In Vivo Microdialysis for Neurotransmitter Analysis: A Comprehensive Guide for Researchers and Drug Developers
This article provides a comprehensive overview of in vivo microdialysis, a minimally invasive sampling technique pivotal for measuring unbound neurotransmitter concentrations in the brain extracellular fluid of awake, freely behaving...
In Vivo Microdialysis for Neurotransmitter Analysis: A Comprehensive Guide for Researchers and Drug Developers
Abstract
This article provides a comprehensive overview of in vivo microdialysis, a minimally invasive sampling technique pivotal for measuring unbound neurotransmitter concentrations in the brain extracellular fluid of awake, freely behaving animals. Tailored for researchers and drug development professionals, it covers the foundational principles and history of the technique, detailed methodological setup and calibration, advanced applications in pharmacokinetics and disease modeling, and troubleshooting for common experimental challenges. By integrating recent advances in analytical chemistry such as UHPLC and LC-MS/MS, and discussing validation against other methods, this guide serves as an essential resource for designing robust microdialysis studies to accelerate neuroscience research and central nervous system drug discovery.
Understanding In Vivo Microdialysis: Principles and Historical Context
Microdialysis is a minimally invasive sampling technique that enables the continuous monitoring of chemical events in the extracellular fluid of living tissues [1] [2]. By mimicking the passive function of a blood capillary, this method allows researchers to obtain a representative sample of the extracellular milieu without removing fluid from the tissue [2]. In neuroscience research, microdialysis has become an indispensable tool for measuring dynamic changes in neurotransmitter release and metabolism in specific brain regions of awake, freely-moving animals, providing critical insights into brain function and the mechanisms of drug action [3] [4].
The fundamental principle governing microdialysis is passive diffusion driven by concentration gradients across a semi-permeable membrane [2]. This technique permits both sampling of endogenous substances and local administration of exogenous compounds, making it uniquely versatile for pharmacological studies [4]. When applied to neurotransmitter monitoring, microdialysis offers the distinct advantage of measuring multiple neurochemicals simultaneously with high sensitivity, often in the picomolar range [3].
Core Principles and Technical Parameters
The Microdialysis Probe: Design and Function
The microdialysis probe serves as an artificial blood vessel, with its core component being a semi-permeable membrane positioned at the tip [1] [4]. The most common design employs a concentric tube structure where perfusion fluid enters through an inner tube, flows to its distal end, reverses direction into the space between the inner tube and outer dialysis membrane, and finally exits through the outlet tube for collection [1] [4]. It is within this space between the tubes that the essential "dialysis" process occurs – the diffusion of molecules between the extracellular fluid and the perfusion fluid [1].
The molecular weight cutoff of the membrane, typically ranging from 20-100 kilodaltons (kDa), determines the size range of molecules that can be sampled [2] [3]. Lower molecular weight cutoffs purify the sample by excluding large molecules, while higher cutoffs enable recovery of peptides and small proteins [4]. The membrane length also significantly influences recovery, with longer membranes generally providing better recovery, though this must be balanced against the size of the brain structure being studied [4].
Critical Factors Affecting Analytic Recovery
The efficiency of analyte recovery in microdialysis – referred to as relative recovery – depends on several interconnected factors [3]. Understanding and optimizing these parameters is essential for obtaining meaningful experimental data:
- Flow Rate: Lower flow rates (e.g., 0.1-1 µL/min) yield more concentrated dialysate by allowing more time for diffusion equilibrium, while higher flow rates (1-5 µL/min) remove more molecules per unit time but produce more dilute samples [2] [4].
- Membrane Surface Area: Larger surface areas, achieved through increased membrane length or diameter, enhance recovery by providing greater exchange area [3].
- Diffusion Characteristics: The diffusion coefficient of the target analyte and its penetration distance through the tissue to the probe membrane significantly influence recovery rates [3].
- Perfusate Composition: The perfusion fluid should ideally match the ionic composition of the extracellular fluid, commonly using artificial cerebrospinal fluid (aCSF) or Ringer's solution to minimize tissue disturbance [2] [3].
Table 1: Key Technical Parameters in Microdialysis Experiment Design
| Parameter | Typical Range | Impact on Recovery | Application Considerations |
|---|---|---|---|
| Flow Rate | 0.1 - 5 µL/min | Inverse relationship with concentration; lower flow = higher concentration | Low flow for concentrated samples; high flow for maximal molecule collection per time unit [2] [4] |
| Membrane Length | 1 - 4 mm | Positive relationship; longer membrane = higher recovery | Limited by size of target brain structure [4] |
| Molecular Weight Cutoff | 20 - 100 kDa | Determines size range of recovered molecules | Low MWCO for small molecules only; high MWCO for peptides/proteins [3] [4] |
| Membrane Material | Various polymers | Affects biocompatibility and fouling potential | CMA, D-I-6-02, and other commercial probes available [5] [6] |
Experimental Protocols
Protocol: Measuring Monoaminergic Neurotransmitters Following Pharmacological Challenge
This protocol outlines the steps for measuring extracellular levels of monoaminergic neurotransmitters (dopamine, DA; norepinephrine, NE; serotonin, 5-HT) and their metabolites in response to drug administration in awake, freely moving mice [6].
Materials and Surgical Preparation
- Animals: Mice (e.g., C57BL/6J)
- Anesthetic: Pentobarbital (Nembutal, 50 mg/kg) or equivalent
- Stereotaxic apparatus equipped with mouse adapter (e.g., David Kopf)
- Dialysis probe: D-I-6-02 with 50,000 Da cut-off (Eicom) or equivalent concentric design probe
- Dental cement for probe fixation
- Guide cannula (for chronic implantation)
Surgical Procedure:
- Anesthetize the mouse and secure it in the stereotaxic apparatus.
- Implant a guide cannula above the target brain region using stereotaxic coordinates from a mouse brain atlas [6].
- Secure the guide cannula to the skull using dental cement.
- Allow animals to recover individually for 2-3 days before experimentation [6].
Microdialysis Sampling and HPLC Analysis
- Perfusion solution: Ringer's solution (147 mM Na+, 4 mM K+, 2.3 mM Ca+, 155.6 mM Cl−) [6]
- Syringe pump (e.g., ESP-64, Eicom) for precise flow control
- Auto injector (e.g., EAS-2, Eicom) for automated sample handling
- HPLC system with electrochemical detection (e.g., HTEC-500, Eicom)
Experimental Procedure:
- Gently insert the microdialysis probe through the guide cannula into the target brain region.
- Place the mouse in a testing cage with free access to food and water.
- Perfuse the probe with Ringer's solution at 2.0 μL/min using a syringe pump [6].
- Collect dialysate samples automatically every 25 minutes using an auto injector [6].
- After collecting at least four baseline samples, administer either saline (control) or drug (e.g., 10 mg/kg BUP) intraperitoneally.
- Continue collecting at least six additional post-administration samples.
- Immediately inject each dialysate sample into the HPLC system for analysis.
HPLC-ECD Conditions [6]:
- Column: SC-50DS (Eicom)
- Mobile phase: 83% 0.1 M acetic acid-citric acid buffer (pH 3.5), 17% methanol, 190 mg/L octanesulfonic acid, 5 mg/L Naâ‚‚EDTA
- Flow rate: 0.23 mL/min
- Detection: Electrochemical detector with graphite electrode at +700 mV vs. Ag/AgCl reference electrode
Histological Verification
- After completing microdialysis measurement, perfuse eosin solution through the probe to mark its placement.
- Euthanize the mouse via pentobarbital overdose.
- Remove and fix the brain in 10% formaldehyde neutral buffer solution.
- Verify probe placement histologically through sectioning and microscopy [6].
Protocol: Integrated Neurotransmitter Analysis with LC-MS/MS
This advanced protocol utilizes liquid chromatography-tandem mass spectrometry (LC-MS/MS) for deep coverage of the brain extracellular metabolome, enabling identification of hundreds of compounds in microliter sample volumes [5].
Sample Collection and Preparation
- Animals: Male Sprague-Dawley rats (~75 days old, 340-375 g)
- Microdialysis probes: CMA 12 Elite with 4 mm membrane and 20,000 Da molecular weight cutoff [5]
- Perfusate: Artificial cerebrospinal fluid (aCSF: 145 mM NaCl, 2.68 mM KCl, 1.40 mM CaClâ‚‚, 1.01 mM MgSOâ‚„, 1.55 mM Naâ‚‚HPOâ‚„, 0.45 mM NaHâ‚‚POâ‚„, 0.25 mM ascorbic acid) [5]
- Flow rate: 1 μL/min during 12-hour collection from striatum [5]
Sample Preparation Options:
- Underivatized Analysis: Pool dialysate samples from multiple animals. For 10-fold concentration, transfer 750 μL aliquots to tapered glass vials, dry in a vacuum centrifuge, and reconstitute with 75 μL of appropriate solvent (9:1 water:methanol for RPLC; 85:15 acetonitrile:water for HILIC) [5].
- Chemical Derivatization: To enhance detection of polar neurotransmitters, derivatize equal aliquots of dialysate with light and heavy (13C6) benzoyl chloride separately to create detectable mass pairs for improved identification [5].
LC-MS/MS Analysis Conditions
- LC System: Thermo Fisher Scientific Vanquish Horizon LC
- Mass Spectrometer: Orbitrap ID-X mass spectrometer
- LC Columns:
- Reversed-phase (2.1 × 100 mm, 1.8 μm HSST3)
- HILIC (2.1 × 100 mm, 1.7 μm BEH Amide)
- Mass Spectrometer Settings [5]:
- Sheath gas: 40; Aux gas: 10; Sweep gas: 1
- Ion transfer tube temperature: 325°C; Vaporizer temperature: 300°C
- Orbitrap resolution: 120,000 (MS1), 60,000 (MS2)
- Scan range: 70-800 m/z
- Spray voltage: ±3200 V (positive/negative mode)
Data Processing and Compound Identification
- Software: MetIDTracker for untargeted MS/MS data
- Spectral Libraries: NIST20, Massbank of North America (MONA), MS-Dial LipidBlast
- Identification Confidence: Match experimental MS/MS spectra to reference libraries with appropriate scoring thresholds [5]
This approach has been shown to enable identification of 479 unique compounds from rat striatal dialysate, with approximately 60% detectable in 5 μL samples without preconcentration [5]. Benzoyl chloride derivatization further expands detection to 872 non-degenerate features, including most small molecule neurotransmitters and dopamine metabolites [5].
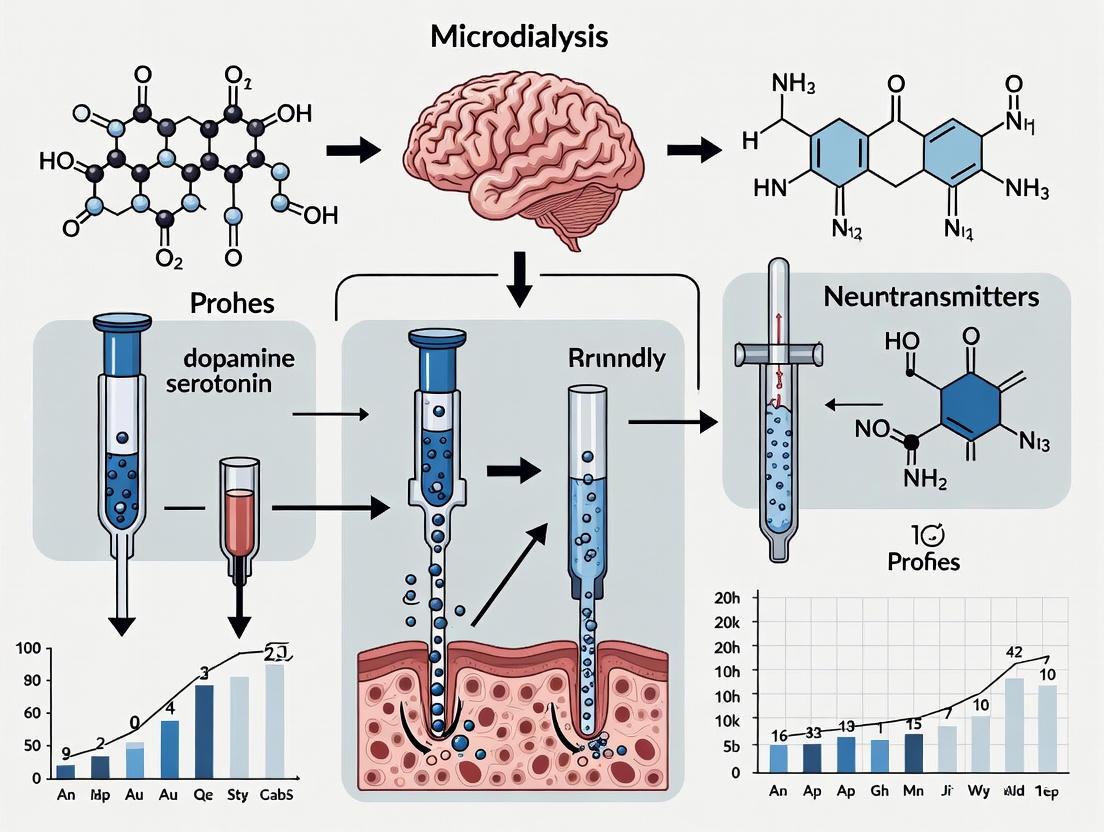
Visualization of Microdialysis Workflows
Microdialysis Principle and Probe Design
Integrated Experimental Workflow
Analytical Approaches and Data Interpretation
Quantitative Analysis of Neurotransmitters
Microdialysis sampling requires careful calibration to relate measured dialysate concentrations to true extracellular concentrations. The relative recovery – defined as the ratio of analyte concentration in the dialysate to that in the extracellular fluid – must be determined for accurate quantification [3]. The zero-net-flux method is often employed for this purpose, where the probe is perfused with different concentrations of the analyte of interest, and the tissue concentration is determined as the point where inflow and outflow concentrations are equal [2].
Table 2: Analytical Methods for Neurotransmitter Detection in Microdialysate
| Analytical Method | Detection Limit | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| HPLC-ECD | Low picomole to femtomole | Monoamines (DA, NE, 5-HT) and metabolites [6] | High sensitivity for electroactive compounds; Relatively low cost [6] | Limited to electroactive compounds; Lower compound identification confidence |
| LC-MS/MS | Low femtomole to attomole | Targeted and untargeted metabolomics; Multiple neurotransmitter classes [5] | High specificity and sensitivity; Broad compound coverage; Structural confirmation via MS/MS [5] | Higher instrument cost; Complex sample preparation; Matrix effects |
| Enzymatic Assays | Picomole | Energy metabolites (glucose, lactate, glycerol) | High specificity for target metabolites; Commercially available kits | Typically limited to single metabolites per assay |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials for Microdialysis Experiments
| Item | Specification | Function/Purpose |
|---|---|---|
| Microdialysis Probes | Concentric design; 1-4 mm membrane length; 20-100 kDa MWCO [5] [6] | Core sampling device implanted in target tissue |
| Perfusion Fluids | Artificial CSF or Ringer's solution [6] [3] | Physiological solution mimicking extracellular fluid composition |
| Syringe Pump | Low flow rate capability (0.1-5 µL/min); High precision [6] | Controls perfusion flow rate through the probe |
| Microvials | Low protein binding; 100-500 µL capacity | Collection of dialysate samples |
| Autosampler | Compatible with microvials; Temperature-controlled [7] | Automated sample handling and injection for HPLC |
| HPLC System | Binary or quaternary pump; Column oven; Autosampler [6] | Separation of analytes prior to detection |
| ECD Detector | Glassy carbon working electrode; Ag/AgCl reference; ±2000 mV range [6] | Sensitive detection of electroactive neurotransmitters |
| Mass Spectrometer | High resolution (Orbitrap, Q-TOF); Tandem MS capability [5] | Identification and quantification of multiple neurochemicals |
| Stereotaxic Apparatus | Species-specific adapters; Digital coordinate readout | Precise probe implantation in target brain regions |
| BMT-145027 | BMT-145027, CAS:2018282-44-3, MF:C23H14ClF3N4, MW:438.84 | Chemical Reagent |
| Notum-IN-1 | [1-(3,4-Dichlorophenyl)-1H-1,2,3-triazol-4-yl]methanol | CAS 338419-11-7. This high-purity [1-(3,4-dichlorophenyl)-1H-1,2,3-triazol-4-yl]methanol is a key triazole building block for antifungal and antimicrobial research. For Research Use Only. Not for human use. |
Applications in Neuropharmacology and Drug Development
Microdialysis provides critical insights for CNS drug development by enabling direct measurement of unbound drug concentrations in the brain extracellular fluid, which more accurately reflects pharmacologically active concentrations than total tissue levels or cerebrospinal fluid measurements [8]. When combined with blood microdialysis in the same animal, researchers can directly determine the unbound partition coefficient (Kp,uu), a key parameter for evaluating brain penetration [8].
