How to Interpret Dose-Response Curves: A Comprehensive Guide for Preclinical Research and Drug Development
This article provides a comprehensive guide for researchers and drug development professionals on interpreting dose-response curves in preclinical research.
How to Interpret Dose-Response Curves: A Comprehensive Guide for Preclinical Research and Drug Development
Abstract
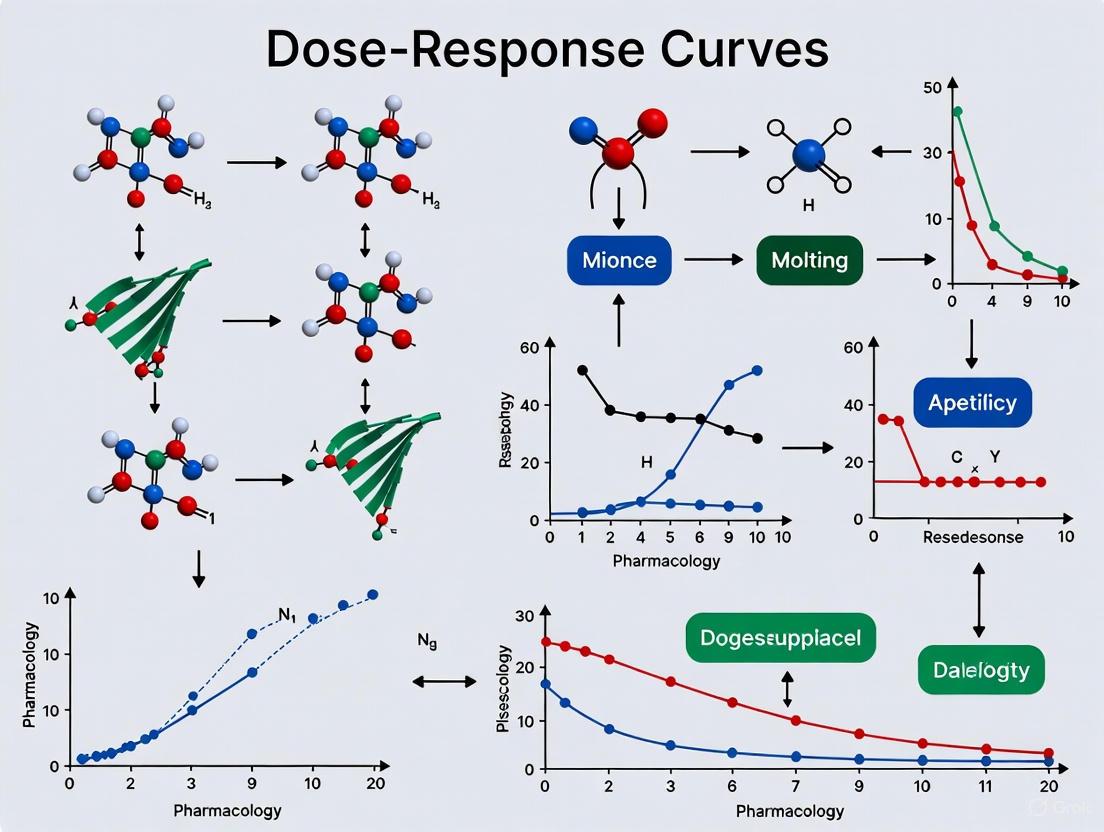
This article provides a comprehensive guide for researchers and drug development professionals on interpreting dose-response curves in preclinical research. It covers foundational principles, from defining key parameters like EC50, Emax, and Hill slope to understanding curve shapes and their biological significance. The guide delves into methodological applications, including step-by-step curve creation, mathematical modeling with Hill and Emax equations, and advanced model-based analysis techniques. It addresses common troubleshooting challenges in experimental design and data interpretation, and explores validation strategies through comparative analysis and meta-analysis. The content synthesizes modern best practices to enhance decision-making in lead optimization and clinical translation, emphasizing the critical role of robust dose-response characterization in successful drug development.
Decoding the Basics: Understanding Dose-Response Curve Fundamentals and Key Parameters
What is a Dose-Response Curve? Defining the Relationship Between Stimulus and Biological Effect
The dose-response relationship is a fundamental principle in pharmacology and toxicology that describes the quantitative relationship between the exposure amount or dose of a substance and the magnitude of the biological effect it produces [1] [2]. This systematic description analyzes what kind of response is generated at the administration of a specific drug dose and is central to determining "safe," "hazardous," and beneficial levels of drugs, pollutants, foods, and other substances to which humans or other organisms are exposed [1]. The well-known adage "the dose makes the poison" effectively captures this concept, reflecting how a small amount of a toxin may have no significant effect, while a large amount could prove fatal [1].
In preclinical research, understanding this relationship is crucial for optimizing clinical outcomes [3]. Dose-response curves are the graphical representations of these relationships, with the applied dose generally plotted on the X-axis and the measured response plotted on the Y-axis [1]. These curves serve as critical tools throughout the drug development pipeline, providing invaluable insights for regulatory documentation regarding efficacy and safety [4].
Key Components and Parameters of Dose-Response Curves
Quantitative Parameters of Dose-Response Curves
Dose-response analysis reveals several critical parameters that characterize compound activity. The following table summarizes these key quantitative measures:
| Parameter | Definition | Research Application |
|---|---|---|
| Potency | Amount of drug required to produce therapeutic effect [4] | Identifies lower effective dosing limits; more potent drugs require lower doses [4] |
| Efficacy (Emax) | Maximum therapeutic response a drug can produce [2] [4] | Determines upper limit of drug effect; distinguishes from potency [4] |
| EC50 | Concentration producing 50% of maximum effect in graded response [2] | Measures agonist potency; standard for comparison in high-throughput screening [1] [4] |
| IC50 | Concentration inhibiting biological process by 50% [4] | Characterizes antagonists/enzyme inhibitors; lower values indicate greater inhibitory potency [4] |
| Slope Factor | Steepness of the curve, quantified by Hill slope [1] | Indicates response sensitivity to dose changes; steeper slopes suggest higher potency at low concentrations [2] |
| Threshold Dose | Minimum dose where measurable response first occurs [2] | Establishes safety boundaries; defines safe vs. potentially harmful exposure levels [2] |
Mathematical Modeling of Dose-Response Relationships
The characteristic sigmoidal shape of many dose-response curves can be mathematically described by the Hill equation [1]. This logistic function models the relationship between drug concentration and effect:
Where:
- E = observed effect at concentration [A]
- Emax = maximum possible effect
- [A] = drug concentration
- EC50 = concentration producing half-maximal effect
- n = Hill coefficient (slope factor) [1]
For more flexible modeling, particularly when baseline effects must be considered, the Emax model is widely employed in drug development:
Where E0 represents the effect at zero dose [1]. This generalized model accommodates various baseline conditions and is the single most common non-linear model for describing dose-response relationships in drug development [1].
Curve Characteristics and Biological Interpretation
The Sigmoidal Curve and Its Phases
The majority of drug molecules follow a sigmoidal dose-response curve when response is plotted against the logarithm of the dose [4]. This characteristic S-shape emerges from biological principles and consists of three distinct phases:
- Lag Phase: At very low doses, the response is minimal because insufficient drug molecules are bound to receptors to trigger a significant biological effect [2] [4].
- Linear Phase: As the dose increases, the response rises steeply in an approximately linear fashion as more receptors become occupied, producing a progressively greater effect [4].
- Plateau Phase: The curve eventually flattens as receptor saturation occurs—all available receptors are occupied, and increasing the dose further cannot produce a greater biological effect [2] [4].
This sigmoidal shape reflects the biological limits of the system and effectively illustrates how drug efficacy develops over a range of doses [2] [4].
Multiphasic and Nonlinear Responses
Not all dose-response relationships follow simple sigmoidal patterns. Biological complexity often produces multiphasic curves that cannot be captured by the classical Hill equation [4]. Research analyzing 11,650 dose-response curves from the Cancer Cell Line Encyclopedia found that approximately 28% were more accurately modeled by multiphasic models [4].
The DOT language diagram below illustrates the workflow for identifying and modeling these complex curve types:
Complex curve types include two inhibitory phases, stimulation followed by inhibition, and three-phase curves [4]. These multiphasic responses may occur when a drug acts on multiple receptors with different sensitivities, exhibits dual effects (stimulatory at low doses and inhibitory at high doses), or when metabolic saturation occurs [4].
Experimental Protocols and Methodologies
Preclinical Dose Range Finding (DRF) Studies
Dose range finding (DRF) studies form the foundation of preclinical drug development, providing crucial safety data to guide dose level selection before advancing into formal toxicology studies [5]. These studies establish two critical parameters: the minimum effective dose (MED) and the maximum tolerated dose (MTD) [5].
The experimental workflow for DRF studies can be visualized as follows:
Key Experimental Steps in DRF Studies
Animal Model Selection: Species selection (rodents and/or non-rodents) directly impacts the relevance and translational value of data for human risk assessment. Selection criteria include drug absorption, distribution, metabolism, excretion (ADME) properties, receptor expression, and physiological relevance to humans [5].
Study Design and Dosing Strategies: A well-designed DRF study includes multiple dosing levels to establish a dose-response relationship. The starting dose is based on prior PK, PD, or in vitro studies, with gradual increases (e.g., 2x, 3x logarithmic increments) until significant toxicity is observed. If severe toxicity occurs, researchers may test intermediate doses to fine-tune the MTD [5].
Safety and Toxicity Assessments: Comprehensive monitoring includes clinical observations, body weight tracking, food consumption, and pathological assessments (hematology, serum chemistry, urinalysis). Gross necropsy followed by preliminary histopathology helps identify organ-specific toxicities [5].
Pharmacokinetics (PK) and Biomarker Evaluation: Measuring exposure metrics—maximum concentration (Cmax), area under the curve (AUC), and half-life—provides insights into dose-exposure relationships. Biomarkers evaluate target engagement and pharmacodynamic effects, offering early indicators of toxicities and confirming PD outcomes [5].
Essential Research Reagents and Solutions
The following table details key research reagents and solutions essential for conducting dose-response experiments:
| Reagent/Solution | Function in Dose-Response Research |
|---|---|
| Cell-Based Assay Systems | Provide biological context for measuring compound effects on living cells in high-throughput screening [4]. |
| Target-Specific Ligands | Agonists and antagonists used to characterize receptor binding and functional responses in pharmacological studies [4]. |
| Molecular Docking Tools | Computational methods to predict binding affinity of compounds to target proteins, informing dose-response modeling [6]. |
| Pathway-Specific Biomarkers | Measurable indicators of target engagement and pharmacodynamic effects at different dose levels [5]. |
| Analytical Standards | Certified reference materials for quantifying drug concentrations in PK studies measuring Cmax, AUC, and half-life [5]. |
Applications in Preclinical Research and Drug Development
Efficacy and Safety Assessment
Dose-response curves enable researchers to estimate both the minimum effective dose and maximum tolerated dose, establishing the therapeutic window where a drug is effective but not toxic [5] [4]. In toxicology, these curves identify critical safety parameters:
- No Observed Adverse Effect Level (NOAEL): The highest dose at which no harmful effects are observed [4].
- Lowest Observed Adverse Effect Level (LOAEL): The lowest dose where a harmful effect is detected [4].
These values are essential for regulatory filings and first-in-human (FIH) dose selection, helping to establish safe margins between efficacious and toxic doses [5].
Agonist and Antagonist Characterization
Dose-response curves critically differentiate how various drug types interact with biological systems:
- Agonists (which activate receptors) typically produce classical sigmoidal curves, with EC50 values indicating potency [4].
- Competitive antagonists (which block receptor activation) shift the agonist curve to the right, requiring higher agonist concentrations to achieve the same effect [4].
- Non-competitive antagonists not only shift the curve but also flatten it by reducing the maximum efficacy (Emax) [4].
Paradigm Shift in Oncology Dose Optimization
Traditional dose-finding for cytotoxic cancer drugs focused primarily on determining the maximum tolerated dose (MTD). However, for modern targeted therapies and immunotherapies, the field is shifting toward defining the optimal biological dose (OBD) that offers a better efficacy-tolerability balance [7]. This new paradigm incorporates PK/PD-driven modeling, biomarker data, and patient-reported outcomes to characterize the dose-response curve and identify a range of possible doses earlier in development [7].
The dose-response curve represents a fundamental conceptual framework in preclinical research, providing a systematic approach to understanding the quantitative relationship between drug exposure and biological effect. Through its key parameters—potency, efficacy, EC50/IC50, and slope—researchers can characterize compound activity, establish therapeutic windows, and identify optimal dosing strategies. The ongoing evolution from simple sigmoidal models to multiphasic frameworks reflects growing recognition of biological complexity, while advances in computational modeling and pathway network analysis offer promising approaches for predicting dose-response relationships in increasingly sophisticated biological systems. For preclinical researchers, mastery of dose-response principles remains essential for translating laboratory findings into safe and effective therapeutic interventions.
In preclinical drug development, the dose-response curve is a fundamental tool for quantifying the biological activity of a compound. This relationship, which is typically sigmoidal when response is plotted against the logarithm of concentration, provides a wealth of information that guides decision-making from early discovery through lead optimization [8] [9]. Proper interpretation of this curve allows researchers to predict therapeutic potential, understand mechanism of action, and identify promising candidates for further development. The curve's shape and position are characterized by three fundamental parameters: the EC50/IC50 (potency), Emax (efficacy), and Hill slope (cooperativity) [10] [11] [8]. This guide provides an in-depth examination of these critical parameters, their biological significance, and the experimental methodologies employed for their accurate determination in preclinical research.
Fundamental Parameters of Dose-Response Curves
EC50 and IC50: Quantifying Potency
The EC50 (half-maximal effective concentration) and IC50 (half-maximal inhibitory concentration) are quantitative measures of a compound's potency, representing the concentration required to produce 50% of the maximum effect or 50% inhibition of a biological process, respectively [12] [13]. In pharmacological terms, potency is defined as the concentration or dose of a drug required to produce 50% of that drug's maximal effect [14]. It is crucial to recognize that potency and efficacy are distinct concepts; a compound can be highly potent (low EC50) yet have limited efficacy (low Emax), or vice versa [14] [9].
The interpretation of these values requires careful consideration of what defines 100% and 0% response [12]. The relative EC50/IC50 is the most common definition, representing the concentration that produces a response halfway between the top and bottom plateaus of the experimental curve itself. In contrast, the absolute EC50/IC50 (sometimes referred to as GI50 in anti-cancer drug screening) is the concentration that produces a response halfway between the values defined by positive and negative controls [12] [15]. The relative definition forms the basis of classical pharmacological analysis, while the absolute approach is sometimes used in specialized contexts such as cell growth inhibition studies [12].
Emax: Quantifying Efficacy
Emax represents the maximum response achievable by a drug at sufficiently high concentrations, reflecting its intrinsic efficacy [14] [16] [8]. Efficacy describes the ability of a drug to initiate a cellular response once bound to its receptor, with higher Emax values indicating a greater capacity to elicit a biological effect [14]. In the context of receptor theory, efficacy expresses "the degree to which different agonists produce varying responses, even when occupying the same proportion of receptors" [14]. It is important to note that efficacy is highly dependent on experimental conditions, including the tissue used, level of receptor expression, and the specific measurement technique employed [14].
Hill Slope: Quantifying Cooperativity and Curve Steepness
The Hill slope (n), also known as the Hill coefficient, quantifies the steepness of the dose-response curve and can indicate cooperative interactions in drug-receptor binding [10] [11]. The Hill coefficient provides a way to quantify the degree of interaction between ligand binding sites [11]. The value of the Hill slope provides critical insights into the binding mechanism:
- n = 1.0: Suggests simple bimolecular binding with no cooperativity, typical of a ligand binding to a single independent receptor site [11] [17].
- n > 1.0: Indicates positive cooperativity, where binding of the first ligand molecule facilitates binding of subsequent molecules, resulting in a steeper curve [11].
- n < 1.0: Suggests negative cooperativity or multiple binding sites with different affinities, producing a shallower curve [11] [15].
Table 1: Key Parameters of Dose-Response Curves
| Parameter | Symbol | Definition | Interpretation | Typical Range |
|---|---|---|---|---|
| Potency | EC50/IC50 | Concentration for 50% maximal effect/inhibition | Lower value = higher potency | pM-mM |
| Efficacy | Emax | Maximum achievable response | Higher value = greater efficacy | 0-100% |
| Cooperativity | Hill slope | Steepness of dose-response curve | n=1: no cooperativityn>1: positive cooperativityn<1: negative cooperativity | Typically 0.5-3 |
Mathematical Foundations: The Hill Equation
The relationship between drug concentration and effect is mathematically described by the Hill equation, originally formulated by Archibald Hill in 1910 to describe the sigmoidal O2 binding curve of hemoglobin [10] [11]. The equation has two closely related forms: one reflecting receptor occupancy and the other describing tissue response.
For tissue response, the Hill equation is expressed as:
[ E = E0 + E{max} \frac{C^n}{EC_{50}^n + C^n} ]
Where:
- (E) = observed biological effect
- (E_0) = baseline effect (can be fixed at 0 for simple models)
- (E_{max}) = maximum possible effect
- (C) = drug concentration
- (EC_{50}) = concentration producing 50% of maximal effect
- (n) = Hill coefficient [16]
This equation can be rearranged to illustrate why the curve is sigmoidal when plotted against log concentration:
[ E = \frac{E{max}}{1 + \exp(-n(\ln C - \ln EC{50}))} ]
This form demonstrates that the effect (E) is described by a logistic function of (\ln C), where (EC_{50}) acts as a location parameter and (n) as a gain parameter controlling steepness [16].
For data analysis, the equation can be linearized by creating a Hill plot:
[ \log\left(\frac{E}{E{max} - E}\right) = n(\log C - \log EC{50}) ]
A plot of (\log(E/(E{max} - E))) versus (\log C) yields a straight line with slope (n) and x-intercept of (\log EC{50}) [11]. However, with modern computing power, nonlinear regression is preferred as it provides more robust parameter estimates without distorting error propagation [11].
Experimental Protocols for Parameter Determination
Saturation Binding Assays for Kd and Bmax Determination
Objective: To determine the equilibrium dissociation constant (Kd) and maximum number of binding sites (Bmax) for a ligand-receptor interaction.
Protocol:
- Receptor Preparation: Prepare membrane fractions or cells expressing the target receptor.
- Radioligand Dilution: Prepare a concentration series of radiolabeled ligand, typically spanning a 100-10,000-fold range centered around the estimated Kd.
- Incubation: Incubate each radioligand concentration with a fixed amount of receptor preparation in appropriate buffer. Include parallel tubes with excess unlabeled ligand (100x Kd) to determine nonspecific binding.
- Separation and Measurement: Separate bound from free ligand by rapid filtration, centrifugation, or other appropriate method. Measure bound radioactivity by scintillation counting.
- Data Analysis: Subtract nonspecific binding from total binding to obtain specific binding. Fit specific binding data to the equation:
[ Y = B{max} \times X^h / (Kd^h + X^h) ]
Where Y is specific binding, X is radioligand concentration, Bmax is maximum binding sites, Kd is equilibrium dissociation constant, and h is Hill slope [17].
Functional Dose-Response Assays for EC50/IC50 and Emax Determination
Objective: To determine the functional potency (EC50/IC50) and efficacy (Emax) of a compound in a biological system.
Protocol:
- Cell/ Tissue Preparation: Prepare cells expressing the target receptor or isolated tissue responsive to the compound.
- Compound Dilution: Prepare serial dilutions of the test compound, typically in log increments (e.g., half-log or full-log dilutions) across a range covering expected inactive to maximal effect concentrations.
- Response Measurement: Apply compound concentrations to the biological system and measure the functional response (e.g., cAMP accumulation, calcium flux, cell viability, contraction force).
- Control Definition: Include appropriate controls to define 0% and 100% response:
- For agonists: Use vehicle control (0%) and maximal concentration of standard agonist (100%)
- For antagonists/ inhibitors: Use vehicle control (0%) and maximal concentration of standard inhibitor (100%) [12]
- Data Analysis: Fit normalized response data to the Hill equation using nonlinear regression algorithms such as Levenberg-Marquardt [10]. For incomplete curves that don't reach plateaus, constraints may be applied based on control values [12].
Data Normalization and Quality Control
Proper normalization is critical for accurate parameter estimation. The three main strategies include:
- External controls: Using separately measured positive and negative controls to define 100% and 0% response [10] [12].
- Extreme concentrations: Using the lowest and highest concentrations of the test substance to define response limits [12].
- Regression plateaus: Using the top and bottom plateau values estimated from nonlinear regression [12].
Fit validation should include assessment of:
- Activity threshold: Setting ranges that define inactive compounds to prevent bogus IC50 calculations for compounds with insufficient activity [10].
- Parameter constraints: Restricting parameters to physiologically plausible ranges when appropriate [10].
- Curve quality metrics: Evaluating R-squared values, confidence intervals of parameters, and visual inspection of residuals [10].
Diagram 1: Experimental workflow for dose-response analysis.
Advanced Interpretation and Biological Significance
Relationship Between Binding and Response
While the Hill equation can describe both receptor binding and functional response, it is crucial to recognize that Kd (binding affinity) and EC50 (functional potency) are not identical parameters [13] [9]. The relationship between occupancy and response is often nonlinear due to signal amplification mechanisms in biological systems [16]. A drug may bind tightly to its receptor (low Kd) yet produce a weak response (high EC50) if it has low efficacy, or conversely, bind weakly yet produce a strong response if the system has high amplification [16] [13].
This distinction has practical implications for drug discovery. A common mistake is assuming that a lower IC50 always means stronger binding, when in fact IC50 depends on experimental conditions, and two compounds with the same Kd could have very different IC50 values in different assays [13]. Kd is better for understanding pure binding affinity, while EC50/IC50 are more relevant for functional inhibition or activation in specific biological contexts [13].
Systematic Variation in Parameters Across Biological Contexts
Different dose-response parameters can vary systematically depending on biological context, carrying distinct information about drug action [15]. In large-scale analyses of anti-cancer drug responses:
- Emax frequently associates with cell type, particularly correlating with cell proliferation rate for cell-cycle inhibitors [15].
- Hill slope often associates with drug class, with certain target classes (e.g., Akt/PI3K/mTOR inhibitors) consistently showing unusually shallow curves (Hill slope < 1) [15].
- IC50 shows variable association with both cell type and drug class, but is often less informative than multi-parametric analysis [15].
These systematic variations highlight why multi-parameter analysis provides more comprehensive insights than potency (IC50) alone, particularly at clinically relevant concentrations near and above IC50 [15].
Table 2: Research Reagent Solutions for Dose-Response Studies
| Reagent/Category | Function | Example Applications |
|---|---|---|
| Radiolabeled Ligands | Quantitative measurement of receptor binding affinity (Kd) and density (Bmax) | Saturation binding assays; competition binding studies |
| Positive/Negative Controls | Define 0% and 100% response for data normalization | Reference agonists/antagonists; vehicle controls |
| Cell Viability Assays | Measure functional responses in cellular systems | ATP-based assays (CellTiter-Glo); apoptosis markers |
| Signal Transduction Assays | Quantify downstream signaling events | cAMP accumulation; calcium flux; phosphorylation status |
| Enzyme/Receptor Preparations | Source of molecular targets | Recombinant enzymes; membrane preparations; cell lines |
Clinical Relevance and Therapeutic Implications
The parameters derived from dose-response curves have direct clinical relevance. Potency (EC50) influences dosing regimens, with more potent drugs typically requiring lower doses to achieve therapeutic effects [9]. Efficacy (Emax) determines the maximum therapeutic benefit achievable with a drug, which is particularly important for diseases requiring strong pharmacological intervention [14] [9]. The Hill slope affects the therapeutic window, as steeper curves (Hill slope > 1) result in a narrower range between ineffective and toxic concentrations [11] [9].
For therapeutic use, it is essential to distinguish between potency and efficacy. A drug may be potent (low EC50) but have limited clinical utility if its maximum efficacy is insufficient for the therapeutic goal [9]. Conversely, a less potent drug with higher maximum efficacy may be more effective at achievable concentrations [9].
Diagram 2: Relationship between drug binding and physiological response.
The comprehensive interpretation of EC50/IC50, Emax, and Hill slope provides critical insights that extend far beyond simple potency rankings. These parameters collectively describe fundamental aspects of drug action: the concentration required for effect (potency), the maximum achievable response (efficacy), and the cooperative nature of the interaction (steepness). Proper experimental design, rigorous data analysis, and multi-parameter interpretation are essential for accurate compound characterization in preclinical research. By moving beyond simplistic IC50 comparisons to embrace the full richness of information contained in dose-response relationships, researchers can make more informed decisions in the drug discovery process, ultimately leading to better candidate selection and improved clinical translation.
In preclinical drug development, the dose-response relationship is a fundamental principle that describes the correlation between the magnitude of a pharmacological effect and the dose or concentration of a drug administered to a biological system [1]. These relationships are crucial for determining "safe," "hazardous," and beneficial exposure levels for drugs and other substances [1]. Understanding these relationships forms the basis for public health policy and clinical trial design [18]. The dose-response relationship, when graphically represented, produces characteristic curves whose shapes reveal critical information about drug potency, efficacy, and mechanism of action [19]. The accurate interpretation of these curve shapes—primarily sigmoidal, linear, and biphasic—is therefore essential for optimizing therapeutic interventions and predicting clinical outcomes.
The analysis of dose-response curves extends across multiple levels of biological organization, from molecular interactions and cellular responses to whole-organism physiology and population-level effects [1]. At each level, the curve shape reflects the underlying biological processes and can be influenced by factors such as receptor binding kinetics, signal transduction pathways, metabolic processes, and homeostatic mechanisms [20]. For preclinical researchers, properly characterizing these curves enables the identification of optimal dosing ranges, prediction of potential toxicities, and selection of promising drug candidates for further development [18]. This guide provides a comprehensive technical framework for interpreting the most common dose-response curve shapes encountered in preclinical research, with emphasis on their biological implications and methodological considerations for accurate characterization.
Fundamental Concepts and Parameters
Before examining specific curve shapes, it is essential to understand the key parameters used to quantify dose-response relationships. These parameters provide the quantitative framework for comparing different compounds and interpreting their biological effects.
Table 1: Key Parameters for Characterizing Dose-Response Relationships
| Parameter | Description | Biological Interpretation |
|---|---|---|
| Potency | Location of curve along dose axis [19] | Concentration required to elicit a response; indicates binding affinity |
| Maximal Efficacy (Emax) | Greatest attainable response [19] | Maximum biological effect achievable with a compound; reflects intrinsic activity |
| Slope | Change in response per unit dose [19] | Steepness of transition from minimal to maximal response; indicates cooperativity |
| EC50/IC50 | Concentration producing 50% of maximal effect [21] | Standard measure of potency for agonists (EC50) or antagonists (IC50) |
| Hill Coefficient (nH) | Parameter describing steepness of sigmoidal curve [1] | Quantitative measure of cooperativity in binding; nH > 1 suggests positive cooperativity |
These parameters are derived through mathematical modeling of experimental data, with the Hill equation and Emax model being commonly used approaches [1]. The Hill equation is particularly valuable for sigmoidal curves and is expressed as E/Emax = [A]^n/(EC50^n + [A]^n), where E is the effect, Emax is the maximal effect, [A] is the drug concentration, EC50 is the concentration producing 50% of maximal effect, and n is the Hill coefficient [1]. The Emax model extends this concept by incorporating a baseline effect (E0) and is expressed as E = E0 + ([A]^n × Emax)/([A]^n + EC50^n) [1]. These models enable researchers to quantify dose-response relationships and make meaningful comparisons between different compounds and experimental conditions.
Sigmoidal Dose-Response Curves
Characteristics and Biological Basis
Sigmoidal curves represent the most frequently observed shape in dose-response relationships, particularly when the dose axis is plotted on a logarithmic scale [21]. These curves are characterized by a gradual increase at low doses, a steep, approximately linear rise at intermediate doses, and a plateau at higher doses [19]. The sigmoidal shape reflects fundamental biological principles, including the law of mass action for receptor-ligand interactions and the concept of occupancy-response relationships [1]. At low concentrations, the response is minimal as few receptors are occupied. As concentration increases, receptor occupancy rises rapidly, leading to a proportional increase in effect. At high concentrations, the response plateaus as receptors become saturated, representing the system's maximal capacity to respond.
The mathematical foundation for sigmoidal curves is often described by the Hill equation or four-parameter logistic (4PL) model, which quantifies the bottom asymptote (basal response), top asymptote (maximal response), slope factor (steepness), and EC50 (potency) [21]. The Hill slope provides valuable information about the cooperativity of the interaction; a slope greater than 1 suggests positive cooperativity, where binding of one ligand molecule facilitates binding of subsequent molecules, while a slope less than 1 may indicate negative cooperativity or system heterogeneity [1]. In receptor pharmacology, the sigmoidal shape reflects the transition from minimal receptor occupancy to saturation, with the steepness of the curve influenced by the degree of spare receptors and the efficiency of signal transduction mechanisms [19].
Experimental Protocol for Characterizing Sigmoidal Responses
The reliable characterization of sigmoidal dose-response relationships requires careful experimental design and execution. The following protocol outlines key methodological considerations:
Dose Selection and Spacing: Select 5-10 concentrations distributed across a broad range to adequately characterize the lower plateau, linear phase, and upper plateau of the curve [21]. Doses should be spaced appropriately, often using logarithmic increments (e.g., 1, 10, 100, 1000 nM) to better visualize the sigmoidal shape and distribute data points equally across the curve [21].
Response Measurement: Quantify effects under steady-state conditions or at the time of peak effect to establish a consistent dose-response relationship independent of time [19]. Responses can be measured at various biological levels, including molecular interactions (e.g., receptor binding), cellular responses (e.g., proliferation, death), tissue effects (e.g., muscle contraction), or whole-organism outcomes (e.g., blood pressure changes) [1].
Data Transformation: Apply logarithmic transformation to dose values when concentrations span several orders of magnitude [21]. Response data may be normalized to percentage values, with the minimum and maximum control responses set to 0% and 100%, respectively, to facilitate comparison across experiments [21].
