Comparative Safety Profiles of Novel vs. Established Drug Classes: A Strategic Framework for Drug Development
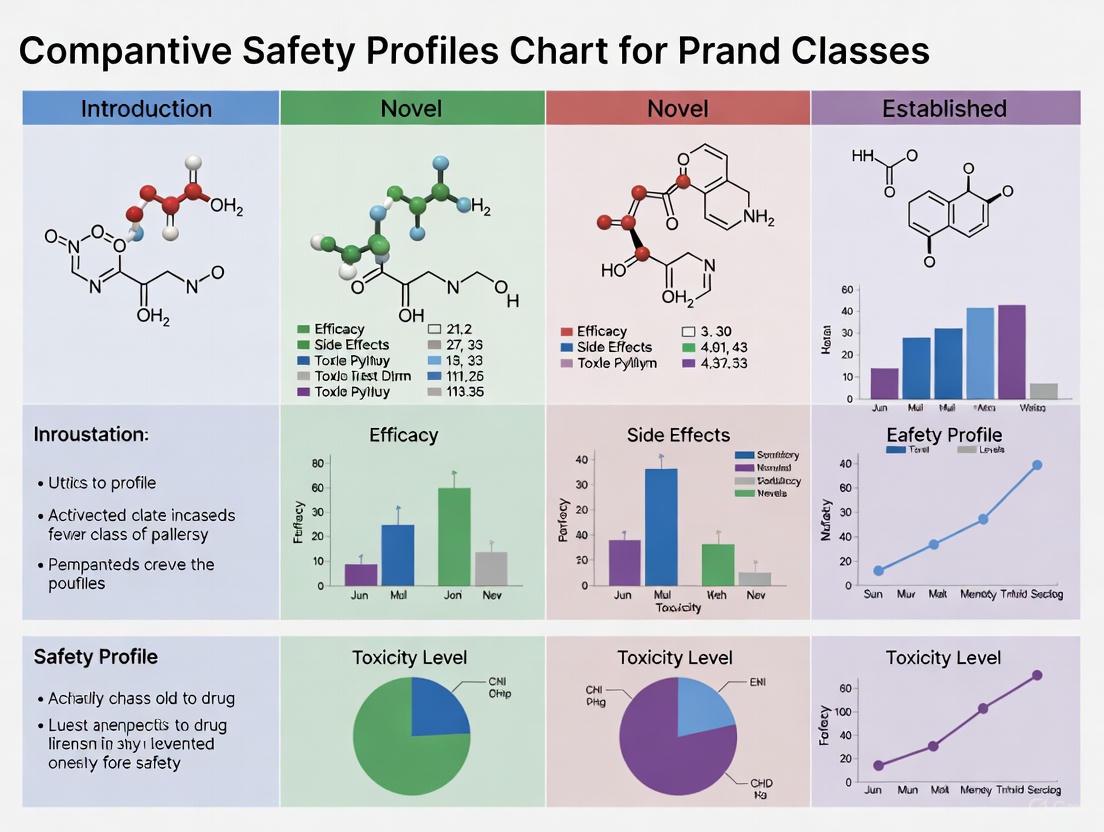
This article provides a comprehensive analysis of the comparative safety profiles of novel and established drug classes, a critical consideration for researchers and drug development professionals.
Comparative Safety Profiles of Novel vs. Established Drug Classes: A Strategic Framework for Drug Development
Abstract
This article provides a comprehensive analysis of the comparative safety profiles of novel and established drug classes, a critical consideration for researchers and drug development professionals. It explores the foundational reasons for safety profile differences, including mechanistic class liabilities and the impact of a drug's lifecycle stage. The piece details advanced methodologies for safety surveillance, from clinical trials to real-world evidence analysis, and offers strategies for troubleshooting common challenges like confounding by indication and signal interpretation. Finally, it presents frameworks for the comparative validation of safety data across drug classes and regulatory environments, synthesizing key takeaways to inform future R&D strategy and regulatory science.
Why Safety Profiles Differ: Foundational Principles and Emerging Patterns
The mechanism of action (MOA) of a pharmaceutical product is a primary determinant of its therapeutic efficacy and its inherent safety profile. A drug's biological target and pathway engagement inevitably shape the adverse event landscape, making certain safety signals a predictable consequence of its pharmacological activity rather than random occurrences. Understanding this relationship is crucial for researchers and drug development professionals, as it influences risk assessment strategies from early discovery through post-market surveillance. This guide examines the critical interplay between drug mechanism and safety, providing a structured comparison of how novel and established drug classes present distinct safety challenges, supported by experimental data and methodological frameworks.
Mechanisms Linking Drug Target to Adverse Events
A drug's mechanism of action can lead to adverse events through several distinct pathways. The diagram below illustrates the primary conceptual routes from pharmacological target engagement to patient harm.
The relationship between mechanism and safety manifests differently across drug classes. On-target adverse events occur when the therapeutic mechanism produces undesired effects in non-target tissues or through excessive pathway modulation, while off-target events result from interaction with unintended biological targets [1]. The presence of mechanistic plausibility—a biologically credible link between drug target and adverse event—significantly increases the likelihood that a safety signal will require regulatory action such as product label updates [2].
Comparative Safety Profiles: Novel vs. Established Drug Classes
The safety profile of a drug class evolves substantially throughout its lifecycle. Newer drug classes often present different safety challenges compared to established therapies, influenced by factors including limited population exposure during pre-approval trials and the novelty of their biological targets.
Table 1: Comparative Analysis of Novel vs. Established Drug Class Safety Considerations
| Characteristic | Novel Drug Classes | Established Drug Classes |
|---|---|---|
| Mechanism Understanding | Limited understanding of downstream effects | Well-characterized safety profile |
| Population Exposure | Restricted diversity and size in pre-marketing trials | Extensive real-world exposure across diverse populations |
| Signal Detection | Higher likelihood of novel, unexpected safety findings | Predominantly known class effects and drug interactions |
| Regulatory Scrutiny | Increased attention due to novelty and limited alternatives | Standard monitoring with established risk management |
| Evidence Base | Primarily preclinical models and limited clinical data | Extensive clinical experience and post-marketing studies |
| Risk Prediction | Dependent on mechanistic plausibility and in silico models | Informed by longitudinal studies and comparative effectiveness |
Evidence suggests that drugs on the market for ≤5 years demonstrate different safety signal patterns compared to more established therapies. One study of European Medicines Agency safety signals found that drugs aged ≤5 years were significantly more likely to require product information updates following signal assessment (adjusted OR 3.9, 95% CI [1.2, 12.7]) [2]. This highlights the "latent liability" of newer agents, where expanded use in broader populations reveals safety concerns not detected in controlled clinical trials.
Case Example: Oncology Targeted Therapies
The contrasting experiences with two novel oncology drug classes—menin inhibitors and CD47 inhibitors—illustrate how mechanism influences safety outcomes. Menin inhibitors, targeting specific genetic subtypes of acute myeloid leukemia (AML), have demonstrated consistent clinical benefit across different compounds in the class with manageable toxicity profiles [3]. In contrast, CD47-targeted therapies, despite promising preclinical results, failed in multiple phase 3 trials due to significant toxicity issues, particularly severe anemia—a predictable consequence of targeting a "don't eat me" signal expressed on red blood cells [3]. This exemplifies how thorough target tissue distribution assessment during development could anticipate such mechanistic toxicities.
Methodological Framework for Safety Signal Investigation
Evaluating the relationship between drug mechanism and safety signals requires systematic assessment protocols. The following experimental workflow outlines a comprehensive approach for investigating mechanism-based safety signals.
Key Methodological Considerations
Data Source Integration: Evidence from multiple data sources significantly increases the predictive value for regulatory action. Signals confirmed through spontaneous reports, observational studies, and preclinical data are 7.8 times more likely to result in product information updates (adjusted OR 7.8, 95% CI [1.5, 40.1]) [2].
Confounding Management: Confounding by indication presents a particular challenge when investigating mechanism-related safety signals. This occurs when the underlying disease or its severity influences both treatment selection and adverse event risk, creating spurious associations [1]. For example, patients with severe depression have higher baseline suicide risk, which may be incorrectly attributed to antidepressant treatment.
Temporal Assessment: Newer drugs may appear to have worse safety profiles due to channeling bias, where patients with more comorbidities or higher risk profiles are preferentially prescribed novel agents [4]. Statistical adjustment for patient characteristics can attenuate these apparent safety differences.
Quantitative Evidence: Factors Predicting Safety-Related Regulatory Actions
Understanding which safety signal characteristics most strongly predict regulatory outcomes helps prioritize investigation resources. The following data summarizes factors associated with product information updates based on European Medicines Agency assessments.
Table 2: Factors Associated with Product Information Updates Following Safety Signal Assessment
| Signal Characteristic | Adjusted Odds Ratio | 95% Confidence Interval | P-value |
|---|---|---|---|
| Evidence in multiple data sources | 7.8 | [1.5, 40.1] | <0.05 |
| Mechanistic plausibility | 3.9 | [1.9, 8.0] | <0.05 |
| Seriousness of the event | 4.2 | [1.3, 13.9] | <0.05 |
| Drug age ≤5 years | 3.9 | [1.2, 12.7] | <0.05 |
Mechanistic plausibility demonstrates one of the strongest associations with regulatory action, nearly quadrupling the odds of product information updates [2]. This underscores the importance of thorough pathway analysis during safety signal assessment, as biologically credible drug-event relationships demand more urgent regulatory attention.
Table 3: Key Research Reagent Solutions for Drug Safety Investigation
| Tool/Resource | Function | Application Context |
|---|---|---|
| FAERS Database | Spontaneous adverse event reporting system | Early signal detection through disproportionality analysis |
| Electronic Health Records | Longitudinal patient data from clinical care | Signal validation in real-world populations |
| OMOP Common Data Model | Standardized data structure across databases | Large-scale network studies across multiple institutions |
| Knowledge Graphs | Representation of drug-event-pathway relationships | Mechanistic plausibility assessment and hypothesis generation |
| Self-Controlled Study Designs | Within-person comparison of risk periods | Control for time-invariant confounding in safety studies |
| High-Dimensional Propensity Scores | Automated confounder identification and adjustment | Addressing confounding in observational safety data |
Recent advances in artificial intelligence are transforming safety signal detection, with knowledge graph-based methods achieving AUCs of 0.92 in classifying known causes of adverse drug reactions [5]. However, researchers must exercise caution with spontaneous reporting databases like FAERS, as methodological limitations and potential for data exploitation can generate spurious signals [6].
The mechanism of action serves as both blueprint for therapeutic efficacy and predictor of potential harm. Understanding the inherent liabilities associated with specific drug targets enables more proactive safety monitoring throughout the product lifecycle. While novel drug classes offer therapeutic breakthroughs, they present distinct safety assessment challenges due to limited population exposure and incomplete understanding of downstream pathway effects. Established drug classes benefit from extensive real-world experience but require vigilance for rare or long-term adverse events. A systematic approach integrating evidence from multiple data sources, assessing mechanistic plausibility, and accounting for confounding factors provides the most robust framework for evaluating drug safety signals. As methodological innovations continue to emerge—particularly in artificial intelligence and real-world evidence analytics—the capacity to anticipate and validate mechanism-based safety concerns will further strengthen the drug development process and post-market surveillance.
For researchers, scientists, and drug development professionals, understanding the evolution of a drug's safety profile throughout its market life is paramount. The "lifecycle effect" describes the dynamic interplay between the time a drug spends on the market and the accumulation of knowledge about its safety in real-world populations. This phenomenon challenges the static view of drug safety established at the time of regulatory approval. The post-marketing phase serves as a continuous, large-scale experiment, where exposure in broader, more heterogeneous populations under less controlled conditions inevitably reveals new safety information. This article synthesizes evidence on how this lifecycle effect manifests, comparing the observed safety profiles of novel versus established drug classes, and outlines the key methodological frameworks used to study it.
Quantitative Evidence: Comparing Safety Over the Market Lifecycle
Empirical studies consistently demonstrate that a drug's observed safety profile changes and typically becomes more refined as its time on the market increases. The data below summarizes key findings from observational studies and regulatory analyses.
Table 1: Summary of Key Studies on Drug Safety and Market Age
| Study Focus | Data Source & Period | Key Finding Related to Market Age | Effect Size / Statistics |
|---|---|---|---|
| First-in-Class vs. Non-First-in-Class Drug Safety [7] | Health Canada approvals (1997-2012); Post-market safety warnings from MedEffect Canada. | First-in-class drugs had a better benefit-to-harm ratio post-market compared to non-first-in-class drugs. | No statistically significant difference in time to first safety warning; trend favored first-in-class. |
| b/tsDMARDs in Rheumatoid Arthritis [4] | Swedish nationwide registers (2006-2022); 33,550 treatment initiations. | Drugs initiated >5 years after market entry were associated with lower rates of safety outcomes vs. those initiated <2 years post-entry. | Unadjusted HR = 0.74 (95% CI: 0.67-0.81); Adjusted HR = 0.93 (95% CI: 0.84-1.03). |
| Adverse Event Reporting in Older Adults [8] | FDA Adverse Event Reporting System (FAERS). | The proportion of patients aged ≥65 in ICSRs has grown from ~20% in 1970 to ~40% in 2020, reflecting increased post-market surveillance in a vulnerable population. | N/A (Demographic trend data) |
Table 2: Analysis of First-in-Class Drug Innovativeness and Review Status [7]
| Drug Category | Total Drugs Evaluated | Number (%) Rated as Innovative | Proportion Receiving Priority Review |
|---|---|---|---|
| First-in-Class | 98 | 16 (16.3%) | Significantly higher than non-first-in-class |
| Non-First-in-Class | 194 | 9 (4.6%) | Significantly lower than first-in-class |
Experimental Protocols for Studying the Lifecycle Effect
Research into the lifecycle effect relies on sophisticated observational study designs and pharmacovigilance methodologies that leverage real-world data (RWD). Below are detailed protocols for key study types cited in this field.
Protocol 1: Retrospective Cohort Study Using National Registers
This protocol is based on the Swedish study investigating the safety of biologic/targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) [4].
- Objective: To investigate rates of key safety outcomes in patients initiating b/tsDMARDs, analyzing trends over time since the market entry of each drug class and by calendar period.
- Data Sources:
- Clinical Quality Register: Swedish Rheumatology Quality Register (for identifying RA patients and their treatments).
- National Administrative and Health Registers: Including the National Patient Register, Cause of Death Register, and Cancer Register (for outcome and covariate data).
- Study Cohorts:
- Primary Cohort: Patients initiating a b/tsDMARD (n = 33,550 initiations).
- Comparison Cohorts:
- An early bionaive RA cohort (n = 16,011).
- A matched general population cohort (n = 111,074).
- Outcomes: The first occurrence of a composite endpoint: major adverse cardiovascular event (MACE), venous thromboembolism (VTE), cancer, or serious infection.
- Statistical Analysis:
- Follow-up: Starts at treatment initiation and continues until the first outcome event, death, emigration, or end of the study period.
- Primary Exposure:
- Time since market entry: Stratified into <2 years, 2-5 years, and >5 years.
- Calendar period of initiation: Grouped as 2006-2010, 2011-2015, 2016-2021.
- Modeling: Calculation of incidence rates (IRs). Use of Cox regression models to calculate Hazard Ratios (HRs), both unadjusted and adjusted for patient characteristics (e.g., age, sex, comorbidities, concomitant medications). The models account for the "channeling" of newer drugs to patients with fewer treatment options or more severe disease.
Protocol 2: Regulatory Database Analysis for Post-Market Safety Warnings
This methodology is derived from the analysis of Health Canada-approved drugs [7].
- Objective: To compare the time to first serious post-market safety warning between first-in-class and non-first-in-class drugs.
- Data Sources:
- Approval Data: Health Canada's annual reports from the Therapeutic Products Directorate and the Biologics and Genetic Therapies Directorate (1997-2012).
- First-in-Class Designation: Determined based on FDA pharmacologic class designations and supplementary commercial databases (e.g., Drug Facts and Comparisons, Pharmaprojects).
- Safety Data: Recalls and Safety Alerts Database on the MedEffect Canada website (a comprehensive list of advisories).
- Safety Endpoint:
- Inclusion: First serious post-market safety advisory or drug withdrawal for safety reasons. Serious advisories were defined as those using bold black print and/or boxed warnings.
- Exclusion: Advisories related to specific batch recalls, manufacturing problems, or medication errors without new safety findings.
- Statistical Analysis:
- Time-to-Event Analysis: Kaplan-Meier survival curves were generated for the time from drug approval until the first safety event.
- Comparison: Curves for first-in-class and non-first-in-class drugs were compared using a Log-rank (Mantel-Cox) test to assess for statistically significant differences in safety experience.
Visualizing the Drug Safety Lifecycle Assessment
The following diagram illustrates the core workflow and key influencing factors in assessing a drug's safety profile throughout its market lifecycle, as described in the cited research.
Drug Safety Lifecycle Assessment Workflow
Cutting-edge research into drug safety lifecycle effects requires access to specific data sources, analytical tools, and methodological frameworks.
Table 3: Essential Research Resources for Drug Lifecycle Safety Studies
| Resource / Tool | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| National Health & Clinical Registers [4] | Data Source | Provides longitudinal, population-level data on drug exposure, patient comorbidities, and clinical outcomes. | Studying safety outcomes in specific disease cohorts (e.g., RA patients on b/tsDMARDs). |
| Spontaneous Reporting Systems (e.g., FAERS) [8] | Data Source | Database of individual case safety reports (ICSRs) for signal detection and analysis of ADRs in subpopulations. | Monitoring the emergence of safety signals in older adults post-market. |
| Pharmacoepidemiological Networks (e.g., ENCePP) [9] | Methodological Framework | A network and guide providing methodological standards for non-interventional studies using RWD. | Ensuring study design and conduct meet international best practice standards. |
| WHO Global Benchmarking Tool (GBT) [10] [11] | Assessment Tool | Evaluates the maturity and functionality of a national regulatory authority's pharmacovigilance system. | Assessing the robustness of the national safety monitoring environment. |
| Indicator-Based Pharmacovigilance Assessment Tool (IPAT) [10] [11] | Assessment Tool | Assesses the function, capacity, and gaps of a national PV system across structure, process, and outcome indicators. | Mapping a country's PV system capacity to contextualize local safety data. |
| Time-to-Event (Survival) Analysis [7] [4] | Statistical Method | Models the time until the occurrence of an event (e.g., a safety warning or adverse outcome), accounting for variable follow-up. | Comparing the time to first major safety warning between different drug classes. |
The evidence confirms that a drug's market age is a critical determinant of its observed safety profile. The journey from a novel therapeutic to an established agent is characterized by an evolving understanding of its risks, shaped by real-world exposure in diverse populations and the accumulation of long-term data. While first-in-class drugs are pillars of therapeutic innovation, their initial safety profile is necessarily incomplete. The lifecycle effect underscores the indispensable role of robust, continuous post-marketing surveillance and advanced pharmacoepidemiological research. For drug development professionals and regulators, a dynamic perspective on drug safety—one that anticipates and systematically monitors its evolution over time—is essential for ultimately optimizing the benefit-risk balance of medicines for all patients.
The evolution of novel drug classes, particularly biologics and small molecules, has transformed the treatment of complex diseases. However, their fundamentally different structural and functional characteristics lead to distinct safety profiles that must be thoroughly understood by researchers, scientists, and drug development professionals. While small molecules—chemically synthesized compounds typically under 1 kilodalton—dominate the pharmaceutical market in volume, biologics—large, complex molecules produced from living organisms—represent the fastest-growing segment of drug development [12] [13]. This divergence in molecular basis creates a critical need for class-specific risk assessment frameworks. Within the context of comparative safety profiles of novel versus established drug classes, this analysis systematically examines the distinct adverse event patterns, underlying biological mechanisms, and risk mitigation strategies for these two therapeutic modalities. Understanding these class-specific risks is not merely academic but fundamental to patient safety, clinical trial design, and post-marketing surveillance systems in an increasingly complex pharmaceutical landscape.
Fundamental Differences Dictating Safety Profiles
The safety profiles of biologics and small molecules are intrinsically linked to their fundamental physicochemical properties and production methods. Small molecules are typically synthesized chemicals with molecular weights below 900 daltons, containing 20-100 atoms, which allows them to readily penetrate cell membranes and access intracellular targets [12] [13]. This accessibility comes with a trade-off: their compact size and ability to interact with multiple enzymatic systems increase the potential for off-target effects and unexpected drug-drug interactions [12]. Their chemical stability at room temperature simplifies storage but does not mitigate their potential for broad systemic interactions.
In contrast, biologics are large, complex molecules (1,000-50,000 atoms) produced through sophisticated biological manufacturing processes in living systems such as Chinese Hamster Ovary (CHO) cells or E. coli [12] [13]. Their substantial size—200-1,000 times larger than small molecules—generally restricts them to extracellular targets and prevents them from freely crossing cell membranes [12]. This size limitation naturally reduces certain off-target risks but introduces other safety considerations related to their high specificity for intended targets, which are often components of the immune system itself. The complex three-dimensional structure of biologics makes them susceptible to denaturation, requiring rigorous cold chain maintenance and specialized administration routes, typically injection or infusion [12]. The manufacturing process itself represents a key differentiator; whereas small molecule production involves reproducible chemical synthesis, biologic production requires precise control of living systems, where minor deviations can significantly impact product safety and efficacy [12].
Table 1: Fundamental Characteristics Influencing Safety Profiles
| Characteristic | Small Molecules | Biologics |
|---|---|---|
| Molecular Size | <900 daltons [12] | Typically 1,000-50,000 atoms [12] [13] |
| Production Method | Chemical synthesis [12] | Living cell systems [12] |
| Typical Administration | Oral (most) [12] [14] | Injection/Infusion [12] |
| Stability | Generally room temperature stable [12] | Typically requires refrigeration [12] |
| Target Accessibility | Intracellular and extracellular [12] | Primarily extracellular [12] |
Methodological Approaches to Safety Assessment
Systematic Review and Meta-Analysis Protocols
Robust safety assessment requires standardized methodologies that enable valid cross-class comparisons. Recent investigations into inflammatory bowel disease (IBD) treatments exemplify a rigorous approach. One comprehensive systematic review and meta-analysis examined randomized controlled trials (RCTs) published from 2000 to 2022, applying a random-effects model with logit transformation to analyze heterogeneity between studies using the I² statistic [15]. This methodology allowed for pooled estimation of adverse event (AE) and serious adverse event (SAE) incidences with 95% confidence intervals across different drug classes including TNF antagonists, anti-integrins, anti-IL agents, and JAK inhibitors [15]. The protocol included exhaustive search strategies across major databases with predefined inclusion criteria focusing on RCTs to ensure quality and comparability of safety data.
Longitudinal Cohort Design for Temporal Safety Patterns
For evaluating how safety profiles evolve post-market, nationwide register-based cohort studies provide essential real-world evidence. A Swedish study conducted from 2006 to 2022 exemplifies this approach, identifying treatment initiators of biologic/targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) alongside reference cohorts [4]. This design enabled calculation of incidence rates (IRs) and hazard ratios (HRs) using Cox regression, adjusted for patient characteristics. Crucially, researchers stratified analyses by both time since market entry of each drug class and calendar year of treatment initiation, allowing dissection of how safety profiles mature independent of changing patient populations [4]. This methodological nuance helps distinguish true safety learning from channeling bias, where newer drugs may be prescribed to higher-risk patients.
