligands and Their Roles
Table 1: Known Ligands of the CD6 Receptor and Their Functional Roles
| Ligand | Alternative Name | Expression | Functional Role in CD6 Pathway |
|---|---|---|---|
| CD166 | ALCAM | Antigen-presenting cells, endothelial cells, various cancer cells [27] | Primary ligand; mediates stable immune synapse formation and T cell adhesion [27] |
| CD318 | CDCP1 | Epithelial cells, cancer stem-like cells [27] | Second identified ligand; binds distinct CD6 epitope; role in adhesion to non-hematopoietic cells [27] |
| CD44 | N/A | Wide tissue distribution | Potential third ligand; recent biochemical evidence supports interaction [27] |
| Galectin-1 & -3 | N/A | Soluble in microenvironment | Binds carbohydrate moieties on CD6; modulates adhesion, migration, and activation [27] |
RO Assay Development for CD6-Targeted Therapy
Comparison of RO Assay Formats
Receptor Occupancy (RO) assays are crucial for quantifying the binding of a therapeutic drug to its specific target on the cell surface, providing a direct measure of pharmacodynamic (PD) effect [6] [7]. These flow cytometry-based assays are particularly valuable for immuno-modulatory therapies, informing dose selection and establishing PK/PD relationships [6] [31]. The table below compares the three primary RO assay formats applicable to CD6-targeting therapeutics like Itolizumab.
Table 2: Comparison of Receptor Occupancy (RO) Assay Formats for CD6-Targeting Therapeutics
| Assay Format | Measurement Principle | Key Reagents | Advantages | Limitations | Suitability for CD6 |
|---|---|---|---|---|---|
| Free Receptor | Measures unoccupied CD6 receptors [6] [32] | Labeled competitive antibody (same epitope as drug) [7] | Directly measures target engagement; ideal for antagonistic drugs [6] | Does not account for drug-induced receptor modulation [6] | High: Directly measures CD6 available for drug binding |
| Occupied Receptor | Measures drug-bound CD6 receptors [6] [31] | Labeled anti-drug antibody (ADA) [6] [7] | Directly quantifies bound drug; useful for low receptor expression [7] [32] | Requires specific, non-competing ADA [6] | Medium: Requires well-characterized anti-idiotypic antibody |
| Total Receptor | Measures both occupied and unoccupied CD6 [6] [32] | Non-competing antibody to a different CD6 epitope [7] | Controls for drug-induced changes in receptor levels [6] | May not distinguish between free and occupied receptor [7] | High: Essential for normalizing data and detecting CD6 modulation |
Assay Selection and Technical Considerations
For CD6-targeted therapies, the free receptor assay is often the preferred format for initial PK/PD modeling, as it directly measures the receptors available for therapeutic binding [6]. However, given that CD6 expression can be modulated upon activation and drug binding, combining a free receptor assay with a total receptor measurement provides the most robust data normalization [6] [7]. This combined approach controls for potential drug-induced changes in total CD6 receptor levels on the cell surface, which is critical for accurate RO interpretation [6].
Key technical challenges in CD6 RO assays include the need for fresh whole blood samples due to potential receptor internalization or apoptosis upon ex vivo storage, and the selection of detection antibodies that do not compete with the therapeutic drug for CD6 binding [7] [32]. Furthermore, the epitope specificity of the anti-CD6 therapeutic antibody is a critical factor. Itolizumab binds to the membrane-distal Domain 1 of CD6, which is distinct from the Domain 3 responsible for CD166 binding [30]. This allows for the development of non-competing antibodies for total receptor assays.
Experimental Protocol & Validation for CD6 RO Assay
Detailed RO Assay Workflow
The following diagram outlines the key steps for performing a flow cytometry-based RO assay for a CD6-targeting therapeutic, integrating both free and total receptor measurements.
Step-by-Step Methodology
This protocol is designed for a dual-format RO assay using human peripheral blood mononuclear cells (PBMCs) or whole blood.
Sample Collection and Preparation:
- Collect peripheral blood in anticoagulant tubes (e.g., EDTA or heparin).
- Process samples within a short time frame (e.g., 4-8 hours) to maintain receptor stability, as CD6 expression and RO can be altered by ex vivo processing [7] [32].
- Split the sample into two aliquots for free and total receptor staining.
Immunostaining for Free and Total CD6:
- Free Receptor Tube: Add a titrated amount of a fluorescently-labeled antibody (e.g., FITC-conjugated) that competes with the therapeutic drug (e.g., Itolizumab) for the same epitope on CD6 Domain 1 [7] [30]. Include antibodies for cell phenotyping (e.g., anti-CD3-PerCP, anti-CD4-APC).
- Total Receptor Tube: Add a fluorescently-labeled antibody (e.g., PE-conjugated) that binds to a different, non-competing epitope on CD6 (e.g., Domain 3) [6] [7]. This antibody will bind regardless of whether the drug is occupied.
- Incubate cells with antibodies in the dark for 20-30 minutes at 4°C, then wash to remove unbound antibody.
Flow Cytometry Data Acquisition:
- Acquire data on a flow cytometer calibrated using reference beads [7].
- Collect a sufficient number of events (e.g., >10,000 CD3+CD4+ T cells) for robust statistical analysis.
Data Analysis and RO Calculation:
- Gating Strategy: Identify the lymphocyte population based on FSC/SSC, then gate on CD3+CD4+ T cells [33].
- Mean Fluorescence Intensity (MFI): Record the MFI of the free receptor signal (FITC) and the total receptor signal (PE) within the CD4+ T cell population.
- % RO Calculation: Calculate the percentage receptor occupancy using the formula: % RO = [1 - (MFIfree / MFItotal)] × 100 [6] [7].
Key Research Reagent Solutions
Table 3: Essential Reagents for CD6 Receptor Occupancy Assay Development
| Reagent / Material | Critical Function | Specification / Clone Example |
|---|---|---|
| Therapeutic Anti-CD6 mAb | Drug for RO assessment; defines target epitope | Itolizumab (binds human CD6 Domain 1) [30] [29] |
| Competitive Anti-CD6 Antibody | Detects unoccupied (free) CD6 receptors | MEM-98 or MT605 clone (binds CD6 Domain 1, competing with Itolizumab) [30] |
| Non-competitive Anti-CD6 Antibody | Detects total CD6 receptors (occupied + free) | OX126 clone (binds CD6 Domain 3, non-competing with Domain 1 mAbs) [30] |
| Cell Phenotyping Antibodies | Identifies T-cell subsets for population-specific RO | Anti-CD3, Anti-CD4, Anti-CD8 [33] |
| Fresh Clinical Samples | Biological matrix for assay validation | Fresh human whole blood or PBMCs from healthy donors and patients [7] [32] |
| Compensation Beads & Controls | Ensures flow cytometry accuracy and reagent specificity | Anti-mouse Ig beads, fluorescence-minus-one (FMO) controls, isotype controls [7] |
Validation and Implementation in Drug Development
Assay Validation Parameters
For RO assays to generate reliable data for regulatory submissions, they must undergo rigorous validation. Key parameters and typical acceptance criteria are summarized below.
Table 4: Key Validation Parameters for a Regulated CD6 RO Assay
| Validation Parameter | Objective | Typical Acceptance Criteria |
|---|---|---|
| Precision | Measure intra- and inter-assay variability | %CV < 15-20% for MFI and derived %RO [7] |
| Accuracy | Determine closeness to true value | Recovery of 80-120% for RO in spiked samples |
| Specificity | Confirm measurement is specific to target | No interference from soluble CD6 (sCD6) or related receptors [27] |
| Stability | Establish sample handling windows | Demonstrate stable RO signal over defined pre-analytical time [7] |
| Robustness | Assess susceptibility to small variations | Consistent performance across operators, instruments, and reagent lots [7] |
| Linearity & Range | Define the quantitative range | Demonstrated across expected clinical RO values (e.g., 10-90% RO) |
Translating RO Data to Clinical Outcomes
Integrating RO data with pharmacokinetic (PK) profiles allows for the construction of mechanism-based PK/PD models. These models are critical for predicting human dose-response relationships based on nonclinical data [6]. For a CD6-targeted therapy like Itolizumab, the goal is to identify a dose and dosing interval that maintains a minimum anticipated biological effect level (MABEL) or a target RO level associated with clinical efficacy in autoimmune diseases, such as reduced T cell activation and Th17 differentiation, while minimizing the risk of adverse effects like over-immunosuppression [6] [29].
The clinical utility of RO was highlighted by the TGN1412 incident, where a starting dose calculated based on no adverse effect level (NOAEL) led to catastrophic cytokine release syndrome in healthy volunteers. Subsequent analysis showed that a MABEL approach based on a target of 10% RO would have resulted in a 30,000-fold lower starting dose, underscoring the critical importance of RO assessment for first-in-human trials of high-risk immunomodulatory products [6].
The successful development of biopharmaceuticals, particularly those targeting cell surface receptors such as monoclonal antibodies and trispecific T-cell engagers, relies on a continuous quantitative understanding of drug-target interactions across all clinical phases. Receptor occupancy (RO) assays serve as the critical pharmacodynamic (PD) bridge connecting initial first-in-human (FIH) dose selection based on the Minimum Anticipated Biological Effect Level (MABEL) to late-phase population PD analyses. This guide examines the application of these fundamental concepts throughout the clinical development lifecycle, comparing methodologies, data requirements, and decision-making impacts at each phase.
Validated RO assays provide the foundational data for understanding target engagement, a concept that spans from early safety assessment to late-phase efficacy optimization [34] [1]. The evolution from simple MABEL determination to complex population PD modeling represents increasing sophistication in how we quantify and utilize drug-target interactions, with each phase building upon the previous one to create a comprehensive understanding of a therapeutic's behavior in humans.
Phase 1: MABEL Determination and Initial RO Assessment
MABEL Fundamentals and Methodological Evolution
First-in-human dose selection for biologics with potent mechanisms has evolved significantly since the TGN1412 incident, which demonstrated that traditional NOAEL (No Observed Adverse Effect Level) approaches could insufficiently predict human toxicity for certain drug classes [35]. The MABEL approach emphasizes determining a starting dose based on the minimal anticipated biological effect rather than solely on toxicity observations, requiring integration of all available in vitro and in vivo information [35].
A systematic review of FIH studies with monoclonal antibodies published between 1990-2013 found that MABEL- or MED-based approaches were used more frequently in 2011–2013 than in 1990–2007 (31.6% vs. 6.3%), reflecting a steady acceptance of regulatory guidance on mitigating FIH risks [35]. The median safety factor was much lower for MABEL-based approaches than for other determination methods (10 vs. 32.2–53), suggesting more precise starting dose estimation [35].
Experimental Protocols for MABEL Determination
Core Protocol Elements:
- In Vitro Potency Assessments: Determine EC50 values for functional responses (e.g., cytokine release, T-cell activation) in human cell-based systems
- Receptor Occupancy Modeling: Calculate expected RO at various concentrations using in vitro binding parameters
- Interspecies Scaling: Adjust for potency differences between animal models and humans using allometric scaling or PK/PD modeling
- Safety Margin Application: Apply appropriate safety factors based on mechanism-related risks and model uncertainty
Modified MABEL Approach: For novel modalities like trispecific T-cell engagers, a modified MABEL strategy identifies a clinically relevant in vitro pharmacology threshold coupled with PK modeling using animal data for allometric scaling [36]. This approach has demonstrated starting doses more than four times higher than traditional MABEL calculations while maintaining safety, significantly reducing the number of subtherapeutic cohorts patients must undergo before reaching potentially efficacious exposures [36].
RO Assay Validation for Phase 1 Applications
Flow cytometry-based RO assays for Phase 1 must be optimized to detect minimal biological effects, requiring rigorous validation parameters [34]:
- Precision: ≤20% CV for precision, ≤25% CV for low abundance targets
- Accuracy: 80-120% recovery of expected values
- Stability: Demonstration of sample stability under expected handling conditions
- Specificity: Minimal interference from matrix components or concomitant medications
Two primary RO assay methodologies are employed in Phase 1 studies [1]:
Table 1: Receptor Occupancy Assay Types for Phase 1 Applications
| Assay Type | Methodology | Data Output | Optimal Use Cases |
|---|---|---|---|
| Competitive Assay | Uses competing and non-competing antibodies to distinguish bound vs. unbound receptors | Percentage of occupied receptors at specific drug concentrations | Targets with well-characterized epitopes and available antibody pairs |
| Saturation Assay | Compares drug-saturated samples (100% RO) with untreated samples to calculate occupancy | Ratio of unsaturated to saturated signal | Targets lacking non-competing antibodies or with complex binding characteristics |
Figure 1: MABEL Determination Workflow for Phase 1 Starting Dose Selection
Phase 2: Exposure-Response and RO-Driven Dose Selection
Transition to Quantitative PK/PD Relationships
Phase 2 studies bridge initial safety experience with therapeutic exploration, requiring more sophisticated RO integration. During this phase, RO data shifts from primarily safety-focused to optimization-driven, establishing exposure-response relationships that inform dose selection for Phase 3 [1].
Population pharmacokinetic (PopPK) approaches become particularly valuable here, as they characterize between-subject variability and identify covariates that influence drug exposure and response [37]. By pooling data from multiple studies and subjects, PopPK modeling enables evaluation of inter-subject variability, covariate effects, and simulation of exposures in diverse populations—all essential for optimizing dosing regimens [38].
Simultaneous PK/PD Modeling Methodology
The seminal work by Sheiner et al. introduced simultaneous PK/PD modeling, which provides significant advantages over sequential analysis [39]:
- Avoids bias in pharmacodynamic parameter estimates when individual PK parameters are imprecise
- Provides more accurate imprecision estimates of PD parameters
- Enables estimation of correlations between PK and PD random effects
- Allows response data to contribute to PK model parameter estimation
The effect-compartment model addresses temporal disconnects between plasma concentrations and response, introducing a hypothetical compartment with first-order elimination (k~eo~) that represents the biophase where the drug exerts its effect [39]. This approach enables characterization of hysteresis loops often observed when response lags behind plasma concentrations.
RO Assay Validation for Phase 2 Applications
Phase 2 RO assays require expanded validation to support dose selection decisions:
- Dynamic Range: Validation across anticipated clinical exposure range
- Covariate Assessment: Evaluation of potential factors affecting RO measurements (e.g., receptor density variability)
- Cross-Validation: Correlation with functional PD biomarkers where available
Phase 3: Population PD and Confirmatory RO Analysis
Population PD for Registration Studies
Phase 3 represents the culmination of the target engagement continuum, where population PD modeling integrates RO data to confirm mechanism of action, establish dosing in special populations, and support labeling claims. Pharmacometric methods are particularly powerful assets when used to build a comprehensive knowledge base of preclinical, early-phase, literature, and competitor data [40].
Population PD approaches in Phase 3 provide a rich, quantitative basis for development decisions and a platform for earlier, more informative communication with regulators [40]. Regulators have come to expect pharmacometric analyses in submissions and apply modeling and simulation themselves to evaluate study designs, labeling, and approval decisions [40].
Advanced RO Assay Applications in Phase 3
Validated RO assays supporting Phase 3 trials must meet stringent requirements for precision and reproducibility, often requiring validation under Good Clinical Laboratory Practice (GCLP) guidelines [34]. Key applications include:
- Dose justification based on target saturation relationships
- Dosing interval optimization through RO duration assessment
- Special population recommendations based on covariate effects on RO
- Drug-drug interaction assessment for immunomodulatory combinations
Table 2: Evolution of RO Assay Applications Across Clinical Development
| Parameter | Phase 1 | Phase 2 | Phase 3 |
|---|---|---|---|
| Primary Purpose | Safety assessment, MABEL confirmation | Exposure-response characterization, dose optimization | Confirmatory evidence, special population dosing |
| Validation Level | Fit-for-purpose with precision/accuracy assessment | Expanded validation across anticipated range | Full GCLP validation for regulatory submission |
| Sample Numbers | Limited to dose-escalation cohorts | Multiple cohorts across dose levels | Large numbers across diverse populations |
| Modeling Approach | Direct relationship between exposure and RO | PK/PD modeling, often with effect compartments | Population PD with covariate analysis |
Integration of RO Data into Population PD Models
Population PD modeling in Phase 3 integrates RO data to answer critical registration questions:
Figure 2: Phase 3 Population PD Modeling Applications
Comparative Performance: Methodologies Across Phases
Quantitative Comparison of MABEL Approaches
The evolution from traditional to modified MABEL approaches has demonstrated significant improvements in development efficiency:
Table 3: Performance Comparison of MABEL Determination Methods
| Method | Typical Safety Factor | Dose Escalation Steps | Time to Therapeutic Dosing | Key Differentiators |
|---|---|---|---|---|
| NOAEL-Based | 32.2-53 [35] | Not significantly different [35] | Longer (more subtherapeutic cohorts) | Relies on animal toxicity endpoints; insufficient for cytokine-release risk [35] |
| Traditional MABEL | 10 [35] | Not significantly different [35] | Moderate | Incorporates in vitro pharmacodynamics; conservative starting doses [35] |
| Modified MABEL | Case-specific (reduced) [36] | Reduced by ~4 cohorts [36] | Shorter (fewer subtherapeutic cohorts) | Integrates PK modeling and clinically relevant thresholds; optimized for efficiency [36] |
Modeling Approach Performance Characteristics
Different modeling strategies offer distinct advantages throughout development:
Table 4: Modeling Method Performance Across Development Phases
| Modeling Approach | Optimal Phase | RO Data Requirements | Regulatory Acceptance | Key Advantages |
|---|---|---|---|---|
| Non-Compartmental Analysis (NCA) | Phase 1 [38] | Minimal (sparse sampling acceptable) | Foundational for early decision making [38] | Direct parameter estimation; minimal assumptions [38] |
| Population PK/PD | Phase 2-3 [38] [37] | Rich or sparse sampling across populations | High for dosing justification and waivers [38] | Handles interindividual variability; supports simulations [37] |
| PBPK | Phase 1 (extrapolation) [38] | Mechanism-informed parameters | Moderate (context-dependent) [38] | Mechanistic insight when clinical data limited [38] |
| Scientific Machine Learning | Phase 3 (large datasets) [41] | Large multimodal datasets | Emerging | No pre-specified covariate relationships required [41] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of RO assays across clinical phases requires carefully selected reagents and methodologies:
Table 5: Essential Research Reagents for RO Assay Implementation
| Reagent/Material | Function | Phase-Specific Considerations | Validation Parameters |
|---|---|---|---|
| Competitive Antibodies | Binds same epitope as drug to detect unoccupied receptors | Phase 1: Critical for MABEL determination; Phase 3: Lot-to-lot consistency | Specificity, cross-reactivity, affinity matching [1] |
| Non-Competitive Antibodies | Binds different epitope to detect total receptor population | Phase 2-3: Essential for calculating percentage RO | Stability, minimal interference with drug binding [1] |
| Anti-Drug Antibodies | Alternative detection method for drug-bound receptors | All phases: Particularly useful when competitive antibodies unavailable | Specificity for drug without target interference [1] |
| Validation Controls | Assay performance qualification | Phase 1: Minimal required set; Phase 3: Comprehensive panel | Precision, accuracy, sensitivity, specificity [34] |
| Biological Matrix | Patient sample context (PBMCs, whole blood) | All phases: Matrix selection profoundly affects assay quality [1] | Stability, minimal processing artifacts [34] |
| G-418 disulfate | G-418 disulfate, CAS:49662-05-7, MF:C20H44N4O18S2, MW:692.7 g/mol | Chemical Reagent | Bench Chemicals |
| IRL 1038 | IRL 1038, MF:C68H92N14O15S2, MW:1409.7 g/mol | Chemical Reagent | Bench Chemicals |
The journey from MABEL determination in Phase 1 to population PD in Phase 3 represents an increasingly sophisticated application of receptor occupancy and pharmacodynamic principles. This continuum enables more efficient drug development through quantitative, evidence-based decision making. The comparative data presented demonstrate that modified MABEL approaches combined with robust RO assay validation and appropriate pharmacometric modeling strategies significantly enhance development efficiency while maintaining patient safety.