Curve Fitting: Implement nonlinear regression analysis using appropriate models such as the four-parameter logistic (4PL) equation: Y = Bottom + (Top - Bottom)/(1 + 10^((LogEC50 - X) × HillSlope)), where X is the logarithm of concentration and Y is the response [21]. Constrain parameters when necessary based on biological plausibility (e.g., fixing the bottom plateau to 0% for essential processes) [21].
Parameter Estimation: Derive key parameters including EC50/IC50, Hill slope, and maximal efficacy from the fitted curve [21]. Evaluate the reliability of these estimates by assessing confidence intervals and goodness-of-fit measures.
Quality Assessment: Verify that the fitted curve adequately describes the data points, with the EC50/IC50 falling within the tested concentration range and plateaus reasonably aligned with control values [21].
Diagram 1: Experimental workflow for characterizing sigmoidal dose-response relationships, showing key steps from experimental design through data analysis and quality assessment.
Research Reagent Solutions for Sigmoidal Response Experiments
Table 2: Essential Reagents for Dose-Response Experiments
| Reagent Category | Specific Examples | Function in Experiment |
|---|---|---|
| Agonists | Full agonists (e.g., nicotine, isoprenaline) [1] | Elicit stimulatory or inhibitory responses; used to characterize receptor activation |
| Antagonists | Competitive antagonists (e.g., propranolol) [1] | Inhibit agonist effects; used to determine receptor specificity and mechanism |
| Allosteric Modulators | Benzodiazepines [1] | Bind to separate sites to enhance or reduce receptor responses; probe complex pharmacology |
| Cell Viability Assays | MTT, ATP-based assays [22] | Quantify cellular responses to drug treatments; measure cytotoxicity or proliferation |
| Signal Transduction Reporters | Calcium-sensitive dyes, cAMP assays [1] | Monitor intracellular signaling events downstream of receptor activation |
| Radioligands | ^3H- or ^125I-labeled compounds [23] | Directly measure receptor binding parameters (affinity, density) |
Linear Dose-Response Curves
Characteristics and Biological Context
Linear dose-response relationships demonstrate a direct proportionality between dose and effect across the tested concentration range without apparent saturation [24]. Unlike sigmoidal curves, linear relationships lack distinct plateaus and inflection points, resulting in a straight-line relationship when plotted on arithmetic coordinates. In preclinical research, linear responses are frequently observed in studies of nutrient effects, essential mineral supplementation, or toxicant exposure within limited concentration ranges [25]. The linear no-threshold (LNT) model, particularly relevant in radiation toxicology, represents a specific application of linear dose-response relationships that assumes cancer risk increases proportionally with dose without a threshold [1].
The biological interpretation of linear relationships varies significantly by context. In some cases, linearity reflects a system with vast receptor capacity or metabolic processes that have not reached saturation within the tested range [19]. In complex interventions such as psychotherapy research, linear relationships may emerge in the Good Enough Level (GEL) model, where the rate of improvement shows a linear relationship with the number of therapy sessions, though the strength of this relationship may vary with total dose [24]. It is important to note that apparent linearity may sometimes result from testing a limited range of concentrations that captures only the central portion of what would otherwise be a sigmoidal relationship.
Methodological Considerations for Linear Relationships
The accurate characterization of linear dose-response relationships presents distinct methodological challenges:
Range Determination: Establish that the tested concentrations adequately represent the biologically relevant range, as linear relationships may transition to nonlinear patterns (plateaus or declines) outside the observed window [21].
Model Selection: Apply appropriate statistical models, including linear regression (Y = a + bX) or random coefficient models for longitudinal data [24]. For repeated measures, multilevel modeling approaches can account for within-subject correlations [24].
Threshold Testing: Evaluate whether the relationship truly lacks a threshold by testing concentrations approaching zero effect. The potential for threshold effects should be carefully considered, as their presence would invalidate strict linearity [1].
Causal Inference: Exercise caution in interpreting linear relationships from observational data, as apparent dose-response patterns may reflect confounding factors rather than causal relationships [24]. Randomized designs strengthen causal interpretations.
Biphasic Dose-Response Curves
Characteristics and Hormetic Responses
Biphasic dose-response curves, characterized by two distinct response phases—typically low-dose stimulation and high-dose inhibition—represent biologically complex relationships that challenge traditional monotonic models [25]. This phenomenon, often termed hormesis, manifests as an adaptive overcompensation to low-level stressor exposure, followed by the expected toxic effects at higher doses [25]. The most consistent quantitative feature of hormetic-biphasic dose responses is the modest stimulatory response, typically only 30-60% greater than control values, observed across biological models, levels of organization, and endpoints [25]. This consistent quantitative signature suggests common underlying mechanisms related to adaptive biological responses.
The biological basis for biphasic responses involves the activation of compensatory processes at low doses that become overwhelmed at higher exposures [25]. In multi-site phosphorylation systems, for example, biphasic responses can emerge from distributive mechanisms involving a single kinase/phosphatase pair, where a hidden competing effect creates the characteristic low-dose stimulation and high-dose inhibition [25]. Similarly, in low-level laser (light) therapy, biphasic patterns observed in vitro (e.g., in ATP production and mitochondrial membrane potential) and in vivo (e.g., in neurological effects in traumatic brain injury models) reflect the Janus nature of reactive oxygen species, which act as beneficial signaling molecules at low concentrations but become harmful cytotoxic agents at high concentrations [25].
Experimental Protocols for Biphasic Response Characterization
The reliable detection and quantification of biphasic dose-response relationships require specialized methodological approaches:
Expanded Dose Range: Implement extended dose ranges that include very low concentrations (often below traditional testing levels) to adequately capture the stimulatory phase [25]. The hormetic zone may shift depending on experimental conditions, requiring careful range-finding studies.
Increased Replication: Enhance statistical power through increased replication, particularly at potential transition points between phases, as biphasic responses often exhibit subtle effects that may be obscured by experimental variability.
Alternative Modeling Approaches: Employ flexible modeling strategies that can accommodate non-monotonicity, such as Gaussian process regression or multiphasic functions [22] [26]. These approaches can quantify uncertainty and identify complex curve shapes without strong a priori assumptions.
Mechanistic Investigation: Design follow-up experiments to elucidate underlying mechanisms when biphasic responses are observed. This may include measuring adaptive response markers, stress pathway activation, or feedback inhibition processes.
Diagram 2: Proposed biological mechanism for biphasic (hormetic) dose-response relationships, showing the transition from adaptive stimulation at low doses to toxicity at high doses.
Complex Biphasic Patterns in Experimental Systems
Biphasic responses manifest across diverse experimental systems, each with distinct methodological implications:
Radiation Exposure: Triphasic dose responses comprising ultra-low-dose inhibition, low-dose stimulation, and high-dose inhibition have been observed in zebrafish embryos exposed to X-rays, with the hormetic zone shifting toward lower doses with application of filters [25]. This pattern suggests that previously reported biphasic responses might represent incomplete characterization of more complex triphasic relationships.
Alcohol Effects: The acute biphasic effects of alcohol on probability discounting (decision-making under uncertainty) vary across the ascending and descending limbs of the blood alcohol concentration curve, reflecting differential engagement of stimulatory and sedative processes [25]. This temporal dimension adds complexity to biphasic response characterization.
Insulin Signaling: Natural systems exploit differential dose responses, as demonstrated by insulin receptors that recognize various ligands with different binding affinities to trigger appropriate metabolic or mitogenic responses through biphasic mechanisms [20].
Comparative Analysis and Interpretation Framework
Integrated Comparison of Curve Shapes
Table 3: Comprehensive Comparison of Dose-Response Curve Shapes
| Characteristic | Sigmoidal | Linear | Biphasic |
|---|---|---|---|
| Shape Description | S-shaped curve with lower plateau, steep phase, upper plateau | Straight-line relationship between dose and response | Two distinct phases: low-dose stimulation, high-dose inhibition |
| Key Parameters | EC50/IC50, Hill slope, Emax, baseline | Slope, intercept | Transition dose, maximum stimulation, inhibition parameters |
| Biological Interpretation | Receptor saturation, cooperative binding | Unsaturated systems, additive effects | Adaptive responses, overload mechanisms |
| Common Contexts | Receptor-ligand interactions, enzyme kinetics [1] | Nutrient effects, radiation risk (LNT) [1] | Hormesis, low-level stress responses [25] |
| Experimental Considerations | 5-10 doses, logarithmic spacing [21] | Linear spacing may suffice | Expanded low-dose range, increased replication [25] |
| Modeling Approaches | Hill equation, 4PL, Emax model [1] [21] | Linear regression, random coefficients | Gaussian processes, multiphasic models [22] |
| Potential Pitfalls | Misinterpretation with limited dose range | Assumption of linearity beyond tested range | Overinterpretation of variable data |
Decision Framework for Curve Interpretation
The accurate interpretation of dose-response curves in preclinical research requires a systematic approach that considers both experimental design factors and biological context:
Range Assessment: Evaluate whether the tested concentration range adequately captures the biologically relevant spectrum. Incomplete curves (missing plateaus for sigmoidal relationships or transition zones for biphasic responses) represent a common source of misinterpretation [21].
Model Selection Criteria: Choose appropriate models based on biological plausibility, statistical fit, and parameter stability. For novel compounds without established mechanisms, flexible approaches such as Gaussian process regression can quantify uncertainty and identify unexpected curve shapes [22].
Context Integration: Consider system-specific factors that influence curve shape, including exposure duration, metabolic pathways, homeostatic mechanisms, and feedback loops. Dose-response relationships may vary significantly with exposure time and route [1].
Validation Strategies: Implement confirmatory experiments using orthogonal approaches when unexpected curve shapes emerge. For example, biphasic responses should be verified through mechanistic studies exploring proposed adaptive processes [25].
Reporting Standards: Document complete methodological details, including dose selection rationale, spacing, replication, normalization procedures, and model constraints, to enable accurate interpretation and replication [21].
The interpretation of dose-response curve shapes—sigmoidal, linear, and biphasic—represents a critical competency in preclinical drug development. Each curve shape provides distinct insights into compound potency, efficacy, and mechanism of action, with direct implications for lead optimization, toxicity assessment, and clinical translation. Sigmoidal curves, the most prevalent in pharmacology, reveal saturation kinetics and cooperative binding through their characteristic parameters. Linear relationships, while less common in receptor pharmacology, emerge in specific contexts including nutrient effects and radiation risk modeling. Biphasic curves challenge traditional monotonic paradigms and highlight the complex adaptive capacity of biological systems.
The reliable characterization of these relationships demands rigorous experimental design, appropriate statistical modeling, and nuanced biological interpretation. As drug development increasingly focuses on targeted therapies and complex biological systems, advanced methodological approaches including model-based inference, Bayesian frameworks, and uncertainty quantification will enhance the accurate interpretation of dose-response relationships [18] [22]. By applying the principles and protocols outlined in this technical guide, preclinical researchers can optimize compound selection, elucidate mechanisms of action, and strengthen the foundation for clinical translation, ultimately advancing therapeutic development through more sophisticated interpretation of dose-response curves.
In preclinical drug development, the dose-response curve is a fundamental tool for quantifying drug-receptor interactions and predicting therapeutic potential. These curves graphically represent the relationship between the concentration of a drug and the magnitude of its effect on a biological system [27]. The precise morphology of these curves—their position, slope, and maximum height—provides critical information about a compound's pharmacological activity, potency, and efficacy. Proper interpretation of these parameters allows researchers to classify drugs as agonists, antagonists, or more complex variants, and to predict their behavior in more complex biological systems [28].
The analysis of curve morphology extends beyond simple classification. Through quantitative methods like Schild analysis, researchers can determine fundamental constants describing drug-receptor interactions, particularly the equilibrium dissociation constant (KB) for competitive antagonists [27]. This guide details how different drug types mechanistically influence dose-response curve morphology and provides the methodological framework for its accurate interpretation in preclinical research.
Core Pharmacological Concepts
Defining Agonists and Antagonists
At the most fundamental level, drugs interacting with receptors can be categorized based on their intrinsic activity:
- Agonists: Molecules that bind to a receptor (affinity) and activate it to produce a cellular response (intrinsic efficacy) [28]. A full agonist produces the maximal system response, while a partial agonist produces a submaximal response, even at full receptor occupancy [29].
- Antagonists: Molecules that bind to the receptor (affinity) but possess zero intrinsic efficacy. They block or dampen the effect of an agonist but produce no effect themselves [28] [29].
- Inverse Agonists: A special class that binds to receptors and suppresses their basal, constitutive (spontaneous) activity, producing an effect opposite to that of an agonist [29].
Advanced Concepts: Constitutive Activity and Functional Selectivity
Modern pharmacology has moved beyond the simple agonist-antagonist dichotomy. Two key concepts refine our understanding:
- Constitutive Receptor Activity: Traditional theory held that receptors are quiescent until activated by a ligand. It is now established that many receptors can spontaneously adopt an active state and signal in the absence of an agonist [29]. This constitutive activity is a system-dependent property that can influence dose-response curves.
- Functional Selectivity (Biased Agonism): A single drug, acting at one receptor subtype, can have multiple intrinsic efficacies that differ depending on which downstream signaling pathway is measured. This means a drug can simultaneously act as an agonist for one pathway and an antagonist for another pathway coupled to the same receptor [29].
Quantitative Analysis of Curve Morphology
The Impact of Agonists on Curve Morphology
Agonists define the control dose-response curve from which all antagonism is measured. The key parameters derived from this curve are:
- Potency (EC50): The concentration of agonist that produces 50% of the maximal response. A lower EC50 indicates higher potency.
- Efficacy (Emax): The maximal response achievable by the agonist.
The intrinsic efficacy of an agonist primarily influences the Emax of the curve. A full agonist will produce the system's maximum response, while a partial agonist will produce a submaximal Emax [29]. The affinity of the agonist primarily influences the EC50 value.
The Impact of Antagonists on Curve Morphology
Antagonists alter the agonist's dose-response curve in characteristic ways that reveal their mechanism of action. The quantitative differences are summarized in Table 1.
Table 1: Quantitative Impact of Antagonist Types on Agonist Dose-Response Curves
| Antagonist Type | Mechanism of Action | Effect on Agonist EC50 | Effect on Agonist Emax | Surmountable by Agonist? |
|---|---|---|---|---|
| Competitive Reversible | Binds reversibly to the same site as the agonist [28]. | Increases (rightward shift) [27] [28]. | No change [28]. | Yes [28]. |
| Competitive Irreversible | Binds irreversibly to the agonist binding site [28]. | Increases. | Decreases [28]. | No [28]. |
| Non-competitive | Binds to an allosteric site, impairing receptor function without blocking agonist binding [28]. | May or may not change. | Decreases [28]. | No [28]. |
Schild Analysis: The Gold Standard for Quantifying Competitive Antagonism
For reversible competitive antagonists, Schild analysis is the preferred method for determining the antagonist's equilibrium constant (KB), a system-independent measure of its affinity [27]. This method is superior to simpler measures like the IC50, which is highly dependent on the experimental conditions, such as the concentration of agonist used [27].
Experimental Protocol for Schild Analysis:
- Generate a control curve: Construct a full dose-response curve for the agonist in the absence of antagonist.
- Generate shifted curves: Repeat the agonist dose-response curve in the presence of at least three different, fixed concentrations of the antagonist [27].
- Calculate the dose ratio (r): For each antagonist concentration [B], calculate the dose ratio at the EC50 level:
r = EC<sub>50,antagonist</sub> / EC<sub>50,control</sub>. - Construct the Schild plot: Plot
log(r - 1)versuslog[B]. - Determine KB: If the plot is linear with a slope of 1, the antagonism is competitive. The X-intercept is equal to
-log(K<sub>B</sub>), allowing direct calculation of the KB [27].
The following diagram illustrates the logical workflow and key outputs of Schild analysis:
Experimental Protocols and the Scientist's Toolkit
Key Methodologies for Curve Generation
Reliable dose-response data requires rigorous experimental design. Below are detailed protocols for core methodologies.
Protocol 1: Functional Dose-Response Curve Assay (e.g., for a Gαs-Coupled GPCR)
- Cell Preparation: Culture cells expressing the target receptor. Seed into multi-well plates at a density ensuring sub-confluent growth at the time of assay.
- Agonist Dilution Series: Prepare a stock solution of the agonist and perform serial dilutions (typically 1:3 or 1:10) in assay buffer to create a concentration range covering expected sub-threshold to maximal effects. Include a vehicle control.
- Stimulation and Response Measurement:
- For a cAMP assay, replace medium with stimulation buffer containing phosphodiesterase inhibitor.
- Add agonist dilutions to respective wells and incubate for a predetermined time (e.g., 30 min at 37°C).
- Lyse cells and quantify accumulated cAMP using a HTRF, ELISA, or AlphaScreen kit according to the manufacturer's instructions.
- Data Analysis: Normalize response data as a percentage of the maximal agonist response. Fit the log(agonist) vs. response data to a four-parameter logistic equation to determine EC50 and Emax.
Protocol 2: Schild Analysis for Antagonist Characterization
- Control Curve: Perform Protocol 1 to generate a control agonist curve.
- Antagonist Pre-incubation: Prepare separate cell samples with at least three increasing concentrations of the antagonist. Include a vehicle control for the antagonist. Pre-incubate for a time sufficient to reach equilibrium (e.g., 30-60 min).
- Agonist Challenge in Antagonist Presence: Without washing out the antagonist, generate a full agonist dose-response curve in each pre-incubated sample, as in Protocol 1.
- Data Processing and Schild Plot Construction: Follow the calculation and plotting steps outlined in Section 3.3.
The Scientist's Toolkit: Essential Research Reagents
Successful execution of these protocols depends on high-quality reagents. Table 2 details essential materials and their functions.
Table 2: Key Research Reagent Solutions for Dose-Response Studies
| Reagent / Material | Function / Explanation |
|---|---|
| Clonal Cell Line | Engineered to stably express the human target receptor, ensuring a consistent, reproducible system for screening and characterization [29]. |
| Reference Agonist | A well-characterized full agonist (e.g., Isoprenaline for β-adrenoceptors) used to define the system's maximum response and for benchmarking test compounds [27]. |
| Reference Antagonist | A known competitive antagonist for the target (e.g., Propranolol for β-adrenoceptors) used as a positive control in antagonism assays and for validating the Schild analysis method [27]. |
| Signal Detection Kit | Commercial kits (e.g., HTRF, ELISA) for quantifying second messengers (cAMP, IP1, Ca2+). Essential for measuring functional receptor activation with high sensitivity and throughput. |
| Fluorescent Probes | Radioactive or fluorescently labeled ligand analogs for performing binding studies to directly determine ligand affinity (KD) and receptor density (Bmax). |
| JR-AB2-011 | JR-AB2-011, CAS:2411853-34-2, MF:C17H14Cl2FN3OS, MW:398.28 |
| ELN318463 racemate | ELN318463 racemate, CAS:851600-86-7, MF:C19H20BrClN2O3S, MW:471.79 |
Visualizing Receptor Signaling Pathways
The interaction between a drug and its receptor is only the first step in a cascade of events that leads to a measurable response. The following diagram illustrates the core signaling pathways involved, highlighting the points where different drug types exert their influence.
The meticulous analysis of dose-response curve morphology remains a cornerstone of preclinical pharmacology. Understanding the characteristic shifts and depressions caused by antagonists, and rigorously quantifying these effects via Schild analysis, provides indispensable insights into mechanism of action and drug affinity [27]. Furthermore, incorporating modern concepts like constitutive activity and functional selectivity is no longer optional for comprehensive drug characterization [29]. These principles explain complex behaviors that traditional models cannot, such as how a drug can act as an agonist in one tissue and an antagonist in another. Mastery of these concepts and techniques ensures that researchers can accurately interpret complex biological data, de-risk drug development projects, and select the most promising candidates for advancement into clinical trials.
The Importance of Threshold Doses and the Linear No-Threshold Model Debate
In preclinical drug development, determining the relationship between the dose of a compound and its resulting biological effect is a fundamental task. This dose-response relationship is critical for understanding a drug's efficacy, safety, and therapeutic window [30]. The conceptual models used to interpret these relationships have profound implications for risk assessment and therapeutic optimization. The linear no-threshold (LNT) model represents one end of the theoretical spectrum, postulating that any dose greater than zero carries some risk, with response increasing linearly from the origin without a threshold [31] [32]. This model stands in contrast to threshold models, which propose the existence of a dose level below which no significant adverse effect occurs, and hormetic models, which suggest that very low doses may actually produce beneficial stimulatory effects [31] [32].
The debate between these models extends beyond theoretical interest, directly impacting how researchers design experiments, interpret data, and establish safety margins for clinical translation. For drug development professionals, this debate influences decisions ranging from initial compound screening to final dose justification for regulatory submission [30]. Approximately 16% of drugs that failed their first FDA review cycle were rejected due to uncertainties in dose selection rationale, highlighting the critical importance of accurate dose-response characterization [30]. Furthermore, about 20% of FDA-approved new molecular entities eventually required label changes regarding dosing after approval, indicating persistent challenges in establishing optimal dosing regimens [30].
The Linear No-Threshold Model: Foundations and Controversies
Historical Development and Scientific Basis
The LNT model has its origins in early 20th-century radiation biology. In 1927, Hermann Muller demonstrated that radiation could cause genetic mutations, for which he received a Nobel Prize [31]. In his Nobel lecture, Muller asserted that mutation frequency was "directly and simply proportional to the dose of irradiation applied" and that there was "no threshold dose" [31]. This concept gained further support from studies by Gilbert N. Lewis and Alex Olson, who proposed that genomic mutation occurred proportionally to radiation dose [31].
The model was solidified in regulatory frameworks through a series of developments from the 1950s to the 1970s. In 1954, the National Council on Radiation Protection (NCRP) introduced the concept of maximum permissible dose, replacing the earlier tolerance dose concept [33]. The Atomic Energy Commission (AEC) subsequently introduced the ALARA principle ("As Low As Reasonably Achievable") in 1972, which implicitly accepted the LNT model by suggesting that any dose, no matter how small, carries some risk [33]. This was further reinforced by the 1972 BEIR (Biological Effects of Ionizing Radiation) report, which provided cancer risk estimates based on linear extrapolation from high-dose data [33].
The LNT model serves as a conservative default in regulatory toxicology because it simplifies risk assessment, especially when data at low doses are limited or uncertain [34] [35]. Regulatory bodies such as the U.S. Nuclear Regulatory Commission (NRC) and the Environmental Protection Agency (EPA) employ the LNT model for establishing protective standards, operating under the precautionary principle that it is better to overestimate than underestimate potential risks [31] [35].
Ongoing Scientific Debate and Challenges
Despite its regulatory acceptance, the LNT model remains scientifically contentious. Critics argue that the model may be overly conservative, potentially leading to excessive regulatory compliance costs without commensurate public health benefits [34] [35]. The model has been challenged on several biological grounds:
- Defense Mechanisms: Opponents note that the LNT model does not fully account for the body's sophisticated defense mechanisms, including DNA repair processes and programmed cell death, which may effectively handle low-level exposures to carcinogens [31].
- Immune Stimulation: Evidence suggests that the immune system response to radiation exposure is nonlinear, with high doses being immunosuppressive while low doses may actually stimulate immune function [32]. This biphasic response contradicts the fundamental assumption of the LNT model.
- Adaptive Responses: Research has documented adaptive responses where low doses of stressors may precondition organisms to better handle subsequent higher doses [33]. The 1994 UNSCEAR report devoted significant attention to these adaptive responses to radiation in cells and organisms [33].
The fundamental challenge in resolving this debate is the epidemiological difficulty of detecting small effects at low doses against background cancer incidence [31] [35]. As noted in the search results, "roughly 4 out of 10 people will develop cancer in their lifetimes" from various causes, making it "functionally impossible" to quantify cancer risk from low-dose radiation exposure well below background levels [35]. This statistical limitation means that the LNT model's applicability at low doses remains an extrapolation rather than an observationally verified fact.
Table 1: Alternative Dose-Response Models in Toxicological Risk Assessment
| Model Type | Fundamental Premise | Regulatory Application | Key Limitations |
|---|---|---|---|
| Linear No-Threshold (LNT) | Risk increases linearly from zero dose; no safe threshold exists | Default model for radiation and carcinogen risk assessment | May overestimate risk at low doses; ignores biological defense mechanisms |
| Threshold | No significant risk below a certain dose threshold | Standard for most toxicological endpoints (e.g., organ toxicity) | Threshold determination has uncertainty; may not protect hypersensitive subpopulations |
| Hormesis | Low doses are beneficial or protective; high doses are harmful | Not routinely used in regulatory settings | Difficult to distinguish from background variation; reproducibility concerns |
Threshold Doses in Preclinical Drug Development
Defining Threshold Concepts in Pharmacology
In preclinical pharmacology, threshold doses represent critical transition points in dose-response relationships. The No Observable Adverse Effect Level (NOAEL) is a fundamental threshold concept, defined as the highest dose at which no statistically or biologically significant adverse effects are observed [36]. Closely related is the Human Equivalent Dose (HED), derived from animal NOAELs and used to establish the Maximum Safe Starting Dose for first-in-human (FIH) clinical trials [36]. These thresholds are essential for determining the therapeutic window - the range between the minimally effective dose and the dose where unacceptable adverse effects occur [36].
The determination of these threshold values is complicated by the fact that pharmacokinetic parameters often change disproportionately across dose ranges. As noted in the search results, "As dose levels increase many of the key ADME processes can become saturated, significantly changing the exposure profile at higher dose levels in different ways" [36]. This nonlinearity means that exposure parameters (e.g., AUC, Cmax) determined at high doses used in toxicology studies may not accurately predict exposure at therapeutically relevant doses, necessitating dedicated pharmacokinetic studies in the pharmacologically active dose range [36].
Methodological Framework for Dose-Finding
A structured approach to dose-finding is critical for successful drug development. Recent initiatives have introduced formal dose-finding frameworks to organize knowledge and facilitate collaboration in multidisciplinary development teams [30]. These frameworks consist of two main components: (1) knowledge collection to establish common understanding of constraints and assumptions, and (2) strategy building to translate knowledge into a development path [30].
These frameworks emphasize an iterative process that spans all phases of drug development, starting before preclinical studies and continuing through confirmatory trials [30]. The approach helps teams address the challenge that "finding the right treatment at the right dose for the right patient at the right time remains difficult due to a multitude of practical, scientific, and/or financial constraints" [30]. Implementation of such frameworks across more than 25 projects has demonstrated benefits including clearer differentiation of dose-finding strategies for different indications and identification of opportunities to generate additional biomarker data to strengthen exposure-response assessment [30].
Experimental Design for Dose-Response Studies
Preclinical Dose-Response Experimentation
Well-designed preclinical dose-response studies are essential for characterizing a compound's pharmacological profile and informing clinical trial design. In tumour-control assays, a common preclinical model, "the response of individual tumours to treatment is observed until a pre-defined follow-up time is reached" [37]. The fraction of controlled tumours at each dose level forms the tumour-control fraction (TCF), which follows a sigmoidal dose-response relationship that can be modeled using logistic regression [37].
A key consideration in designing these experiments is sample size calculation, which must account for the nonlinear nature of dose-response relationships. Monte-Carlo-based approaches have been developed to estimate the required number of animals in two-arm tumour-control assays comparing dose-modifying factors between control and experimental arms [37]. These methods are particularly important for detecting effects in heterogeneous tumour models with varying radiosensitivity [37].
The selection of appropriate dose levels and spacing is another critical design element. As noted in recent methodological research, "A dose-response design requires more thought relative to a simpler study design, needing parameters for the number of doses, the dose values, and the sample size per dose" [38]. Statistical power calculations guide these parameter choices to ensure reliable comparison of dose-response curves between experimental conditions [38].
Advanced Computational Approaches
Modern computational methods are enhancing dose-response modeling capabilities. Multi-output Gaussian Process (MOGP) models represent an advanced approach that simultaneously predicts responses at all tested doses, enabling assessment of any dose-response summary statistic [39]. Unlike traditional methods that require selection of summary metrics (e.g., ICâ‚…â‚€, AUC), MOGP models describe the relationship between genomic features, chemical properties, and responses across the entire dose range [39].
These models also facilitate biomarker discovery through feature importance analysis using methods like Kullback-Leibler (KL) divergence to identify genomic features most relevant to dose-response relationships [39]. For example, this approach identified EZH2 gene mutation as a novel biomarker of BRAF inhibitor response that had not been detected through conventional ANOVA analysis [39].
Table 2: Essential Research Reagents and Tools for Dose-Response Studies
| Reagent/Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| In Vivo Model Systems | Patient-derived xenografts, genetically engineered models, heterogeneous tumour cohorts [37] | Tumour-control assays, efficacy and potency assessment | Model selection affects translational relevance; heterogeneity requires larger sample sizes |
| Computational Tools | Multi-output Gaussian Process (MOGP) models [39], Monte Carlo simulation [37] | Dose-response prediction, sample size calculation, biomarker discovery | Requires specialized statistical expertise; validated against experimental standards |
| Biomarker Assays | Genomic variation analysis, copy number alteration assessment, DNA methylation profiling [39] | Mechanism of action studies, response biomarker identification | Multi-omics integration improves predictive accuracy; requires appropriate normalization |
Decision Framework for Model Selection
Criteria for Model Application
Selecting an appropriate dose-response model requires consideration of multiple factors. The mechanism of action of the stressor or therapeutic agent should guide model selection. For mutagenic agents that directly damage DNA, the LNT model may be more appropriate, while for agents with receptor-mediated effects, threshold models are generally more applicable [32]. The biological context is equally important, considering factors such as tissue type, repair capacity, and exposure duration [33].
The intended application and regulatory requirements also influence model selection. Risk assessment for public health protection often employs more conservative models like LNT, while therapeutic optimization may focus on accurately characterizing the therapeutic window using threshold concepts [36]. Practical constraints, including the feasibility of collecting sufficient data at low doses to distinguish between models, often dictate the default to LNT as a precautionary approach [34] [35].
Integrated Risk-Benefit Assessment
A comprehensive approach to dose-response interpretation must integrate both risks and benefits. The LNT model focuses exclusively on risk, while threshold and hormesis models incorporate potential benefits at low doses [32]. In drug development, this integration is formalized through the benefit-risk assessment, which quantifies the therapeutic window based on relative exposure-time profiles for both pharmacodynamic and adverse effects [36].