In non-human primate studies, brain microdialysis has demonstrated particular translational value due to similarities in blood-brain barrier transporter expression between primates and humans [8]. For example, studies with carbamazepine – a non-P-gp substrate – have validated the technique, showing brain extracellular fluid concentrations reaching approximately 80% of free plasma concentrations, consistent with passive diffusion across the blood-brain barrier [8].
Beyond pharmacokinetic applications, microdialysis enables real-time monitoring of neurotransmitter responses to drug administration, facilitating comprehensive pharmacokinetic-pharmacodynamic (PK-PD) relationships for CNS-active compounds [4] [8]. This capability is particularly valuable for understanding the mechanisms of drugs for psychiatric and neurological disorders, where neurotransmitter dynamics are often central to therapeutic effects.
The accurate measurement of neurotransmitter dynamics in the awake, behaving brain remains a central challenge in neuroscience and drug development. Microdialysis has evolved to meet this challenge, transforming from a rudimentary sampling concept into a sophisticated, minimally-invasive technique that enables continuous measurement of unbound analyte concentrations in the extracellular fluid of virtually any tissue [9]. This evolution from early "dialytrodes" to modern hollow-fiber membranes represents a critical advancement in our ability to monitor neurochemical processes in vivo [10]. The technique's unique capability to sample endogenous neurotransmitters, hormones, and metabolites directly from the brain's extracellular space, while simultaneously permitting local drug delivery, has established it as a gold standard in neurochemical monitoring [11] [9]. This application note traces the historical development of microdialysis, details current protocols for neurotransmitter monitoring, and provides resources for implementing this powerful technique in neuroscience research and drug development programs.
Historical Development: From Dialytrodes to Hollow Fibers
The conceptual foundation of microdialysis was laid in the early 1960s with the use of push-pull cannulas and implanted dialysis sacs to study tissue biochemistry [12] [9]. These early approaches faced significant limitations, including limited sample number and poor temporal resolution. A critical advancement came in 1972 with the development of the first "dialytrode" by Delgado et al., which featured a slowly perfused dialysis bag that carried samples to an accessible site [12]. Ungerstedt and Pycock introduced the revolutionary "hollow fiber" concept in 1974, replacing dialysis bags with tubular semipermeable membranes approximately 200-300 μm in diameter [9]. This innovation dramatically improved sampling efficiency and formed the basis for the modern microdialysis probe.
The subsequent refinement of the needle probe design, consisting of a shaft with a hollow fiber at its tip that could be inserted into tissue via a guide cannula, established microdialysis as a practical and reliable neuroscientific tool [10]. The 1980s witnessed the coupling of microdialysis with high-performance liquid chromatography (HPLC) and electrochemical detection, enabling precise quantification of monoamines and other neurotransmitters [11]. This period also saw the technique's expansion beyond neurotransmitter monitoring to include energy substrates, drugs, and metabolites, solidifying its role in neuroscience and clinical research [12] [10].
Table 1: Evolution of Microdialysis Technology
| Time Period | Key Development | Primary Innovation | Significant Advancement |
|---|---|---|---|
| Early 1960s | Dialysis Sacs & Push-Pull Cannulas [12] [9] | First implantation into tissues to study biochemistry | Direct access to brain extracellular fluid |
| 1972 | Dialytrode [12] | Perfused dialysis bag with carried sample | Improved sample collection and accessibility |
| 1974 | Hollow Fiber [9] | Tubular semipermeable membrane (~200-300 μm diameter) | Dramatically improved sampling efficiency and reliability |
| 1980s | HPLC & Electrochemical Detection Coupling [11] | Analytical chemistry integration | Precise quantification of monoamines and neurotransmitters |
| 1990s-Present | Clinical Applications & Miniaturization [10] [11] | Human tissue monitoring & improved probe designs | Expanded to clinical settings, higher temporal and spatial resolution |
The following diagram illustrates the key developmental milestones in microdialysis technology:
Principles and Methodological Framework
Core Principles of Microdialysis
Microdialysis operates on the principle of passive diffusion across a semipermeable membrane, enabling the exchange of small molecules between the extracellular fluid and a perfused physiological solution [11] [9]. A typical microdialysis probe consists of a double-lumen catheter with a semipermeable membrane at its tip, which is implanted into the brain region of interest and perfused with an isotonic solution at controlled flow rates (typically 0.1-5 μL/min) [11]. The membrane's molecular weight cut-off (usually 6-100 kDa) determines which molecules can diffuse through, excluding larger proteins and macromolecules [9]. This molecular size exclusion allows microdialysis to sample specifically the free, unbound fraction of neurotransmitters and drugs that represents the pharmacologically active concentration [13].
The recovery of analytes – defined as the ratio of analyte concentration in the dialysate to that in the extracellular fluid – is a critical parameter in microdialysis methodology [9]. Recovery depends on several factors including membrane surface area, pore size, flow rate, and tissue properties [11]. Lower flow rates (<1 μL/min) typically increase relative recovery but decrease absolute recovery, necessitating careful optimization based on experimental requirements [11].
Calibration Methods
Accurate quantification of extracellular concentrations requires appropriate calibration methods to determine relative recovery [9]. The most common approaches include:
- No-Net-Flux Method: The probe is perfused with at least four different concentrations of the analyte of interest, and the point at which no net diffusion occurs represents the true extracellular concentration [9].
- Retrodialysis: Uses an internal standard added to the perfusate, assuming equal diffusion rates in both directions to estimate in vivo recovery [11] [9]. This method is particularly useful for exogenous compounds.
- Low-Flow-Rate Method: Extraction ratios are measured at different flow rates and extrapolated to zero flow, where complete equilibrium theoretically occurs [9].
- Dynamic No-Net-Flux Method: An extension of the no-net-flux method that allows determination of recovery over time, making it suitable for studies evaluating responses to drug challenges [9].
Table 2: Comparison of Microdialysis Calibration Methods
| Calibration Method | Principle | Best Suited Applications | Key Advantages | Important Limitations |
|---|---|---|---|---|
| No-Net-Flux [9] | Perfusion with varying analyte concentrations to find no-net-flux point | Endogenous compounds under steady-state conditions | Direct measurement of extracellular concentration | Requires steady-state conditions; time-consuming |
| Retrodialysis [11] [9] | Measurement of analyte disappearance from perfusate | Exogenous compounds; clinical settings | Simple implementation; suitable for drugs | Not applicable to endogenous compounds |
| Low-Flow-Rate [9] | Extrapolation from multiple flow rates to zero flow | Both endogenous and exogenous compounds | No addition of analyte required | Long calibration times; impractical for some applications |
| Dynamic No-Net-Flux [9] | Multiple subjects with single concentrations combined for regression | Endogenous compound response to challenges | Enables recovery determination over time | Requires multiple subjects/animals |
Experimental Protocols: Measuring Neurotransmitters in Awake Non-Human Primates
The following protocol describes the implementation of brain microdialysis in awake rhesus macaques to compare cortical neurotransmitter concentrations across different cognitive states, based on recently published methodology [14]. This approach enables simultaneous measurement of multiple neurotransmitters, including GABA, glutamate, norepinephrine, epinephrine, dopamine, serotonin, and choline, during performance of behavioral tasks.
Materials and Equipment
Table 3: Essential Research Reagents and Equipment
| Category | Specific Item | Function/Application |
|---|---|---|
| Surgical Components | Stereotactic frame, guide cannulas, removable insets | Precise probe implantation and stabilization |
| Microdialysis Probes | Concentric design hollow fiber probes, molecular weight cut-off 20-100 kDa | Sampling of neurotransmitters from extracellular fluid |
| Perfusion System | Micronfusion pump, microtubing, physiological perfusion solution (artificial CSF) | Controlled delivery of perfusion fluid to probe |
| Sample Collection | Microvials, refrigerated fraction collector | Maintenance of sample integrity post-collection |
| Analytical Instrumentation | UPLC-ESI-MS system, analytical column, mobile phases | Separation and quantification of neurotransmitters |
| Calibration Standards | GABA, glutamate, monoamines, choline reference standards | Method calibration and quantification |
Procedure
Guide Cannula Implantation: Under aseptic conditions and general anesthesia, implant guide cannulas with removable insets positioned above the target brain region (e.g., visual middle temporal area MT) using stereotactic coordinates. Secure the assembly within a standard recording chamber.
Postoperative Recovery: Allow a minimum of 2 weeks for surgical recovery before commencing experiments. Monitor animal health and wound healing throughout this period.
Probe Insertion and Equilibration: On experimental days, carefully replace the guide inset with a microdialysis probe, ensuring the membrane extends to the target depth. Begin perfusion with artificial cerebrospinal fluid at 1.0 μL/min and allow a minimum of 2 hours for stabilization of neurotransmitter levels post-insertion.
Sample Collection During Behavioral States: Collect dialysate samples at 20-minute intervals (<20 μL volume) during defined behavioral conditions:
- Active State: Animal engaged in cognitive tasks
- Inactive State: Animal at rest in testing apparatus Collect a minimum of 3 samples per behavioral condition to establish stable baseline measures.
Sample Processing: Immediately store collected samples at -80°C until analysis. Avoid multiple freeze-thaw cycles to maintain analyte stability.
Analytical Separation and Quantification:
- Utilize ultra-performance liquid chromatography with electrospray ionization-mass spectrometry (UPLC-ESI-MS)
- Employ a C18 reversed-phase column maintained at 35°C
- Implement a gradient elution with mobile phases consisting of 0.1% formic acid in water and 0.1% formic acid in acetonitrile
- Use multiple reaction monitoring (MRM) for maximal sensitivity and specificity
Data Analysis:
- Quantify neurotransmitter concentrations using external calibration curves
- Normalize data across subjects using protein content or probe recovery measurements
- Compare concentration variations between active and inactive states using appropriate statistical tests (e.g., paired t-tests, ANOVA with post-hoc comparisons)
- Analyze correlated concentration changes between neurotransmitter pairs
The following workflow diagram illustrates the key steps in this protocol:
Technical Notes and Optimization
- Flow Rate Considerations: Lower flow rates (0.1-0.5 μL/min) increase relative recovery but require longer collection intervals, creating a trade-off between concentration and temporal resolution [11].
- Temporal Resolution: Typical sample collection intervals range from 5-30 minutes, balancing analytical sensitivity with the ability to detect neurochemical fluctuations [13].
- Probe Placement Validation: Histological verification of probe placement is essential following experiment completion to confirm target region specificity.
- Behavioral State Transitions: Allow sufficient transition time between behavioral conditions to establish new steady-state neurotransmitter levels.
Applications in Neuroscience Research and Drug Development
Microdialysis has become an indispensable tool in neuroscience, enabling the quantification of neurotransmitters including dopamine, serotonin, glutamate, and acetylcholine in the brain during behavioral and pharmacological interventions [11]. The method allows for studies in awake, freely moving animals, facilitating correlation of neurochemical measures with specific behaviors [13]. Key application areas include:
- Neurodegenerative Disorders: Investigating neurochemical changes in Parkinson's disease, where microdialysis has revealed increased striatal tonic dopamine levels in response to subthalamic nucleus deep brain stimulation in rodent models [11].
- Neuropharmacology: Studying pharmacokinetics and pharmacodynamics of drugs in brain tissue, including assessment of blood-brain barrier transport and local drug delivery by measuring unbound drug concentrations [11] [13].
- Neurocritical Care: Monitoring biochemical markers of ischemia, such as glutamate and lactate/pyruvate ratios, in patients with traumatic brain injury, stroke, and subarachnoid hemorrhage, enabling early detection of secondary damage and guiding therapeutic interventions [10] [11].
- Drug Development: Evaluating tissue penetration of chemotherapeutic agents in tumors and antibiotics at infection sites, providing critical data on target site pharmacokinetics that cannot be obtained through plasma monitoring alone [10] [13].
Technical Challenges and Future Directions
Despite its widespread utility, microdialysis faces several technical challenges. Probe implantation causes tissue damage, with a concentric gradient of damaged cells extending approximately 250 μm from the probe, potentially confounding data interpretation [11]. The typical probe diameter of 200-300 μm significantly exceeds the intercapillary distance in rodent brains (approximately 30 μm), resulting in blood vessel damage, blood-brain barrier compromise, and rapid inflammatory responses including gliosis [11]. These tissue reactions can reduce probe stability and impede analyte diffusion. Temporal resolution is constrained by perfusion flow rates and sample volume requirements, typically limiting measurements to 5-minute intervals or longer [11].
Future developments focus on probe miniaturization through microfabrication techniques, with silicon microdialysis probes now reaching dimensions as small as 45 by 180 μm [11]. Emerging innovations include aptamer-based biosensors for selective molecular detection, multimodal devices combining chemical sensing with stimulation and electrophysiological recording, and segmented flow techniques that improve temporal resolution to under 15 seconds [11] [13]. Retrodialysis of anti-inflammatory agents like dexamethasone has shown promise in reducing glial scarring and restoring normal neurotransmitter dynamics around the probe [11]. These advances continue to enhance the spatiotemporal resolution and expand the capabilities of microdialysis in neuroscience research.
From its origins in basic dialytrode technology to the sophisticated hollow-fiber systems in use today, microdialysis has established itself as a fundamental tool for monitoring neurochemical dynamics in vivo. The technique's unique capacity to provide continuous measurement of unbound analyte concentrations in the extracellular fluid of virtually any tissue has made it invaluable for both basic neuroscience research and drug development. When implemented using the protocols described herein, microdialysis enables comprehensive investigation of neurotransmitter systems and their complex interplay in cognitive functions and behavioral states. As the technique continues to evolve through miniaturization, improved analytical coupling, and enhanced temporal resolution, its applications in understanding brain function and developing novel therapeutics will continue to expand.
In vivo microdialysis has revolutionized neuroscience research by enabling direct sampling of unbound neurotransmitters from the interstitial fluid of specific brain regions in behaving animals [12]. This technique provides critical insights into brain function by measuring the pharmacologically active fraction of neurotransmitters that interact with receptors to modulate neural circuits and behavior [15] [16]. Unlike traditional methods that measure total tissue content, microdialysis captures the dynamic, unbound neurotransmitter concentrations that reflect moment-to-moment neuronal activity and synaptic communication [17]. This Application Note details the scientific rationale for measuring unbound neurotransmitter concentrations and provides established protocols for implementing microdialysis in neurotransmitter research.
Core Advantages of Measuring Unbound Concentrations
The measurement of unbound extracellular neurotransmitter concentrations provides distinct advantages over total tissue content measurement for understanding brain function and drug effects.
Table 1: Key Advantages of Measuring Unbound Neurotransmitter Concentrations
| Advantage | Scientific Rationale | Research Application |
|---|---|---|
| Measures Pharmacologically Active Fraction | Unbound extracellular concentration directly correlates with receptor occupancy and activation [15]. | Essential for accurate pharmacokinetic/pharmacodynamic (PK/PD) modeling and determining therapeutic drug concentrations at target sites [16]. |
| Provides High Temporal Resolution | Continuous sampling allows monitoring of neurotransmitter flux in response to stimuli or drugs with minute-to-minute resolution [17]. | Ideal for studying neurotransmitter dynamics in behaviors like learning, addiction, and in response to pharmacological challenges [12] [17]. |
| Yields Protein-Free Samples | The semi-permeable membrane excludes macromolecules, including degrading enzymes, providing stable analytes ready for analysis [15]. | Enables direct injection into analytical systems (e.g., LC-EC, LC-MS) without additional sample cleanup, reducing analyte loss [15]. |
| Maintains Physiological Integrity | No fluid removal from the tissue, enabling continuous long-term sampling with minimal physiological disruption [15]. | Critical for chronic studies of neurotransmitter regulation in awake, freely moving animals, improving translational validity [12]. |
| Enables Anatomical Specificity | Small, precisely implanted probes allow sampling from discrete brain regions (e.g., striatum, nucleus accumbens) [12]. | Facilitates investigation of neurochemical heterogeneity across brain circuits implicated in specific disorders [15]. |
Experimental Protocols
Protocol 1: Conventional Microdialysis in Freely Moving Rats
This protocol details the steps for measuring basal and stimulated neurotransmitter release in the rat brain.