As drug modalities grow more complex—including bispecifics, trispecific TCEs, and other engineered proteins—the integration of validated target engagement biomarkers with advanced modeling approaches will become increasingly critical for success. Emerging methodologies, including scientific machine learning and high-dimensional flow cytometry, promise even deeper insights into drug-receptor interactions across clinical development phases [1] [41].
Navigating Complex Challenges and Implementing RO Assay Best Practices
Receptor occupancy (RO) assays are essential pharmacodynamic biomarkers used to assess target engagement for biotherapeutics, supporting pharmacokinetic/pharmacodynamic (PK/PD) modeling in clinical studies [5]. These flow cytometry-based assays provide critical data on the extent and duration of drug-receptor binding, informing dose selection and administration frequency [1]. However, their development and implementation face significant technical challenges that can compromise data accuracy and clinical utility. Receptor modulation—including internalization, degradation, and downregulation—presents particular difficulties as these processes can alter receptor availability during sample processing and analysis [5] [1]. Additionally, accurately quantifying RO for targets with low antigen density remains problematic due to limitations in assay sensitivity and dynamic range [42] [43].
These technical hurdles are especially pronounced when developing immunotherapies, where understanding the precise relationship between receptor engagement and biological effect is paramount [44]. Factors such as receptor shedding, internalization following drug binding, and changes in cell surface receptor numbers over time can profoundly complicate RO interpretation [14]. This guide systematically compares current methodologies and technological approaches to address these challenges, providing researchers with validated strategies to enhance assay robustness across diverse therapeutic contexts.
Receptor Internalization: Mechanisms and Experimental Assessment
Molecular Mechanisms of Receptor Internalization
Receptor internalization is a fundamental cellular process that directly impacts RO assay accuracy by altering available target receptors. In dendritic cells (DCs), therapeutic antibodies are primarily internalized through three well-characterized pathways [45] [46]:
Clathrin-Mediated Endocytosis (CME): The major endocytic pathway in mammalian cells, CME is essential for regulating cell signaling and mediates nutrient uptake. Upon receptor binding, activated receptors are phosphorylated, initiating a cascade that forms clathrin-coated pits that invaginate to form clathrin-coated vesicles [45] [46]. These vesicles subsequently fuse with early endosomes to deliver their cargo. DCs express several receptors mediating CME, including C-type lectin receptors, sialic acid binding immunoglobulin-like lectins, death receptors, scavenger receptors, and Fc receptors [45].
Macropinocytosis: This constitutive pathway in DCs mediates non-specific uptake of soluble antigens through actin polymerization at the plasma membrane, leading to membrane ruffling and formation of large endocytic vesicles (macropinosomes) [45] [46]. The process is regulated by small GTPases Rac1 and Cdc42, modifications of submembranous pH, and Na+/H+ exchanger activity [45].
Phagocytosis: This specialized mechanism for internalizing large particles (>0.5 μm) is particularly relevant for aggregated antibodies or immune complexes [46].
The following diagram illustrates these primary internalization pathways used by dendritic cells for therapeutic antibody uptake:
For chimeric antigen receptor (CAR)-T therapies, receptor internalization follows distinct kinetics. CAR molecules are quickly downmodulated upon encountering tumor antigens through rapid ubiquitination of intracellular domains and subsequent internalization for lysosomal degradation [42]. This downmodulation impacts CAR-T cell efficacy, particularly against low-antigen-expressing cancers [43].
Advanced Internalization Assays: Real-Time Imaging vs. Flow Cytometry
Traditional flow cytometry-based internalization assays face limitations including low throughput, restricted DC supply, and endpoint-only data [47]. A breakthrough real-time imaging approach using the IncuCyte platform with Biotracker Orange labeling addresses these challenges:
Table 1: Comparison of Internalization Assay Methodologies
| Parameter | Traditional Flow Cytometry | IncuCyte Real-Time Imaging |
|---|---|---|
| Throughput | Low (limited by DC availability) | High-throughput screening capable |
| Cell Requirement | Substantial number of primary DCs | 5-10% of flow cytometry requirements |
| Temporal Resolution | Endpoint measurements only | Continuous kinetic monitoring |
| Data Output | Quantitative internalization only | Internalization + cell morphology |
| Modality Compatibility | Restricted to Fc-containing antibodies | Suitable for diverse biotherapeutic formats |
| Predictive Performance | Moderate correlation with clinical immunogenicity | High correlation with clinical ADA results |
Experimental Protocol: Real-Time DC Internalization Assay [47]
Antibody Labeling:
- Buffer exchange antibodies to PBS pH 7.4 using 10K MWCO desalting columns
- Determine concentration by A280 measurement and dilute to 2 mg/mL
- Reconstitute BioTracker Orange-NHS dye to 10 mM in DMSO
- Add 5-fold molar excess dye to antibody and incubate 1 hour at room temperature
- Remove free dye using 40K MWCO desalting columns
Quality Control:
- Determine conjugate concentration and degree of labeling (DOL) using:
[protein](mg/mL) = [A280 - (A551 × CF280/551)] × protein Mw(Da) × DF / εprDOL = (A551 × DF) / (ε551, pH7.4 × [protein(M)])
- Characterize conjugate distribution by intact LC-MS
- Determine conjugate concentration and degree of labeling (DOL) using:
Internalization Assay:
- Seed labeled DCs in 96-well plates
- Add labeled antibodies at relevant concentrations
- Monitor continuously using IncuCyte system
- Quantify internalization kinetics through image analysis
This optimized protocol demonstrated significant improvements in predicting immunogenicity risk using a panel of 25 therapeutic antibodies with known clinical anti-drug antibody (ADA) results, outperforming previous flow cytometry-based methods [47].
Receptor Modulation: Experimental Strategies and Mitigation
Receptor Occupancy Assay Formats and Applications
Receptor modulation—including internalization, degradation, and shedding—presents substantial challenges for accurate RO measurement. Different RO assay formats offer specific advantages for addressing these challenges:
Table 2: Receptor Occupancy Assay Formats for Addressing Receptor Modulation
| Assay Format | Mechanism | Clinical Application | Advantages for Modulation Studies |
|---|---|---|---|
| Free Receptor Assay | Measures unoccupied receptors using competing antibodies | Typically used for antagonistic therapeutics that block ligand binding | Direct assessment of available receptors despite internalization |
| Direct Assessment of Bound Receptor | Measures therapeutic antibodies bound to receptors using anti-therapeutic detection | Applied when monoclonal antibodies to the receptor are unavailable | Bypasses need for receptor-specific reagents affected by modulation |
| Total Receptor Assay | Combines therapeutic binding with alternative antibody to different epitope | Useful where receptor levels or cell numbers change over time | Accounts for receptor density fluctuations |
| Receptor Modulation Assay | Measures effect of therapeutic binding on receptor function | Monitoring receptor shedding or inhibition/activation of internalization | Directly quantifies modulation dynamics |
| Functional Receptor Occupancy Assay | Measures biological effects of therapeutic binding (e.g., cytokine production) | Cell proliferation or cytokine production with safety/efficacy implications | Provides functional correlation beyond mere binding |
Experimental Protocol: Competitive RO Assay for Modulation Studies [1]
Sample Preparation:
- Use fresh whole blood specimens (receptor binding can be disrupted by cell isolation/cryopreservation)
- Test different vacutainers to maximize stability and precision
- Avoid PBMC processing when possible (can negatively impact drug binding)
Staining Procedure:
- Divide sample into two aliquots
- Add competitive antibody (binds same epitope as drug) to identify free receptors
- Add non-competitive antibody (binds different epitope) to identify total receptors
- Include phenotypic markers to gate on specific cell populations of interest
- Incubate, lyse red blood cells, wash, and analyze by flow cytometry
Data Analysis:
- Calculate RO using formula:
RO (%) = [1 - (Mean Fluorescence Intensity with competitive antibody / Mean Fluorescence Intensity with non-competitive antibody)] × 100 - Normalize to internal controls to account for receptor density changes
- Correlate with pharmacokinetic data for PK/PD modeling
- Calculate RO using formula:
This approach enables researchers to monitor receptor occupancy despite modulation events, providing more accurate assessment of target engagement [1].
Mitigating Internalization Artifacts in RO Assays
The relationship between receptor signaling and internalization presents particular challenges for B cell receptor (BCR) and CAR-T studies. Research demonstrates that following BCR ligation, a small subpopulation of receptors are phosphorylated and selectively retained at the cell surface as signaling scaffolds, while the larger population of non-phosphorylated receptors is rapidly endocytosed [48]. These processes are mutually exclusive because the same tyrosine-based motifs mediate signaling when phosphorylated but internalization when not phosphorylated [48].
For CAR-T therapies, preventing excessive internalization and degradation represents a key strategy for improving efficacy. Studies show that blocking ubiquitination by mutating intracellular lysine residues enhances recycling of internalized CAR, resulting in more effective long-term tumor killing activity [42]. The increased effectiveness is more pronounced with 4-1BB costimulatory domains compared to CD28 domains [42].
Low Antigen Expression: Enhancement Strategies and Sensitivity Optimization
Engineering Approaches for Low Antigen Sensitivity
Low antigen expression presents significant challenges for both RO assays and therapeutic efficacy. Conventional CAR-T therapies require hundreds of antigen molecules for activation, compared to single peptide-MHC complexes sufficient for native T cell receptor activation [43]. This limited sensitivity restricts CAR-T efficacy against cancers with low antigen expression and contributes to relapse through antigen escape mechanisms [43].
Recent engineering approaches have dramatically improved antigen sensitivity:
IDR-Induced CAR Condensation [43]
- Strategy: Fuse intrinsically disordered regions (IDRs) from FUS, EWS, or TAF15 to CAR C-terminus to promote biomolecular condensation
- Mechanism: IDR fusion promotes CAR clustering, enhances synapse mechanical strength, and improves membrane-proximal signaling
- Results:
- 2-3× higher cytotoxicity against CD19low cancer cells
- Increased granzyme A, granzyme B, perforin, FasL, and IFNγ secretion
- Improved antitumor effects in both blood cancer and solid tumor models
- No spontaneous activation in absence of antigen
Experimental Protocol: IDR CAR Construct Design [43]
Vector Design:
- Use standard CAR backbone (e.g., CD19-targeting FMC63 scFv, CD8α stalk/transmembrane, 41BB/CD28/CD3ζ signaling)
- Fuse selected IDR (FUS, EWS, TAF15) to C-terminus of CD3ζ
- Include superfolder GFP tag for visualization and folding enhancement
- Package into lentivirus for primary T cell transduction
Functional Validation:
- Test cytotoxicity against target cells with high and low antigen expression
- Measure cytotoxic factor secretion (granzymes, perforin, cytokines)
- Assess synapse formation and signaling molecule phosphorylation
- Evaluate in vivo antitumor activity in immune-deficient NSG mice
This engineering approach enhances signaling efficiency without spontaneous activation, addressing the fundamental limitation of CAR antigen sensitivity [43].
Technical Optimization for Low Antigen Detection
Accurate RO measurement for low-abundance targets requires specialized methodological considerations:
Sample Matrix Optimization [1]
- Use fresh whole blood over PBMCs when possible (processing can alter receptor availability)
- Test multiple vacutainer types to maximize receptor stability
- Establish strict sample processing timelines to minimize ex vivo receptor modulation
- Consider stabilizing additives (e.g., Transfix, CytoChex) for remote site sampling
Assay Design Enhancements [14]
- Employ high-sensitivity flow cytometers with enhanced detection capabilities
- Utilize bright fluorophores (PE, APC) rather than FITC for low-density targets
- Implement extended counting times or higher event collection for rare populations
- Include amplification steps (biotin-streptavidin systems) cautiously to avoid background
The following diagram illustrates the integrated workflow for addressing key technical challenges in receptor occupancy assays:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successfully addressing technical hurdles in RO assays requires carefully selected reagents and methodologies. The following toolkit compiles essential resources for robust internalization, modulation, and low antigen expression studies:
Table 3: Essential Research Reagent Solutions for Technical Challenge Mitigation
| Reagent/Material | Primary Function | Specific Application | Considerations & Alternatives |
|---|---|---|---|
| BioTracker Orange-NHS Dye | Direct protein labeling for live-cell imaging | Real-time internalization assays without Fc dependence | Degree of labeling (DOL) 2-4 optimal; avoid over-labeling |
| Competitive & Non-competitive Antibodies | Differentiate bound vs. free receptors | RO assays for modulating receptors | Verify epitope non-overlap; test specificity rigorously |
| Stabilizing Blood Collection Tubes (Transfix, CytoChex) | Preserve receptor expression ex vivo | Multi-site trials with processing delays | Validate compatibility with target receptor first |
| IncuCyte Live-Cell Analysis System | Kinetic imaging of internalization | High-throughput DC internalization screening | Alternative: Traditional flow cytometry with reduced throughput |
| IDR Fusion Constructs (FUS, EWS, TAF15) | Enhance CAR clustering and signaling | Improving CAR-T efficacy against low-antigen targets | No spontaneous activation reported; superior to aggregation approaches |
| Phosphorylation-Specific Antibodies | Detect signaling vs. internalization fates | Studying mutual exclusivity of signaling/internalization | Critical for BCR studies; requires rapid fixation protocols |
| Ubiquitination Mutants (Lysine to Arginine) | Prevent CAR degradation and enhance recycling | Improving CAR-T persistence and sustained cytotoxicity | More effective with 4-1BB vs. CD28 costimulatory domains |
| High-Sensitivity Flow Cytometers | Detect low-abundance antigens | RO assays for low-expression targets | Enhanced photon detection systems; reduced background noise |
| HS014 | HS014, MF:C71H94N20O17S2, MW:1563.8 g/mol | Chemical Reagent | Bench Chemicals |
Addressing the technical hurdles of receptor modulation, internalization, and low antigen expression requires integrated methodological approaches. The strategies compared in this guide demonstrate that real-time imaging platforms, carefully selected RO assay formats, and innovative engineering solutions can significantly enhance data quality and predictive accuracy. As the field advances, emerging technologies like single-cell RNA sequencing and high-dimensional flow cytometry promise even deeper insights into drug-receptor interactions [1]. Furthermore, the continued development of biomolecular condensate engineering through IDR fusion represents a promising avenue for improving therapeutic sensitivity against low-antigen targets [43].
Successful implementation of these approaches requires rigorous validation and understanding of the underlying biological processes. By systematically addressing these technical challenges, researchers can develop more robust RO assays that accurately reflect in vivo target engagement, ultimately enabling more informed decision-making in drug development and optimization of therapeutic efficacy across diverse clinical contexts.
Receptor occupancy (RO) assays provide critical pharmacodynamic data by quantifying the binding of biotherapeutic agents to their cell surface targets, playing an indispensable role in dose selection and optimization throughout drug development [49] [6]. However, the reliability of RO data is profoundly influenced by preanalytical variables including sample matrix selection, stabilization methods, and logistical handling. Flow cytometry-based RO assays are particularly vulnerable to sample-related artifacts because they measure labile drug-receptor interactions on viable cells [50] [5]. The dynamic equilibrium between bound and unbound therapeutic can be disrupted during sample collection, storage, or processing, potentially leading to inaccurate RO measurements and misguided clinical decisions [21] [1]. This guide examines critical sample considerations through an analytical lens, providing comparative data and methodological frameworks to enhance the validity of RO data in target engagement research.
Matrix Selection: Comparative Analysis and Experimental Approaches
The choice of sample matrix significantly influences assay performance, as different matrices preserve the native drug-receptor interaction with varying efficacy. The optimal matrix maintains receptor expression, cellular viability, and the delicate equilibrium between bound and free therapeutic agent.
Comparative Analysis of Sample Matrices
Table 1: Comparison of Sample Matrices for Receptor Occupancy Assays
| Matrix Type | Key Advantages | Key Limitations | Optimal Applications | Impact on RO Measurement |
|---|---|---|---|---|
| Fresh Whole Blood | Preserves native drug-receptor equilibrium; minimal processing artifacts [6] | Limited stability window; logistical challenges [5] | Phase I studies requiring precise PK/PD correlation [14] | High fidelity; reflects in vivo state accurately |
| Stabilized Whole Blood | Extended stability; accommodates shipping logistics [14] | Potential alteration of receptor epitopes or binding characteristics [21] | Multi-site clinical trials requiring batch analysis [1] | Variable; requires validation against fresh blood |
| PBMCs (isolated) | Removes interfering serum components; enables cryopreservation [1] | Processing may perturb drug-receptor equilibrium; potential for cell loss [6] [31] | Studies requiring cell subset analysis or international collaborations [14] | May underestimate RO due to dissociation during processing |
Experimental Protocol for Matrix Validation
To determine the optimal matrix for a specific RO assay, a systematic comparison protocol should be implemented:
Sample Collection: Collect blood from consented donors (n≥5) into multiple anticoagulant tubes (e.g., EDTA, heparin, citrate) [21].
Matrix Processing:
- Aliquot 1: Analyze fresh whole blood within 2 hours of collection (reference standard)
- Aliquot 2: Treat with commercial stabilizers (Transfix, Cyto-Chex)
- Aliquot 3: Isate PBMCs using Ficoll density gradient centrifugation
- Aliquot 4: Process with proprietary stabilization tubes [14]
Stability Time Course: For each matrix, measure RO at predetermined intervals (0, 6, 24, 48, 72 hours) under simulated shipping conditions (ambient temperature and 4°C) [5].
Data Analysis: Calculate percentage change in RO measurements relative to the fresh whole blood baseline. Establish acceptability thresholds based on assay requirements (<20% deviation is typically acceptable for pharmacodynamic biomarkers) [6].
This experimental approach generates quantitative data on matrix-dependent RO stability, enabling evidence-based selection for specific trial designs.
Sample Stabilization: Methods and Methodologies
Stabilization strategies aim to preserve the native drug-receptor interaction while extending analytical windows to accommodate clinical logistics.