The dose-finding framework mentioned in the search results provides a structure for this integrated assessment, helping teams "establish a common ground of knowns and unknowns about a drug, the disease and target population(s) and the wider development context, and for mapping this knowledge onto viable strategies" [30]. This approach emphasizes starting early in development and revising often as new knowledge is acquired [30].
Decision Framework for Dose-Response Model Selection
The debate between the linear no-threshold model and threshold models represents more than a theoretical scientific dispute—it embodies fundamental differences in approach to risk characterization and therapeutic optimization. For researchers and drug development professionals, understanding the strengths and limitations of each model is essential for appropriate study design and data interpretation.
The LNT model provides a conservative, precautionary approach valuable for public health protection, particularly when data are limited [34] [31]. However, its application may lead to overly stringent standards that do not account for biological defense mechanisms or potential benefits at low doses [31] [32]. Threshold models often better reflect biological reality for many endpoints but require more extensive data to establish no-effect levels [36].
Moving forward, the field will benefit from continued refinement of experimental frameworks that generate high-quality dose-response data across the entire dose spectrum [30] [38]. Additionally, the development of sophisticated computational approaches like multi-output Gaussian Process models will enhance our ability to extract maximum information from limited data [39]. Ultimately, the appropriate model depends on the specific biological context, mechanism of action, and intended application—requiring researchers to exercise informed judgment rather than relying on one-size-fits-all approaches.
As dose-response modeling continues to evolve, the integration of advanced computational methods with rigorous experimental design promises to refine our understanding of threshold phenomena and improve the efficiency of drug development. This progression will better equip researchers to establish therapeutic windows that maximize efficacy while minimizing risk, ultimately benefiting both drug developers and patients.
From Data to Decisions: Practical Methods for Curve Generation, Modeling, and Analysis
In preclinical research, a dose-response curve is a critical tool for quantifying the relationship between the dose or concentration of a substance (e.g., a drug) and the magnitude of the effect it produces in a biological system. Establishing this relationship is fundamental to drug development, as it helps determine crucial parameters like a drug's potency and efficacy. In modern oncology drug development, for example, the focus has shifted from simply finding the maximum tolerated dose (MTD) for cytotoxic drugs to defining the optimal biological dose (OBD) for targeted therapies, which often offers a better efficacy-tolerability balance [7]. Accurately interpreting these curves allows researchers to make informed predictions about therapeutic potential and safety profiles before a candidate drug progresses to clinical trials. This guide provides a detailed protocol for generating, modeling, and interpreting dose-response data, framed within the context of a rigorous preclinical research workflow.
Experimental Design and Data Collection
Key Research Reagents and Materials
A successful dose-response experiment relies on high-quality, well-characterized reagents and a robust experimental design. The table below summarizes essential materials and their functions.
Table 1: Essential Research Reagents and Materials for Dose-Response Experiments
| Item | Function/Description |
|---|---|
| Test Compound | The investigational drug or substance. A pure, stable compound with a known molecular weight and solubility profile is essential. |
| Solvent/Vehicle | A solvent (e.g., DMSO, saline) to dissolve the compound. It must not exert any biological effects on its own at the concentrations used. |
| Biological System | The in vitro model (e.g., cell lines, primary cells, enzymes) or in vivo model (e.g., animal models) used to measure the response. |
| Assay Reagents | Kits and chemicals required to quantify the biological effect (e.g., cell viability assays like MTT, ATP-based luminescence, or target engagement assays). |
| Positive/Negative Controls | Compounds with known activity (positive control) and vehicle-only treatments (negative control) to validate the assay's performance. |
Step-by-Step Experimental Protocol
Compound Preparation:
- Prepare a high-concentration stock solution of the test compound in a suitable vehicle, ensuring complete dissolution.
- Serially dilute the stock to create a range of concentrations (typically 8-12 doses) covering several orders of magnitude (e.g., from 1 nM to 100 µM). Using a logarithmic scale (e.g., half-log or 1:3 serial dilutions) is standard practice.
Treatment and Incubation:
- Apply the compound dilutions to your biological system (e.g., plate cells in a 96-well plate and add compound). Each concentration should be tested in multiple replicates (a minimum of 3 is standard) to account for biological and technical variability.
- Include vehicle-only controls (0% effect) and a control for maximum effect (e.g., a well-characterized inhibitor for 100% inhibition, or a cell lysate for 0% viability).
- Incubate the system for a predetermined time that is physiologically relevant.
Response Measurement:
- After incubation, quantify the biological effect using an appropriate assay. For cell viability, this could be a colorimetric or luminescent assay.
- Record the raw output data (e.g., absorbance, luminescence, fluorescence) for each well.
The following workflow diagram summarizes the key stages of a dose-response experiment.
Figure 1: Dose-Response Experimental Workflow
Data Analysis and Curve Fitting
Data Normalization and Preparation
Before fitting a curve, raw data must be normalized to a percentage of effect relative to the controls.
- For Inhibitory Responses (e.g., cell viability):
Normalized Response (%) = 100 × [1 - (Raw_Data - Min_Effect) / (Max_Effect - Min_Effect)]WhereMax_Effectis the average signal from the vehicle control (0% inhibition) andMin_Effectis the average signal from the maximum inhibition control (100% inhibition).
Curve Fitting with Parametric Models
The normalized data is then fit to a parametric model. The most common model for dose-response data is the four-parameter logistic (4PL) model, also known as the Hill equation:
Y = Bottom + (Top - Bottom) / (1 + 10^((LogIC50 - X) * HillSlope))
Where:
Yis the response.Xis the logarithm of the concentration.Bottomis the minimum response plateau (efficacy of a full antagonist).Topis the maximum response plateau (efficacy of a full agonist).LogIC50orLogEC50is the logarithm of the concentration that produces 50% of the maximal effect. It is a measure of potency.HillSlope(or Hill coefficient) describes the steepness of the curve.
Nonlinear regression is used to find the best-fit parameters. Advanced modeling approaches, such as Multi-output Gaussian Process (MOGP) models, are also being developed to predict full dose-response curves from genomic and chemical features, which can be particularly useful when experimental data is limited [39].
Table 2: Key Parameters Derived from a Fitted Dose-Response Curve
| Parameter | Interpretation | Units |
|---|---|---|
| Top / Bottom | Efficacy: The maximum (Top) and minimum (Bottom) possible effect of the compound. | % Response |
| IC₅₀ / EC₅₀ | Potency: The concentration that gives a 50% effect. IC₅₀ is for inhibition; EC₅₀ is for stimulation. | nM or µM |
| Hill Slope | Cooperativity: A slope >1 suggests positive cooperativity; <1 suggests negative cooperativity. | Unitless |
Interpretation and Applications in Preclinical Research
Extracting Biologically Meaningful Insights
The parameters from the fitted curve provide critical insights for lead optimization and decision-making.
- Potency (ICâ‚…â‚€/ECâ‚…â‚€): This value allows for the comparison of different compounds. A lower ICâ‚…â‚€ indicates a more potent compound. However, potency alone is not sufficient; efficacy and the therapeutic window are often more critical.
- Efficacy (Top/Bottom): A compound with high potency but low efficacy (a low "Top" value for an agonist) may be less therapeutically valuable than a slightly less potent compound with full efficacy.
- Assessing Similarity: In multiregional trials or when comparing subgroups, statistical tests can assess the similarity of dose-response curves. Powerful bootstrap tests have been developed to determine if the maximal deviation between two curves falls below a pre-specified similarity threshold, which is crucial for confirming that a drug's effects are consistent across different populations [40].
Advanced Context: Drug Combinations and Response Surfaces
For drug combinations, the analysis becomes more complex. Instead of a single curve, the response is a surface defined by the concentrations of two drugs. Methods like functional output regression (e.g., the comboKR model) can predict this full, continuous response surface, which is more informative than predicting single synergy scores and allows for the application of various synergy models in post-analysis [41]. The following diagram illustrates the logical process of analyzing a dose-response experiment to support research decisions.
Figure 2: Dose-Response Data Interpretation Logic
Methodological Considerations and Limitations
While dose-response curves are powerful, their interpretation requires careful consideration of the methodological context. A systematic review of methods in complex interventions like psychotherapy highlighted limitations of common approaches, noting that multilevel modeling techniques, while informative, often limit causal interpretations, and that non-parametric methods are constrained by their own assumptions [3]. Furthermore, the traditional approach of determining the maximum tolerated dose (MTD) in the first treatment cycle is often not appropriate for modern targeted therapies, underscoring the need for methods that characterize the full dose-response curve to identify an optimal biological dose (OBD) [7]. No single model can capture all biological phenomena, and the choice of model must be justified by the underlying biology of the system under investigation.
In preclinical drug development, the relationship between the concentration of a drug and the magnitude of its biological effect is fundamental for characterizing pharmacological activity. Dose-response relationships describe the magnitude of a biochemical, cellular, or organismal response as a function of exposure to a stimulus or stressor (typically a chemical) after a certain exposure time [1]. Quantitative analysis of these relationships through mathematical modeling allows researchers to determine safe, hazardous, and beneficial levels of drugs, pollutants, foods, and other substances to which humans or organisms are exposed [1]. The Hill Equation and Emax models represent cornerstone mathematical frameworks in pharmacology for analyzing these relationships, enabling the estimation of critical parameters such as drug potency, efficacy, and therapeutic index [42] [1] [16]. These models provide the foundation for rational dose selection in later-stage clinical trials and ultimately inform public health policy and regulatory decisions [1] [43].
Theoretical Foundations: From Receptor Binding to Response
Law of Mass Action and Receptor Theory
The theoretical foundation for the Hill Equation and Emax models originates from the law of mass action and classical receptor theory [16]. This framework describes the interaction between a drug (agonist molecule, A) and its biological target (receptor, R) as a reversible chemical reaction:
[ A + R \ \leftrightharpoons \ AR ]
where [A], [R], and [AR] represent the concentrations of the agonist, receptor, and agonist-receptor complex, respectively [16]. At equilibrium, the relationship between these components is defined by the equilibrium dissociation constant (Kd):
[ Kd = \frac{k{-1}}{k_1} = \frac{[A][R]}{[AR]} ]
where k₠and k₋₠are the rate constants for the forward and backward reactions, respectively [16]. The Kd represents the concentration of agonist required to occupy 50% of receptors at equilibrium and serves as a measure of binding affinity—a lower Kd indicates higher affinity [44].
The fractional occupancy of receptors is derived from the relationship between [AR] and the total receptor concentration ([R_t] = [R] + [AR]):
[ \frac{[AR]}{[Rt]} = \frac{[A]}{[A] + Kd} ]
This equation describes the proportion of receptors bound to agonist at a given concentration [A] [16]. In the simplest model, the biological effect (E) is directly proportional to fractional occupancy, leading to the fundamental equation:
[ E = E{max} \frac{[A]}{[A] + Kd} ]
where E_max represents the maximum possible effect when all receptors are occupied [16]. This simple relationship establishes the theoretical basis for more sophisticated models that account for the complexities of real biological systems.
Signal Amplification and the Concept of Efficacy
In many biological systems, the relationship between receptor occupancy and effect is not directly proportional due to signal amplification mechanisms [16]. A. J. Clark's early assumption that effect is directly proportional to receptor occupancy and that maximum effect occurs only with full receptor occupancy was challenged by R. P. Stephenson, who demonstrated that a maximum effect can be produced without total occupancy of receptors (spare receptors) [43]. Stephenson introduced the concept of efficacy as a measure of the ability of a drug to activate receptors and cause a response [43]. This theoretical advancement explained why some high-efficacy agonists can produce maximal responses while occupying only a small fraction of available receptors, a phenomenon with significant implications for understanding drug potency and selectivity in preclinical research.
The Hill Equation: Mathematical Formulation and Interpretation
Core Equation and Parameters
The Hill Equation provides a mathematical framework for describing sigmoidal relationships between drug concentration and biological response. The standard form of the equation is:
[ E = E0 + \frac{E{max} \times C^n}{EC_{50}^n + C^n} ]
Where:
- E is the effect at concentration C
- Eâ‚€ is the baseline effect in the absence of drug
- E_max is the maximum possible effect above baseline
- ECâ‚…â‚€ is the concentration that produces 50% of the maximal effect
- n is the Hill coefficient (or slope factor) that describes the steepness of the curve [42] [1] [16]
When the baseline effect Eâ‚€ is zero, the equation simplifies to:
[ E = \frac{E{max} \times C^n}{EC{50}^n + C^n} ]
This equation can be rearranged to show its relationship to a logistic function of the logarithm of concentration:
[ E = \frac{E{max}}{1 + \exp(-n(\ln C - \ln EC{50}))} ]
This form reveals that the Hill Equation describes a sigmoidal relationship between the logarithm of concentration and effect [16].
Biological Interpretation of Parameters
Each parameter in the Hill Equation has specific biological and pharmacological significance:
ECâ‚…â‚€: This parameter represents drug potency, defined as the concentration required to achieve 50% of the maximum effect. Lower ECâ‚…â‚€ values indicate higher potency, meaning less drug is required to elicit a half-maximal response [1] [44]. In preclinical screening, this parameter allows researchers to compare the relative activities of different compounds.
E_max: This parameter represents drug efficacy, defined as the maximum possible response achievable with the drug. It reflects the functional ability of a drug to activate receptors and produce a cellular response, independent of its potency [44]. Compounds with equal efficacy may have different potencies, and vice versa.
Hill coefficient (n): This parameter describes the steepness of the concentration-response relationship. A Hill coefficient of 1 suggests a hyperbolic curve with simple bimolecular binding, while values greater than 1 indicate positive cooperativity in the interaction between drug and receptor [42] [1]. As the Hill coefficient increases, the curve becomes steeper and more closely resembles an "all-or-nothing" response [42].
Table 1: Interpretation of Hill Equation Parameters in Preclinical Research
| Parameter | Pharmacological Term | Biological Interpretation | Research Significance |
|---|---|---|---|
| ECâ‚…â‚€ | Potency | Concentration for half-maximal effect | Compound screening and selection |
| E_max | Efficacy | Maximum possible response | Therapeutic potential assessment |
| n | Hill coefficient | Steepness of curve, cooperativity | Mechanism of action insights |
| Eâ‚€ | Baseline effect | Response without drug | Experimental system validation |
The Emax Model: Extensions and Applications
Relationship to Hill Equation
The Emax model is fundamentally based on the Hill Equation and is used to model continuous-valued effects or responses observed when a drug is administered [16]. In its basic form, the Emax model is identical to the Hill Equation:
[ E = E{max} \frac{C^n}{EC{50}^n + C^n} ]
where E is the observed biological effect, C is the plasma concentration (typically molar concentration), E_max is the maximum possible effect, ECâ‚…â‚€ is the concentration producing 50% of maximum effect, and n is the Hill coefficient describing curve steepness [16]. The Emax model represents a pharmacodynamic model as it models the effect of a drug at a given concentration rather than the concentration-time relationship (pharmacokinetics) [16].
Extended Emax Model Formulations
For more complex biological scenarios, extended versions of the Emax model have been developed:
- Baseline Effect Model: When there is a measurable baseline effect (Eâ‚€) in the absence of drug:
[ E = E0 + E{max} \frac{C^n}{EC_{50}^n + C^n} ]
- Inhibition Model: For drugs that decrease an effect rather than increase it:
[ E = E0 - I{max} \frac{C^n}{IC_{50}^n + C^n} ]
where I_max is the maximum inhibition and ICâ‚…â‚€ is the concentration producing 50% of maximum inhibition [16].
- Multiphasic Models: For dose-response curves with multiple inflection points, a generalized model combining multiple independent processes:
[ E(C) = \prod{i=1}^n Ei(C) = \prod{i=1}^n \left( \frac{{E{\infty}}i \times C^{Hi}}{{EC{50}}i^{Hi} + C^{Hi}} \right) ]
This approach can describe complex responses including combined agonist-antagonist effects or multiple phases of inhibition [45].
Applications in Combination Therapy
The Emax model has been successfully applied to analyze drug combination effects using the Loewe additivity model [46]. This approach defines an interaction index (II) to quantify synergistic, additive, or antagonistic effects:
[ II = \frac{d1}{D{y,1}} + \frac{d2}{D{y,2}} ]
where dâ‚ and dâ‚‚ are combination doses, and D{y,1} and D{y,2} are doses of individual drugs required to produce the same effect y [46]. An interaction index less than 1 indicates synergy, equal to 1 indicates additivity, and greater than 1 indicates antagonism [46]. This quantitative framework is particularly valuable in preclinical development of combination therapies for complex diseases like cancer and AIDS, where multi-drug regimens often show superior efficacy to monotherapies [46].
Experimental Protocols for Dose-Response Analysis
Experimental Design Considerations
Well-designed experiments are essential for generating reliable dose-response data and accurate parameter estimates. Key considerations include:
Concentration Range: Studies should cover a reasonably wide dose/concentration range with appropriate duration to ascertain net drug exposure and the ultimate fate of biomarkers or outcomes [42]. A wide range of systemic drug concentrations is typically required for accurate and precise estimation of pharmacodynamic parameters [42].
Replication: Studies should involve a minimum of two to three doses to adequately estimate the nonlinear parameters of most pharmacodynamic models [42]. For more complex systems, more extensive datasets are required as these models typically incorporate multiple nonlinear processes and pharmacodynamic endpoints [42].
Temporal Aspects: For many drugs, pharmacological effects lag behind plasma concentrations, resulting in hysteresis in effect versus concentration plots [42]. This may require incorporating a "biophase" compartment or effect compartment to model the distributional delay between plasma concentrations and effects [42].
Data Collection and Preprocessing
Proper data collection and preprocessing are critical for robust model fitting:
Assay Considerations: Determine whether data represent free (unbound) or total drug concentrations, and whether measurements include parent drug, active metabolites, or both [47]. The sampling matrix (e.g., plasma vs. whole blood) may influence the pharmacokinetic model and its interpretation [47].
Normalization: Data normalization accounts for plate-to-plate variation in high-throughput screens. Common approaches include:
- % Inhibition = [(Negative Control - Test Value) / (Negative Control - Positive Control)] × 100
- % Activation = [(Test Value - Negative Control) / (Positive Control - Negative Control)] × 100 [10]
Handling of Limits: Assays have a lower limit of quantification (LLOQ) below which concentrations cannot be reliably measured [47]. Methods such as imputing below-LOQ concentrations as 0 or LLOQ/2 have been shown to be inaccurate; specialized statistical methods are preferred for handling censored data [47].
Curve Fitting and Parameter Estimation
Model parameters are typically estimated using nonlinear regression techniques:
Algorithm Selection: The Levenberg-Marquardt algorithm is commonly used for nonlinear regression of dose-response data [10]. For population modeling, more advanced methods like first-order conditional estimation (FOCE) or stochastic approximation expectation-maximization (SAEM) may be employed [47].
Parameter Constraints: Fit parameters (minimum response, maximum response, Hill slope, ECâ‚…â‚€) can be allowed to float freely or constrained based on prior knowledge [10]. For example, constraining the Hill slope to positive values may be appropriate for inhibition assays.
Model Selection: The Bayesian Information Criterion (BIC) is recommended for comparing models with different numbers of parameters, as it penalizes overfitting more strongly than other criteria [45]. A drop in BIC of 2-6 provides "positive" evidence, while a drop greater than 10 provides "very strong" evidence for selecting one model over another [47].
Table 2: Research Reagent Solutions for Dose-Response Experiments
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| Cell-Based Assay Systems (e.g., HCT-8 human ileocecal adenocarcinoma cells) | Model biological system for response measurement | Maintain appropriate culture conditions (e.g., folic acid concentration) [46] |
| Absorbance-Based Viability/Cell Growth Assays | Quantification of biological response | 96-well plate readers measuring absorbance 0-2 units [46] |
| Positive/Negative Control Compounds | Data normalization and quality control | Essential for % inhibition/activation calculations [10] |
| Automated Liquid Handling Systems | High-throughput screening | Enables testing of numerous concentration points and replicates [45] |
| Specialized Software (e.g., CDD Vault, Dr.Fit) | Curve fitting and parameter estimation | Implements Hill Equation with appropriate algorithms [10] [45] |
Visualization of Dose-Response Relationships
Conceptual Workflow for Dose-Response Analysis
The following diagram illustrates the complete workflow from experimental design to model interpretation in dose-response studies:
Dose-Response Analysis Workflow from Experiment to Decision
Model Selection Framework
This diagram illustrates the decision process for selecting appropriate mathematical models based on data characteristics:
Decision Framework for Dose-Response Model Selection
Advanced Applications and Special Considerations
Temporal Aspects: Biophase Distribution Models
For many drugs, a temporal disconnect exists between plasma concentrations and pharmacological effects, resulting in counterclockwise hysteresis in concentration-effect plots [42]. This occurs when distribution to the site of action represents a rate-limiting process. To account for this phenomenon, biophase distribution models incorporate a hypothetical effect compartment linked to the plasma compartment:
[ \frac{dCe}{dt} = k{eo} \times (Cp - Ce) ]
where Câ‚‘ is the drug concentration in the effect compartment (biophase), Câ‚š is the plasma concentration, and kâ‚‘â‚’ is the first-order rate constant for drug transfer into and out of the effect compartment [42]. This approach allows researchers to model the time course of drug effects more accurately and distinguish between pharmacokinetic and pharmacodynamic sources of delay.
Multiphasic Dose-Response Relationships
In cancer pharmacology and other fields, a significant proportion of dose-response curves (approximately 28% in one large screen of 11,650 curves) exhibit multiphasic features that cannot be adequately described by a standard Hill equation [45]. These cases may show:
- Combined agonist-antagonist effects at different concentration ranges
- Multiple inflection points in the inhibitory phase
- Hormetic effects (stimulatory effects at low concentrations, inhibitory at high concentrations) [45]
For such complex responses, automated fitting procedures and software (e.g., Dr.Fit) have been developed that can generate and rank models with varying degrees of multiphasic features [45]. These approaches treat each phase as an independent dose-dependent process and combine them using a multiplicative model:
[ E(C) = \prod{i=1}^n Ei(C) ]
where Eáµ¢(C) represents the contribution of each independent process to the overall response [45].
Population Modeling Approaches
Population pharmacokinetic/pharmacodynamic (PK/PD) modeling uses nonlinear mixed-effects models to study pharmacokinetics at the population level, simultaneously evaluating data from all individuals in a population [47]. This approach:
- Characterizes typical concentration-time courses within a population (structural model)
- Accounts for unexplained random variability (statistical model)
- Identifies subject characteristics (covariates) that explain variability [47]
Population modeling does not require "rich" data (many observations per subject) and can utilize sparse sampling schemes, making it particularly valuable for preclinical and clinical studies where extensive sampling is impractical or unethical [47].
The Hill Equation and Emax models provide fundamental mathematical frameworks for quantitative analysis of dose-response relationships in preclinical research. These models enable researchers to extract critical parameters describing drug potency (ECâ‚…â‚€), efficacy (E_max), and curve steepness (Hill coefficient), facilitating informed decisions in drug discovery and development. Proper experimental design, appropriate model selection, and rigorous parameter estimation are essential for reliable application of these modeling approaches. As drug development advances, these classical models continue to serve as the foundation for more sophisticated approaches addressing complex biological phenomena, including multiphasic responses, temporal delays, and population variability. Mastery of these fundamental modeling techniques remains indispensable for researchers aiming to translate preclinical findings into effective therapeutic strategies.
In preclinical drug discovery, the accurate interpretation of dose-response curves is a foundational activity that bridges early compound screening and first-in-human trials. Uncertainty in establishing a relationship between drug dose and observed biological effect remains a major cause of delay and failure in drug development pipelines. A study examining FDA rejections between 2000 and 2012 found that dose uncertainty was the most frequent reason for denying first-time marketing applications for new molecular entities, resulting in median approval delays of 14.5 months, extending in some cases to 6.5 years [48].
Model-Informed Drug Development (MIDD) has emerged as a powerful quantitative framework to address these challenges. MIDD is defined as "a quantitative framework for prediction and extrapolation, centered on knowledge and inference generated from integrated models of compound, mechanism and disease level data and aimed at improving the quality, efficiency and cost effectiveness of decision making" [49]. This approach integrates diverse data sources—from in vitro studies, preclinical experiments, and clinical trials—into mathematical models that characterize the exposure-response relationship, enabling more informed decision-making throughout the drug development lifecycle.
Among the specific methodologies within the MIDD toolkit, the Multiple Comparisons Procedure - Modelling (MCP-Mod) approach has gained significant regulatory acceptance for efficient dose-response analysis and dose selection [48]. This whitepaper provides an in-depth technical examination of these advanced approaches, with particular focus on their application to interpreting dose-response curves in preclinical research.
Theoretical Foundations: MIDD and MCP-Mod
Model-Informed Drug Development (MIDD)
Core Principles and Regulatory Context
MIDD represents an evolution from traditional drug development approaches by systematically integrating mathematical modeling and simulation into the R&D process. The U.S. Food and Drug Administration (FDA) and other regulatory authorities globally have invested significantly in advancing these approaches, which span the continuum from conception of a drug candidate through post-approval monitoring [50]. The fundamental premise of MIDD is that R&D decisions are "informed" rather than exclusively "based" on model-derived outputs, acknowledging the complementary role of quantitative approaches alongside traditional evidence [49].
The strategic integration of MIDD provides substantial business value and R&D efficiency. Companies like Pfizer and Merck & Co/MSD have reported significant cost savings—up to $100 million annually in clinical trial budgets and $0.5 billion through MIDD-impacted decision-making, respectively [49]. Beyond internal decision-making, MIDD supports regulatory assessment regarding trial design, dose selection, and extrapolation to special populations [49].
Key Modeling Approaches in MIDD
MIDD encompasses a spectrum of quantitative modeling techniques:
- Population Pharmacokinetics (popPK): Characterizes drug disposition and its variability in patient populations.
- Physiologically-Based Pharmacokinetic (PBPK) Modeling: Mechanistically simulates drug absorption, distribution, metabolism, and excretion based on physiology.
- Exposure-Response Modeling: Quantifies relationships between drug exposure (e.g., concentration) and pharmacological effects (efficacy and safety).
- Quantitative Systems Pharmacology (QSP): Integrates drug mechanisms with disease pathophysiology using systems biology approaches.
- Disease Progression Modeling: Mathematically describes the natural time-course of disease and drug effects [51] [50].
MCP-Mod: A Robust Statistical Framework
Conceptual Foundation and Regulatory Acceptance
MCP-Mod (Multiple Comparisons Procedure - Modelling) is an innovative statistical methodology specifically designed for dose-finding studies. It addresses two primary Phase II objectives: (1) establishing proof-of-concept that a drug works as intended, and (2) determining appropriate doses for Phase III testing [48]. Traditionally, dose-response analysis employed either multiple comparison procedures (MCP) or modeling approaches, each with inherent limitations. MCP-Mod integrates both strategies, combining the flexibility of modeling for dose estimation with the robustness of MCP against model misspecification [48].
Regulatory agencies including the FDA (2016) and European Medicines Agency (EMA, 2014) have qualified MCP-Mod as fit-for-purpose for design and analysis of phase 2 dose-finding studies [48]. The FDA has stated that "the methodology is scientifically sound" and "advantageous in that it considers model uncertainty and is efficient in the use of the available data compared to traditional pairwise comparisons" [48].
Technical Implementation
The MCP-Mod procedure operates through a structured, two-stage process:
Stage 1: Trial Design
- Define a suitable study population to represent the underlying true dose-response shape.
- Pre-specify candidate dose-response models based on available information.
- Determine doses and calculate sample size to achieve targeted performance characteristics.
Stage 2: Trial Analysis
- Assess the presence of a dose-response signal using a trend test derived from pre-specified candidate models (MCP step).
- Perform parametric modeling or model averaging to estimate the dose-response relationship and identify the optimal dose for confirmatory trials (Mod step) [48].
This dual approach enables rigorous statistical testing while accommodating the inherent uncertainty in dose-response shape, resulting in higher efficiency and greater robustness compared to traditional methods.
Advanced Methodologies: Integrating MIDD and MCP-Mod in Preclinical Research
Multi-Output Gaussian Process (MOGP) for Dose-Response Modeling
Technical Framework
Recent advances in dose-response modeling have introduced Multi-output Gaussian Process (MOGP) models to address limitations of traditional approaches. Unlike methods that model summary statistics (e.g., ICâ‚…â‚€, AUC) extracted from dose-response curves, MOGP simultaneously predicts all dose-responses and uncovers their biomarkers [39]. This approach describes the relationship between genomic features, chemical properties, and every response at every dose, enabling assessment of drug efficacy using any dose-response metric.
In practical implementation, MOGP models cell viabilities for various dose concentrations as outputs, while employing methods like Kullback-Leibler (KL) divergence to determine feature relevance and importance [39]. This probabilistic framework addresses variability from experimental standards and curve fitting uncertainties, providing confidence intervals and estimating biomarker probability.
Application in Preclinical Context
A study applying MOGP to data from the Genomics of Drug Sensitivity in Cancer (GDSC) demonstrated its effectiveness across ten cancer types and multiple drugs [39]. The approach was particularly valuable for BRAF inhibitor response prediction, where it identified EZH2 gene mutation as a novel predictive biomarker that had not been detected as statistically significant through traditional ANOVA analysis [39]. This demonstrates MOGP's enhanced sensitivity in biomarker discovery from dose-response data.
The MOGP framework offers particular advantages when dealing with limited drug screening experiments for training, maintaining predictive accuracy even with small sample sizes [39]. This characteristic makes it particularly valuable for preclinical research where extensive screening may be resource-prohibitive.
Experimental Design Considerations for Preclinical Dose-Response Studies
Statistical Power and Sample Size
Proper design of in vivo dose-response comparison studies requires careful consideration of multiple parameters: number of doses, dose values, and sample size per dose [38]. Statistical power calculation is essential for differentiating several compounds in terms of efficacy and potency during lead optimization. The MCP-Mod framework facilitates this process by enabling sample size determination based on targeted performance characteristics for the specific candidate models being tested [48].