Combination Therapy Safety Assessment
As therapeutic strategies grow more complex, assessing safety of combination regimens requires specialized methodologies. An updated systematic review and meta-analysis on combining biologics and/or small molecules in refractory IBD employed an inverse variance model to calculate pooled estimates for AEs and clinical responses across 27 studies encompassing 619 patients and 631 therapeutic trials [16]. This approach enabled direct comparison of AE rates across specific drug combinations—from upadacitinib + vedolizumab (0% AEs) to natalizumab + anti-TNF (92.3% AEs)—providing crucial safety data for clinical decision-making in treatment-resistant cases [16].
Comparative Safety Data Analysis
Adverse Event Incidence Across Therapeutic Areas
Quantitative safety data reveals distinct patterns between drug classes across indications. In inflammatory bowel disease, meta-analysis shows the overall incidence of any adverse events is notably similar between classes—67.0% (95% CI, 66.2%-67.8%) for Crohn's disease and 63.6% (95% CI, 63.0%-64.3%) for ulcerative colitis [15]. However, the nature of these adverse events differs significantly. The most common AEs for biologics are infections (ranging from 21.5% to 32.6% in CD patients across different biologic classes), reflecting their immunomodulatory mechanisms [15]. For small molecule JAK inhibitors in the same population, infections remain concerning (13.7%-18.4%) but distinctive laboratory abnormalities like increased lactic dehydrogenase levels (23.1%) emerge as class-specific findings [15].
The temporal dimension of safety profiles reveals another critical distinction. Research on rheumatoid arthritis treatments shows that biologics and targeted synthetic DMARDs initiated within 2 years of market entry appear associated with higher adverse event rates (unadjusted HR = 0.74 for >5 years vs <2 years since market entry) [4]. This "newness risk" attenuates when adjusting for patient characteristics (adjusted HR = 0.93), suggesting initial channeling of newer agents to higher-risk patients partly explains this phenomenon [4].
Table 2: Comparative Adverse Event Profiles in Inflammatory Bowel Disease
| Parameter | Biologics (TNF antagonists, anti-integrins, anti-IL agents) | Small Molecules (JAK inhibitors) |
|---|---|---|
| Any AE Incidence (CD) | 67.0% (95% CI, 66.2%-67.8%) [15] | 67.0% (95% CI, 66.2%-67.8%)* [15] |
| Serious AE Incidence (CD) | 7.3% (95% CI, 6.9%-7.7%) [15] | 7.3% (95% CI, 6.9%-7.7%)* [15] |
| Most Common AE Type | Infections (21.5%-32.6%) [15] | Infections (13.7%-18.4%) + increased LDH (23.1%) [15] |
| Serious Infection Risk | Significant across classes [15] | Significant but with distinctive lab abnormalities [15] |
Note: The meta-analysis provided overall AE rates for IBD treatments collectively; JAK inhibitors contributed to these overall rates.
Combination Therapy Risk Assessment
Combination therapies present particularly complex safety considerations. Evidence from inflammatory bowel disease demonstrates that specific pairings carry dramatically different risk profiles. The highest rates of serious adverse events are observed with combinations such as upadacitinib + ustekinumab (23% SAEs), while other combinations like natalizumab + anti-TNF or tofacitinib + ustekinumab show no serious adverse events in studied populations [16]. This extreme variability underscores that combination safety is not class-wide but highly dependent on specific mechanistic interactions.
Mechanistic Basis for Observed Safety Differences
Immunogenicity and Off-Target Effects
The fundamental mechanistic differences between biologics and small molecules create distinct safety challenges. Biologics, particularly monoclonal antibodies, achieve their high specificity through structural complementarity with target proteins, but their biological origin makes them inherently immunogenic [12]. This can lead to the development of anti-drug antibodies that not only reduce efficacy but may cause complex immune-mediated adverse events, including cytokine release syndromes and anaphylactoid reactions [12]. The diagram below illustrates the distinct immune activation pathways between biologics and small molecules:
In contrast, small molecules most commonly cause adverse effects through off-target interactions with enzymes, receptors, and transporters unrelated to their primary therapeutic targets [12]. Their metabolism through systems like cytochrome P450 creates potential for drug-drug interactions and metabolite-mediated toxicities that are less common with biologics [12]. Additionally, their ability to penetrate tissues broadly—including crossing the blood-brain barrier—while therapeutically advantageous for CNS targets, increases the risk of organ-specific toxicities in sensitive tissues [12] [14].
Target-Specific versus System-Wide Effects
The precision of biologics creates a paradoxical safety profile: while causing fewer traditionally defined "off-target" effects, their highly specific action on immune targets can result in profound immunosuppression with associated infection risks [15] [16]. Small molecules, particularly those in classes like JAK inhibitors, may exhibit more systemic effects due to their broader impact on intracellular signaling networks, leading to laboratory abnormalities such as increased lactic dehydrogenase and lipid profile changes [15]. The workflow below outlines the distinct safety assessment priorities for each class:
The Research Toolkit: Essential Reagents and Methodologies
Core Reagent Solutions for Safety Assessment
Table 3: Essential Research Reagents for Safety Assessment
| Reagent/Method | Primary Function | Class Application |
|---|---|---|
| Anti-Drug Antibody (ADA) Assays | Detect and quantify immunogenic response to biologic therapeutics [12] | Primarily Biologics |
| Cytokine Panels | Measure inflammatory cytokine release indicative of cytokine storm [12] | Primarily Biologics |
| Cytochrome P450 Screening | Identify metabolic interactions and potential drug-drug interactions [12] | Primarily Small Molecules |
| hERG Channel Assays | Assess potential for QT interval prolongation and cardiac arrhythmia [13] | Primarily Small Molecules |
| Liver Microsome Systems | Evaluate metabolic stability and metabolite-mediated toxicity [13] | Primarily Small Molecules |
| Fc Receptor Binding Assays | Characterize immune effector functions of monoclonal antibodies [12] | Primarily Biologics |
| Alliin | Alliin (S-allyl-L-cysteine sulfoxide) | High-purity Alliin, the key biosynthetic precursor to allicin in garlic. Explore its role in antimicrobial and cancer research. For Research Use Only. Not for human consumption. |
| Spiramycin III | Spiramycin III, MF:C46H78N2O15, MW:899.1 g/mol | Chemical Reagent |
The comparative analysis of safety patterns between biologics and small molecules reveals that each class presents distinctive risk profiles rooted in their fundamental characteristics. Biologics demonstrate target-specific risks, primarily infection vulnerability and immunogenic reactions, while small molecules exhibit systemic interaction risks, including off-target effects, metabolic interactions, and organ toxicities. These differences necessitate class-specific safety assessment protocols throughout the drug development lifecycle—from preclinical screening through post-marketing surveillance. For researchers and drug development professionals, this evidence underscores that safety optimization requires embracing these inherent differences rather than applying one-size-fits-all approaches. Future directions should include developing more sophisticated immunogenicity prediction platforms for biologics and advanced metabolite toxicity forecasting for small molecules. As combination therapies grow more common, understanding the interactive safety profiles of these two classes will become increasingly crucial for developing effective treatments with manageable risk-benefit ratios across therapeutic areas.
The rapid pace of pharmaceutical innovation brings transformative treatments to patients, yet it also presents the critical challenge of comprehensively characterizing safety profiles before widespread clinical use. For researchers, scientists, and drug development professionals, understanding the evolving safety themes among recently approved novel therapeutics is paramount for designing safer drugs, optimizing clinical trial safety monitoring, and implementing effective pharmacovigilance strategies. This analysis examines therapeutic agents approved by the FDA in 2024-2025, focusing on comparative safety profiles across drug classes, methodological advances in safety signal detection, and the emergence of class-specific adverse event patterns. By synthesizing data from clinical trials, real-world evidence, and regulatory documents, this guide provides a framework for evaluating safety in the context of both established and emerging drug classes, offering insights that can inform future drug development and post-marketing surveillance protocols.
Comparative Safety Profiles of Recent Novel Therapeutics
The safety assessment of novel therapeutics approved between 2024 and 2025 reveals distinct patterns across therapeutic classes, with important implications for both clinical development and post-marketing surveillance strategies.
Oncology and Hematology Agents
Oncology drugs continue to dominate the novel therapeutic landscape, with several targeted therapies demonstrating improved safety profiles compared to traditional cytotoxic chemotherapy, while still presenting unique safety challenges.
Table 1: Safety Profile Comparison of Select 2024-2025 Oncology/Hematology Agents
| Drug Name (Brand) | Approval Date | Mechanism of Action | Primary Indication | Notable Safety Findings | Comparison to Established Alternatives |
|---|---|---|---|---|---|
| Telisotuzumab Vedotin (Emrelis) [17] | May 14, 2025 | c-Met-directed antibody-drug conjugate | MET-overexpressed non-squamous NSCLC | Manufacturer includes special handling information; classified as hazardous [18] | Novel mechanism; requires specialized safety protocols compared to standard NSCLC therapies |
| Datopotamab Deruxtecan (Datroway) [17] | January 17, 2025 | Trop-2 directed antibody-drug conjugate | HR-positive, HER2-negative breast cancer | Manufacturer includes special handling information; classified as hazardous [18] | Different safety profile compared to other ADC platforms; requires specific monitoring |
| Ziftomenib (Komzifti) [17] | November 13, 2025 | Menin inhibitor | R/R NPM1-mutant AML | Complete response rate demonstrated with specific hematological recovery profile [19] | First-in-class mechanism; safety profile distinct from conventional AML therapies |
| Revuforj [19] | November 15, 2024 | Menin inhibitor | R/R acute leukemia | CRh rate of 21.2%; bleeding, nausea, musculoskeletal pain, infection reported [19] | Novel targeted approach with different adverse event profile compared to standard chemotherapy |
The identification of several recently approved drugs on the NIOSH List of Hazardous Drugs in Healthcare Settings, 2024 underscores the importance of specialized handling protocols for novel targeted therapies, particularly antibody-drug conjugates [18]. These requirements present unique safety considerations not only for patients but also for healthcare personnel involved in drug preparation and administration.
Cardiovascular and Metabolic Therapeutics
Recent approvals in cardiovascular and metabolic diseases show a trend toward targeted mechanisms with generally favorable safety profiles, though with some novel adverse event patterns.
Table 2: Safety Profile Comparison of Select 2024-2025 Cardiovascular/Metabolic Agents
| Drug Name (Brand) | Approval Date | Mechanism of Action | Primary Indication | Notable Safety Findings | Comparison to Established Alternatives |
|---|---|---|---|---|---|
| Plozasiran (Redemplo) [17] | November 18, 2025 | RNAi therapeutic | Familial chylomicronemia syndrome | Novel mechanism with specific monitoring requirements | Distinct from traditional triglyceride-lowering approaches; requires long-term safety assessment |
| Inclisiran [20] | Approved pre-2024; recent safety analysis | PCSK9 synthesis inhibitor | Hypercholesterolemia | Real-world evidence shows higher gastrointestinal disorders and infections vs. other PCSK9 inhibitors; potential advantages in eye, skin, and administration site disorders [20] | Different safety profile compared to monoclonal antibody PCSK9 inhibitors despite similar indication |
| Atrasentan (Vanrafia) [17] | April 2, 2025 | Endothelin A receptor antagonist | IgA nephropathy | Proteinuria reduction with specific monitoring requirements | Novel approach to nephropathy management with distinct safety considerations |
| Tryvio [19] | March 19, 2024 | Endothelin A/B receptor antagonist | Hypertension | Liver issues, fetal harm, reduced sperm counts in males [19] | Dual endothelin receptor blockade with different safety profile compared to selective antagonists |
The comparative analysis of inclisiran safety profiles using FDA Adverse Event Reporting System (FAERS) data demonstrates how real-world evidence can reveal important safety differentiations even within the same drug class [20]. This highlights the value of post-marketing surveillance in characterizing the safety profiles of novel therapeutic mechanisms.
Neurological, Ophthalmic, and Rare Disease Therapeutics
Recent approvals for neurological, ophthalmic, and rare diseases demonstrate the challenge of balancing significant efficacy with manageable safety profiles in often vulnerable patient populations.
Table 3: Safety Profile Comparison of Select 2024-2025 Neurological/Ophthalmic/Rare Disease Agents
| Drug Name (Brand) | Approval Date | Mechanism of Action | Primary Indication | Notable Safety Findings | Comparison to Established Alternatives |
|---|---|---|---|---|---|
| Acoltremon (Tryptyr) [17] [21] | May 28, 2025 | TRPM8 agonist | Dry eye disease | Instillation-site pain (50% of patients) but low discontinuation rate (<1%) [21] | First-in-class mechanism with localized rather than systemic safety concerns |
| Suzetrigine (Journavx) [17] [21] | January 30, 2025 | NaV1.8 channel blocker | Moderate-to-severe acute pain | Itching, rash, muscle spasms, increased CPK, decreased eGFR; no addiction or dependence shown [21] | Non-opioid analgesic with fundamentally different safety profile compared to opioids and NSAIDs |
| Dordaviprone (Modeyso) [17] | August 6, 2025 | Not specified in sources | Diffuse midline glioma | Safety profile under characterization in post-approval setting | Novel approach for a challenging malignancy with limited treatment options |
| Kygevvi [17] | November 3, 2025 | Combination product (doxecitine and doxribtimine) | Thymidine kinase 2 deficiency | Safety profile in pediatric population requiring characterization | Ultra-rare disease therapy with limited comparative safety data |
The approval of suzetrigine as a first-in-class, non-opioid analgesic with no evidence of addiction or dependence in human or animal studies represents a significant advancement in pain management safety, addressing a critical need for effective analgesics without opioid-related risks [21].
Methodological Advances in Safety Assessment
The evaluation of novel therapeutic safety has evolved significantly, with important innovations in both pre-approval clinical trial design and post-approval surveillance methodologies.
Selective Safety Data Collection in Clinical Trials
The FDA has recently emphasized Selective Safety Data Collection (SSDC) as a strategic approach to optimize clinical trial efficiency while maintaining rigorous safety assessment [22]. This methodology involves:
- Prospective Planning: Deliberate curtailment of non-essential safety data collection in studies where the drug's safety profile is already well-characterized
- Focused Monitoring: Maintaining comprehensive collection for serious adverse events, adverse events leading to discontinuation, and adverse events of special interest, while reducing burden for known, non-serious adverse events
- Resource Optimization: Decreasing participant, investigator, sponsor, and regulatory burden to facilitate more efficient clinical research
The International Council on Harmonisation finalized the E19 guideline on selective safety data collection nearly three years ago, yet industry adoption remains limited due to concerns about regulatory requirements across different jurisdictions and conservative corporate approaches to safety data [22].
Real-World Evidence for Comparative Safety Profiling
Recent analyses demonstrate the growing importance of real-world evidence in characterizing the safety profiles of novel therapeutics compared to established alternatives:
Diagram: Real-World Evidence Safety Assessment Workflow
The comparative analysis of inclisiran using FAERS data exemplifies this approach, identifying 136 safety signals through disproportionality analysis (Reporting Odds Ratio method) and comparing them with other PCSK9 inhibitors at the System Organ Class, High Level Group Term, and Preferred Term levels [20]. This methodology revealed that inclisiran had a greater number of adverse drug events in 'Gastrointestinal disorders' and 'Infections and infestations' compared to other PCSK9 inhibitors, while demonstrating potential advantages in 'Eye disorders,' 'Skin and subcutaneous tissue disorders' and 'General disorders and administration site conditions' [20].
The "Channelling" Effect in New Drug Safety Assessment
A nationwide register-based cohort study conducted in Sweden from 2006 to 2022 revealed important methodological considerations for evaluating the safety of newly marketed therapeutics:
Diagram: Temporal Dynamics of New Drug Safety Assessment
This research found that b/tsDMARD treatments initiated >5 years since market entry were associated with significantly lower adverse event rates compared to those initiated <2 years since market entry (unadjusted HR = 0.74; 95% CI = 0.67-0.81) [4]. This association was substantially attenuated after adjusting for patient characteristics (adjusted HR = 0.93; 95% CI = 0.84-1.03), suggesting that modest channelling of newer drugs to higher-risk patients makes their safety profile appear worse when new on the market [4].
Emerging Safety Themes and Patterns
Analysis of recent drug approvals reveals several consistent themes in the safety profiles of novel therapeutics across different drug classes and therapeutic areas.
Class-Specific Adverse Event Patterns
Novel Mechanism-Specific Toxicity: Targeted therapies continue to demonstrate unique adverse event profiles directly related to their mechanisms of action, such as the specific safety considerations with menin inhibitors in leukemia treatment [19].
Platform Technology Considerations: The emergence of RNA-based therapeutics, including small interfering RNA (siRNA) agents like plozasiran, presents novel safety considerations distinct from traditional small molecules or biologic approaches [17].
Special Handling Requirements: The classification of several recently approved agents, particularly antibody-drug conjugates, as hazardous drugs requiring special handling underscores the importance of considering occupational safety alongside patient safety [18].
Temporal Dynamics in Safety Profile Characterization
The Swedish registry study highlights how safety profiles evolve over time as drugs transition from limited clinical trial populations to broader real-world use [4]. This research demonstrated that adjusted adverse event rates for b/tsDMARDs declined significantly over the study period (adjusted HR = 0.74 for 2016-2021 vs. 2006-2010), despite constant rates in the background population, suggesting improvements in patient selection, monitoring, and management of comorbidities [4].
Risk Mitigation and Individualization Strategies
Recent approvals increasingly incorporate targeted risk mitigation strategies, including:
Biomarker-Driven Patient Selection: Several recently approved oncology agents (e.g., telisotuzumab vedotin, datopotamab deruxtecan) require specific biomarker testing, which may help optimize the benefit-risk ratio for individual patients [17].
Special Population Considerations: The varying safety profiles observed in different patient subgroups (e.g., the age-specific cohorts in the mRNA-1083 trials) highlight the importance of individualized safety assessment [23].
Experimental Protocols for Safety Assessment
Real-World Evidence Safety Signal Detection Protocol
The following protocol, adapted from recent comparative safety studies, provides a framework for systematic post-marketing safety assessment:
Step 1: Data Source Identification
- Utilize the FDA Adverse Event Reporting System (FAERS) or similar national pharmacovigilance databases
- Collect reports from a defined time period (e.g., January 2021 to September 2023) [20]
- Include appropriate comparator drugs with similar indications or mechanisms
Step 2: Signal Detection Methodology
- Employ disproportionality analysis using Reporting Odds Ratio (ROR) method
- Calculate ROR with 95% confidence intervals
- Define significant signals using predetermined thresholds (e.g., lower bound of 95% CI >1, minimum number of cases)
Step 3: Stratified Analysis
- Analyze safety signals at multiple levels: System Organ Class (SOC), High Level Group Term (HLGT), and Preferred Term (PT) [20]
- Compare novel therapeutic against multiple appropriate comparators
- Conduct sensitivity analyses to assess robustness of findings
Step 4: Clinical Interpretation
- Evaluate identified signals in context of known mechanism of action
- Assess potential confounders and channeling biases
- Consider clinical relevance and potential impact on risk-benefit assessment
Selective Safety Data Collection Implementation Protocol
Based on FDA C3TI White Paper and ICH E19 Guideline [22]:
Step 1: Eligibility Assessment
- Determine if the investigational drug has an adequately characterized safety profile from previous studies (typically ≥1200 subjects)
- Assess whether the study population is similar to previously studied populations
- Identify known adverse reactions with well-characterized incidence rates
Step 2: Protocol Development
- Prospectively define which safety data will be collected comprehensively:
- Serious adverse events
- Adverse events leading to discontinuation
- Adverse events of special interest
- Specific laboratory parameters of concern
- Identify data that may be collected in a targeted manner:
- Non-serious adverse events with known incidence
- Routine laboratory parameters with established profiles
- Non-clinically significant findings
Step 3: Implementation and Monitoring
- Develop targeted data collection forms
- Train investigative sites on selective collection approach
- Implement quality control measures to ensure critical safety data integrity
Step 4: Regulatory Alignment
- Engage with regulatory authorities through meeting requests or protocol review
- Address cross-regional differences in safety data expectations
- Document justification for selective collection approach
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Safety Assessment Studies
| Reagent/Solution | Function in Safety Assessment | Application Context |
|---|---|---|
| FAERS Database [20] | Spontaneous adverse event reporting data for signal detection | Post-marketing safety surveillance; comparative safety studies |
| ROR Analysis Scripts | Statistical analysis for disproportionality in adverse event reporting | Quantitative signal detection in pharmacovigilance databases |
| Electronic Health Record Data Models | Structured real-world data for longitudinal safety assessment | Observational safety studies; comparative effectiveness research |
| ICH E19 Guideline Framework [22] | Protocol template for selective safety data collection | Clinical trial design optimization |
| USP Drug Classification System [24] | Standardized drug categorization for comparative analysis | Formulary review; drug class safety comparisons |
| Biomarker Assay Kits | Patient selection and safety monitoring | Targeted therapy safety assessment; personalized safety monitoring |
| Lipid Nanoparticle Formulations [23] | Delivery system for nucleic acid-based therapeutics | Platform technology safety evaluation |
| N-Caffeoyldopamine | N-Caffeoyldopamine, CAS:105955-00-8, MF:C17H17NO5, MW:315.32 g/mol | Chemical Reagent |
| Sophocarpine monohydrate | Sophocarpine monohydrate, MF:C15H24N2O2, MW:264.36 g/mol | Chemical Reagent |
The comparative safety assessment of novel therapeutics approved in 2024-2025 reveals several critical themes for drug development professionals. First, real-world evidence methodologies have become increasingly sophisticated, enabling more nuanced comparative safety assessments between novel and established therapies [20]. Second, the temporal evolution of safety profiles must be carefully considered, as "channelling" effects can make new drugs appear less safe initially than they may prove to be with broader clinical experience [4]. Third, innovative clinical trial approaches such as selective safety data collection offer opportunities to optimize research efficiency while maintaining rigorous safety assessment [22]. Finally, class-specific and mechanism-based safety patterns continue to emerge, necessitating therapeutic area-specific safety monitoring strategies. As the pharmaceutical development landscape continues to evolve with increasingly novel mechanisms and platform technologies, these safety assessment principles and methodologies will remain essential for characterizing the benefit-risk profile of new therapeutics and ensuring their safe and effective use in appropriate patient populations.
From Trial to Real-World: Methodologies for Robust Safety Surveillance
The journey of a drug from the laboratory to the patient involves a continuous and evolving safety assessment framework that stretches from preclinical development through post-marketing surveillance. This comprehensive lifecycle approach is critical for protecting public health, as the safety profile of a pharmaceutical product is not fully characterized at the initial approval stage. Clinical trials, while rigorous, have inherent limitations including restricted patient populations, limited duration, and controlled conditions that do not fully represent real-world usage [25]. The controlled environment of pre-marketing studies typically involves only several hundred to several thousand carefully selected participants, making it difficult to detect rare adverse events or long-term safety issues that may only emerge when the drug is used by millions of diverse patients in clinical practice [25].