Probe Implantation and Animal Preparation
- Probe Selection: Use a concentric cannula design (250-350 μm diameter) with a polyacrylonitrile or regenerated cellulose membrane (e.g., [15]).
- Surgical Implantation: Anesthetize the rat and stereotaxically implant a guide cannula above the target brain region (e.g., striatum). Secure the cannula to the skull with dental acrylic and jeweler's screws. Allow a 24-48 hour recovery period before experimentation.
- Probe Insertion: On the experiment day, carefully insert the microdialysis probe through the guide cannula, extending the membrane into the target region.
Perfusion and Sample Collection
- Perfusion Fluid: Use an isotonic, buffered artificial cerebrospinal fluid (aCSF). For acetylcholine measurements, include a cholinesterase inhibitor (e.g., neostigmine, 0.1 μM) in the perfusate [12].
- Flow Rate: Perfuse the probe at a slow, constant rate ( 1.0 - 2.0 μL/min ) using a high-precision syringe pump [17].
- Sample Collection: Begin collection after an initial equilibration period (typically 60-120 minutes). Collect dialysate samples into microvials at 10-30 minute intervals. Keep samples on ice or a refrigerated fraction collector to preserve analyte integrity.
Analytical Determination
- Analysis: Analyze samples promptly using a suitable analytical method. For monoamines (dopamine, serotonin, norepinephrine), use Liquid Chromatography with Electrochemical Detection (LC-EC) [12] [15]. For amino acids (glutamate, GABA), use LC with fluorescence detection following derivatization.
- Quantification: Quantify neurotransmitter concentrations by comparing peak areas from dialysates against freshly prepared external standards.
Protocol 2: Quantitative Microdialysis (No-Net-Flux Method)
This method determines the true extracellular concentration (Ctrue) by accounting for variable probe recovery [12].
- Perfusate with Analytic: Following the establishment of a stable baseline, perfuse the probe with aCSF containing at least four different known concentrations of the target neurotransmitter (Cin), including zero.
- Measure Dialysate Concentration: For each perfused concentration (Cin), measure the corresponding dialysate concentration (Cout).
- Calculate Gain/Loss: Calculate the difference between Cout and Cin (i.e., Cout - Cin) for each concentration.
- Plot and Determine Ctrue: Plot (Cout - Cin) against Cintrue.
Workflow and Pathway Visualizations
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of microdialysis requires specific reagents and instrumentation.
Table 2: Essential Materials for Microdialysis Experiments
| Item | Function/Description | Example Application |
|---|---|---|
| Concentric Microdialysis Probe | A semi-permeable hollow fiber membrane on a concentric cannula for implantation into brain tissue [15]. | Sampling from discrete brain regions like striatum or hippocampus in rodents. |
| Artificial Cerebrospinal Fluid (aCSF) | Isotonic, buffered perfusion solution mimicking the ionic composition of brain extracellular fluid [12]. | Standard perfusate for collecting most neurotransmitters (e.g., monoamines, amino acids). |
| High-Precision Syringe Pump | Delivers perfusate at a constant, ultra-low flow rate (0.1 - 2.0 µL/min) [17]. | Critical for maintaining consistent recovery and temporal resolution. |
| Microsampling Vials | Small-volume collection vials to hold dialysate samples, often kept chilled. | Prevents analyte degradation during collection periods. |
| Liquid Chromatography System | Analytical instrument for separating neurotransmitters in the dialysate prior to detection [15]. | Standard setup for resolving complex mixtures of neurotransmitters and metabolites. |
| Electrochemical (EC) Detector | Highly sensitive detector that measures current from oxidation/reduction of electroactive analytes [15]. | Detection of monoamines (dopamine, serotonin, norepinephrine) and their metabolites. |
| ARS-1323-alkyne | ARS-1323-alkyne, MF:C28H27ClF2N6O3, MW:569.0 g/mol | Chemical Reagent |
| MMP-9-IN-9 | MMP-9-IN-9, CAS:206549-55-5, MF:C27H33N3O5S, MW:511.64 | Chemical Reagent |
The Critical Role in Systems Pharmacology and Target Site Measurement
Systems pharmacology represents a paradigm shift from traditional, single-target drug discovery to a holistic, network-based approach. This field uses computational and experimental systems biology to understand drug action across multiple scales of biological organization, explaining both therapeutic and adverse effects [18]. A core challenge in this domain is the accurate measurement of neurotransmitters at the target site, which is critical for developing a mechanistic understanding of drug action in the context of an individual's genomic status and environmental exposure [18]. Techniques like in vivo microdialysis are therefore indispensable, providing direct, quantitative insights into neurochemical dynamics in awake, behaving organisms [14].
Core Principles of Systems Pharmacology
Network-Based Drug Action Analysis
Systems pharmacology analyses rely on constructing and interpreting biological networks. In these models:
- Nodes represent entities such as drugs, proteins, genes, or diseases [18].
- Edges represent the connections between them, which can be defined by protein-protein interactions, drug-target binding, or transcriptional regulation [18].
- This framework allows researchers to transcend multiple scales of organization, from atomic-level drug-target interactions to organismal-level phenotypes, thereby avoiding the "black-box" assumptions of older models [18].
The Imperative for Direct Target Site Measurement
The theoretical power of network models must be grounded with empirical data. Direct measurement of neurotransmitter concentrations is crucial because:
- It provides quantitative, temporal data on neurotransmitter release, which is hypothesized to be a strong indicator of a drug's addictive liability and potential for abuse [19].
- It enables the development and validation of kinetic models of drug action, such as those used in neurotransmitter PET (ntPET) analysis, which characterizes the temporal profile of neurotransmitter release [19].
- Integrating these precise measurements with network models allows for the development of predictive models of therapeutic efficacy and adverse event risk [18].
Application Notes: Experimental Protocols for In Vivo Neurotransmitter Measurement
Protocol: Brain Microdialysis in Awake Non-Human Primates
This protocol details a method for comparing concentrations of cortical neurotransmitters between different cognitive states [14].
I. Surgical Implantation and Guide Cannulation
- Implant semi-chronic guide cannulas stereotaxically targeting the brain region of interest (e.g., the visual middle temporal area (MT)).
- Integrate the guides with a standard recording chamber, allowing flexible access to diverse brain regions, including areas deep within the sulcus.
- Ensure all procedures adhere to institutional animal care and use committee guidelines.
II. Microdialysis Probe Insertion and Sampling
- On the experimental day, insert a microdialysis probe through the guide cannula.
- Perfuse the probe with an artificial cerebrospinal fluid (aCSF) solution at a low flow rate (e.g., 1-2 µL/min).
- Collect dialysate samples at defined intervals (e.g., every 10-20 minutes) during distinct behavioral states, such as 'active' (engaged in a cognitive task) and 'inactive' (resting) conditions.
- Maintain a cold chain for samples prior to analysis.
III. Neurochemical Analysis via UPLC-ESI-MS
- Analyze the dialysate samples using Ultra-Performance Liquid Chromatography with Electrospray Ionization-Mass Spectrometry (UPLC-ESI-MS).
- This method allows for the reliable concentration measurement of a broad spectrum of neurotransmitters from small sample volumes (<20 µl).
- Key analytes include: GABA, glutamate, norepinephrine, epinephrine, dopamine, serotonin, and choline [14].
IV. Data Analysis and Interpretation
- Calculate absolute concentrations of neurotransmitters by comparing sample chromatograms to standard curves.
- Compare mean concentration levels between behavioral states using appropriate statistical tests (e.g., t-tests, ANOVA).
- Perform correlation analysis on neurotransmitter concentration changes to investigate the complex interplay between different neurochemical systems [14].
Protocol: Estimating Neurotransmitter Kinetics with ntPET
This protocol describes a neuroimaging approach to estimate the kinetics of stimulus-induced neurotransmitter release in humans [19].
I. PET Scanning Protocol
- Administer a radio-labeled receptor ligand tracer intravenously.
- Conduct two dynamic PET scans on the same subject: one during a resting state (constant neurotransmitter level) and another during an activation state (time-varying neurotransmitter level induced by a pharmacological or cognitive challenge).
- Acquire data over a period sufficient to capture tracer uptake and retention (e.g., 60-90 minutes).
II. Tracer Input Function (TIF) Determination
- Arterial (ART) Method (Gold Standard): Obtain arterial blood samples throughout the scan. Process the samples to measure the concentration of the unmetabolized tracer in plasma to derive the TIF directly [19].
- Reference (REF) Method (Practical Alternative): Derive the TIF from PET data acquired in a reference region that has negligible receptor density. This avoids the need for arterial cannulation [19].
III. Kinetic Modeling with ntPET
- Fit the PET data from both the rest and activation scans simultaneously using the ntPET model.
- The model is an extension of the two-tissue compartment model and includes competition between the tracer and endogenous neurotransmitter for receptor sites.
- Concurrently estimate two sets of parameters:
- ΘTR: Parameters describing the uptake and retention of the tracer.
- ΘNT: Parameters describing the temporal profile (timing and magnitude) of neurotransmitter release in the activation condition [19].
Data Presentation and Quantitative Analysis
The following tables summarize key quantitative findings and methodological comparisons from the featured research.
Table 1: Neurotransmitter Concentration Changes Measured by Microdialysis in Awake Behaving Primates
| Neurotransmitter | Role in Brain Function | Observation in Active vs. Inactive States | Analysis Method |
|---|---|---|---|
| GABA | Primary inhibitory neurotransmitter | Subtle concentration variations observed [14] | UPLC-ESI-MS |
| Glutamate | Primary excitatory neurotransmitter | Subtle concentration variations observed [14] | UPLC-ESI-MS |
| Dopamine | Reward, motivation, motor control | Subtle concentration variations observed [14] | UPLC-ESI-MS |
| Norepinephrine | Arousal, alertness, stress | Subtle concentration variations observed [14] | UPLC-ESI-MS |
| Serotonin | Mood, appetite, sleep | Subtle concentration variations observed [14] | UPLC-ESI-MS |
| Acetylcholine | Learning, memory, attention | Measured via its precursor, Choline [14] | UPLC-ESI-MS |
Table 2: Comparison of ntPET Methodologies for Estimating Neurotransmitter Kinetics
| Feature | ART (Arteral) Method | REF (Reference) Method | |
|---|---|---|---|
| Tracer Input Function (TIF) | Measured from arterial blood samples [19] | Derived from a reference brain region [19] | |
| Invasiveness | High (requires arterial cannulation) [19] | Low (non-invasive) [19] | |
| Cost & Complexity | High (burdensome sample processing) [19] | Low (simplified protocol) [19] | |
| Key Assumption | Plasma radioactivity accurately reflects tracer input | Reference region has negligible receptor density [19] | |
| Robustness to Metabolites | Deteriorates with uncorrected radiometabolites [19] | Not applicable | N/A |
| Robustness to Reference Region Binding | Not applicable | Performance preserved even with 40% receptor density in reference region [19] | N/A |
| Temporal Precision | Better than 3 minutes for early NT peaks [19] | Better than 3 minutes for early NT peaks [19] |
Visualization of Workflows and Signaling
The following diagrams, generated with Graphviz DOT language, illustrate the core experimental and conceptual frameworks.
Microdialysis Workflow
ntPET Kinetic Modeling
Network Pharmacology Paradigm
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Systems Pharmacology and Target Site Measurement
| Tool / Reagent | Function / Application | Example Sources / Databases |
|---|---|---|
| Microdialysis Probes & Guides | Semi-chronic implantation for repeated sampling in awake, behaving subjects [14]. | Custom or commercial systems (e.g., CMA Microdialysis) |
| UPLC-ESI-MS System | High-sensitivity quantification of a broad spectrum of neurotransmitters from small sample volumes [14]. | Waters, Agilent, Sciex |
| Radio-labeled PET Tracers | Molecules that bind to specific neuroreceptors, enabling quantification of receptor availability and NT release via displacement [19]. | Cyclotron-produced isotopes (e.g., 11C, 18F) |
| Drug-Target Databases | Provide curated information on known and predicted interactions between drugs and their protein targets [20]. | DrugBank, ChEMBL, SwissTargetPrediction |
| Protein-Protein Interaction Databases | Supply high-confidence data on physical and functional interactions between proteins for network construction [20]. | STRING, BioGRID, IntAct |
| Pathway Analysis Tools | Identify biological pathways overrepresented in a set of genes or proteins derived from network analysis [20]. | KEGG, Reactome, DAVID, g:Profiler |
| Network Visualization Software | Enable the construction, visualization, and topological analysis of complex drug-target-disease networks [20]. | Cytoscape, Gephi, NetworkX |
| Sofosbuvir D6 | Sofosbuvir D6, MF:C22H29FN3O9P, MW:535.5 g/mol | Chemical Reagent |
| Pasireotide L-aspartate salt | Pasireotide (L-Aspartate Salt) | Pasireotide (L-aspartate salt) is a multireceptor-targeted somatostatin analog for endocrine and oncology research. This product is for research use only (RUO). |
Executing Microdialysis Studies: From Probe Implantation to Advanced Analytics
Microdialysis is an in vivo sampling technique that enables the monitoring of neurotransmitters and other molecules in the interstitial fluid of tissues, particularly the brain [12]. This method is based on the implantation of a probe containing a semi-permeable membrane into the region of interest. The probe is perfused with a solution that closely mimics the ionic composition of the extracellular fluid, allowing substances to diffuse across the membrane based on concentration gradients [13]. The design of the microdialysis probe—encompassing its membrane material, molecular weight cut-off (MWCO), and physical configuration—is paramount to the success of an experiment. These factors collectively determine the efficiency of analyte recovery, the spatial resolution of the sampling, and the degree of tissue response, all of which are critical for generating reliable and interpretable neurochemical data [21] [11].
This application note provides a structured overview of the key considerations for probe design and selection, framed within the context of measuring neurotransmitters in awake, freely moving animals. It is intended to serve as a practical guide for researchers, scientists, and drug development professionals engaged in in vivo research.
Membrane Types and Molecular Weight Cut-Off (MWCO)
The dialysis membrane is the core component of a microdialysis probe, and its characteristics directly govern which molecules are sampled.
Membrane Materials
Membranes are typically fabricated from regenerated cellulose or synthetic polymers, each with distinct properties [22].
- Regenerated Cellulose: These membranes are highly hydrophilic and exhibit low protein adsorption. However, their surface hydroxyl groups can activate the complement system, leading to reduced hemocompatibility [22].
- Synthetic Polymers: This category includes materials such as polysulfone, polyethersulfone, and polyacrylonitrile. Synthetic membranes are characterized by their asymmetric structure, which features a thin inner selective layer and a supportive outer layer. They offer superior biocompatibility, reduced activation of blood components, and greater flexibility in tuning pore sizes and surface characteristics [22].
Molecular Weight Cut-Off (MWCO)
The MWCO is a critical parameter that defines the size-exclusion properties of the membrane. It is most often defined as the lowest molecular weight of a standard globular solute for which the membrane retains greater than 90% of the solute [23] [24]. It is crucial to understand that MWCO is a nominal rating and not an absolute barrier; diffusion of molecules near the specified MWCO will be slower compared to significantly smaller molecules [23].
The following table summarizes the retention characteristics of membranes with different MWCO ratings, demonstrating how retention increases with solute molecular mass.
Table 1: Molecular Weight Cut-Off (MWCO) and Analyte Retention Profiles for Dialysis Membranes
| Nominal MWCO | Analyte Retention Characteristics |
|---|---|
| 2 kDa | Retains >90% of molecules ~2,000 Da and larger; significantly slower dialysis rates for small ions due to thicker membrane and smaller pores [23]. |
| 3.5 kDa | Retains ~90% of a ~3,500 Da globular protein; allows efficient passage of small molecules like salts [23]. |
| 7 kDa | Retains >90% of a ~7,000 Da peptide; suitable for sampling small neurotransmitters while retaining some neuropeptides [23]. |
| 10 kDa | Retains proteins with a molecular mass ≥10,000 Da; a common choice for sampling classic neurotransmitters (e.g., glutamate, GABA, monoamines) [23]. |
| 20 kDa | Retains the majority of large proteins; enables sampling of a broader range of neuropeptides and larger molecules [23]. |
For neurochemical studies, probes with MWCO values ranging from 20,000 to 60,000 Da are commonly employed [21]. This range is optimal for sampling small-molecular-weight neurotransmitters such as monoamines and amino acids while effectively excluding larger macromolecules like proteins. This yields a protein-free sample that typically requires no further cleanup before analysis [13]. When the target analytes are larger, such as neuropeptides, a membrane with a higher MWCO (e.g., 100 kDa) may be necessary, though recovery for these molecules often remains low (below 5%) due to their size [11].