Stabilization Mechanisms and Applications
Table 2: Stabilization Methods for RO Assay Samples
| Stabilization Method | Mechanism of Action | Implementation Protocol | Effect on RO Assay |
|---|---|---|---|
| Chemical Fixation (Transfix) | Cross-links cell surface proteins; arrests cellular metabolism [21] | Direct addition to whole blood (volume/volume); incubation for 5-15 minutes at room temperature [14] | Preserves cellular architecture but may mask epitopes; requires extensive validation |
| Metabolic Inhibition (Sodium Azide) | Suppresses energy-dependent receptor internalization and shedding [21] | Addition to final concentration of 0.1% w/v; maintain at 4°C during processing | Maintains surface expression but limited long-term stabilization |
| Protease Inhibition | Prevents receptor cleavage/shedding from cell surface [21] | Cocktail addition targeting serine, cysteine, and metalloproteases | Particularly valuable for receptors prone to shedding (e.g., CD16, CD62L) |
| Temperature Control | Slows biochemical reactions and cellular processes [21] | Consistent maintenance at 4°C from collection to analysis | Simplest approach but limited to short timeframes (<24 hours) |
Experimental Workflow for Stabilization Method Validation
The following workflow diagram illustrates the key decision points in selecting and validating sample stabilization methods:
Diagram 1: Sample Stabilization Validation Workflow
Research Reagent Solutions for Stabilization Studies
Table 3: Essential Reagents for Sample Stabilization Experiments
| Reagent Category | Specific Examples | Function in Stabilization | Implementation Considerations |
|---|---|---|---|
| Commercial Stabilizers | Transfix, Cyto-Chex, Streck Cell Preservative | Cross-linking or stabilizing cell surface proteins | Lot-to-lot variability testing required [21] |
| Protease Inhibitors | PMSF, AEBSF, EDTA, Complete Protease Inhibitor Cocktail | Inhibit receptor shedding | Must be compatible with flow cytometry detection |
| Metabolic Inhibitors | Sodium Azide, 2-Deoxyglucose | Suppress receptor internalization | May interfere with functional assays |
| Anticoagulants | EDTA, Heparin, Citrate | Prevent coagulation and maintain cell viability | Can affect receptor expression and drug binding [21] |
| Viability Markers | 7-AAD, Propidium Iodide, Fixable Viability Dyes | Identify compromised cells for exclusion | Must be validated with stabilization method |
Specimen Logistics: Operationalizing Robust Sample Management
The journey from patient collection to analytical testing introduces multiple variables that can compromise RO data integrity. Strategic logistical planning mitigates these risks through standardized procedures and continuous monitoring.
Logistics Framework and Stability Validation
Implementing a comprehensive specimen logistics framework requires systematic validation of shipping conditions and stability limits:
Temperature Mapping: Document RO stability under various temperature conditions (4°C, ambient, temperature cycling) to establish acceptable shipping parameters [14].
Time Course Analysis: Determine maximum allowable time-to-processing through controlled stability studies simulating worst-case shipping scenarios [5].
Agitation Testing: Evaluate impact of vibration and movement during shipping on RO measurements using orbital shakers to simulate transport conditions.
Comparative Testing: Validate performance of commercial stabilization systems against fresh whole blood standards across multiple donors and sites [1].
Specimen Journey and Monitoring Points
The following diagram maps the critical control points in the specimen logistics pathway where monitoring and intervention preserve sample integrity:
Diagram 2: Specimen Logistics Pathway with Critical Control Points
Experimental Protocol for Logistics Validation
A comprehensive logistics validation study should incorporate these elements:
Simulated Shipping Experiments:
- Prepare fresh whole blood samples from healthy donors (n≥3)
- Spike with therapeutic antibody at concentrations spanning expected clinical levels
- Divide into three treatment arms: (1) No stabilization, (2) Chemical stabilization, (3) Temperature control only
- Subject samples to simulated shipping conditions (vibration, temperature variation, extended hold times)
- Analyze RO at predetermined intervals against non-shipped controls
Acceptance Criteria Establishment:
- Define maximum permissible deviation from baseline RO measurements (±20% typically acceptable for PD biomarkers)
- Establish minimum cell viability thresholds (>90% for robust analysis)
- Set limits for coefficient of variation in replicate samples (<15% for precision)
Clinical Site Training:
- Develop standardized operating procedures for sample handling
- Create visual guides for critical steps in the collection and stabilization process
- Implement competency assessments for site personnel [14]
The generation of reliable receptor occupancy data demands meticulous attention to sample-related variables throughout the experimental workflow. Matrix selection establishes the foundation for data quality, with fresh whole blood generally providing the most accurate reflection of in vivo receptor engagement but presenting logistical challenges. Stabilization methods extend analytical windows but require thorough validation to ensure they do not perturb the drug-receptor interaction. Specimen logistics complete the framework, ensuring that samples maintain integrity from collection to analysis. By systematically addressing these critical sample considerations through the experimental approaches outlined herein, researchers can significantly enhance the reliability of RO data, thereby strengthening dose selection decisions and accelerating the development of biotherapeutic agents.
Receptor occupancy (RO) assays are critical for quantifying how therapeutic drugs bind to their targets on cell surfaces, providing essential pharmacodynamic biomarker data in biopharmaceutical development [6] [21]. These assays typically utilize competitive antibodies (which bind the same epitope as the drug) and non-competitive antibodies (which bind a different epitope) to measure free receptors, total receptors, or drug-occupied receptors [7] [6]. However, researchers frequently encounter a fundamental limitation: the lack of appropriately characterized competitive or non-competitive antibody reagents for their target of interest. This reagent scarcity can significantly impede drug development programs, particularly for novel targets where well-characterized reagents may not yet exist. This guide compares experimental strategies to overcome these limitations, providing validated approaches for generating reliable RO data even with constrained reagent availability.
Core Assay Formats and Their Reagent Requirements
The selection of RO assay format is largely dictated by the drug's mechanism of action and the availability of key reagents [6] [1]. The table below summarizes the three primary formats and their specific reagent dependencies.
Table 1: Core Receptor Occupancy Assay Formats and Reagent Requirements
| Assay Format | Measured Parameter | Key Reagents Required | Primary Applications |
|---|---|---|---|
| Free Receptor Assay [6] [21] | Proportion of receptors not bound by drug | Competitive antibody or labeled drug | Antagonistic drugs that block ligand binding; determining available target sites |
| Total Receptor Assay [6] [21] | Both free and drug-occupied receptors | Non-competitive antibody binding to a distinct epitope | When drug causes receptor up/down-regulation or cell ablation; normalization |
| Bound Receptor Assay [6] [21] | Proportion of receptors bound by drug | Anti-drug antibody (ADA) that does not compete for binding | Low receptor expression; rare cell populations; direct drug binding measurement |
The following diagram illustrates the logical relationship between assay objectives and the selection of these core formats.
Alternative Strategies When Ideal Reagents Are Unavailable
Strategy 1: Saturation Binding Assay
When a competitive antibody is unavailable, a saturation binding assay provides a reliable alternative. This method does not require a competing antibody but instead uses the therapeutic drug itself as a key reagent [1].
Table 2: Saturation Binding Assay Protocol
| Step | Procedure | Purpose | Critical Controls |
|---|---|---|---|
| 1. Sample Split | Divide patient sample into two equal aliquots | Create paired samples for comparison | Ensure identical cell counts and viability |
| 2. Saturation | Saturate one aliquot with excess unlabeled drug | Mimic 100% receptor occupancy | Use known positive control for saturation efficiency |
| 3. Staining | Add therapeutic dose to both aliquots; detect with anti-drug antibody | Measure binding in saturated vs. natural state | Include unstained and isotype controls |
| 4. Calculation | Calculate RO ratio: (1 - MFIunsaturated/MFIsaturated) × 100 | Determine percentage occupancy | Validate with samples of known occupancy |
This method's workflow is straightforward yet effective, as visualized below.
Strategy 2: Early Identification of Non-Competitive Binders
For novel therapeutic development, a proactive strategy involves using yeast surface display libraries with specialized fluorescence-activated cell sorting to directly identify non-competitive antibody fragments during initial library screening [51]. This approach incorporates a labeled orthosteric ligand during library sorting, enabling early selection of binders that do not compete with the natural ligand for the binding site. This method not only identifies non-competitive binders early but also provides additional criteria to refine candidates with desirable properties, ultimately improving the drug discovery process [51].
Strategy 3: Orthogonal Validation with Limited Reagents
When only partially characterized reagents are available, orthogonal validation methods become essential. This approach uses non-antibody-based methods to measure the same target protein, providing strong validation for the assay results [52]. Key orthogonal methods include:
- Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling: Using nonlinear PK profiles to theoretically derive RO when direct measurement isn't feasible [6]
- Ligand Accumulation Measurement: Quantifying accumulation of receptor ligands in circulation as an indirect RO measure [6]
- Downstream Signaling Analysis: Monitoring phosphorylation events or cytokine production as functional correlates of target engagement [21]
Experimental Protocols for Critical Methodologies
Protocol 1: Saturation Binding Assay for Free Receptor Quantification
This protocol adapts the saturation approach when competitive antibodies are unavailable [1].
Sample Preparation:
- Collect fresh whole blood in appropriate anticoagulants (test EDTA, heparin, and citrate for optimal performance)
- Process within 2 hours of collection or stabilize with commercial reagents (Transfix or Cyto-Chex)
- Maintain samples at 4°C throughout processing to minimize receptor internalization
Staining Procedure:
- Divide sample into two 100μL aliquots with identical cell counts
- Add excess unlabeled drug (100x Kd concentration) to Aliquot A
- Incubate both aliquots with therapeutic concentration of drug for 30 minutes at 4°C
- Wash with cold PBS to remove unbound drug
- Add fluorescently-labeled anti-drug antibody to both aliquots
- Incubate for 30 minutes at 4°C in the dark
- Add viability dye and surface phenotype markers
- Acquire immediately on flow cytometer
Data Analysis:
- Gate on live, target cell population using phenotypic markers
- Calculate Mean Fluorescence Intensity (MFI) for both aliquots
- Apply formula: % RO = [1 - (MFIunsaturated/MFIsaturated)] × 100
- Include background subtraction using isotype controls
Protocol 2: Validation of Reagent Specificity
When working with any antibody reagent, rigorous validation is essential. The following table summarizes key validation approaches.
Table 3: Antibody Validation Methods to Ensure Reagent Reliability
| Validation Method | Experimental Approach | Interpretation of Specificity | Limitations |
|---|---|---|---|
| CRISPR-Cas9 Knockout [53] | Delete gene encoding target protein in cell lines | Loss of antibody signal confirms specificity | Not suitable for essential genes; may affect cell viability |
| siRNA Knockdown [53] | Reduce target protein expression via mRNA silencing | Significant signal reduction indicates specificity | Limited utility for proteins with long half-lives |
| Relative Expression [53] | Test across cell types with known expression differences | Signal correlates with expected expression pattern | Requires knowledge of natural expression variation |
| Orthogonal Validation [52] | Compare with non-antibody-based method | Consistent results between methods confirms specificity | Requires establishment of alternative quantification method |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successfully implementing RO assays requires careful selection of reagents and controls. The following table details essential materials and their functions in overcoming reagent limitations.
Table 4: Key Research Reagent Solutions for RO Assays
| Reagent/Category | Specific Function | Application Notes |
|---|---|---|
| Anti-Drug Antibodies (ADA) [6] | Detect bound therapeutic without competing for receptor binding | Critical for bound receptor assays; should be non-neutralizing |
| Bright Fluorophores (e.g., Brilliant Violet) [21] | Enhance detection sensitivity for low-abundance receptors | Compensate for low signal intensity; improve dynamic range |
| Stabilizing Reagents (Transfix, Cyto-Chex) [21] | Preserve receptor expression and RO status during shipping | Enable complex sample logistics; validate for each target |
| Competitive & Non-competitive Antibodies [1] | Measure free and total receptors respectively | Test multiple clones during development; characterize epitopes |
| CRISPR-Cas9 Modified Cells [53] | Provide negative controls for antibody validation | Essential for establishing assay specificity; use early development |
| Sodium Azide/Protease Inhibitors [21] | Prevent receptor internalization and shedding during processing | Maintain receptor integrity; particularly important for internalizing targets |
Navigating reagent limitations for competitive and non-competitive antibodies requires strategic methodological adaptations. The saturation binding assay provides a robust alternative when competitive antibodies are unavailable, while emerging technologies like yeast surface display enable proactive identification of non-competitive binders early in drug discovery. Rigorous antibody validation through knockout models, orthogonal approaches, and careful control selection remains fundamental to all RO assays, regardless of format. By implementing these strategies, researchers can generate reliable, reproducible receptor occupancy data to inform critical decisions on therapeutic dose selection and optimization, even when ideal reagents are constrained. As the field advances, continued development of standardized validation practices and sharing of reagent characterization data across the scientific community will further enhance our ability to overcome these common challenges in biopharmaceutical development.
In the field of drug development, accurate assessment of target engagement is paramount for demonstrating that a biotherapeutic effectively binds its intended receptor or antigen. Receptor occupancy (RO) assays are critical tools for quantifying this engagement, providing essential pharmacodynamic data that informs dose selection and frequency [1]. However, the accurate measurement of RO is frequently compromised by two primary biological confounders: the development of anti-drug antibodies (ADAs) and the occurrence of steric hindrance.
ADAs are immune responses triggered by the therapeutic agent itself, which can range from clinically insignificant antibodies to those that profoundly alter drug pharmacokinetics, efficacy, and safety [54]. Steric hindrance, a biophysical phenomenon, occurs when the binding of one molecule physically blocks the access of another to its nearby epitope due to spatial constraints [55] [56]. In the context of RO assays, this often manifests when the drug itself obstructs the detection antibody's binding site.
The interference from these factors can lead to significant underestimation of total drug concentration or receptor occupancy, potentially confounding critical decisions during drug development [57]. This guide objectively compares current methodologies to mitigate these confounders, providing experimental data and protocols to support robust RO assay validation.
Mechanisms of Interference: ADA and Steric Hindrance
The Challenge of Anti-Drug Antibodies (ADAs)
The administration of biological drugs can provoke an immune response leading to ADA development. These antibodies are categorized as either binding antibodies, which attach to the drug without directly blocking its activity, or neutralizing antibodies (NAbs), which inhibit the drug's biological function [54]. The formation of ADA-drug complexes interferes with ligand binding assays (LBAs) through two primary mechanisms:
- Epitope Blocking: ADAs bind to the very epitopes recognized by the assay's detection antibodies.
- Steric Hindrance: Even if ADAs bind to non-overlapping epitopes, their sheer size can physically prevent the assay antibodies from accessing their target sites on the drug or receptor [57].
The consequence is the measurement of free drug concentration (drug not bound by ADA) rather than the total drug concentration, leading to a potentially severe underestimation of exposure and misinterpretation of pharmacodynamic relationships [57].
Fundamental Principles of Steric Hindrance
Steric hindrance is a fundamental principle in molecular interactions. It is defined as the physical prevention of simultaneous binding to closely spaced epitopes on an antigen due to spatial constraints [56]. In receptor occupancy assays, this becomes a critical concern in two scenarios:
- Therapeutic Blocking: When a biotherapeutic is bound to its target, it can sterically hinder the subsequent binding of a competing antibody used in the flow cytometry panel to detect free receptors [1].
- Detection Limitations: The presence of variable domain glycans (VDGs) on antibodies can sterically impede the Fc-Fc interactions necessary for efficient oligomerization and complement activation [58]. This same principle applies to the assembly of immune complexes in detection systems.
Table 1: Key Characteristics of Biological Confounders in RO Assays
| Confounder | Mechanism of Interference | Primary Impact on RO Assays |
|---|---|---|
| Anti-Drug Antibodies (ADAs) | Formation of ADA-drug complexes that block epitopes or create steric blockade | Underestimation of total drug concentration; false low RO reading |
| Steric Hindrance | Physical blockage of an antibody's paratope by a nearby bound molecule (e.g., drug or glycan) | Inability to detect occupied receptors; false high reading of free receptors |
Comparative Analysis of Mitigation Strategies
Several strategies have been developed to overcome ADA and steric hindrance interference. The following section compares the experimental performance of these key approaches.
Strategies to Overcome ADA Interference
A primary method to address ADA interference is the physical dissociation of ADA-drug complexes prior to analysis. The table below compares different sample pre-treatment methods based on their ability to tolerate drug interference.
Table 2: Comparison of Sample Pre-Treatment Methods for Enhancing Drug Tolerance in ADA Assays
| Pre-treatment Method | Reported Drug Tolerance (μg/mL) | Brief Principle | Key Advantage |
|---|---|---|---|
| Acid Dissociation | 20 | Uses low pH to dissociate immune complexes | Simplicity |
| Affinity Capture Extraction (ACE) | 50 | Captures ADAs while washing away free drug | Specificity |
| Solid-Phase Extraction w/ Acid Dissociation (SPEAD) | 100 | Combines solid-phase capture with acid dissociation | Improved tolerance over acid alone |
| Bead-Based Extraction & Acid Dissociation (BEAD) | 500 | Uses beads for capture and acid elution | High drug tolerance |
| Precipitation & Acid Dissociation (PandA) | 1,000 | Precipitates complexes followed by acid dissociation | Very high drug tolerance |
| Heat Pre-treatment | Effective at >85°C [57] | Denatures ADAs irreversibly via heat | Completeness of ADA ablation |
Heat pre-treatment has emerged as a particularly robust method. Experimental data demonstrates that incubating ADA-spiked samples at a minimum of 85°C for 5 minutes in a shallow water bath prior to analysis by a traditional electrochemiluminescence (ECL) assay completely removed ADA interference. This method also resolved parallelism issues in non-clinical study samples, confirming its utility for providing accurate total drug concentration measurements [57].
Strategies to Overcome Steric Hindrance
Mitigating steric hindrance requires strategic assay design rather than sample pre-treatment. The most effective approach involves the careful selection and validation of critical reagents.
Table 3: Assay Design Strategies to Mitigate Steric Hindrance
| Strategy | Application Context | Mechanism of Mitigation |
|---|---|---|
| Use of Non-Competitive Antibodies | Flow Cytometry RO Assays | employs an antibody that binds to a different, non-overlapping epitope on the target receptor to quantify total receptor count, unimpeded by drug binding [1]. |
| Saturation Assay Format | Flow Cytometry RO Assays | One portion of the sample is saturated with drug to simulate 100% RO. The ratio of signal in the non-saturated vs. saturated portions reveals the true RO, canceling out hindrance effects [1]. |
| Epitope Mapping & Characterization | General Assay Development | Using techniques like X-ray crystallography and SPR to define the precise binding site of therapeutic and detection antibodies allows for the rational selection of non-interfering reagent pairs [55]. |
The power of the non-competitive antibody strategy is illustrated by the structural analysis of the therapeutic antibody LM609. Research showed that LM609 binds to the headpiece of the αVβ3 integrin near the RGD-binding site. Critically, it inhibits ligand binding not by directly occluding the site, but via steric hindrance, physically blocking access for larger ligands [55]. This underscores that hindrance can be a therapeutic mechanism, but also a confounder that must be designed around in assays.
Experimental Protocols for Validation
Protocol for Validating Heat Pre-treatment for ADA Mitigation
This protocol is adapted from a study demonstrating that heat pre-treatment can abolish ADA interference in ligand binding assays [57].
1. Principle: Irreversible denaturation of interfering ADAs in patient samples through heat exposure, allowing for accurate measurement of total drug concentration.
2. Materials:
- Traditional ECL assay reagents (biotin- and ruthenium-tagged detection antibodies, calibration standards, dilution buffer, read buffer)
- MSD GOLD Small Spot Streptavidin Plate
- SECTOR Imager 6000 or similar ECL plate reader
- Shallow water bath capable of maintaining 56–100°C
- Thermo Plastic Elastomer push caps for tubes
3. Procedure: 1. Dilute 10 μL of each calibration standard, quality control, and study sample with 90 μL of an appropriate dilution buffer in 0.75 mL tubes. 2. Cap the tubes securely and incubate them in a shallow water bath at 85°C for 5 minutes. Note: The water level must be low enough to prevent flotation of tube racks. 3. Remove the tubes and decap them. 4. Continue with the standard ECL assay procedure: add 200 μL of the pre-mixed detection antibody solution (AB mix) to each tube. 5. Vortex and incubate on a plate shaker (400 rpm) at room temperature for 60 minutes. 6. While incubating, block a 96-well ECL plate with blocking buffer for 10 minutes, then wash. 7. Transfer 50 μL from each reaction tube in duplicate to the washed plate. 8. Incubate the plate on a shaker (400 rpm) at room temperature for 60 minutes. 9. Wash the plate, add 150 μL of 2x read buffer, and read the plate within 10 minutes.