The transition from a drug's initial approval to its widespread use represents a crucial phase where safety monitoring intensifies rather than diminishes. Post-marketing surveillance serves as the safety net that identifies previously unknown adverse effects, confirms known risks in broader populations, and provides evidence for regulatory decision-making throughout a product's entire lifecycle [26]. This systematic monitoring has evolved from reactive reporting systems to proactive safety monitoring platforms that integrate diverse data sources, leverage advanced analytics, and respond to safety signals with unprecedented speed and accuracy [26]. As we advance through 2025, global regulatory authorities increasingly demand comprehensive patient safety monitoring throughout a product's entire lifecycle, with sophisticated frameworks that have been fundamentally reshaped by technological innovation and an growing emphasis on real-world evidence generation [26] [27].
Methodological Framework: Surveillance Approaches Across the Lifecycle
Preclinical to Pre-marketing Safety Assessment
The safety assessment of pharmaceutical products begins long before human exposure, starting with rigorous preclinical evaluation. The methodological foundation established during these early stages creates the baseline against which all subsequent safety findings are measured. Preclinical studies utilize in vitro and in vivo models to identify potential toxicities, establish initial safety parameters, and determine first-in-human dosing levels. While these studies provide essential preliminary safety data, their predictive value for human outcomes is limited by species-specific differences and the artificial experimental conditions.
The transition to human studies marks a critical escalation in safety assessment, with clinical trials proceeding through phased investigations that progressively expand the patient population and exposure duration. Phase I trials focus primarily on safety and tolerability in small numbers of healthy volunteers (20-100), establishing the preliminary safety profile and pharmacokinetic parameters [25]. Phase II trials expand to include larger groups of patients (100-300) and begin to evaluate both efficacy and further refine the safety assessment, while Phase III trials involve even larger populations (1,000-3,000 or more) to confirm efficacy and monitor less common adverse events [25]. Despite this progressive expansion, the total pre-marketing exposure remains insufficient to detect rare adverse events occurring at frequencies below approximately 1 in 1,000 recipients [25].
Table 1: Key Limitations of Pre-marketing Clinical Trials in Safety Assessment
| Limitation Factor | Clinical Trial Constraints | Implications for Safety Profile |
|---|---|---|
| Population Size | Typically several hundred to several thousand participants [25] | Inability to detect rare adverse events (<1 in 1,000) |
| Population Diversity | Carefully selected participants with strict inclusion/exclusion criteria [25] | Limited data in elderly, pregnant women, patients with comorbidities |
| Duration | Months to a few years [25] | Inability to identify long-term or latent adverse effects |
| Concomitant Medications | Often restricted or controlled | Limited assessment of complex drug-drug interactions |
| Real-world Usage | Controlled administration and adherence monitoring | Poor prediction of actual use patterns, including off-label use |
Post-Marketing Surveillance Methodologies
Upon regulatory approval and market entry, drugs enter the most extensive testing ground—real-world clinical practice—where comprehensive post-marketing surveillance systems are activated. These systems employ complementary methodologies to monitor drug safety in diverse patient populations and usage scenarios.
Passive surveillance, primarily through spontaneous reporting systems, represents the foundational approach to post-marketing safety monitoring. These systems collect voluntary reports of suspected adverse drug reactions from healthcare professionals, patients, and manufacturers through programs such as the FDA's MedWatch (feeding into the FDA Adverse Event Reporting System - FAERS) and the UK's Yellow Card Scheme [25]. While spontaneous reporting provides broad population coverage and potential for early signal detection, it suffers from significant underreporting (estimated at 1-10% of all adverse events) and various reporting biases that limit its reliability for quantifying risks [25].
Active surveillance methodologies proactively seek safety information through systematic data collection approaches. These include:
- Patient registries that offer longitudinal follow-up of specific patient populations and provide detailed information about disease progression, treatment outcomes, and safety experiences [26]
- Electronic health records (EHRs) that contain comprehensive clinical information from routine healthcare delivery, enabling large-scale safety monitoring and real-world effectiveness studies [26]
- Claims databases that offer population-level exposure and outcome data with extensive coverage and long-term follow-up capabilities [26]
- Digital health technologies including wearable devices, mobile applications, and remote monitoring systems that generate continuous streams of health data [26]
Table 2: Comparison of Primary Post-Marketing Surveillance Data Sources
| Data Source | Key Strengths | Principal Limitations |
|---|---|---|
| Spontaneous Reporting Systems | Early signal detection, global coverage, detailed case narratives [26] | Underreporting, reporting bias, limited denominator data [26] |
| Electronic Health Records (EHRs) | Comprehensive clinical data, large populations, real-world context [26] | Data quality variability, limited standardization, privacy concerns [26] |
| Claims Databases | Population coverage, long-term follow-up, health economics data [26] | Limited clinical detail, coding accuracy, administrative focus [26] |
| Patient Registries | Longitudinal follow-up, detailed clinical data, specific populations [26] | Limited generalizability, resource intensive, potential selection bias [26] |
| Digital Health Technologies | Continuous monitoring, objective measures, patient engagement [26] | Data validation challenges, technology barriers, privacy concerns [26] |
The following diagram illustrates the integrated safety surveillance workflow throughout the drug development lifecycle:
Technological Advancements Reshaping Safety Surveillance
Artificial Intelligence and Machine Learning Applications
The integration of artificial intelligence (AI) technologies is revolutionizing safety surveillance capabilities across the drug development lifecycle. Machine learning algorithms, particularly natural language processing (NLP) techniques, have dramatically enhanced the ability to extract and analyze safety information from previously inaccessible unstructured data sources, including clinical notes, social media, and scientific literature [5]. The evolution of AI applications in pharmacovigilance has progressed through three distinct phases: early applications focused on enhancing signal detection in spontaneous reporting systems; expansion into unstructured data analysis using NLP; and current advanced machine learning approaches that integrate diverse data sources to capture complex relationships [5].
The performance of these AI methodologies has been quantitatively demonstrated across multiple data sources. As shown in Table 3, AI approaches achieve high classification accuracy for adverse drug reaction detection, with F-scores ranging from 0.66 to 0.97 and area under the curve (AUC) metrics from 0.76 to 0.99 across different data types and analytical challenges [5]. These capabilities enable more sophisticated safety monitoring and signal detection than ever before possible, with systems that can analyze patterns across multiple data sources simultaneously to detect subtle associations that traditional methods might miss [26].
Table 3: Performance Metrics of AI Methods for Adverse Drug Reaction Detection Across Data Sources
| Data Source | AI Method | Sample Size | Performance Metric | Reference |
|---|---|---|---|---|
| Social Media (Twitter) | Conditional Random Fields | 1,784 tweets | F-score: 0.72 | [5] |
| Social Media (DailyStrength) | Conditional Random Fields | 6,279 reviews | F-score: 0.82 | [5] |
| EHR Clinical Notes | Bi-LSTM with Attention Mechanism | 1,089 notes | F-score: 0.66 | [5] |
| FAERS Database | Multi-task Deep Learning Framework | 141,752 drug-ADR interactions | AUC: 0.96 | [5] |
| Open TG-GATEs & FAERS (Duodenal Ulcer) | Deep Neural Networks | 300 drug-ADR associations | AUC: 0.94-0.99 | [5] |
| Korea National Spontaneous Reporting Database (Nivolumab) | Gradient Boosting Machine | 136 suspected AEs | AUC: 0.95 | [5] |
Real-World Evidence and Data Linkage Technologies
The growing emphasis on real-world evidence (RWE) has transformed post-marketing surveillance from reactive reporting systems to proactive safety monitoring platforms. Regulatory frameworks such as the FDA's Real-World Evidence Program, established following the 21st Century Cures Act, have created pathways for incorporating RWE into regulatory decision-making for both safety and effectiveness assessments [27]. The European Medicines Agency has similarly advanced its capabilities through the Data Analysis and Real World Interrogation Network (DARWIN EU), which was fully operationalized in 2024 [27].
Privacy-preserving record linkage (PPRL) technologies, including tokenization methods, have enabled the secure linking of disparate datasets while maintaining patient confidentiality [27]. These approaches allow researchers to connect pre-market clinical trial data with post-market real-world data at the individual level, creating comprehensive longitudinal safety profiles that bridge the artificial divide between pre-approval and post-approval monitoring. This technological advancement supports more continuous safety assessment throughout the product lifecycle and addresses the fundamental limitation of fragmented safety data across different healthcare settings and time periods [27].
Comparative Analysis: Novel versus Established Drug Classes
Quantitative Safety Assessment Across Drug Lifecycle Stages
The comparative safety profiles of novel versus established drug classes reveal important patterns in how safety understanding evolves throughout a product's lifecycle. A recent nationwide register-based cohort study conducted in Sweden from 2006 to 2022 examined safety outcomes in patients with rheumatoid arthritis initiating biologic/targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) [4]. The research analyzed 33,550 treatment initiations alongside reference cohorts, with the primary outcome being the first occurrence of major adverse cardiovascular events, venous thromboembolism, cancer, or serious infection [4].
The findings demonstrated that b/tsDMARD treatments initiated more than 5 years since market entry of that class were associated with significantly lower outcome rates compared to those initiated within 2 years of market entry (unadjusted Hazard Ratio [HR] = 0.74; 95% CI = 0.67-0.81) [4]. This association was substantially attenuated after adjusting for patient characteristics (adjusted HR = 0.93; 95% CI = 0.84-1.03), suggesting that initial safety signals for newer drugs may be influenced by "modest channelling" of higher-risk patients to newer therapeutic options [4]. This phenomenon makes the safety profile of b/tsDMARDs appear worse when new on the market, highlighting the importance of accounting for prescribing patterns and patient selection biases when evaluating early post-marketing safety data [4].
The following diagram illustrates the relationship between time since market entry and observed safety outcomes:
Case Studies: Novel Therapeutic Mechanisms and Safety Learning Curves
The comparative safety evolution is further illustrated by examining specific therapeutic classes with novel mechanisms of action. In acute myeloid leukemia (AML), menin inhibitors have demonstrated promising safety and efficacy profiles in clinical development for relapsed/refractory AML, particularly for patients with NPM1-mutated disease affecting approximately 35% of AML patients [3]. The consistent clinical benefit observed across different compounds in this class suggests the menin pathway represents a genuinely important therapeutic target with a manageable safety profile [3].
In contrast, CD47-targeted therapies for AML showed promising preclinical results but failed to translate into meaningful clinical benefits due to significant toxicity issues, particularly severe anemia, leading to the discontinuation of multiple development programs [3]. This experience highlights how novel mechanisms may present unexpected safety challenges that only become apparent in clinical testing, emphasizing the critical importance of rigorous clinical evaluation even for promising laboratory results.
For novel drug modalities including gene therapies, antisense oligonucleotides, and RNA interference technologies, the safety surveillance framework must adapt to address unique safety considerations. Gene therapies such as RGX-121 for Mucopolysaccharidosis type II (Hunter syndrome) represent one-time interventions with potential long-term safety implications that require extended monitoring periods [28]. Similarly, novel RNA-targeted therapies including donidalorsen (an antisense oligonucleotide for hereditary angioedema) and plozasiran (an RNA interference therapeutic for severe hypertriglyceridemia) introduce new mechanism-specific safety considerations that must be carefully monitored throughout their market life [28].
Regulatory Frameworks and Future Directions
Evolving Global Regulatory Expectations
Regulatory expectations for safety surveillance have significantly strengthened globally, with authorities implementing new requirements and enforcement mechanisms that directly impact pharmaceutical operations. The FDA's requirements center on the FDA Adverse Event Reporting System (FAERS) and Risk Evaluation and Mitigation Strategies (REMS) programs, with recent enhancements to the Sentinel Initiative that leverage real-world data for active surveillance and safety signal detection [26]. The European Medicines Agency has similarly enhanced EudraVigilance capabilities to support advanced signal detection and real-world evidence generation, enabling more sophisticated analysis of post-marketing safety data [26].
The International Council for Harmonisation (ICH) standards provide harmonized guidelines for post-marketing surveillance activities, including case report formatting, periodic safety reporting, and signal detection methodologies [26]. These guidelines continue to evolve to address emerging data sources and analytical capabilities, with recent updates focusing on digital health technologies, patient-reported outcomes, and artificial intelligence applications in post-marketing surveillance [26]. Additionally, regulatory authorities maintain post-marketing requirement (PMR) and post-marketing commitment (PMC) authorities that allow them to require manufacturers to conduct additional safety studies after approval to assess possible serious risks [29].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagent Solutions for Advanced Safety Surveillance
| Tool Category | Specific Technologies | Research Application |
|---|---|---|
| AI-Powered Signal Detection | Natural Language Processing (NLP) algorithms, Deep Neural Networks, Knowledge Graphs [5] | Extraction of adverse event information from unstructured clinical notes, social media, and scientific literature |
| Real-World Data Linkage | Privacy-Preserving Record Linkage (PPRL) platforms, Tokenization solutions [27] | Secure linking of disparate datasets (EHRs, claims, registries) while maintaining patient confidentiality |
| Active Surveillance Systems | Sentinel Initiative infrastructure, DARWIN EU network [26] [27] | Large-scale active monitoring of medical product safety using real-world healthcare data |
| Biomarker Assessment | Genomic sequencing panels, Proteomic profiling platforms, Immunoassay systems | Identification and validation of safety biomarkers for novel drug classes |
| Digital Health Technologies | Wearable sensors, Mobile health applications, Remote patient monitoring platforms [26] | Continuous, real-world safety monitoring outside traditional clinical settings |
| Asperglaucide | Asperglaucide, MF:C27H28N2O4, MW:444.5 g/mol | Chemical Reagent |
| ACHP | ACHP, CAS:1844858-31-6, MF:C21H24N4O2, MW:364.4 g/mol | Chemical Reagent |
Future Outlook: Integrated Safety Surveillance Beyond 2025
The future evolution of safety surveillance will likely focus on more integrated, patient-centric approaches that leverage emerging technologies and data sources. Patient-centric approaches will increasingly prioritize patient experiences and outcomes while engaging patients as active participants in safety monitoring through digital health technologies and patient-reported outcome measures [26]. Continuous safety learning systems will enable real-time adaptation of safety knowledge and risk management strategies based on emerging evidence, creating more dynamic and responsive safety surveillance frameworks [26].
The growing application of artificial intelligence across the safety surveillance landscape will further transform pharmacovigilance practices, though significant challenges remain in ensuring these technologies function as intended in real-world implementation [5]. Key considerations include ensuring AI's consistent and transparent performance, reducing multiple sources of bias, addressing interpretability issues, and managing the unintended consequences of deploying multiple interacting AI systems in complex healthcare environments [5]. As these technological and methodological advances mature, the historical distinction between pre-marketing and post-marketing safety assessment will continue to blur, replaced by more continuous, integrated safety surveillance frameworks that span the entire therapeutic lifecycle.
The evolving framework for safety surveillance from preclinical to post-marketing represents a critical continuum in therapeutic development and patient protection. The comparative analysis of novel versus established drug classes demonstrates how safety profiles mature and become better characterized throughout a product's lifecycle, with important implications for clinical practice and regulatory decision-making. The integration of advanced technologies including artificial intelligence, real-world evidence generation, and privacy-preserving data linkage methods is fundamentally transforming safety surveillance capabilities, enabling more proactive, comprehensive, and responsive monitoring approaches.
As novel therapeutic modalities continue to emerge—from gene therapies to RNA-targeted treatments—the safety surveillance framework must similarly evolve to address new challenges and opportunities. The future of drug safety monitoring lies in increasingly integrated, patient-centric, and data-driven approaches that leverage continuous learning systems to protect patient health while enabling appropriate access to beneficial therapeutics. For researchers, scientists, and drug development professionals, understanding this evolving landscape is essential for designing robust safety surveillance strategies that meet both scientific standards and regulatory expectations across the entire therapeutic lifecycle.
Real-World Evidence (RWE) is clinical evidence regarding the usage, benefits, and risks of medical products derived from the analysis of Real-World Data (RWD)—data collected outside the controlled environment of traditional randomized controlled trials (RCTs) [30]. In the critical field of comparative drug safety, RWE provides indispensable insights into how novel and established drug classes perform across diverse patient populations in routine clinical practice, filling evidence gaps that RCTs alone cannot address [31] [32].
The fundamental value of RWE in safety assessment lies in its ability to capture clinical outcomes across broad, heterogeneous populations that are often underrepresented in clinical trials, including the elderly, those with multiple comorbidities, racial and ethnic minorities, and patients from varying socioeconomic backgrounds [33] [34]. This capability makes RWE particularly vital for evaluating comparative safety profiles across different demographic groups, thereby addressing pressing needs in health equity and precision medicine [31] [33].
The foundation of robust RWE lies in the selection of appropriate, high-quality data sources that capture the experiences of diverse patient populations. These sources vary in their strengths, limitations, and suitability for addressing specific safety research questions.
Table 1: Key Real-World Data Sources for Comparative Safety Studies
| Data Source | Primary Strengths | Key Limitations | Best Use Cases for Safety |
|---|---|---|---|
| Electronic Health Records (EHRs) | Rich clinical detail (lab values, physician notes, diagnoses); captures diverse care settings [31] [30] | Unstructured data requires NLP; potential missing data outside system [30] [32] | Identifying rare adverse events; safety in patients with complex comorbidities [35] |
| Claims & Billing Data | Large populations; longitudinal tracking of diagnoses, procedures, pharmacy fills [31] [32] | Limited clinical granularity; coding inaccuracies [32] | Drug utilization patterns; hypothesis-generating safety signal detection [36] |
| Disease & Product Registries | Detailed, curated data on specific conditions/therapies; often include patient-reported outcomes [31] [32] | Potential selection bias (often academic centers); limited generalizability [32] | Long-term safety of novel drug classes in specific diseases [35] |
| Patient-Generated Health Data (PGHD) | Direct patient perspective on symptoms, QoL, behaviors; real-time data from wearables [31] [32] | Variable data quality; privacy concerns; requires validation [32] | Monitoring functional outcomes & tolerability in daily life [36] |
Each data source contributes uniquely to understanding drug safety. EHRs from large healthcare systems like PEDSnet provided the necessary clinical detail and pediatric population for a safety study supporting a new dosing regimen for Vimpat (lacosamide) [35]. In contrast, the FDA Sentinel System—a distributed network of claims and administrative data—enabled a rapid assessment of uterine bleeding risk with oral anticoagulants across a massive population, leading to a class-wide label change [35].
Methodological Framework: RWE Study Designs for Comparative Safety
Selecting an appropriate study design is paramount for generating reliable evidence about the comparative safety of drugs. The choice depends on the research question, data availability, and specific sources of bias that must be addressed.
Core Observational Study Designs
Retrospective Cohort Studies: This design identifies a group of patients exposed to a drug and follows them forward in time (retrospectively) to observe outcomes, comparing them to an unexposed or alternatively exposed group [30] [36]. It is highly efficient for studying multiple outcomes from a single exposure and is well-suited for safety surveillance in large databases. A key methodological enhancement is the "new-user" design, which identifies patients at the initiation of therapy, thereby avoiding prevalent user bias that can distort safety signals [32]. For example, an FDA study using Medicare claims data employed a retrospective cohort design to identify an increased risk of severe hypocalcemia with Prolia (denosumab) in patients with advanced chronic kidney disease, resulting in a Boxed Warning [35].
Case-Control Studies: This design starts with patients who have experienced the outcome of interest (e.g., a specific adverse event) and matches them to controls without the outcome, then looks back to compare prior drug exposures [30]. It is particularly powerful for studying rare adverse events where a cohort design would be inefficient, as it ensures sufficient cases for meaningful analysis. Careful matching of cases and controls on potential confounders (e.g., age, comorbidities) is critical for validity.
Cross-sectional Studies (Case Series): These studies provide a snapshot of a population at a single point in time, describing the frequency and characteristics of adverse events [30]. While useful for hypothesis generation and characterizing the natural history of a drug's safety profile, they generally cannot establish causality due to the lack of temporal sequence between exposure and outcome.
Advanced Methodological Approaches
External Control Arms (ECA): Also known as historical controls, ECAs use existing RWD to construct a control group for a single-arm trial, providing a comparative context for safety assessment when randomized controls are unethical or impractical [37] [35]. This approach was pivotal for the approval of Aurlumyn (iloprost) for severe frostbite, where a retrospective cohort study of frostbite patients from medical records served as confirmatory evidence against the treated group [35]. However, ECAs are frequently critiqued by regulators and HTA bodies due to potential methodological biases from unmeasured confounders [37] [38].
Hybrid Study Designs: Combining elements of RCTs and RWE, these designs leverage the strengths of both. The approval of Actemra (tocilizumab) provides a landmark example, where an RCT used RWD from national death records as the primary source for its efficacy endpoint (28-day mortality) [35]. This hybrid approach can increase efficiency and enhance the real-world applicability of trial results.
The following diagram illustrates the typical workflow for designing and conducting an RWE study for drug safety.
Analytical Techniques for Mitigating Bias and Confounding
A primary challenge in RWE is managing bias and confounding inherent in observational data. Advanced statistical techniques are essential for producing credible safety evidence.
Propensity Score (PS) Methods: This family of techniques aims to simulate randomization by creating a balanced comparison between treated and untreated groups [30]. The propensity score is the probability of a patient receiving the treatment of interest, given their observed baseline characteristics. Propensity Score Matching is the most common application, where each patient in the treatment group is matched to one or more patients in the control group with a similar PS, creating a pseudo-randomized cohort for analysis [30] [32]. Alternative approaches include PS weighting, stratification, and covariate adjustment using the PS, each with specific advantages depending on the data structure and sample size.
Machine Learning (ML) and Artificial Intelligence (AI): ML algorithms are increasingly deployed to detect complex patterns and predict outcomes within large RWD sets [31] [30]. Natural Language Processing (NLP), a subfield of AI, is particularly valuable for extracting structured information from unstructured clinical narratives in EHRs, such as physician notes, which often contain crucial details about adverse drug reactions that are not captured in coded data [30] [32].
Sensitivity Analyses: These are critical for assessing the robustness of safety findings. They test how inferred results might change if key assumptions (e.g., about unmeasured confounders) were different [32]. By quantifying the potential impact of residual bias, sensitivity analyses provide regulators and researchers with greater confidence in the conclusions drawn from RWE.
Regulatory Landscape and Case Studies of RWE in Safety
Regulatory bodies globally are increasingly accepting RWE to support safety assessments, though acceptance for efficacy claims remains more variable [37] [36] [35].
Table 2: Regulatory Case Studies: RWE for Drug Safety and Labeling
| Drug / Product | Regulatory Action & Date | RWE Source & Design | Role of RWE & Impact |
|---|---|---|---|
| Prolia (Denosumab) | FDA Boxed Warning (2024) | Data: Medicare claimsDesign: Retrospective cohort | Role: Safety; Identified risk of severe hypocalcemia in advanced CKD patients [35] |
| Oral Anticoagulants | Class-wide Labeling Change (2021) | Data: Sentinel System (claims)Design: Retrospective cohort | Role: Safety; Quantified risk of clinically significant uterine bleeding [35] |
| Vimpat (Lacosamide) | Labeling Expansion (2023) | Data: PEDSnet EHRsDesign: Retrospective cohort | Role: Safety; Provided additional pediatric safety data for new dosing [35] |
| Beta Blockers | Safety Labeling Change (2025) | Data: Sentinel SystemDesign: Retrospective cohort | Role: Safety; Associated beta blocker use with hypoglycemia in pediatric populations [35] |
The regulatory landscape is evolving, with initiatives like the European Union's Joint Clinical Assessment in 2025 pushing for more synergetic standards between regulators and Health Technology Assessment (HTA) bodies like NICE (UK), G-BA (Germany), and HAS (France) [37]. However, a significant challenge remains: discrepancies in RWE acceptability across these different agencies for the same product, often due to divergent standards for methodological rigor and evidence sufficiency [37] [38].