Probe Configurations
The physical design of the microdialysis probe must be matched to the target tissue and the experimental goals. The most common configurations are detailed below.
Table 2: Common Microdialysis Probe Configurations and Their Applications
| Probe Configuration | Physical Description | Typical Applications | Key Considerations |
|---|---|---|---|
| Concentric Cannula | Stainless steel shaft with a short dialysis membrane (1-4 mm) at the tip [21]. | Neuroscience research in specific brain regions of rodents [21]. | Offers high spatial resolution. Outer diameter typically 200-500 μm for rat brain studies [21]. |
| Linear (Side-by-Side) | A dialysis membrane (4-10 mm) bridging two pieces of flexible tubing [21]. | Sampling soft, homogeneous tissues like liver, muscle, heart, and skin [21]. | Larger surface area for sampling; less spatial precision than concentric design [21]. |
| Flexible | Similar to concentric design but uses flexible tubing to minimize vessel damage [21]. | Intravascular sampling from blood vessels [21]. | Can bend with animal movement; analyte recoveries are generally higher from blood [21]. |
| Shunt | Designed to sample from flowing fluids in vivo or in vitro [21]. | Sampling bile in awake animals or desalting protein samples [21]. | Allows continuous sampling from ductal systems. |
Experimental Protocol: Simultaneous Measurement of Neurotransmitters and Neuronal Activity
This protocol details a procedure for integrating microdialysis with local field potential (LFP) recordings to study the effects of amyloid-beta oligomers (Aβo) on hippocampal glutamate and GABA levels and neuronal hyperactivity in rats [25] [26].
Materials and Reagents
Table 3: Research Reagent Solutions for Microdialysis and Neurotransmitter Analysis
| Reagent/Material | Function/Application | Example/Specification |
|---|---|---|
| Amyloid-beta (1-42) | Preparation of amyloid-beta oligomers (Aβo) to model Alzheimer's disease pathology [25]. | Reconstituted according to established protocols to form soluble oligomers [25]. |
| Artificial Cerebrospinal Fluid (aCSF) | Perfusion solution for the microdialysis probe [6]. | Ionic composition similar to extracellular fluid (e.g., 147 mM Na+, 4 mM K+, 2.3 mM Ca2+, 155.6 mM Cl-) [6]. |
| Microdialysis Probe | In vivo sampling device [21]. | Concentric design with a MWCO of 50,000 Da, suitable for sampling glutamate and GABA [6]. |
| LFP Electrode | Recording neuronal activity [25]. | Custom-assembled electrode coupled to the microdialysis cannula [25]. |
| HPLC System with Detector | Quantitative analysis of neurotransmitters in dialysate [6]. | High-performance liquid chromatography with electrochemical detection (HPLC-ECD) [6]. |
| Mass Spectrometry | Highly sensitive and selective analysis of neurotransmitters [11]. | Used as an alternative or complementary method to HPLC for glutamate and GABA quantification [25]. |
Step-by-Step Procedure
- Probe and Electrode Assembly: Assemble a custom complex that integrates a microdialysis cannula with an LFP recording electrode. Ensure the dialysis membrane at the tip and the electrode contacts are properly aligned [25].
- Surgical Implantation: Anesthetize the rat and secure it in a stereotaxic apparatus. Implant the assembly complex into the target hippocampal region using stereotaxic coordinates. Fix the assembly firmly to the skull using dental cement [25] [6].
- Post-operative Recovery: House the animal individually and allow it to recover for 2-3 days after surgery before commencing experiments [6].
- Simultaneous LFP Recording and Microdialysis:
- Connect the implanted probe to a microsyringe pump and perfuse with aCSF at a flow rate of 2.0 μL/min [6].
- Connect the LFP electrode to the recording system.
- Place the rat in a testing cage where it can move freely.
- Collect dialysate samples automatically at set intervals (e.g., every 25 minutes) and inject them directly into the HPLC system [6].
- Record LFP signals continuously throughout the session.
- Baseline and Intervention:
- Collect at least four dialysate samples to establish stable baseline levels of neurotransmitters and LFP activity.
- Administer the intervention (e.g., intracerebral injection of Aβo or systemic drug administration) [25] [6].
- Continue collecting dialysate samples and LFP data for the desired post-intervention period.
- Sample Analysis: Analyze the dialysate samples using HPLC-ECD or LC-MS/MS to quantify concentrations of glutamate, GABA, and other neurotransmitters of interest [25] [6].
- Histological Verification: Upon experiment completion, perfuse the brain with a dye or fixative, remove the brain, and verify the probe and electrode placement histologically [6].
The workflow for this integrated protocol is as follows:
Critical Factors Influencing Probe Performance
Recovery and Flow Rate
Recovery refers to the efficiency with which an analyte is collected from the extracellular fluid into the dialysate. It is a central concept in microdialysis quantification [12].
- Relative Recovery: The concentration of the analyte in the dialysate divided by its concentration in the external medium. It is inversely related to flow rate [12] [11].
- Absolute Recovery: The total mass of an analyte collected per unit of time. It is directly related to flow rate [11].
For high relative recovery of neurotransmitters, lower flow rates (e.g., 0.1 - 1.0 μL/min) are recommended as they allow more time for analyte equilibration across the membrane [11]. However, this results in lower sample volumes, which can challenge analytical detection. A balance must be struck based on the sensitivity of the analytical method.
Tissue Considerations and Limitations
Probe implantation inevitably causes tissue trauma, including inflammation, hemorrhage, and gliosis (the development of a fibrin-like polymer around the probe) [21]. This glial scar can act as a physical barrier, increasing the diffusional distance and adversely affecting recovery over time [21] [11]. To mitigate this:
- Allow a recovery period of ~24 hours after probe implantation before starting experiments to stabilize the initial tissue response [21].
- Consider using smaller, miniaturized probes to reduce tissue damage and improve spatial resolution [11].
- The use of retrodialysis with anti-inflammatory agents (e.g., dexamethasone) has been shown to reduce glial scarring [11].
The careful selection and design of a microdialysis probe are foundational to successful in vivo neurochemical monitoring. The choice of membrane material and its MWCO determines the selectivity of sampling, while the probe configuration must be suited to the anatomical site. Furthermore, critical operational parameters like flow rate directly impact analyte recovery and temporal resolution. By understanding and optimizing these factors—as outlined in this application note—researchers can robustly apply microdialysis to investigate the dynamic changes in neurotransmitters that underlie behavior, disease states, and drug effects.
Surgical Implantation and Guide Cannula Placement in Rodent Brain Regions
This application note provides a detailed protocol for the surgical implantation of guide cannulas into specific brain regions of rodents, a foundational technique for in vivo research methodologies such as microdialysis. Microdialysis is a critical in vivo sampling technique that allows for the measurement of neurotransmitters, metabolites, and drugs in the extracellular fluid of discrete brain regions of awake, freely-moving animals [17]. The successful implementation of this procedure enables researchers to investigate the neurochemical correlates of behavior and the pharmacodynamic profiles of drugs for disorders such as addiction, Parkinson's disease, and depression [17]. This guide details the materials, surgical steps, and post-operative care required for reproducible and minimally invasive cannula implantation.
Experimental Protocols
Pre-Surgical Preparation
- Animals: Adult rodents (mice or rats) are housed under standard conditions with ad libitum access to food and water.
- Anesthesia: Prepare an anesthetic mixture. For mice, one effective protocol uses a mixture of medetomidine hydrochloride (0.3 mg/kg), butorphanol tartrate (5.0 mg/kg), and midazolam (4.0 mg/kg) administered via intraperitoneal (i.p.) injection [27]. Ensure the depth of anesthesia is sufficient by checking for the absence of pedal and corneal reflexes.
- Stereotaxic Instrument Setup: Secure the anesthetized animal in the stereotaxic frame using ear bars and a bite bar. Maintain body temperature using a heated pad. Apply ophthalmic ointment to prevent corneal drying. Shave the scalp and disinfect the surgical site with alternating scrubs of iodine and ethanol [28].
Surgical Implantation Procedure
- Incision and Skull Exposure: Make a midline incision of the scalp (~1.5-2 cm) and retract the skin and underlying fascia to clearly expose the skull [28].
- Skull Preparation and Landmark Identification: Gently scrape the skull surface with a scalpel blade to create an uneven surface, which improves the adhesion of the subsequent dental cement [28]. Identify the cranial landmarks, bregma and lambda, and ensure the skull is level by confirming the dorsoventral (DV) coordinate at both points is equal.
- Stabilizing Screw Placement: Drill two small holes into the skull, away from the cannula implantation site, using an 18-gauge needle or a surgical drill. Anchor miniature steel screws into these holes; they will provide structural support for the dental cement head-cap [27] [28].
- Cannula Targeting and Implantation:
- Calculate the target coordinates for your brain region of interest relative to bregma. For example, for targeting the BNST in mice, coordinates may be: Anteroposterior (AP): +1.6 mm, Mediolateral (ML): -0.5 mm, Dorsoventral (DV): -4.1 mm from the dura [27].
- Raise the guide cannula and drill a burr hole at the calculated AP and ML coordinates.
- Lower the guide cannula slowly to the target DV coordinate. For bilateral injections where cannulas may interfere, they can be implanted at a 60° angle to the vertical axis [27].
- Securing the Cannula: Prepare dental acrylic cement (e.g., GC Unifast II). Mix the powder and liquid to a viscous consistency and apply it around the base of the guide cannula and the stabilizing screws, forming a stable head-cap [27]. Ensure the cement does not obstruct the cannula lumen.
- Wound Closure and Recovery: After the cement has fully hardened, carefully retract the stereotaxic arm. Insert a dummy cannula into the guide cannula to prevent occlusion [27]. Suture the skin around the head-cap if necessary. Administer a reversal agent for the anesthesia (e.g., atipamezole for medetomidine) if applicable, and place the animal in a warmed recovery cage until it is fully ambulatory. Post-operative analgesia (e.g., Meloxicam) should be provided [28].
Post-Operative Care and Drug Infusion
- Handling: Handle guide cannula-implanted mice daily for several days prior to behavioral testing to acclimatize them to the infusion procedure [27].
- Topical Analgesia: To manage post-surgical pain, a local anesthetic cream like EMLA (containing lidocaine and prilocaine) can be applied to the surgical site twice daily until behavioral experiments begin [27].
- Microinfusion Protocol:
- Connect the treatment (internal) cannula to a length of tubing pre-filled with your drug solution or artificial cerebrospinal fluid (aCSF). The cannula is then connected to a microsyringe (e.g., 5-µL Hamilton syringe) mounted on an infusion pump.
- Gently remove the dummy cannula and insert the treatment cannula, which extends 1-2 mm beyond the guide cannula tip.
- Infuse the solution at a slow, controlled rate (e.g., 0.1 µL over 1 minute) [27].
- After the infusion is complete, leave the cannula in place for an additional period (e.g., at least 5 minutes) to allow for diffusion and prevent backflow along the injection track [27].
- Remove the treatment cannula, replace the dummy cannula, and return the animal to its home cage. Behavioral testing can typically begin after a set pre-treatment interval (e.g., 30 minutes).
Key Data and Specifications
Table 1: Exemplary Stereotaxic Coordinates for Guide Cannula Implantation in the Mouse BNST
| Hemisphere | Approach Angle | Anteroposterior (AP) | Mediolateral (ML) | Dorsoventral (DV) | Reference |
|---|---|---|---|---|---|
| Right | Anterior (60°) | +1.6 mm from bregma | -0.5 mm from bregma | -4.1 mm from dura | [27] |
| Left | Posterior (60°) | -3.05 mm from bregma | -0.5 mm from bregma | -4.4 mm from dura | [27] |
Table 2: Anesthesia and Infusion Parameters
| Parameter | Specification | Protocol Reference |
|---|---|---|
| Anesthetic Cocktail | Medetomidine (0.3 mg/kg); Butorphanol (5.0 mg/kg); Midazolam (4.0 mg/kg) | [27] |
| Infusion Volume | 0.1 - 0.125 µL | [27] |
| Infusion Rate | 0.1 µL/min | [27] |
| Post-Infusion Dwell Time | ≥ 5 minutes | [27] |
Workflow and Signaling Visualizations
Surgical Workflow
Diagram Title: Guide Cannula Implantation Workflow
Microdialysis Principle
Diagram Title: Microdialysis Sampling Principle
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item Name & Specification | Function/Application |
|---|---|
| Guide Cannula (e.g., AG-8; 8 mm length, o.d. = 0.5 mm) | Permanent guide surgically implanted to target brain region, allows repeated insertion of injection probe [27]. |
| Dummy Cannula (e.g., AD-8) | Occludes the guide cannula between infusions to prevent contamination and patency loss [27]. |
| Artificial Cerebrospinal Fluid (aCSF) | Physiological buffer used to dissolve drugs/compounds for infusion and as a vehicle control [27]. |
| Dental Acrylic Cement (e.g., GC Unifast II) | Forms a stable, hardened head-cap to secure the guide cannula and screws to the skull [27]. |
| Microsyringe (e.g., 5-µL Hamilton syringe) | Precision syringe used with an infusion pump to deliver nanoliter-to-microliter volumes of solution at a constant rate [27]. |
| Stereotaxic Frame | Apparatus to rigidly hold the animal's head and allow precise 3D navigation for cannula placement based on a brain atlas [27] [28]. |
| Hck-IN-1 | Hck-IN-1, CAS:1473404-51-1, MF:C16H11ClN6O3S, MW:402.81 |
| TMV-IN-10 | 2-Pyridin-3-yl-5-(3,4,5-trimethoxyphenyl)-1,3,4-oxadiazole |
Accurate measurement of neurotransmitter dynamics in the living brain is fundamental to neuroscience research and neuropharmacology. Cerebral microdialysis stands as a versatile in vivo sampling technique that enables the continuous collection of unbound analytes from the extracellular fluid of specific brain regions in awake, freely-moving animals [11] [17]. The core principle of microdialysis involves implanting a probe with a semipermeable membrane into the tissue, perfusing it with a physiological solution, and collecting the dialysate for analysis [9]. However, a complete equilibrium is never achieved due to constant perfusate flow, meaning the analyte concentration in the dialysate is lower than the true extracellular concentration [9]. Consequently, determining a calibration factor, or recovery, is critical for quantifying true extracellular levels [9]. This Application Note details three established calibration methods—No-Net-Flux, Retrodialysis, and Low-Flow-Rate—providing structured protocols and recommendations to ensure robust and reliable data in neurotransmitter research.
Principles of Microdialysis Calibration
Calibration in microdialysis is essential because the concentration of an analyte measured in the dialysate (Cout) is only a fraction of its actual concentration in the extracellular fluid (CECF). The recovery is defined as the ratio Cout/CECF [9]. The selection of an appropriate calibration method depends on the experimental design, the nature of the analyte (endogenous or exogenous), and whether steady-state conditions can be achieved or are required [29] [9]. The three techniques covered herein are based on distinct principles, summarized in Table 1.
Table 1: Comparison of Key Microdialysis Calibration Methods
| Method | Principle | Best For | Key Advantage | Key Limitation |
|---|---|---|---|---|
| No-Net-Flux [9] [30] | Perfusing multiple known analyte concentrations; CECF and recovery are determined from the x-intercept and slope of the (Cout-Cin) vs. Cin plot. | Endogenous compounds (e.g., neurotransmitters) at steady state. | Provides a direct, model-free measure of CECF at steady state. | Requires steady state; time-consuming as multiple concentrations are perfused. |
| Retrodialysis [9] [30] [31] | Using the analyte itself or a similar calibrator; recovery = (Cin - Cout) / Cin. Assumes diffusion is equal in both directions. | Exogenous compounds (e.g., drugs); allows for real-time calibration. | Enables continuous monitoring of recovery during the experiment. | Not suitable for most endogenous compounds; requires a validated calibrator. |
| Low-Flow-Rate [9] | Perfusing with blank solution at varying low flow rates; recovery increases as flow rate decreases. CECF is estimated by extrapolating to zero flow. | Applications where tissue concentration is stable over a long period. | Conceptually simple. | Long calibration times to collect sufficient sample volume at low flows. |
The following diagram illustrates the logical decision process for selecting the most appropriate calibration method based on key experimental parameters.