4. Key Validation Parameters:
- Sensitivity: Confirm the assay's lower limit of quantification is maintained post-heat treatment.
- Parallelism: Demonstrate that diluted samples show linearity, indicating the removal of ADA-induced non-parallelism.
- Stability: Establish the stability of the analyte through the heat pre-treatment step.
Protocol for a Steric Hindrance-Aware RO Assay by Flow Cytometry
This protocol outlines a strategy using competing and non-competing antibodies to negate steric hindrance from the drug itself [1].
1. Principle: Use a pair of antibodies to independently quantify free and total receptors, enabling the calculation of RO regardless of drug-induced steric blocking.
2. Materials:
- Fresh or properly cryopreserved PBMCs from treated subjects
- A flow cytometry panel including phenotypic markers for cell populations of interest
- Critical Reagent 1: A drug-competing antibody (conjugated to a specific fluorochrome)
- Critical Reagent 2: A non-competing antibody that binds a different epitope on the target receptor (conjugated to a different fluorochrome)
- Flow cytometer
3. Procedure:
1. Prepare single-cell suspensions from patient samples (e.g., PBMCs).
2. Split the sample into aliquots for staining.
3. Staining for Free Receptors: To one aliquot, add the competing antibody. This antibody will only bind to receptors not occupied by the drug, as it is sterically hindered from binding if the drug is present.
4. Staining for Total Receptors: To another aliquot, add the non-competing antibody. This antibody binds to an epitope not blocked by the drug, allowing it to stain all receptors regardless of drug occupancy.
5. Include all other phenotypic markers in both tubes to gate on the relevant cell populations.
6. Run the samples on the flow cytometer.
7. Data Analysis: Calculate the Receptor Occupancy (%) using the formula:
RO % = [1 - (Mean Fluorescence Intensity (MFI) of Competing Antibody / MFI of Non-Competing Antibody)] × 100
4. Key Validation Parameters:
- Specificity: Confirm the competing antibody is indeed blocked by the drug and that the non-competing antibody binds independently.
- Linearity & Range: Validate the RO calculation across expected receptor expression and occupancy levels.
- Stability: Ensure the staining is robust across sample handling conditions.
Visualization of Workflows and Mechanisms
Mechanism of Steric Hindrance and Assay Interference
The following diagram illustrates how steric hindrance and ADAs confound traditional assays and how strategic reagent selection provides a solution.
Experimental Workflow for ADA Mitigation by Heat Pre-treatment
This flowchart outlines the key steps in the heat pre-treatment protocol for removing ADA interference from PK samples.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful mitigation of ADA and steric hindrance relies on high-quality, well-characterized reagents. The following table details key materials required for the experiments described in this guide.
Table 4: Essential Research Reagents for Confounder Mitigation
| Reagent/Material | Critical Function | Application Note |
|---|---|---|
| Non-Competing Antibody | Binds to target receptor at an epitope distinct from the drug-binding site to quantify total receptor pool. | Must be rigorously validated for lack of interference with the therapeutic drug [1]. |
| Competing Antibody | Binds the same epitope as the drug; its signal inversely correlates with receptor occupancy. | Used in tandem with the non-competing antibody to calculate RO [1]. |
| Phenotypic Marker Panel | Identifies specific cell subsets of interest within a heterogeneous sample (e.g., PBMCs). | Crucial for ensuring RO is measured on the correct population [1]. |
| Positive Control ADA | Serves as a quality control to validate the performance of ADA detection and mitigation methods. | Polyclonal antibodies from immunized animals are typically used [54]. |
| Tagged Detection Antibodies | Enable signal generation in immunoassays (e.g., biotin/ruthenium for ECL). | Must retain binding affinity after any sample pre-treatment (e.g., heat) [57]. |
| Stable Calibrators & Controls | Define the standard curve and monitor assay performance for both PK and RO assays. | Prepared in a matching matrix to study samples [57]. |
The confounding effects of anti-drug antibodies and steric hindrance present significant but surmountable challenges in the validation of robust receptor occupancy assays. As demonstrated, heat pre-treatment offers a simple and effective physical method to abolish ADA interference, allowing for the accurate measurement of total drug concentration. For steric hindrance, a strategic assay design that leverages non-competitive antibody pairs or saturation formats is the most reliable path to accurate RO quantification.
The choice of mitigation strategy must be guided by the specific drug, its target, and the nature of the interference. By implementing and validating these protocols, researchers can generate highly confident target engagement data, thereby de-risking drug development and ensuring that critical decisions on dosing and efficacy are based on accurate, reliable pharmacodynamic biomarkers.
Receptor occupancy (RO) assays have become a critical element in the preclinical and clinical development of protein-based therapies, providing quantitative insights into the binding of a therapeutic agent to its cellular target [2]. These assays contribute essential data to pharmacokinetic/pharmacodynamic (PK/PD) modeling, helping to bridge preclinical study data and enable the selection of a safe starting dose and dose escalation scheme for first-in-human clinical studies [2] [6]. The reliability and accuracy of RO data, however, are heavily dependent on the rigorous optimization of key assay parameters, including cell density, incubation times, and temperature. Flow and mass cytometry have emerged as ideal platforms for RO assays as they enable advanced phenotyping of the cellular subsets expressing the drug target receptors [2] [59]. This guide objectively compares the performance impact of these critical parameters across different experimental conditions and technology platforms, providing researchers with a structured framework for assay validation.
Experimental Methodologies for Parameter Optimization
Flow Cytometry-Based RO Assay Protocol
The development of flow cytometry-based RO methods requires careful assay design, key reagent characterization, and thorough planning for implementation to ensure reliable and high-quality results [6]. A typical protocol for a free receptor assay format involves the following key steps:
Sample Collection and Preparation: Whole blood is collected into appropriate anticoagulant-containing vacutainers. The choice of anticoagulant can markedly affect cell stability and receptor expression levels [21]. Some laboratories implement proprietary stabilizers, such as Proteomic Stabilizer, followed by storage at -80°C for future analysis [59].
Cell Staining and Incubation: Approximately 100 μL of whole blood is incubated with a fluorescence-labeled detection reagent (e.g., 2.5 μg/mL of a labeled therapeutic antibody) and a panel of phenotypic markers for immune cell identification [60]. The mixture is incubated for 1 hour at 2°C–8°C, protecting it from light [60].
Red Blood Cell Lysis and Fixation: Following incubation, 2 mL of lysing solution is added to remove red blood cells. After washing, cells are resuspended and fixed with 2% paraformaldehyde before analysis [60].
Data Acquisition and Analysis: Samples are analyzed on a flow cytometer. The geometric mean of the specific staining signal is used for quantification, with isotype control values subtracted to derive the specific signal [60]. Receptor occupancy is typically calculated as a percentage of baseline measurements.
Mass Cytometry-Based RO Assay Protocol
Mass cytometry, which uses metal-conjugated antibodies detected by mass spectrometry, reduces signal overlap and allows for higher-parameter measurements [59]. A representative protocol includes:
Cell Preparation and Barcoding: Peripheral blood leukocytes are obtained, permeabilized, and barcoded using a palladium-based barcoding kit to enable sample multiplexing [59].
Antibody Staining: Cells are stained with a metal-conjugated antibody cocktail containing anti-drug and anti-receptor antibodies at saturating concentrations. Staining is performed in a 100 μL volume for 30 minutes at room temperature with intermittent vortexing [59].
Signal Standardization: Quantum Simply Cellular (QSC) beads with known antibody binding capacity are stained with the same metal-conjugated antibodies and used to standardize signal intensity across channels with different detection sensitivities, correcting for potential over- or underestimation of RO [59].
Comparative Analysis of Key Parameters
The table below summarizes optimized parameters for different RO assay methodologies, synthesized from multiple experimental studies:
Table 1: Comparative Analysis of Key Parameters in RO Assays
| Parameter | Flow Cytometry | Mass Cytometry | LC-MS/MS Based |
|---|---|---|---|
| Cell Density/Input | 100 μL whole blood [60] | 1.5×10ⶠcells in 100 μL staining volume [59] | Brain tissue homogenates [61] |
| Incubation Time | 1 hour [60] | 30 minutes [59] | Not explicitly specified |
| Temperature | 2°C–8°C [60] | Room temperature [59] | Not explicitly specified |
| Detection System | Fluorescence [6] | Inductively-coupled plasma mass spectrometry [59] | Liquid chromatography-tandem mass spectrometry [61] |
| Key Quality Controls | Isotype controls, sample stability testing [60] [21] | Mass-minus-one controls, biological negative controls, QSC bead standardization [59] | Tracer characterization, specificity testing [61] |
Impact of Parameter Optimization on Data Quality
Cell Density and Sample Stability Maintaining optimal cell density is crucial for assay precision. Flow cytometry typically uses fixed volumes of whole blood (e.g., 100 μL), while mass cytometry employs controlled cell numbers (e.g., 1.5×10ⶠcells) [59] [60]. Sample stability represents a critical limitation in clinical trials, and different processing methods can significantly impact results. For instance, PBMC processing can negatively affect drug binding, leading to RO underestimation [1]. The selection of anticoagulants in blood collection tubes can also markedly affect cell stability and receptor expression levels [21].
Incubation Time and Temperature Incubation parameters directly influence binding kinetics and assay integrity. Flow cytometry protocols often use longer incubation times (1 hour) at refrigerated temperatures (2°C–8°C) to minimize receptor internalization and degradation [60] [21]. In contrast, mass cytometry methods may employ shorter incubations (30 minutes) at room temperature [59]. These differences reflect platform-specific requirements, with mass cytometry requiring more stringent temperature control during metal tag detection.
Technical Standardization The use of QSC beads in mass cytometry demonstrates the importance of standardization for accurate RO determination. This approach corrects for varying sensitivity across mass cytometer detection ranges, which can otherwise lead to misinterpretation of RO when drug and receptor are detected in different channels [59].
Experimental Workflow for RO Assays
The following diagram illustrates the generalized workflow for receptor occupancy assays, integrating key optimization parameters:
RO Assay Workflow
Research Reagent Solutions
The table below details essential reagents and materials required for implementing robust receptor occupancy assays:
Table 2: Essential Research Reagents for RO Assays
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| Detection Antibodies | Quantify free, occupied, or total receptors | Competitive and non-competitive anti-receptor antibodies; anti-drug antibodies [6] [1] |
| Phenotypic Markers | Identify cell populations of interest | Metal-conjugated antibodies for immune cell subsets (CD3, CD4, CD8, etc.) [59] [60] |
| Stabilization Reagents | Preserve sample integrity | Proteomic stabilizer [59], Transfix, Cyto-chex [21] |
| Standardization Beads | Normalize signals across detection channels | Quantum Simply Cellular (QSC) beads with known antibody binding capacity [59] |
| Cell Processing Reagents | Prepare samples for analysis | Red blood cell lysis buffer, fixation buffer (paraformaldehyde) [59] [60] |
| Vacutainers | Blood collection with anticoagulants | Testing different vacutainers to maximize stability and precision [1] [21] |
The optimization of cell density, incubation times, and temperature parameters represents a fundamental requirement for generating reliable receptor occupancy data in drug development. Flow cytometry offers well-established protocols with refrigerated incubation conditions to maintain receptor integrity, while mass cytometry provides higher-parameter capability but requires sophisticated standardization approaches like QSC beads to address sensitivity variations across detection channels. The selection of appropriate sample matrices and rigorous validation of pre-analytical conditions are equally critical for clinical trial success. As RO assays continue to evolve with emerging technologies, the systematic optimization of these key parameters will remain essential for accurate PK/PD modeling and rational dose selection in biopharmaceutical development.
Biospecific therapeutics, particularly bispecific antibodies (BsAbs), represent a paradigm shift in targeted drug development by enabling a single molecule to engage two distinct biological targets simultaneously [62]. This dual-targeting capability unlocks novel mechanisms of action that extend beyond mere combinations of monoclonal antibodies, including redirecting immune cells to tumor sites, blocking multiple signaling pathways synergistically, and facilitating complex formation between receptors [63]. The global pharmaceutical landscape has witnessed rapid adoption of this innovative approach, with regulatory approvals for BsAbs accelerating significantly since 2021 across oncology and autoimmune diseases [64] [63]. However, this sophisticated therapeutic modality introduces unprecedented challenges for preclinical and clinical development, necessitating equally advanced analytical frameworks to demonstrate target engagement and establish dose-response relationships.
The validation of receptor occupancy (RO) assays has emerged as a critical pharmacodynamic biomarker framework in biospecific therapeutic development [14] [21]. These assays provide essential data on the extent and duration of target engagement, forming a crucial bridge between pharmacokinetic measurements of drug concentration and observed biological effects [1]. For multi-target drugs, the complexity of RO assessment increases exponentially, requiring sophisticated assay designs that can accurately quantify engagement at both targets simultaneously while accounting for potential cooperative effects, internalization dynamics, and differential expression patterns across tissues [14]. This comparison guide examines the unique challenges posed by biospecific therapeutics through the lens of RO assay validation, providing researchers with methodological frameworks for objective performance assessment against conventional single-target alternatives.
Mechanistic Classes and Approved Agents of Bispecific Therapeutics
Structural and Functional Classification of Bispecific Formats
BsAbs can be broadly classified into two structural categories: IgG-like formats containing Fc regions and fragment-based formats lacking Fc domains [62] [63]. IgG-like BsAbs maintain traditional antibody characteristics including longer half-life through FcRn-mediated recycling and potential Fc-mediated effector functions such as antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC) [62]. To address chain mispairing issues during synthesis, technologies like "knobs-into-holes" ensure correct heavy chain assembly, while CrossMab solutions resolve light chain mispairing [62]. Fragment-based BsAbs such as bispecific T-cell engagers (BiTEs) comprise tandem single-chain variable fragments connected by flexible peptide linkers, offering advantages in tumor penetration but suffering from shorter half-lives (typically 2-4 hours) that may require fusion to Fc domains or albumin-binding molecules for extended duration [62].
From a functional perspective, BsAbs operate through three primary mechanisms: (1) bridging immune cells to tumor cells to facilitate cytotoxic killing; (2) concurrently blocking multiple signaling pathways to overcome compensatory resistance mechanisms; and (3) facilitating protein complex formation to initiate specific biological responses [63]. The strategic selection of format and mechanism depends fundamentally on the therapeutic context and desired pharmacological profile, with each approach presenting distinct validation requirements for target engagement assessment.
Clinically Approved Bispecific Antibodies
Table 1: FDA-Approved Bispecific Antibodies for Solid Tumors
| Name | Targets | Indication | Mechanistic Class |
|---|---|---|---|
| Amivantamab | EGFR × cMET | Non-small cell lung cancer | Antigen-cross-linked |
| Tarlatamab | DLL3 × CD3 | Small cell lung cancer | Bridging immune cells |
| Tebentafusp | gp100 × CD3 | Uveal melanoma | Bridging immune cells |
| Zanidatamab | HER2 × HER2 | Biliary tract cancer | Antigen-cross-linked |
| Zenocutuzumab | HER2 × HER3 | NRG1+ solid tumors | Antigen-cross-linked |
| Cadonilimab* | PD-1 × CTLA-4 | Cervical cancer | Dual immunomodulator |
| Ivonescimab* | PD-1 × VEGF | Non-small cell lung cancer | Dual immunomodulator |
Approved in China [64]
The expanding regulatory approvals for BsAbs highlight both the clinical potential and increasing complexity of this therapeutic class. Cadonilimab represents a significant engineering achievement as a tetravalent BsAb with four antigen-binding sites, enabling enhanced antigen binding affinity and more efficient immune response elicitation [63]. Unlike simple combinations of anti-PD-1 and anti-CTLA-4 antibodies, cadonilimab can induce formation of cell doublets by simultaneously binding CTLA-4 and PD-1 on separate cells, demonstrating a unique mechanism exceeding mere combinatorial effects [63]. These advanced structural configurations necessitate equally sophisticated bioanalytical approaches to confirm that both binding sites engage their intended targets simultaneously under physiological conditions.
Receptor Occupancy Assay Methodologies for Multi-Target Drugs
Assay Design Strategies for Target Engagement Assessment
RO assays quantify and characterize the binding of therapeutic biologics to their cell surface targets, providing critical data on pharmacodynamics that informs dose selection and administration schedules [14] [21]. For multi-target drugs, several specialized assay formats have been developed, each with distinct advantages and implementation requirements:
- Free Receptor Assays: Measure unoccupied receptors using labeled competitive antibodies that bind epitopes overlapping with the therapeutic's binding site. These assays are particularly valuable for antagonistic drugs that block ligand binding and downstream signaling [14] [21].
- Total Receptor Assays: Utilize a non-competitive antibody binding to a different epitope on the same receptor to quantify total receptor expression regardless of therapeutic occupancy. This approach is essential when receptor levels or cell numbers fluctuate during treatment [14] [21].
- Bound Receptor Assays: Directly detect therapeutic antibodies bound to their receptors using anti-therapeutic secondary antibodies, providing insight into drug stability and target engagement magnitude, especially valuable for low-abundance receptors [21].
- Functional RO Assays: Examine biological consequences of target engagement such as cytokine production or phosphorylation status of downstream signaling molecules, connecting occupancy directly to pharmacological effects [21].
- Receptor Modulation Assays: Monitor therapy-induced changes in receptor function including shedding or internalization rates that may evolve with continued treatment or dose escalation [21].
Each format generates complementary data, and a comprehensive RO assessment strategy for bispecific therapeutics often requires multiple parallel methodologies to fully characterize the complex engagement profile.
Experimental Protocol for Flow Cytometry-Based RO Assays
Robust RO assessment for biospecific therapeutics relies on carefully validated flow cytometry methods executed with strict attention to technical details [14] [21] [1]:
Sample Preparation Considerations:
- Anticoagulant Selection: Choice of anticoagulant (EDTA, heparin, or citrate) significantly impacts cell stability and receptor expression. Comparative testing is essential during assay validation [21].
- Stabilization Methods: Commercial stabilizers (Transfix, Cyto-chex) or PBMC isolation may be necessary but can alter equilibrium between free and drug-bound receptors. This effect must be characterized before selection [21].
- Temperature Control: Receptor internalization and shedding during processing can be minimized through strict temperature control (4°C), sodium azide pretreatment, or protease inhibitor cocktails [21].
- Sample Age: Shipping time from clinical sites to testing laboratories critically impacts result quality due to progressive degradation, necessitating strict stability testing and potentially standardized fixative collection tubes [14].
Experimental Setup: The saturation assay approach, particularly valuable when competitive antibodies are unavailable, involves splitting samples into saturated (100% RO reference) and unsaturated (actual patient binding) portions [1]. A secondary anti-drug antibody then detects bound therapeutic, with the ratio between conditions revealing RO levels. For complex multi-target drugs, this approach may need implementation for each target individually and in combination.