Dose Selection Strategy
The selection of appropriate dose levels represents a critical design consideration. Optimal dose selection should:
- Cover the anticipated range of activity from no effect to maximum effect
- Include doses sufficiently spaced to detect differences in response
- Incorporate sufficient replication at each dose level to estimate variability
- Consider practical constraints of compound supply and animal use [38]
The integration of MIDD approaches at this stage allows for leveraging prior knowledge from in vitro studies or compounds with similar mechanisms to inform dose selection, potentially reducing the number of dose levels required while maintaining study informativeness.
Practical Implementation: Protocols and Workflows
Integrated MIDD-MCP-Mod Workflow for Preclinical Dose-Response Analysis
The following diagram illustrates the integrated workflow combining MIDD and MCP-Mod approaches for preclinical dose-response analysis:
Experimental Protocol: MOGP for Dose-Response and Biomarker Discovery
Data Collection and Preprocessing
Dose-Response Data Acquisition: Conduct drug screening experiments across multiple dose concentrations (typically 6-8 concentrations in serial dilution). Record cell viability or other relevant response metrics for each dose [39].
Molecular Feature Extraction:
- Collect genetic variations in high-confidence cancer genes
- Obtain copy number alteration (CNA) status of recurrent altered chromosomal segments (RACSs)
- Extract DNA methylation status of informative CpG islands (iCpGs)
- Retrieve chemical features of drugs from databases like PubChem [39]
Data Normalization: Normalize response metrics to account for plate-to-plate variability and control for background effects using appropriate normalization methods (e.g., Z-score, B-score).
Model Training and Validation
MOGP Implementation: Configure MOGP with a coregionalization kernel to model correlations between outputs at different doses. Initialize hyperparameters using maximum likelihood estimation.
Feature Relevance Assessment: Apply Kullback-Leibler (KL) divergence to measure the importance of each genomic and chemical feature. Calculate average KL-Relevance scoring values across multiple cross-validation folds [39].
Model Validation: Perform k-fold cross-validation (typically k=5 or k=10) to assess predictive performance. Evaluate using metrics such as root mean square error (RMSE) for continuous responses or area under the receiver operating characteristic curve (AUC-ROC) for binary responses.
Biomarker Identification and Dose-Response Prediction
Biomarker Discovery: Rank features by their KL-Relevance scores. Compare with traditional statistical approaches (e.g., ANOVA) to identify novel biomarkers that may be missed by conventional methods [39].
Dose-Response Curve Prediction: Use trained MOGP to predict complete dose-response curves for new experiments, including confidence intervals quantifying prediction uncertainty.
Cross-Study Validation: Assess model performance across different cancer types and when training data is limited to evaluate robustness and generalizability [39].
MCP-Mod Experimental Protocol for Preclinical Dose-Finding
Study Design Phase
Candidate Model Selection: Pre-specify a set of candidate dose-response models (typically 4-6 models) representing plausible shapes of the dose-response relationship. Common models include:
- Emax model
- Logistic model
- Linear model
- Quadratic model
- Sigmoid Emax model [48]
Dose Selection: Choose dose levels based on prior knowledge from in vitro studies or similar compounds. Include a vehicle control and sufficient doses to characterize the dose-response relationship.
Sample Size Calculation: Determine sample size per dose group using simulation-based power analysis to achieve target power (typically 80-90%) for detecting a clinically relevant effect size across candidate models.
Data Analysis Phase
MCP Step (Signal Detection):
- For each candidate model, calculate the optimal contrast coefficients
- Compute the test statistics for each candidate model
- Adjust for multiple testing using appropriate methods (e.g., Bonferroni, Dunnett)
- Establish proof-of-concept if at least one model shows statistical significance [48]
Mod Step (Dose-Response Modeling and Dose Selection):
- Select the best-fitting model from the significant candidates using model selection criteria (e.g., Akaike Information Criterion [AIC], Bayesian Information Criterion [BIC])
- Alternatively, use model averaging to combine estimates from multiple models
- Estimate the dose-response relationship using the selected model(s)
- Identify target doses (e.g., ED₅₀, ED₉₀) for further development [48]
Applications and Impact Assessment
MIDD Applications in Drug Development
Table 1: MIDD Applications Across Drug Development Stages
| Development Stage | MIDD Application | Impact |
|---|---|---|
| Early Discovery | In vitro-in vivo extrapolation (IVIVE) | Predicts human pharmacokinetics from in vitro data [51] |
| Preclinical Development | Lead optimization through PBPK modeling | Differentiates compounds for efficacy and potency [38] |
| Phase I | First-in-human dose selection | Determines safe starting dose and dose escalation scheme [50] |
| Phase II | Dose-response characterization using MCP-Mod | Identifies optimal doses for Phase III [48] |
| Phase III | Exposure-response analysis | Supports dosing recommendations in label [51] |
| Regulatory Submission | Pediatric extrapolation | Leverages adult data to minimize pediatric trials [50] |
| Post-Marketing | Model-informed precision dosing | Optimizes dosing for special populations [49] |
Research Reagent Solutions for Dose-Response Studies
Table 2: Essential Research Reagents and Materials for Dose-Response Experiments
| Reagent/Material | Function | Application in Dose-Response Studies |
|---|---|---|
| Cell Lines | In vitro model system | Provide biological context for drug screening; cancer cell lines commonly used [39] |
| Compound Libraries | Source of therapeutic candidates | Enable high-throughput screening across multiple concentrations [39] |
| Viability Assays | Measure cellular response | Quantify effect of drug treatment (e.g., ATP-based, resazurin assays) [39] |
| Genomic Profiling Tools | Characterize molecular features | Identify biomarkers of response (mutations, CNAs, methylation) [39] |
| PBPK Modeling Software | Simulate pharmacokinetics | Predict tissue exposure and inform dose selection [51] [50] |
| Statistical Software | Implement MCP-Mod and MOGP | Perform dose-response analysis and modeling [39] [48] |
The integration of Model-Informed Drug Development approaches with robust statistical methods like MCP-Mod represents a paradigm shift in preclinical dose-response analysis. These methodologies provide a quantitative framework that enhances the efficiency, robustness, and informativeness of dose-response interpretation, directly addressing a major source of failure in drug development pipelines.
The multi-output Gaussian Process (MOGP) approach advances traditional dose-response modeling by simultaneously predicting responses across all doses while identifying biomarkers, offering particular value when dealing with limited experimental data [39]. Meanwhile, MCP-Mod provides a regulatory-endorsed framework for confirmatory dose-response analysis and dose selection [48].
For researchers and drug development professionals, adopting these "beyond basic" approaches requires investment in specialized expertise and tools but offers substantial returns in development efficiency and success rates. As the field evolves, the integration of artificial intelligence, machine learning, and real-world evidence with these established methodologies promises to further enhance their predictive power and application across the drug development continuum [50].
Leveraging Dose-Exposure-Response Relationships for Enhanced Prediction
The successful translation of preclinical findings to clinical applications hinges on a robust understanding of dose-exposure-response (DER) relationships. These relationships form the quantitative foundation for predicting human efficacy and safety, guiding critical decisions in drug development. This whitepaper provides an in-depth technical guide to interpreting dose-response curves within preclinical research, detailing advanced methodological frameworks for analysis, essential experimental protocols, and practical tools for enhancing predictive accuracy. By integrating pharmacokinetic (PK) and pharmacodynamic (PD) modeling with similarity testing, researchers can bridge the translational gap, de-risking the development of novel therapeutics.
In drug development, the dose-exposure-response relationship is a critical pathway that links the administered dose of a compound to its concentration in the body (exposure) and the resulting biological effect (response). In preclinical research, accurately characterizing this relationship is paramount for selecting viable drug candidates and designing first-in-human trials [52].
The core components are:
- Dose: The amount of a drug administered.
- Exposure: The pharmacokinetic (PK) profile of the drug, encompassing its Absorption, Distribution, Metabolism, and Excretion (ADME).
- Response: The pharmacodynamic (PD) effect, which can be either therapeutic (efficacy) or adverse (toxicity).
The primary objective of DER analysis is to build a quantitative model that predicts a drug's behavior in humans based on preclinical data. This model informs key go/no-go decisions and helps establish a safe starting dose and dosing regimen for clinical trials [52].
Quantitative Frameworks for Analysis
Pharmacokinetic-Pharmacodynamic (PK/PD) Modeling
PK/PD modeling integrates two interconnected processes to describe the time course of drug effects. Pharmacokinetics defines what the body does to the drug, while pharmacodynamics defines what the drug does to the body [52].
Table 1: Core Components of Integrated PK/PD Models
| Component | Description | Typical Parameters |
|---|---|---|
| PK Model | Describes the time course of drug concentration in plasma and at the effect site. | Clearance (CL), Volume of Distribution (Vd), Half-life (tâ‚/â‚‚), Bioavailability (F) |
| PD Model | Links the drug concentration at the effect site to the intensity of the observed effect. | Maximum Effect (Eₘâ‚â‚“), Concentration for 50% Effect (ECâ‚…â‚€), Hill Coefficient (γ) |
| Link Model | A mathematical function (e.g., an effect compartment) that accounts for the temporal disconnect between plasma concentration and observed effect. | Rate constant for equilibration (kâ‚‘â‚€) |
These models are essential for establishing dose-exposure-response relationships, which inform dose range finding and safety margins [52].
Statistical Similarity Testing of Dose-Response Curves
In multiregional trials or when comparing subgroups to a full population, it is crucial to determine if dose-response relationships are consistent. Similarity can be assessed by testing if the maximal deviation between two dose-response curves falls below a pre-specified similarity threshold, δ [40].
The statistical hypothesis for a single subgroup comparison is structured as:
- Null Hypothesis (Hâ‚€): The maximum deviation between the subgroup and full population curves is greater than or equal to
δ(i.e., the curves are not similar). - Alternative Hypothesis (Hâ‚): The maximum deviation is less than
δ(i.e., the curves are similar) [40].
This framework employs powerful parametric bootstrap tests to evaluate similarity over the entire dose range, not just at the administered dose levels, providing a more comprehensive assessment [40]. The overall population effect at a dose d is often modeled as a weighted average: μ‾(d, β) = ∑ pℓ * μℓ(d, βℓ), where pℓ represents the proportion of subgroup ℓ in the population, and μℓ is its regional dose-response model [40].
Experimental Protocols and Methodologies
Core Preclinical Workflow for DER Characterization
A systematic, multi-stage approach is required to generate high-quality data for DER modeling.
Detailed Experimental Protocols
Protocol 1: Proof-of-Concept (POC) and Efficacy Modeling
- Objective: To validate that a drug candidate produces the desired therapeutic effect in a relevant disease model and to characterize the initial dose-response relationship [52].
- Methodology:
- Model Selection: Utilize established in vivo disease models (e.g., xenograft models for oncology, induced pathology for other diseases).
- Dosing Regimen: Administer the compound at multiple dose levels, including a vehicle control group. Doses are typically selected based on prior in vitro data.
- Endpoint Measurement: Quantify a relevant biomarker or functional endpoint that accurately reflects the disease modification or therapeutic effect.
- Data Analysis: Fit the response data to standard dose-response models (e.g., Emax model) to estimate the Minimum Effective Dose (MED) [52].
Protocol 2: Integrated PK/PD Study
- Objective: To determine the relationship between the administered dose, the time course of plasma and tissue concentrations, and the resulting pharmacological effect [52].
- Methodology:
- Dosing and Sampling: Administer a single dose (e.g., IV and oral for bioavailability) and collect serial blood samples at predetermined time points.
- Bioanalysis: Use highly sensitive analytical techniques like UPLC-MS/MS to quantify drug concentrations in plasma [52].
- Effect Monitoring: Measure the PD endpoint concurrently with PK sampling.
- Modeling: The PK data are fit to a compartmental model (e.g., two-compartment model). The resulting concentration-time profile is then linked to the effect-time profile using a direct-effect or indirect-response PD model to derive ECâ‚…â‚€ and Emax [52].
Protocol 3: Dose Range Finding (DRF) and Safety Pharmacology
- Objective: To identify the Maximum Tolerated Dose (MTD) and refine the therapeutic window (the range between MED and MTD) [52].
- Methodology:
- Study Design: Conduct subchronic repeated-dose studies in two species (rodent and non-rodent) as per ICH guidelines.
- Endpoint Assessment: Monitor for clinical signs, body weight changes, clinical pathology, and histopathology.
- Data Analysis: The No Observed Adverse Effect Level (NOAEL) is determined from these studies, which is critical for calculating the safety margin for human trials [52].
- Safety Pharmacology: Conduct dedicated studies focused on vital organ systems (cardiovascular, CNS, respiratory) as outlined in ICH S7A and S7B guidelines [52].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following reagents and tools are fundamental for conducting the experiments described in this whitepaper.
Table 2: Key Research Reagent Solutions for DER Studies
| Reagent / Material | Function and Application |
|---|---|
| UPLC-MS/MS Systems | Provides highly sensitive and specific quantification of drug concentrations and biomarkers in biological matrices (e.g., plasma, tissue homogenates) for robust PK and biomarker data [52]. |
| Validated Disease Models | Well-characterized in vivo models (e.g., patient-derived xenografts, genetically engineered models) that reliably recapitulate human disease for meaningful efficacy (POC) testing [52]. |
| Clinical Chemistry & Hematology Analyzers | Automated systems for processing blood samples to assess toxicity and organ function in DRF and toxicology studies by measuring analytes like ALT, AST, creatinine, etc. [52]. |
| Specific Biomarker Assays | Validated immunoassays (e.g., ELISA, MSD) or molecular assays to quantitatively measure PD endpoints and biomarkers of efficacy and toxicity [52]. |
| PK/PD Modeling Software | Professional software platforms (e.g., Phoenix WinNonlin, NONMEM, R) used for non-compartmental analysis, compartmental modeling, and deriving exposure-response relationships [52]. |
| YQ128 | YQ128, CAS:2454246-18-3, MF:C27H29ClN2O4S2, MW:545.11 |
| CYP2A6-IN-2 | CYP2A6-IN-2, MF:C12H16F3N, MW:231.26 g/mol |
Advanced Analytical Visualizations
Logic of Similarity Testing in Dose-Response Analysis
This diagram illustrates the statistical decision process for determining if a subgroup's dose-response curve is similar to the full population's curve.
Integrated PK/PD Modeling Workflow
This chart outlines the sequential process of building and applying an integrated PK/PD model from raw data to clinical prediction.
A rigorous, model-based approach to DER relationships in preclinical research is no longer optional but a necessity for efficient drug development. By systematically integrating PK/PD modeling and statistical similarity testing, researchers can transform raw data into powerful predictive tools. This methodology enables the identification of promising drug candidates with a higher probability of clinical success, ensures patient safety by establishing scientifically justified starting doses, and optimizes resource allocation. Mastering these principles is fundamental to bridging the translational gap and delivering new therapies to patients.
In preclinical research, the dose-response relationship is a cornerstone principle for evaluating the pharmacological and toxicological effects of chemical compounds [1]. Determining the relationship between the dose of a drug and the magnitude of its effect enables researchers to identify safe and effective dosing levels, calculate critical potency parameters, and establish therapeutic windows [53] [19]. Modern analysis of these relationships relies heavily on specialized software tools and statistical programming environments that enable robust curve fitting, parameter estimation, and visualization. This technical guide provides researchers and drug development professionals with comprehensive methodologies for implementing dose-response analysis using R, Python, and specialized packages, framed within the context of a preclinical research workflow.
Core Concepts and Key Parameters
Dose-response curves are typically sigmoidal in shape when response is plotted against the logarithm of the dose [1]. The curve's parameters provide crucial information about a compound's biological activity:
- EC~50~ (Half Maximal Effective Concentration): The concentration that produces 50% of the maximal response, serving as a standard measure of compound potency [53].
- E~max~ (Maximal Efficacy): The greatest attainable response from the drug, representing its maximum biological effect [19].
- Hill Coefficient (n~H~): Describes the steepness of the curve, indicating cooperativity in binding [1].
These parameters are typically derived from fitting experimental data to established mathematical models, most commonly the Hill equation [1]:
[E = E0 + \frac{[A]^n \times E{max}}{[A]^n + EC_{50}^n}]
Where (E) is the effect, ([A]) is the drug concentration, (E0) is the baseline effect, (n) is the Hill coefficient, (E{max}) is the maximum effect, and (EC_{50}) is the half-maximal effective concentration.
Analysis with R
Core Packages and Functions
R provides a comprehensive ecosystem for dose-response analysis through specialized packages. The following table summarizes key packages and their primary functions:
Table 1: Essential R Packages for Dose-Response Analysis
| Package | Primary Function | Key Features | Typical Use Cases |
|---|---|---|---|
| drc [54] | Nonlinear regression analysis | Fits various dose-response models, calculates EC values, compares curves | Standard monophasic curve fitting, potency estimation |
| bmd [54] | Benchmark dose analysis | Derives BMD and BMDL values for risk assessment | Toxicological risk assessment, points of departure |
| ggplot2 [55] | Data visualization | Creates publication-quality graphs with high customization | Visualizing raw data and fitted curves, multi-panel figures |
Implementation Workflow
The following Graphviz diagram illustrates the standard dose-response analysis workflow in R:
Detailed Protocol: Analyzing Tumor Incidence Data
This protocol follows the workflow described in a dose-response modeling training module [54].
1. Environment Setup and Data Loading
2. Data Visualization and Exploration
3. Curve Fitting with drm() Function
4. Benchmark Dose Calculation
5. Final Visualization with Fitted Curve
Analysis with Python
Core Libraries and Functions
Python offers several specialized libraries for dose-response analysis, particularly in high-throughput screening contexts. The following table summarizes the primary tools:
Table 2: Essential Python Libraries for Dose-Response Analysis
| Library/Package | Primary Function | Key Features | Typical Use Cases |
|---|---|---|---|
| curve_curator [56] | Dose-dependent data analysis | Classical 4-parameter fitting, effect potency/size estimation, statistical significance | High-throughput screening, automated curve fitting |
| scipy.optimize | Nonlinear curve fitting | Curve fitting algorithms (least squares) | Custom model implementation |
| matplotlib/seaborn [55] | Data visualization | Static and dynamic plotting capabilities | Creating publication-quality figures |
Implementation Workflow
The following Graphviz diagram illustrates the CurveCurator analysis workflow for high-throughput dose-response data:
Detailed Protocol: High-Throughput Screening Analysis with CurveCurator
CurveCurator is specifically designed for large-scale dose-dependent datasets, using a classical 4-parameter equation to estimate effect potency, effect size, and statistical significance [56].
1. Environment Setup and Installation
2. Configuration File Preparation (TOML Format)
3. Input Data Formatting Create a tab-separated file (viability_screen.txt) with the following structure:
4. Execution and Analysis
5. Output Interpretation CurveCurator generates several output files:
- curve_fits.csv: Contains fitted parameters (EC~50~, E~max~, Hill coefficient) and statistical measures
- dashboard.html: Interactive dashboard for data exploration
- fdr_estimate.csv: False discovery rate estimates (when using -f flag)
Advanced Analysis: Multiphasic Dose-Response Curves
Specialized Tools for Complex Curves
Standard Hill equation modeling assumes a single inflection point, but approximately 28% of cases in large cancer cell viability screens show multiphasic features better described by more complex models [45]. The Dr.Fit software provides specialized capabilities for these scenarios.
Mathematical Framework for Multiphasic Curves For dose-response curves with multiple inflection points, the response E(C) at concentration C can be modeled as:
[E(C) = \prod{i=1}^{n} Ei(C)]
where each phase (E_i(C)) is described by:
[Ei(C) = E{0,i} + \frac{E{\infty,i} - E{0,i}}{1 + \left(\frac{EC{50,i}}{C}\right)^{ni}}]
This approach combines dependent, cooperative effects (Hill model) with independent effects (Bliss approach) [45].
Implementation with Dr.Fit Software
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Dose-Response Experiments
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| Cell Viability Assays (e.g., MTT, CellTiter-Glo) | Quantify live cells after compound treatment | Choose assay compatible with detection method and cell type |
| Chemical Z Stock Solutions [54] | Test compound for dose-response evaluation | Prepare in appropriate solvent, ensure stability |
| Positive Control Compounds | Validate experimental system | Use established reference compounds with known EC~50~ values |
| Vehicle Control Solvents (e.g., DMSO) | Control for solvent effects | Keep concentration constant across all doses |
| Cell Culture Media | Maintain cells during compound exposure | Ensure compatibility with test compounds |
| 96 or 384-well Microplates | High-throughput screening format | Choose plates with low autofluorescence for assay type |
| Vilazodone D8 | Vilazodone D8, MF:C26H27N5O2, MW:449.6 g/mol | Chemical Reagent |
| STOCK2S-26016 | STOCK2S-26016, CAS:2193076-44-5, MF:C20H19N3O2, MW:333.391 | Chemical Reagent |
Quality Control and Validation
Model Selection Criteria
Proper model selection is critical for accurate parameter estimation:
- Bayesian Information Criterion (BIC): Preferred for robust model ranking as it penalizes overfitting more strongly than other criteria [45]
- Visual Inspection: Always visually confirm that the fitted curve appropriately follows the data trends
- Goodness-of-fit Metrics: Evaluate R², residual plots, and confidence intervals of parameter estimates
Handling Common Challenges
- Multiphasic Responses: Use automated fitting procedures that compare multiple models when standard Hill equation fitting proves inadequate [45]
- High-Throughput Data Quality: Implement 2D-thresholding approaches to reduce false positives in large-scale screens [56]
- Outlier Detection: Use Median Absolute Deviation (MAD) analysis to identify problematic experimental replicates [56]
Implementing robust dose-response analysis requires appropriate selection of statistical tools and methodologies tailored to the specific research context. R provides comprehensive capabilities for standard curve fitting and benchmark dose analysis through the drc and bmd packages [54], while Python's curve_curator offers specialized functionality for high-throughput screening environments [56]. For complex multiphasic responses, specialized tools like Dr.Fit enable automated identification and modeling of curves with multiple inflection points [45]. By following the detailed protocols and workflows outlined in this guide, preclinical researchers can ensure accurate quantification of critical pharmacological parameters, ultimately supporting more informed decisions in drug development.
Overcoming Challenges: Troubleshooting Common Pitfalls and Optimizing Experimental Design
In preclinical drug development, the dose-response curve represents a fundamental tool for characterizing the pharmacological profile of a compound, informing critical decisions about efficacy, safety, and first-in-human dosing [4]. However, the reliability of these curves is profoundly dependent on the quality of the underlying data. Issues of biological variability, undetected outliers, and inadequate sample sizes can distort the shape of the curve, leading to inaccurate estimates of key parameters such as potency (EC50/IC50) and efficacy (Emax) [57] [4]. These inaccuracies can misdirect subsequent clinical development, resulting in wasted resources and potential patient risk.
This technical guide examines the core data quality challenges—variability, outliers, and sample size—within the context of preclinical dose-response research. It provides researchers and drug development professionals with structured methodologies to recognize, quantify, and resolve these issues, thereby enhancing the translational potential of preclinical findings.
Fundamental Concepts: The Dose-Response Relationship
Key Parameters of a Dose-Response Curve
The following table summarizes the critical parameters derived from dose-response analysis [4].
| Parameter | Definition | Interpretation in Preclinical Research |
|---|---|---|
| Potency (EC50/IC50) | The concentration of a drug that produces 50% of its maximum effect (EC50) or causes 50% inhibition (IC50). | Indicates the strength of the drug. A lower value denotes higher potency. |
| Efficacy (Emax) | The maximum possible effect a drug can produce, regardless of dose. | Reflects the therapeutic potential and biological capability of the drug. |
| Slope | The steepness of the linear portion of the curve. | Suggests the number of drug molecules required to elicit a response and can indicate the mechanism of action. |
| Therapeutic Window | The range between the minimum effective dose and the dose where toxicity begins. | Assessed by comparing efficacy and toxicity curves; crucial for predicting safety margins. |
The Shape of the Curve: Beyond the Simple Sigmoid
While many drug molecules follow a classic sigmoidal curve when response is plotted against the logarithm of the dose, not all relationships are this straightforward [4]. A significant proportion of dose-response curves exhibit multiphasic features, which represent a combination of stimulatory and inhibitory effects [4]. Recognizing these complex shapes is vital, as forcing a monophasic model can lead to a fundamental misinterpretation of the drug's biological activity. Other causes of nonlinearity include a drug acting on multiple receptors or metabolic saturation [4].
Recognizing and Quantifying Data Quality Issues
Biological and Technical Variability
Variability introduces "noise" that can obscure the true "signal" of a drug's effect. Biological variability stems from inherent differences in experimental models, while technical variability arises from measurement instruments, reagent batches, and operator techniques [57]. High variability flattens the dose-response curve, making it difficult to accurately determine the EC50 and the steepness of the slope.
Quantification: Calculate the standard deviation (SD) and coefficient of variation (CV) for replicate measurements at each dose level. A high CV relative to the effect size indicates a problematic signal-to-noise ratio.
Outliers
Outliers are data points that deviate markedly from other observations and can significantly skew curve-fitting algorithms. They may be caused by technical errors (e.g., pipetting mistakes, instrument glitches) or genuine biological phenomena [58].
Identification: Use statistical tests like Grubbs' test or the ROUT method (Q=1%) to identify outliers objectively. However, the criteria for outlier exclusion must be defined a priori in the experimental protocol to prevent data manipulation [57] [59].
Inadequate Sample Size
An underpowered study with a small sample size is a pervasive source of poor data quality in preclinical research [57] [60]. It reduces the precision of parameter estimates and increases the likelihood of both false-positive (Type I) and false-negative (Type II) errors. This is particularly critical for dose-response studies, where the goal is to model a continuous relationship accurately.
Consequences: Inadequate sample size leads to wide confidence intervals around EC50 and Emax estimates, making it difficult to distinguish a true biphasic curve from a monophasic one with high noise, or to reliably detect a shallow slope [57].
Resolving Data Quality Issues: Experimental Protocols and Statistical Methods
Strategies to Mitigate Variability
- Standardization of Protocols: Implement and document Standard Operating Procedures (SOPs) for all experimental steps, including animal handling, cell culture, and analytical techniques [58].
- Environmental Controls: Rigorously control environmental factors such as temperature, humidity, and light cycles for in vivo studies.
- Replication: Include a sufficient number of technical and biological replicates. Technical replicates assess the precision of the measurement, while biological replicates assess the effect across different subjects or samples, providing a better estimate of population variability [57].
- Randomization and Blinding: Randomize the order of treatments and sample processing to avoid systematic bias. Use blinding during data collection and analysis to prevent subconscious influence on results [57] [61].
A Framework for Handling Outliers
- Predefine Criteria: Before starting the experiment, define in the statistical analysis plan which outlier test will be used and the significance threshold (e.g., p < 0.01 for the Grubbs' test) [59].
- Document and Investigate: When an outlier is identified, document the event thoroughly. Investigate potential technical causes by reviewing laboratory notebooks and instrument logs.
- Analyze with and without: Perform the primary data analysis both with and without the outlier. If the overall conclusion (e.g., the estimated EC50) changes significantly upon removal, the results should be interpreted with extreme caution.
- Use Robust Regression: For curve fitting, consider robust regression methods that are less sensitive to outliers than ordinary least squares regression.
Determining an Adequate Sample Size
Sample size calculation is an ethical imperative, as an overly small sample is unscientific and an overly large one is wasteful [60]. The calculation must be performed a priori and requires the following inputs [57]:
- Desired Power (1-β): Typically set at 80% or 90%. This is the probability of detecting a true effect.
- Significance Level (α): Typically set at 0.05.
- Effect Size (δ): The minimum biologically relevant difference you wish to detect (e.g., a 20% change in response).
- Variability (σ): An estimate of the standard deviation of the outcome, often obtained from pilot data or previous literature.
Illustration: For a study comparing the mean grip strength between a treated and untreated animal group (assuming a normal distribution), the required sample size per group (n) can be calculated. With α=0.05, power=80%, a mean of 400g (untreated), and a standard deviation of 20g, detecting an effect size of 40g requires only ~5 rats per group. However, to detect a smaller effect of 20g, the required sample size increases to ~16 per group [57].
The table below contrasts the sample size required for a continuous outcome versus a binary outcome derived from the same underlying data, highlighting the efficiency of continuous measurements [57].
| Outcome Type | Scenario Description | Total Sample Size Required (Power ≥80%) |
|---|---|---|
| Continuous | Compare mean grip strength (placebo: 400g, treated: 440g, SD: 20g). | 10 animals |
| Binary | Compare proportion with grip strength ≥430g (placebo: 6.68%, treated: 30.85%). | 74 animals |
| Binary | Compare proportion with grip strength ≥425g (placebo: 10.56%, treated: 22.66%). | 296 animals |
The Scientist's Toolkit: Essential Reagents and Research Solutions
| Tool / Reagent | Function in Dose-Response Studies |
|---|---|
| Cell-Based Assay Systems (e.g., FLIPR Penta) | Enable high-throughput kinetic screening for lead compound identification and toxicology, generating robust data for concentration-response curves [4]. |
| Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling Software | Integrates dose-exposure-response relationships to optimize dosing regimens and anticipate interspecies differences [52]. |
| Multiphasic Curve Fitting Software (e.g., Dr.Fit) | Accurately models complex dose-response curves with multiple inflection points, which a standard sigmoidal model cannot capture [4]. |
| Statistical Power Analysis Tools (e.g., G*Power, PASS) | Calculates the minimum sample size required for a study to be sufficiently powered, protecting against false negatives [57] [60]. |
| Master Data Management (MDM) Solutions | Creates a unified view of data from disparate sources (EHRs, lab systems), eliminating redundancies and ensuring consistency for integrated analysis [58]. |
| Sporogen AO-1 | Sporogen AO-1, CAS:88418-12-6, MF:C15H20O3, MW:248.32 g/mol |
| (R)-BRD3731 | (R)-BRD3731, CAS:2056262-07-6, MF:C24H31N3O, MW:377.532 |
A Protocol for Robust Preclinical Dose-Response Experiments
This detailed protocol is designed to integrate the resolution of data quality issues directly into the experimental workflow.
Title: Protocol for a Robust In Vivo Dose-Response Study to Determine the Efficacy of a Novel Compound.
Objective: To establish the dose-response relationship of compound X on [Specific Outcome, e.g., tumor volume reduction] in [Specific Model, e.g., a mouse xenograft model], and accurately estimate EC50 and Emax.