No-Net-Flux Method
Principle and Workflow
The No-Net-Flux (ZNF) method is a steady-state technique used primarily for quantifying basal levels of endogenous neurotransmitters [9] [30]. The probe is perfused with at least four different concentrations of the analyte of interest (Cin), including zero, and the resulting dialysate concentration (Cout) is measured for each. The difference (Cout - Cin) is plotted against Cin. The x-intercept of the resulting regression line represents the point of no-net-flux, which is the true CECF. The slope of the line corresponds to the relative recovery [9] [30].
Detailed Experimental Protocol
Application: Determining basal extracellular concentration of a neurotransmitter (e.g., Dopamine, Glutamate).
Pre-experimental Considerations:
- Animal Model: Typically performed in rodents (rats or mice). The animal should be awake and freely moving in a cage system designed for microdialysis.
- Probe Implantation: A microdialysis guide cannula is surgically implanted into the brain region of interest (e.g., striatum, prefrontal cortex) under anesthesia. Animals are allowed to recover for 24-48 hours before the experiment to minimize acute tissue damage effects [11].
- Analytical Setup: Ensure the analytical method (e.g., HPLC-ECD, LC-MS/MS) is optimized for the target analyte with established sensitivity and linearity in the expected concentration range [11] [32].
Procedure:
- Prepare Perfusate Solutions: Prepare artificial cerebrospinal fluid (aCSF) containing the analyte (e.g., dopamine) at several known concentrations (e.g., 0 nM, 5 nM, 10 nM, 20 nM). The concentrations should bracket the expected CECF.
- Insert Probe and Establish Basal Flow: Insert the microdialysis probe through the guide cannula and begin perfusing with blank aCSF at a constant flow rate (typically 1.0-2.0 μL/min) using a high-precision syringe pump.
- Equilibration Period: Allow the system to equilibrate for 1-2 hours after probe insertion to establish a stable baseline.
- Sample Collection for ZNF:
- Perfuse the first concentration of analyte (Cin1) for a sufficient period to reach steady state (typically 30-45 minutes).
- Collect 2-3 consecutive dialysate samples under steady-state conditions. The sample volume is determined by the flow rate and collection interval (e.g., 20 μL at 1 μL/min over 20 minutes).
- Immediately analyze each sample or store at -80°C to prevent degradation.
- Repeat steps 4a-4c for each of the remaining perfusate concentrations (Cin2, Cin3, Cin4). The order of concentrations should be randomized to minimize time-dependent effects.
- Data Analysis:
- Calculate the mean Cout for each perfused concentration Cin.
- For each concentration, calculate the net flux: (Cout - Cin).
- Plot net flux (Y-axis) against Cin (X-axis) and perform linear regression.
- The X-intercept (where Y=0) is the estimated CECF.
- The slope of the regression line is the relative recovery.
Retrodialysis Method
Principle and Workflow
Retrodialysis (or reverse dialysis) is a powerful method for calibrating the delivery and sampling of exogenous compounds, such as drugs [30] [31]. It operates on the principle that the diffusion of a molecule across the semipermeable membrane is equal in both directions. The probe is perfused with a known concentration of the drug (or a structurally similar calibrator), and the disappearance of the drug from the perfusate is measured. The recovery is calculated as (Cin - Cout) / Cin [9]. This recovery factor is then used to calculate CECF from Cout during subsequent drug sampling experiments.
Detailed Experimental Protocol
Application: Determining the recovery of an exogenous drug (e.g., Zidovudine, Selinexor) for subsequent pharmacokinetic studies.
Pre-experimental Considerations:
- Calibrator Selection: For "Retrodialysis by Drug," the drug itself is used. For "Retrodialysis by Calibrator," a compound with very similar physicochemical properties (e.g., size, lipophilicity, diffusion coefficient) must be selected and validated in vitro [30].
- Stability and Binding: Assess the drug's stability in the perfusate and its potential for non-specific binding to the tubing and probe components. For hydrophobic drugs, adding agents like bovine serum albumin (BSA) or DMSO to the perfusate may be necessary to minimize binding and improve recovery [29].
Procedure:
- In Vitro Validation (Recommended): Before the in vivo experiment, validate the recovery and calibrator similarity in a beaker containing stirred aCSF (with or without BSA) at 37°C [29]. This confirms the probe's functionality and the calibrator's suitability.
- In Vivo Calibration:
- Prepare the perfusate solution containing a known concentration of the drug or calibrator (Cin).
- Implant the probe and begin perfusion with blank aCSF as in the ZNF protocol. After equilibration, switch the perfusion line to the drug-containing solution.
- Allow the system to equilibrate (e.g., 60 minutes) for the loss of drug to stabilize.
- Collect multiple consecutive dialysate samples (e.g., 3 samples over 60-90 minutes).
- Measure the concentration of the drug/calibrator in the collected dialysate (Cout).
- Switching to Sampling Mode: To begin the actual experiment, switch the perfusate back to blank aCSF. After a washout period, administer the drug systemically (e.g., intraperitoneally or intravenously) and collect dialysate samples to measure Cout of the drug over time.
- Data Analysis:
- Calculate the relative recovery (RR) from the retrodialysis phase: RR = (Cin - Cout) / Cin.
- For each sample collected during the systemic drug experiment, calculate the true extracellular concentration: CECF = Cout / RR.
Low-Flow-Rate Method
Principle and Workflow
The Low-Flow-Rate method leverages the inverse relationship between flow rate and relative recovery [9]. At very low flow rates, the dialysate has more time to equilibrate with the extracellular fluid, increasing recovery. By perfusing the probe with blank solution at several low flow rates and measuring Cout, one can extrapolate the data to a theoretical flow rate of zero, where Cout would equal CECF.
Detailed Experimental Protocol
Application: Estimating CECF when the tissue concentration is stable over an extended period.
Procedure:
- Probe Implantation and Equilibration: Implant the probe and perfuse with blank aCSF at a standard flow rate (e.g., 1.5 μL/min) for 1-2 hours to establish a baseline.
- Sample Collection at Multiple Flow Rates:
- Sequentially perfuse the probe with blank aCSF at a series of decreasing flow rates (e.g., 2.0, 1.0, 0.5, 0.2 μL/min).
- At each flow rate, allow sufficient time for the system to stabilize (this can take 60-90 minutes at the lowest rates).
- Collect multiple dialysate samples once Cout has stabilized at each flow rate.
- Analyze samples to determine Cout at each flow rate (Q).
- Data Analysis:
- Plot Cout (Y-axis) against the flow rate Q (X-axis).
- Fit a non-linear regression curve (e.g., based on an exponential decay model) to the data points.
- Extrapolate the curve to a flow rate of zero. The corresponding Cout value is the estimated CECF.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of microdialysis calibration requires specific, high-quality materials. The following table lists key solutions and components.
Table 2: Key Research Reagent Solutions and Materials
| Item Name | Function/Application | Example & Notes |
|---|---|---|
| Artificial Cerebrospinal Fluid (aCSF) | Standard perfusion medium; mimics ionic composition of brain ECF. | Contains NaCl, KCl, CaCl₂, MgCl₂, NaHCO₃, etc.; pH adjusted to 7.4 [29] [11]. |
| Bovine Serum Albumin (BSA) | Additive to perfusate to reduce non-specific binding of hydrophobic drugs to the system. | Used at 0.5%-1.5% in Ringer's solution to improve recovery of lipophilic compounds [29]. |
| Dimethylsulfoxid (DMSO) | Solvent for dissolving highly lipophilic drugs in the perfusate. | Use at low concentrations (e.g., 0.01%-0.1%) to minimize biological effects [29]. |
| Microdialysis Probes | Core sampling device with a semipermeable membrane. | Various designs (e.g., concentric, linear); membrane MW cut-off (6-100 kDa) must be appropriate for the analyte [11] [9]. |
| High-Precision Syringe Pump | Delivers perfusate at a constant, low flow rate. | Critical for maintaining stable flow rates from 0.1 to 5.0 μL/min [11] [17]. |
| Analyte Standards | For perfusate preparation in ZNF/Retrodialysis and for analytical calibration. | High-purity neurotransmitters or drugs for preparing known Cin solutions [30]. |
| LQZ-7I | LQZ-7I, MF:C20H14F2N4, MW:348.3 g/mol | Chemical Reagent |
| ABMA | ABMA, MF:C18H24BrNO, MW:350.3 g/mol | Chemical Reagent |
The choice of calibration method is a critical determinant of data validity in cerebral microdialysis. The No-Net-Flux method is ideal for directly measuring basal levels of endogenous neurotransmitters under steady-state conditions. Retrodialysis is the method of choice for exogenous drug studies, offering the significant advantage of real-time calibration during an experiment. The Low-Flow-Rate method provides an alternative for estimating CECF when prolonged stable conditions can be met. By following the detailed protocols and considerations outlined in this document, researchers can select and implement the optimal calibration strategy, thereby generating accurate and pharmacologically relevant data on brain neurochemistry for drug development and neuroscience research.
In vivo microdialysis is a cornerstone technique in neuroscience research, enabling the continuous sampling of extracellular fluid from specific brain regions of awake, freely-moving animals [17]. This technique allows researchers to monitor dynamic changes in neurotransmitters, their metabolites, and other small molecules in response to pharmacological interventions or behavioral paradigms [12]. The analytical challenge, however, lies in the minute volumes (typically microliters) and low concentrations (often femtomolar to picomolar) of the collected dialysates, necessitating highly sensitive and selective analytical detection methods [33] [17].
This application note details three advanced analytical coupling strategies—UHPLC-ECD, LC-MS/MS, and chemical derivatization—that provide robust solutions for quantifying neurotransmitters from microdialysis samples. We present standardized protocols, performance metrics, and practical guidance to empower researchers in selecting and implementing the optimal methodology for their specific research questions in drug development and neuropharmacology.
UHPLC with Electrochemical Detection (UHPLC-ECD)
Principles and Applications
Electrochemical detection (ECD) operates on the principle of amperometry, measuring the electrical current generated when electrochemically active substances undergo oxidation or reduction reactions at an electrode surface [34]. ECD is exceptionally suited for analyzing monoamine neurotransmitters and their metabolites, such as dopamine (DA), serotonin (5-HT), 3,4-dihydroxyphenylacetic acid (DOPAC), and 5-hydroxyindoleacetic acid (5-HIAA), which are inherently electroactive [33]. The coupling with UHPLC provides superior separation efficiency with smaller particle size columns, resulting in finer chromatographic peaks, enhanced resolution, and shorter run times compared to conventional HPLC [33].
Performance Data
The following table summarizes typical performance characteristics of UHPLC-ECD for key neurotransmitters:
Table 1: Representative UHPLC-ECD Performance Metrics for Neurotransmitters
| Analyte | Limit of Detection (LOD) | Limit of Quantification (LOQ) | Linear Range (L.R.) | Run Time | Reference |
|---|---|---|---|---|---|
| Serotonin (5-HT) | ~0.5 fmol per sample | ~1.5 fmol per sample | Not Specified | ~12 min | [33] |
| Dopamine (DA) | Femtomolar range | Picomolar range | >7 orders of magnitude* | 5-30 min | [33] [35] |
| Monoamines and Metabolites | Not Specified | Not Specified | Not Specified | ~12 min | [33] |
*The enormous linear dynamic range of ECD, exceeding 7 orders of magnitude (e.g., from 10 pmol/L to 100 µmol/L), is a key advantage, allowing for the quantification of compounds across a wide concentration range with the same instrument [34].
Detailed Protocol: UHPLC-ECD for Monoamines
Workflow Overview:
Step-by-Step Procedure:
Mobile Phase Preparation: Prepare a reversed-phase compatible mobile phase. A common formulation is 50-100 mM sodium phosphate or citrate buffer, pH 3.0-4.0, containing an ion-pairing reagent (e.g., 0.5-1.0 mM octanesulfonic acid), 0.1 mM EDTA, and 5-15% methanol or acetonitrile [33]. Filter through a 0.22 µm membrane and degass thoroughly.
System Calibration: Prepare a series of standard solutions containing known concentrations of target analytes (e.g., DA, 5-HT, DOPAC, HVA, 5-HIAA) in the perfusion fluid (e.g., artificial cerebrospinal fluid). Inject these to establish a calibration curve for each analyte.
Sample Preparation: Thaw microdialysis samples on ice. Centrifuge at high speed (e.g., 10,000 x g for 5-10 minutes) to remove any particulate matter. The sample can often be injected directly without further processing, as microdialysis inherently removes proteins and other macromolecules [17] [12].
UHPLC-ECD Analysis:
- Column: Reverse-phase C18 column (e.g., 100 mm x 2.1 mm, 1.7-1.8 µm particle size).
- Flow Rate: 0.2 - 0.4 mL/min.
- Temperature: Maintain column oven at 30-40°C.
- Injection Volume: 5-20 µL.
- ECD Parameters: Use a glassy carbon working electrode. The applied potential is typically between +0.6 to +0.8 V vs. a reference electrode (e.g., Ag/AgCl), but should be optimized for maximal signal-to-noise for your target analytes [33].
Maintenance: Polish the glassy carbon working electrode weekly with alumina slurry to maintain a reflective surface and ensure reproducibility [33].
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS)
Principles and Applications
LC-MS/MS combines the physical separation capabilities of liquid chromatography with the exceptional mass analysis power of a triple quadrupole mass spectrometer [36]. This technique provides high specificity by isolating a precursor ion in the first quadrupole, fragmenting it in the collision cell, and then monitoring a unique product ion in the third quadrupole [36]. LC-MS/MS is ideal for a broad range of analytes, including non-electroactive neurotransmitters, neuropeptides, and drugs, and is less susceptible to matrix effects from complex samples compared to ECD when proper sample preparation is employed [37] [38].
Performance Data
Table 2: Representative LC-MS/MS Performance Characteristics
| Parameter | Specification | Application Note |
|---|---|---|
| Mass Range | < ~4,000 m/z | [36] |
| Sensitivity | Can detect some compounds below 1 part per trillion | [36] |
| Reproducibility | Excellent when stable labeled internal standards are used | [36] |
| Specificity | High (based on unique mass/charge transitions) | [36] |
Detailed Protocol: LC-MS/MS for Neurotransmitters
Workflow Overview:
Step-by-Step Procedure:
Internal Standard Addition: To each microdialysis sample (e.g., 10-20 µL), add a known amount of stable-isotope labeled internal standard (SIL-IS) for each analyte. The SIL-IS corrects for variability in sample preparation and ion suppression/enhancement during ionization, significantly improving reproducibility [36] [38].
Sample Preparation (Select one method):
- Supported Liquid Extraction (SLE): Load the sample onto an SLE cartridge packed with diatomaceous earth. After absorption, wash with an organic solvent (e.g., methyl tert-butyl ether) to partition analytes. Elute, then evaporate the solvent and reconstitute in a 50:50 methanol:water solution compatible with the LC mobile phase [37] [38].
- Protein Precipitation (PPT): For high-protein matrices, add a precipitating agent (e.g., cold acetonitrile, methanol/ZnSOâ‚„) to the sample. Vortex, centrifuge, and collect the supernatant for injection. This is fast and simple but provides less matrix depletion than SLE [38].
- Dilution: For low-protein matrices like microdialysates, simple dilution with LC-MS grade water or mobile phase may be sufficient ("dilute-and-shoot") [38].
LC-MS/MS Analysis:
- Chromatography: Use a reverse-phase column (e.g., C18, 50-100 mm x 2.1 mm, sub-2 µm). The mobile phase is typically water and methanol or acetonitrile, both modified with 0.1% formic acid or ammonium acetate to facilitate ionization.
- Mass Spectrometry:
- Ionization: Electrospray Ionization (ESI), positive or negative mode.
- Data Acquisition: Multiple Reaction Monitoring (MRM). For each analyte, optimize the MS parameters to define the precursor ion > product ion transition, collision energy, and declustering potential. Example for Dopamine: Precursor ion [M+H]+ m/z 154 → Product ion m/z 137.