Data Analysis and Interpretation: RO is typically calculated as percentage saturation using the formula: RO = [Antibody-Receptor Complex] / [Total Receptor] × 100% [21]. Additional outputs include bound receptor expression percentages and receptor density measurements. Data normalization against appropriate controls (isotype controls, fluorescence minus one) is essential for accurate interpretation, particularly when receptor expression levels change during treatment [21].
Figure 1: Receptor Occupancy Assay Development Workflow. The process begins with critical sample preparation considerations before advancing to assay format selection and implementation, culminating in data analysis that correlates occupancy with pharmacokinetic and pharmacodynamic parameters.
Comparative Performance Analysis: Bispecific Therapeutics vs. Conventional Approaches
Therapeutic Performance Metrics
Table 2: Efficacy Comparison Between Bispecific Antibodies and Monoclonal Antibody Combinations
| Therapeutic Approach | Clinical Context | Key Efficacy Metrics | Advantages | Limitations |
|---|---|---|---|---|
| BsAbs (Cadonilimab) | Relapsed/Metastatic Cervical Cancer | Enhanced progression-free survival vs. standard care | Single molecule with fixed stoichiometry; Unique intercellular bridging [63] | Complex manufacturing; Novel toxicity profiles |
| BsAbs (Blinatumomab) | R/R B-cell Acute Lymphoblastic Leukemia | Higher complete remission rates vs. chemotherapy [65] | Redirects cytotoxic T cells to tumor cells; No MHC restriction [65] | Continuous IV infusion required due to short half-life |
| mAb Combinations (Anti-PD-1 + Anti-CTLA-4) | Advanced Melanoma | Synergistic antitumor effects vs. monotherapy [65] | Flexible dosing of individual components; Established safety knowledge | Increased immune-related adverse events [65] |
| BsAbs (Amivantamab) | EGFR-mutated NSCLC with MET-driven resistance | Activity where EGFR inhibitors fail [62] | Simultaneously blocks primary resistance pathways | Unique toxicities like rash and paronychia |
BsAbs demonstrate several distinctive advantages over conventional monoclonal antibody combinations. Unlike combination therapies where each antibody distributes independently, BsAbs maintain fixed stoichiometry between target-binding entities, ensuring coordinated pharmacodynamics at both sites of action [63]. Furthermore, certain BsAbs like cadonilimab can induce unique biological functions such as forming intercellular bridges between PD-1 and CTLA-4 expressing cells—a phenomenon not observed with combination therapy using nivolumab and ipilimumab [63]. This capability to create novel biological interactions represents a key differentiator of BsAbs beyond mere convenience of administration.
Safety and Toxicity Profiles
The safety profiles of BsAbs often diverge significantly from both single-agent monoclonal antibodies and their combinations. T-cell engaging BsAbs frequently induce cytokine release syndrome (CRS) due to potent immune cell activation, requiring sophisticated management protocols [64]. The affinity optimization of each binding arm presents a critical balancing act—for instance, PSMA/CD3 BsAbs with lower CD3 affinity demonstrated improved tumor cell killing with reduced CRS incidence and severity compared to higher affinity variants [62]. Additionally, BsAbs targeting multiple tumor antigens like HER2 T-cell dependent bispecific antibodies can achieve enhanced tumor selectivity through careful affinity tuning, preferentially binding cells with high HER2 expression while sparing normal tissues with lower expression levels [62].
Beyond CRS, BsAbs targeting immune checkpoints may exhibit inflammatory toxicities distinct from corresponding monoclonal antibody combinations. The integrated nature of dual targeting can result in unexpected immune activation patterns or off-target effects not observed with individual agents. Furthermore, the complex architectures and engineered sequences of many BsAbs may heighten immunogenicity risk, potentially leading to anti-drug antibody development that compromises long-term efficacy [63].
Advanced Applications and Research Applications
Bispecific Antibody-Drug Conjugates
The integration of BsAbs with antibody-drug conjugate (ADC) technology represents a frontier in targeted cancer therapy with potential to address fundamental challenges in solid tumor treatment [66]. Bispecific ADCs employ dual-targeting strategies to enhance tumor specificity and counter heterogeneity through several sophisticated targeting logics:
- AND Gate Approaches: Require concurrent expression of both antigens for optimal binding and internalization, maximizing tumor selectivity but potentially limiting activity in heterogeneous tumors where antigen expression varies between cells [66].
- OR Gate Approaches: Bind efficiently to cells expressing either target antigen, addressing heterogeneity but potentially reducing tumor specificity [66].
- AND/OR Gate Approaches: Combine a "clean" but heterogeneously expressed target with a more broadly expressed target, balancing selectivity and coverage [66].
Target selection for bispecific ADCs requires meticulous consideration of co-expression patterns, internalization efficiency, and normal tissue expression [66]. Beyond simple "1+1" combinations, advanced formats including 2+2 or asymmetric 2+1 configurations may better address complex tumor biology, though these introduce additional development challenges [66].
Figure 2: Bispecific ADC Targeting Strategies. AND gate approaches require co-expression of both antigens for optimal binding, while OR gate strategies address heterogeneous tumors where antigens are expressed differentially across cell populations.
Beyond Oncology: Autoimmune Disease Applications
While oncology has dominated BsAb development, autoimmune diseases represent a promising application area where simultaneous targeting of multiple inflammatory pathways may yield superior efficacy compared to single-agent approaches [67]. A novel BsAb targeting TNF-α and IL-6 receptor demonstrated simultaneous neutralization of both pathways in rheumatoid arthritis models, inhibiting TNF-α-mediated cytotoxicity while suppressing IL-6-induced STAT3 phosphorylation [67]. This dual-pathway inhibition addresses the significant limitation of conventional biologic DMARDs, where approximately 30-40% of rheumatoid arthritis patients fail to respond adequately to anti-TNF monotherapy [67].
The development of BsAbs for chronic conditions necessitates particular attention to long-term safety and immunogenicity profiles, which may differ substantially from oncology applications where treatment duration is often limited. Additionally, RO assay strategies for autoimmune applications must account for different target expression patterns in peripheral blood versus inflamed tissues and potentially lower required occupancy levels for efficacy compared to oncology settings.
Essential Research Reagent Solutions
Table 3: Key Reagents for Receptor Occupancy Assay Development
| Reagent Category | Specific Examples | Function in RO Assays | Technical Considerations |
|---|---|---|---|
| Competitive Antibodies | Unlabeled anti-receptor antibodies competing with therapeutic | Quantify free/unoccupied receptors | Must bind overlapping epitope with therapeutic; Specificity critical |
| Non-competitive Antibodies | Antibodies binding different epitope on same receptor | Measure total receptor expression regardless of occupancy | Epitope must not interfere with therapeutic binding |
| Detection Antibodies | Anti-therapeutic secondary antibodies | Directly measure bound therapeutic | Fluorochrome brightness should match receptor abundance |
| Stabilization Reagents | Transfix, CytoChex, Smart Tube | Preserve receptor expression during shipment | Compatibility with target antigen must be verified |
| Viability Markers | 7-AAD, viability dyes | Exclude dead cells from analysis | Should not interfere with receptor detection |
| Cell Population Markers | CD3, CD19, lineage-specific antibodies | Identify specific cell subsets for analysis | Panel design must avoid spectral overlap |
| Reference Standards | Frozen control PBMCs, bead sets | Instrument standardization and assay control | Lot-to-lot consistency critical for longitudinal studies |
The successful implementation of RO assays depends heavily on careful reagent selection and validation [14] [21] [1]. Consistent lot use or thorough lot-to-lot comparisons are particularly important for long-term studies, as minor variations in antibody affinity or specificity can significantly impact occupancy measurements [21]. For bispecific therapeutics, the reagent panel must often be expanded to include detection systems for both targets simultaneously, increasing complexity and potential for interference. Additionally, the growing sophistication of flow cytometry instrumentation enables more complex panels but necessitates enhanced compensation controls and validation procedures to ensure data accuracy across multiple fluorescence channels [1].
Biospecific therapeutics represent a transformative advancement in targeted drug development with demonstrated clinical benefits across multiple disease areas. However, their unique mechanisms of action and complex pharmacological profiles present distinct challenges for preclinical and clinical development, particularly in validating target engagement through receptor occupancy assays. The multi-specific nature of these molecules demands sophisticated bioanalytical approaches that can simultaneously quantify engagement at multiple targets while accounting for potential cooperative effects and dynamic changes in receptor expression.
As the field progresses, emerging technologies including high-dimensional flow cytometry, single-cell RNA sequencing, and computational modeling promise to enhance our understanding of the complex relationship between target engagement, pathway modulation, and ultimate clinical response [1]. Furthermore, the application of BsAbs beyond oncology to autoimmune diseases, infectious diseases, and other therapeutic areas will necessitate adaptation of current RO assessment strategies to different biological contexts and regulatory requirements. Through continued refinement of receptor occupancy assay methodologies and their integration with complementary pharmacokinetic and pharmacodynamic assessments, the drug development community can fully realize the potential of biospecific therapeutics while ensuring their safe and effective deployment for patients in need.
Establishing Assay Robustness: A Fit-for-Purpose Validation Framework
Principles of Fit-for-Purpose Validation for Clinical RO Biomarker Assays
Receptor occupancy (RO) assays are flow cytometry-based pharmacodynamic biomarkers that quantitatively measure the binding of a biotherapeutic drug to its specific target on the cell surface [7]. These assays provide critical data on target engagement, helping researchers understand a drug's mechanism of action, guide dose selection, and establish pharmacokinetic/pharmacodynamic (PK/PD) relationships [14]. The "fit-for-purpose" validation paradigm recognizes that the extent and focus of assay validation should be tailored to the specific context of use (COU), which includes the study phase, the biological and analytical characteristics of the biomarker, and the impact of the data on decision-making [68] [69].
This approach ensures scientific rigor while appropriately allocating resources, acknowledging that validation requirements for an exploratory biomarker in early-phase research differ substantially from those used to support primary endpoints in late-phase trials or regulatory submissions [69]. For RO assays, this is particularly relevant due to their typical use as pharmacodynamic markers in first-in-human studies, where they often support critical go/no-go decisions and dose optimization [5]. The fundamental principle is that the same biomarker may require different validation approaches depending on whether it's used to measure pharmacodynamic response, stratify patients, or support efficacy claims [69].
Regulatory Framework and Biomarker Context of Use
Regulatory Foundations and Biomarker Categories
Regulatory agencies, including the U.S. Food and Drug Administration (FDA), emphasize the importance of Context of Use (COU) in biomarker development and validation [68]. The FDA defines COU as "a concise description of the biomarker's specified use in drug development" and categorizes biomarkers through the BEST (Biomarkers, EndpointS, and other Tools) Resource [68]. RO assays typically fall under pharmacodynamic/response biomarkers, which provide evidence of a biological response to a therapeutic intervention [68].
The fit-for-purpose approach is reinforced in recent regulatory guidance, which suggests using ICH M10 (the standard for bioanalytical method validation for drugs) as a starting point but acknowledges that biomarker assays require unique considerations [70] [71]. This is particularly true for RO assays, which measure endogenous molecules on cell surfaces rather than exogenous drug compounds, presenting distinct challenges for calibration, matrix effects, and precision targets [69].
Evolving Context of Use in Drug Development
The validation requirements for an RO assay dynamically evolve throughout the drug development lifecycle. As a program advances from early to late phases, the context of use may change significantly, necessitating revalidation or additional validation activities [69].
Table: Evolution of RO Assay Context of Use Through Development Phases
| Development Phase | Primary Context of Use | Key Validation Focus |
|---|---|---|
| Preclinical | Target verification, mechanism of action [21] | Analytical specificity, reagent characterization [14] |
| Phase 1 | Pharmacodynamic response, dose selection [14] [21] | Precision at baseline, sample stability, robustness [7] |
| Phase 2 | Efficacy of dosing regimens [14] [21] | Reproducibility across sites, receptor modulation effects [7] |
| Phase 3 | Population pharmacodynamics, long-term safety [14] [21] | Comprehensive validation, transfer to multiple labs [7] |
RO Assay Formats and Methodological Considerations
Comparative Analysis of RO Assay Formats
RO assays can be configured in multiple formats, each with distinct advantages and applications. The selection of the appropriate format depends on the drug's mechanism of action, the biological characteristics of the target receptor, and the availability of specific reagents [14] [21].
Table: Comparison of Receptor Occupancy Assay Formats
| Assay Format | Measured Parameter | Best Applications | Technical Considerations |
|---|---|---|---|
| Free Receptor | Unoccupied receptors using competing antibody [14] [7] | Antagonistic drugs that block ligand binding [21] | Requires antibody that competes with therapeutic for same epitope [7] |
| Total Receptor | Both free and total receptor populations [14] [7] | When receptor expression changes over time [21] | Requires non-competing antibody to different epitope [7] |
| Bound Receptor | Therapeutic antibodies bound to receptor [14] [21] | Low receptor expression or rare cell types [21] | Uses anti-therapeutic antibody; enhances sensitivity [21] |
| Receptor Modulation | Effect on target receptor function [14] [21] | Drugs causing receptor shedding or internalization [21] | Measures functional changes beyond simple binding [14] |
| Functional RO | Biological effects of binding [14] [21] | When safety/efficacy implications are paramount [21] | Measures downstream effects (e.g., cytokine production) [14] |
Essential Research Reagents and Materials
The development of robust RO assays requires carefully selected reagents and materials that ensure reproducibility and reliability throughout the validation process.
Table: Essential Research Reagent Solutions for RO Assay Development
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Specific Antibody Clones | Detect free, bound, or total receptor [7] [21] | Must not compete with therapeutic antibody; test multiple clones [7] |
| Fluorochrome-Conjugated Detection Reagents | Enable measurement by flow cytometry [21] | Bright fluorophores (e.g., Brilliant Violet) enhance sensitivity for low-expression receptors [21] |
| Stabilizing Reagents (Transfix, CytoChex) | Preserve sample integrity [14] [21] | Critical for clinical trials with complex logistics; must be compatible with target receptor [14] |
| Reference Beads | Standardize instrument performance [7] | Enable standardization across multiple labs and instruments [7] |
| Viability Stains | Exclude dead cells from analysis [21] | Improve data quality by focusing on intact cells [21] |
| Isotype Controls/FMO Controls | Establish background signal [7] [21] | Essential for defining positive and negative populations [7] |
Experimental Design and Validation Workflow
The validation of RO assays follows a systematic approach that begins with thorough experimental design and progresses through development, validation, and transfer phases. The entire process is governed by the intended context of use and requires careful consideration of biological, technical, and practical factors.
Diagram 1: Fit-for-Purpose RO Assay Validation Workflow. This workflow illustrates the systematic process for developing and validating RO assays, with each stage building upon the previous one, all guided by the defined Context of Use.
Sample Management and Stability Assessment
Sample stability represents one of the most critical challenges in RO assay validation, as these assays often require fresh whole blood samples and measure labile receptor-drug interactions [7] [5]. Biological factors such as receptor downregulation, internalization, or cell trafficking can significantly impact results if not properly controlled [5].
Stability testing should evaluate multiple factors including shipment time from clinical site to lab, sample age effects on data quality, compatibility of target receptor with stabilizing fixatives, and stability of fixed samples [14]. To address these challenges, researchers implement various strategies such as shipping samples on ice packs, pre-treating cells with sodium azide or protease inhibitor cocktails, and performing the RO assay at 4°C to minimize receptor shedding and internalization [21].
The selection of anticoagulants can markedly affect cell stability, receptor expression levels, and even the binding of the drug to its target receptor [21]. Different processing methods should be thoroughly examined during validation, as the use of commercially available stabilizing reagents or preparation of PBMCs may impact the dynamic equilibrium of free and biotherapeutic-bound receptors [21].
Validation Parameters and Acceptance Criteria
Fit-for-Purpose Validation Criteria
The validation parameters for RO assays should be customized based on study phase, endpoint significance, and data usage [7]. This tailored approach ensures appropriate resource allocation while maintaining scientific rigor for the intended context of use.
Table: Fit-for-Purpose Validation Parameters for RO Assays
| Validation Parameter | Exploratory Assays | Secondary Endpoint Assays | Primary Endpoint Assays |
|---|---|---|---|
| Precision | Limited replication (n=3), focus on baseline variability [69] | Intermediate precision with multiple operators [7] | Comprehensive inter-operator, inter-instrument, inter-day [7] |
| Accuracy | Demonstration of parallelism [70] | Surrogate matrix and surrogate analyte approaches [70] | Standard addition or background subtraction methods [70] |
| Sample Stability | Initial assessment of critical limitations [14] | Defined stability under various conditions [7] | Comprehensive stability profile [7] |
| Sensitivity | Limit of detection established [7] | Limit of quantification defined [7] | Clinical decision point sensitivity [69] |
| Specificity | Cell population identification [21] | Specificity across disease states [7] | Interference testing with related receptors [7] |
| Reproducibility | Single-site validation [7] | Partial transfer to second site [7] | Full multi-site validation [7] |
Experimental Protocols for Key Validation Parameters
Precision and Reproducibility Assessment
For RO assays, precision evaluation must account for the intrinsic day-to-day variability of flow cytometry testing [21]. The experimental protocol should include:
- Instrument Standardization: All instrumentation must be standardized across sites using reference beads, with daily quality controls for instrument performance [7] [21]. Mean fluorescent intensity (MFI) values should be tracked to ensure consistent antibody saturation across all detected markers [7].
- Multi-Operator Validation: At least three operators should be trained to ensure coverage throughout the study duration, particularly for real-time assays where sample processing is time-sensitive [7].
- Inter-Site Validation: When multiple laboratories are involved in global clinical trials, a bridging study should be performed using at least three different drug concentrations to validate reproducibility within defined acceptance criteria [7]. Utilizing reagents from the same lots across sites minimizes lot-to-lot variability [7].
Sample Stability Testing Protocol
Comprehensive stability testing is essential for RO assays due to their sensitivity to sample handling conditions:
- Matrix Comparison: Validate assay performance across different sample matrices (whole blood, fixed whole blood, PBMCs) to determine optimal processing methods [21].
- Time-Course Experiments: Establish stability profiles at multiple timepoints (e.g., 0, 6, 12, 24, 48 hours) using multiple donors and analysts to define acceptable sample processing windows [7].
- Temperature Conditions: Evaluate stability under various shipping and storage conditions (room temperature, 4°C, with stabilizing reagents) to simulate real-world clinical trial scenarios [21].
- Freeze-Thaw Stability: For assays utilizing frozen samples, assess receptor integrity and binding characteristics after multiple freeze-thaw cycles [7].
Implementation in Clinical Development and Data Interpretation
RO Assay Implementation Across Clinical Phases
The application of RO assays evolves throughout the drug development process, with each phase leveraging the biomarker data for distinct decision-making purposes:
Diagram 2: RO Assay Implementation Throughout Clinical Development. This diagram shows how RO assay applications evolve from preclinical target verification to population pharmacodynamics in late-phase trials.
Data Interpretation and Calculation Methods
RO data are typically calculated and reported as percent saturation using the ratio of free receptor versus the total number of receptors measured [21]. The fundamental calculation is:
RO% = [Antibody-Receptor Complex] / [Total Receptor] × 100 [21]
However, alternative outputs include percent bound receptor expression, reported by utilizing a secondary detection antibody that binds to the receptor-bound therapeutic [21]. The specific mathematical model should be validated during assay development and consistently applied throughout the clinical study.