Implementing robust RWE studies requires a suite of methodological tools, data resources, and technological platforms.
Table 3: Essential Reagents and Resources for RWE Studies
| Tool / Resource | Category | Primary Function | Application in Safety Research |
|---|---|---|---|
| OHDSI / OMOP CDM | Data Standardization | Provides a common data model to standardize and analyze disparate RWD sources [32] | Enables large-scale, reproducible safety surveillance across international data networks |
| FDA Sentinel System | Distributed Data Network | A national system for monitoring medical product safety using pre-defined, executable queries [35] | Rapid querying of safety signals across millions of patients while maintaining data privacy |
| PROC PS Matching | Statistical Software (SAS) | Implements propensity score matching and related techniques for confounding adjustment | Creates balanced comparison cohorts to estimate comparative safety and hazard ratios |
| R (ggplot2, tableone) | Statistical Software (R) | Open-source environment for data manipulation, statistical analysis, and creation of publication-quality graphics | Comprehensive analysis from data cleaning and cohort description to advanced modeling and visualization |
| Aetion Evidence Platform | RWE Analytics Platform | Rapid-cycle analytics platform that executes validated study designs on RWD [39] | Accelerates hypothesis testing for safety signals using principles of causal inference |
| Flatiron Health Platform | Curated Oncology RWD | A longitudinal, demographically diverse database derived from de-identified EHR data from oncology practices [39] | Comparative safety studies of novel vs. established oncology therapies in real-world patient populations |
RWE has firmly established itself as a cornerstone of modern pharmacovigilance, providing critical insights into the comparative safety of novel and established drug classes across diverse real-world populations. The strategic application of rigorous study designs—including cohort, case-control, and external control analyses—coupled with advanced methodological techniques to mitigate bias, is essential for generating evidence that is both scientifically valid and actionable for regulatory and clinical decision-making.
As the field advances, the integration of digital health technologies and artificial intelligence with traditional RWD sources will further enhance our ability to detect and understand safety signals [31]. The ongoing harmonization of regulatory and HTA standards for RWE evaluation will be crucial to ensuring that these insights ultimately contribute to safer, more equitable, and more personalized patient care [37] [38]. For researchers and drug development professionals, mastering this complex and evolving landscape is no longer optional but a fundamental requirement for advancing public health.
In modern drug development, the timely anticipation of safety liabilities is paramount for protecting patient health and de-risking pharmaceutical R&D. Translational safety intelligence represents a paradigm shift from reactive drug safety monitoring to a proactive model that integrates and analyzes data across the entire drug lifecycle—from preclinical discovery to post-marketing surveillance. This approach aims to systematically translate safety signals from laboratory models to human clinical outcomes, enabling researchers to identify, validate, and mitigate potential risks earlier in the development process [40]. The fundamental challenge this field addresses is the translational gap between preclinical findings and clinical adverse events, a disconnect arising from biological differences between species, methodological variations in toxicity assessment, and the limited scope of pre-approval clinical trials [41].
This guide objectively compares leading technological approaches in translational safety intelligence, with particular focus on the OFF-X platform and its alternatives. By examining their respective data sources, methodological frameworks, and application contexts, we provide drug development professionals with evidence-based insights to inform their safety assessment strategies.
Comparative Platforms and Databases for Safety Intelligence
Table 1: Comparative Analysis of Translational Safety Intelligence Platforms
| Platform/Database | Primary Focus | Data Sources | Key Analytical Capabilities | Regulatory Connectivity |
|---|---|---|---|---|
| OFF-X [40] | Comprehensive translational safety | Preclinical toxicity data, clinical adverse events, pharmacovigilance data, regulatory documents, real-world evidence (FAERS, JADER) | Benchmarking safety profiles, predictive toxicity assessment, signal prioritization, structure-toxicity exploration | FDA material transfer agreement; EMA, PMDA label comparison |
| eTRANSAFE ToxHub [41] | Translational safety assessment | Legacy preclinical data (SEND format), clinical trial data, off-target pharmacology data | Semantic mapping between preclinical and clinical ontologies, read-across analysis, predictive modeling | SEND-standardized data format for regulatory submission |
| ClinicalTrials.gov-based Analytics [42] | Clinical trial adverse event mining | Aggregate adverse event data from ClinicalTrials.gov repository | Semantic querying, visual analytics of AE rates, flower glyph visualization | Source of mandatory clinical trial results reporting |
| FDA Sentinel Initiative [43] | Post-market safety surveillance | Electronic health records, insurance claims databases, registries | Active real-time surveillance, signal detection in approved products | FDA regulatory safety assessment |
Quantitative Data Support
Table 2: Empirical Evidence on Drug Safety Challenges and Platform Applications
| Evidence Category | Finding | Implication for Safety Intelligence |
|---|---|---|
| Clinical Trial Limitations [44] | RCTs are underpowered to detect rare adverse events; only 14% of serious ADRs are detected by time of approval | Platforms must integrate data beyond pre-marketing trials |
| First-in-Class Drug Safety [7] | No significant difference in post-market safety warnings between first-in-class (98 drugs) vs. non-first-in-class (194 drugs) | Safety prediction cannot rely solely on mechanistic novelty |
| Semantic Mining Capability [42] | Platform analyzing 42,000+ ClinicalTrials.gov studies enabled rapid AE comparison across drug classes | Automated analysis of public data can complement traditional meta-analyses |
| Data Integration Scale [40] | OFF-X covers 39,000+ drugs and biologics, 15,000+ targets, and 14,000+ adverse events | Comprehensive coverage requires substantial data infrastructure |
Experimental Protocols for Translational Safety Assessment
Protocol 1: Preclinical-Clinical Translation Analysis
Objective: To systematically evaluate the translational concordance between preclinical toxicology findings and clinical adverse drug reactions for a specific target or pathway.
Methodology:
- Compound Selection: Identify compounds with shared molecular targets or mechanisms of action using ontology-based querying [41].
- Data Extraction:
- Semantic Mapping: Apply ontology alignment tools (e.g., using SNOMED CT as an intermediary) to bridge preclinical observations (e.g., SEND terms) with clinical adverse events (MedDRA terms) [41].
- Concordance Analysis: Calculate translational concordance rates by organ system and severity grade. Employ statistical methods to identify significant associations.
- Visualization: Generate flower glyphs or heat maps to represent adverse event rates across multiple organ systems and treatment groups [42].
Protocol 2: Class-Wide Safety Benchmarking
Objective: To compare the safety profiles of novel drug classes against established therapies for specific therapeutic areas (e.g., AML treatments).
Methodology:
- Class Definition: Define drug classes by molecular target or mechanism of action (e.g., menin inhibitors vs. CD47 inhibitors in AML) [3].
- Data Aggregation: Collect integrated preclinical and clinical safety data for each class member from translational platforms (OFF-X, eTRANSAFE) and public repositories [40] [41].
- Safety Index Calculation: Develop composite safety scores incorporating:
- Preclinical toxicity incidence and severity
- Clinical adverse event frequencies and seriousness
- Regulatory actions (boxed warnings, contraindications)
- Comparative Analysis: Employ statistical methods (e.g., meta-analytic approaches) to compare safety profiles across classes, adjusting for trial duration, patient population, and indication.
- Pathway Mapping: Visualize safety liabilities within biological pathways to identify potential mechanistic explanations for class effects [40].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Resources for Translational Safety
| Tool/Resource | Function | Application Context |
|---|---|---|
| Standardized Ontologies (MedDRA, SEND, SNOMED CT) [41] | Semantic interoperability between preclinical and clinical data | Enables cross-species data mapping and integrated analysis |
| Toxicity Pathway Maps [40] | Graphical representation of biological cascades leading to adverse outcomes | Identifies and prioritizes investigational target safety based on signaling cascades |
| Structure-Toxicity Explorer [40] | Correlates chemical substructures with specific safety liabilities | Supports medicinal chemistry optimization during lead candidate selection |
| Adverse Event Visual Analytics (Flower Glyphs) [42] | Intuitive visualization of AE rates across multiple organ systems | Facilitates rapid safety comparison between treatment groups in clinical trials |
| Target Class Safety Score [40] | Quantifies emerging safety liabilities for target classes | Enables monitoring of class effects across development pipeline |
| NSC624206 | NSC624206, MF:C19H33Cl2NS2, MW:410.5 g/mol | Chemical Reagent |
| WAY-100635 maleate | WAY-100635 maleate, MF:C29H38N4O6, MW:538.6 g/mol | Chemical Reagent |
Analysis of Safety Intelligence in Action: Case Examples
Case Study 1: Menin vs. CD47 Inhibitors in AML
The contrasting clinical trajectories of menin inhibitors and CD47 inhibitors in acute myeloid leukemia (AML) illustrate the value of robust safety intelligence. Menin inhibitors (e.g., revumenib) demonstrated consistent clinical benefit across compounds in the class, supporting the target's therapeutic validity [3]. Conversely, CD47 inhibitors showed promising preclinical results but failed in multiple phase 3 trials due to significant toxicity issues, particularly severe anemia, without corresponding survival benefits [3]. This case highlights how platforms that integrate preclinical biology with early clinical findings could potentially identify such liabilities earlier through better understanding of target biology and translational pathways.
Case Study 2: Predictive Performance for First-in-Class Drugs
Research examining Health Canada approvals from 1997-2012 found no significant difference in post-market safety warnings between first-in-class (98 drugs) and non-first-in-class drugs (194 drugs) [7]. This finding challenges assumptions about the inherent risk profile of novel mechanisms and underscores the need for sophisticated prediction tools that look beyond mechanistic novelty alone. Platforms like OFF-X that incorporate data on signaling pathways and target class liabilities may offer more nuanced predictive capabilities for novel drug classes [40].
Translational safety intelligence platforms represent a critical advancement in pharmacovigilance, moving the field from reactive monitoring to proactive risk anticipation. The comparative analysis presented in this guide demonstrates that while platforms differ in their specific approaches and data sources, they share a common goal: bridging the translational gap between preclinical findings and clinical outcomes.
For researchers and drug development professionals, strategic implementation of these tools requires matching platform capabilities to specific use cases. OFF-X offers comprehensive coverage across the development lifecycle, while specialized resources like eTRANSAFE provide deep translational insights through semantic mapping, and ClinicalTrials.gov mining enables rapid safety comparisons [40] [41] [42]. The most effective safety intelligence strategies will likely integrate multiple approaches, leveraging the strengths of each to build a more complete understanding of drug safety profiles throughout the development pipeline.
As these technologies continue to evolve, their integration with emerging methodologies like molecular pathological epidemiology [45] and adaptive clinical trial designs [45] will further enhance our ability to anticipate safety liabilities, ultimately leading to safer therapeutics for patients.
For researchers and drug development professionals, navigating the complex interplay between global harmonization initiatives and stringent local regulatory requirements represents a critical challenge in bringing new therapies to market. The international framework for safety reporting is built upon a foundation of harmonized principles, designed to streamline drug development and ensure consistent patient protection worldwide. However, the practical implementation of these principles varies significantly across regulatory jurisdictions, creating a complex compliance landscape that can impact everything from clinical trial design to post-market surveillance.
This guide examines the current state of global harmonization versus local requirements within the context of comparative safety profiling of novel versus established drug classes. By objectively comparing the regulatory frameworks, data requirements, and compliance methodologies across major regions, we provide a structured approach for scientific teams to navigate these complexities while maintaining rigorous safety assessment standards throughout the drug development lifecycle.
Global Harmonization Frameworks and Key Initiatives
Global harmonization efforts aim to create consistent standards for safety reporting across international borders, reducing redundant requirements and accelerating patient access to innovative therapies. Several key organizations drive these initiatives through guideline development and regulatory convergence.
Table 1: Major Global Harmonization Initiatives Impacting Drug Safety (2025)
| Organization/Initiative | Key Guidelines/Updates (2025) | Primary Focus | Impact on Safety Reporting |
|---|---|---|---|
| International Council for Harmonisation (ICH) | ICH E6(R3): Good Clinical Practice (Final) [46] | Modernizes clinical trial framework with risk-based approaches | Promotes innovative trial designs while maintaining participant protection and data quality |
| ICH | ICH E2D(R1): Post-Approval Safety Data (Step 4) [46] | Standardizes post-approval safety data management | Establishes consistent requirements for safety data collection after drug approval |
| World Health Organization (WHO) | Guideline on Balanced National Policies for Controlled Medicines [47] | Ensures access to controlled medicines while managing risks | Provides framework for countries to develop policies ensuring safe, equitable access to essential medicines |
| International Medical Device Regulators Forum (IMDRF) | Good Machine Learning Practice for Medical Device Development [48] | Regulates AI/ML in medical products | Creates standards for safety and effectiveness of AI-driven healthcare technologies |
The ICH E6(R3) guideline, finalized in 2025, introduces more flexible, risk-based approaches to clinical trial conduct, embracing modern innovations in trial design and technology while maintaining fundamental patient protection and data integrity standards [46]. This update reflects the evolving landscape of clinical research, particularly relevant for assessing safety profiles of novel drug classes where traditional trial designs may be insufficient.
Concurrently, the WHO's new guideline on controlled medicines addresses global disparities in access while emphasizing safety controls, particularly important for drugs with abuse potential or novel safety concerns [47]. These harmonization efforts provide an overarching framework that national regulators increasingly reference when developing their local requirements.
Regional Implementation: A Comparative Analysis of Local Requirements
Despite global harmonization initiatives, local implementation varies significantly, creating a complex patchwork of requirements that drug developers must navigate. The "building block" approach of GHS allows countries to select which hazard classes and communication elements align with their existing regulatory structures, resulting in substantial regional differences [49].
Table 2: Comparative Analysis of Regional Safety Reporting Requirements (2025)
| Region/Authority | Key Local Requirements | Update Timelines | Unique Regional Considerations |
|---|---|---|---|
| United States (FDA) | Expedited Programs for Regenerative Medicine Therapies (draft) [46] | Draft guidance issued 2025 | RMAT designation and accelerated approval pathways for serious conditions |
| European Union (EMA) | Reflection Paper on Patient Experience Data [46] | Draft released September 2025 | Encourages inclusion of patient perspectives throughout product lifecycle |
| Canada (Health Canada) | Good Pharmacovigilance Practices (GVP) Inspection Guidelines (draft update) [46] | Consultation closed September 2025 | Updated risk classification guide for PV inspection findings, replacing 2013 version |
| China (NMPA) | Revised Clinical Trial Policies [46] | Effective September 2025 | Accelerated trial approval timelines (~30%), adaptive designs permitted |
| Australia (TGA) | Adoption of GVP Module I & ICH E9(R1) [46] | Effective September 2025 | Aligns with EMA's pharmacovigilance systems and introduces estimand framework |
The European Medicines Agency (EMA) has emphasized patient-centric approaches in recent updates, with a 2025 reflection paper encouraging medicine developers to systematically gather and include patient experience data throughout the product lifecycle [46]. This represents a significant evolution in safety reporting, moving beyond traditional adverse event collection to incorporate patient perspectives on treatment benefits and risks.
Meanwhile, China's NMPA has implemented substantial reforms to streamline clinical development, reducing trial approval timelines by approximately 30% and allowing adaptive trial designs with real-time protocol modifications under stricter safety oversight [46]. These changes align China's GCP standards closer to international norms while maintaining specific local requirements that reflect regional healthcare priorities.
Experimental Design for Comparative Safety Assessment
Standardized Methodologies for Safety Data Collection
Robust comparative safety assessment requires standardized methodologies that can be applied across different regulatory environments while accommodating local requirements. The experimental framework must generate data that satisfies both global harmonization principles and specific regional expectations.
Core Safety Assessment Protocol:
- Preclinical Safety Profiling: Comprehensive in vitro and in vivo toxicology studies following ICH S and M guidelines
- Clinical Trial Safety Monitoring: Systematic adverse event collection using standardized MedDRA terminology
- Comparative Analytics: Direct comparison of novel agents against established standards using consistent metrics
- Post-Market Surveillance: Proactive safety monitoring through registries, active surveillance systems, and real-world evidence generation
For novel drug classes like menin inhibitors for AML, which have demonstrated consistent clinical benefit across different compounds, safety assessment must focus on class-specific adverse effects while comparing them to established treatment regimens [3]. This approach enables researchers to identify both the unique safety profile of the novel mechanism and its relative safety advantages compared to standard care.
Safety Signaling Pathways and Detection Workflows
Modern safety assessment requires sophisticated methodologies for signal detection, validation, and management across multiple data sources. The diagram below illustrates the core workflow for safety signal management in the context of global pharmacovigilance operations.
Diagram 1: Safety Signal Management Workflow
This structured approach to signal management aligns with EU GVP Module IX requirements while accommodating region-specific expectations for signal validation and confirmation [50] [51]. The workflow emphasizes the importance of data quality assessment before initiating regulatory actions, ensuring that potential safety signals are properly validated against established pharmacological principles and clinical context.
Comparative Safety Data: Novel vs. Established Drug Classes
Objective comparison of safety profiles between novel and established drug classes requires standardized metrics and consistent methodologies across different regulatory environments. The tabular data below illustrates a structured approach to this comparative analysis.
Table 3: Structured Safety Comparison Framework for Novel vs. Established Drug Classes
| Safety Assessment Parameter | Novel Drug Class (Menin Inhibitors) | Established Drug Class (CD47 Inhibitors) | Regional Reporting Variations |
|---|---|---|---|
| Mechanism-Based Toxicities | Differentiation syndrome, QT prolongation [3] | Severe anemia, transfusion dependence [3] | EU: Emphasis on risk minimization measures; US: Focus on serious adverse event reporting |
| Overall Risk-Benefit Profile | Favorable in specific genetic subtypes (NPM1-mutated AML) [3] | Unfavorable due to toxicity burden without survival benefit [3] | FDA: Accelerated approval possible for serious conditions; EMA: Requires demonstration of meaningful clinical benefit |
| Clinical Trial Discontinuation Rates | Low (consistent clinical benefit across class) [3] | High (multiple phase 3 trial failures) [3] | Consistent requirements across regions, but interpretation of discontinuation data may vary |
| Post-Market Safety Study Requirements | Long-term follow-up for combination approaches [46] | Limited due to development program discontinuation [3] | FDA: May require post-market commitments; EMA: Focused on risk management system effectiveness |
The contrasting experience between menin inhibitors and CD47 inhibitors in AML illustrates the importance of rigorous safety assessment throughout development. While menin inhibitors have demonstrated consistent clinical benefit leading to approval and frontline combination studies, CD47 inhibitors showed promising preclinical results but failed in phase 3 trials due to significant toxicity issues, particularly severe anemia [3]. This highlights that novel mechanisms require particularly careful safety evaluation, as their risk profiles may differ substantially from established drug classes.
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing robust safety assessment strategies requires specific methodological tools and frameworks. The following table details essential components for designing studies that meet both global harmonization principles and local regulatory requirements.
Table 4: Essential Research Reagent Solutions for International Safety Assessment
| Tool/Reagent | Function in Safety Assessment | Application in Global Context |
|---|---|---|
| MedDRA Terminology | Standardized medical dictionary for coding adverse events | Required for US, EU, Japan; facilitates global data pooling and analysis |
| EudraVigilance System | EU's system for managing and analyzing safety reports | Mandatory for EU-based trials; must be integrated with global safety databases |
| ESTRI Gateway | Electronic standards for transmission of regulatory information | Supports electronic submission of safety reports to multiple regulatory authorities |
| CIOMS Forms | Standardized forms for expedited safety reporting | Internationally recognized format accepted by most regulatory authorities |
| PSUR/PBRER Templates | Periodic safety update reporting templates | ICH-harmonized format with regional implementation variations |
| Ruboxistaurin HCl | Ruboxistaurin HCl, MF:C28H29ClN4O3, MW:505.0 g/mol | Chemical Reagent |
| RG14620 | RG14620, CAS:138989-56-7, MF:C14H8Cl2N2, MW:275.1 g/mol | Chemical Reagent |
These tools form the foundation for compliant safety reporting across multiple jurisdictions. The MedDRA terminology system provides a standardized vocabulary for adverse event reporting, while the CIOMS forms facilitate expedited reporting of serious unexpected adverse reactions [50] [51]. Implementation of these tools requires careful planning to ensure consistency across different regions while accommodating specific local requirements for submission formats and timelines.
Strategic Implementation: Navigating Global vs. Local Requirements
Successfully navigating the complex landscape of global harmonization and local requirements demands systematic approaches and strategic planning. The diagram below illustrates a decision framework for managing safety reporting across multiple jurisdictions.
Diagram 2: Global-Local Compliance Strategy Framework
Effective implementation requires pharmaceutical companies to first establish a comprehensive global safety strategy based on harmonized principles, then identify specific local requirements in target markets [49]. This approach enables teams to develop streamlined processes that satisfy the most stringent requirements while maintaining flexibility for region-specific adaptations.
Key strategic considerations include:
- Maintaining a globally harmonized safety database with capabilities for regional reporting variations
- Implementing robust change control processes to monitor evolving regulatory requirements
- Establishing clear protocols for managing discrepancies in safety reporting timelines across regions
- Developing training programs that address both global standards and local implementation requirements
Navigating the complex interplay between global harmonization and local requirements remains a significant challenge in international safety reporting. The continuing evolution of ICH guidelines, regional implementation differences, and emerging technologies like AI in drug development ensure that this landscape will continue to change rapidly [48].
Successful navigation requires both technical expertise in safety assessment methodologies and strategic thinking about regulatory compliance. By understanding the common foundations and specific variations across major markets, drug development professionals can create efficient, compliant safety reporting systems that facilitate global development while meeting local requirements. This approach ultimately supports the timely availability of novel therapies with well-characterized safety profiles, benefiting patients worldwide while maintaining the highest standards of safety surveillance.
Solving Safety Surveillance Challenges: Optimization and Risk Mitigation
Addressing Confounding and Channeling Bias in Observational Safety Studies
Observational studies have become indispensable in the evaluation of drug safety profiles, particularly in the post-marketing phase where pre-approval clinical trials face limitations in detecting rare, delayed, or subgroup-specific adverse events [52]. These studies leverage large population databases—including administrative claims data and electronic health records—to provide adequate sample sizes and follow-up length necessary for robust safety signal detection [52]. However, the non-randomized nature of these studies introduces significant methodological challenges, primarily through confounding and channeling biases that can distort the true relationship between drug exposure and safety outcomes.
Confounding occurs when a risk factor for the outcome is unequally distributed between exposure groups, potentially strengthening, weakening, or even reversing the true exposure-outcome association [53]. Channeling bias represents a specific form of confounding where drugs with similar therapeutic indications are preferentially prescribed to patients with varying baseline prognoses, particularly problematic when comparing older versus newer pharmaceuticals within the same therapeutic class [54]. This article provides a comprehensive comparison of methodological approaches for addressing these biases, with specific application to evaluating the comparative safety profiles of novel versus established drug classes.