Chemical Derivatization Strategies
Principles and Applications
Chemical derivatization involves reacting the target analyte with a chemical reagent to form a new compound (derivative) with more favorable properties [39]. For neurotransmitter analysis, common goals are to:
- Improve Sensitivity: Attach a moiety that enhances ionization efficiency for MS or increases electrochemical activity [39].
- Enable Detection: Allow for the detection of compounds that lack native chromophores, fluorophores, or electroactive groups.
- Enhance Specificity: Distinguish isobaric compounds (same mass) by giving them different fragmentation patterns or retention times [39].
A prominent application is in MALDI imaging mass spectrometry, where derivatization is used to detect endogenous amine metabolites, such as amino acids and neurotransmitters, directly in tissue sections [39].
Detailed Protocol: Derivatization for MALDI Imaging
Workflow Overview:
Step-by-Step Procedure:
Derivatization Solution Preparation: Prepare a solution containing the derivatization reagent, such as 4-hydroxy-3-methoxycinnamaldehyde (CA), mixed with a MALDI matrix (e.g., ferulic acid) in a suitable organic solvent [39].
Tissue Preparation and Derivatization: Cryosection fresh-frozen tissue (e.g., brain) at an appropriate thickness (e.g., 10-20 µm). Thaw-mount the section onto a MALDI target plate. Apply the derivatization/matrix solution uniformly to the tissue surface using a spray coater or other automated deposition system [39].
MALDI Imaging: Place the target into the MALDI mass spectrometer. Acquire data in imaging mode with high mass resolution. The derivatization reaction typically occurs on-target during the application process.
Validation: To unambiguously confirm the identity of the detected metabolites, analyze tissue extracts from adjacent sections using HPLC-MS/MS. This step is critical to distinguish target metabolites from isobaric compounds [39].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Neurotransmitter Analysis
| Item | Function | Application Note |
|---|---|---|
| C18 Reverse-Phase Column | Hydrophobic interaction-based separation of analytes. The workhorse for most monoamine and metabolite separations. | [33] [37] |
| HILIC Column | Separates polar compounds retained via hydrophilic interactions. Ideal for metabolic studies. Incompatible with high-salt ECD buffers. | [33] [37] |
| Glassy Carbon (GC) Electrode | The working electrode for ECD where oxidation/reduction of electroactive analytes occurs. | [33] |
| Stable Isotope-Labeled Internal Standards (SIL-IS) | Added to samples to correct for losses during preparation and matrix effects during ionization, crucial for quantitative LC-MS/MS. | [36] [38] |
| 4-Hydroxy-3-methoxycinnamaldehyde (CA) | A derivatization reagent that reacts with amine groups to enhance sensitivity and specificity for MALDI imaging of neurotransmitters. | [39] |
| Solid Supported Liquid Extraction (SLE) Plates | A medium for efficient liquid-liquid extraction in a 96-well plate format, providing clean-up and concentration of analytes for LC-MS/MS. | [37] [38] |
| Ion-Pairing Reagents (e.g., Octanesulfonic acid) | Added to the mobile phase to facilitate the retention of ionic analytes (like monoamines) on reverse-phase columns. | [33] |
| GNF362 | GNF362, MF:C22H21F3N6, MW:426.4 g/mol | Chemical Reagent |
| Mutant IDH1-IN-4 | Mutant IDH1-IN-4, MF:C25H34N4O3, MW:438.6 g/mol | Chemical Reagent |
The selection of an appropriate analytical coupling strategy is paramount for the success of microdialysis-based research. UHPLC-ECD stands out for its exceptional sensitivity, cost-effectiveness, and simplicity for electroactive monoamines. LC-MS/MS offers unparalleled specificity and versatility for a broader analyte panel, including non-electroactive compounds. Finally, chemical derivatization extends the reach of advanced techniques like MALDI imaging to endogenous amines, enabling spatial localization in tissues. By implementing the detailed protocols and leveraging the performance data provided herein, researchers can robustly quantify neurotransmitters to advance our understanding of brain function and drug effects.
Microdialysis is an established in vivo sampling technique essential for measuring neurotransmitter levels in the brain extracellular fluid of awake, freely-moving animals [17]. Its principle is based on the implantation of a semi-permeable membrane probe into a specific brain region. When perfused with a physiological solution, the probe allows for the continuous collection of molecules from the extracellular space, providing crucial data on neurochemical changes in response to pharmacological treatments or disease states [17] [40]. A powerful extension of this technique is retrodialysis (or reverse dialysis), which leverages the same principles to deliver drugs locally into the brain tissue via the perfusion fluid [17]. This application is particularly valuable for circumventing the blood-brain barrier (BBB), minimizing systemic side effects, and establishing direct causal links between drug concentration at a target site and its pharmacological effect [17] [41]. This Application Note details how retrodialysis is innovatively applied in pharmacokinetic/pharmacodynamic (PK/PD) studies, research on neurodegenerative disease models, and localized drug delivery.
Retrodialysis in PK/PD and Neurodegenerative Disease Research
The following table summarizes the core applications of retrodialysis in contemporary neuroscience research.
Table 1: Core Applications of Retrodialysis in Neuroscience
| Application Area | Key Objectives | Measured Endpoints | Relevant Disease Models |
|---|---|---|---|
| PK/PD Modeling | Elucidate the relationship between local drug concentration (PK) and neurochemical or behavioral response (PD) [17]. | - Unbound drug concentration in brain interstitial fluid [42]- Changes in neurotransmitter release (e.g., dopamine, glutamate) [17]- Altered neuronal activity or behavior. | Used across models, including Parkinson's disease (6-OHDA rats) and Alzheimer's disease (APP/PS1 mice) [42]. |
| Localized Drug Delivery | Overcome the blood-brain barrier to achieve high local drug concentrations and minimize systemic exposure [17] [41]. | - Drug efficacy at the target site- Reduction in off-target effects- Validation of new therapeutic targets. | Essential for testing drugs for Alzheimer's disease, Parkinson's disease, brain tumors, and epilepsy [41]. |
| Disease Modeling & Validation | Understand neurochemical deficits and validate novel therapeutic strategies within specific neural circuits [43] [17]. | - Disease-specific neurotransmitter alterations (e.g., dopamine in PD; acetylcholine in AD) [17]- Rescue of neurochemical and behavioral deficits. | Parkinson's disease (6-OHDA, α-synuclein models), Alzheimer's disease (APP/PS1, Tau models), ALS, and Huntington's disease [43] [42]. |
A critical consideration in CNS PK/PD is the free drug hypothesis, which states that the unbound drug concentration at the target site drives pharmacological activity [42]. Research has revealed that the unbound drug fraction (fu,brain) can be significantly altered in the brains of patients with Alzheimer's disease (AD) or Parkinson's disease (PD) compared to healthy controls [42]. For instance, the unbound fraction of prazosin was found to be 2.5 times higher in AD brain tissue and 2.1 times higher in PD brain tissue [42]. These findings underscore the necessity of using retrodialysis in disease-relevant models to obtain accurate PK/PD data for effective drug development.
Advanced Experimental Protocols
Protocol: Retrodialysis for Local Pharmacokinetics in a Rodent PD Model
This protocol outlines the use of retrodialysis to administer a novel anti-parkinsonian drug and measure its local concentration and neurochemical effects in the striatum of a 6-hydroxydopamine (6-OHDA) lesioned rat model [42].
Research Reagent Solutions
- Therapeutic Agent: Novel D2/D3 dopamine receptor agonist (e.g., 1 mM solution in artificial cerebrospinal fluid (aCSF)).
- Perfusion Fluid: Artificial Cerebrospinal Fluid (aCSF). Function: Physiological solution used to perfuse the microdialysis probe, maintaining ionic homeostasis and serving as the vehicle for drug delivery during retrodialysis [17].
- 6-Hydroxydopamine (6-OHDA): Function: A neurotoxin used to selectively lesion dopaminergic neurons in the medial forebrain bundle, creating a well-established rat model of Parkinson's disease for preclinical research [42].
- Internal Standard for LC-MS/MS: Deuterated analog of the drug candidate. Function: Used in mass spectrometry to account for variability in sample preparation and instrument response, ensuring accurate quantification of the drug candidate [17].
Procedure
- Animal Model Preparation: Anesthetize adult Sprague-Dawley rats and unilaterally lesion the medial forebrain bundle with 8 μg of 6-OHDA neurotoxin. Allow 4 weeks for degeneration of nigrostriatal neurons and validate the lesion using apomorphine-induced rotation tests [42].
- Guide Cannula Implantation: Implant a guide cannula stereotaxically above the striatum on the lesioned side. Allow a 5-7 day recovery and surgical healing period.
- Microdialysis Probe Insertion: On the experimental day, insert a commercially available concentric microdialysis probe (e.g., 4 mm membrane length, 20 kDa MWCO) through the guide cannula, ensuring the membrane is positioned within the striatum.
- Perfusion and Baseline Collection: Perfuse the probe with aCSF at a constant flow rate of 2.0 μL/min using a microinfusion pump. Allow a 2-hour equilibration period, then collect baseline dialysate samples every 20 minutes for one hour [17].
- Retrodialysis (Local Drug Administration): Switch the perfusion solution from aCSF to aCSF containing the 1 mM D2/D3 agonist. Maintain this retrodialysis for a 2-hour period, continuing to collect dialysate samples every 20 minutes.
- Sample Analysis:
- Pharmacokinetics (PK): Analyze 15 μL of each dialysate sample using Liquid Chromatography with tandem mass spectrometry (LC-MS/MS) to determine the unbound concentration of the drug in the striatal extracellular fluid over time [17].
- Pharmacodynamics (PD): Use the remaining dialysate to measure changes in extracellular dopamine, glutamate, and GABA levels via High-Performance Liquid Chromatography with electrochemical detection (HPLC-ECD) [17].
- Data Analysis: Plot the local drug concentration (PK) against the resulting change in neurotransmitter levels (PD) to establish a PK/PD relationship for the drug within the diseased brain tissue.
Protocol: Target Validation in an Alzheimer's Disease Mouse Model using hiPSC-Derived Microglia
This protocol combines retrodialysis with human-induced pluripotent stem cell (hiPSC) technology to validate the role of neuroinflammation in Alzheimer's disease (AD) [44] [17].
Research Reagent Solutions
- hiPSC-Derived Microglia: Generated from AD patients and healthy donors using a specialized differentiation protocol [44]. Function: To provide a human-relevant cell model that recapitulates the innate immune response in the AD brain, complementing animal studies.
- CSF1R Inhibitor: (e.g, PLX5622, 100 μM in aCSF). Function: A selective compound that inhibits the Colony Stimulating Factor 1 Receptor (CSF1R), which is critical for microglial survival and activation, allowing for the investigation of microglial modulation on disease pathology [44].
- Cortical Organoids: 3D structures derived from hiPSCs. Function: To model the complex cellular architecture of the human brain, including neurons, astrocytes, and oligodendrocytes, providing a more physiologically relevant environment for studying cell-cell interactions in AD [44].
Procedure
- hiPSC Differentiation: Differentiate hiPSCs from AD patients (e.g., carrying PSEN1 mutations) and isogenic controls into microglia and cortical organoids using established protocols [44].
- Tri-culture Setup: Incorporate the AD or control hiPSC-derived microglia into the corresponding cortical organoids to establish a 3D tri-culture system that models the neuroinflammatory environment of the AD brain [44].
- In Vivo Microdialysis in APP/PS1 Mice: Perform guide cannula implantation and microdialysis in the hippocampus of an APP/PS1 transgenic mouse model of AD amyloidosis [42].
- Baseline Neurotransmitter Sampling: Collect baseline dialysate samples from the hippocampus while perfusing with aCSF. Analyze for glutamate and GABA levels as indicators of synaptic function, and for inflammatory cytokines.
- Retrodialysis of CSF1R Inhibitor: Switch the perfusion fluid to aCSF containing the 100 μM CSF1R inhibitor. Administer via retrodialysis for 4 hours to locally suppress microglial activity in the mouse hippocampus.
- Post-Treatment Sampling: Continue to collect dialysate samples for 2 hours after the retrodialysis period ends.
- Ex Vivo Analysis: At the endpoint, collect brain tissue for immunohistochemical analysis of amyloid-β plaque burden and microglial activation (e.g., IBA1 and CD68 staining).
- Data Integration: Correlate the local suppression of microglial activity (confirmed by histology) with changes in neuroinflammatory markers in the dialysate and synaptic function to validate CSF1R as a therapeutic target for AD.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Research Reagents for Retrodialysis Experiments
| Reagent / Material | Function & Application |
|---|---|
| Artificial Cerebrospinal Fluid (aCSF) | Standard perfusion fluid for microdialysis; serves as the vehicle for drug delivery during retrodialysis, maintaining ionic and osmotic balance [17]. |
| hiPSC-Derived Neural Cells | Patient-specific neurons (e.g., dopaminergic, cortical), astrocytes, and microglia for creating human-relevant disease models and testing compound effects in vitro and in organoids [44]. |
| LC-MS/MS & HPLC-ECD | Analytical techniques for quantifying drug concentrations (LC-MS/MS) and neurotransmitter levels (HPLC-ECD) in microdialysate samples with high sensitivity and specificity [17]. |
| Selective Neurotoxins | 6-Hydroxydopamine (6-OHDA) for creating Parkinson's disease models; used to validate the neurochemical basis of behavioral deficits [42]. |
| Small Molecule Inhibitors/Agonists | Pharmacological tools (e.g., CSF1R inhibitors, receptor agonists) delivered via retrodialysis for target validation and mechanism of action studies [44] [17]. |
| SLM6031434 | SLM6031434, MF:C22H30F3N5O2, MW:453.5 g/mol |
| Tetromycin C5 | Tetromycin C5, MF:C50H65NO13, MW:888.0 g/mol |
Workflow and Signaling Pathways
Retrodialysis Experimental Workflow
The following diagram illustrates the integrated workflow of a retrodialysis experiment, from in vivo sampling to data analysis.
Neuroinflammatory Signaling in Alzheimer's Disease
This diagram outlines a key signaling pathway relevant to neurodegenerative disease research, which can be modulated using retrodialysis.
Optimizing Recovery and Data Quality: A Troubleshooting Guide
In the realm of in vivo neuroscience research and drug development, microdialysis stands as a pivotal technique for monitoring extracellular concentrations of neurotransmitters, neuromodulators, and drugs directly in the brains of conscious animals [29] [45]. The core principle of microdialysis involves implanting a semi-permeable membrane probe into brain tissue, perfusing it with an artificial cerebrospinal fluid (aCSF), and collecting the dialysate for analysis [46]. The reliability of data obtained through this method hinges critically on recovery—the efficiency with which molecules cross the dialysis membrane from the extracellular fluid into the perfusate [46]. This Application Note details the fundamental relationship between recovery and key experimental parameters—flow rate, membrane length, and diffusion—providing structured protocols and data to optimize microdialysis experiments for accurate neurotransmitter measurement.
Theoretical Principles: The Mathematics of Recovery
The recovery of a substance by a microdialysis probe is primarily governed by its diffusion properties. The extraction fraction (Ed) is a key calibration parameter, defined as the ratio of the analyte's concentration in the dialysate (Coutlet) to its true concentration in the extracellular fluid (C∞ECF), when the perfusate inlet concentration (Cinlet) is zero [46]. This relationship is formalized as:
Ed = (Coutlet - Cinlet) / (C∞ECF - Cinlet) [46]
When Cinlet = 0, this simplifies to Ed = Coutlet / C∞ECF, meaning the dialysate concentration is a direct percentage of the actual extracellular concentration [46]. The value of Ed is not a fixed probe characteristic but is dynamically influenced by the perfusate flow rate, the membrane's surface area and material, the physicochemical properties of the analyte, and the diffusion characteristics of the surrounding tissue [46].
The Critical Interplay of Parameters
The following diagram illustrates the logical relationships and combined effects of flow rate, membrane length, and diffusion on the ultimate goal of achieving high-fidelity data in microdialysis.