Step 1: Pre-Experimental Planning
- Sample Size Justification: Conduct an a priori power analysis based on pilot data or published effect sizes for similar compounds. Justify the final sample size (n) per group in the protocol [57] [60].
- Pre-registration and SAP: Prospectively register the study protocol and upload a detailed Statistical Analysis Plan (SAP) to a public repository, as recommended by SPIRIT 2025 guidelines [59]. The SAP must include predefined criteria for outlier handling, the primary model for curve fitting (e.g., 4-parameter logistic model), and methods for handling missing data.
- Randomization and Blinding Scheme: Generate a randomization sequence for assigning animals to dose groups. Implement blinding so that personnel measuring the outcome are unaware of the group assignments [57] [61].
Step 2: In-Life Experiment Execution
- Dose Administration: Administer the compound at a minimum of 5-6 logarithmically spaced dose levels, plus a vehicle control group. Include a reference compound if available.
- Data Collection: Measure the primary outcome consistently using calibrated instruments. Record all raw data electronically. Note any potential confounding events (e.g., animal illness, technical error) in a laboratory notebook.
Step 3: Data Analysis and Curve Fitting
- Quality Control Check: Plot raw data to visually inspect for variability and potential outliers. Apply the predefined outlier criteria.
- Curve Fitting: Fit the data to the predefined model using nonlinear regression. Use methods like Akaike Information Criterion (AIC) to compare models if multiphasic curves are suspected.
- Parameter Estimation and CI Calculation: Report the estimated EC50, Emax, and slope along with their 95% confidence intervals (CIs). The width of the CIs provides immediate insight into the precision of your estimates, which is directly related to data quality and sample size [57].
The integrity of preclinical dose-response data is non-negotiable for making informed decisions in the drug development pipeline. By proactively addressing variability through rigorous experimental design, establishing transparent protocols for handling outliers, and justifying sample sizes through statistical power analysis, researchers can significantly enhance the quality and translational relevance of their findings. Adherence to evolving best practices and reporting guidelines, such as SPIRIT 2025, ensures that the limitations and strengths of the data are clear, ultimately building a more reliable foundation for clinical trials [59].
In preclinical research, the accurate interpretation of dose-response relationships is fundamental to drug development, yet this process is frequently compromised by curve-fitting problems and model selection errors. Dose-response curves typically follow a sigmoidal pattern when response is plotted against the logarithm of the dose, characterized by parameters including potency (EC50), slope, maximum effect (Emax), and threshold dose [62]. The standard practice of converting hyperbolic dose-response relationships to log-linear sigmoidal curves expands the clinically relevant 20%-80% effect range for better visualization, but this transformation can introduce interpretation artifacts when improper statistical models are applied [62] [63]. These challenges are particularly acute in complex interventions such as psychotherapy trials and oncology dose optimization, where traditional maximum tolerated dose approaches are being replaced by optimal biological dose determination requiring more sophisticated modeling techniques [3] [7].
The fundamental challenge resides in the tension between model complexity and interpretability. Overly simplistic models, such as assuming simple linear relationships when biological processes typically follow sigmoidal curves, can lead to significant misinterpretation of drug potency and efficacy [63]. Conversely, excessively complex models with too many parameters may result in overfitting, where models describe random noise rather than true underlying biological relationships. The integrity of preclinical research depends on addressing these curve-fitting challenges through appropriate model selection, validation, and interpretation.
Common Curve-Fitting Pitfalls and Their Impact on Research
Model Selection Errors
Incorrect Functional Form Assumption A prevalent error in dose-response analysis is the presumption of simple linear relationships when biological processes typically exhibit sigmoidal characteristics. Statistical analyses often fail to account for the modest beginnings, accelerated mid-range response, and upper asymptote saturation that define most pharmacological responses [63]. This mis-specification problem is particularly acute in observational research, where the underlying mechanisms may be insufficiently understood. The Gompertz curve represents one example of a parametric sigmoidal function that is asymmetric in nature, with the upper level approached more slowly than the initial baseline, but its application requires sophisticated statistical understanding often lacking among preclinical researchers [63].
Overfitting with Excessive Parameters Complex models with numerous parameters can create the illusion of excellent fit by describing random noise rather than true biological relationships. This overfitting problem reduces model generalizability and predictive power when applied to new datasets. The phenomenon is especially problematic in machine learning approaches to dose-response prediction, where functional random forest methods face computational constraints and may not capture significant variations due to their smoothing approach [39]. Multi-output Gaussian process models have shown promise in addressing these limitations by modeling responses at all doses simultaneously, thereby enabling assessment of any dose-response summary statistic while maintaining appropriate complexity [39].
Analytical and Interpretation Pitfalls
Table 1: Common Analytical Pitfalls in Dose-Response Modeling
| Pitfall Category | Specific Issue | Consequence | Recommended Mitigation |
|---|---|---|---|
| Interpretation Biases | Confounding by disease severity | Spurious inverse correlations | Detailed matched analyses, propensity scoring |
| Placebo effect gradients | Misattribution of treatment effects | Rigorous double-blinding procedures | |
| Absence of gradients | False negative conclusions | Scrutinize selected dose range | |
| Analysis Errors | Measurement error around dose | Underestimation of relationships | Scrupulous data on actual administered dose |
| Arbitrary category boundaries | Contrived distinctions | Biological rationale for category definitions | |
| Assuming simple linear model | Mischaracterization of relationships | Consider sigmoidal fitting approaches | |
| Special Situations | Survival bias | Overlooking earlier events | Clear time-zero for cohort analysis |
| Healthy user bias | Inverse selection bias | Careful comorbidity measurements | |
| Thresholds of symptom severity | Imprecision in subjective assessment | Objective endpoints where possible |
Confounding by Indication Observational research into dose-response relationships is particularly vulnerable to confounding by indication, where greater disease severity leads to both higher treatment intensity and poorer outcomes, creating spurious inverse correlations [63]. This phenomenon is evident in infertility research, where the number of therapy cycles paradoxically correlates negatively with success rates because patients with more severe underlying conditions require more intensive treatment [63]. Traditional statistical corrections, including propensity score analyses, often fail to fully account for this bias because detailed information on disease severity is typically crude or incomplete in most observational datasets.
Measurement and Scaling Issues Dose-response relationships assume both predictor and outcome variables are measured on rigorous interval scales, an assumption more feasible in agricultural science than clinical research [63]. The ubiquitous use of ordinal scales in medicine, such as Glasgow Coma Scale scores or pain scales, renders quantitative interpretation of dose-response coefficients potentially misleading. Simultaneously, random measurement errors in exposure data cause regression models to underestimate true relationships, while non-random misclassification can exaggerate effect sizes [63]. These measurement challenges are compounded by variability in experimental systems, where ED50 values show significant variation even across experimental replicates [64].
Methodological Frameworks for Robust Dose-Response Analysis
Advanced Statistical Modeling Approaches
Multi-Output Gaussian Process (MOGP) Models Recent methodological advances have introduced MOGP models that simultaneously predict all dose-responses and uncover biomarkers by describing the relationship between genomic features, chemical properties, and every response at every dose [39]. This approach addresses fundamental limitations of conventional machine learning methods that require selection of summary metrics (e.g., IC50, AUC) and cannot predict responses at all tested doses. The MOGP framework employs a probabilistic multi-output model to assess drug efficacy using any dose-response metric, significantly reducing data requirements while improving prediction precision [39]. A key innovation of this approach is the use of Kullback-Leibler divergence to measure feature importance and identify biomarkers, as demonstrated in the identification of EZH2 as a novel biomarker of BRAF inhibitor response in melanoma [39].
SynergyLMM Framework for Combination Studies For drug combination experiments, the SynergyLMM framework provides a comprehensive modeling approach that accommodates complex experimental designs, including multi-drug combinations, through longitudinal drug interaction analysis [65]. This method employs either exponential or Gompertz tumor growth kinetics with a linear mixed model to capture inter-animal heterogeneity and dynamic changes in combination effects. The framework supports multiple synergy scoring models (Bliss independence, highest single agent, response additivity) with uncertainty quantification and statistical assessment of synergy and antagonism [65]. The implementation includes model diagnostics and statistical power analysis, enabling researchers to optimize study designs by determining appropriate animal numbers and follow-up timepoints required to achieve sufficient statistical power.
Model Validation and Qualification Protocols
Model-Informed Precision Dosing (MIPD) Validation The accuracy of model-informed precision dosing depends critically on appropriate model selection and validation. A systematic framework for qualifying mechanistic models integrates key concepts from ASME V&V 40 and EMA's QIG guidelines, emphasizing context of use and uncertainty quantification [66]. This approach involves evaluating population pharmacokinetic models based on:
- Target Population Similarity: Assessing how closely the modeled population matches the intended population for precision dosing, considering age distribution, ethnicity/race, clinical care environment, and dosing regimens [67].
- Model Performance Verification: Testing selected models on example data from the intended population to verify appropriate performance before clinical implementation [67].
- Software Implementation Validation: Ensuring successful translation and validation of the selected model into precision dosing software prior to clinical deployment [67].
Comprehensive Statistical Diagnosis The SynergyLMM framework exemplifies rigorous model validation through comprehensive statistical diagnosis to assess how well models fit data, identify outlier observations, and detect highly influential subjects [65]. This process includes:
- Growth Model Selection: Choosing between exponential and Gompertz growth models based on diagnostic plots and performance metrics [65].
- Residual Analysis: Examining patterns in residuals to identify systematic misfitting.
- Influence Diagnostics: Identifying individual observations or subjects that disproportionately impact model parameters.
- Sensitivity Analysis: Assessing model stability under varying assumptions and data conditions.
Table 2: Experimental Protocols for Dose-Response Model Validation
| Protocol Phase | Key Procedures | Data Requirements | Validation Metrics |
|---|---|---|---|
| Preclinical Model Development | Multi-dose screening across cell lines | Genomic features, drug chemical properties | Prediction accuracy on holdout samples |
| Biomarker identification via KL-divergence | Genetic variations, copy number alterations, DNA methylation | Concordance with known biological pathways | |
| In Vivo Combination Studies | Longitudinal tumor measurement | Tumor volume or luminescence signal over time | Model diagnostics (residual patterns, influence) |
| Mixed-effect model fitting | Multiple treatment groups with control animals | Synergy score statistical significance | |
| Model Qualification | Context of use definition | Clearly defined decision-making context | Credibility evidence based on risk |
| Uncertainty quantification | Variability in experimental measurements | Confidence intervals for parameters | |
| Clinical Translation | Bayesian parameter estimation | Patient demographics, therapeutic drug monitoring | Target attainment for exposure metrics |
Experimental Protocols for Robust Dose-Response Modeling
Multi-Output Gaussian Process Implementation
Data Collection and Preprocessing
- Cell Line Screening: Conduct dose-response experiments across a panel of cancer cell lines representing multiple cancer types. The Genomics of Drug Sensitivity in Cancer (GDSC) database provides a representative example, encompassing dose-responses from treatment of ten drugs on 442 human cancer cell lines across ten cancer types [39].
- Molecular Feature Extraction: Extract three types of molecular features: genetic variations in high-confidence cancer genes, copy number alteration status of recurrent altered chromosomal segments, and DNA methylation status of informative CpG islands [39].
- Chemical Property Characterization: Obtain chemical features for investigated drugs from PubChem database, representing compounds as chemical graphs for quantitative analysis [39].
Model Training and Validation
- Kernel Specification: Implement MOGP with appropriately specified kernel functions to capture correlations across different doses and biological contexts.
- Feature Relevance Assessment: Apply Kullback-Leibler divergence to measure importance of each genomic feature and identify biomarkers based on their impact on model predictions [39].
- Cross-Study Validation: Evaluate model performance through cross-study tests where training and testing occur on different datasets to assess generalizability and avoid overfitting [39].
SynergyLMM Framework for In Vivo Combination Studies
Experimental Design Considerations
- Longitudinal Measurement: Collect tumor burden measurements (volume or luminescence) at multiple time points across treatment and control groups, with normalization against treatment initiation timepoints to adjust for variability in initial tumor burden [65].
- Appropriate Group Sizing: Include sufficient animals per treatment group to detect synergistic effects with adequate statistical power, utilizing the framework's power analysis tools to optimize sample size [65].
- Timepoint Selection: Schedule measurements to capture dynamic changes in combination effects, with more frequent sampling during periods of expected rapid change.
Statistical Implementation
- Reference Model Selection: Choose appropriate synergy reference models (Bliss independence, highest single agent, or response additivity) based on the biological mechanism under investigation [65].
- Mixed-Effect Model Fitting: Implement linear mixed-effect models for exponential growth or non-linear mixed-effect models for Gompertz growth to estimate growth rate parameters for each treatment group [65].
- Time-Resolved Synergy Scoring: Calculate time-dependent synergy scores with corresponding confidence intervals and p-values to assess statistical significance of synergistic or antagonistic effects at different time points [65].
Visualization of Methodological Approaches
Dose-Response Modeling Workflow with Quality Control Checkpoints
Factors Influencing Dose-Response Relationship Accuracy
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Computational Tools for Dose-Response Studies
| Reagent/Tool Category | Specific Examples | Function in Dose-Response Research | Implementation Considerations |
|---|---|---|---|
| Computational Modeling Platforms | Edsim++, MwPharm++, PrecisePK, InsightRX Nova | Bayesian estimation for model-informed precision dosing | Compatibility with existing clinical systems, regulatory acceptance |
| Statistical Frameworks | SynergyLMM, Multi-Output Gaussian Process, invivoSyn | Longitudinal analysis of combination therapy effects | Programming requirements (R vs. web-tool), statistical expertise |
| Biological Reference Materials | High-confidence cancer cell lines (GDSC database), Patient-derived xenografts | Representative models for screening and validation | Relevance to human biology, passage number documentation |
| Biomarker Assay Technologies | Genetic variation panels, Copy number alteration arrays, DNA methylation profiling | Biomarker discovery and validation for response prediction | Analytical validation, reproducibility across laboratories |
| Drug Compound Libraries | PubChem database, Targeted therapy collections (BRAF inhibitors) | Standardized compounds for screening initiatives | Compound purity, stability in experimental conditions |
| Data Resources | Genomics of Drug Sensitivity in Cancer (GDSC), Cell line molecular feature databases | Reference data for model training and validation | Data quality, standardization across sources |
The accurate interpretation of dose-response relationships in preclinical research requires meticulous attention to curve-fitting methodologies, model selection procedures, and validation protocols. By implementing robust statistical frameworks like Multi-Output Gaussian Processes and SynergyLMM, researchers can overcome common pitfalls including overfitting, confounding by indication, and incorrect functional form specification [39] [65]. The emerging paradigm emphasizes model qualification based on context of use, comprehensive uncertainty quantification, and integration of biological plausibility assessments into the modeling workflow [66].
Future advancements in dose-response modeling will likely incorporate more sophisticated machine learning approaches while maintaining rigorous validation standards. The integration of high-dimensional molecular data with chemical properties through frameworks like MOGP represents a promising direction for personalized therapy optimization [39]. Furthermore, the development of standardized model qualification frameworks across regulatory agencies and industry stakeholders will enhance the reliability and reproducibility of dose-response predictions, ultimately accelerating the translation of preclinical findings to clinical applications [66]. As these methodologies evolve, the fundamental principles of appropriate model selection, comprehensive validation, and cautious interpretation will remain essential for deriving meaningful insights from dose-response relationships.
In preclinical research, the fundamental principle of "the dose makes the poison" has long been guided by an expectation of monotonicity, where increasing doses of a substance lead to proportionally increasing biological effects. However, this foundational model fails to capture the complexity of non-monotonic dose-response curves (NMDRCs), which demonstrate a change in the direction of the slope within the tested dose range, creating distinctive U-shaped or inverted U-shaped curves [68] [69]. These curves represent a significant paradigm challenge for researchers and risk assessors, as effects observed at lower doses cannot be reliably predicted by the response observed at higher doses [68].
The presence of NMDRCs has been documented in response to various substances, including nutrients, vitamins, pharmacological compounds, hormones, and endocrine-disrupting chemicals (EDCs) [68]. Their existence complicates one of the most fundamental assumptions in toxicology: that high-dose testing can be used to extrapolate to lower doses anticipated to be 'safe' for human exposures [68]. When NMDRCs occur below the toxicological no-observed-adverse-effect-level (NOAEL), this assumption is falsified, necessitating a reevaluation of traditional testing and risk assessment frameworks [68].
Mechanisms Behind Non-Monotonic Responses
Biological Foundations of NMDRCs
Non-monotonic dose responses emerge from complex biological systems rather than being statistical artifacts or experimental noise. Multiple mechanistic pathways can give rise to these unexpected response patterns, often involving receptor dynamics and feedback loops that do not operate in simple linear fashions.
Table 1: Primary Biological Mechanisms Generating NMDRCs
| Mechanism | Process Description | Example Substances |
|---|---|---|
| Receptor Competition | At higher concentrations, ligands may bind to lower-affinity receptors with opposing effects, changing the overall response direction [68]. | Endocrine-disrupting chemicals |
| Feedback Loops | Cellular feedback mechanisms may become activated at specific threshold doses, paradoxically reducing the observed effect as dose increases further. | Hormones, pharmaceuticals |
| Protein Saturation | Saturation of binding proteins or metabolic enzymes at intermediate doses can alter the bioavailability of a compound [68]. | Vitamins, hormones |
| Multiple Target Engagement | Engagement of different biological targets with varying affinities and opposing physiological effects as concentration increases. | Drugs with polypharmacology |
System Visualization of NMDRC Mechanisms
The following diagram illustrates the key biological pathways that can generate non-monotonic responses:
Experimental Design for NMDRC Detection
Optimal Dose Selection and Spacing
Conventional toxicity studies typically examine only 3-4 dose levels, usually focused on higher doses to identify the NOAEL [68]. This approach often misses non-monotonic effects occurring at lower doses. Statistical optimal design theory recommends more strategic dose selection to effectively characterize potential NMDRCs [70].
For robust detection of NMDRCs, studies should include:
- Multiple dose groups with adequate spacing across the anticipated response range [70]
- Sufficient sample sizes at each dose level to detect potential biphasic patterns
- Dose levels below the NOAEL and even below established reference doses to identify potential low-dose effects [68]
- Appropriate statistical power to detect non-monotonic trends rather than just pairwise comparisons to control
Research indicates that D-optimal experimental designs for dose-response studies often require control plus only three strategically placed dose levels to effectively model nonlinear responses while minimizing the total number of experimental units needed [70].
Quantitative Data Analysis Methods
Proper statistical analysis is crucial for distinguishing true NMDRCs from experimental variability. Recommended approaches include:
- Model comparison techniques that test the goodness-of-fit of non-monotonic models (U-shaped, inverted U-shaped) against standard monotonic models
- Benchmark dose (BMD) modeling as an alternative to traditional NOAEL approaches [70]
- Resampling methods to assess the reliability of observed non-monotonic patterns
- Mechanistic modeling that incorporates biological understanding of the system being studied
Regulatory and Risk Assessment Implications
Current Regulatory Challenges
The presence of NMDRCs presents significant challenges to conventional risk assessment paradigms. Regulatory agencies have historically operated under the assumption that NMDRCs are not common for adverse outcomes and are not relevant for chemical safety regulation [68]. However, evidence continues to emerge that challenges this position.
Three key scenarios demonstrate the regulatory implications of NMDRCs:
Table 2: Regulatory Implications of NMDRC Location in Dose-Response Curve
| Scenario | Description | Regulatory Impact | Documented Examples |
|---|---|---|---|
| Case 1: Above NOAEL | NMDRCs observed at high doses above the NOAEL | Minimal impact on reference dose setting; may provide mechanistic insight [68]. | TCDD effects on cell-mediated immunity in male rats (1-90 µg/kg/d) [68] |
| Case 2: Between NOAEL and RfD | NMDRCs occur between the NOAEL and reference dose (RfD) | Challenges the validity of extrapolating from high doses; suggests true NOAEL may be lower [68]. | Permethrin alteration of dopamine transport in mice (1.5 mg/kg/d) [68] |
| Case 3: Below RfD | NMDRCs observed at or below the established RfD | Indicates RfD may be scientifically flawed and insufficiently protective [68]. | Chlorothalonil effects on amphibian survival (0.0000164-0.0164 ppm) [68] |
The Scientific Debate
There remains significant scientific debate regarding the prevalence and regulatory significance of NMDRCs. While some researchers argue that NMDRCs are common, particularly for endocrine disruptors, and necessitate fundamental changes in chemical testing [69], regulatory evaluations have been more cautious.
The U.S. Environmental Protection Agency's scientific review concluded that while NMDRCs do occur, they are "not commonly identified in vivo and are rarely seen in whole-organism studies after low-dose or long-term exposure" [69]. Similarly, the European Food Safety Authority noted that "the hypothesis that NMDR is a general phenomenon for substances in the area of food safety is not substantiated" [69].
This ongoing debate highlights the need for rigorous, reproducible science and systematic reviews of the evidence regarding NMDRCs and their impact on public health protection.
Essential Research Toolkit
Experimental Reagents and Materials
Table 3: Essential Research Reagents for NMDRC Studies
| Reagent/Material | Function in NMDRC Research | Application Notes |
|---|---|---|
| Multiple Dose Concentrations | Testing across broad concentration range to detect slope changes | Should span from below environmental exposure levels to above expected NOAEL [68] |
| Positive Control Compounds | Validating experimental sensitivity to detect NMDRCs | Known NMDRC compounds (e.g., BPA, specific phthalates) [68] |
| Cell Culture Systems with Endogenous Receptor Expression | Studying receptor-mediated NMDRC mechanisms | Systems with intact feedback loops (e.g., pituitary cells, breast cancer cells) |
| Animal Models with Sensitive Endpoints | Detecting low-dose effects in vivo | Models with quantifiable endocrine-sensitive endpoints (e.g., anogenital distance, tissue weights) [68] |
| Chemical-Specific Analytical Standards | Accurate quantification of exposure concentrations | Essential for verifying actual delivered dose in complex biological systems |
| KIN101 | KIN101, CAS:610753-87-2, MF:C16H11BrO5S, MW:395.22 | Chemical Reagent |
Experimental Workflow for NMDRC Investigation
The following diagram outlines a systematic approach for investigating potential non-monotonic dose responses in preclinical research:
Non-monotonic dose-response curves represent both a challenge and an opportunity in preclinical research and drug development. While they complicate traditional dose-response paradigms and risk assessment methodologies, they also offer insights into the complex biological systems we seek to understand and modulate. The effective interpretation of NMDRCs requires sophisticated experimental design, rigorous statistical analysis, and a mechanistic understanding of the biological pathways involved. As research in this field advances, incorporating these considerations into standard practice will be essential for developing therapeutic agents that fully account for the complexity of biological systems, ultimately leading to more effective and safer drugs.
In preclinical drug development, the accurate characterization of the dose-response relationship is a critical determinant of success for subsequent clinical trials. A well-designed dose-ranging study does more than identify a single active dose; it maps the entire pharmacological profile of a compound, revealing its therapeutic window and informing crucial go/no-go decisions [18]. The core objective is to select a range of doses, the number of dose levels, and appropriate spacing between them that will adequately capture the shape of the dose-response curve—including its steep ascending phase, point of diminishing returns, and ultimate efficacy plateau [18] [7]. This foundational work in preclinical models directly enables the translation of pharmacological insights into viable clinical trial designs, forming the bedrock of model-informed drug development [71].
The traditional approach in oncology, for instance, which focused on finding the maximum tolerated dose (MTD), is often unsuitable for modern targeted therapies that may have a wider therapeutic index [72] [7]. A poorly designed dose-finding strategy can lead to late-stage attrition, failure to recognize a compound's full potential, or post-marketing requirements to re-evaluate dosing, as has been the case for over 50% of recently approved cancer drugs [72]. This guide outlines the core principles and methodologies for designing robust preclinical dose-ranging studies to ensure the accurate and efficient characterization of a drug's pharmacological profile.
Fundamental Concepts of Dose-Response Curves
A dose-response curve is a graphical representation of the relationship between the dose of a drug and the magnitude of the biological response it elicits. Interpreting these curves requires an understanding of several key parameters [4].
- Efficacy: This refers to the maximum therapeutic response a drug can produce. It is represented by the upper plateau of the curve. A more efficacious drug will achieve a greater maximal effect, resulting in a taller curve [4].
- Potency: Potency indicates the dose required to produce a given effect, typically measured by the half-maximal effective concentration (EC50). A more potent drug has a lower EC50, which shifts the curve to the left. It is crucial to note that potency is distinct from efficacy; a drug can be highly potent (effective at low doses) but have limited overall efficacy [4].
- Slope: The steepness of the linear portion of the curve defines how sensitive the response is to changes in drug concentration. A steeper slope implies that a small change in dose will result in a large change in effect [4].
Most drug molecules follow a sigmoidal curve when the dose is plotted on a logarithmic scale. This shape compresses a wide range of concentrations for better visualization and reveals the exponential increase in response at lower doses, followed by a plateau at higher doses as the system reaches saturation [4]. However, not all responses are monophasic. Multiphasic curves, which may feature multiple inflection points, can occur when a drug acts on multiple receptors with different sensitivities or has dual effects (e.g., stimulatory at low doses and inhibitory at high doses) [4].
Table 1: Key Parameters of a Dose-Response Curve
| Parameter | Definition | Interpretation in Drug Development |
|---|---|---|
| Efficacy (Emax) | The maximum achievable therapeutic effect. | Determines the drug's ultimate therapeutic potential. |
| Potency (EC50/IC50) | The dose or concentration that produces 50% of the maximum effect. | Informs the starting dose range; lower EC50 indicates higher potency. |
| Slope | The steepness of the linear phase of the curve. | Indicates the sensitivity of the response to dose changes; critical for predicting the therapeutic window. |
| Therapeutic Window | The range of doses between the minimal effective dose and the onset of unacceptable toxicity. | The primary goal of optimization, balancing efficacy and safety. |
Core Design Strategies for Dose-Ranging Studies
Selecting the Appropriate Dose Range
Defining the dose range is the first and most critical step. The range must be sufficiently wide to capture the minimum desired effect all the way to the maximum possible effect, including the plateau phase.
- Starting Dose and Lower Bound: The lowest dose tested should be based on a target exposure level predicted from nonclinical models to have a high probability of producing a minimal biological effect. This often involves pharmacokinetic-pharmacodynamic (PK/PD) modeling that integrates data on target engagement, pathway modulation, and efficacy in disease models [71]. For cytotoxic agents, this might be a low fraction of the estimated MTD, while for targeted therapies, it may be based on the optimal biological dose (OBD) required for full target suppression [7].
- Upper Bound: The highest dose should be one that is anticipated to achieve maximal efficacy (Emax) or, in the case of toxicological studies, a dose that produces clear toxicity to define the upper limit. The goal is to clearly observe the plateau of the efficacy curve, ensuring that the maximum response has been characterized. For therapies with a known risk of toxicity, the upper bound may be guided by the no observed adverse effect level (NOAEL) and lowest observed adverse effect level (LOAEL) from toxicology studies [4].
Determining the Number of Dose Levels
The number of dose levels is a balance between the need for a high-resolution curve and practical constraints of resources and animal use.
- Minimum Requirements: A minimum of four dose levels is generally required to confidently fit a sigmoidal curve and estimate its parameters (slope, EC50, Emax). However, this provides limited resolution [18].
- Optimal Resolution: Including 5 to 8 dose levels is often recommended to reliably capture the shape of the curve, especially if it is multiphasic or if the slope is unknown. A greater number of doses increases the precision of the model fit and provides robustness against outliers [18] [7].
- Model-Based Approaches: In advanced designs, model-based methods like the MCP-Mod (Multiple Comparison Procedure – Modeling) can be employed. This approach uses a set of candidate models (e.g., Emax, logistic, sigmoidal) and relies on a powerful testing procedure to identify the most likely shape of the dose-response curve, which can inform the efficient placement of dose groups [18].
Strategies for Dose Spacing
Proper spacing between dose levels is essential to efficiently characterize the dynamic regions of the curve without unnecessary redundancy.
- Logarithmic Spacing: Using doses that are incremented on a logarithmic scale (e.g., half-log or quarter-log increments) is the most common and effective strategy. This approach provides higher resolution at lower doses where the curve is often steep and the response changes rapidly, while efficiently covering a wide range of concentrations [4]. For example, a series might be: 1, 3, 10, 30, 100 mg/kg.
- Adaptive and Response-Driven Spacing: In some innovative trial designs, dose escalation and spacing can be informed by real-time data from ongoing experiments. While more common in clinical trials, the principle can be applied to complex preclinical models. This may involve starting with wider spacing and then "backfilling" intermediate doses in regions of high interest, such as near the anticipated EC50 or the onset of toxicity [72].
Table 2: Summary of Dose-Ranging Design Strategies
| Design Element | Considerations | Recommended Strategy |
|---|---|---|
| Dose Range | Must capture from minimal effect to maximal effect/plateau. | Lower bound from target exposure/PK-PD models; upper bound to define Emax or toxicity. |
| Number of Dose Levels | Balance between curve resolution and resource use. | Minimum of 4; 5-8 for robust characterization and model fitting. |
| Dose Spacing | Efficiently characterize steep and plateau phases. | Logarithmic spacing (e.g., half-log increments) to provide higher resolution at lower doses. |
| Study Readouts | Should inform on both efficacy and safety. | Integrate efficacy endpoints (e.g., tumor growth inhibition) with longitudinal toxicity and PK data. |
Experimental Protocols for Dose-Response Characterization
A Standard Protocol for In Vivo Efficacy Studies
This protocol outlines a robust methodology for establishing a dose-response relationship in a mouse xenograft model of cancer, a common preclinical scenario.
- Cell Line and Model Establishment: Select a human cancer cell line relevant to the drug's mechanism of action. Culture cells and subcutaneously inoculate them into immunodeficient mice (e.g., NSG or nude mice). Allow tumors to establish until they reach a predetermined volume (e.g., 100-150 mm³) before randomizing animals into study groups.
- Dose Group Randomization: Randomize tumor-bearing mice into 5-7 experimental groups (e.g., vehicle control, and 4-6 escalating dose levels of the investigational drug). Include a positive control arm (e.g., a standard-of-care therapy) if applicable. Use a group size that provides adequate statistical power (typically n=8-10 per group).