Understanding Key Biases in Safety Research
Confounding and Its Variants
In observational studies, a factor is considered a confounder when it meets three criteria: (1) it is a risk factor for the outcome, (2) it is associated with the exposure of interest, and (3) it is not an intermediate variable on the causal pathway between exposure and outcome [53]. Several specialized forms of confounding present particular challenges in pharmacoepidemiology:
- Confounding by Indication: This prevalent bias occurs when the clinical indication for treatment (e.g., disease presence or severity) also affects the outcome [53]. For instance, in a study comparing aldosterone antagonist use versus nonuse for heart failure, clinicians preferentially prescribe these drugs to sicker patients, creating a spurious association between treatment and increased mortality if disease severity is not adequately controlled [53].
- Confounding by Frailty: This bias arises when frailer patients near the end of life are less likely to receive preventive therapies, making treatments appear more beneficial than they truly are [53]. This phenomenon explains implausibly large mortality reductions (40-60%) observed in some influenza vaccine studies in older adults [53].
- Time-Varying Confounding: This occurs when confounders change over time and are affected by previous exposure [53]. In studies of erythropoietin-stimulating agent (ESA) dose and mortality, hemoglobin levels represent a time-varying confounder as they predict ESA dose, are influenced by prior ESA dose, and independently associate with mortality [53].
Channeling Bias in Drug Safety Evaluations
Channeling bias represents a specialized form of confounding particularly relevant to comparative drug safety studies. It occurs when "drug therapies with similar indications are preferentially prescribed to groups of patients with varying baseline prognoses" [54]. This phenomenon is especially problematic when comparing newer versus older drugs from the same therapeutic class, as clinicians may reserve novel agents for patients who have failed established treatments or for those with more severe disease manifestations. The non-random assignment of patients to treatment groups in observational studies creates imbalances in risk factors that can bias treatment effect estimates unless adequately addressed through specialized methodological approaches [54].
Additional Methodological Challenges
Beyond confounding, observational safety studies face several other biases that require careful consideration:
- Selection Bias: Distortions that result from procedures used to select subjects and factors that determine study participation [55]. This includes "healthy user bias" where prevalent drug users are "survivors" of early pharmacotherapy, potentially excluding those who discontinued due to early adverse reactions [55].
- Protopathic Bias: Also called reverse causation, this occurs when drug initiation happens in response to symptoms of an undiagnosed disease [55]. For example, analgesic use for pain caused by an undiagnosed tumor might create a spurious association between the drug and cancer development [55].
- Surveillance/Detection Bias: Arises when one exposure group has higher probability of outcome detection due to increased medical surveillance [55]. Post-menopausal estrogen exposure associates with increased bleeding that triggers endometrial cancer screening, potentially overestimating cancer risk due to detection bias [55].
- Competition Bias: In spontaneous reporting databases, well-established drug-event associations can mask signals for less recognized associations [56]. Removing reports involving known high-risk drugs (e.g., antithrombotics for hemorrhage studies) can unmask previously obscured safety signals [56].
Table 1: Key Biases in Observational Safety Studies and Their Impact
| Bias Type | Definition | Potential Impact on Safety Signals |
|---|---|---|
| Confounding by Indication | Treatment indication independently affects outcome | Can make treatments appear harmful (e.g., sicker patients receive drug and have worse outcomes) |
| Channeling Bias | Newer vs. older drugs prescribed to patients with different prognoses | Biases comparative safety estimates between drug classes |
| Selection Bias | Study participants differ systematically from target population | May underestimate risk if "healthy user" effect present |
| Protopathic Bias | Drug initiated for early symptoms of undiagnosed condition | Creates false association between drug and outcome |
| Competition Bias | Known safety signals mask unknown signals in databases | Obscures genuine safety signals for less recognized associations |
Methodological Approaches for Bias Mitigation
Design-Phase Strategies
Addressing bias begins with thoughtful study design, which offers several robust approaches for mitigating confounding and channeling biases:
- Active Comparator Design: Rather than comparing a drug to non-use, this approach selects an active comparator with the same clinical indication and therapeutic role [53] [54]. This design directly mitigates channeling bias by ensuring comparison groups have similar underlying indications for treatment. The active comparator new-user design represents a particularly robust implementation of this approach, comparing two active treatments initiated by new users [55].
- New-User Design: Restricting analyses to incident users (patients starting treatment during the study period) helps mitigate prevalent user biases, where "survivors" of early treatment periods may be healthier than new initiators [55]. This design requires absence of prior use of the study drug during a predefined washout period and ensures all patients enter the study at a similar point in treatment history [55].
- Restriction: Setting specific criteria for study inclusion can eliminate or reduce confounding by those criteria [53]. For example, restricting a study to males under 65 years would eliminate confounding by sex and reduce confounding by age [53]. While implementable, this approach reduces sample size and may limit generalizability [53].
- Matching: Creating matched sets of patients with similar values for key confounders balances these factors between exposure groups [53]. In studies of benzodiazepines and fracture risk, matching users and non-users by age and sex helps control confounding by these factors [53]. Like restriction, matching becomes challenging with multiple confounders and may exclude unmatched patients [53].
Analysis-Phase Methodologies
Advanced statistical methods applied during analysis provide additional tools for addressing residual confounding:
- Propensity Score Methods: These approaches create a summary score representing a patient's predicted probability of receiving the treatment of interest given their measured baseline characteristics [53] [54]. Propensity score matching creates matched cohorts of treated and comparator patients with similar propensity scores [53], while propensity score weighting creates a pseudo-population where treated and comparator groups have similar baseline characteristics [53]. These methods are particularly valuable when the number of outcome events is limited relative to the number of potential confounders [53].
- Multivariable Adjustment: Including potential confounders as covariates in regression models represents the most common analytic approach for confounding control [53]. While straightforward to implement, this method only controls for measured confounders and the number of adjustable confounders is limited by the number of outcome events [53].
- G-Methods: Complex analytic approaches, including g-estimation, inverse probability weighting, and g-computation, appropriately handle time-varying confounding in settings with time-varying exposures [53]. These methods require advanced statistical expertise but provide robust solutions for complex longitudinal data structures [53].
- Within-Individual Designs: Methods like self-controlled case series (SCCS) and case-crossover studies use each patient as their own control, comparing different observation periods within the same individual [52]. These designs automatically control for time-invariant confounders (e.g., genetics, socioeconomic status, chronic comorbidities) that are difficult to measure or adjust for using conventional methods [52].
Table 2: Comparison of Methods for Addressing Confounding and Channeling Bias
| Method | Implementation Phase | Key Mechanism | Advantages | Limitations |
|---|---|---|---|---|
| Active Comparator Design | Design | Compares similar indications | Mitigates channeling bias; clinically relevant | Requires comparable alternative treatment |
| New-User Design | Design | Restricts to incident users | Reduces prevalent user bias | May limit sample size and long-term exposure data |
| Propensity Score Matching | Analysis | Balances measured covariates | Handles multiple confounders with limited events | Only addresses measured confounders |
| Within-Individual Designs | Design/Analysis | Self-controlled comparison | Controls for time-invariant factors | Requires specific exposure and outcome patterns |
| Multivariable Adjustment | Analysis | Statistical adjustment in models | Easily implemented | Limited by number of events and measured variables |
Comparative Analysis of Methodological Performance
Quantitative Comparison of Bias Control Methods
The performance of different methodological approaches can be evaluated through their application in comparative drug safety studies. Research examining first-in-class drugs approved by Health Canada from 1997-2012 demonstrated the value of rigorous methodology in safety assessments [7]. This study, which utilized comprehensive safety data from MedEffect Canada and innovative therapeutic classifications, found no difference in safety outcomes between first-in-class and non-first-in-class drugs when appropriate methodologies were applied [7]. Importantly, the benefit-to-harm ratio for first-in-class drugs was actually better than for non-first-in-class drugs when measured by post-market safety warnings and withdrawals [7].
The selection of appropriate comparator groups significantly influences safety estimates. Active comparator designs typically produce more valid safety estimates than non-user comparisons, particularly for channeling bias mitigation [54]. For instance, in studies comparing novel oral anticoagulants to warfarin, active comparator designs have demonstrated better control for cardiovascular risk profiles that differ between these treatment groups in clinical practice.
Case Studies in Bias Mitigation
- Gastrointestinal Bleeding and Dabigatran: A retrospective cohort study investigating gastroprotective agents (GPAs) and gastrointestinal bleeding (GIB) risk in dabigatran users demonstrated proper adjustment for confounding [52]. Using electronic medical records and Poisson regression with adjustment for baseline medical conditions and concurrent medications, the study found a 48% reduction in GIB risk among GPA users compared to non-users (IRR 0.52; 95% CI 0.35-0.77) [52].
- Venous Thromboembolism and Oral Contraceptives: A nested case-control study investigating combined oral contraceptives and venous thromboembolism (VTE) risk utilized comprehensive matching and conditional logistic regression to address confounding [52]. The study matched each case with up to five controls by birth year and practice, finding current use of any combined oral contraceptive significantly increased VTE risk (adjusted OR 2.97, 95% CI 2.78-3.17) compared to no exposure [52].
- Competition Bias in Signal Detection: Research analyzing spontaneous reporting databases demonstrated that removing reports involving drugs with well-established safety associations (e.g., antithrombotics for hemorrhage reports) unmasked previously obscured safety signals [56]. This approach revealed ten potentially significant signals that were previously masked, with three subsequently confirmed as true positives (isotretinoin, methylprednisolone, and milnacipran) [56].
Experimental Protocols for Bias Assessment
Protocol for Active Comparator New-User Design
Objective: To compare incidence of targeted adverse events between novel and established drug classes while minimizing channeling and confounding biases.
Population Selection:
- Identify all new users of either the novel drug (exposure group) or established comparator (reference group) within a defined enrollment period
- Apply strict washout period (e.g., 6-12 months) with no use of either drug class to ensure incident user status
- Require continuous database enrollment during baseline period (e.g., 6-12 months) to ascertain comorbidity and medication history
Covariate Assessment:
- Extract data on demographic characteristics, comorbidities, concomitant medications, and healthcare utilization during baseline period
- Include specific measures of disease severity and indication for treatment where available
- Document prior exposure to other medications in the same therapeutic area
Propensity Score Estimation:
- Estimate propensity scores using logistic regression with treatment group as outcome and all measured baseline characteristics as predictors
- Check propensity score distribution overlap between groups and consider trimming if substantial non-overlap exists
- Implement propensity score matching (1:1 or 1:N) using caliper matching (e.g., caliper = 0.2 standard deviations of the logit of the propensity score)
- Assess balance of covariates after matching using standardized differences (<0.1 indicates good balance)
Outcome Assessment:
- Define clear operational criteria for safety outcomes using validated coding algorithms where available
- Implement lag periods for outcomes potentially subject to protopathic bias
- Censor follow-up at treatment discontinuation, switching, or end of study period
Analysis:
- Calculate incidence rates and hazard ratios using Cox proportional hazards models with robust variance estimators
- Include the matching strata in the outcome model to account for matched design
- Conduct sensitivity analyses using different propensity score implementations (weighting, stratification)
- Perform quantitative bias analysis to evaluate potential impact of unmeasured confounding
Protocol for Self-Controlled Case Series
Objective: To evaluate association between drug exposure and acute adverse events while controlling for time-invariant confounding.
Study Population:
- Identify all individuals with at least one occurrence of the outcome of interest during the observation period
- Require documented exposure to the study drug during the observation period
- Define observation period for each individual based on data availability and biological plausibility
Risk Period Definition:
- Define risk periods based on pharmacological properties (e.g., 0-30 days post-initiation)
- Establish pre-risk periods if transient risk changes are plausible
- Designate all other person-time as control periods
Analysis:
- Use conditional Poisson regression to compare event rates between risk and control periods
- Adjust for age and calendar time through stratification or inclusion as covariates
- Account for between-individual variability in exposure patterns
- Conduct sensitivity analyses with varying risk period definitions
Diagram 1: Self-Controlled Case Series Workflow. This within-individual design uses each patient as their own control to eliminate time-invariant confounding.
Visualization Strategies for Safety Data
Principles for Effective Safety Data Visualization
Effective visualization of safety data enhances pattern recognition and facilitates communication of complex methodological concepts:
- Know Your Audience and Message: Tailor visualizations to the technical expertise of the target audience (regulators, clinicians, researchers) and ensure each visualization conveys a clear take-home message [57].
- Leverage Preattentive Attributes: Utilize visual properties processed preattentively by the human visual system (position, length, color hue, intensity) to highlight important patterns [57].
- Ensure Color Contrast and Accessibility: Select color palettes with sufficient contrast and consider colorblind-friendly schemes [57] [58]. For critical information, avoid relying solely on color to convey meaning.
- Avoid Chartjunk: Eliminate unnecessary visual elements that do not contribute to information transfer, maintaining clean, focused visualizations [57].
Recommended Visualization Approaches by Data Type
- Time-to-Event Data: Kaplan-Meier curves effectively display safety outcomes over time, particularly for comparing multiple exposure groups [7]. These curves appropriately account for variable follow-up time and censoring.
- Comparative Safety Profiles: Forest plots efficiently present multiple hazard ratios with confidence intervals, allowing rapid assessment of safety signals across different outcomes or patient subgroups.
- Covariate Balance: Love plots (standardized differences before and after matching) effectively demonstrate the success of propensity score methods in achieving balance between treatment groups.
- Temporal Patterns: Line charts ideally display trends in adverse event rates over time, while heatmaps can reveal clustering of safety events across multiple dimensions [59].
Diagram 2: Comprehensive Bias Mitigation Strategy. Integrated approach combining design-phase and analysis-phase methods with rigorous bias assessment.
Table 3: Key Methodological Approaches for Specific Bias Challenges
| Bias Challenge | Recommended Methods | Key Considerations |
|---|---|---|
| Channeling Bias (New vs. old drugs) | Active comparator new-user design with propensity score weighting | Ensure comparator drugs have same indication; assess balance of disease severity measures |
| Time-Varying Confounding (e.g., ESA and mortality) | G-methods (marginal structural models) | Carefully specify time-varying confounders affected by prior exposure |
| Unmeasured Confounding | Quantitative bias analysis, self-controlled designs | Quantify how strong unmeasured confounder would need to be to explain observed association |
| Protopathic Bias (Reverse causation) | Exposure lag periods, latency analyses | Exclude exposure immediately before outcome based on biological plausibility |
| Competition Bias (Spontaneous reports) | Exclusion of reports with strong competing associations | Remove cases and non-cases related to drugs with well-established associations |
| Prevalent User Bias | New-user design with adequate washout | Distinguish new users from treatment-experienced patients |
Addressing confounding and channeling bias requires thoughtful integration of design and analysis strategies tailored to the specific methodological challenges in observational safety studies. The active comparator new-user design combined with propensity score methods represents a particularly robust approach for comparative safety studies between novel and established drug classes, directly addressing channeling bias concerns [53] [55] [54]. Within-individual designs offer powerful alternatives that automatically control for time-invariant confounding [52], while quantitative bias analysis provides a framework for assessing the potential impact of residual confounding.
The evolving methodological landscape continues to provide increasingly sophisticated tools for mitigating biases in observational safety research. By strategically applying these methods and transparently reporting their limitations, researchers can generate more valid evidence regarding the comparative safety profiles of therapeutic alternatives, ultimately supporting safer medication use in clinical practice. As the field advances, integration of multiple methodological approaches with sensitivity analyses will further strengthen the evidentiary foundation from observational safety studies.
In the critical field of pharmacovigilance, distinguishing true safety signals from background noise represents a fundamental challenge for researchers and drug development professionals. The expanding volume of real-world data (RWD) presents both unprecedented opportunities for safety surveillance and significant challenges in signal discrimination. As regulatory landscapes evolve, the systematic approach to signal detection and management has become increasingly sophisticated, integrating advanced statistical methods, diverse data sources, and structured validation frameworks. This comparative analysis examines the methodologies, tools, and strategic frameworks essential for effective signal prioritization within the broader context of evaluating novel versus established drug classes.
Understanding Signals and Noise in Pharmacovigilance
Defining Signal and Noise
In drug safety monitoring, a signal is defined as "information that arises from one or multiple sources suggesting a new potentially causal association, or a new aspect of a known association, between an intervention and an event" [60]. This information must be scientifically plausible, reproducible across data sources, and clinically relevant. Crucially, a signal represents a hypothesis requiring validation rather than a confirmed safety issue.
In contrast, noise comprises irrelevant data, random variations, false positives, or confounding patterns that can obscure genuine signals. Noise often originates from reporting biases, confounding variables, data quality issues, or chance associations that lack biological plausibility [61] [60].
The Signal-to-Noise Challenge in Modern Pharmacovigilance
The proliferation of RWD sources has dramatically increased the complexity of signal detection. Traditional spontaneous reporting systems now complement electronic health records (EHRs), claims databases, patient registries, and digital health technologies [26]. While these sources provide comprehensive real-world evidence, they also introduce new dimensions of noise that must be filtered through sophisticated analytical approaches. Under-reporting in spontaneous systems and fragmentation across data sources further complicate signal detection efforts [62].
Methodologies for Signal Detection: A Comparative Analysis
Statistical Foundations and Disproportionality Analysis
Modern signal detection employs quantitative methods to identify unexpected drug-event associations by comparing observed reporting frequencies against expected baselines [60]. The following table summarizes core statistical approaches:
Table 1: Key Statistical Methods for Signal Detection
| Method | Mechanism | Applications | Regulatory Use |
|---|---|---|---|
| Proportional Reporting Ratio (PRR) | Compares specific drug-event rate to all other drugs | Initial signal filtering | EMA, FDA for initial screening |
| Reporting Odds Ratio (ROR) | Assesses odds of drug-event pair versus all combinations | Spontaneous report analysis | Preferred by EMA for robustness |
| Bayesian Confidence Propagation Neural Network (BCPNN) | Estimates association strength using Bayesian logic | Early-phase signal detection | WHO Uppsala Monitoring Centre |
| Information Component (IC) | Logarithmic measure of disproportionality with statistical shrinkage | Handling sparse data | WHO programmes |
These disproportionality methods function by analyzing frequency patterns within large safety databases to identify statistical associations that exceed predetermined thresholds [60]. However, each method carries limitations, including susceptibility to over-reporting biases from media attention or legal campaigns, under-reporting from passive surveillance, and confounding by indication overlap [60].
Real-World Data Integration and Advanced Analytics
The 2025 pharmacovigilance landscape increasingly leverages real-world data (RWD) from electronic health records, medical claims, and patient registries to enhance traditional signal detection methods [62]. Enabled by frameworks such as the FDA's Real-World Evidence Program, this approach addresses limitations of pre-market clinical trials, which are often underpowered to detect rare safety issues [62].
Privacy-preserving record linkage (PPRL) methods, including tokenization, enable longitudinal safety monitoring across disparate data sources while protecting patient confidentiality [62]. This facilitates more comprehensive safety assessment, particularly for rare events, off-label use, and long-term risks that may not emerge during clinical development.
Artificial intelligence and machine learning are revolutionizing signal detection capabilities. Natural language processing (NLP) algorithms extract safety information from unstructured clinical notes and narrative case reports, while machine learning models identify complex patterns across multiple data sources simultaneously [26]. These advanced analytics enable detection of subtle associations that traditional methods might miss.
Figure 1: Integrated Signal Detection and Management Workflow
Signal Validation and Prioritization Frameworks
Validation Protocols and Criteria
Signal validation determines whether a statistical association warrants further investigation through systematic assessment of multiple factors [60]:
- Strength of Association: Statistical significance and magnitude of disproportionality measures
- Biological Plausibility: Consistency with known pharmacological mechanisms or drug class effects
- Temporal Relationship: Logical sequence between drug exposure and event onset
- Dechallenge/Rechallenge Data: Event resolution upon discontinuation and recurrence upon re-exposure
- Consistency Across Sources: Reproducibility of the signal in multiple databases or study designs
Prioritization Matrices and Risk Assessment
Validated signals undergo triage to allocate limited resources effectively. Prioritization considers [60]:
- Clinical Severity: Seriousness of the adverse event (fatality, hospitalization, disability)
- Population Impact: Number of patients exposed and vulnerability of affected population
- Preventability: Availability of risk mitigation strategies or monitoring approaches
- Therapeutic Context: Benefit-risk profile considering available alternatives
Table 2: Signal Prioritization Matrix Based on Severity and Population Impact
| Severity/Population Impact | Low Exposure | Medium Exposure | High Exposure |
|---|---|---|---|
| Minor/Reversible Events | Low Priority | Medium Priority | Medium Priority |
| Serious Medical Events | Medium Priority | High Priority | High Priority |
| Life-Threatening/Death | High Priority | Critical Priority | Critical Priority |
| Unknown Significance | Low Priority | Medium Priority | High Priority |
Comparative Safety Assessment: Novel vs. Established Drug Classes
Methodological Framework for Comparative Studies
Robust comparative safety assessment requires carefully designed methodologies to minimize confounding and bias. The following experimental protocol exemplifies approaches used in recent comparative effectiveness research:
Table 3: Experimental Protocol for Comparative Safety Studies
| Study Component | Protocol Specification | Rationale |
|---|---|---|
| Data Sources | EHR databases mapped to OMOP CDM v5.3 from multiple healthcare systems | Ensures standardized data structure and interoperability |
| Study Population | Patients with specific conditions (e.g., T2D + hypertension) initiating second-line therapy after metformin | New-user design minimizes confounding by indication |
| Exposure Cohorts | Non-overlapping cohorts for each drug class (e.g., SGLT2is, GLP-1 RAs, DPP4is, SUs, insulin) | Enables head-to-head comparisons between therapeutic options |
| Outcome Measures | Primary: 3-point MACE (MI, stroke, cardiac death); Secondary: Safety outcomes (CKD, etc.) | Comprehensive assessment of cardiovascular and safety endpoints |
| Statistical Analysis | Propensity score matching with Cox proportional hazards models; IPTW sensitivity analysis | Addresses confounding; tests robustness of findings |
| Covariate Balance | Standardized mean differences (SMD < 0.1) indicating negligible imbalance | Ensures comparability between treatment cohorts |
This methodological framework was implemented in a recent multicenter analysis comparing cardiovascular outcomes of hypoglycemic agents in patients with type 2 diabetes and hypertension [63]. The study demonstrated superior cardiovascular safety profiles for novel drug classes (GLP-1 RAs, DPP4is) compared to traditional therapies (insulin, sulfonylureas), with GLP-1 RAs showing a 52% lower risk of 3-point MACE compared to insulin (HR: 0.48 [0.31–0.76]) [63].