Quantitative Data and Comparative Analysis
Table 1: The influence of key experimental parameters on microdialysis recovery and application.
| Parameter | Impact on Relative Recovery (%) | Impact on Absolute Recovery (Mass) | Temporal Resolution | Spatial Resolution | Primary Application Context |
|---|---|---|---|---|---|
| Flow Rate | Inversely proportional. Highest recovery at ultra-slow flows (e.g., 0.1-0.5 µL/min) [46]. | Directly proportional. Higher flows (e.g., 1-2 µL/min) yield more total analyte per unit time [32]. | Higher flow rates enable better resolution (e.g., seconds with 2-3 nL droplets) [32]. | Indirectly affected via probe size. | Balancing accurate concentration estimation (low flow) with detectability and temporal resolution (high flow). |
| Membrane Length | Directly proportional. A longer membrane provides a greater surface area for diffusion, increasing Ed [46]. | Directly proportional. More analyte is collected with a longer membrane. | Unaffected. | Inversely proportional. Longer membranes sample from a larger, less specific brain volume. | Targeting specific small nuclei vs. measuring from larger brain regions. |
| Analyte Properties | Diffusion coefficient-dependent. Small, hydrophilic molecules have higher recovery than large, hydrophobic ones prone to Non-Specific Binding (NSB) [29]. | Similarly affected by NSB, which reduces the absolute amount of analyte recovered. | Can be affected if NSB causes carry-over between samples. | Unaffected. | Dictates requirements for probe material, surface coatings, and perfusate composition (e.g., adding BSA) [29]. |
Illustrative Experimental Data
Table 2: Example experimental data demonstrating the relationship between flow rate, membrane length, and relative recovery.
| Flow Rate (µL/min) | Membrane Length (mm) | Analyte | Approximate Relative Recovery (Ed) (%) | Notes | Source Context |
|---|---|---|---|---|---|
| 0.5 | 1-4 | Dopamine, Acetylcholine, etc. | ~10-20% | Used for baseline monitoring of neurotransmitters with good temporal resolution (minutes) [32] [45]. | In vivo rodent studies |
| 1.0 | 1-4 | Dopamine, Acetylcholine, etc. | ~5-15% | A standard, balanced flow rate for general use [46]. | In vivo rodent studies |
| 2.0 | 1-4 | Dopamine, Acetylcholine, etc. | <10% | Yields higher absolute mass for low-concentration analytes but poorer relative recovery [46]. | In vivo rodent studies |
| 0.1 (Ultra-slow) | 1-4 | Dopamine, Acetylcholine, etc. | Can approach >50% | "Zero/ultra-slow flow rate method" used to maximize recovery, albeit with small sample volumes [46]. | Calibration methods |
| 1.0 | 1 | Small Molecules | Lower | Shorter membrane, lower recovery, higher spatial precision. | Principle [46] |
| 1.0 | 4 | Small Molecules | Higher | Longer membrane, higher recovery, lower spatial precision. | Principle [46] |
Essential Protocols
Protocol 1: Determining Optimal Flow Rate and Recovery
Objective: To establish the relationship between flow rate and relative recovery for a specific analyte and probe configuration in vitro.
Materials:
- Microdialysis system (pump, probe, fraction collector)
- Target analyte standard
- Artificial Cerebrospinal Fluid (aCSF)
- Stirred bath or vial maintained at 37°C
- Analytical instrument (e.g., LC-MS/MS, HPLC-EC)
Method:
- Setup: Immerse the microdialysis probe in a vigorously stirred solution of a known analyte concentration (e.g., 100 ng/mL) in aCSF at 37°C [29] [46].
- Perfusion: Perfuse the probe with blank aCSF at a series of flow rates (e.g., 0.2, 0.5, 1.0, 1.5, and 2.0 µL/min). Allow 30-60 minutes for equilibration at each new flow rate.
- Collection: Collect at least three dialysate samples at each flow rate.
- Analysis: Quantify the analyte concentration (Coutlet) in each dialysate sample.
- Calculation: Calculate the relative recovery (Ed) at each flow rate using the formula: Ed = (Coutlet / Cexternal) × 100%, where Cexternal is the known concentration in the external bath [46].
- Decision: Plot Ed against flow rate to visualize the inverse relationship. The optimal flow rate is a balance between a sufficiently high Ed and an acceptable collection time for your analytical sensitivity.
Protocol 2: In Vivo Retrodialysis for Calibration
Objective: To determine the in vivo recovery of a probe after implantation, which accounts for the resistance to diffusion posed by the tissue.
Materials:
- Animal with implanted microdialysis probe.
- Isotopic or structural analog of the analyte of interest ("internal standard").
- aCSF.
Method:
- Post-Implantation: After surgical implantation of the probe and a suitable recovery period (e.g., 24 hours), connect the awake, freely moving animal to the system.
- Perfusion with Standard: Perfuse the probe with a solution containing a known concentration of the calibrator (Cperfusate).
- Collection: Collect dialysate samples.
- Analysis: Measure the concentration of the calibrator in the dialysate (Cdialysate).
- Calculation: Calculate the in vivo recovery via retrodialysis: Ed = (Cperfusate - Cdialysate) / Cperfusate [46] [45]. This value estimates the loss of the calibrator from the probe, which is assumed to be equal to the recovery of the native analyte from the brain into the probe.
- Application: Use this calculated Ed to estimate the true extracellular concentration: CECF = Cdialysate / Ed, where Cdialysate is the concentration of the endogenous analyte measured in subsequent experiments.
The workflow for this critical calibration protocol is outlined below.
Protocol 3: Mitigating Non-Specific Binding (NSB) for Hydrophobic Compounds
Objective: To minimize the loss of hydrophobic drugs (e.g., Actinomycin D, Selinexor, Ulixertinib) to the microdialysis apparatus, thereby improving recovery and reducing carry-over [29].
Materials:
- Fluorinated ethylene propylene (FEP) or polyetheretherketone (PEEK) tubing.
- Surface-coated probes or additives like Bovine Serum Albumin (BSA).
- Glass sample vials.
Method:
- Material Selection: Use FEP or PEEK tubing instead of standard materials, as they demonstrate lower protein binding and adsorption [29].
- Surface Coating: Pre-treat the microdialysis system (syringes, tubing, probes) with a solution containing a carrier protein like BSA (0.5%-1.5%) to saturate binding sites [29].
- Perfusate Modification: Add BSA (e.g., 0.5%-1.5%) or a minimal percentage of an organic solvent like DMSO (e.g., 0.01%-0.1%) to the perfusate (aCSF) to enhance the solubility of hydrophobic compounds and reduce their interaction with the system [29].
- Container Choice: Collect dialysate in low-bind polypropylene or glass vials to prevent post-collection analyte loss [29].
- Validation: Perform a "nominal concentration test" by pumping a solution of known drug concentration through the entire system and measuring the output. A recovery close to 100% indicates successful NSB mitigation [29].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential materials and reagents for microdialysis experiments focusing on recovery optimization.
| Item | Function & Rationale | Example Usage & Notes |
|---|---|---|
| Artificial Cerebrospinal Fluid (aCSF) | The physiological perfusate that mimics the ionic composition of brain ECF, minimizing tissue disturbance during perfusion. | Standard solution for most in vivo experiments. Composition is critical for maintaining tissue health. |
| Bovine Serum Albumin (BSA) | A carrier protein added to the perfusate (0.5%-1.5%) to saturate non-specific binding sites on the microdialysis apparatus, crucial for recovering hydrophobic compounds [29]. | Used in recovery experiments for lipophilic drugs like Selinexor and Ulixertinib to significantly improve apparent recovery [29]. |
| Dimethylsulfoxid (DMSO) | A small percentage (0.01%-0.1%) can be added to aCSF to increase the solubility of highly hydrophobic drugs, reducing their adhesion to system components [29]. | Use at the lowest effective concentration to avoid physiological effects on the brain tissue. |
| Internal Standard for Retrodialysis | An isotopic label or structural analog of the target analyte. Its loss from the perfusate (retrodialysis) is used to calculate the in vivo recovery of the native analyte [46]. | Critical for quantitative microdialysis, as it accounts for animal-to-animal and tissue-specific variations in recovery. |
| Low-Bind Tubes (Glass, Polypropylene) | Sample collection vials with surfaces that minimize adsorption of the analyte, ensuring accurate post-collection analysis, especially for peptides and hydrophobic molecules [29]. | Always use for storing dialysate samples prior to analysis. |
| FEP/PEEK Tubing | Tubing materials with low binding properties for biomolecules, reducing analyte loss between the probe and the collection vial [29]. | Preferable over standard plastic tubing for critical applications, especially with novel or hydrophobic compounds. |
| GRK6-IN-3 | GRK6-IN-3, MF:C17H20N4O2, MW:312.37 g/mol | Chemical Reagent |
| TH1834 | TH1834, MF:C33H40N6O3, MW:568.7 g/mol | Chemical Reagent |
Mastering the dynamics of recovery is not merely a technical exercise but a fundamental requirement for generating pharmacologically and physiologically relevant data from microdialysis experiments. As demonstrated, there is no single "perfect" setting; the choice of flow rate, membrane length, and strategies to manage diffusion and NSB must be deliberately tailored to the specific research question, whether it demands high temporal resolution, absolute quantitative accuracy, or the successful measurement of challenging hydrophobic drug candidates. By applying the principles, protocols, and practical recommendations outlined in this document, researchers can significantly enhance the validity and impact of their in vivo neurochemical research and drug development efforts.
The accurate measurement of neurotransmitters and xenobiotics in vivo is a cornerstone of modern pharmacological and neuroscience research. However, the integrity of this data is critically threatened by a pervasive yet often overlooked technical issue: the non-specific adsorption of lipophilic compounds to the polymeric tubing and components of dynamic systems like microdialysis setups. This adsorption is governed by a molecule's lipophilicity, often quantified by its partition coefficient (LogP); compounds with higher LogP values are more hydrophobic and exhibit a greater propensity to bind irreversibly to system surfaces [29]. This phenomenon leads to substantial analyte loss, low recovery rates, and significant carry-over effects, which in turn distort pharmacokinetic data, compromise calculated parameters like the unbound plasma-to-brain partition coefficient (Kp,uu), and ultimately jeopardize the validity of scientific conclusions [47] [29]. This Application Note delineates the scope of this adsorption problem, presents a systematic experimental framework for its quantification, and provides evidence-based strategies for its mitigation, specifically within the context of microdialysis techniques for in vivo neurotransmitter research.
The Adsorption Phenomenon: Mechanisms and Impact
Non-specific binding (NSB) occurs when lipophilic molecules interact with and adhere to the surfaces of materials they contact, such as perfusion tubing, probe membranes, and collection vials. This process is not merely a surface-level interaction; for certain materials, it involves bulk absorption, where molecules diffuse into the polymer matrix itself [48]. This is particularly problematic for polydimethylsiloxane (PDMS), a material valued for its oxygen permeability and flexibility in organ-on-chip and microfluidic devices. PDMS acts as a "sponge" for lipophilic compounds, leading to their substantial depletion from perfusion media and their subsequent slow, uncontrolled release, which can cause cross-contamination between experimental runs [48].
The impact of this adsorption is twofold. First, it directly reduces the measured concentration of the analyte, leading to an underestimation of its true level in the extracellular fluid. Second, the retained analyte can leach out in subsequent experiments, creating a background signal that obscures accurate measurement [29] [48]. The extent of adsorption is not uniform; it is highly specific to each material-substrate combination [47]. Furthermore, the deposition of proteins on the inner surfaces of the tubing over time can alter these interactions in unpredictable ways, adding another layer of complexity to the problem [47].
Quantitative Material Comparison: Sorption Profiles
The choice of tubing material is perhaps the most critical factor in managing adsorption. The following table summarizes the performance of common materials when exposed to compounds of varying lipophilicity, based on empirical data.
Table 1: Tubing Material Sorption Profiles for Lipophilic Compounds
| Material | Key Characteristics | Sorption Behavior | Recommended Applications |
|---|---|---|---|
| Silicone / PDMS | Highly flexible, gas permeable, biocompatible. | Very high sorption and bulk absorption of lipophilic molecules. Slow release leads to carry-over. | Avoid for lipophilic compounds. Suitable for gases or hydrophilic molecules. |
| Polyvinyl Chloride (PVC) | Flexible, common in medical tubing. | High adsorption for a wide range of drugs; capacity is substrate-specific [47]. | Use with caution. Pre-conditioning with proteinaceous solutions may help. |
| Polyethylene (PE) | Semi-flexible, low protein binding. | Very low lipid loss; superior performance for lipid-soluble compounds like oleic acid [49]. | Highly recommended for perfusing lipids and lipophilic compounds. |
| Fluorinated Polymers (FEP, Teflon) | Chemically inert, rigid. | Minimal adsorption; considered the most inert material [47] [29]. | Ideal for chemically diverse or highly lipophilic compounds. Rigidity can limit use. |
| Cyclic Olefin Copolymer (COC) | Rigid, excellent optical clarity, chemical stability. | Significantly lower sorption than PDMS; primarily surface adsorption with easier washout [48]. | Excellent alternative to PDMS in microfluidics and analytical systems for lipophilic drugs. |
The data clearly establishes that material lipophilicity is a primary driver of sorption. For instance, in static incubation studies, the highly lipophilic drug imipramine (LogP = 4.80) showed near-total loss (0.0384 µM recovered from 100 µM) in PDMS devices, while recovery was significantly higher (31.5 µM) in COC devices [48]. Similarly, loperamide (LogP = 5.13) exhibited profound sorption in PDMS systems [48].
Beyond the material itself, the surface-to-volume ratio is a critical parameter. In microfluidic systems with small channel diameters, the contact surface area is large relative to the fluid volume, dramatically amplifying the impact of wall adsorption or absorption [48]. This makes material selection even more crucial in microdialysis and organ-on-chip applications compared to macroscopic systems.
Experimental Protocols for Assessing Adsorption
Before embarking on critical in vivo experiments, it is essential to characterize the adsorption profile of your target compound to the selected system. The following protocols provide a framework for this assessment.
Protocol: Nominal Concentration Test for System Recovery
This test evaluates total analyte loss across the entire experimental setup, including vials, tubing, and probes [29].
- Preparation: Prepare a solution of your test compound at a known concentration (e.g., 100 ng/mL) in the perfusate (e.g., Ringer's solution with 0.5-1.5% BSA).
- Transfer and Collection: Transfer this solution through the complete microdialysis system, including the probe, mimicking the intended flow rate (e.g., 0.5 µL/min).
- Control Samples: Simultaneously, deposit the same solution directly into the collection vials (e.g., polypropylene, plastic microdialysis tubes, glass).
- Analysis: Quantify the analyte concentration in the collected samples and the control samples using UPLC-MS/MS.
- Calculation: Calculate the percent recovery for each condition using the formula:
- Recovery (%) = (Ccollected / Ccontrol) × 100 A recovery significantly below 100% indicates substantial non-specific binding.
Protocol: Tubing and Retention Test
This protocol isolates and quantifies adsorption specifically to the tubing material [29].
- Setup: Connect a 1-meter length of the tubing to be tested (e.g., FEP or PEEK) to a glass syringe filled with the drug solution.
- Sample Collection: Perfuse the solution at the operational flow rate. Collect samples at the tubing outlet at multiple time points (e.g., T1=1h, T2=2h, T3=3h).
- Syringe Control: Also collect samples directly from the syringe before (S1) and after (S2) perfusion.
- Washout Phase: Clean the syringe, refill with a clean perfusate (without drug), and perfuse through the same tubing. Collect samples (T4-T6) to check for analyte desorption.
- Analysis and Calculation:
- Calculate initial recovery: Recovery (%) = (CTn / CS1) × 100
- Calculate carry-over: Carry-over = C_Tn (from washout phase)
Data Interpretation and Decision Framework
The data gathered from these protocols can be interpreted using the following workflow to guide material and method selection.
Diagram 1: A decision tree for diagnosing and addressing adsorption issues based on experimental results.
Strategies for Mitigation and Best Practices
Based on the characterized adsorption profiles, researchers can deploy several effective mitigation strategies.
- Material Substitution: The most effective strategy is to replace high-sorption materials like silicone and PVC with inert alternatives. Fluorinated polymers (FEP), polyethylene (PE), and cyclic olefin copolymer (COC) are superior choices that minimize analyte loss [48] [49] [47].
- Surface Coating and Additives: Pre-saturating the binding sites can reduce analyte loss. This is achieved by:
- System Passivation and Washout: For systems where inert materials are not feasible, a rigorous cleaning and washout protocol with an appropriate solvent (e.g., ethanol, acetonitrile) is essential to prevent carry-over from one experiment to the next [48].