For proper interpretation, researchers must consider biological context, including whether receptor expression changes in response to drug binding (upregulation or downregulation), the impact of receptor internalization on measurements, and the relationship between occupancy levels and pharmacological effects [7] [21]. The optimal therapeutic occupancy level may vary depending on the mechanism of action, with some therapies requiring full saturation for efficacy while others may achieve desired effects at partial occupancy [14].
Fit-for-purpose validation of receptor occupancy assays represents a science-driven framework that aligns validation rigor with clinical context and decision-making impact. By implementing a tailored approach that considers assay format, stage of development, and specific context of use, researchers can generate robust, reliable data to guide drug development decisions while optimizing resource utilization. The continuous evaluation of validation parameters based on evolving clinical needs ensures that RO assays maintain their critical role in accelerating the development of safe and effective biotherapeutics.
Receptor occupancy (RO) assays are critical pharmacodynamic tools in biopharmaceutical development, designed to quantify the binding of a therapeutic agent to its extracellular target on the cell surface [50] [6]. When combined with pharmacokinetic (PK) data, RO results help model PK/PD relationships and inform dose selection decisions throughout the drug development lifecycle, from first-in-human studies to late-phase trials [50] [6] [14]. The validation of these assays presents unique challenges beyond those of standard flow cytometric methods, requiring special consideration of the stability of both the target-bound therapeutic and the target receptor itself [50]. This guide provides a comprehensive comparison of RO assay technologies and methodologies, focusing on the core validation parameters of precision, sensitivity, specificity, and stability, with supporting experimental data and protocols.
Comparative Performance of RO Assay Technologies
The development of RO assays employs various technological platforms, each with distinct performance characteristics and applications. The table below summarizes the key validation parameters for the predominant technologies.
Table 1: Performance Comparison of RO Assay Technologies
| Technology Platform | Typical Precision (%CV) | Sensitivity | Specificity Considerations | Sample Stability Requirements |
|---|---|---|---|---|
| Flow Cytometry (Free/Bound Receptor) [6] [14] | <15-20% (Inter-assay) [21] | Dependent on receptor density and fluorophore brightness [6] [21] | High; ensured via competitive/non-competitive antibody reagents [6] [72] | Critical; requires fresh whole blood, stabilizing tubes, or controlled shipment conditions [14] [21] |
| Flow Cytometry (Total Receptor) [6] [14] | <15-20% (Inter-assay) [21] | Can be enhanced for low-expression targets [6] | High; uses antibody to a different, non-competing epitope [6] [72] | Critical; subject to receptor modulation over time [14] |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) [4] | High (Data not specified) | Exceptionally high; enables real-time RO assessment [4] | Very high; based on chemical specificity for the drug-receptor complex [4] | Can be more robust for certain analytes; avoids issues with cell surface protein instability [4] |
Experimental Protocols for Key Validation Experiments
Protocol for Determining Assay Precision and Sensitivity
Precision, measured as the percentage coefficient of variation (%CV), is fundamental for assessing an assay's reproducibility, while sensitivity defines its lower limit of detection [21].
- Sample Preparation: Prepare a minimum of five replicates of quality control (QC) samples at three different concentration levels (low, medium, and high) representing the expected RO range in the study samples [21].
- Assay Execution: Analyze the QC samples across multiple validation runs, performed on different days by different analysts, to capture inter-assay precision. For intra-assay precision, all replicates are analyzed within a single run [21].
- Data Analysis: Calculate the mean, standard deviation, and %CV for the RO measurements at each QC level. An inter-assay %CV of less than 20-25% is often considered acceptable for validated flow cytometry-based RO assays [21].
- Sensitivity Determination: The limit of detection (LOD) is established by testing serially diluted samples with low receptor expression. The lowest concentration at which the signal can be reliably distinguished from background with a defined precision and accuracy is declared the LOD [6].
Protocol for Establishing Assay Specificity
Specificity ensures that the assay accurately measures the intended target—free, bound, or total receptor—without interference.
- Reagent Selection:
- Free Receptor Assay: Use a labeled detection reagent (e.g., competitive antibody or the drug itself) that binds the same epitope as the therapeutic [6] [72].
- Bound Receptor Assay: Use a fluorescently labeled anti-drug antibody (ADA) that is non-neutralizing and does not compete with receptor binding [6] [14].
- Total Receptor Assay: Use a non-competitive antibody that binds to a different epitope on the target receptor [6] [72].
- Validation Testing: Demonstrate that the detection signal decreases with increasing concentrations of the therapeutic drug in a dose-dependent manner for free receptor assays. Conversely, the signal should increase for bound receptor assays [72]. The use of a non-competitive antibody for total receptor measurement should show a constant signal, independent of drug occupancy, confirming specificity for the total receptor pool [72].
Protocol for Assessing Assay Stability
Sample stability is a major challenge for RO assays and must be rigorously characterized to define sample handling procedures [14] [21].
- Matrix Selection: The assay is typically developed in fresh whole blood, the intended sample matrix for clinical trials [6] [14].
- Stability Time Course: Collect healthy donor blood and hold it at room temperature or 4°C for various time intervals (e.g., 0, 6, 24, 48, 72 hours) before processing and analysis [21].
- Stabilization Evaluation: Test the use of commercial stabilizing reagents (e.g., Transfix, CytoChex) or additives like sodium azide and protease inhibitors to mitigate receptor shedding or internalization during shipment [21].
- Data Interpretation: The stability profile is established by monitoring changes in RO values and the fluorescence intensity of detection reagents over time. The acceptable hold time is defined as the period before a statistically significant change in the RO measurement occurs [21].
Signaling Pathways and Experimental Workflows
RO Assay Formats and Selection Logic
This diagram illustrates the three primary RO assay formats and the decision-making logic for selecting the appropriate format based on the drug's mechanism of action (MOA).
RO Assay Validation Workflow
This workflow outlines the key stages and parameters in a systematic approach to RO assay validation.
The Scientist's Toolkit: Key Research Reagent Solutions
The successful development and validation of an RO assay depend on a suite of critical reagents and materials.
Table 2: Essential Research Reagents and Materials for RO Assays
| Reagent / Material | Function and Role in Validation | Key Considerations |
|---|---|---|
| Competitive Antibody [6] [21] | Detection reagent for free receptor assays; competes with the therapeutic for the same epitope. | Must be well-characterized and have comparable affinity to the drug. Critical for establishing specificity. |
| Non-competitive Antibody [6] [72] | Detection reagent for total receptor assays; binds to a different epitope than the therapeutic. | Confirms that changes in free receptor signal are not due to changes in total receptor number. |
| Anti-Drug Antibody (ADA) [6] [14] | Detection reagent for bound receptor assays; binds to the therapeutic agent itself. | Must be non-neutralizing to avoid disrupting the drug-receptor interaction. |
| Bright Fluorophores [6] [21] | Conjugated to detection antibodies to provide a measurable signal. | Essential for targets with low receptor expression to ensure adequate sensitivity and dynamic range (e.g., Brilliant Violet series). |
| Stabilizing Tubes [14] [21] | Commercial collection tubes (e.g., Transfix, CytoChex) containing stabilizers. | Preserve cell surface epitopes and RO status during sample shipment; stability is a key validation parameter. |
| Fluorochrome-Labeled Therapeutic [72] | Used as a direct detection reagent in some free receptor assay formats. | Requires validation that the conjugation process does not alter the drug's binding affinity or specificity. |
| Characterized Cell Line | Serves as a positive control and system suitability check. | Should express the target receptor at a known, consistent level to monitor assay performance over time. |
The rigorous validation of precision, sensitivity, specificity, and stability is paramount for generating reliable receptor occupancy data that can confidently inform drug development decisions. Flow cytometry remains the dominant platform for RO assays, offering flexibility in format but demanding careful attention to sample stability and reagent specificity [50] [6] [14]. Emerging technologies like LC-MS/MS present compelling alternatives for specific applications, such as small molecule drugs like clopidogrel, by providing real-time occupancy data with high specificity [4]. The choice of assay format and the stringency of validation must always be fit-for-purpose, aligned with the drug's mechanism of action and the intended use of the data throughout the clinical trial lifecycle [14] [21]. By adhering to structured experimental protocols and leveraging the appropriate toolkit of reagents, researchers can ensure their RO assays deliver the robust, high-quality pharmacodynamic biomarkers necessary to bridge pharmacokinetics with clinical efficacy and safety.
Receptor occupancy (RO) assays are critical pharmacodynamic tools in clinical development for immuno-modulatory therapies, quantifying the binding of a therapeutic drug to its specific cell surface target [7]. These flow cytometry-based assays provide essential data on target engagement, which facilitates dose selection and pharmacological monitoring [7]. However, researchers often encounter divergent results when employing different RO assay formats, creating challenges in data interpretation and decision-making. These discrepancies arise from fundamental differences in what each format measures and their technical vulnerabilities. This comparative analysis examines the three principal RO assay formats—free receptor, total receptor, and direct assessment of bound receptor—to provide clarity on interpreting conflicting results. By understanding the unique characteristics, applications, and limitations of each format, researchers can better navigate complex RO data and select the optimal format for their specific therapeutic program.
Comparative Analysis of RO Assay Formats
The choice of RO assay format significantly influences the experimental data obtained and its biological interpretation. Each format employs distinct detection strategies and provides complementary information about drug-receptor interactions.
Table 1: Key Characteristics of Receptor Occupancy Assay Formats
| Assay Format | Measured Parameter | Detection Strategy | Optimal Use Cases | Technical Considerations |
|---|---|---|---|---|
| Free Receptor | Proportion of unbound receptor | Fluorochrome-conjugated antibody competing with drug for same epitope [7] | Determining drug dose-response relationships [7] | Susceptible to artifacts from receptor internalization; requires rapid sample processing [7] |
| Total Receptor | Both free and drug-bound receptor | Two antibodies: one competing, one binding different epitope [7] | Monitoring drug-induced receptor regulation [7] | Requires availability of a non-competing antibody; more complex reagent validation [7] |
| Direct Bound Receptor | Drug-receptor complexes | Antibody binding directly to the therapeutic drug [7] | Low receptor expression or rare target cells [7] | Enhanced sensitivity; depends on quality of anti-drug reagent [7] |
The experimental workflow for developing and executing any RO format requires careful planning and validation, as outlined in the diagram below.
Experimental Protocols & Methodologies
Free Receptor Assay Protocol
The free receptor assay requires specific steps to ensure accurate measurement of unoccupied receptors while preventing ex vivo artifacts.
- Sample Preparation: Collect fresh whole blood in anticoagulant tubes (e.g., sodium heparin). Process samples immediately or within a validated stability window to prevent receptor internalization or degradation [7].
- Staining Procedure:
- Aliquot 100 μL of whole blood into flow cytometry tubes.
- Add a titrated concentration of fluorochrome-conjugated detection antibody that competes with the drug for the same epitope.
- Incubate in the dark for 30 minutes at 4°C.
- Add erythrocyte lysis buffer and incubate for 10 minutes at room temperature.
- Centrifuge at 500 × g for 5 minutes and aspirate supernatant.
- Wash cells with phosphate-buffered saline (PBS) containing 1% bovine serum albumin (BSA).
- Resuspend cell pellet in 200-300 μL of fixation buffer (e.g., 1-4% paraformaldehyde) or acquisition buffer for immediate analysis.
- Flow Cytometry Acquisition: Acquire samples on a flow cytometer calibrated using reference beads (e.g., CS&T beads). Standardize instrument settings, including laser voltages and compensation, based on the established SOP [7].
- Data Analysis: Identify target cell population using forward and side scatter properties and specific cell surface markers. Report free receptor levels as Mean Fluorescence Intensity (MFI) or percentage of positive cells.
Total Receptor Assay Protocol
The total receptor assay builds upon the free receptor protocol but incorporates an additional detection antibody.
- Sample Preparation: Identical to the free receptor assay, emphasizing fresh sample processing.
- Staining Procedure:
- Aliquot 100 μL of whole blood into two tubes: one for the "free receptor" stain and one for the "total receptor" stain.
- Tube 1 (Free Receptor): Add competing antibody as described in section 3.1.
- Tube 2 (Total Receptor): Add both the competing antibody and a non-competing antibody conjugated to a different fluorochrome. This non-competing antibody binds to a different epitope on the receptor not obscured by drug binding [7].
- Complete staining, lysis, washing, and fixation steps as in section 3.1.
- Flow Cytometry Acquisition: Acquire both tubes using the same standardized instrument settings.
- Data Analysis: Analyze the target cell population in both tubes. The MFI from the non-competing antibody in Tube 2 represents the total receptor level, regardless of drug occupancy.
Direct Assessment of Bound Receptor Protocol
This format directly detects the drug bound to its receptor, offering advantages for challenging biological contexts.
- Sample Preparation: Follow the same sample handling procedures as other formats.
- Staining Procedure:
- Aliquot 100 μL of whole blood.
- Add a fluorochrome-conjugated antibody that specifically binds to the therapeutic drug itself (anti-idiotypic antibody) [7].
- Include appropriate controls: an isotype control and a fluorescence minus one (FMO) control to set gating boundaries.
- Complete lysis, washing, and fixation steps as previously described.
- Flow Cytometry Acquisition: Acquire samples using standardized settings.
- Data Analysis: Gate on target cell population. The MFI of the anti-drug antibody staining directly corresponds to the amount of cell-bound drug.
Interpretation of Divergent Results
Divergent results between RO assay formats are not merely technical artifacts but often reflect distinct biological or pharmacological phenomena. The relationship between these formats and the possible explanations for divergent results are illustrated below.
Biological vs Technical Causes of Divergence
Table 2: Interpretation of Divergent RO Results Across Assay Formats
| Divergence Pattern | Potential Biological Explanation | Potential Technical Artifact | Recommended Action |
|---|---|---|---|
| High free receptor + High total receptor | Incomplete target engagement; sub-therapeutic drug dosing [7] | Inadequate detection antibody concentration; improper instrument calibration | Generate a saturation curve to ensure antibody is used at saturating concentrations; verify flow cytometer performance with reference beads [7] |
| Low free receptor + High total receptor | Successful target engagement without receptor modulation [7] | — | Interpret as optimal drug coverage with stable receptor expression |
| Low free receptor + Low total receptor | Drug-induced receptor downregulation [7] | Loss of epitope recognition for non-competing antibody; sample degradation | Validate non-competing antibody performance; verify sample stability and processing timelines [7] |
| Discrepancy between free and direct bound assays | Differential sensitivity to receptor internalization | Poor affinity of anti-drug antibody; drug dissociation during processing | Compare assay performance using samples with known drug concentrations; validate staining conditions |
Validation & Standardization Considerations
Robust validation and standardization are paramount for generating reliable and reproducible RO data, particularly when comparing results across different formats or laboratories.
Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for RO Assays
| Reagent/Material | Function | Critical Quality Attributes |
|---|---|---|
| Viability Dye | Exclude dead cells from analysis | Minimal nonspecific staining; compatibility with fixation |
| Fluorochrome-conjugated Antibodies | Detect free, total, or drug-bound receptors | High specificity; appropriate brightness; minimal lot-to-lot variability [7] |
| Erythrocyte Lysis Buffer | Remove red blood cells | Preserves target cell integrity and surface epitopes |
| Cell Fixation Solution | Stabilize sample for analysis | Maintains light scatter properties and antigen integrity |
| Reference Beads (e.g., CS&T) | Standardize flow cytometer performance | Stable fluorescence; covers multiple laser lines [7] |
| Isotype Controls | Establish background staining levels | Matches host species and isotype of detection antibodies |
| FMO Controls | Determine positive/negative population boundaries | Contains all antibodies in the panel except one |
Assay Validation Parameters
For RO assays used as secondary endpoints in clinical trials, rigorous validation is required [7]. Key parameters include:
- Precision and Accuracy: Assess intra-assay, inter-assay, and inter-operator variability. Test at least three operators to ensure coverage over the study's lifespan [7].
- Sample Stability: Define the acceptable timeframe from sample collection to analysis. For RO assays requiring fresh whole blood, validate stability under various shipping and storage conditions [7].
- Robustness: Evaluate assay performance under varying conditions (e.g., different reagent incubations times, temperature excursions).
- Linearity and Sensitivity: Establish the assay's dynamic range and limit of detection, particularly important for RO assays used for dose determination [7].
The comparative analysis of RO assay formats reveals that each method provides a distinct perspective on drug-receptor interactions, and apparent discrepancies often yield valuable biological insights. The free receptor assay is ideal for dose determination, the total receptor format uniquely detects receptor regulation, and the direct bound receptor format offers superior sensitivity for challenging targets. The optimal format selection depends primarily on the study objective, receptor biology, and reagent availability. By implementing standardized protocols, comprehensive validation, and controlled reagent solutions, researchers can confidently interpret divergent RO results across different formats. This approach enables more accurate assessment of target engagement and supports the rational development of safe, effective immuno-modulatory therapies.
Receptor occupancy (RO) assays are critical pharmacodynamic (PD) biomarkers in the clinical development of large-molecule therapeutics, such as monoclonal antibodies (mAbs) and bispecific antibodies [15] [6]. These flow cytometry-based assays quantitatively measure the binding of a therapeutic drug to its specific cell surface target, providing essential data on target engagement that informs dose selection and establishes pharmacokinetic-pharmacodynamic (PK-PD) relationships [7] [6]. In the context of immuno-modulatory therapies like checkpoint inhibitors, RO assessment becomes particularly valuable for confirming mechanism of action and guiding dose decisions in early-phase clinical trials [15] [21].
This case study examines the specific validation of a "total-drug-bound" RO assay for RG7769 (also known as RO7121661), a bispecific antibody targeting both PD-1 and TIM3 on T cells, which was developed using an IgG1 P329GLALA "Fc-silent" backbone to minimize effector functions [15]. The assay was validated for use in a Phase I dose escalation study (NP40435, NCT03708328) and addresses the particular challenge of accurately measuring target engagement in patients with prior exposure to anti-PD-1 therapies, where steric hindrance from competing antibodies can complicate interpretation [15] [73].
RO Assay Formats: Comparative Approaches and Selection Rationale
Three principal formats exist for flow cytometry-based RO assays, each with distinct advantages and applications [6] [21]:
Table 1: Comparison of Primary Receptor Occupancy Assay Formats
| Assay Format | Measurement Focus | Detection Method | Key Applications |
|---|---|---|---|
| Free Receptor | Proportion of receptors not bound by drug | Fluorochrome-conjugated antibody competing with drug for same epitope [7] | Preferred for antagonistic drugs blocking ligand binding [6] [21] |
| Total Receptor | Both free and drug-occupied receptors | Two antibodies: one competitive, one binding different epitope [7] | When drug affects receptor regulation; provides normalization [6] [21] |
| Drug-Occupied Receptor (Total-Drug-Bound) | Proportion of receptors bound by drug | Anti-drug antibody detecting bound therapeutic [15] [6] | Low receptor expression; rare cell types; avoids reagent competition issues [15] [7] |
Rationale for Total-Drug-Bound Format Selection for RG7769
For RG7769, the "total-drug-bound" format was selected due to several compelling factors. First, the development of a traditional total PD-1 receptor assay proved infeasible because RG7769 binding to PD-1 sterically hindered the binding of PD-1 detection antibodies, reducing signal intensity [15] [73]. Second, the researchers developed a novel detection reagent—an anti-P329GLALA-PE antibody—that specifically recognizes the engineered Fc portion of RG7769, enabling direct detection of the bound therapeutic without interfering with its target binding [15]. This approach offered particular advantages in potential immunogenicity scenarios, as anti-drug antibodies typically target the variable regions rather than the engineered Fc region [15].