Case Study: AML Therapeutics Safety Profile Evolution
The comparative safety landscape is well-illustrated by developments in acute myeloid leukemia (AML) therapeutics. Novel menin inhibitors have demonstrated consistent clinical benefit with acceptable safety profiles in relapsed/refractory AML, leading to regulatory approval [3]. In contrast, CD47 inhibitor programs showed promising preclinical results but failed in phase 3 trials due to significant toxicity issues, particularly severe anemia, without corresponding survival benefits [3]. This contrast underscores the critical importance of rigorous clinical testing and the reality that promising laboratory results do not always predict clinical safety success.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Solutions for Signal Detection and Management
| Tool/Solution | Function | Application Context |
|---|---|---|
| OMOP Common Data Model | Standardized structure for heterogeneous healthcare data | Enables large-scale analytics across multiple databases |
| Standardized MedDRA Queries (SMQs) | Predefined groupings of related MedDRA terms | Streamlines analysis of large datasets with coding consistency |
| Privacy-Preserving Record Linkage (PPRL) | Tokenization methods for data linkage | Enables longitudinal follow-up while protecting patient privacy |
| Federated Analysis Networks | Distributed analytics without data centralization | Supports multi-database studies (e.g., OHDSI, Sentinel Initiative) |
| Signal Management Platforms | End-to-end workflow systems for signal tracking | Ensures auditability and compliance with regulatory requirements |
| Natural Language Processing (NLP) | Text mining of unstructured clinical narratives | Extracts safety information from clinical notes and case reports |
Regulatory Frameworks and Compliance Considerations
Evolving Global Standards
Regulatory authorities worldwide have strengthened expectations for signal detection and management. The FDA's Sentinel Initiative leverages RWD for active surveillance, while the EMA's EudraVigilance system enables advanced signal detection across member states [26]. The ICH E2E and GVP Module IX guidelines provide harmonized frameworks for pharmacovigilance planning and signal management [60].
Regulatory mandates require pharmaceutical companies to maintain comprehensive signal detection processes with full traceability and auditability. The FDA requires prompt communication of validated signals through 15-day "Alert Reports," while the EMA expects documented signal tracking and periodic assessment in Periodic Safety Update Reports (PSURs) and Risk Management Plans (RMPs) [60].
Figure 2: Regulatory Evidence Generation and Submission Framework
Effective signal detection and management requires a balanced integration of traditional pharmacovigilance methods with innovative approaches leveraging real-world data and advanced analytics. The strategic prioritization of signals demands both quantitative rigor and clinical judgment to distinguish meaningful safety findings from statistical noise. As regulatory expectations evolve and data sources expand, the framework for signal management will continue to incorporate more sophisticated methodologies while maintaining focus on patient safety. The comparative assessment of novel versus established drug classes exemplifies the critical importance of robust signal detection in characterizing the evolving benefit-risk profiles of therapeutic interventions throughout their lifecycle.
In the modern drug development landscape, characterizing a novel therapeutic's safety profile is insufficient; it must be contextualized against established treatment alternatives to inform regulatory decisions, clinical use, and risk-benefit assessments. This comparative approach moves beyond isolated safety reporting to generate evidence that directly positions a new drug within the existing therapeutic armamentarium. For researchers and drug development professionals, executing robust safety benchmarking requires a sophisticated understanding of evolving regulatory frameworks, advanced methodological approaches, and the strategic application of large-scale real-world data. The process is particularly critical when introducing novel drug classes with mechanisms of action distinct from conventional treatments, as it helps delineate unique safety signals from class-effects and identifies potential therapeutic advantages for specific patient populations. This guide synthesizes current methodologies, regulatory expectations, and practical protocols for conducting rigorous comparative safety analyses that meet the evidential standards of both regulatory agencies and the scientific community.
Regulatory and Methodological Foundations
Evolving Regulatory Frameworks for Safety Assessment
Global regulatory science initiatives are continuously refining requirements for comparative drug safety assessment. The U.S. Food and Drug Administration's (FDA) Generic Drug User Fee Amendments (GDUFA) Science and Research Program exemplifies this evolution, emphasizing "innovative methodologies and design recommendations for demonstrating therapeutic equivalence" and addressing "common regulatory challenges and solutions for generic products with complex drug substances, excipients, and formulations" [64]. While initially focused on generics, these methodological advances influence comparative assessment paradigms for all drug classes. Similarly, the European Medicines Agency (EMA) operates under Directive 2001/83/EC, which establishes requirements for generic medicines and hybrid applications that rely in part on existing safety and efficacy data [65]. Understanding these frameworks is essential for designing compliant safety benchmarking studies that adequately address regional regulatory requirements while generating globally relevant evidence.
Foundational Concepts in Safety Benchmarking
Therapeutic Equivalence and Bioequivalence: The foundational principle for generic drugs establishes that pharmaceutical equivalents must demonstrate comparable rate and extent of absorption without significant formulation-related safety or efficacy differences [65] [66]. This concept, while directly applicable to generics, informs broader thinking about clinical interchangeability.
Authorized Generics Distinction: It is crucial to differentiate between true generic drugs and "authorized generics," which are the brand-name product marketed without the brand name on its label [67]. While authorized generics are therapeutically equivalent to their branded counterparts by definition, they differ from ANDA-approved generics which must demonstrate bioequivalence through rigorous testing.
Safety Signal Detection: Defined as information that suggests a new potentially causal association or aspect of this association between an intervention and an event or set of related events, either adverse or beneficial, that is judged to be of sufficient likelihood to justify verificatory action [68]. Modern signal detection has evolved from passive surveillance to proactive, predictive analysis using advanced computational methods.
Methodological Approaches to Safety Benchmarking
Disproportionality Analysis Using Spontaneous Reporting Systems
The FDA Adverse Event Reporting System (FAERS) database represents a cornerstone resource for post-marketing safety surveillance and comparative risk assessment. A recent study analyzing the safety profiles of bevacizumab versus alkylating agents (temozolomide and lomustine) in glioblastoma management demonstrates the application of this methodology [68]. The research design incorporated data from 49,368,071 adverse event reports spanning Q1 2004 to Q4 2023, with specific focus on glioblastoma indications.
Experimental Protocol: FAERS Disproportionality Analysis
Data Acquisition and Processing: Extract demographic, drug, adverse event, outcome, and indication data from FAERS. Implement robust de-duplication following FDA guidelines: retain most recent report for identical CASEIDs; when CASEID and FDA_DT identical, select record with larger PRIMARYID [68].
Study Population Definition: Isolate reports where drug indication is specifically recorded as glioblastoma. Include only reports where "role_cod" is "Primary Suspect" or "Secondary Suspect" to ensure drug-event relatedness.
Statistical Analysis - Reporting Odds Ratio (ROR):
- Construct 2×2 contingency tables comparing target drug events to other drug events
- Calculate ROR = (a/c)/(b/d), where:
- a = reports of target event with target drug
- b = reports of other events with target drug
- c = reports of target event with other drugs
- d = reports of other events with other drugs
- Compute 95% confidence interval: e^[ln(ROR) ± 1.96√(1/a + 1/b + 1/c + 1/d)]
- Signal detection threshold: lower bound of 95% CI >1 with ≥3 cases [68]
Clinical Interpretation: Compare safety signals at both System Organ Class and Preferred Term levels using Medical Dictionary for Regulatory Activities terminology.
Table 1: Key Demographic Characteristics from FAERS Analysis of Glioblastoma Therapies
| Characteristic | Bevacizumab (n=3,323) | Temozolomide (n=5,283) | Lomustine (n=427) |
|---|---|---|---|
| Male Patients | 47.2% | 45.1% | 46.4% |
| Age Distribution | Primarily 18-75 years | Primarily 18-75 years | Primarily 18-75 years |
| Primary Reporter | Physicians | Physicians | Physicians |
| Top Reporting Country | United States | United States | United States |
Table 2: Comparative Adverse Event Profiles from FAERS Analysis (Q1 2004 - Q4 2023)
| Drug | Most Frequent Adverse Events | Signal Strengths (vs. Comparator) | Safety Advantages |
|---|---|---|---|
| Bevacizumab | Fatigue (n=276), Hypertension (n=220), Headache (n=199) | Stronger association with "vascular disorders," "renal and urinary disorders," "hypertension" vs. temozolomide | Lower incidence of hematological adverse events |
| Temozolomide | Thrombocytopenia (n=581), Disease progression (n=475), Drug ineffectiveness (n=356) | N/A (used as reference) | N/A |
| Lomustine | Thrombocytopenia, Neutropenia, Leukopenia | Not included in comparative analysis due to limited reports | N/A |
Incorporating Advanced Technologies in Safety Assessment
The field of pharmacovigilance is undergoing rapid transformation through technological innovation. Artificial intelligence and machine learning are being deployed to augment human expertise in safety monitoring, achieving "greater efficiency, accuracy, and compliance in safety monitoring processes" [69]. The integration of quantum computing in 2024 marked a significant advancement, enabling systems to "process complex biological interactions and potential adverse effects in minutes rather than months" with reported 98% accuracy rates in early signal detection [70]. These technologies facilitate more sophisticated comparative analyses by identifying complex patterns across multidimensional data that traditional methods might miss.
The emergence of the Global Safety Database Network in late 2024 has created unprecedented opportunities for real-time safety signal sharing across continents, using blockchain technology to ensure data integrity while facilitating instant information exchange [70]. This interconnected network enables researchers to benchmark safety profiles against global datasets rather than regionally limited samples.
Experimental Design and Visualization
Safety Benchmarking Workflow
The following diagram illustrates the comprehensive workflow for conducting comparative drug safety analysis, integrating both traditional and advanced methodological approaches:
FAERS Data Analysis Methodology
The detailed process for extracting, processing, and analyzing FAERS data follows this specific pathway to ensure regulatory-grade results:
Table 3: Essential Research Resources for Comparative Drug Safety Analysis
| Resource/Solution | Function in Safety Benchmarking | Application Example |
|---|---|---|
| FDA Adverse Event Reporting System (FAERS) | Spontaneous reporting database for post-marketing surveillance | Detecting disproportionate reporting of adverse events for specific drug classes [68] |
| MedDRA (Medical Dictionary for Regulatory Activities) | Standardized terminology for adverse event classification | Coding AEs at System Organ Class and Preferred Term levels for consistent analysis [68] |
| Orange Book (FDA) | Identifies therapeutic equivalence evaluations | Determining reference listed drugs and approved alternatives for comparison [71] |
| Authorized Generic Drug Database (FDA) | Lists brand-name drugs marketed without brand name | Differentiating authorized generics from ANDA-approved generics in analyses [67] |
| Quantum-Enhanced AI Systems | Advanced signal detection through computational power | Predicting potential safety signals before clinical manifestation [70] |
| Global Safety Database Network | International safety data sharing platform | Benchmarking against global safety profiles rather than regional data [70] |
| R Statistical Software | Open-source environment for disproportionality analysis | Calculating reporting odds ratios and confidence intervals [68] |
Contextualizing a novel drug's safety profile against established therapeutic classes requires methodologically sound approaches that leverage both traditional pharmacovigilance tools and emerging technologies. The FAERS disproportionality analysis demonstrated with glioblastoma therapies provides a validated framework for quantitative safety comparison, while advanced technologies like AI and quantum computing offer transformative potential for predictive safety analytics. As regulatory science continues to evolve—exemplified by initiatives like the FDA's GDUFA program—successful safety benchmarking will depend on researchers' ability to integrate multidimensional evidence within robust methodological frameworks. The resulting comparative safety profiles not only inform regulatory decisions but ultimately enhance therapeutic individualization by identifying distinct risk-benefit considerations for specific patient populations.
In the dynamic landscape of drug development, understanding and managing the safety profiles of novel therapeutic agents compared to established treatments is paramount for researchers and development professionals. The transition from controlled clinical trials to real-world application often reveals unforeseen safety challenges that require sophisticated mitigation strategies. This guide objectively compares the safety performance of various drug classes across therapeutic areas, examining how identified risks are managed throughout the product lifecycle. By analyzing direct comparative evidence, we aim to illuminate the evolving nature of drug safety profiling and the strategic implementation of risk mitigation frameworks that protect patients while maximizing therapeutic benefits.
Case Study 1: Cardiovascular Safety in Antidiabetic Therapies
Experimental Methodology
This multicenter cohort study employed a retrospective, comparative new-user design analyzing electronic health records from two databases mapped to the Observational Medical Outcome Partnership Common Data Model [63]. The study population included adults with type 2 diabetes and hypertension who had previously received metformin monotherapy and subsequently initiated a second-line antidiabetic agent from one of seven major drug classes: insulin, sulfonylureas (SUs), glucagon-like peptide-1 receptor agonists (GLP-1 RAs), dipeptidyl peptidase-4 inhibitors (DPP4is), glinides, acarbose, and sodium-glucose transporter 2 inhibitors (SGLT2is) [63].
To address confounding, researchers developed propensity score models via logistic regression for each drug class pair, incorporating demographic, clinical, and medical history covariates. Variable-ratio propensity score matching used a nearest neighbor algorithm with a caliper of 0.02 standard deviations. Covariate balance was assessed using standardized mean differences (<0.1 indicating negligible imbalance). Kaplan-Meier curves visualized cumulative incidence proportions, and Cox proportional hazards models estimated hazard ratios with 95% confidence intervals for 17 predefined effectiveness and safety outcomes [63].
Comparative Safety and Efficacy Data
Table 1: Cardiovascular Outcomes for Antidiabetic Medications in T2D Patients with Hypertension
| Drug Class Comparison | Hazard Ratio (HR) | 95% Confidence Interval | Outcome Measure |
|---|---|---|---|
| GLP-1 RAs vs. Insulin | 0.48 | 0.31-0.76 | 3-point MACE |
| DPP4is vs. Insulin | 0.70 | 0.57-0.85 | 3-point MACE |
| Glinides vs. Insulin | 0.70 | 0.52-0.94 | 3-point MACE |
| SUs vs. DPP4is | 1.30 | 1.06-1.59 | 3-point MACE |
| DPP4is vs. Acarbose | 0.62 | 0.51-0.76 | 3-point MACE |
| GLP-1 RAs vs. Acarbose | 0.47 | 0.29-0.75 | 3-point MACE |
Table 2: Safety Outcomes for Antidiabetic Medications in T2D Patients with Hypertension
| Drug Class | Safety Outcomes |
|---|---|
| DPP4is | Associated with reduced risk of chronic kidney disease |
| Insulin | Associated with reduced risks of inflammatory polyarthritis and insomnia |
| DPP4is | Associated with higher risks of coronary atherosclerotic diseases and hypertensive heart disease |
Risk Mitigation Framework
For antidiabetic medications with identified cardiovascular risks, several mitigation strategies have been implemented in clinical practice. These include enhanced cardiovascular monitoring for patients on medications with higher MACE risk, regular renal function assessments for patients on nephroprotective agents, and consideration of individual patient risk factors when selecting therapeutic regimens. The comparative safety data enables clinicians to tailor treatment approaches that maximize glycemic control while minimizing cardiovascular complications in this high-risk population [63].
Case Study 2: Safety Evolution of Biologics in Rheumatoid Arthritis
Experimental Methodology
A nationwide register-based cohort study was conducted from 2006 to 2022 using the Swedish Rheumatology Quality Register and national registers [4]. Researchers identified 33,550 treatment initiations of biologic/targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs), along with an early bionaive rheumatoid arthritis cohort (n = 16,011) and a matched general population cohort (n = 111,074) [4].
The primary outcome was the first occurrence of a major adverse cardiovascular event, venous thromboembolism, cancer, or serious infection. Investigators stratified rates by time since market entry of each b/tsDMARD class at treatment initiation and by calendar year of treatment initiation. They calculated incidence rates and hazard ratios using Cox regression with adjustment for patient characteristics, examining 5,862 observed events in the b/tsDMARD initiator cohort [4].
Comparative Safety Data
Table 3: Safety Outcomes for b/tsDMARDs Based on Time Since Market Entry
| Time Since Market Entry | Unadjusted HR | 95% CI | Adjusted HR | 95% CI | Outcome |
|---|---|---|---|---|---|
| >5 years vs. <2 years | 0.74 | 0.67-0.81 | 0.93 | 0.84-1.03 | Composite safety outcome |
| 2016-2021 vs. 2006-2010 | - | - | 0.74 | 0.69-0.80 | Composite safety outcome |
Risk Mitigation and Evolution
The study revealed that "modest channelling makes the safety profile of b/tsDMARDs appear worse when new on the market" [4]. This phenomenon, where newer drugs are initially prescribed to patients with more severe disease or comorbidities, creates the appearance of worse safety profiles that attenuate as prescribing expands to broader populations. Additionally, declining incidences of typical RA comorbidities in b/tsDMARD initiators during recent years suggest that "the bar defining an 'acceptable' safety profile for new b/tsDMARDs for use in RA should be lower(ed)" [4]. This indicates that real-world evidence gathered over time provides a more accurate safety profile than initial post-market data alone.
Case Study 3: Novel Agents in Acute Myeloid Leukemia
Experimental Methodology
Clinical development programs for novel AML agents have employed traditional phase 3 randomized controlled trials comparing new targeted agents against established standard-of-care regimens [3]. For menin inhibitors, studies focused on specific genetic subtypes (particularly NPM1-mutated and KMT2A-rearranged AML) in relapsed/refractory settings. These trials incorporated rigorous safety monitoring for on-target toxicities and mechanism-based adverse effects, with response assessment by standardized hematologic criteria [3].
Similarly, CD47 inhibitor trials employed standard oncology trial designs but faced unique challenges in assessing the risk-benefit balance due to significant toxicity issues that emerged during later-stage testing. The contrasting outcomes between these drug classes provide valuable insights into predictive safety modeling and risk mitigation in oncology drug development [3].
Comparative Efficacy and Safety Data
Table 4: Comparison of Novel AML Therapeutic Agents
| Drug Class | Mechanism of Action | Efficacy Findings | Safety Findings | Development Status |
|---|---|---|---|---|
| Menin Inhibitors | Blocks menin-KMT2A/MLL interaction | Consistent clinical benefit across compounds in class | Manageable safety profile | Approved for R/R AML |
| CD47 Inhibitors | Inhibits "don't eat me" signal on cancer cells | Failed to demonstrate meaningful clinical benefit in Phase 3 | Significant toxicity issues, particularly severe anemia | Multiple programs discontinued |
Risk Mitigation Strategies
The successful development of menin inhibitors exemplifies targeted risk mitigation through patient selection based on specific genetic alterations, which enriched for responsive populations while limiting exposure in those unlikely to benefit. In contrast, CD47 inhibitors faced challenges despite promising preclinical results, highlighting that "promising laboratory results don't always predict clinical success for patients" [3]. This case underscores the importance of early toxicity detection and the potential limitations of preclinical models in predicting human safety profiles, especially for novel mechanisms of action.
Case Study 4: REMS Implementation for Antipsychotic Therapy
Experimental Protocol
Zyprexa Relprevv (olanzapine) provides a documented example of Risk Evaluation and Mitigation Strategies (REMS) implementation for managing a specific, serious drug risk [72]. The drug can cause serious reactions following injection called post-injection delirium sedation syndrome, with symptoms including profound sedation, coma, and delirium occurring within 3 hours after administration [72].
To mitigate this risk, the FDA required the manufacturer to develop a REMS program focusing on administrative controls rather than altering the drug's chemical properties. The REMS mandates that the drug be administered only in certified healthcare facilities with immediate access to emergency response services [72].
Risk Mitigation Outcomes
The Zyprexa Relprevv REMS program demonstrates several key risk mitigation principles: (1) targeted intervention for specific serious risks rather than all potential adverse events; (2) environmental controls through restricted administration settings; (3) professional education and certification requirements; and (4) structured post-marketing monitoring [72]. This approach has enabled continued availability of a therapeutically beneficial agent while managing a potentially life-threatening adverse effect that occurs with every injection, albeit at a low frequency (less than 1%) [72].
Visualizing Safety Signal Detection Workflows
AI-Enhanced Pharmacovigilance Pathway
REMS Implementation Logic
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 5: Key Reagents for Comparative Drug Safety Research
| Research Tool | Application in Safety Research | Example Use Case |
|---|---|---|
| OMOP Common Data Model | Standardizes electronic health record data across institutions for large-scale safety studies | Enabled multicenter analysis of antidiabetic drug safety [63] |
| Propensity Score Matching Algorithms | Balances covariates across treatment cohorts in observational studies to reduce confounding | Compared cardiovascular outcomes across diabetes drug classes [63] |
| Natural Language Processing (NLP) Tools | Extracts adverse event information from unstructured clinical notes and patient reports | Identified adverse drug reactions from EHR clinical narratives [5] |
| Knowledge Graphs | Represents complex relationships between drugs, adverse events, and patient factors | Classified known causes of ADRs with 0.92 AUC [5] |
| REMS Framework | Structured risk management program for drugs with serious safety concerns | Managed post-injection delirium risk with Zyprexa Relprevv [72] |
The comparative analysis of safety risk mitigation across therapeutic areas reveals several consistent themes. First, real-world evidence gathered through robust observational study designs provides critical insights that complement pre-marketing clinical trials [4] [63]. Second, targeted risk minimization strategies such as REMS programs can successfully manage specific serious risks while preserving patient access to beneficial therapies [72]. Third, artificial intelligence and advanced analytics are transforming safety signal detection, enabling more proactive risk identification across diverse data sources [73] [5] [26]. Finally, the evolution of safety profiles over time necessitates continuous monitoring and reassessment of risk-benefit balances throughout a product's lifecycle [4] [26]. These case studies demonstrate that effective safety risk mitigation requires multidisciplinary approaches integrating rigorous methodology, technological innovation, and thoughtful regulatory frameworks to protect patient welfare while advancing therapeutic options.
Validating and Comparing Safety Data Across Drugs and Regulatory Landscapes
The management of type 2 diabetes has undergone a paradigm shift, moving beyond glycemic control to encompass comprehensive cardiovascular and renal risk reduction. This evolution has been driven by the introduction of novel drug classes, notably sodium-glucose cotransporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 receptor agonists (GLP-1 RAs), which demonstrate significant cardiorenal benefits alongside their glucose-lowering effects. Understanding the comparative safety profiles of these therapeutic classes is crucial for optimizing treatment strategies in high-risk patient populations. This guide provides a systematic, evidence-based comparison of contemporary diabetes therapies, with a specific focus on their head-to-head cardiovascular and renal safety profiles, to inform researchers, scientists, and drug development professionals.
Quantitative Outcomes: Comparative Efficacy Data
Table 1: Network Meta-Analysis of Cardiovascular and Renal Outcomes (T2DM with CKD) [74]
| Outcome | SGLT2 Inhibitors (P-score) | GLP-1 RAs (P-score) | DPP-4 Inhibitors |
|---|---|---|---|
| Composite Renal Outcome | 0.94 (Superior) | Lower benefit | Limited benefits |
| eGFR decline >40% or RRT | 0.99 (Superior) | Lower benefit | Limited benefits |
| MACE | 0.93 (Superior) | Lower benefit | Limited benefits |
| Hospitalization for Heart Failure | 1.00 (Superior) | Lower benefit | Limited benefits |
| Myocardial Infarction | Lower benefit | 0.87 (Superior) | Limited benefits |
| Stroke | Lower benefit | 0.83 (Superior) | Limited benefits |
| All-cause Mortality | 0.83 (Highly Effective) | 0.83 (Highly Effective) | Limited benefits |
Table 2: Observational Study Data on GLP-1 RA Combination Therapy vs. Monotherapy (Hazard Ratios) [75]
| Outcome | GLP-1 RA + SGLT2i vs. SGLT2i Monotherapy | GLP-1 RA + SGLT2i vs. GLP-1 RA Monotherapy |
|---|---|---|
| MACE | 0.59 (95% CI 0.47–0.75) | Not Significant |
| Myocardial Infarction | 0.73 (95% CI 0.61–0.88) | 0.93 (95% CI 0.88–0.97) |
| Stroke | 0.72 (95% CI 0.53–0.97) | 0.92 (95% CI 0.88–0.96) |
| All-cause Mortality | 0.57 (95% CI 0.48–0.67) | 0.59 (95% CI 0.49–0.70) |
| HF Hospitalization/Events | 0.71 (95% CI 0.59–0.86) | 0.84 (95% CI 0.81–0.88) |
| CV Mortality | Not Significant | 0.35 (95% CI 0.15–0.81) |
| Serious Renal Events | Not Reported | 0.43 (95% CI 0.23–0.80) |
Mechanistic Insights: Signaling Pathways and Molecular Targets
SGLT2 inhibitors and GLP-1 RAs provide cardiorenal protection through distinct yet potentially complementary mechanisms. SGLT2 inhibitors act primarily on the proximal tubule of the kidney, while GLP-1 RAs exert systemic effects via receptor-mediated signaling pathways.