- Dosing Regimen: Administer the drug according to a pre-defined schedule (e.g., daily oral gavage, twice-weekly intraperitoneal injection) for the duration of the study (typically 3-4 weeks). The dose levels should be selected based on prior PK and tolerability data to span from a sub-therapeutic to a maximally effective or tolerated dose.
- Endpoint Monitoring:
- Efficacy: Measure tumor volumes using calipers 2-3 times per week. Calculate tumor growth inhibition (TGI) for each group. At the end of the study, tumors may be harvested for downstream biomarker analysis (e.g., immunohistochemistry for target engagement, pharmacodynamic markers).
- Toxicity: Monitor mice daily for clinical signs of toxicity. Record body weight at least twice weekly as a general indicator of systemic toxicity. Collect blood samples at specified timepoints for clinical chemistry and hematological analysis.
- Pharmacokinetics (PK): In a parallel satellite study, collect plasma at multiple timepoints after a single dose and at steady-state to determine exposure metrics (e.g., Cmax, AUC, trough concentration). This PK data is essential for linking dose to exposure and response [71].
- Data Analysis: Fit the dose-response data at study endpoint (e.g., % TGI) to a nonlinear regression model (e.g., sigmoidal dose-response model) to estimate EC50, Emax, and the hill slope. Perform exposure-response modeling by plotting the pharmacological response against drug exposure (AUC or Cmax) to strengthen the understanding of the relationship [71].
Accounting for Variable Growth Rates in Cell-Based Screening
In high-throughput cell-based screening, varying cellular growth rates can introduce significant bias into traditional viability-based metrics. The Normalized Drug Response (NDR) metric was developed to address this by utilizing both positive and negative control conditions over the entire experimental timeline [73].
- Experimental Setup: Plate cells in multi-well plates and treat with a serial dilution of the test compound. Include negative control wells (vehicle-treated) and positive control wells (with a cytocidal agent) on every plate.
- Time-Point Measurements: Measure a viability readout (e.g., luminescence, fluorescence) at the start of the experiment (T0) and at the end of the incubation period (Tend). This is a key differentiator from metrics that only use an end-point measurement.
- Calculation of NDR: The NDR metric calculates the drug-induced effect by normalizing the fold-change in the drug-treated well to the fold-changes observed in both the negative and positive controls. This accounts for differences in cell growth rates and variable background noise across plates, leading to more accurate and consistent quantification of drug effects, including lethal, growth-inhibitory, and even growth-stimulatory responses [73].
Visualization of the Dose Selection Workflow
The following diagram illustrates the logical workflow and key decision points for designing a dose-ranging study, from initial planning to final analysis.
Diagram Title: Dose-Ranging Study Design Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Successful execution of dose-response studies relies on a suite of specialized reagents and tools. The following table details essential materials and their functions in generating robust dose-response data.
Table 3: Research Reagent Solutions for Dose-Response Studies
| Reagent / Tool | Function in Dose-Response Studies |
|---|---|
| Viability Assay Kits (e.g., MTI, CellTiter-Glo) | Measure cell proliferation or cytotoxicity in response to treatment in cell-based screens. Provides the primary quantitative readout for effect. |
| Validated Antibodies | Detect and quantify target engagement (e.g., phosphorylation status) and downstream pharmacodynamic (PD) biomarkers in cell lysates or tissue sections. |
| PK/PD Modeling Software (e.g., Phoenix WinNonlin) | Perform nonlinear regression to fit dose-response curves, estimate parameters (EC50, Emax), and build integrated pharmacokinetic-pharmacodynamic models. |
| High-Throughput Screening Systems (e.g., FLIPR Penta) | Automate the delivery of compounds and measurement of cellular responses (e.g., calcium flux, viability) across large dose matrices in microtiter plates. |
| Multiplex Cytokine Panels | Profile the secretion of multiple cytokines and chemokines in response to treatment, which is crucial for assessing the immune response and inflammatory toxicity. |
| ePRO Platforms | In clinical translation, electronic Patient-Reported Outcome platforms capture the patient's perspective on symptomatic adverse events, vital for understanding tolerability. |
A strategically designed dose-ranging study is not a mere formality but a cornerstone of informative preclinical research. By thoughtfully selecting a wide enough dose range, employing a sufficient number of dose levels, and using logarithmic spacing, researchers can generate high-quality data that accurately defines the dose-response relationship. Integrating these design principles with robust experimental protocols and model-informed analysis, such as PK/PD modeling, maximizes the likelihood of identifying a true therapeutic window. This rigorous approach in preclinical studies de-risks downstream clinical development, ensuring that the first trials in humans evaluate doses that are both safe and capable of demonstrating the full therapeutic potential of a new drug.
The transition from promising preclinical results to successful clinical outcomes remains a formidable challenge in drug development. This whitepaper examines the multifactorial origins of translational gaps in dose-response relationships, focusing on biological disparities, methodological shortcomings, and model limitations that compromise predictive validity. By analyzing high-attrition rates and specific case studies, we identify critical disconnects between animal models and human pathophysiology. The paper further proposes a framework for enhancing translational relevance through advanced model systems, optimized study designs, and rigorous biomarker validation strategies aimed at improving the predictive power of preclinical dose-response data.
Translational research, designed to bridge basic scientific discovery and clinical application, faces a persistent crisis of predictivity. Despite significant investments in basic science, advances in technology, and enhanced knowledge of human disease, the translation of these findings into therapeutic advances has been far slower than expected [74]. The attrition rates are staggering: nine out of ten drug candidates fail in Phase I, II, and III clinical trials, and more than 95% of drugs entering human trials fail to gain approval [75] [74]. This failure represents not just a financial loss—with the cost of developing each novel drug exceeding $1-2 billion—but also a critical delay in delivering effective treatments to patients [75]. This gap between preclinical promise and clinical utility, often termed the "Valley of Death," is particularly pronounced in the interpretation of dose-response curves, which serve as fundamental tools for establishing compound efficacy and safety [74]. Understanding why these preclinical curves frequently fail to predict human response is essential for innovating drug development paradigms and improving patient outcomes.
Quantifying the Problem: The Translational Failure Rate
The challenges in translation are not merely anecdotal; they are reflected in concrete, quantitative data that highlight the scope and financial impact of the problem.
Table 1: Attrition Rates in Drug Development [75] [74]
| Development Phase | Failure Rate | Primary Causes of Failure |
|---|---|---|
| Preclinical Research | ~99.9% of concepts abandoned | Poor hypothesis, irreproducible data, ambiguous models |
| Phase I Clinical Trials | ~90% of entering candidates fail | Unexpected human toxicity (e.g., TGN1412, BIA 10-2474) |
| Phase II & III Clinical Trials | ~90% of remaining candidates fail | Lack of effectiveness, poor safety profiles not predicted preclinically |
| Overall Approval | ~0.1% of initial candidates | Cumulative failures across all stages |
Table 2: Economic and Temporal Costs of Drug Development [75] [74]
| Metric | Value | Implication |
|---|---|---|
| Time from Discovery to Approval | 10-15 years | Slow delivery of new treatments to patients |
| Cost per Approved Novel Drug | $1-2 billion | High financial risk for developers |
| Return on R&D Investment | <$1 returned per $1 spent (average) | Unsustainable model for innovation |
Root Causes of the Dose-Response Translational Gap
The disconnect between preclinical and clinical dose-response is not attributable to a single cause but arises from a complex interplay of biological, methodological, and model-system limitations.
Biological and Physiological Disparities
- Species-Specific Pathophysiology: Animal models, typically inbred and housed in controlled environments, cannot fully recapitulate the genetic diversity, disease heterogeneity, and complex comorbidities of human patient populations [76]. A drug candidate screened in younger animals for age-related conditions like Alzheimer's disease provides erroneous results that do not mimic the clinical condition in the elderly [75].
- Divergent Immune and Metabolic Responses: Biological differences in immune system function, metabolic pathways, and organ physiology between animals and humans can lead to dramatically different responses to the same compound. The catastrophic failure of the drug TGN1412, which caused severe systemic organ failure in humans at a dose 500 times lower than the safe dose found in animal studies, is a prime example of this discordance [75].
Methodological and Design Flaws
- Inadequate Experimental Design: Preclinical studies often suffer from small sample sizes, a lack of robust validation frameworks, and poor reproducibility across cohorts [75] [76]. Furthermore, the statistical designs of many preclinical studies are not optimized for extrapolation to the more variable conditions of human trials [70].
- Misapplied Dose-Response Modeling: The investigation of dose-response relationships is often guided by convention rather than optimal statistical design. Suboptimal choice of dose levels and sample size allocation can lead to imprecise parameter estimates for critical values like the ED50 (half-maximal effective dose) and the slope of the curve, reducing the predictive utility of the model [70] [19].
- Improper Model Selection: A single preclinical model cannot simulate all criteria of a complex clinical condition. Relying on a single model type, without validation across a combination of models, increases the risk of failure when the drug moves into humans [75].
Limitations of Preclinical Model Systems
- Poor Human Biological Correlation: Traditional animal models and 2D cell cultures are often poor predictors of human clinical disease. For instance, despite the exploration of various pathophysiological mechanisms in preclinical models for acute kidney injury (AKI), no AKI therapies have proven efficacious in human studies [75].
- Failure to Capture Tumor Microenvironment: In oncology, a major translational gap exists because conventional models fail to replicate the highly heterogeneous and evolving tumor microenvironment (TME) found in human patients, including the complex interactions between immune, stromal, and endothelial cells [76].
Diagram 1: Root causes of translational failure.
Enhancing Translational Fidelity: Strategies and Solutions
Bridging the translational gap requires a multi-pronged approach that leverages advanced technologies, robust experimental design, and data-driven decision-making.
Adoption of Human-Relevant Model Systems
To improve the clinical predictability of preclinical findings, the field is moving toward more sophisticated models that better mimic human physiology.
- Patient-Derived Xenografts (PDX): These models, derived from patient tumor tissue implanted into immunodeficient mice, more effectively recapitulate the characteristics, heterogeneity, and evolution of human cancers. PDX models have played a key role in validating biomarkers like HER2 and BRAF and were instrumental in demonstrating that KRAS mutant models do not respond to cetuximab [76].
- 3D Organoids and Co-Culture Systems: Organoids are 3D structures that recapitulate the identity and function of the organ or tissue being modeled. They retain characteristic biomarker expression more effectively than 2D cultures. 3D co-culture systems that incorporate multiple cell types (immune, stromal, endothelial) provide a more physiologically accurate platform for studying cellular interactions and the tumor microenvironment [75] [76].
- Clinical Trials in a Dish (CTiD): This emerging approach uses cells procured from specific patient populations to test promising therapies for safety and efficacy directly on human cells in vitro, allowing for the development of drugs tailored to specific genetic subgroups [75].
Optimized Preclinical Experimental Design
Enhancing the quality and predictive power of preclinical dose-response studies requires the application of rigorous statistical principles.
- D-Optimal Design for Dose-Response: Statistical optimal design theory allows researchers to set experimental conditions (e.g., dose levels, measurement times) to minimize the number of required subjects while maximizing the precision of the results. For common dose-response functions (log-logistic, log-normal, Weibull), D-optimal designs often require a control group plus only three optimally chosen dose levels, making efficient use of resources [70].
- Longitudinal and Functional Validation: Moving beyond single time-point measurements to repeatedly assess biomarkers and functional endpoints over time provides a dynamic view of drug effects and disease progression. This approach captures temporal dynamics that are critical for understanding therapeutic impact and de-risking clinical progression [76].
Table 3: Key Research Reagent Solutions for Enhanced Translation
| Reagent / Model System | Function in Translational Research |
|---|---|
| Patient-Derived Xenografts (PDX) | Recapitulates human tumor heterogeneity and evolution in vivo; used for biomarker validation (e.g., HER2, BRAF, KRAS). |
| 3D Organoids | 3D culture models that retain tissue-specific architecture and biomarker expression; used for personalized therapy prediction. |
| 3D Co-culture Systems | Incorporates multiple cell types to model the tumor microenvironment; identifies biomarkers for treatment resistance. |
| Multi-omics Profiling (Genomics, Transcriptomics, Proteomics) | Identifies context-specific, clinically actionable biomarkers by analyzing multiple layers of biological information. |
| AI/ML Platforms | Analyzes large, complex datasets to identify predictive patterns in biomarker behavior and clinical outcomes. |
Data Integration and Advanced Analytics
- Multi-Omics Integration: Rather than focusing on single targets, integrating data from genomics, transcriptomics, and proteomics helps identify context-specific, clinically actionable biomarkers that might be missed with a single-method approach [76].
- Artificial Intelligence and Machine Learning: AI and ML models are revolutionizing biomarker discovery and dose-response prediction by identifying complex patterns in large datasets that are beyond human capacity to discern. These technologies can enhance precision in screening and prognosis, ultimately improving clinical trial success rates [75] [76].
Diagram 2: Evolving from traditional to enhanced workflows.
The persistent gap between preclinical dose-response curves and clinical outcomes is a critical bottleneck in drug development, rooted in biological disparities, methodological flaws, and the limitations of traditional model systems. However, the strategic integration of human-relevant models like PDX and organoids, the application of statistically rigorous experimental designs, and the power of multi-omics data and AI-driven analytics provide a tangible pathway to bridge this "Valley of Death." By adopting these advanced tools and frameworks, researchers can enhance the predictive validity of preclinical studies, thereby increasing the success rate of clinical trials and accelerating the delivery of effective therapies to patients.
Ensuring Robustness: Validation Techniques and Comparative Analysis Across Compounds and Studies
In preclinical drug development, the accurate characterization of dose-response relationships is fundamental for determining compound efficacy, safety, and optimal dosing regimens. Validation frameworks provide the critical foundation for ensuring that mathematical and statistical models used to interpret these relationships are reliable, reproducible, and predictive. The Organisation for Economic Co-operation and Development (OECD) principles for validation establish a standardized approach, particularly through their fourth principle which mandates appropriate measures of goodness-of-fit, robustness, and predictivity for quantitative structure-activity relationship (QSAR) models [77] [78]. These validation categories form a triad of essential checks that collectively determine a model's trustworthiness for decision-making in therapeutic development.
Within preclinical research, dose-response modeling presents unique challenges that necessitate rigorous validation approaches. These models must accurately capture the relationship between compound concentration and biological effect while accounting for complex biological variability and experimental constraints. The interpretation of dose-response curves relies heavily on the validity of the underlying model, whether for determining half-maximal inhibitory concentration (IC50), effective dose (ED50), or maximal efficacy parameters [52] [79]. Without proper validation, models may appear deceptively accurate on limited datasets but fail to generalize to new experimental conditions or biological systems, potentially leading to costly errors in candidate selection and progression.
The relevance of different validation metrics varies significantly with sample size and model type [77] [78]. For instance, goodness-of-fit parameters can misleadingly overestimate model quality on small samples, particularly for complex nonlinear models like artificial neural networks or support vector machines [78]. This introduction establishes the critical importance of comprehensive validation frameworks specifically tailored to preclinical dose-response research, where accurate model interpretation directly impacts development success.
Core Principles of Model Validation
OECD Validation Framework
The OECD validation principles provide a systematic framework for evaluating quantitative models used in regulatory contexts. The five OECD principles include: (1) a defined endpoint, (2) an unambiguous algorithm, (3) a defined domain of applicability, (4) appropriate measures of goodness-of-fit, robustness, and predictivity, and (5) a mechanistic interpretation when possible [77]. For dose-response modeling in preclinical research, the fourth principle is particularly relevant as it specifically addresses the three validation categories that form the core of model assessment.
The OECD guidance clearly distinguishes between internal validation, which assesses goodness-of-fit and robustness using training set data, and external validation, which evaluates predictivity using an independent test set not involved in model development [77]. This distinction is crucial for dose-response modeling because it ensures that models are evaluated not only on their ability to describe the data used for their creation but also on their capacity to predict outcomes for new compounds or experimental conditions.
Interdependence of Validation Parameters
Validation parameters are not independent measures but rather interconnected aspects of model performance. Research has demonstrated that goodness-of-fit and robustness parameters correlate quite well across sample sizes for linear models, suggesting potential redundancy in some cases [77] [78]. However, for nonlinear models, these same parameters may provide complementary information about different aspects of model behavior.
The relationship between internal and external validation parameters reveals complex dependencies. Studies have found that the assignment of data to training or test sets can cause negative correlations between internal and external validation parameters, particularly when easily modeled data are concentrated in one set and challenging data in the other [78]. This highlights the importance of thoughtful experimental design and data splitting strategies in preclinical dose-response studies to ensure representative distribution of chemical space and biological responses across both training and validation sets.
Table 1: Core Validation Categories According to OECD Principles
| Validation Category | Definition | Common Parameters | Primary Data Source |
|---|---|---|---|
| Goodness-of-Fit | How well the model reproduces response variables on which parameters were optimized | R², RMSE, AIC, BIC | Training set |
| Robustness | Model stability when fitted to reduced or resampled datasets | Q²LOO, Q²LMO, bootstrap confidence intervals | Cross-validation of training set |
| Predictivity | Model performance on new, previously unseen data | Q²F2, CCC, MAE | External test set |
Goodness-of-Fit Assessment in Dose-Response Modeling
Fundamental Concepts and Parameters
Goodness-of-fit (GOF) measures quantify how well a model reproduces the observed data used for its development. In dose-response modeling, this involves assessing how closely the fitted curve matches experimental observations across the tested concentration range. The most common GOF parameters include the coefficient of determination (R²), which measures the proportion of variance explained by the model, and the root mean square error (RMSE), which quantifies the average deviation between observed and predicted responses [77] [78].
For dose-response models specifically, additional specialized GOF measures may include weighted residuals analysis to ensure error consistency across the concentration range and visual inspection of curve fitting to identify systematic deviations from expected sigmoidal or other characteristic shapes. It is important to recognize that GOF parameters are necessary but insufficient for establishing model reliability, as they can be optimized to fit training data without ensuring generalizability.
Limitations and Sample Size Dependencies
A critical finding in validation research is that goodness-of-fit parameters misleadingly overestimate models on small samples [77] [78]. This has profound implications for preclinical dose-response studies, where sample sizes are often limited due to practical constraints. The overestimation occurs because models with sufficient complexity can effectively memorize training data patterns rather than learning the underlying relationship, a phenomenon known as overfitting.
The risk of overfitting varies with model type. For linear models such as multiple linear regression (MLR), GOF inflation on small samples is moderate but still significant. In contrast, for highly flexible nonlinear models including neural networks (ANN) and support vector machines (SVR), the feasibility of GOF parameters is often questionable because these models can achieve near-perfect fit to training data while having poor predictive performance [78]. This underscores the necessity of complementing GOF measures with robustness and predictivity assessments, particularly for complex models.
Robustness Evaluation Techniques
Cross-Validation Methods
Robustness evaluation assesses model stability when trained on variations of the original dataset. Cross-validation techniques are the primary approach for robustness assessment, with leave-one-out (LOO) and leave-many-out (LMO) being the most common implementations. In LOO, each observation is sequentially omitted from model training and used as a single-point test set, while LMO involves removing multiple observations simultaneously [77].
Research has demonstrated that LOO and LMO cross-validation parameters can be rescaled to each other across all model types, suggesting that the computationally most feasible method can be selected based on model characteristics and dataset size [78]. For dose-response modeling with limited biological replicates, LOO may be preferred, while for larger datasets with multiple technical replicates, LMO provides a more thorough assessment of robustness.
Randomization Tests
Y-scrambling or randomization tests provide another crucial robustness assessment by evaluating the possibility of chance correlation. In this approach, the response variable (e.g., biological effect) is randomly shuffled while maintaining the predictor matrix (e.g., compound concentrations or structural descriptors), and models are rebuilt using the scrambled data [77] [78]. The process is repeated multiple times to establish the distribution of model performance metrics under the null hypothesis of no meaningful relationship.
Studies suggest that the simplest y-scrambling method is sufficient for estimating chance correlation, with more complex x-y randomization approaches providing negligible additional value [78]. For dose-response modeling, randomization tests are particularly valuable for verifying that the observed concentration-effect relationship is unlikely to occur by random chance, especially when working with novel compound classes or unusual response patterns.
Table 2: Robustness Evaluation Techniques for Dose-Response Models
| Technique | Procedure | Advantages | Limitations |
|---|---|---|---|
| Leave-One-Out (LOO) Cross-Validation | Iteratively remove single data points, rebuild model, predict omitted point | Efficient with limited data, comprehensive usage of all data | Can overestimate robustness for highly correlated data |
| Leave-Many-Out (LMO) Cross-Validation | Remove data subsets, rebuild model, predict omitted subset | Better estimate of true prediction error | Computationally intensive, requires sufficient data |
| Y-Scrambling | Randomize response variable, rebuild models | Tests for chance correlation, simple implementation | Does not assess model predictive ability |
| Bootstrap Resampling | Create multiple datasets by sampling with replacement | Robust confidence intervals, works with small samples | Can underestimate variance in very small samples |
Predictive Ability and External Validation
External Test Set Validation
Predictivity assessment through external validation represents the most rigorous evaluation of model performance. This involves testing the model on completely novel data not used in any model development steps, including parameter estimation, hyperparameter tuning, or variable selection [77]. For dose-response modeling, this typically means reserving a portion of compounds or experimental replicates exclusively for final validation.
Common parameters for assessing predictivity include Q²F2, which measures prediction accuracy on external data, and the concordance correlation coefficient (CCC), which evaluates agreement between observed and predicted values [77]. These metrics should be complemented with visual assessments of prediction versus observation plots to identify systematic biases or heteroscedasticity that might not be captured by summary statistics.
Domain of Applicability
The domain of applicability defines the boundaries within which a model can be reliably applied based on the chemical space and biological systems represented in the training data [77]. Establishing this domain is particularly important for dose-response models intended to predict activity for novel compound classes. Approaches for defining applicability domains include leverage analysis to identify extrapolations outside the modeled chemical space and similarity metrics to quantify resemblance to training compounds.
For preclinical dose-response modeling, careful consideration of the applicability domain helps prevent inappropriate extrapolation beyond validated conditions, such as predicting effects for structurally dissimilar compounds or in different biological systems than those used in model development. This is essential for establishing the boundaries of valid interpretation for dose-response curves.
Experimental Design and Protocol Development
Sample Size Considerations
The sample size dependence of validation parameters necessitates careful consideration of experimental design in preclinical dose-response studies. Research has shown that most validation parameters stabilize only beyond certain sample thresholds, with small samples producing misleadingly optimistic model assessments [77] [78]. While optimal sample sizes are context-dependent, studies suggest that fewer than 20 observations generally provide unreliable validation for most dose-response models.
For complex models with many parameters, such as multi-output Gaussian processes (MOGP) for dose-response prediction, larger sample sizes are particularly important [39]. Multi-output models that simultaneously predict responses at all tested concentrations offer advantages in efficiency but require careful validation across the entire response surface rather than at individual concentrations.
Statistical Modeling Approaches
Various statistical approaches are available for dose-response modeling, each with distinct validation considerations. Linear models including multiple linear regression (MLR) and partial least squares (PLS) regression generally have more straightforward validation, with goodness-of-fit and robustness parameters that correlate well across sample sizes [78]. Nonlinear approaches such as artificial neural networks (ANN), support vector machines (SVR), and Gaussian processes offer greater flexibility but require more rigorous validation to guard against overfitting.
Emerging approaches like Multi-output Gaussian Process (MOGP) models enable simultaneous prediction of all dose-responses and can uncover biomarkers associated with response patterns [39]. These models require specialized validation protocols that account for correlations across multiple outputs and the probabilistic nature of predictions.
Dose-Response Model Validation Workflow
Advanced Methodologies and Emerging Approaches
Machine Learning in Dose-Response Modeling
Machine learning approaches are increasingly applied to dose-response modeling, bringing both opportunities and validation challenges. Methods such as support vector machines, neural networks, and ensemble methods can capture complex nonlinear relationships but are particularly prone to overfitting without proper validation [39] [78]. The bias-variance tradeoff fundamental to machine learning emphasizes that as model flexibility increases, validation becomes more critical to ensure generalizability beyond the training data.
Recent advances include multi-output prediction of dose-response curves using approaches like Multi-output Gaussian Processes (MOGP), which enable simultaneous prediction across all tested concentrations and can facilitate drug repositioning and biomarker discovery [39]. These methods require validation frameworks that account for correlations across outputs and provide uncertainty estimates for full dose-response curves rather than single summary parameters.
Grouped Data Analysis in Preclinical Research
Preclinical dose-response studies often involve clustered and nested data structures where experimental units are not fully independent, such as when animals are group-housed, share litters, or when multiple measurements are taken from the same cell culture preparation [80]. Ignoring these structures in validation can undermine the validity of analyses by artificially inflating apparent precision and producing improperly narrow confidence intervals.
Valid approaches for grouped data include multilevel modeling, generalized estimating equations, and mixed-effects models that appropriately account for within-cluster correlation [80] [24]. For dose-response studies specifically, these approaches can model both within-subject and between-subject variation in concentration-response relationships, providing more accurate estimates of parameter uncertainty and model performance.
Implementation Framework and Research Reagents
Practical Implementation Protocol
Implementing a comprehensive validation framework for dose-response modeling involves sequential stages:
Experimental Design Phase: Determine appropriate sample size, dose selection, and replication strategy based on anticipated effect size and variability. Define data splitting strategy for training and test sets before conducting experiments.
Model Development Phase: Select appropriate model structure (linear, Emax, sigmoidal, machine learning) based on biological plausibility and data characteristics. Estimate parameters using training data only.
Internal Validation Phase: Assess goodness-of-fit using R², RMSE, and visual residual analysis. Evaluate robustness through cross-validation (LOO or LMO) and randomization tests.
External Validation Phase: Test final model on held-out test data using Q²F2, CCC, and prediction-error metrics. Compare performance to null models and established approaches.
Applicability Assessment: Define domain of applicability using leverage and similarity metrics. Document limitations for appropriate future use.
This protocol ensures systematic evaluation across all validation categories and provides evidence for model reliability in preclinical decision-making.
Research Reagent Solutions for Dose-Response Validation
Table 3: Essential Research Reagents and Platforms for Dose-Response Modeling
| Reagent/Platform | Function in Validation | Application Context |
|---|---|---|
| oncoReveal CDx | FDA-approved targeted NGS panel covering 22 genes | Genomic biomarker identification for response validation [81] |
| TSO500 | Comprehensive pan-cancer panel covering 523 DNA and 55 RNA variants | Molecular characterization for applicability domain definition [81] |
| Aspyre Lung | Ultra-sensitive PCR panel for NSCLC biomarkers in DNA/RNA | Targeted biomarker assessment in specific therapeutic areas [81] |
| R Statistical Environment | Platform for dose-response modeling and validation | Implementation of linear, nonlinear, and machine learning models [79] |
| gnm Package (R) | Generalized nonlinear modeling | Dose-response curve fitting with formal validation [79] |
| glmmTMB Package (R) | Generalized linear mixed models | Dose-response modeling with random effects for grouped data [79] |
| Multi-output Gaussian Processes | Simultaneous prediction of all dose-responses | Advanced modeling with uncertainty quantification [39] |
Validation Metrics for Dose-Response Models
Comprehensive validation frameworks encompassing goodness-of-fit, robustness, and predictivity assessments are essential for reliable interpretation of dose-response relationships in preclinical research. The OECD principles provide a validated foundation for this process, but implementation must be adapted to address the specific challenges of dose-response modeling, including sample size limitations, nested data structures, and complex nonlinear relationships.
Emerging methodologies such as multi-output Gaussian processes and advanced machine learning approaches offer powerful new capabilities for dose-response prediction but necessitate even more rigorous validation to ensure their reliability in decision-making. By adopting systematic validation protocols that account for model purpose, complexity, and intended application domain, researchers can significantly enhance the quality and interpretability of dose-response curves throughout the drug development pipeline.
The integration of robust validation practices from early preclinical stages establishes a foundation of evidence that supports subsequent clinical development, regulatory review, and ultimately, therapeutic success. As dose-response modeling continues to evolve with technological advances, validation frameworks must similarly advance to ensure that model interpretations remain grounded in statistical rigor and biological plausibility.
In preclinical drug development, the dose-response relationship serves as a foundational principle for quantifying the pharmacological activity of drug candidates. This relationship, typically visualized through dose-response curves, provides the critical framework for understanding two distinct pharmacological properties: potency and efficacy. These parameters form the basis for comparing drug candidates and predicting their therapeutic potential [14]. While often conflated, potency and efficacy represent different characteristics of drug action, each with specific implications for drug selection, dosing regimen design, and ultimately, clinical success.
This guide examines the methodological approaches for the rigorous comparison of potency and efficacy between drug candidates, framed within the context of dose-response curve interpretation in preclinical research. The accurate discrimination between these properties enables researchers to select candidates with the optimal balance of biological activity and therapeutic window, thereby de-risking the subsequent stages of drug development.
Defining Core Concepts: Potency and Efficacy
Pharmacological Definitions
Potency is defined as the concentration (EC50) or dose (ED50) of a drug required to produce 50% of that drug's maximal effect. A drug is considered more potent if it achieves its half-maximal effect at a lower concentration. Potency is a quantitative measure of drug strength [14] [82].
Efficacy (Emax) refers to the maximum biological effect a drug can produce, regardless of dose. Once this magnitude of effect is reached, increasing the dose will not produce a greater response. Efficacy represents the qualitative ability of a drug to activate receptors and produce a response [14] [82].
Intrinsic Activity is a related concept describing a drug's maximal efficacy as a fraction of the maximal efficacy produced by a full agonist of the same type acting through the same receptors under the same conditions [14].
Conceptual Differentiation
The fundamental distinction lies in what each parameter measures: potency concerns "how much" drug is needed, while efficacy concerns "how well" the drug works at its maximum effect. A common analogy illustrates this difference: if two pain relievers both ultimately eliminate a headache (equal efficacy), the one that does so at a lower dose is more potent. However, a highly potent drug may have limited clinical utility if its maximum effect (efficacy) is insufficient to treat the condition [82].