This format also enabled simultaneous assessment of both relative RO (%) and quantitative antibody binding capacity (ABC), providing two complementary dimensions of pharmacodynamic data from the same assay [15]. The ABC measurement proved crucial for identifying the impact of prior anti-PD-1 therapy, as it revealed approximately two-fold fewer available binding sites for RG7769 on T cells from patients recently treated with anti-PD-1 antibodies [15] [73].
Experimental Methodology and Workflow
Sample Collection and Processing
The validated RO assay utilized fresh patient whole blood samples collected in sodium heparin tubes [15]. For the staining procedure, 100μl of whole blood was incubated with RG7769 or control antibodies, followed by red blood cell lysis using PharmLyse buffer [15]. After lysis, cells were washed twice with PBS and stained with the antibody panel for flow cytometric analysis [15]. This direct whole-blood staining approach prior to lysis was designed to maintain the native receptor-drug binding equilibrium, which could be disrupted by peripheral blood mononuclear cell (PBMC) isolation procedures [15].
Antibody Panel and Staining Strategy
The optimized staining panel for the RG7769 RO assay included:
- Anti-P329GLALA-PE: The primary detection reagent specifically binding to the engineered Fc region of RG7769 [15]
- CD45-PerCP-Cy5.5 (clone HI30): Leukocyte marker [15]
- CD3-APC (clone OKT3): T-cell marker [15]
- CD56-PE: Natural killer cell marker (used in characterization studies) [15]
- CD4/CD8 antibodies: For T-cell subset discrimination [15]
The researchers implemented a three-tube system for the RO assay: (1) a maximum binding control tube with saturating RG7769 concentrations; (2) a patient sample tube with endogenous RG7769; and (3) a background control tube with isotype control [15].
Flow Cytometry and Quantification Methods
Samples were analyzed on a BD FACS-Symphony flow cytometer equipped with five lasers (355, 405, 488, 561, and 637 nm) [15]. For quantification, the assay utilized BD QuantiBRITE beads to convert mean fluorescence intensity (MFI) values to antibody binding capacity (ABC) units, providing a quasi-quantitative measurement of RG7769 bound per cell [15] [73]. Two calculation methods were compared: a traditional percent RO calculation using the formula RO% = (MFIsample - MFIbackground) / (MFImax - MFIbackground) × 100, and an MFI-based approach that directly used the anti-PGLALA-PE signal [15]. The validation demonstrated that the MFI-based method offered superior precision and robustness, particularly for CD8+ T cells [15].
Diagram 1: Experimental workflow for the total-drug-bound RO assay
Key Validation Parameters and Performance Characteristics
Fit-for-Purpose Validation Approach
The RG7769 RO assay underwent fit-for-purpose validation according to the specific context of its use in a Phase I dose escalation study [15]. This approach tailors the validation parameters and acceptance criteria based on the study phase, endpoint significance, and intended application of the data [7]. For this exploratory endpoint, key validation parameters included inter-assay precision, sample stability, and robustness [15] [7].
Quantitative Performance Data
Table 2: Validation Performance Characteristics of the RG7769 RO Assay
| Validation Parameter | Performance Result | Experimental Details |
|---|---|---|
| Inter-Assay Precision | CV < 20% for CD3+ and CD4+ T cells; Higher variability for CD8+ T cells with %RO method [15] | Precision assessed across multiple runs and operators [15] [7] |
| Sample Stability | Established stability windows for different processing and storage conditions [15] | Stability testing included multiple timepoints and conditions relevant to clinical trial logistics [7] [21] |
| Specificity | Anti-PGLALA-PE specifically detected IgG1-PGLALA without cross-reactivity [15] | Testing against related antibody formats and human IgG [15] |
| Robustness | MFI-based calculation demonstrated superior robustness compared to %RO method [15] | Method comparison across different sample types and conditions [15] |
The validation particularly emphasized precision and sample stability, as these factors are critical for longitudinal monitoring in clinical trials where samples may be processed at different sites or times [7]. The stability of the RO signal was thoroughly characterized to establish appropriate sample handling windows, a crucial consideration for clinical trial logistics [7] [21].
Critical Findings: Steric Hindrance from Prior Anti-PD-1 Therapy
Differential Binding in Treatment-Naïve vs. Treatment-Experienced Patients
A pivotal finding from the clinical application of this RO assay was the stark difference in RG7769 binding capacity between checkpoint-inhibitor (CPI) naïve patients and those with recent anti-PD-1 exposure [15] [73]. While both patient groups achieved complete T-cell RO (~100%) at sufficient drug concentrations, the maximum number of T-cell binding sites for RG7769 pre-dosing was approximately two-fold lower in patients who had recently undergone anti-PD-1 treatment [15]. This finding demonstrated that while relative RO could reach saturation in both populations, the absolute number of engaged targets was substantially reduced in previously treated patients [15].
Mechanism of Steric Hindrance
The reduced binding capacity resulted from steric hindrance exerted by competing anti-PD-1 mAbs that remained bound to PD-1 even after treatment cessation, effectively masking available drug binding sites [15] [73]. This phenomenon occurs because the relatively small extracellular domain of PD-1 can accommodate only a limited number of antibodies simultaneously [15]. When patients transition from one PD-1-targeting therapy to another (such as from a monospecific anti-PD-1 to the bispecific RG7769), residual drug from the prior treatment can block binding of the new therapeutic, leading to potential underestimation of available target receptors [15].
Diagram 2: Mechanism of steric hindrance from prior anti-PD-1 treatment
Essential Reagents and Research Tools
Table 3: Key Research Reagent Solutions for Total-Drug-Bound RO Assays
| Reagent/Resource | Specific Example | Function in RO Assay |
|---|---|---|
| Anti-Drug Detection Antibody | Anti-P329GLALA-PE [15] | Specifically detects bound therapeutic without interfering with target binding [15] |
| Cell Surface Markers | CD45-PerCP-Cy5.5, CD3-APC, CD4/CD8 antibodies [15] | Identifies target cell populations and subsets for population-specific RO analysis [15] [7] |
| Quantification Standards | BD QuantiBRITE Beads [15] | Converts fluorescence intensity to antibody binding capacity (ABC) for quantitative assessment [15] |
| Viability & Activation Reagents | Staphylococcus aureus enterotoxin B (SEB), anti-CD3/anti-CD28 beads [15] | Modulates target receptor expression in validation studies; SEB upregulates PD-1 and TIM-3 [15] |
| Sample Stabilization Reagents | Transfix, Cyto-chex [21] | Preserves receptor expression and binding equilibrium for clinical trial logistics [21] |
Implications for Dose Selection and Clinical Development
The RG7769 RO assay provided critical insights for clinical development, particularly regarding dose selection in different patient populations. The demonstration that complete RO could be achieved in both CPI-naïve and CPI-experienced patients supported the pharmacological activity of RG7769 across the intended treatment population [15]. However, the discovery of reduced binding sites in previously treated patients highlighted the importance of quantitative ABC assessment alongside relative RO measurements [15] [73].
This finding has broader implications for the development of sequential immunotherapy approaches, suggesting that washout periods or dosing adjustments may be necessary when transitioning patients between therapies targeting the same receptor [15]. Furthermore, it underscores the value of RO assays not merely as confirmatory biomarkers of target engagement, but as tools for optimizing therapeutic strategy throughout clinical development [15] [6].
The validation of the total-drug-bound RO assay for RG7769 demonstrates a sophisticated approach to addressing complex pharmacodynamic challenges in bispecific antibody development. By developing a novel anti-PGLALA detection reagent and implementing a fit-for-purpose validation strategy, the researchers created a robust assay capable of generating reliable RO data even in the presence of potential interferents like anti-drug antibodies or residual competing therapeutics [15].
The key innovation of this case study lies not only in the technical validation of the assay itself, but in its application to uncover clinically relevant biological phenomena—specifically, the steric hindrance from prior anti-PD-1 therapy that reduces available binding sites for subsequent PD-1-targeting treatments [15] [73]. This finding emphasizes the importance of incorporating quantitative binding capacity measurements alongside traditional relative RO percentages, particularly in patient populations with prior exposure to competing therapeutics [15].
For researchers developing RO assays for immuno-modulatory therapies, this case study highlights several best practices: the value of total-drug-bound formats when traditional approaches face reagent limitations, the importance of assessing both relative and quantitative binding parameters, and the critical need to validate assays in clinically relevant scenarios, including patients with prior exposure to related therapeutics [15] [7] [6]. As the immuno-oncology landscape continues to evolve with increasingly complex multi-specific molecules, such sophisticated RO assay approaches will become ever more essential for rational therapeutic development and optimal clinical dose selection.
Receptor occupancy (RO) assays are crucial for assessing target engagement in biopharmaceutical development, yet different methodological approaches can yield conflicting clinical data. This was prominently observed with nivolumab, a programmed cell death 1 (PD-1) immune checkpoint inhibitor, where reported RO values varied substantially between clinical studies. This review examines how model-based analyses resolved these discrepancies by elucidating how assay design features—particularly measurement strategies (free vs. bound receptor) and normalization approaches (baseline vs. time-point specific)—fundamentally influence RO interpretation. Through the nivolumab case study, we demonstrate how quantitative systems pharmacology (QSP) modeling provides a mechanistic framework to reconcile seemingly inconsistent data, offering valuable insights for robust RO assay design and interpretation in drug development.
Receptor occupancy assays quantitatively measure how a biotherapeutic binds to its cellular target, providing critical insights into pharmacokinetic-pharmacodynamic (PK-PD) relationships [3]. These assays have become essential biomarkers for protein-based therapeutics targeting cellular antigens, particularly in immuno-oncology and immunology [74]. RO assays support decision-making across the drug development lifecycle, from guiding starting doses in Phase I trials to defining efficacious dosing ranges in later phases [74].
Flow cytometry has emerged as the platform of choice for RO studies due to its ability to measure specific targets using fluorescent tags in complex cell populations [74]. Different RO assay formats can be designed, including: (1) free receptor detection using competitive antibodies to determine unoccupied receptors; (2) total receptor detection using non-competitive antibodies to measure all expressed receptors; and (3) bound receptor measurement using anti-drug antibodies to detect the biotherapeutic bound to its target [74]. Despite their utility, RO assays present interpretation challenges, as demonstrated by the conflicting data obtained for nivolumab, which initially raised questions about assay reliability and dose selection [3].
The Nivolumab RO Discrepancy: A Clinical Data Conundrum
Nivolumab, a human IgG4 monoclonal antibody targeting PD-1, demonstrated efficacy across multiple cancers and received regulatory approval at various doses, including 3 mg/kg every 2 weeks (Q2W), 240 mg flat dose Q2W, and 480 mg flat dose every 4 weeks (Q4W) [75] [76]. However, comprehensive analysis of clinical RO data revealed puzzling discrepancies:
Table 1: Conflicting Nivolumab RO Data from Clinical Studies
| Study Reference | Reported RO | Dose Levels | Sample Processing | Assay Methodology |
|---|---|---|---|---|
| Phase 1 (NCT00730639) | ~70% mean trough RO | 0.1-10 mg/kg Q2W | Cryopreserved PBMCs | Bound receptor measurement normalized to baseline |
| Metastatic RCC (NCT01358721) | ≥90% sustainable RO | 0.3, 2, 10 mg/kg Q3W | Fresh whole blood | Not specified |
| Later Studies | ~99% on CD8+ T cells | 3 mg/kg or 240/480 mg | Cryopreserved PBMCs | Varied methodologies |
The initial Phase 1 study reported mean trough RO of approximately 70% even at the highest doses (10 mg/kg), with a mean peak occupancy of 85% immediately after infusion [3]. Surprisingly, subsequent studies demonstrated sustainable RO ≥90% across all dose levels, including lower doses (0.3 mg/kg and 2 mg/kg) [3]. This discrepancy raised fundamental questions about the relationship between dose, exposure, and target engagement for nivolumab.
Initially, these differences were attributed to sample processing variables—specifically, the use of frozen peripheral blood mononuclear cells (PBMCs) in Phase 1 versus freshly isolated PBMCs in the metastatic renal cell carcinoma (RCC) study [3]. Cryopreservation requires dimethyl sulfoxide, which must be removed during thawing and may compromise assay integrity [3]. However, a hypothesis emerged that the core issue might stem from fundamental differences in how RO was calculated across assays rather than technical artifacts alone [3].
Model-Based Analysis: Resolving the Discrepancy
QSP Modeling Approach
Quantitative systems pharmacology (QSP) modeling provided a mechanistic framework to reconcile the conflicting RO data. A population PK-PD model was developed that incorporated key physiological processes: nivolumab pharmacokinetics, receptor binding dynamics, and internalization rates [3]. The model structure accounted for the interplay between free PD-1 receptors, drug-bound receptors, and their differential internalization rates.
Critical to resolving the discrepancy was the understanding that the internalization rate of bound receptors (PD-1 occupied by nivolumab) is higher than the degradation rate of free PD-1 receptors [3]. This differential turnover creates a dynamic system where measurement approach significantly influences calculated RO values.
Impact of RO Calculation Methods
The model demonstrated that four different equations for calculating RO from the same underlying receptor dynamics could yield substantially different results:
Table 2: RO Calculation Methods and Their Impact
| Calculation Method | Measurement Approach | Normalization | Reported RO Level | Key Characteristics |
|---|---|---|---|---|
| Equation 1 | Free receptor | Baseline | Highest | Overlapping profiles with Eq 2 |
| Equation 2 | Free receptor | Each time point | High | Slightly lower than Eq 1 |
| Equation 3 | Bound receptor | Baseline | Lowest | Complex profile with sharp peak |
| Equation 4 | Bound receptor | Each time point | Medium | Sustained high occupancy |
The simulations revealed that RO calculated using Equation 3 (bound receptor measurement normalized to baseline) produced trough RO values of 60-70%, aligning with Phase 1 data [3]. In contrast, Equation 4 (bound receptor measurement normalized to total receptors at each time point) yielded ≥90% occupancy throughout the dosing interval, matching the metastatic RCC study observations [3]. This mathematical explanation demonstrated that the apparently conflicting data actually represented complementary perspectives on the same biological system.
Experimental Validation
The model predictions were validated against clinical data through several approaches:
Peripheral Blood Monitoring: RO was assessed on circulating CD3+ T cells using flow cytometry at baseline and week 8 post-treatment [77]. The data fitted to a maximum possible effect (Emax) model as a function of nivolumab concentration demonstrated that peripheral PD-1 occupancy was saturated at doses ≥0.3 mg/kg [77].
Dose-Response Relationships: Integrated PK-PD analyses revealed that while a positive dose-dependent objective response trend was observed across tumor types, this relationship plateaued at nivolumab doses of ≥1 mg/kg for melanoma and renal cell carcinoma, and ≥3 mg/kg for non-small cell lung cancer [77]. This plateau effect correlated with RO saturation.
Trough Concentration Monitoring: Population PK modeling established relationships between steady-state trough concentrations (Cminss) and clinical outcomes. The 3 mg/kg Q2W dose provided target saturation while maintaining a favorable benefit-risk profile across tumor types [77].
Experimental Protocols for RO Assessment
Flow Cytometry-Based RO Assays
The following protocols represent methodologies applicable for RO assessment of therapeutic antibodies like nivolumab:
Free Receptor Detection Protocol:
- Collect fresh whole blood or PBMCs in EDTA tubes
- Stain with competitive fluorescently-labeled antibody targeting the receptor epitope distinct from the therapeutic binding site
- Incubate for 30 minutes at 4°C in the dark
- Add erythrocyte lysis buffer and incubate for 10 minutes
- Wash cells with PBS containing 1% BSA
- Analyze by flow cytometry using appropriate gating strategies for target cell populations
- Normalize fluorescence intensity to baseline levels from pre-dose samples [74]
Total Receptor Detection Protocol:
- Process samples as above through step 1
- Stain with non-competitive antibody recognizing receptor epitopes unaffected by therapeutic binding
- Follow steps 3-6 from above protocol
- Calculate total receptor expression regardless of therapeutic occupancy [74]
Bound Receptor Detection Protocol:
- Process samples as above through step 1
- Stain with fluorescently-labeled anti-drug antibody that recognizes the therapeutic without disrupting target binding
- Follow steps 3-6 from above protocol
- Normalize using either baseline (Equation 3) or time-point specific (Equation 4) approaches [3] [74]
Sample Processing Considerations
The choice between fresh and cryopreserved samples significantly impacts RO measurements:
Fresh Whole Blood Processing:
- Immediate processing after collection
- Minimal manipulation preserves receptor integrity
- Requires access to flow cytometry facilities within 24-48 hours
- May yield higher RO values due to minimal receptor loss [3]
Cryopreserved PBMC Processing:
- Isolate PBMCs using density gradient centrifugation
- Cryopreserve in controlled-rate freezer with cryoprotectant (e.g., DMSO)
- Store in liquid nitrogen until analysis
- Thaw rapidly at 37°C with careful removal of cryoprotectant
- May modestly underestimate RO due to receptor manipulation [3]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for RO Assay Development
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Fluorescently-labeled competitive antibodies | Detect free, unoccupied receptors | Must bind epitope distinct from therapeutic binding site |
| Fluorescently-labeled non-competitive antibodies | Detect total receptor population | Should recognize epitopes unaffected by drug binding |
| Anti-drug antibodies with fluorescent conjugates | Detect drug-bound receptors | Should not disrupt drug-receptor interaction |
| EDTA blood collection tubes | Preserve sample integrity | Maintain cell viability during transport |
| Erythrocyte lysis buffer | Remove red blood cells | Improves flow cytometry resolution |
| Cryopreservation medium with DMSO | Long-term sample storage | Requires controlled freezing to maintain viability |
| Flow cytometry calibration beads | Instrument standardization | Enable cross-experiment data comparison |
| Viability dyes (e.g., 7-AAD, propidium iodide) | Exclude dead cells | Critical for accurate RO measurement |
| Cell stimulation cocktails (optional) | Modulate receptor expression | For functional RO assessments |
Implications for Drug Development
The nivolumab RO case study offers several critical lessons for drug development:
Standardization of RO Assay Protocols: The field requires greater standardization in how RO assays are designed, particularly in specifying whether free, bound, or total receptor measurements are being used and what normalization approach is employed [3]. Without this standardization, cross-study comparisons remain challenging.
Model-Informed Drug Development: The successful resolution of the nivolumab RO discrepancy demonstrates the power of QSP modeling to deconvolute complex biological relationships [3]. Regulatory agencies increasingly recognize the value of such modeling approaches for dose selection, particularly for biologics where target-mediated drug disposition may be significant.
Dose Selection Strategies: For nivolumab, the integrated analysis including RO data supported the selection of 3 mg/kg Q2W as a unified dosing regimen across tumor types [77]. This dose provided consistent target saturation while maintaining a favorable benefit-risk profile, demonstrating that RO data, when properly interpreted, can inform optimal dosing strategies.
Beyond Peripheral RO: While peripheral blood RO monitoring provides valuable insights, it may not fully reflect intratumoral target engagement [75]. Model-based simulations of intratumoral RO provide additional evidence to support dosing regimens, particularly for extended-interval dosing such as 480 mg Q4W [75].