Diagram 1: Distinct mechanistic pathways of SGLT2 inhibitors and GLP-1 receptor agonists. SGLT2 inhibitors act primarily on renal tubules to promote glucosuria and natriuresis, while GLP-1 RAs exert multi-system effects through receptor binding.
SGLT2 Inhibitor-Specific Pathways
The cardiorenal benefits of SGLT2 inhibitors extend beyond glycemic control through multiple interconnected pathways. The inhibition of sodium and glucose reabsorption in the proximal tubule promotes natriuresis and osmotic diuresis, reducing plasma volume and blood pressure [76]. This leads to a restoration of the tubuloglomerular feedback mechanism, reducing intraglomerular pressure and kidney hyperfiltration, a key factor in their renoprotective effect [77]. Additionally, SGLT2 inhibition shifts myocardial and renal fuel metabolism from fatty acids and glucose to ketone bodies, improving energy efficiency and reducing oxidative stress [77]. They also suppress the activation of the sympathetic nervous system and inflammatory pathways, contributing to overall cardiovascular protection.
GLP-1 Receptor Agonist-Specific Pathways
GLP-1 RAs mediate their effects through binding to widely distributed GLP-1 receptors. Their cardiovascular benefits are largely attributed to direct and indirect atheroprotective effects. They reduce postprandial lipemia, inhibit macrophage activation and plaque formation, and decrease vascular inflammation [78]. GLP-1 RAs also promote weight loss through central effects on appetite regulation and slow gastric emptying. Furthermore, they have been shown to reduce blood pressure via mechanisms that may include natriuresis and improved endothelial function. Their renal benefits may be secondary to improved glycemic control, weight loss, and blood pressure reduction, as well as potential direct anti-inflammatory effects on the kidney [78].
Experimental Protocols: Methodologies for Head-to-Head Comparison
Robust evaluation of cardiorenal safety requires well-designed clinical trials and sophisticated analysis of real-world data. The following protocols detail the methodologies generating the comparative evidence.
Network Meta-Analysis Protocol
Objective: To compare the relative efficacy of SGLT2 inhibitors, GLP-1 RAs, and DPP-4 inhibitors on cardiovascular and renal outcomes in patients with type 2 diabetes and chronic kidney disease.
Search Strategy: A systematic literature search was performed in electronic databases including PubMed, Scopus, and clinical trial registries for randomized controlled trials (RCTs) published between 2014 and 2024 [74].
Inclusion Criteria:
- Population: Adults with T2DM and CKD.
- Intervention: SGLT2 inhibitors, GLP-1 RAs, or DPP-4 inhibitors.
- Comparator: Placebo or active comparator.
- Outcomes: Primary outcomes included (1) major adverse CV events (MACE), (2) composite renal outcomes, (3) all-cause mortality. Secondary outcomes included heart failure, stroke, and progression of albuminuria.
Data Extraction and Analysis: Two reviewers independently extracted data. A frequentist network meta-analysis was performed within a multivariate random-effects meta-analysis framework. Treatments were ranked using P-scores, which measure the extent of certainty that one treatment is better than another. Statistical inconsistency was assessed using the design-by-treatment interaction model.
Real-World Comparative Effectiveness Study Protocol
Objective: To compare the kidney, cardiovascular, and mortality risks of three different GLP-1 RAs (liraglutide, semaglutide, and dulaglutide) in a routine care setting.
Data Source: Retrospective analysis of the Veterans Affairs health system data, a comprehensive source of patient and medication information [78].
Study Population: 21,790 veterans with type 2 diabetes. The population was predominantly older white males.
Exposure and Comparison: Patients were categorized based on initiation of liraglutide, semaglutide, or dulaglutide.
Outcomes: Incident cardiovascular events, kidney outcomes, and all-cause mortality.
Statistical Analysis: To account for confounding, researchers used inverse probability of treatment weighting based on propensity scores. Hazard ratios with 95% confidence intervals were calculated for the outcomes comparing the different GLP-1 RAs.
Limitations: The observational nature prevents definitive causal inference, and results may not be fully generalizable to non-veteran or more diverse populations [78].
Combination Therapy: Synergistic Potential and Workflow
Emerging evidence suggests that combination therapy with SGLT2 inhibitors and GLP-1 RAs may provide additive cardiorenal benefits, leveraging their distinct mechanisms of action.
Table 3: Analysis of Dual-Agent Combination Therapies [75]
| Therapy Combination | Compared to Monotherapy | Key Outcome Benefits (Hazard Ratio) |
|---|---|---|
| GLP-1 RA + SGLT2i | SGLT2i monotherapy | MACE: 0.59; All-cause Mortality: 0.57; HF Hosp: 0.71 |
| GLP-1 RA + SGLT2i | GLP-1 RA monotherapy | CV Mortality: 0.35; Serious Renal Events: 0.43; All-cause Mortality: 0.59 |
| SGLT2i + Finerenone | SGLT2i or Finerenone monotherapy | Reduced all-cause mortality and major adverse kidney events |
Diagram 2: A strategic workflow for evaluating and implementing combination SGLT2 inhibitor and GLP-1 RA therapy in clinical practice or trial design, based on individual patient risk profiles.
Evidence from both RCTs and large real-world cohorts indicates that the combination of an SGLT2 inhibitor and a GLP-1 RA confers cardiorenal protection beyond that achieved with either agent alone [75]. A meta-analysis of observational studies found that compared to SGLT2i monotherapy, the combination with a GLP-1 RA significantly reduced the risk of MACE, all-cause mortality, and heart failure hospitalization. Similarly, when compared to GLP-1 RA monotherapy, the combination significantly reduced the risk of cardiovascular mortality and serious renal events. The complementary mechanisms of these two drug classes provide a physiological basis for these additive benefits, suggesting that their effects on different pathways create a synergistic protective profile.
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Reagents and Resources for Cardiorenal Outcomes Research
| Reagent / Resource | Primary Function | Application Example |
|---|---|---|
| Randomized Controlled Trial (RCT) Databases | Provides gold-standard efficacy and safety data from controlled settings. | Network meta-analyses (e.g., [74]); Drug approval applications. |
| Real-World Data (RWD) Repositories | Offers insights into long-term effectiveness and safety in diverse populations. | VA health system data for GLP-1 RA comparison [78]. |
| Network Meta-Analysis Software (R packages) | Enables statistical comparison of multiple treatments across different trials. | Frequentist NMA to generate P-scores and treatment rankings [74]. |
| Propensity Score Matching/Weighting Methods | Reduces confounding in observational studies to approximate randomization. | Comparing outcomes between drug initiators in electronic health records [78]. |
| Serum and Urine Biomarker Assays | Quantifies renal function and damage (e.g., eGFR, UACR). | Measuring albuminuria progression in CKD trials [74] [79]. |
| Major Adverse Cardiovascular Events (MACE) Adjudication Committees | Standardizes and validates cardiovascular endpoint classification in trials. | Ensuring consistent MACE definition across multi-center trials. |
| Major Adverse Kidney Events (MAKE) Composite Endpoints | Standardizes assessment of hard renal outcomes in clinical trials. | Combining ESRD, eGFR decline, and renal/CV death [75]. |
For researchers and drug development professionals, the drug label serves as a primary tool for communicating critical scientific information necessary for the safe and effective use of pharmaceuticals [80]. In an era of global drug development, where safety information is gathered from multiple regions, the scientific content in drug labeling is expected to represent the most current and consistent information across countries where medicines are approved [80]. This analysis examines the concordance of safety-related information in product labeling for novel therapeutics concurrently approved in Japan and the United States, framing this discordance within broader research on comparative safety profiles of novel versus established drug classes.
International inconsistencies in drug labeling present potential risks to patients in countries where accurate or up-to-date information is not fully available [80]. Previous studies have noted concerning discrepancies in safety information across regulatory jurisdictions. For instance, a comparison of drug labeling between Denmark and the US revealed low consistency in information related to adverse drug reactions [80] [81]. The present analysis builds upon this research by systematically investigating concordance patterns between two major regulatory authorities – Japan's Pharmaceuticals and Medical Devices Agency (PMDA) and the US Food and Drug Administration (FDA) – focusing specifically on new active substances approved within a closely aligned timeframe.
Methodological Framework
Study Design and Drug Selection
This analysis is based on a systematic review of all new active substances (NASs) approved in Japan between 2014 and 2020 that were also approved in the US within 6 months from the date of Japanese approval [80]. From 271 NASs approved in Japan during this period, 182 were also approved in the US, with 45 drugs meeting the criterion of concurrent approval (within 6 months) and forming the final study cohort [80].
The Anatomical Therapeutic Chemical (ATC) classification system was used to categorize the included drugs, with Level L (antineoplastic and immunomodulating agents) representing the most common category at approximately 44.4% (20/45) of all included drugs [80]. Nine of the 45 drugs were identified as first-in-class (FIC) drugs, and the marketing authorization holder (MAH) was the same in both countries for 35 out of 45 drugs [80].
Data Collection and Concordance Assessment
Safety-related information was defined as safety event terms described in any of the safety-related sections in drug labeling [80]. For Japanese labeling, these sections included: WARNINGS, CONTRAINDICATIONS, PRECAUTIONS CONCERNING INDICATIONS, PRECAUTIONS CONCERNING DOSAGE AND ADMINISTRATION, IMPORTANT PRECAUTIONS, INTERACTIONS, and ADVERSE REACTIONS [80]. For US labeling, the sections included: BOXED WARNING, CONTRAINDICATIONS, WARNINGS AND PRECAUTIONS, ADVERSE REACTIONS, and DRUG INSTRUCTIONS [80].
Each identified item of safety-related information was reviewed for concordance between the two countries using the Medical Dictionary for Regulatory Activities (MedDRA)/J version 23.0 [80]. Safety event terms were first coded to MedDRA Low Level Terms, with concordance assessed using Preferred Terms (PT). Concordant safety-related information was defined as an exact match of drug-safety-related term between the two countries [80]. The concordance rate for each NAS was calculated by dividing the number of concordant safety-related terms by the total number of safety-related information raised in either of the two countries.
Statistical Analysis
Factors associated with concordance rate were examined using five groups of explanatory variables: (1) development strategy of the NAS [at least 1 multi-regional clinical trial (MRCT) conducted in both Japan and the US versus no MRCT], (2) ATC classification (L versus others), (3) first-in-class (FIC) drug status (yes/no), (4) country ahead in approval (Japan/the US), and (5) MAH in each country (same/different) [80]. Difference in distribution of concordance rate was analyzed across groups for each variable using the Mann–Whitney U test, with variables with a level of significance p < 0.1 considered to indicate statistical significance [80].
A specialized analysis was conducted for black box warnings (BBW), referred to as "boxed warning" in the US and "warning" in Japan, which represent safety warnings to inform healthcare professionals about fatal or serious adverse reactions [80]. When a BBW was present for a NAS in both countries, the content was reviewed and safety-related information was identified, coded, and assessed for concordance using the same methodology described above.
The following diagram illustrates the complete research workflow for the cross-national labeling analysis:
Quantitative Findings
The analysis revealed a remarkably low level of concordance between Japan and the US in safety information found in drug labeling, with only 20.4% of safety-related terms matching exactly between the two countries for the 45 new active substances studied [80]. This discordance persisted even for clinically critical information highlighted by Black Box Warnings, where the mean concordance rate among the 9 drugs with BBW in both countries was only 32.9% [80].
Table 1: Overall Concordance Rates in Safety Information
| Analysis Category | Number of Drugs | Concordance Rate |
|---|---|---|
| Overall Safety Information | 45 NASs | 20.4% |
| Drugs with Black Box Warnings in Both Countries | 9 NASs | 32.9% |
Factors Influencing Concordance
Statistical analysis identified several factors significantly associated with concordance rates. The development strategy of the drugs, particularly whether at least one multi-regional clinical trial (MRCT) was conducted in both Japan and the US, showed a significant association with concordance rates [80]. Additionally, having the same marketing authorization holder (MAH) in both countries was significantly associated with higher concordance rates [80].
Other factors analyzed included ATC classification (specifically category L for antineoplastic and immunomodulating agents versus others), first-in-class drug status, and which country was ahead in approval, though their specific impact magnitudes were not detailed in the available data [80].
Table 2: Factors Associated with Labeling Concordance
| Factor | Association with Concordance | Statistical Significance |
|---|---|---|
| Development Strategy (MRCT in both countries) | Significant association | p < 0.1 |
| Same Marketing Authorization Holder | Significant association | p < 0.1 |
| ATC Classification (L vs. others) | Analyzed, specific association not detailed | Not specified |
| First-in-Class Drug Status | Analyzed, specific association not detailed | Not specified |
| Country Ahead in Approval | Analyzed, specific association not detailed | Not specified |
The relationship between these factors and labeling concordance can be visualized through the following conceptual framework:
Case Studies in Safety Discordance
Novel Drug Classes and Safety Profile Evolution
The discordance in safety labeling takes on additional significance when considering the evolving understanding of safety profiles for novel drug classes. Recent research on biologic/targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) for rheumatoid arthritis demonstrates that newly marketed drugs may appear to have worse safety profiles due to "modest channelling" – where higher-risk patients may be preferentially prescribed newer treatments [4].
A nationwide register-based cohort study conducted from 2006 to 2022 found that b/tsDMARD treatments initiated >5 years since market entry of that class were associated with lower rates of major adverse cardiovascular events, venous thromboembolism, cancer, or serious infection compared to those initiated <2 years since market entry (unadjusted HR = 0.74; 95% CI = 0.67-0.81) [4]. This association was attenuated after adjusting for patient characteristics (adjusted HR = 0.93; 95% CI = 0.84-1.03), suggesting that initial safety signals may reflect prescribing patterns rather than inherent drug properties [4].
Contrasting Development Pathways: Menin vs. CD47 Inhibitors in AML
The divergent development pathways of menin inhibitors and CD47 inhibitors in acute myeloid leukemia (AML) illustrate how safety considerations manifest differently in labeling across therapeutic classes. Menin inhibitors have emerged as promising treatments for specific genetic subtypes of AML, with the first-in-class menin inhibitor revumenib receiving approval for relapsed/refractory AML [3]. These inhibitors have demonstrated consistent clinical benefit across different compounds in the class, suggesting the pathway represents a genuinely important therapeutic target [3].
In contrast, CD47-targeted therapies showed promising preclinical results but failed to translate into meaningful clinical benefits due to significant toxicity issues, particularly severe anemia [3]. Patients considered for CD47 inhibitor trials faced substantial adverse effect burdens without corresponding survival benefits, leading to the discontinuation of multiple development programs [3]. This experience highlights the importance of rigorous clinical testing and the reality that promising laboratory results do not always predict clinical success for patients, inevitably resulting in divergent safety labeling across regulatory jurisdictions.
Research Toolkit for Labeling Analysis
Table 3: Essential Research Resources for Cross-National Labeling Analysis
| Resource Category | Specific Tools/Databases | Primary Function |
|---|---|---|
| Regulatory Approval Databases | PMDA List of Approved Products [80], FDA Drugs@FDA [80] | Identification of new active substances and approval dates |
| Drug Classification Systems | Anatomical Therapeutic Chemical (ATC) Classification [80] | Standardized categorization of therapeutic products |
| Medical Terminology Coding | Medical Dictionary for Regulatory Activities (MedDRA) [80] | Standardized coding of adverse event terminology |
| Drug Labeling Repositories | SAFE-DI [80], Drugs@FDA [80] | Access to official drug labeling documents |
| Statistical Analysis Software | StatsDirect [80] | Statistical analysis of concordance rates and associated factors |
Implications for Drug Development and Regulation
The low concordance rate between Japan and the US highlights the need for greater transparency in decision-making processes about safety information in drug labeling by both industry and regulators [80]. This transparency is particularly crucial for first-in-class drugs that utilize novel mechanisms of action, as they often lack established safety benchmarks [28]. The year 2025 is poised to see several first-in-class therapy approvals, including donidalorsen for hereditary angioedema, fitusiran for hemophilia A and B, ivonescimab for non-small cell lung cancer, mirdametinib for neurofibromatosis type 1-associated plexiform neurofibromas, and plozasiran for severe hypertriglyceridemia [28]. Each of these novel mechanisms presents unique safety consideration challenges that may contribute to further discordance in international labeling if not addressed systematically.
The findings also underscore the importance of international harmonization initiatives in pharmacovigilance and regulatory science. While scientific, cultural, and regulatory differences between countries may legitimately lead to different safety interpretations and labeling requirements, the substantial discordance observed even for concurrently approved drugs suggests opportunities for improved alignment. This alignment is especially valuable for anticancer and immunomodulating agents, which represented the largest therapeutic category in the study and often have global development and usage patterns [80].
Future research should explore the specific reasons behind discordant safety decisions, including examination of underlying clinical data interpretations, regulatory philosophies, and cultural factors influencing risk-benefit assessments. Such investigations would help establish whether observed discordances represent legitimate differences in scientific interpretation or potentially addressable inconsistencies in regulatory processes.
The safety profile of a pharmaceutical product is not a static label but a dynamic entity that evolves throughout a drug's lifecycle. Long-term safety validation is the critical, ongoing process of tracking and evaluating adverse drug reactions over extended periods and across expanding patient populations. This process is fundamental to understanding how a drug's safety profile stabilizes, providing the comprehensive data necessary for clinicians, regulators, and researchers to accurately assess its benefit-risk balance. The necessity for this longitudinal approach is underscored by the inherent limitations of pre-marketing clinical trials, which, while controlled and rigorous, are often limited in duration, size, and diversity of participants. Consequently, they are ill-equipped to detect rare, latent, or long-term adverse effects that may only become apparent after widespread use in real-world clinical practice [82] [83].
This guide objectively compares the methodologies and evidence generated for evaluating the safety of novel versus established drug classes, framing the discussion within the broader context of comparative safety profile research. The stabilization of a safety profile is not merely the passage of time but a complex process influenced by accumulating patient exposure, refinement of prescribing patterns, and the maturation of post-marketing surveillance data. For drug development professionals, understanding this trajectory is essential for risk management, regulatory strategy, and ultimately, for safeguarding patient health. This article will summarize key quantitative data, detail experimental protocols for safety studies, and provide a toolkit for navigating this complex field.
Comparative Safety Data: Novel vs. Established Drug Classes
Quantitative data from rigorous studies provide the most compelling evidence of how safety profiles evolve. The tables below synthesize findings from recent research, highlighting trends in safety outcomes between newly marketed and well-established pharmaceuticals.
Table 1: Comparative Safety Outcomes for Rheumatoid Arthritis b/tsDMARDs Over Time
| Parameter | Treatment Initiated <2 Years Post-Market | Treatment Initiated >5 Years Post-Market | Statistical Significance |
|---|---|---|---|
| Unadjusted Hazard Ratio (HR) for Composite Safety Outcome* | 1.00 (Reference) | 0.74 | 95% CI: 0.67-0.81 |
| Adjusted Hazard Ratio (HR) for Composite Safety Outcome* | 1.00 (Reference) | 0.93 | 95% CI: 0.84-1.03 |
| Proposed Mechanism for Apparent Risk | Modest channelling of higher-risk patients to newer drugs | Accumulated real-world experience, more appropriate prescribing | Attenuation after adjusting for patient characteristics [4] |
*Composite outcome: Major Adverse Cardiovascular Event (MACE), Venous Thromboembolism (VTE), Cancer, or Serious Infection.
Table 2: General Comparison of Evidence Sources for Safety Validation
| Evidence Source | Typical Timeline | Key Strengths | Key Limitations |
|---|---|---|---|
| Pre-Market Clinical Trials (Phases I-III) | 1-5 years | Controlled conditions, rigorous data collection, causal inference [82] | Homogeneous populations, limited size, short duration, inability to detect rare events [82] [83] |
| Post-Marketing Studies (Phase IV) & Observational Research | 5+ years | Large, diverse patient populations, assessment of long-term and rare outcomes [82] | Potential for confounding and bias, imputation of causality is less certain [82] |
| Spontaneous Reporting Systems | Entire product lifecycle | Broad, nationwide coverage, early signal detection | Under-reporting, incomplete data, cannot determine incidence |
A landmark nationwide register-based cohort study in Sweden (2006-2022) on rheumatoid arthritis treatments clearly demonstrates this stabilization process. The study found that biologic/targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) initiated more than five years after a drug class's market entry were associated with significantly lower rates of a composite safety outcome (including serious infections, cardiovascular events, cancer, and venous thromboembolism) compared to those initiated within two years of market entry. The initial, unadjusted hazard ratio (HR) of 0.74 suggested a substantial improvement in safety. However, this association was greatly attenuated after adjusting for patient characteristics (adjusted HR 0.93), indicating that "modest channelling" of patients with higher inherent risk to newer drugs makes the safety profile of novel agents appear worse than it truly is. This highlights the critical importance of sophisticated statistical adjustment in observational safety studies [4].
Furthermore, a systematic landscape review of 30 systematic reviews across seven therapeutic areas found that while a majority (79.7%) of pooled relative effect estimates from randomized controlled trials (RCTs) and observational studies showed no statistically significant difference, extreme differences occurred in 43.2% of comparisons. This indicates significant variability in how safety and effectiveness are quantified across different study designs and over time, necessitating a careful, multi-source approach to evidence synthesis [82].
Methodological Frameworks for Safety Validation
The stabilization of a drug's safety profile is tracked through a structured sequence of methodological approaches, from initial controlled trials to long-term, real-world observation. The following workflow outlines this continuum.
Detailed Experimental and Observational Protocols
The path to a stabilized safety profile relies on distinct but interconnected methodological pillars.
Pre-Marketing Clinical Trial Protocols (Phases I-III)
Clinical trials are the foundation of initial safety assessment. Their protocols are highly standardized and controlled.
- Phase I: Focused primarily on safety and pharmacokinetics in a small group (20-80) of healthy volunteers. The goal is to identify frequent side effects and understand how the drug is metabolized and excreted [84].
- Phase II: Emphasizes preliminary data on effectiveness in patients (a few dozen to 300) with the target disease or condition. Safety continues to be evaluated, and short-term side effects are studied in a more relevant population [84].
- Phase III: Large-scale studies (several hundred to 3,000) that gather more extensive information on safety and effectiveness. These studies examine different populations, dosages, and use of the drug in combination with other drugs. They are designed to confirm efficacy and monitor adverse reactions from broad use [84]. All phases are overseen by Institutional Review Boards (IRBs) to ensure ethical conduct and participant safety, reflecting ethical codes like the Declaration of Helsinki [83].
Post-Marketing Surveillance and Observational Study Protocols
Once a drug is marketed, the nature of safety evidence gathering shifts dramatically toward observational and regulatory-mandated studies.
- Post-Marketing Requirement (PMR) and Commitment (PMC) Studies: These are studies required by or agreed to by a sponsor and conducted after FDA approval to gather additional information about a product's safety, efficacy, or optimal use [84].