Table 1: Key Characteristics of Potency and Efficacy
| Parameter | Definition | Quantitative Measure | Primary Influence |
|---|---|---|---|
| Potency | Dose needed to produce 50% of maximal effect | EC50 or ED50 | Affinity for receptor & pharmacokinetics |
| Efficacy | Maximum achievable effect regardless of dose | Emax | Intrinsic activity & signal transduction efficiency |
Experimental Protocols for Dose-Response Analysis
Standardized Dose-Response Curves
The generation of reliable dose-response curves requires meticulous experimental design. The following protocol outlines a standardized approach for in vitro assessment of drug candidates:
Cell Line Selection and Culture: Utilize clinically relevant cell lines expressing the target of interest. Maintain cells in appropriate media and conditions to ensure consistent growth and receptor expression. For cancer studies, the Genomics of Drug Sensitivity in Cancer (GDSC) database provides validated models [39].
Dose Range Selection: Employ a broad dose range (typically 8-12 concentrations) spanning several orders of magnitude (e.g., 1 nM to 100 μM) to adequately capture the full concentration-effect relationship, from threshold to maximal response.
Response Measurement: Quantify the pharmacological response using validated assays specific to the mechanism of action (e.g., cell viability assays for cytotoxics, cAMP accumulation for GPCR agonists, or phosphorylation status for kinase inhibitors).
Replication and Controls: Perform experiments with a minimum of three technical replicates and three independent biological replicates. Include appropriate controls (vehicle, positive control with known efficacy, and negative control).
Incubation Time Optimization: Determine the optimal incubation time that allows for equilibrium binding and full signal transduction, which may require time-course experiments for new targets.
Data Analysis and Curve Fitting
Once experimental data is collected, analysis proceeds through these methodical steps:
Data Normalization: Normalize response data to positive (maximal effect) and negative (basal effect) controls, typically expressed as percentage response.
Nonlinear Regression Analysis: Fit normalized data to a four-parameter logistic (4PL) curve using specialized software (e.g., GraphPad Prism, R):
Response = Bottom + (Top - Bottom) / (1 + 10^((LogEC50 - Log[Drug]) * HillSlope))Parameter Estimation: Derive key parameters from the fitted curve:
- EC50/ED50: Concentration/dose producing 50% of maximal effect (potency indicator)
- Emax: Maximum effect achieved (efficacy indicator)
- Hill Slope: Steepness of the curve, which may suggest cooperativity
Statistical Comparison: Use extra sum-of-squares F-test or Akaike Information Criterion (AIC) to determine if curves and parameters for different drug candidates are statistically different.
Advanced Modeling Approaches
Recent advances in dose-response modeling have introduced more sophisticated computational approaches:
Multi-Output Gaussian Process (MOGP) Models: These probabilistic models simultaneously predict responses at all tested doses, enabling assessment of any dose-response summary statistic without pre-selection. MOGP models are particularly valuable when dealing with heterogeneous data sets and limited sample sizes [39].
Quantitative Systems Pharmacology (QSP): QSP models integrate drug exposure, target binding, and downstream physiological effects within a mechanistic framework. These models are especially useful for placing efficacy and potency metrics in the context of disease pathophysiology and for comparative analyses between drug candidates [83].
Diagram 1: Pharmacological Pathway from Dose to Clinical Outcome
Quantitative Analysis and Data Interpretation
Comparative Parameters from Dose-Response Curves
The systematic comparison of drug candidates requires analysis of multiple derived parameters from dose-response experiments:
Table 2: Key Quantitative Parameters from Dose-Response Analysis
| Parameter | Symbol | Interpretation | Calculation Method |
|---|---|---|---|
| Half-Maximal Effective Concentration | EC50 | Concentration producing 50% of Emax; primary potency measure | Derived from curve fitting of concentration-response data |
| Maximal Effect | Emax | Upper asymptote of curve; absolute efficacy measure | Derived from curve fitting; expressed as % of system maximum |
| Hill Coefficient | nH | Steepness of curve; >1 suggests positive cooperativity | Slope parameter in 4-parameter logistic equation |
| Relative Potency | - | Ratio of equi-effective doses; unitless comparison | EC50 Candidate B / EC50 Candidate A |
| Therapeutic Index | TI | TD50/ED50; safety margin estimate | Requires separate efficacy and toxicity dose-response curves |
Interpreting Curve Relationships
Different curve profiles reveal distinct pharmacological characteristics:
Parallel Shift with Equal Emax: Candidates with parallel curves reaching the same Emax but different EC50 values differ primarily in potency. The left-shifted curve indicates higher potency [14].
Different Emax with Same EC50: Candidates with equal EC50 but different maximum responses differ in efficacy, suggesting varying levels of intrinsic activity [14].
Varying Slope and Emax: Candidates with different curve steepness and maximum effects differ in both mechanistic properties (e.g., cooperativity) and efficacy, requiring careful analysis of the therapeutic concentration range.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Reagents for Dose-Response Studies
| Reagent/Material | Function in Analysis | Application Context |
|---|---|---|
| Validated Cell Lines | Provide consistent biological system expressing target of interest | All in vitro pharmacology studies |
| Reference Agonists/Antagonists | Serve as benchmark for potency and efficacy comparisons | Assay validation and standardization |
| Selective Pathway Inhibitors | Elucidate mechanism of action and signaling pathways | Target engagement confirmation |
| Cell Viability Assays (MTT, CellTiter-Glo) | Quantify cellular response to drug treatment | Cytotoxicity and proliferation studies |
| Second Messenger Assays (cAMP, Ca2+) | Measure immediate downstream signaling events | GPCR and ion channel drug screening |
| Phospho-Specific Antibodies | Detect phosphorylation status of signaling nodes | Kinase inhibitor characterization |
| High-Content Imaging Systems | Multiparametric analysis of morphological changes | Phenotypic screening and toxicity assessment |
Application in Drug Development Decision-Making
Candidate Selection Criteria
The integration of potency and efficacy data into candidate selection follows a structured approach:
Target Product Profile Alignment: Evaluate candidates against predefined target product profile requirements, giving priority to efficacy for diseases requiring maximal response, and considering potency for targets with dosing constraints.
Therapeutic Index Consideration: Candidates with high potency but narrow therapeutic indices require more careful dosing strategies and may present greater development risks [82].
Differentiation Strategy: In competitive therapeutic areas, a combination of high efficacy and optimal potency provides significant market advantages through improved dosing convenience and therapeutic outcomes [82].
Regulatory and Clinical Translation
Understanding the distinction between potency and efficacy guides critical regulatory and development decisions:
Regulatory Emphasis: Regulatory bodies primarily focus on efficacy data to ensure meaningful clinical benefits, while potency information is crucial for labeling and dosing instructions [82].
Formulation Strategy: Potency data directly influences formulation development, with highly potent compounds requiring specialized delivery systems for accurate low-dose administration.
Clinical Trial Design: Phase I dose-ranging studies use preclinical potency (EC50/ED50) and efficacy (Emax) data to inform starting doses and escalation schemes, while Phase II/III trials focus on confirming clinical efficacy.
Diagram 2: Drug Candidate Selection Workflow
The rigorous comparison of potency and efficacy through dose-response analysis provides the foundational framework for informed decision-making in preclinical drug development. By implementing standardized experimental protocols, applying appropriate analytical methods, and correctly interpreting the resulting parameters, researchers can effectively discriminate between drug candidates and select those with the optimal pharmacological profile for clinical advancement. As drug discovery evolves, the integration of traditional dose-response methodologies with advanced computational approaches like MOGP and QSP modeling will further enhance our ability to predict clinical performance from preclinical data, ultimately accelerating the development of novel therapeutics.
In preclinical research, the interpretation of dose-response curves forms the foundation for understanding a drug's pharmacological profile. The relationship between the dose of a drug administered and the magnitude of the effect it produces is fundamental to quantifying both efficacy and toxicity [4]. This relationship is typically visualized through dose-response curves, which are graphical representations that depict how biological responses change as drug concentration increases [84]. These curves allow researchers to identify the optimal dose range that maximizes therapeutic benefit while minimizing adverse effects, ultimately informing critical safety parameters such as the therapeutic index and safety margin [85] [86].
The shape and critical points of a dose-response curve reveal valuable information regarding a drug's mechanism of action, potency, and efficacy [4]. By analyzing these curves, researchers can estimate the minimum effective doses and maximum tolerated doses, which are essential for establishing a drug's safety profile before proceeding to clinical trials [18]. This guide provides an in-depth technical examination of how to calculate, interpret, and apply therapeutic index and safety margin within the context of dose-response analysis in preclinical drug development.
Core Concepts in Dose-Response Analysis
Key Parameters from Dose-Response Curves
Dose-response analysis yields several critical parameters that characterize drug activity:
Potency: The dose required to produce a defined therapeutic effect. The more potent a drug is, the lower the dose necessary to yield the same response. Potency is typically quantified by the EC50 (half-maximal effective concentration) or ED50 (median effective dose) values [84] [4].
Efficacy: The maximum therapeutic response a drug can produce, regardless of dose. This is distinct from potency and often more clinically significant. Efficacy is determined by the height of the dose-response curve plateau [4].
Slope: The steepness of the linear portion of the dose-response curve determines how sensitive the response is to changes in drug concentration. A steeper slope indicates that a small change in dose produces a large change in effect [86] [4].
For toxic effects, parallel parameters are used: TD50 (median toxic dose) and LD50 (median lethal dose, typically determined in animal studies) [85].
The Sigmoidal Dose-Response Curve
Most drugs follow a sigmoidal (S-shaped) dose-response curve when response is plotted against the logarithm of the dose [84] [4]. This curve has three distinct phases:
Lag Phase: At low doses, the response is minimal as drug concentrations are insufficient to significantly activate receptors or pathways.
Linear Phase: Response increases exponentially with increasing dose until it reaches a point where the relationship becomes linear. This phase typically encompasses the EC50/ED50 point.
Plateau Phase: Further increases in dose produce diminishing returns in effect until the maximum response (Emax) is reached [4].
The sigmoidal shape results from the fundamental principles of drug-receptor interactions and represents the transition from insufficient receptor occupancy through proportional response to ultimately, saturation of available receptors [84].
Defining Therapeutic Index and Safety Margin
Therapeutic Index (TI)
The Therapeutic Index (TI) is a quantitative measurement of the relative safety of a drug that compares the dose that produces toxicity to the dose needed to produce the desired therapeutic response [85] [87]. Classically, TI is calculated using the 50% dose-response points according to the following formula:
TI = TD50 / ED50 or TI = LD50 / ED50 [85] [86]
Where:
- TD50 = Toxic dose for 50% of the population
- LD50 = Lethal dose for 50% of the population (from animal studies)
- ED50 = Effective dose for 50% of the population
A higher TI value indicates a wider margin between effective and toxic doses, representing a more favorable safety profile [85] [86]. For instance, the opioid remifentanil has a TI of 33,000:1, indicating exceptional forgiveness in dosing, while drugs like digoxin have a TI of approximately 2:1, requiring careful therapeutic drug monitoring [85].
Limitations of Therapeutic Index and the Need for Safety Margin
The classical Therapeutic Index has significant limitations in fully characterizing drug safety. By using median values (50% points), the TI fails to account for the variability in individual sensitivity to both therapeutic and toxic effects [86]. This limitation is particularly problematic when the dose-response curves for efficacy and toxicity have different slopes, or when the curves overlap at non-median points [86].
To address these limitations, the Margin of Safety (MOS) was developed as a more conservative safety parameter. The MOS typically compares doses at the extreme ends of the response spectrum:
MOS = TD1 / ED99 or MOS = LD1 / ED99 [86]
Where:
- TD1 = Toxic dose for 1% of the population
- LD1 = Lethal dose for 1% of the population
- ED99 = Effective dose for 99% of the population
The MOS provides a more protective safety assessment by ensuring that even highly sensitive individuals (who experience toxicity at low doses) are protected, while ensuring that the vast majority of the population (99%) still receives therapeutic benefit [86].
Figure 1: Relationship between dose-response curves and safety parameters, showing how Therapeutic Index and Margin of Safety are derived and related.
Calculation Methodologies and Experimental Protocols
Determining ED50, TD50, and LD50
The foundation for calculating safety parameters lies in accurately determining the key dose-response values through well-designed experimental protocols.
ED50 Determination Protocol
Experimental Design: Administer a minimum of five different doses of the test compound to groups of experimental animals (typically 6-10 animals per group). Doses should span the anticipated effective range and be spaced logarithmically [84].
Response Measurement: Measure the specific therapeutic endpoint of interest for each animal at predetermined time points. This could include biochemical markers, behavioral responses, or physiological changes.
Data Analysis: Plot the percentage of animals showing the desired therapeutic effect (or the magnitude of effect for continuous data) against the logarithm of the dose.
Curve Fitting: Fit a sigmoidal curve to the data using nonlinear regression analysis. The ED50 is the dose at which 50% of the maximum therapeutic response is observed [84].
LD50 Determination Protocol (OECD Guidelines)
Dose Selection: Based on range-finding studies, select a series of doses that are expected to cause mortality ranging from 0% to 100%.
Animal Administration: Administer the test compound to groups of healthy adult animals (typically 5-20 animals per group, with reduced numbers encouraged under modern ethical guidelines) [88].
Observation Period: Monitor animals for mortality over a predetermined period (typically 14 days for acute toxicity studies), recording all observations.
Statistical Analysis: Calculate the LD50 using appropriate statistical methods such as the probit, logit, or Spearman-Karber methods [88].
Advanced Calculation Approaches
Modern approaches to calculating safety parameters have evolved beyond the classical formulas:
Exposure-Based TI: In drug development settings, TI is increasingly calculated based on plasma exposure levels rather than administered dose, accounting for inter-individual variability in pharmacokinetics [85].
Probabilistic Framework: A unified probabilistic framework for dose-response assessment has been developed that distinguishes between individual and population-level dose response and incorporates both uncertainty and variability in toxicity as a function of human exposure [89].
Model-Informed Approaches: Modeling approaches support dose-response characterization by utilizing data across dose levels to fit a continuous curve rather than analyzing each dose level separately. Model-based methods, such as Emax modeling or MCP-Mod, incorporate assumptions about the dose-response relationship to improve the precision of dose-response and target dose estimation [18].
Comparative Analysis of Safety Parameters
Therapeutic Indices of Common Drugs
Table 1: Therapeutic Indices of Selected Pharmaceutical Agents
| Drug | Therapeutic Index | Clinical Implications |
|---|---|---|
| Remifentanil [85] | 33,000:1 | Exceptionally wide safety margin; minimal risk of overdose at therapeutic doses |
| Diazepam [85] | 100:1 | Moderate safety margin; requires careful dosing |
| Morphine [85] | 70:1 | Moderate safety margin; risk of respiratory depression at higher doses |
| Cocaine [85] | 15:1 | Narrow safety margin; high abuse and toxicity potential |
| Ethanol [85] | 10:1 | Narrow safety margin; risk of acute poisoning |
| Digoxin [85] | 2:1 | Very narrow safety margin; requires therapeutic drug monitoring |
Comparison of TI and MOS Values
Table 2: Comparison of TI and MOS Values for Various Substances
| Substance | TI (Classical) | MOS (Conservative) | Notable Characteristics |
|---|---|---|---|
| Amphetamine (dog) [88] | 2.95 | 0.03 | Significant difference between TI and MOS indicates high sensitivity in subpopulation |
| Lysergic acid diethylamide (rabbit) [88] | 15.0 | 0.15 | Moderate TI but very low MOS indicates unpredictable toxicity |
| Potassium permanganate (mouse) [88] | 1499.7 | 15.1 | High TI and moderate MOS indicates relatively predictable toxicity |
| Crotalus durissus terrificus venom [88] | 0.69 | 0.003 | TI <1 indicates higher toxicity than efficacy; extremely low MOS |
Advanced Concepts and Modern Applications
Therapeutic Index in Targeted Therapies
The concept of therapeutic index has evolved significantly with the advent of targeted therapies, particularly in oncology:
Radiotherapy Therapeutic Ratio: In cancer radiotherapy, the therapeutic ratio is determined by the maximum radiation dose for killing cancer cells and the minimum radiation dose causing acute or late morbidity in normal tissues. Both parameters have sigmoidal dose-response curves, and a favorable outcome occurs when the dose-response for tumor tissue is greater than that of normal tissue for the same dose [85].
Molecular Targeting: The effective therapeutic index can be enhanced through targeting technologies that concentrate the therapeutic agent in its desirable area of effect. Molecular targeting of DNA repair pathways can lead to radiosensitization or radioprotection, improving the therapeutic ratio [85].
Machine Learning Approaches
Modern computational approaches are enhancing dose-response prediction and therapeutic index estimation:
Multi-Output Gaussian Process (MOGP) Models: These models simultaneously predict all dose-responses and uncover their biomarkers by describing the relationship between genomic features, chemical properties, and every response at every dose. MOGP models enable assessment of drug efficacy using any dose-response metric and have shown effectiveness in accurately predicting dose-responses across different cancer types [39].
Biomarker Discovery: Machine learning models can identify biomarkers of response by measuring feature importance. For example, MOGP models with Kullback-Leibler divergence relevance scoring have identified EZH2 gene mutation as a novel biomarker of BRAF inhibitor response, which was not detected through traditional ANOVA analysis [39].
Regulatory Considerations
Regulatory agencies evaluate dose-response analysis to determine the therapeutic window where a drug is effective but not toxic. This analysis informs drug approval decisions and dosing guidelines. Importantly, dose-response curves help determine safety margins for vulnerable populations, including children, the elderly, and pregnant women [4].
The International Council for Harmonisation (ICH) guidelines emphasize the importance of characterizing dose-response relationships for both desired and adverse effects, requiring manufacturers to establish a well-characterized efficacy-safety relationship before drug approval [18].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Dose-Response and Safety Parameter Studies
| Research Tool | Function | Application Context |
|---|---|---|
| FLIPR Penta High-Throughput System [4] | High-throughput kinetic screening | Toxicology and lead compound identification |
| Benchmark Dose Software (BMDS) [90] | Dose-response modeling | Statistical analysis of toxicological data for risk assessment |
| Multi-Output Gaussian Process Models [39] | Predicting dose-response curves | Drug repositioning and biomarker discovery across cancer types |
| Dr-Fit Software [4] | Automated fitting of multiphasic dose-response curves | Analysis of complex drug mechanisms with multiple biological phases |
| PubChem Database [39] | Chemical feature repository | Source of drug chemical properties for predictive modeling |
| Cancer Cell Line Encyclopedia [4] | Drug response database | Reference dataset for validating predictive models |
Interpretation Guidelines and Decision Frameworks
Clinical Decision-Making Based on TI and MOS
Interpreting therapeutic index and safety margin values requires contextual understanding:
TI > 100: Generally considered safe for most clinical applications without specialized monitoring [85].
TI 10-100: Requires standard clinical monitoring and patient education about potential side effects [85].
TI < 10: Narrow therapeutic index; warrants therapeutic drug monitoring, individualized dosing, and careful patient selection [85].
MOS < 1: Indicates that toxic effects may occur at doses lower than fully effective doses for some individuals. Such drugs require extreme caution in clinical use [86].
Integrating TI with Other Pharmacological Parameters
A comprehensive safety assessment integrates therapeutic index with other key parameters:
Therapeutic Window: The range of doses between the minimum effective concentration and the minimum toxic concentration [85].
No Observed Adverse Effect Level (NOAEL): The highest dose at which no harmful effects are observed [4].
Lowest Observed Adverse Effect Level (LOAEL): The lowest dose where a harmful effect is observed [4].
Protective Index: Similar to safety-based therapeutic index but uses TD50 instead of LD50, often more informative about a substance's relative safety since toxicity often occurs at levels far below lethal effects [85].
Figure 2: Decision framework for clinical monitoring strategies based on Therapeutic Index and Margin of Safety values.
Therapeutic index and safety margin remain cornerstone concepts in preclinical pharmacology, providing critical quantitative measurements of a drug's relative safety. While classical calculations using ED50 and TD50/LD50 values offer fundamental insights, modern drug development increasingly relies on more sophisticated approaches including exposure-based calculations, probabilistic frameworks, and machine learning models that incorporate biomarker data [85] [89] [39].
Proper interpretation of these safety parameters requires understanding their limitations and contextualizing them within the complete pharmacological profile of a drug. As personalized medicine advances, the future of therapeutic indexing lies in developing patient-specific safety parameters that incorporate individual genetic, physiological, and environmental factors to optimize the balance between efficacy and toxicity for each patient.
The accurate calculation and interpretation of therapeutic index and safety margin from dose-response data remains an essential competency for researchers and drug development professionals, forming the basis for informed decision-making throughout the drug development pipeline from preclinical studies to clinical application.
Dose-response meta-analysis (DRMA) is a powerful statistical methodology that quantifies the relationship between the dose or exposure level of a treatment, nutrient, or toxic agent and a specific outcome of interest across multiple studies. Unlike conventional meta-analysis that compares only two groups (e.g., treatment vs. control), DRMA investigates how the effect magnitude changes across different exposure levels, enabling the identification of potential nonlinear patterns, threshold effects, and optimal dosage ranges. This approach is particularly valuable in preclinical research and drug development, where understanding the precise relationship between compound concentration and biological response is fundamental to establishing therapeutic efficacy and safety profiles [91] [92].
The core objective of dose-response meta-analysis is to synthesize evidence from multiple independent studies to model the functional form of the relationship between exposure and response. This process allows researchers to address critical questions that cannot be answered by simple pair-wise comparisons: What is the shape of the dose-response relationship? Is there a dose level beyond which no further benefit is observed? What is the lowest effective dose? By applying rigorous statistical modeling to pooled data, DRMA provides a more nuanced and informative evidence synthesis than traditional methods, making it an indispensable tool for evidence-based decision-making in pharmaceutical development, toxicology, and clinical practice [70].
The interpretation of dose-response curves in preclinical research constitutes a fundamental aspect of this methodology. These curves graphically represent the relationship between the dose of a compound and the magnitude of the biological response, providing critical insights into potency, efficacy, and therapeutic window. In preclinical settings, accurately characterizing these relationships informs lead compound optimization, dosing regimen design for initial clinical trials, and safety assessment. The meta-analytic approach strengthens this interpretation by increasing statistical power and precision through pooled data, enabling more reliable estimation of curve parameters and facilitating the exploration of between-study heterogeneity in reported dose-response relationships [93] [70].
Fundamental Methodological Framework
Core Statistical Models
Dose-response meta-analysis typically employs nonlinear models to capture the relationship between exposure and outcome. Three common functions used in toxicology and pharmacology, as identified by Ritz (2010), include [70]:
- Log-logistic model:
f(x;b,c,d,e) = c + (d-c) / [1 + exp(b(log(x)-log(e)))] - Log-normal model:
f(x;b,c,d,e) = c + (d-c) * Φ(-b(log(x)-log(e))) - Weibull model:
f(x;b,c,d,e) = c + (d-c) * exp(-exp(b(log(x)-log(e))))
In these models, parameters c and d represent the lower and upper asymptotic limits of the response, e typically represents the ED~50~ (dose producing half-maximal effect) or inflection point, and b determines the slope or steepness of the curve at dose e. These models are fitted using maximum likelihood or nonlinear least-squares estimation to pooled data from multiple studies, often within a random-effects framework to account for between-study heterogeneity [70].
The statistical analysis in DRMA is typically performed using a two-stage approach. In the first stage, study-specific dose-response relationships are estimated using a method that accounts for the correlation of effects across dose levels within each study. In the second stage, the study-specific curves are combined to derive an overall dose-response relationship. Alternatively, a one-stage approach using mixed models can be implemented, which models all data simultaneously while incorporating random effects to account for between-study variability. The selection between these approaches depends on the number of available studies, the consistency of dose levels across studies, and the computational resources available [91] [92].
Data Extraction and Preparation
The success of a dose-response meta-analysis critically depends on rigorous data extraction and standardization. Key data items that must be extracted from each primary study include [93] [91]:
- Number of subjects or experimental units for each dose level
- Outcome measures for each dose level (means, proportions, counts)
- Variability measures for each dose level (standard deviations, standard errors, confidence intervals)
- Dose values and units of measurement
- Covariate information that might explain heterogeneity
When studies report doses in different units or compounds with varying bioactivity, dose standardization is essential. This may involve conversion to common units, normalization to body surface area or weight, or expression as a percentage of maximum tolerated dose. For phytochemicals like curcumin or sulforaphane, where bioavailability varies considerably based on formulation, this standardization presents particular challenges that must be transparently addressed [93] [92].
A critical aspect of data preparation involves handling missing data, which is common in published reports. Authors may need to be contacted for complete dataset information. When not available, statistical techniques such as multiple imputation or algebraic transformations can be employed to derive missing variability measures from available statistics (e.g., p-values, confidence intervals) [91].
Experimental Design Considerations for Dose-Response Studies
Optimal Design Principles
The experimental design of dose-response studies significantly influences the precision of parameter estimates. Statistical optimal design theory provides a framework for selecting dose levels and allocating samples to minimize the number of experimental units required while maintaining desired precision. According to research on optimal experimental designs for dose-response studies, the key principles include [70]:
- D-optimality: Selecting dose levels that minimize the variance of parameter estimates, typically requiring control plus only three dose levels for four-parameter models
- Allocation efficiency: Distributing experimental units across dose levels to maximize information gain
- Practical constraints: Balancing statistical optimality with physical and administrative limitations (e.g., 96-well plate capacities in cytotoxicity studies)
For the commonly used nonlinear models in toxicology, D-optimal designs generally place dose levels at the extremes (to estimate asymptotes) and near the ED~50~ region (where the curve has maximum slope), with an additional point in the transition region to better define the curve shape. This approach stands in contrast to traditional designs motivated by convention rather than statistical efficiency [70].
Bayesian Optimal Designs
A significant challenge in designing dose-response studies is that optimal designs depend on prior knowledge of the model parameters, which are unknown before conducting the experiment. This circular problem is addressed through Bayesian optimal designs, which incorporate uncertainty about the prior parameter estimates. Bayesian designs consider a distribution of possible parameter values rather than fixed values, resulting in designs that are robust to misspecification of initial parameter estimates [70].
These designs are particularly valuable in preclinical research, where prior information may be available from similar compounds or preliminary experiments. The Bayesian approach allows researchers to formally incorporate this information into the design process, leading to more efficient experiments and reducing the risk of inadequate dose placement that could compromise the study objectives [70].
Table 1: Key Characteristics of Common Dose-Response Models
| Model | Function Form | Parameters | EDâ‚…â‚€ Position | Common Applications |
|---|---|---|---|---|
| Log-Logistic | (f(x) = c + \frac{d-c}{1+\exp(b(\log(x)-\log(e)))}) | c: lower asymptoted: upper asymptotee: EDâ‚…â‚€b: slope | e corresponds to EDâ‚…â‚€ | Herbicide studies,Bioassay research |
| Log-Normal | (f(x) = c + (d-c) \cdot \Phi(-b(\log(x)-\log(e)))) | c: lower asymptoted: upper asymptotee: EDâ‚…â‚€b: slope | e corresponds to EDâ‚…â‚€ | Toxicology,Environmental risk assessment |
| Weibull | (f(x) = c + (d-c) \cdot \exp(-\exp(b(\log(x)-\log(e))))) | c: lower asymptoted: upper asymptotee: inflection pointb: shape | Does not directly correspond to EDâ‚…â‚€ | Failure time analysis,Cell survival curves |
Current Applications in Preclinical and Clinical Research
Phytochemical Research
Dose-response meta-analysis has been increasingly applied to evaluate the effects of natural compounds in both preclinical and clinical settings. A recent systematic review and meta-analysis examined the effects of turmeric/curcumin supplementation on anthropometric indices in subjects with prediabetes and type 2 diabetes mellitus. This comprehensive analysis of 20 randomized controlled trials demonstrated that curcumin supplementation significantly decreased body weight, waist circumference, and fat mass percentage in diabetic patients, with a dose-response relationship indicating optimal effects at specific dosage ranges [92].
Similarly, a systematic review and meta-analysis of preclinical studies investigated sulforaphane's role in osteosarcoma treatment. The analysis of 10 eligible articles revealed that sulforaphane, a naturally occurring isothiocyanate found in cruciferous vegetables, exhibited potent anti-cancer properties through multiple mechanisms including reduced cell viability, induced apoptosis, cell cycle arrest, and decreased invasiveness and migration. The meta-analysis highlighted clear dose-dependent effects while also noting challenges related to bioavailability that must be considered when interpreting dose-response relationships for this compound [93].
Nutritional Intervention Studies
In the field of nutritional sciences, dose-response meta-analysis has been instrumental in establishing evidence-based recommendations for nutrient intake. A dose-response meta-analysis of randomized clinical trials investigated the effects of omega-3 supplementation on body weight in patients with cancer cachexia. This analysis revealed a non-significant linear relationship between omega-3 dosage and body weight, with supplementation of ≤1 gram increasing body weight while higher doses (>1 gram) resulted in decreased body weight. The study demonstrated the importance of considering patient characteristics such as age and baseline weight when interpreting dose-response relationships, as significant effects were observed specifically in older patients (≥67 years) with lower baseline weight (≤60 kg) [91].
These applications demonstrate the value of DRMA for identifying not only whether an intervention is effective, but also the specific conditions under which it is most effective, including optimal dosing ranges and patient subgroups most likely to benefit. This level of precision is particularly valuable for developing personalized medicine approaches and targeted therapeutic strategies [91] [92].
Implementation Protocols and Analytical Workflow
PRISMA-Guided Systematic Review
The foundation of a robust dose-response meta-analysis is a comprehensive systematic literature review conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The protocol should be registered in advance with international platforms such as PROSPERO or INPLASY to enhance transparency and reduce reporting bias. The search strategy should encompass multiple electronic databases (e.g., PubMed, EMBASE, Web of Science, Scopus) using a combination of Medical Subject Headings (MeSH) and free-text terms related to the intervention and outcomes of interest [93] [91] [92].