The nivolumab experience exemplifies how seemingly discrepant clinical RO data can be reconciled through rigorous model-based analysis. The resolution hinged on recognizing that different assay methodologies—specifically, bound versus free receptor measurement and baseline versus time-point specific normalization—fundamentally alter RO interpretation. This case study underscores that receptor occupancy is not an absolute measurement but rather a contextual one dependent on methodological choices.
For researchers developing therapeutic antibodies, these findings highlight the critical importance of clearly specifying RO assay methodologies and interpreting data within an appropriate mechanistic framework. QSP modeling provides powerful tools to bridge methodological differences and extract biologically meaningful insights from complex RO datasets. As the field advances, standardized approaches to RO assessment coupled with model-based interpretation will enhance our ability to make informed decisions about target engagement and dose selection across the drug development continuum.
Implementing Rigorous Quality Control and Ensuring Assay Reproducibility
Receptor occupancy (RO) assays are pivotal pharmacodynamic (PD) biomarkers in biotherapeutic development, generating critical data on how a drug engages its target receptor. This data is coupled with pharmacokinetic (PK) profiles to model essential PK/PD relationships [78]. These assays are utilized throughout the drug development pipeline, from early-stage compound screening and demonstrating target engagement in disease models to determining starting doses for clinical trials. In later stages, RO data directly informs critical decisions on dose selection and administration schedules [78]. The core principle of an RO assay is the qualitative and/or quantitative assessment of drug binding to its target receptor at a given concentration, which is fundamental for understanding the potential clinical efficacy and safety of therapeutics, including radiopharmaceuticals [79]. Ensuring the quality and reproducibility of these assays is therefore not merely a technical exercise but a fundamental requirement for robust drug development.
Methodological Comparison of RO Assays
Different technical approaches can be taken to investigate the binding of biotherapeutics, each with distinct advantages and specific reagent requirements. The choice of method often depends on the scientific question and the availability of specific detection reagents [78].
Competing vs. Non-Competing Antibodies Method
This method requires two specific antibodies. The competing antibody binds to the same epitope as the drug product, thus quantifying the number of unoccupied targets. The non-competing antibody binds to a different epitope on the same target, quantifying the total number of available receptors. The Receptor Occupancy level is then calculated as the ratio of the signal from the competing antibody to that of the non-competing antibody [78].
Saturated vs. Non-Saturated with Direct Detection
This approach is particularly useful when monoclonal antibodies to the receptor are not available. In this protocol, one aliquot of the sample is saturated with the drug, forcing all available target sites to be occupied, which provides the total receptor number. A second aliquot is left untreated, reflecting the in vivo drug-binding state. The bound drug is then detected directly, often with a labeled secondary antibody. The RO is calculated as the ratio of the signal from the non-saturated sample to that of the saturated sample [78].
Saturated vs. Non-Saturated with Functional Readout
This method follows the same saturation principle but uses a functional correlate instead of direct drug detection. One sample portion is saturated with the drug product, while the other is treated with an isotypic control. Following an in vitro stimulation, the production of cytokines or other functional markers is measured in both conditions. The ratio of cytokine production from the drug-saturated sample to the control sample provides the functional RO. This assay is ideal for measuring the occupancy of bi-modal antibodies [78].
Table 1: Comparison of Key Receptor Occupancy Assay Methodologies
| Methodology | Key Principle | Reagent Requirements | Primary Application |
|---|---|---|---|
| Competing vs. Non-Competing [78] | Ratio of competing (unoccupied receptors) and non-competing (total receptors) antibody signals. | Two specific antibodies binding different epitopes. | Standard RO measurement for monoclonal-based therapies. |
| Saturation with Direct Detection [78] | Ratio of drug signal in non-saturated (current occupancy) vs. saturated (total receptors) samples. | Drug product and a detection antibody for the drug. | Situations where anti-receptor antibodies are unavailable. |
| Saturation with Functional Readout [78] | Ratio of functional output (e.g., cytokine) from drug-saturated vs. control-saturated samples. | Drug product and a method to measure functional output. | Measuring RO for bi-modal antibodies; assessing functional impact. |
Experimental Protocols for Key RO Assays
Protocol: RO Assay via Competing vs. Non-Competing Antibodies
This protocol uses multiparametric flow cytometry for simultaneous detection of RO and other PD markers [78].
- Sample Preparation: Collect whole blood or PBMCs from subjects infused with the drug product and from untreated controls [78].
- Staining:
- Split the sample and stain with the competing antibody (fluorochrome-conjugated).
- In parallel, stain a separate aliquot with the non-competing antibody (conjugated with a different fluorochrome).
- Flow Cytometry Analysis: Acquire data on a flow cytometer configured for the fluorochromes used.
- Data Analysis:
- Gate on the target cell population.
- Determine the median fluorescence intensity (MFI) for both the competing and non-competing antibodies.
- Calculate RO: The level of receptor occupancy is derived from the ratio of the competing to the non-competing signal [78].
Protocol: Platelet P2Y12 Receptor Occupancy Assessment
This specific protocol employs liquid chromatography–tandem mass spectrometry (LC-MS/MS) for real-time RO assessment, as validated in animal models [80].
- Sample Collection: Draw blood samples into appropriate anticoagulant tubes.
- Platelet Isolation: Isolate platelets from the whole blood via centrifugation.
- Sample Processing: Lyse platelets and process to extract the drug-target complex for analysis.
- LC-MS/MS Analysis:
- Inject the sample into a validated LC-MS/MS system.
- Use a specific mass transition to detect and quantify the level of occupied P2Y12 receptor.
- Data Interpretation: The level of platelet P2Y12 occupancy directly correlates with the inhibitory effect on platelet aggregation and reflects clinical factors like dosage, drug-drug interactions, and conditions like type 2 diabetes mellitus [80].
A Framework for Quality Control and Assay Reproducibility
Implementing rigorous quality control (QC) is non-negotiable for generating reliable and reproducible RO data. A comprehensive QC strategy encompasses multiple stages from assay development to execution.
Key QC Parameters and Industry Standards
Adherence to established quality standards, such as Good Clinical Laboratory Practice (GCLP), is essential for assays used in clinical decision-making [78]. Key parameters include:
- Reagent Quality Control: Conduct extensive screening during assay development to determine reagent specificity. Perform rigorous QC on reagents to ensure saturation of the target while maximizing the signal-to-noise ratio. Maintain consistency between reagent batches used in longitudinal quantitative assays to minimize variability [78] [79].
- Instrument Quality Control: Implement rigorous and routine instrumental quality control to ensure longitudinal consistency of data generation over the entire course of a study [79].
- Matrix and Sample Stability: Make optimal matrix selection (e.g., whole blood or PBMC) during assay development based on the target and biology [78]. Evaluate the stability of receptors after sample collection, as this can significantly impact assay design and the validity of results [79].
Table 2: Essential Quality Control Parameters for RO Assays
| QC Area | Key Parameter | Industry Standard/Best Practice |
|---|---|---|
| Reagent QC [78] [79] | Specificity, Signal-to-Noise, Batch Consistency | Extensive screening during development; rigorous QC for saturation and consistency. |
| Instrument QC [79] | Longitudinal Consistency | Regular calibration and monitoring using standardized controls to ensure data stability. |
| Sample & Matrix [78] [79] | Matrix Selection, Receptor Stability | Optimal selection of whole blood or PBMC; assessment of post-collection receptor stability. |
| Regulatory Compliance [78] | Overall Assay Conduct | Adherence to relevant regulatory requirements (e.g., GCLP). |
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents critical for successfully developing and running robust RO assays.
Table 3: Key Research Reagent Solutions for Receptor Occupancy Assays
| Reagent / Material | Function in RO Assays |
|---|---|
| Competing Antibody [78] | Binds the same epitope as the drug; quantifies unoccupied (free) receptors. |
| Non-Competing Antibody [78] | Binds a different epitope; quantifies total available receptors. |
| Fluorescently-Labeled Therapeutic Agent [79] | Used for direct detection of bound receptors in the absence of anti-receptor antibodies. |
| Detection Antibody (Secondary Antibody) [78] | Fluorochrome-conjugated antibody used to detect the bound primary drug in saturation assays. |
| Viability Dye | Distinguishes live cells from dead cells during flow cytometry, improving accuracy. |
| Cell Stimulation Cocktail [78] | Used in functional RO assays to induce a measurable output (e.g., cytokine production). |
| Cytokine Detection Antibodies [78] | Used to measure the functional readout (e.g., via intracellular staining) in functional RO assays. |
Workflow and Pathway Visualization
Receptor Occupancy Assay Development and QC Workflow
The diagram below outlines the critical steps in developing and validating a robust receptor occupancy assay, integrating key quality control checkpoints.
PK/PD Relationship in Receptor Occupancy
This diagram illustrates the central role of receptor occupancy assays in bridging pharmacokinetic (PK) data and pharmacodynamic (PD) effects, forming a critical feedback loop for dose optimization.
Conclusion
The validation of robust receptor occupancy assays is not merely a regulatory checkbox but a fundamental component of rational drug development. As demonstrated, a deep understanding of foundational concepts, careful selection of methodological approaches, proactive troubleshooting, and rigorous fit-for-purpose validation are all critical for generating reliable RO data. This data directly empowers informed decision-making, from first-in-human dose selection to optimizing therapeutic regimens in late-stage trials. Future directions will see RO assays becoming even more integral, especially with the rise of complex modalities like bispecific antibodies and cell therapies. The continued advancement of technologies such as high-dimensional flow cytometry and the adoption of quantitative systems pharmacology (QSP) modeling will further refine our ability to interpret RO data, solidifying its role in accelerating the development of safer and more effective biotherapeutics.
References
- 1. Drug Target Engagement with Flow Cytometry Receptor ... [https://cellcarta.com/science-hub/celltalk-roassays/]
- 2. ICCS 2025 [https://cytometry.org/public-admin/mobile/show_presentation.php?abstractno=90]
- 3. Receptor occupancy assessment and interpretation in terms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9762804/]
- 4. Real-time platelet P2Y12 receptor occupancy as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11873646/]
- 5. Developing And Validating Clinical Receptor Occupancy ... [https://www.cellandgene.com/doc/developing-and-validating-clinical-receptor-occupancy-pharmacodynamic-biomarker-assays-0001]
- 6. Receptor occupancy assessment by flow cytometry as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5042057/]
- 7. Immuno-modulatory with Flow Cytometry-Based Receptor ... [https://www.precisionformedicine.com/blog/advancing-clinical-development-of-immuno-modulatory-therapies-with-flow-cytometry-based-receptor-occupancy-assays/]
- 8. CCR5 Receptor Occupancy Analysis Reveals Increased ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.794638/full]
- 9. The calm after the cytokine storm: lessons from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2269728/]
- 10. TGN1412 – learning from a clinical trials disaster [https://nibsc.org/about_us/worldwide_impact/tgn1412.aspx]
- 11. TGN1412 - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/tgn1412]
- 12. Monoclonal antibody TGN1412 trial failure explained by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2990151/]
- 13. Receptor Occupancy Measurement by Flow Cytometry [https://www.itrlab.com/receptor-occupancy-measurement-by-flow-cytometry/]
- 14. Receptor Occupancy Assay by Flow Cytometry [https://www.precisionformedicine.com/specialty-lab-services/flow-cytometry/receptor-occupancy/]
- 15. A human receptor occupancy assay to measure antiâ€PDâ€1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8451911/]
- 16. Editorial: Application of PKPD modeling in drug discovery ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1614689/full]
- 17. Integrated PK/PD Modeling Relates Smoothened Inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11706246/]
- 18. Physiologically Based Pharmacokinetic Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541349/]
- 19. Mass spectrometry methods and mathematical PK/PD ... [https://www.nature.com/articles/s41467-025-56985-6]
- 20. CellTraceâ„¢ Yellow Cell Proliferation Kit, for flow cytometry 20 Assays [https://www.thermofisher.com/order/catalog/product/C34573]
- 21. Comprehensive Guide to Receptor Occupancy Assays [https://kcasbio.com/blogs/receptor-occupancy-definition-overview-applications/]
- 22. Receptor Occupancy (RO) Assay [https://www.creative-biolabs.com/drug-discovery/therapeutics/receptor-occupancy-ro-assays.htm]
- 23. New opportunities in immunogenicity [https://www.iconplc.com/insights/blog/2025/01/03/new-opportunities-immunogenicity]
- 24. Designing a multicolor flow cytometry protocol [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/designing-a-multicolor-protocol]
- 25. Flow Cytometry Panel Design: The Basics [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-71/bioprobes-71-flow-cytometry-panel-design.html]
- 26. Predicting the Onset of Nonlinear Pharmacokinetics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6202475/]
- 27. Ligands of CD6: roles in the pathogenesis and treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11747410/]
- 28. The OT-II model reveals dual in vitro and in vivo ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1571590/full]
- 29. T cell activation and differentiation is modulated by a CD6 ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0180088]
- 30. CD6 monoclonal antibodies differ in epitope, kinetics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6142284/]
- 31. Receptor Occupancy Flow Cytometry Assays [https://www.bioagilytix.com/blog/receptor-occupancy-flow-cytometry-assays/]
- 32. Best Practices for Receptor Occupancy using Flow Cytometry [https://kcasbio.com/blogs/five-things-to-remember-when-developing-receptor-occupancy-assays-using-flow-cytometry/]
- 33. EuroFlow antibody panels for standardized n-dimensional ... [https://www.nature.com/articles/leu2012120]
- 34. Best practices for optimization and validation of flow ... [https://pubmed.ncbi.nlm.nih.gov/33259706/]
- 35. Determination of the starting dose in the first-in-human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5153257/]
- 36. Modified MABEL Approach for First-in-Human Dose ... [https://www.allucent.com/resources/case-study/modified-mabel-approach-for-fih-dose-selection]
- 37. Population PK (PopPK): The What, The How, and The Why [https://www.quantics.co.uk/blog/poppk-the-what-the-how-and-the-why/]
- 38. Utilizing NCA, PopPK/PD, and PBPK Tools for MIDD Success [https://premier-research.com/perspectives/choosing-the-right-pk-modeling-approach-utilizing-nca-poppk-pd-and-pbpk-tools-for-midd-success/]
- 39. In the Cradle of Pharmacometric Methodology - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12087688/]
- 40. Modeling Successful Phase III Trials [https://www.appliedclinicaltrialsonline.com/view/modeling-successful-phase-iii-trials]
- 41. Comparing Scientific Machine Learning With Population ... [https://pubmed.ncbi.nlm.nih.gov/39921335/]
- 42. Tailoring CAR surface density and dynamics to improve CAR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12049969/]
- 43. IDR-induced CAR condensation improves the cytotoxicity ... [https://www.nature.com/articles/s41589-025-02031-x]
- 44. Design and Validation of a Model of a Receptor Occupancy ... [https://td2inc.com/lp-fcsl-poster-2024-design-and-validation-of-a-model-of-a-receptor-occupancy-assay]
- 45. Antigen-presenting cell internalization is key for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447527/]
- 46. Antigen-presenting cell internalization is key for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1617395/full]
- 47. A real-time imaging approach to quantify dendritic cell ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1632302/full]
- 48. B Cell Antigen Receptor Signaling and Internalization Are ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.0040200]
- 49. How validated receptor occupancy flow cytometry assays ... [https://pubmed.ncbi.nlm.nih.gov/26332593/]
- 50. Recommendations for the development and validation of ... [https://pubmed.ncbi.nlm.nih.gov/26566147/]
- 51. A platform for the early selection of non-competitive ... [https://pubmed.ncbi.nlm.nih.gov/39344812/]
- 52. Guide to Antibody Validation Techniques [https://www.neobiotechnologies.com/resources/antibody-validation-methods/?srsltid=AfmBOor61bVmyDjOatbcbXq_LarZKyr3qwOU7-DAynfCNJhyXnL1tlsZ]
- 53. Raising the Bar for Antibody Validation: Knockouts ... [https://www.thermofisher.com/blog/behindthebench/raising-the-bar-for-antibody-validation-knockouts-knockdowns-and-beyond/]
- 54. Definition, Guidelines, and Anti-Drug Antibody Detection [https://dmpkservice.wuxiapptec.com/articles/379-immunogenicity-testing-definition-guidelines-and-anti-drug-antibody-detection/]
- 55. The Therapeutic Antibody LM609 Selectively Inhibits ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5689087/]
- 56. Steric effects in antibody reactions with polyvalent antigen - PubMed [https://pubmed.ncbi.nlm.nih.gov/2465456/]
- 57. Heat pre-treatment can abolish anti-drug antibody interference ... [https://aapsopen.springeropen.com/articles/10.1186/s41120-022-00056-3]
- 58. Modulation of immunoglobulin G oligomerization by variable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12305304/]
- 59. Optimization of Receptor Occupancy Assays in Mass Cytometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6590231/]
- 60. Evaluation of assay interference and interpretation of CXCR4 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5064743/]
- 61. In vivo receptor occupancy assay of histamine H3 ... [https://www.sciencedirect.com/science/article/abs/pii/S1056871912000342]
- 62. Bispecific antibodies in cancer therapy: Target selection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10501874/]
- 63. Bispecific antibodies: unleashing a new era in oncology ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02390-y]
- 64. Bispecific Antibodies in Solid Tumors: Advances and ... [https://pubmed.ncbi.nlm.nih.gov/40565299/]
- 65. Efficacy and safety of bispecific antibodies vs. immune ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-01956-6]
- 66. The challenges in solid tumour targeting with bispecific ADCs [https://www.ddw-online.com/the-challenges-in-solid-tumour-targeting-with-bispecific-adcs-34873-202505/]
- 67. A novel bispecific antibody targeting TNF-α and IL-6 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511189/]
- 68. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 69. Unlocking the Power of Biomarkers in Early Phase Clinical ... [https://www.agilexbiolabs.com/biomarker-revolution-fit-for-purpose-validation-drug-development/]
- 70. FDA Guidance for Industry on Bioanalytical Method ... [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 71. The 2025 FDA Biomarker Guidance: Understanding ... [https://www.linkedin.com/pulse/2025-fda-biomarker-guidance-understanding-lxoke]
- 72. Design and Validation of a Model of a Receptor Occupancy ... [https://td2inc.com/sitc-2024-poster-design-and-validation-of-a-model-of-a-receptor-occupancy-assay]
- 73. A human receptor occupancy assay to measure antiâ€PD [https://www.bohrium.com/paper-details/a-human-receptor-occupancy-assay-to-measure-anti-pd-1-binding-in-patients-with-prior-anti-pd-1/812490752436207618-6200]
- 74. Fit for Flow Cytometry, Part 1: Ideal for Receptor ... [https://www.bioagilytix.com/blog/the-fit-for-flow-cytometry-part-1-ideal-for-receptor-occupancy-assessment/]
- 75. Model-based evaluation of the efficacy and safety ... [https://www.sciencedirect.com/science/article/pii/S0923753419360703]
- 76. Pharmacokinetics and clinical outcomes of low-dose ... [https://link.springer.com/article/10.1007/s00280-024-04697-x]
- 77. Nivolumab dose selection: challenges, opportunities, and ... [https://jitc.biomedcentral.com/articles/10.1186/s40425-016-0177-2]
- 78. Receptor Occupancy (RO) Assays [https://cellcarta.com/receptor-occupancy-assays/]
- 79. Receptor Occupancy Assay - Alfa Cytology [https://www.rdcthera.com/receptor-occupancy-assay.html]
- 80. Real-time platelet P2Y12 receptor occupancy as a ... [https://www.sciencedirect.com/science/article/pii/S2211383524003277]