- Register-Based Cohort Studies: As exemplified by the Swedish rheumatoid arthritis study [4], this powerful observational design involves:
- Data Source: Linking national healthcare registers (e.g., disease-specific clinical registers, prescription drug registers, patient registers, cause of death registers).
- Cohort Definition: Identifying initiators of the drug of interest and appropriate comparator cohorts (e.g., initiators of an established drug, or a general population cohort).
- Outcome Ascertainment: Using validated register-based codes to identify safety outcomes of interest.
- Statistical Analysis: Calculating incidence rates and using Cox regression models to estimate hazard ratios, adjusting for a wide range of potential confounders (e.g., age, sex, comorbidities, concomitant medications).
Comparative Effectiveness and Safety Protocols
Systematic reviews and meta-analyses that compare RCTs with observational studies represent a higher-order methodology for validating evidence consistency. The protocol for the 2021 systematic review [82] involved:
- Search Strategy: Systematic searches of PubMed and Embase for literature reviews published between 1990 and 2020.
- Eligibility Criteria: Including reviews that reported pooled relative treatment effects (e.g., Risk Ratios, Odds Ratios) for both RCTs and observational studies (cohort or case-control) on pharmaceutical interventions.
- Data Extraction & Analysis: Extracting pooled estimates and calculating the ratio of the relative effect from observational studies over that from RCTs (e.g., RR~obs~/RR~rct~). Consistency was evaluated based on statistical significance, confidence interval overlap, and direction of effect.
Conducting robust long-term safety validation requires a suite of specialized data, methodological, and regulatory tools.
Table 3: Key Research Reagent Solutions for Safety Validation Studies
| Tool / Resource | Category | Primary Function in Safety Research |
|---|---|---|
| National Electronic Health Registries (e.g., Swedish Rheumatology Quality Register) | Data Source | Provide large-scale, longitudinal, real-world data on drug exposure, patient comorbidities, and clinical outcomes for cohort studies [4]. |
| International Guidelines (ICH E2E, CIOMS VI/VIII) | Methodological & Regulatory Framework | Provide standardized frameworks for pharmacovigilance planning, risk management, and the design of safety surveillance studies [83]. |
| Propensity Score Matching/Analysis | Statistical Method | Aims to reduce selection bias and confounding in observational studies by simulating randomization, allowing for more valid comparisons between treatment groups [82]. |
| Adverse Event Expedited Reporting Systems (e.g., FDA's MedWatch) | Regulatory Tool | Mandatory systems for the rapid reporting of serious adverse events to regulatory authorities, serving as an early warning system for new safety signals [83]. |
| Periodic Benefit-Risk Evaluation Report (PBRER) | Regulatory Tool | A standardized aggregate report prepared by sponsors for regulators that provides an integrated analysis of the benefit-risk balance of a medicinal product, incorporating new safety information at defined intervals [83]. |
| k-Anonymization & Data Perturbation | Data Privacy Tool | Statistical disclosure control techniques used to generate privacy-preserving data visualizations and outputs from sensitive individual-level data, enabling analysis without breaching confidentiality [85]. |
The journey from a novel therapeutic agent to an established drug with a well-understood safety profile is a continuous process of evidence accumulation and validation. The quantitative data and methodological frameworks presented herein demonstrate that the apparent safety risks of new drugs are often initially inflated due to channeling bias and the heightened scrutiny of limited pre-market data. Over time, with the accumulation of vast real-world experience from diverse patient populations and the application of sophisticated observational study designs, a more accurate and typically more favorable safety profile emerges. This stabilization of knowledge is not automatic; it is the direct result of a rigorous, multi-modal global safety surveillance system that integrates controlled trial data with robust post-marketing studies. For researchers and drug development professionals, mastering these comparative methodologies is paramount to accurately characterizing the long-term safety of medicines, ensuring that the benefits of novel therapies continue to outweigh their risks throughout their market life.
The evaluation of a drug's benefit-risk ratio (BRA) is a continuous, multidimensional process essential throughout its entire lifecycle, from discovery and clinical development to post-market surveillance [86]. It involves a qualitative assessment of quantitative data, balancing therapeutic efficacy against safety risks [86]. No single methodology provides a fully satisfactory solution, as reducing this complex balance to simple metrics is challenging [86]. However, consistency and transparency are paramount, especially within the context of comparative safety profiles of novel versus established drug classes [86] [87]. A drug's benefit-risk profile is not static; it evolves as new safety information emerges from pharmacovigilance activities and new therapeutic alternatives become available, necessitating a framework for ongoing comparison [86].
Methodological Frameworks for Quantitative Assessment
A shift from qualitative, intuitive assessments toward structured, quantitative frameworks is underway to improve reproducibility, transparency, and facilitate serial assessments throughout a drug's lifecycle [87]. These methodologies aim to provide an aggregate metric for holistic comparison between therapies.
Core Quantitative Model
A fundamental quantitative approach frames the benefit-risk balance as a ratio, incorporating the frequency and severity of both benefits and harms, as well as the severity of the underlying disease [87]. The core equation can be expressed as:
Benefit-Risk Ratio = [Frequency of Benefit × Severity of Disease] / [Frequency of Adverse Reaction × Severity of Adverse Reaction] [87]
When the numerator exceeds the denominator, benefits are considered to outweigh the risks. This model requires operational definitions for its components. Severity is often defined by the impact on a person's ability to function normally, specifically the ability to carry out Activities of Daily Living (ADLs) [87]. Standardized grading scales like the Common Terminology Criteria for Adverse Events (CTCAE) provide a foundation for quantifying severity [87].
The Clavien-Dindo Risk Matrix Approach
A more advanced model leverages the Clavien-Dindo classification scheme to create a standardized risk matrix [88]. This system grades adverse events from I (minor) to V (death) based on the intervention required. Risk (R) is calculated using a weighted formula that combines the probability of occurrence (O) and severity (S):
R = (O^y × W) × (S^x) [88]
Where W is a weighting factor. The overall risk of a therapy (R_therapy) is the sum of the risk indices for all adverse event grades (A-E, corresponding to Clavien-Dindo grades I-V):
Rtherapy = RA + RB + RC + RD + RE [88]
The benefit is conceptualized as the reduction in risk achieved by the therapy compared to the natural risk of the illness without treatment (R_illness). The final benefit-risk ratio is then:
Benefit-Risk Ratio = Rillness / Rtherapy [88]
This allows for the direct comparison of different therapies or the same therapy over time.
Data Mining in Pharmacovigilance
Beyond structured trials, data mining algorithms (DMAs) are critical for transforming large datasets into meaningful safety knowledge [89]. These high-throughput methods uncover hidden relationships of potential clinical significance.
- Spontaneous Reporting Systems (SRS): DMAs like disproportionality analysis are applied to databases such as the FDA Adverse Event Reporting System (FAERS) to generate statistical associations for millions of drug-event combinations, serving as initial safety signals [89].
- Electronic Health Records (EHRs) and Claims Data: These real-world data sources offer a more complete record of patient medical history and are increasingly used for confirmatory analysis and active surveillance, as they are representative of routine clinical care [89].
- Novel Data Sources: Research is exploring chemical/biological knowledge bases (e.g., DrugBank) and biomedical literature to predict ADEs based on molecular structure and biological pathways, enabling a more proactive approach to pharmacovigilance [89].
Comparative Data Analysis: Frameworks and Findings
The following tables summarize the key methodologies and data sources used in modern benefit-risk analysis.
Table 1: Comparison of Quantitative Benefit-Risk Assessment Frameworks
| Framework Feature | Core Ratio Model [87] | Clavien-Dindo Risk Matrix [88] |
|---|---|---|
| Core Principle | Ratio of benefit to risk | Risk of illness without therapy vs. risk of therapy |
| Key Components | Frequency of benefit, Severity of disease, Frequency of AR, Severity of AR | Probability of harm, Severity of harm (Clavien-Dindo grade) |
| Quantification | Semi-quantitative; relies on grading scales (e.g., CTCAE) | Fully quantitative; generates a numerical risk index (High, Medium, Low) |
| Primary Application | Initial, high-level assessment | Comparative analysis of surgical and therapeutic outcomes |
| Advantages | Intuitively simple, incorporates disease severity | Standardized severity scale, allows for baselining and graphical comparison |
Table 2: Data Sources for Safety Signal Identification and Confirmation
| Data Source | Strengths | Limitations | Role in BRA |
|---|---|---|---|
| Randomized Controlled Trials (RCTs) [86] | Gold standard for efficacy; controlled environment minimizes bias. | Limited size and duration; cannot detect rare or delayed ADRs. | Foundation for pre-approval BRA; establishes efficacy. |
| Spontaneous Reporting Systems (SRS) [89] | Large population coverage; communicates genuine health concerns. | Passive system; subject to over-reporting and incomplete data. | Initial signal generation for post-marketing safety. |
| Electronic Health Records & Claims Data [89] | Representative of real-world care; complete medical history. | Require complex processing; pervasive confounding. | Signal confirmation and strengthening; active surveillance. |
| Chemical/Biological Databases [89] | Enables proactive prediction based on molecular structure. | Predictive and requires clinical validation. | Augments ADE discovery; informs preclinical BRA. |
Experimental & Analytical Protocols
Workflow for an Integrated Safety Assessment
The following diagram illustrates the logical workflow for integrating data from multiple sources to conduct a comprehensive benefit-risk assessment.
Integrated BRA Workflow
Quantitative BRA Framework Logic
This diagram details the logical sequence and calculations involved in a quantitative benefit-risk assessment using the core ratio model.
Quantitative BRA Logic
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Resources for BRA Research
| Item / Resource | Function in Benefit-Risk Assessment |
|---|---|
| Common Terminology Criteria for Adverse Events (CTCAE) [87] | Provides a standardized grading system (Grade 1-5) for adverse event severity based on impact on activities of daily living. |
| Clavien-Dindo Classification Scheme [88] | A harm-graded classification system for surgical and therapeutic complications, used for standardizing severity inputs in risk matrices. |
| Structured Query Languages (SQL) & Data Warehouses | Enable extraction and management of large-scale safety data from electronic health records and administrative claims databases. |
| Statistical Software (R, Python, SAS) | Essential for running data mining algorithms, performing disproportionality analysis, and executing complex statistical models for signal detection. |
| FDA AERS/VigiBase SRS Data | Primary source of spontaneous report data for initial hypothesis-free signal generation and quantification of reporting frequencies. |
Conclusion
The comparative safety assessment of novel and established drug classes is a dynamic, multi-stage process that extends well beyond initial approval. A drug's safety profile is not static but is shaped by its mechanism, the patient populations treated, and the duration of real-world exposure. Success requires a proactive, integrated strategy that leverages translational tools for early risk anticipation, robust real-world evidence methodologies to complement clinical trials, and a global perspective on safety data. Future progress hinges on greater regulatory harmonization, the development of advanced analytics for signal detection, and a shift towards more predictive safety models. By adopting this comprehensive framework, drug developers can better de-risk pipelines, optimize trial designs, and ultimately deliver safer therapeutics to patients.
References
- 1. analytical insights in deciphering drug safety evidence [https://www.frontiersin.org/journals/drug-safety-and-regulation/articles/10.3389/fdsfr.2024.1445998/full]
- 2. Characteristics of drugs safety signals that predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6055643/]
- 3. Comparing Safety and Efficacy of Novel AML Agents ... [https://www.ajmc.com/view/comparing-safety-and-efficacy-of-novel-aml-agents-against-established-regimens]
- 4. Do newly approved drugs have a worse observed safety ... [https://www.sciencedirect.com/science/article/pii/S0003496725000755]
- 5. Artificial intelligence in pharmacovigilance: advancing drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317250/]
- 6. Exclusive: Journal bans drug safety database papers as ... [https://retractionwatch.com/2025/09/16/exclusive-journal-bans-drug-safety-database-papers-as-they-flood-the-literature/]
- 7. How Safe and Innovative Are First-in-Class Drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5221712/]
- 8. Drug safety in healthy aging - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11993726/]
- 9. Strengthening Pharmacoepidemiology in a Changing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611502/]
- 10. A comparative analysis of three pharmacovigilance system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12237061/]
- 11. A comparative analysis of three pharmacovigilance system ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0327363]
- 12. Biologics vs Small Molecules: A New Era in Drug ... [https://synergbiopharma.com/biologics-vs-small-molecules/]
- 13. Small Molecules: Unsung Heroes of Pharma [https://www.drugpatentwatch.com/blog/small-molecules-unsung-heroes-of-pharma/?srsltid=AfmBOoosQ6cRrsMiwSHysxrphcqjvoSDTjp6WFB6h4U72NJnukcU3VQo]
- 14. Are small-molecule drugs having their big moment? [https://www.definitivehc.com/blog/small-molecule-drug-rise]
- 15. Adverse events of biologic or small molecule therapies in ... [https://www.sciencedirect.com/science/article/pii/S2405844024013884]
- 16. Safety and Effectiveness of Combining Biologics and Small ... [https://pubmed.ncbi.nlm.nih.gov/40845197/]
- 17. Novel Drug Approvals for 2025 [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 18. NIOSH List of Hazardous Drugs in Healthcare Settings, 2024 [https://www.cdc.gov/niosh/docs/2025-103/default.html]
- 19. Blockbuster Small-Molecule Drugs Approved by the FDA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114780/]
- 20. A comparative analysis of the safety profiles between ... [https://pubmed.ncbi.nlm.nih.gov/39645587/]
- 21. New Drug Review 2025 [https://www.uspharmacist.com/article/new-drug-review-2025]
- 22. FDA Issues White Paper on Selective Safety Data Collection [https://www.thefdalawblog.com/2025/08/sometimes-less-is-more-fda-issues-white-paper-on-selective-safety-data-collection/]
- 23. Comparing Moderna's mRNA-1083 and Pfizer's dual-target ... [https://www.nature.com/articles/s41541-025-01145-6]
- 24. USP DC [https://www.usp.org/health-quality-safety/usp-drug-classification-system]
- 25. Post marketing drug surveillance: Critical for Safer ... [https://lifebit.ai/blog/post-marketing-drug-surveillance/]
- 26. Post-Marketing Surveillance in 2025: Evolving Strategies ... [https://www.vitrana.com/post-marketing-surveillance-in-2025-evolving-strategies-for-real-world-safety-monitoring/]
- 27. Leveraging real-world data for safety signal detection and ... [https://www.frontiersin.org/journals/drug-safety-and-regulation/articles/10.3389/fdsfr.2025.1626822/full]
- 28. Ten first-in-class drugs on track for FDA approval in 2025 [https://www.labiotech.eu/best-biotech/first-in-class-drugs-to-watch-2025/]
- 29. Postmarketing Requirements and Commitments: Reports [https://www.fda.gov/drugs/postmarketing-requirements-and-commitments-introduction/postmarketing-requirements-and-commitments-reports]
- 30. Real-World Evidence: Methodologies for Integrating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12514902/]
- 31. Harnessing digital health technologies and real-world ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290384/]
- 32. Real-World Evidence: A Guide to RWE Analysis & ... [https://intuitionlabs.ai/articles/real-world-evidence-analysis]
- 33. How Real-World Evidence Can Help Increase Diversity in ... [https://veranahealth.com/how-real-world-evidence-can-help-increase-diversity-in-clinical-trials/]
- 34. Diversity in Clinical Trials: A Scientific Imperative for 2025 [https://www.wcgclinical.com/insights/diversity-in-clinical-trials-a-scientific-imperative-for-2025/]
- 35. FDA use of Real-World Evidence in Regulatory Decision ... [https://www.fda.gov/science-research/real-world-evidence/fda-use-real-world-evidence-regulatory-decision-making]
- 36. Real-World Evidence in FDA Approvals for Labeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446098/]
- 37. A Review and Comparative Case Study Analysis of Real- ... [https://www.sciencedirect.com/science/article/pii/S1098301524028596]
- 38. Regulatory and Payer Evaluation of Real-World Evidence [https://www.drugepi.org/dope/rwe-roundtable-2025]
- 39. 36 Top RWE Platforms in 2025 [https://www.mahalo.health/insights/top-real-world-evidence-rwe-platforms]
- 40. OFF X Preclinical & Clinical Safety Intelligence [https://clarivate.com/life-sciences-healthcare/research-development/pharmacovigilance-drug-safety/off-x/]
- 41. The eTRANSAFE Project on Translational Safety Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7999019/]
- 42. Semantic and visual mining of adverse drug events from ... [https://www.sciencedirect.com/science/article/abs/pii/S0933365721000671]
- 43. Step 5: FDA Post-Market Drug Safety Monitoring [https://www.fda.gov/patients/drug-development-process/step-5-fda-post-market-drug-safety-monitoring]
- 44. Drug safety assessment in clinical trials: methodological ... [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-13-138]
- 45. What Can We Learn About Drug Safety and Other Effects in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6917880/]
- 46. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 47. WHO unveils new guideline to improve global access ... [https://www.who.int/news/item/26-05-2025-who-unveils-new-guideline-to-improve-global-access-to-controlled-medicines]
- 48. Global Regulatory Harmonization Efforts in 2025 [https://www.freyrsolutions.com/blog/global-regulatory-harmonization-efforts-in-2025]
- 49. Global GHS Implementation Differences: 2025 Country Guide [https://www.complianceandrisks.com/blog/global-ghs-implementation-differences-by-country-a-definitive-guide-for-multinational-compliance-teams/]
- 50. Global Regulatory Requirements for Drug Safety & ... [https://www.businesswire.com/news/home/20251028171308/en/Global-Regulatory-Requirements-for-Drug-Safety-Pharmacovigilance-Product-Safety-Effective-Risk-Assessment-and-Alignment-with-Evolving-U.S.-EU-and-UK-Regulatory-Expectations-November-25-2025---ResearchAndMarkets.com]
- 51. Global Regulatory Requirements for Drug Safety & ... [https://finance.yahoo.com/news/global-regulatory-requirements-drug-safety-090300173.html]
- 52. Medication safety research by observational study design [https://pmc.ncbi.nlm.nih.gov/articles/PMC4909784/]
- 53. Confounding in Observational Studies Evaluating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8786092/]
- 54. Addressing the issue of channeling bias in observational ... [https://pubmed.ncbi.nlm.nih.gov/17138506/]
- 55. Chapter 6: Methods to address bias and confounding - ENCePP [https://encepp.europa.eu/encepp-toolkit/methodological-guide/chapter-6-methods-address-bias-and-confounding_en]
- 56. Effect of Competition Bias in Safety Signal Generation [https://pubmed.ncbi.nlm.nih.gov/22967190/]
- 57. Designing Effective Data Visualizations [https://guides.library.jhu.edu/datavisualization/design]
- 58. Working with the text backplate in Windows High Contrast [https://www.gwhitworth.com/posts/2019/high-contrast-text-backplate/]
- 59. Visualizing Quantitative Data: Best Practices [https://ajelix.com/data/visualizing-quantitative-data-best-practices/]
- 60. Signal Detection & Management Mastery in ... [https://ccrps.org/clinical-research-blog/signal-detection-amp-management-mastery-in-pharmacovigilance]
- 61. Signals vs. Noise: How to Identify the Most Important ... [https://www.linkedin.com/pulse/signals-vs-noise-how-identify-most-important-trends-before-hamman-2ug6f]
- 62. Leveraging real-world data for safety signal detection and risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576344/]
- 63. Comparative cardiovascular outcomes and safety of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369064/]
- 64. Advancing Generic Drug Development ... [https://www.fda.gov/drugs/news-events-human-drugs/advancing-generic-drug-development-translating-science-approval-2025-10072025]
- 65. Are Generic Drugs Less Safe than their Branded ... [https://www.drugpatentwatch.com/blog/are-generics-less-safe/?srsltid=AfmBOoqWvz0HxdYkQFtM0nFpen0W4M0zIGSzeWrAMR8V4QTXVpGNlqxz]
- 66. Brand-Name vs. Generic Drugs [https://www.hattiesburgclinic.com/blog-brand-name-vs-generic-drugs/]
- 67. FDA List of Authorized Generic Drugs [https://www.fda.gov/drugs/abbreviated-new-drug-application-anda/fda-list-authorized-generic-drugs]
- 68. Comparative safety analysis of bevacizumab and alkylating ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1595642/full]
- 69. World Drug Safety Congress Americas 2025 [https://www.iqvia.com/events/2025/09/world-drug-safety-congress-americas-2025]
- 70. Pharmacovigilance conference 2025: the future of drug ... [https://lsacademy.com/en/pharmacovigilance-conference-2025-the-future-of-drug-safety-monitoring/]
- 71. INVESTIGATING GENERICS: America's Overlooked Drug ... [https://medshadow.org/are-generic-drugs-safe/]
- 72. Risk Evaluation and Mitigation Strategies | REMS [https://www.fda.gov/drugs/drug-safety-and-availability/risk-evaluation-and-mitigation-strategies-rems]
- 73. Enhancing Drug Safety: Pharmacovigilance Trends 2025 [https://zenovel.com/drug-safety-through-smarter-monitoring/]
- 74. Comparative analysis on renal and cardiovascular ... [https://pubmed.ncbi.nlm.nih.gov/40798873/]
- 75. Cardiovascular and renal outcomes of dual combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12487346/]
- 76. Sodium-Glucose Transport 2 (SGLT2) Inhibitors - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK576405/]
- 77. SGLT2 inhibitors across various patient populations in the ... [https://www.nature.com/articles/s44324-025-00068-z]
- 78. Study compares the kidney, cardiovascular and mortality ... [https://www.news-medical.net/news/20251120/Study-compares-the-kidney-cardiovascular-and-mortality-risks-of-three-different-GLP-1-RAs.aspx]
- 79. New class of antihypertensive medications may have both ... [https://www.news-medical.net/news/20250908/New-class-of-antihypertensive-medications-may-have-both-kidney-and-cardio-protective-benefits.aspx]
- 80. A Comparison of Safety Information in Drug Labeling at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9310370/]
- 81. A Comparison of Safety Information in Drug Labeling at the ... [https://www.semanticscholar.org/paper/A-Comparison-of-Safety-Information-in-Drug-Labeling-Hoshino-Narukawa/0d1fb52eb959c7807661cdaa4525138b9d856a95]
- 82. Comparative effectiveness and safety of pharmaceuticals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647453/]
- 83. Safety Surveillance During Drug Development [https://link.springer.com/article/10.1007/s12325-023-02492-3]
- 84. The FDA's Drug Review Process: Ensuring Drugs Are Safe ... [https://www.fda.gov/drugs/information-consumers-and-patients-drugs/fdas-drug-review-process-ensuring-drugs-are-safe-and-effective]
- 85. Privacy preserving data visualizations - EPJ Data Science [https://epjdatascience.springeropen.com/articles/10.1140/epjds/s13688-020-00257-4]
- 86. Assessing the benefit:risk ratio of a drug - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3181998/]
- 87. An Approach to a Benefit-Risk Framework [https://acrpnet.org/2024/04/12/an-approach-to-a-benefit-risk-framework]
- 88. A Quantitative Benefit-Risk Analysis & ... [https://www.outsourcedpharma.com/doc/a-quantitative-benefit-risk-analysis-benefit-risk-ratio-using-real-world-data-part-i-0001]
- 89. Novel Data Mining Methodologies for Adverse Drug Event ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3675775/]