The study selection process involves a rigorous two-stage screening of titles/abstracts followed by full-text assessment against predetermined inclusion and exclusion criteria. For dose-response meta-analysis, specific inclusion criteria typically encompass studies that [93] [92]:
- Report on at least three different dose levels of the intervention
- Provide quantitative data on both exposure and outcome variables
- Include appropriate measures of variance or sufficient data to calculate them
- Use a study design that minimizes confounding (e.g., randomized controlled trials for clinical questions)
Data extraction should be performed independently by at least two reviewers using a standardized form, with disagreements resolved through consensus or third-party adjudication. The Cochrane Risk of Bias tool is commonly employed to assess study quality, evaluating domains such as random sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other potential sources of bias [92].
Statistical Analysis Pipeline
The analytical workflow for dose-response meta-analysis involves several sequential steps:
Data transformation and standardization: Convert all doses to common units and transform effect sizes to appropriate metrics for analysis.
Study-specific curve estimation: Fit candidate dose-response models (e.g., linear, quadratic, restricted cubic splines) to data from each study.
Pooled analysis: Combine study-specific curves using random-effects meta-analysis to account for between-study heterogeneity.
Goodness-of-fit evaluation: Assess model fit using statistical measures (e.g., Akaike Information Criterion, Bayesian Information Criterion) and graphical diagnostics.
Sensitivity and subgroup analyses: Evaluate the robustness of findings to various assumptions and explore potential sources of heterogeneity.
Publication bias assessment: Use statistical tests (e.g., Egger's test) and graphical methods (e.g., funnel plots) to evaluate potential small-study effects.
Advanced techniques such as multivariate meta-analysis may be employed to account for correlations between multiple dose-response estimates from the same study, while multilevel meta-analysis can address hierarchical data structures commonly encountered in synthesized evidence [91] [92].
Table 2: Research Reagent Solutions for Dose-Response Studies
| Reagent/Category | Function in Dose-Response Research | Example Applications |
|---|---|---|
| Cell Viability Assays (MTT, CCK-8) | Quantify cellular metabolic activity as proxy for viability across compound concentrations | Determine ICâ‚…â‚€ values in cytotoxicity studies [93] |
| Apoptosis Detection Kits (Annexin V, Caspase-3) | Measure programmed cell death induction at different drug doses | Evaluate chemotherapeutic mechanisms of action [93] |
| Reactive Oxygen Species (ROS) Detection Probes | Quantify oxidative stress levels in response to increasing compound concentrations | Study antioxidant or pro-oxidant compound effects [93] |
| Polyunsaturated Fatty Acids (Omega-3) | Modulate inflammatory pathways in nutrition intervention studies | Cancer cachexia management studies [91] |
| Curcumin/Turmeric Formulations | Test anti-inflammatory and metabolic effects with enhanced bioavailability | Diabetes and prediabetes intervention trials [92] |
| Sulforaphane Preparations | Investigate chemopreventive properties in cancer models | Osteosarcoma therapeutic studies [93] |
Advanced Methodological Considerations
Heterogeneity and Model Selection
A critical challenge in dose-response meta-analysis is dealing with between-study heterogeneity, which can arise from differences in study populations, methodologies, intervention formulations, and outcome measurements. The presence of heterogeneity should be quantified using statistics such as I², which describes the percentage of total variation across studies that is due to heterogeneity rather than chance. When substantial heterogeneity is detected, several approaches can be employed [91] [92]:
- Meta-regression: Explore the influence of study-level covariates on the dose-response relationship
- Subgroup analysis: Estimate separate dose-response curves for different study categories
- Random-effects models: Incorporate heterogeneity into the uncertainty of the overall effect estimate
- Multivariate models: Account for multiple correlated outcomes or dose-response relationships
Model selection is another crucial consideration, as the choice of dose-response function can significantly influence conclusions. While parametric models (e.g., log-logistic, Weibull) offer parsimony and biological interpretability, they impose specific shapes on the relationship. Flexible approaches such as restricted cubic splines require fewer assumptions about the functional form but demand more data points. Model adequacy should be assessed through both statistical goodness-of-fit measures and visual inspection of residuals [70].
Bayesian Approaches in Dose-Response Meta-Analysis
Bayesian methods offer several advantages for dose-response meta-analysis, particularly when dealing with complex evidence synthesis scenarios. The Bayesian framework naturally incorporates parameter uncertainty, allows for the integration of prior knowledge (e.g., from preclinical studies), and facilitates more intuitive interpretation of results through credible intervals. Bayesian approaches are especially valuable for [70]:
- Network meta-analysis: Comparing multiple interventions simultaneously while preserving randomization
- Hierarchical modeling: Accounting for multi-level data structures (e.g., studies, centers, patients)
- Evidence synthesis: Combining dose-response evidence from different study designs (e.g., randomized trials and observational studies)
- Predictive applications: Estimating expected outcomes at untested dose levels
Implementation of Bayesian dose-response meta-analysis typically requires Markov chain Monte Carlo (MCMC) methods and specialized software such as WinBUGS, JAGS, or Stan. While computationally intensive, these approaches provide maximum flexibility for modeling complex dose-response relationships and incorporating various sources of evidence [70].
Dose-response meta-analysis represents a sophisticated methodological advancement beyond conventional meta-analytic techniques, enabling researchers to characterize the functional relationship between exposure levels and health outcomes across multiple studies. The application of DRMA in preclinical research is particularly valuable for drug development, where understanding the precise relationship between compound concentration and biological response informs critical decisions about compound selection, dosing regimen design, and safety assessment.
The interpretation of dose-response curves derived from meta-analysis requires careful consideration of both statistical and biological factors. Key elements include the shape of the relationship (linear, monotonic, non-monotonic), the potency of the intervention (often represented by the ED~50~), the steepness of the response curve, and the maximum efficacy achievable. By synthesizing evidence across multiple studies, DRMA provides more precise estimates of these parameters than individual studies alone, contributing to more evidence-based preclinical research and translational science.
As methodological innovations continue to emerge, including Bayesian approaches, multivariate methods, and complex modeling of heterogeneous data, the application of dose-response meta-analysis is expected to expand further. These advances will enhance our ability to derive meaningful conclusions from synthesized evidence, ultimately supporting more informed decision-making in pharmaceutical development, toxicological risk assessment, and clinical practice.
In preclinical drug development, the dose-response curve is a fundamental quantitative tool that describes the relationship between the dose of a therapeutic agent and the magnitude of its effect. Properly interpreting these curves requires rigorous benchmarking against established standards and therapeutic comparators. This process transforms raw experimental data into meaningful insights about a candidate compound's efficacy, potency, and potential clinical utility. The fundamental challenge in preclinical valuation lies in the fact that biotech doesn't fit neatly into traditional valuation frameworks, with revenue often nonexistent and profits potentially years away [94]. Despite these challenges, accurate benchmarking provides critical decision-making tools for prioritizing drug candidates and de-risking development pipelines.
Beyond simple potency comparisons, modern dose-response analysis reveals subtler pharmacological properties, including slope factors, efficacy ceilings, and toxicological thresholds. Within the context of a broader thesis on dose-response interpretation, this guide establishes standardized methodologies for comparing your experimental results to established therapeutic standards across multiple dimensions. The integration of advanced computational approaches with robust experimental design now enables researchers to extract significantly more information from dose-response experiments than was previously possible, supporting more reliable go/no-go decisions in the drug development pipeline [39].
Foundational Concepts and Quantitative Benchmarks
Core Parameters for Therapeutic Benchmarking
The comparison of dose-response relationships relies on quantifying specific pharmacological parameters that can be statistically compared across experimental conditions. The table below outlines the essential metrics used in therapeutic benchmarking:
Table 1: Core Dose-Response Parameters for Therapeutic Benchmarking
| Parameter | Description | Interpretation | Benchmarking Utility |
|---|---|---|---|
| ECâ‚…â‚€/ICâ‚…â‚€ | Concentration producing 50% of maximal effect or inhibition | Measure of compound potency | Lower values indicate greater potency; direct comparison to established therapeutics |
| Eₘâ‚â‚“ | Maximal efficacy achievable | Biological system's response capacity | Determines if candidate matches or exceeds efficacy of standard therapy |
| Hill Slope | Steepness of the dose-response curve | Cooperativity in binding or signaling | Differentiates mechanism of action; indicates therapeutic window |
| Therapeutic Index | Ratio between toxic and therapeutic doses | Safety margin | Compared to standard-of-care; determines potential clinical viability |
| Area Under Curve (AUC) | Integrated response across all doses | Overall compound activity | Comprehensive efficacy assessment across concentration range |
Established Benchmark Values by Therapeutic Area
Different therapeutic classes exhibit characteristic benchmark ranges based on their mechanisms of action and target biology. The following table provides representative benchmark values for major drug classes:
Table 2: Representative Benchmark Ranges by Therapeutic Class
| Therapeutic Class | Typical ECâ‚…â‚€ Range | Typical Eₘâ‚â‚“ Expectation | Standard Comparator Examples |
|---|---|---|---|
| Oncology (cytotoxic) | nM-pM range | >80% tumor growth inhibition | Doxorubicin, Paclitaxel, Cisplatin |
| Receptor Agonists | Low nM range | Full receptor activation (100%) | Isoproterenol (β-adrenergic), Morphine (opioid) |
| Enzyme Inhibitors | nM range | >90% enzyme inhibition | Lisinopril (ACE), Statins (HMG-CoA reductase) |
| Ion Channel Blockers | µM-nM range | Varies by channel function | Verapamil (Ca²âº), Amiodarone (Kâº), Lidocaine (Naâº) |
| Antibiotics | µg/mL range | >99% bacterial killing | Penicillin, Ciprofloxacin, Vancomycin |
Methodological Framework for Curve Comparison
Experimental Design for Robust Comparisons
Valid benchmarking requires carefully controlled experiments that minimize variability and ensure fair comparisons. The following protocol outlines a standardized approach:
Direct Comparator Assay Protocol
- Parallel Plate Design: Test reference standards and experimental compounds on the same multi-well plate to minimize inter-assay variability
- Dose Range Selection: Utilize 8-12 concentrations in a logarithmic series (e.g., half-log dilutions) that bracket the expected ECâ‚…â‚€ values
- Replication Scheme: Include minimum of n=6 technical replicates per concentration and three independent experimental repeats (N=3)
- Control Placement: Position positive (reference therapeutic) and negative (vehicle) controls on every plate
- Blinded Analysis: Code compounds to prevent bias during data collection and initial analysis
For complex models such as heterogeneous tumour populations, specialized statistical approaches are required. A Monte-Carlo-based method can estimate required sample sizes in a two-arm tumour-control assay comparing dose modifying factors (DMF) between control and experimental arms [37]. This approach addresses scenarios where traditional power calculations are inadequate due to population heterogeneity in preclinical models.
Statistical Approaches for Curve Similarity Assessment
Determining whether two dose-response curves are statistically equivalent requires specialized hypothesis testing frameworks. Modern equivalence testing evaluates whether the maximal deviation between dose-response curves falls below a pre-specified similarity threshold (δ) [40]. The parametric bootstrap test for curve similarity involves:
- Model Specification: Define parametric models for each curve (e.g., 4-parameter logistic model)
- Parameter Estimation: Calculate maximum likelihood estimates for all model parameters
- Distance Metric Calculation: Compute maximal absolute difference between curves across the dose range
- Bootstrap Resampling: Generate resampled datasets under the null hypothesis of non-similarity
- Critical Value Determination: Establish the 95th percentile of the bootstrap distribution for the distance metric
- Similarity Conclusion: Reject non-similarity if the observed maximal difference is less than the critical value
This methodology can be extended to simultaneously compare multiple subgroups against a full population, which is particularly valuable in multiregional trial contexts where consistency across populations must be demonstrated [40].
Computational and Modeling Approaches
Multi-Output Gaussian Process for Enhanced Prediction
Advanced machine learning approaches now enable more sophisticated dose-response benchmarking. The Multi-Output Gaussian Process (MOGP) model simultaneously predicts all dose-responses and uncovers their biomarkers by describing the relationship between genomic features, chemical properties, and every response at every dose [39]. This approach offers significant advantages over traditional methods:
- Reduced Data Requirements: Accurate predictions with limited training data
- Comprehensive Assessment: Enables evaluation using any dose-response metric without pre-specification
- Biomarker Identification: Utilizes Kullback-Leibler divergence to identify features most relevant to drug response
- Uncertainty Quantification: Provides probabilistic predictions with confidence intervals
In practice, MOGP models have demonstrated utility in identifying novel biomarkers, such as discovering EZH2 gene mutation as a biomarker of BRAF inhibitor response that was not detected by conventional ANOVA analysis [39].
Indirect Comparison Methodology
When direct head-to-head experimental data is unavailable, indirect comparison methods enable estimation of relative treatment effects. The three primary approaches include:
Matching-Adjusted Indirect Comparison (MAIC)
- Re-weights individual patient data to match aggregate baseline characteristics of comparator study
- Can enhance power in some scenarios but risks type I error inflation
- Performance depends on careful selection of effect modifiers
Simulated Treatment Comparison (STC)
- Uses regression modeling to adjust for cross-trial differences
- Incorporates prognostic factors and effect modifiers
- Similar to MAIC, can be prone to bias if confounders are not properly adjusted
Bucher Method
- Preserves within-study randomization through simple analytic approach
- Performs well in situations without cross-trial differences or effect modification
- Considered more conservative but potentially less biased
Research indicates that indirect comparisons are considerably underpowered compared to direct head-to-head trials, and no single method demonstrates substantially superior performance across all scenarios [95] [96]. The choice of method should be guided by data availability and the presence of potential effect modifiers.
Experimental Protocols for Specific Applications
Tumor Control Dose-Response Assay
For oncology applications, tumor control assays provide critical dose-response data with direct clinical relevance:
Protocol: Tumor Control Dose-Response in Heterogeneous Models
- Model Selection: Utilize 6+ tumor models with different sensitivity profiles to capture population heterogeneity
- Treatment Groups: Randomize animals to receive different radiation dose levels (e.g., 0-80 Gy in 10 Gy increments)
- Endpoint Definition: Monitor tumors for recurrence until pre-defined follow-up time (typically 90-120 days)
- Response Classification: Label tumors as controlled (1) if no recurrence during follow-up, otherwise not controlled (0)
- Data Analysis: Calculate tumor-control probability (TCP) using logistic regression: TCP(d) = 1 / (1 + exp(-(β₀ + βâ‚×d)))
- Benchmark Comparison: Compute dose-modifying factor (DMF) relative to standard treatment: DMF = (βâ‚,reference - βâ‚,experimental) / βâ‚,reference
This approach specifically addresses population heterogeneity in preclinical models, which is essential for predicting clinical performance where patient populations are genetically diverse [37].
Signaling Pathway Inhibition Benchmarking
For targeted therapies, benchmarking requires specialized approaches that capture pathway-specific effects:
Protocol: Pathway Inhibition Dose-Response
- Pathway Activation: Stimulate signaling pathway with specific agonist (e.g., EGF for EGFR pathway)
- Compound Treatment: Apply test compounds and reference standards across concentration range
- Readout Measurement: Quantify phosphorylated targets via Western blot or phospho-ELISA
- Normalization: Express results as percentage of maximal pathway activation
- Curve Fitting: Apply four-parameter logistic model to determine ICâ‚…â‚€ for pathway inhibition
- Selectivity Assessment: Compare pathway ICâ‚…â‚€ to cytotoxicity ICâ‚…â‚€ to determine therapeutic window
Visualization of Workflows and Relationships
Experimental Workflow for Dose-Response Benchmarking
Figure 1: Dose-Response Benchmarking Workflow
Statistical Decision Framework for Curve Similarity
Figure 2: Curve Similarity Testing Framework
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for Dose-Response Benchmarking
| Reagent Category | Specific Examples | Function in Benchmarking | Quality Control Requirements |
|---|---|---|---|
| Reference Standards | USP compendial standards, Certified reference materials | Analytical comparators for assay validation | >98% purity, Certificate of Analysis, Stability data |
| Cell Line Panels | NCI-60, Cancer Cell Line Encyclopedia (CCLE) | Models of disease heterogeneity | Authentication via STR profiling, Mycoplasma testing |
| Pathway Reporters | Luciferase-based pathway assays, FRET biosensors | Quantification of specific pathway modulation | Validated response to known agonists/antagonists |
| Viability Assays | MTT, CellTiter-Glo, ATP-based assays | High-throughput cytotoxicity assessment | Linear range determination, Z'-factor validation |
| Signal Detection | Phospho-specific antibodies, Enzyme substrates | Molecular target engagement measurement | Specificity validation, Cross-reactivity profiling |
Implementation in Drug Development Decision-Making
Effective benchmarking of dose-response curves directly impacts portfolio strategy and resource allocation decisions in pharmaceutical R&D. Companies are increasingly leveraging AI and digital twins to create virtual replicas of patients for early testing of novel drug candidates [97]. These simulations help determine potential therapeutic effectiveness and accelerate clinical development decisions.
The integration of real-world evidence and multimodal capabilities that combine clinical, genomic, and patient-reported data is becoming a priority for 56% of life sciences companies, though only 21% view their current capabilities as robust in this area [97]. This gap represents both a challenge and opportunity for improving preclinical to clinical translation.
Furthermore, statistical approaches for assessing similarity in multiregional clinical trials are particularly relevant, as they evaluate whether dose-response relationships observed in global populations can be reliably extended to specific regions or subgroups [40]. These methods help identify intrinsic and extrinsic factors that could impact drug response across diverse populations.
Robust benchmarking of dose-response curves against established therapeutics remains a cornerstone of effective preclinical research. By implementing the standardized methodologies, statistical approaches, and experimental protocols outlined in this guide, researchers can generate more reliable, reproducible, and clinically predictive comparisons. As the industry faces increasing pressure to improve R&D productivity, these rigorous benchmarking approaches will play a critical role in prioritizing the most promising therapeutic candidates and advancing them efficiently through development pipelines.
Conclusion
Mastering the interpretation of dose-response curves is fundamental to successful preclinical research and drug development. A thorough understanding of key parameters—EC50 for potency, Emax for efficacy, and Hill slope for cooperativity—provides critical insights into a compound's biological activity. However, accurate interpretation requires more than just parameter calculation; it demands robust experimental design, appropriate mathematical modeling, and awareness of common pitfalls in translation from in vitro to in vivo systems and ultimately to clinical applications. The future of dose-response analysis lies in increasingly sophisticated model-informed drug development approaches, including adaptive trial designs and integrated dose-exposure-response modeling. These advanced techniques, combined with the foundational principles covered in this guide, will enable researchers to make more informed decisions in lead optimization, improve prediction of clinical outcomes, and ultimately enhance the efficiency of bringing new therapeutics to market. As personalized medicine advances, dose-response characterization will play an even greater role in tailoring treatments to specific patient populations and individual biomarkers.
References
- 1. – Dose - Wikipedia response relationship [https://en.wikipedia.org/wiki/Dose%E2%80%93response_relationship]
- 2. : Dose , Response & Examples Relationship Definition Curve [https://www.vedantu.com/biology/dose-response-relationship]
- 3. Reviewing methodological approaches to dose-response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12082932/]
- 4. - Dose | Response and Applications | Danaher Life... Curve Definition [https://lifesciences.danaher.com/us/en/library/dose-response-curve.html]
- 5. Best Practices for Preclinical Dose Range Finding Studies [https://www.altasciences.com/resource-center/blog/dose-range-finding-best-practices-preclinical-studies-blog]
- 6. Quantitative modeling of dose–response and drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4476235/]
- 7. Review Dose optimization in cancer drug development [https://www.sciencedirect.com/science/article/pii/S0959804925003752]
- 8. Mastering Dose- Response Curves [https://www.numberanalytics.com/blog/mastering-dose-response-curves-neuropharmacology]
- 9. How to Interpret Dose- Response Curves [https://www.sigmaaldrich.com/BE/en/technical-documents/technical-article/protein-biology/interrogation-protein-pathways/how-to-interpret-dose-response-curves]
- 10. Hill Equation: Setting up a dose-response curve - CDD Support [https://support.collaborativedrug.com/hc/en-us/articles/35945212110868-Hill-Equation-Setting-up-a-dose-response-curve]
- 11. Hill equation (biochemistry) [https://en.wikipedia.org/wiki/Hill_equation_(biochemistry)]
- 12. 50% of what? How exactly are IC50 and EC50 defined? [https://www.graphpad.com/support/faq/50-of-what-how-exactly-are-ic50-and-ec50-defined/]
- 13. IC50, EC50 and Kd: What is the Difference and Why Do ... [https://www.promegaconnections.com/ic50-ec50-and-kd-what-is-the-difference-and-why-do-they-matter/]
- 14. Potency and efficacy | Deranged Physiology [https://derangedphysiology.com/main/cicm-primary-exam/pharmacodynamics/Chapter-415/potency-and-efficacy]
- 15. Metrics other than potency reveal systematic variation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3947796/]
- 16. Notes on the Emax model [https://blog.djnavarro.net/posts/2024-01-09_emax-models/]
- 17. Equation: Specific binding with Hill slope [https://www.graphpad.com/guides/prism/latest/curve-fitting/reg_specific_hill.htm]
- 18. Dose-response characterization: A key to success in drug ... [https://pubmed.ncbi.nlm.nih.gov/40626332/]
- 19. Dose-Response Relationships - Clinical Pharmacology [https://www.merckmanuals.com/professional/clinical-pharmacology/pharmacodynamics/dose-response-relationships]
- 20. Steady-State Differential Dose Response in Biological Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5985043/]
- 21. How Do I Perform a Dose-Response Experiment? [https://www.graphpad.com/support/faq/how-do-i-perform-a-dose-response-experiment/]
- 22. A statistical framework for assessing pharmacological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7746236/]
- 23. Analysis and comparison of sigmoidal curves: application to dose-response data - PubMed [https://pubmed.ncbi.nlm.nih.gov/2610264/]
- 24. Reviewing methodological approaches to dose-response ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02585-3]
- 25. biphasic dose-response curve: Topics by Science.gov [https://www.science.gov/topicpages/b/biphasic+dose-response+curve.html]
- 26. A Practical Guide to Conducting Dose-Response Meta ... [https://meth.psychopen.eu/index.php/meth/article/view/14733]
- 27. Taking The Time To Study Competitive Antagonism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2189774/]
- 28. Agonist-Antagonist - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/agonist-antagonist]
- 29. Making Sense of Pharmacology: Inverse Agonism and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6165953/]
- 30. A framework to guide dose & regimen strategy for clinical drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8592517/]
- 31. Linear no-threshold model [https://en.wikipedia.org/wiki/Linear_no-threshold_model]
- 32. Linear No-Threshold Model - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/linear-no-threshold-model]
- 33. The Linear, No-Threshold Model - Radiation In Medicine - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK232710/]
- 34. The linear no-threshold debate: where do we go from here? [https://pubmed.ncbi.nlm.nih.gov/9547494/]
- 35. How To Regulate Radiation Exposure [https://thebreakthrough.org/issues/energy/how-to-regulate-radiation-exposure]
- 36. Preclinical Pharmacokinetics in Drug Development [https://www.allucent.com/resources/blog/role-pre-clinical-pharmacokinetics-early-drug-development]
- 37. Sample-size calculation for preclinical dose–response ... [https://www.sciencedirect.com/science/article/abs/pii/S0167814021060953]
- 38. Strategy for Designing In Vivo Dose-Response ... [https://pubmed.ncbi.nlm.nih.gov/39015015/]
- 39. Multi-output prediction of dose–response curves enables ... [https://www.nature.com/articles/s41698-024-00691-x]
- 40. Testing for Similarity of Dose Response in Multiregional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417559/]
- 41. Predicting drug combination response surfaces [https://www.nature.com/articles/s44386-024-00004-z]
- 42. Mechanism-Based Pharmacodynamic Modeling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3684160/]
- 43. Concentration-effect and dose-response relations in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2000728/]
- 44. How to Interpret Dose-Response Curves [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/protein-biology/interrogation-protein-pathways/how-to-interpret-dose-response-curves?srsltid=AfmBOoqDLQ0V9rPF0D_GQ6spF5fIEGNB_BAgDprjhGdZbcgUbPB0_SXN]
- 45. An automated fitting procedure and software for dose ... [https://www.nature.com/articles/srep14701]
- 46. Emax model and interaction index for assessing drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2974574/]
- 47. Introduction to Pharmacokinetic Modeling Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636497/]
- 48. MCP-Mod (Multiple Comparisons Procedure - Modelling) ... [https://www.statsols.com/articles/mcp-mod]
- 49. Good Practices in Modelâ€Informed Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4809625/]
- 50. Model-Informed Drug Development Training Course [https://c-path.org/training/model-informed-drug-development-training-course/]
- 51. Review: Role of Model-Informed Drug Development ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9097888/]
- 52. Preclinical research strategies for drug development [https://amsbiopharma.com/preclinical-research-drug-development/]
- 53. How to Interpret Dose-Response Curves [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/protein-biology/interrogation-protein-pathways/how-to-interpret-dose-response-curves?srsltid=AfmBOorOLDvFMoQgt94OANTcuLRZzzxSMg23980e_ul8twzAjL3ZR-Di]
- 54. 2.1 Dose-Response Modeling - GitHub Pages [https://uncsrp.github.io/Data-Analysis-Training-Modules/dose-response-modeling.html]
- 55. Data Visualisation in Clinical Research [https://careers.iconplc.com/blogs/2025-2/data-visualisation-in-clinical-research]
- 56. kusterlab/curve_curator: Analysis platform for large-scale ... [https://github.com/kusterlab/curve_curator]
- 57. Statistical Considerations for Preclinical Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4466166/]
- 58. Healthcare Data Quality Management Simplified for 2025 [https://blog.nalashaahealth.com/the-guide-to-healthcare-data-quality-management-in-2025/]
- 59. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 60. Sample Size and its Importance in Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6970301/]
- 61. What differentiates clinical trial statistics from preclinical ... [https://www.nature.com/articles/s41467-024-51486-4]
- 62. Graded dose-response curves [https://derangedphysiology.com/main/cicm-primary-exam/pharmacodynamics/Chapter-412/graded-dose-response-curves]
- 63. A Dose of Reality About Dose–Response Relationships [https://pmc.ncbi.nlm.nih.gov/articles/PMC10713937/]
- 64. How to Interpret Dose-Response Curves [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/protein-biology/interrogation-protein-pathways/how-to-interpret-dose-response-curves?srsltid=AfmBOop1kXV6Hkhk2lrzUol0GQhEnRDNpHWT-W0y_3CcUlS6VgZWzvk-]
- 65. Improved analysis of in vivo drug combination experiments ... [https://www.nature.com/articles/s41467-025-65218-9]
- 66. Qualification of mechanistic models in biopharmaceutical ... [https://www.sciencedirect.com/science/article/pii/S0022354924005458]
- 67. Tutorial on model selection and validation of model input into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10725261/]
- 68. Nonmonotonic Dose–Response Curves Occur in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6137554/]
- 69. Non-Monotonic Dose Responses - Endocrine Science Matters [https://endocrinesciencematters.org/non-monotonic-dose-responses-2/non-monotonic-dose-responses-technical-overview/]
- 70. Optimal experimental designs for dose–response studies with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4655015/]
- 71. FDA-AACR Strategies for Optimizing Dosages for Oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536354/]
- 72. Key Considerations for Improving Dosage Optimization in ... [https://www.aacr.org/blog/2025/10/03/key-considerations-for-improving-dosage-optimization-in-oncology/]
- 73. A normalized drug response metric improves accuracy and ... [https://www.nature.com/articles/s42003-020-0765-z]
- 74. Lost in translation: the valley of death across preclinical and ... [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]
- 75. Bridging the gap between preclinical and clinical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10043823/]
- 76. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 77. The Relevance of Goodnessâ€ofâ€fit, Robustness and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9787734/]
- 78. The Relevance of Goodness-of-fit, Robustness and ... [https://pubmed.ncbi.nlm.nih.gov/35773201/]
- 79. Enhancing binary dose–response analysis in clinical and ... [https://www.accscience.com/journal/JCTR/articles/online_first/5749]
- 80. A brief guide to statistical analysis of grouped data in ... [https://www.nature.com/articles/s42255-025-01323-9]
- 81. Preclinical Genomic Insights for Therapeutic Development [https://cellcarta.com/science-hub/preclinical-genomic-insights/]
- 82. What is the difference between efficacy and potency in ... [https://synapse.patsnap.com/article/what-is-the-difference-between-efficacy-and-potency-in-drug-development]
- 83. Quantitative Systems Pharmacology: An Exemplar Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6617832/]
- 84. How to Interpret Dose-Response Curves [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/protein-biology/interrogation-protein-pathways/how-to-interpret-dose-response-curves?srsltid=AfmBOopGZK0GX2fZAypQaUOw8QqjtUcQcvy_Qq5OTTwq-iBpRR1rK1Hl]
- 85. Therapeutic index [https://en.wikipedia.org/wiki/Therapeutic_index]
- 86. 2.4: Determining the Safety of a Drug [https://chem.libretexts.org/Bookshelves/Environmental_Chemistry/Toxicology_MSDT/6%3A_Principles_of_Toxicology/Section_2%3A_Dose_and_Dose_Response/2.4%3A_Determining_the_Safety_of_a_Drug]
- 87. Therapeutic Index [https://pharmacologycanada.org/Therapeutic-Index]
- 88. Comparative therapeutic index, lethal time and safety margin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7296648/]
- 89. A Unified Probabilistic Framework for Dose–Response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4671238/]
- 90. Dose Response Assessment - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/dose-response-assessment]
- 91. A dose–response meta-analysis of randomized clinical ... [https://www.sciencedirect.com/science/article/abs/pii/S2405457723023756]
- 92. The effect of turmeric/curcumin supplementation on ... [https://www.nature.com/articles/s41387-025-00386-7]
- 93. Sulforaphane's Role in Osteosarcoma Treatment [https://www.mdpi.com/2227-9059/13/5/1048]
- 94. Biotech Valuation Multiples: 2025 Insights & Trends [https://www.finrofca.com/news/biotech-revenue-multiples-2025]
- 95. Comparison of Methods for Estimating Therapy Effects by ... [https://pubmed.ncbi.nlm.nih.gov/32659160/]
- 96. Comparison of Methods for Estimating Therapy... [https://www.ovid.com/journals/medm/fulltext/10.1177/0272989x20929309~comparison-of-methods-for-estimating-therapy-effects-by]
- 97. 2025 life sciences outlook | Deloitte Insights [https://www.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-life-sciences-executive-outlook.html]