- Comprehensive Calibration: Employ a robust calibration method that accounts for probe-specific recovery in the experimental matrix. Retrodialysis (or reverse dialysis), where the probe is perfused with a known concentration of the analyte and the loss is measured, is a widely used technique to determine in vivo recovery [29] [17].
Table 2: The Scientist's Toolkit: Essential Reagents and Materials for Minimizing Adsorption
| Item | Function & Rationale | Example Usage & Notes |
|---|---|---|
| Polyethylene (PE) Tubing | Low binding material for lipophilic compounds. | Use for perfusion lines; optimal for lipid-soluble compounds like oleic acid [49]. |
| Fluorinated Ethylene Propylene (FEP) Tubing | Chemically inert tubing with minimal non-specific binding. | Ideal as connection tubing between the probe and collection vial for hydrophobic drugs [29]. |
| Cyclic Olefin Copolymer (COC) Devices | Rigid microfluidic material with low small molecule sorption. | Use for microfluidic chips or organ-on-chip devices to ensure accurate drug concentration dosing [48]. |
| Bovine Serum Albumin (BSA) | Carrier protein that blocks adsorption sites on surfaces. | Add at 0.5-1.5% to Ringer's perfusate to saturate binding sites and improve recovery [29]. |
| Dimethyl Sulfoxide (DMSO) | Organic co-solvent to enhance solubility of hydrophobic analytes. | Use at low concentrations (e.g., 0.01-0.1%) to keep compounds in solution and reduce surface binding [29]. |
| UPLC-MS/MS System | Highly sensitive analytical instrument for quantifying low analyte concentrations. | Essential for accurately measuring the low concentrations recovered from in vivo microdialysis samples [29] [5]. |
The adsorption of lipophilic compounds to tubing materials is a significant, yet manageable, challenge in microdialysis and other dynamic in vitro and in vivo systems. A systematic approach—beginning with the characterization of the compound's adsorption profile using the outlined protocols, followed by the strategic selection of inert materials like COC, FEP, or PE, and the judicious use of additives like BSA—is fundamental to obtaining reliable and reproducible neurochemical data. By proactively addressing this issue, researchers can enhance the accuracy of their measurements of neurotransmitters and xenobiotics, thereby strengthening the foundation of pharmacological and neuroscientific discovery.
In vivo microdialysis is a minimally-invasive sampling technique that enables continuous measurement of unbound analyte concentrations in the extracellular fluid of virtually any tissue [9]. The core principle involves implanting a probe with a semipermeable membrane into the tissue of interest, then perfusing it with an aqueous solution that closely resembles the ionic composition of the surrounding tissue fluid [9] [11]. The composition of this perfusate is critically important for obtaining physiologically relevant data, as it directly influences the biochemical environment and recovery of analytes across the membrane. An optimal perfusate must maintain tissue viability, prevent fluid exchange-induced perturbations, and facilitate accurate measurement of neurotransmitters, drugs, and metabolites [50] [51].
The most fundamental perfusate for brain microdialysis is artificial cerebrospinal fluid (aCSF), which mimics the ionic composition of native CSF to minimize osmotic stress and cellular damage during perfusion [50]. Beyond base aCSF formulation, researchers incorporate specific additives to address experimental challenges. Bovine serum albumin (BSA) serves as a critical additive for preventing analyte adhesion to tubing and membranes, particularly for lipophilic compounds [52]. The strategic formulation of perfusate with aCSF and additives like BSA represents a cornerstone technique for valid in vivo neurochemical measurement.
Physiological Basis for Perfusate Design
Cerebrospinal Fluid Composition and Function
Cerebrospinal fluid is a meticulously regulated extracellular fluid that bathes the brain and spinal cord, providing mechanical protection, nutrient delivery, and waste clearance [53]. In adults, total CSF volume measures approximately 150 ml, with daily production ranging from 400 to 600 ml, resulting in complete renewal 4-5 times daily [53]. This continuous turnover maintains a stable neuronal environment despite fluctuations in blood composition.
Normal CSF exhibits distinct ionic characteristics compared to plasma, with higher concentrations of sodium, chloride, and magnesium but lower concentrations of potassium and calcium [53]. The protein content is markedly lower than in plasma, with normal protein concentration ranging from 15 to 45 mg/dL [53]. This minimal protein content reduces nonspecific binding but presents challenges for recovering lipophilic molecules during microdialysis.
Table 1: Physiological Cerebrospinal Fluid Composition
| Parameter | Normal Range | Function |
|---|---|---|
| Sodium | ~140 mEq/L | Maintains osmotic pressure and neuronal excitability |
| Chloride | ~120 mEq/L | Maintains electroneutrality and fluid balance |
| Potassium | ~2.8 mEq/L | Regulates resting membrane potential |
| Calcium | ~2.3 mEq/L | Modulates neurotransmitter release and neuronal signaling |
| Glucose | 50-80 mg/dL | Primary energy substrate for neural tissue |
| Protein | 15-45 mg/dL | Minimal content reduces nonspecific binding |
| pH | 7.31-7.34 | Maintains optimal enzyme function and neuronal activity |
The brain's glymphatic system, first described in 2012, represents a crucial waste-clearance pathway that depends on CSF flow [53]. This system comprises perivascular spaces where CSF enters the brain along arterial vessels, exchanges with interstitial fluid, and exits along venous pathways, facilitating clearance of metabolic waste products like β-amyloid and tau proteins [53]. Glymphatic activity peaks during non-rapid eye movement sleep, highlighting the dynamic nature of brain fluid exchange [53].
Theoretical Principles of Analyte Recovery
Microdialysis operates on the principle of passive diffusion across a semipermeable membrane driven by concentration gradients [11] [9]. Analyte recovery is defined as the ratio of analyte concentration in the dialysate to that in the extracellular fluid, influenced by membrane properties, flow rates, and tissue characteristics [11] [9].
Two primary recovery metrics guide experimental design:
- Relative recovery: The ratio of analyte concentration in dialysate to that in extracellular fluid [11]
- Absolute recovery: The total mass of analyte collected over time [11]
Flow rate critically impacts recovery characteristics. Lower flow rates (<1 μL/min) increase relative recovery by allowing more time for equilibration but decrease absolute recovery, while higher flow rates increase absolute recovery but reduce relative recovery due to limited equilibration time [11]. This inverse relationship necessitates careful optimization based on experimental goals, whether prioritizing concentration accuracy (favoring low flow) or mass detection (favoring higher flow).
Standard aCSF Formulations and Optimization
Basic aCSF Composition
Artificial cerebrospinal fluid formulations aim to replicate the ionic milieu of native CSF while maintaining tissue viability during microdialysis procedures. The standard aCSF composition used in cerebral microdialysis typically includes [50]:
- 145 mmol/L NaCl - Primary osmolarity component
- 2.7-4.0 mmol/L KCl - Maintains neuronal membrane potential
- 1.2-3.0 mmol/L CaClâ‚‚ - Essential for neurotransmitter release
- 0.85-1.5 mmol/L MgClâ‚‚ - Modulates neuronal excitability
This basic formulation preserves physiological ion gradients and prevents cellular swelling or shrinkage during perfusion. The specific concentration ranges accommodate methodological variations while maintaining core physiological principles. Some protocols incorporate bicarbonate buffer systems (22-27 mmol/L NaHCO₃) when maintaining physiological pH under carbonation conditions is necessary [11].
Table 2: Standard aCSF Formulations for Microdialysis
| Component | Concentration Range | Physiological Role | Considerations |
|---|---|---|---|
| NaCl | 145-147 mM | Primary osmolyte maintaining 290-310 mOsm/L | Adjust based on target osmolarity |
| KCl | 2.7-4.0 mM | Neuronal resting potential | Elevated levels may increase baseline neurotransmitters |
| CaClâ‚‚ | 1.2-3.0 mM | Synaptic vesicle fusion and release | Critical for evoked neurotransmitter release studies |
| MgClâ‚‚ | 0.85-1.5 mM | NMDA receptor modulation | Higher concentrations may suppress excitatory transmission |
| NaHâ‚‚POâ‚„/Naâ‚‚HPOâ‚„ | 1.0-2.0 mM | pH buffering capacity | Concentration depends on buffer system selection |
| NaHCO₃ | 22-27 mM | Physiological pH buffer | Requires carbonation with 95% O₂/5% CO₂ |
Osmotic Considerations and Additives
Osmotic balance represents a critical factor in perfusate design, as significant deviations from physiological osmolarity (290-310 mOsm/L) can induce cellular swelling or shrinkage, altering neurotransmitter release and reuptake mechanisms [51]. Research demonstrates that the molecular weight cutoff of microdialysis membranes significantly influences fluid dynamics, with 100-kDa membranes exhibiting substantial fluid loss compared to 20-kDa membranes due to enhanced convective flow [51].
Beyond base ions, researchers incorporate specialized additives to address specific experimental needs:
- Antioxidants (ascorbic acid, uric acid): Protect oxidizable neurotransmitters like dopamine
- Antimicrobial agents (gentamicin, azide): Prevent microbial growth in prolonged experiments
- Enzyme inhibitors (pargyline): Block metabolic degradation of target analytes
- BSA (0.5%-4% w/v): Prevents adsorption of lipophilic compounds to surfaces
The selection and concentration of additives must balance experimental requirements with potential physiological perturbations, as even minor compositional changes can influence neuronal function and analyte recovery.
Bovine Serum Albumin as a Critical Perfusate Additive
Mechanisms of Action
Bovine serum albumin serves as a multifunctional additive in microdialysis perfusate, primarily addressing the challenge of surface adsorption. The hydrophobic binding pockets of BSA molecule sequester lipophilic compounds, preventing their loss to polymeric surfaces of tubing and membranes [52]. This mechanism is particularly crucial for highly lipophilic drugs and neurotransmitters with limited aqueous solubility.
Experimental evidence demonstrates BSA's efficacy in improving recovery. In studies of FLZ, a lipophilic anti-Parkinson's agent, researchers used BSA-containing Ringer's solution (4% w/v) to maintain consistent recovery and prevent drug adsorption [52]. Similarly, protein-bound drugs exhibit enhanced recovery when perfusate contains BSA at physiologically relevant concentrations, as the protein more accurately mimics the binding environment of extracellular fluid.
Practical Implementation Guidelines
The effective use of BSA in microdialysis perfusate requires attention to several technical considerations:
Concentration Optimization: BSA is typically used at 0.5-4% (w/v) in aCSF or Ringer's solution [52]. Lower concentrations may suffice for moderately lipophilic compounds, while highly adhesive molecules require higher concentrations (2-4%).
Solution Preparation: BSA should be dissolved gently in aCSF using a magnetic stirrer to prevent foaming and protein denaturation. The solution should be freshly prepared or aliquoted and stored at -20°C to prevent microbial contamination.
Sterilization: BSA-containing solutions require filtration through 0.2μm membranes rather than autoclaving, as heat denaturation alters binding characteristics.
Compatibility Assessment: Researchers should verify that BSA does not interfere with analytical detection methods, particularly when using mass spectrometry or electrochemical detection.
Physiological Relevance: While BSA improves recovery, its concentration should be considered when interpreting unbound fraction data, as it may influence free drug concentrations through binding interactions.
Experimental Protocols and Methodologies
Preparation of BSA-Enriched aCSF Perfusate
Materials Required:
- Ultra-pure water (Milli-Q or equivalent)
- ACSF-grade salts (NaCl, KCl, CaClâ‚‚, MgClâ‚‚)
- Pharmaceutical-grade BSA (Fraction V, ≥96% purity)
- 0.2μm sterile syringe filters
- pH meter and calibration standards
- Osmometer for verification
Step-by-Step Protocol:
Prepare Base aCSF Solution:
- Dissolve 7.25g NaCl, 0.21g KCl, 0.28g CaClâ‚‚, and 0.10g MgClâ‚‚ in 900mL ultra-pure water
- Add appropriate buffer salts (e.g., 1.0g NaH₂PO₄ and 2.0g NaHCO₃ if using bicarbonate buffer)
- Adjust pH to 7.3-7.4 using NaOH or HCl as needed
- Adjust final volume to 1000mL and verify osmolarity (290-310 mOsm/L)
Incorporate BSA Additive:
- Slowly add 4.0g BSA to 100mL base aCSF while gently stirring at 4°C
- Continue stirring until complete dissolution (approximately 30-60 minutes)
- Avoid vortexing or vigorous shaking to prevent protein foaming
Sterilization and Storage:
- Filter the BSA-aCSF solution through 0.2μm membrane filter under low pressure
- Aliquot into sterile vials for single-use application
- Store at -20°C for up to 30 days or at 4°C for immediate use (within 24 hours)
Quality Control Measures:
- Verify post-preparation pH and adjust if necessary
- Confirm absence of particulate matter before loading into syringe pump
- Perform recovery validation with standard analytes before experimental use
Recovery Calibration Methods
Accurate quantification requires calibration to determine relative recovery, which can be performed using several established methods:
No-Net-Flux Method:
- Perfuse probe with at least four different concentrations of analyte of interest
- Measure steady-state concentrations leaving probe (Cout)
- Plot Cout-Cin versus Cin - x-intercept represents true extracellular concentration [9]
- Provides robust quantification under steady-state conditions
Retrodialysis Method:
- Perfuse probe with analyte-containing solution or structural analog
- Monitor disappearance of drug from probe during perfusion
- Calculate recovery as (Cin-Cout)/Cin [9]
- Particularly suitable for exogenous compounds in clinical settings
Low-Flow-Rate Method:
- Perfuse probe with blank aCSF at progressively decreasing flow rates
- Plot extraction ratios against corresponding flow rates
- Extrapolate to zero-flow to determine extracellular concentration [9]
- Useful for minimizing calibration time while maintaining accuracy
Table 3: Recovery Calibration Methods Comparison
| Method | Principles | Best Applications | Limitations |
|---|---|---|---|
| No-Net-Flux | Multiple perfusate concentrations to find equilibrium point | Endogenous compounds under steady-state conditions | Time-consuming; requires multiple concentration preparations |
| Retrodialysis | Uses analyte disappearance rate to calculate recovery | Exogenous compounds; clinical microdialysis studies | Not suitable for endogenous compounds without analog |
| Low-Flow-Rate | Extrapolates recovery from flow rate relationships | Rapid screening; minimal sample volume availability | Limited by long calibration times at very low flow rates |
| Dynamic No-Net-Flux | Combines data from multiple subjects at single concentration | Studies of drug effects on endogenous compounds | Requires multiple subjects/animals for complete dataset |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Microdialysis Studies
| Reagent Category | Specific Examples | Function | Usage Considerations |
|---|---|---|---|
| Base aCSF Salts | NaCl, KCl, CaClâ‚‚, MgClâ‚‚ | Replicate ionic CSF environment | Use highest purity (>99.9%) to minimize contaminant introduction |
| Buffer Systems | NaH₂PO₄/Na₂HPO₄, NaHCO₃ | Maintain physiological pH (7.3-7.4) | Bicarbonate requires carbonation with 95% O₂/5% CO₂ |
| Protein Additives | Bovine Serum Albumin (Fraction V) | Prevent adsorption of lipophilic compounds | Use 0.5-4% w/v; filter sterilize without heating |
| Antioxidants | Ascorbic acid (0.1-0.3 mM) | Protect oxidizable neurotransmitters | Particularly crucial for monoamines like dopamine and serotonin |
| Antimicrobial Agents | Gentamicin (0.1 mg/mL) | Prevent bacterial growth in prolonged experiments | Verify no interference with analytical detection methods |
| Enzyme Inhibitors | Pargyline (MAO inhibitor) | Prevent metabolic degradation of amines | Concentration-dependent effects require careful optimization |
| Calibration Standards | Target analytes or structural analogs | Determine relative recovery in situ | Use pharmaceutical-grade standards for accurate quantification |
Application Notes and Troubleshooting
Practical Implementation Considerations
Successful implementation of aCSF with BSA additives requires attention to several practical aspects:
Flow Rate Optimization:
- Typical flow rates: 0.1-5.0 μL/min for brain microdialysis [9]
- Lower flow rates (0.1-1.0 μL/min): Maximize relative recovery for concentration determination
- Higher flow rates (1.0-5.0 μL/min): Increase absolute recovery for low-concentration analytes
- Balance temporal resolution with recovery efficiency based on experimental goals
Membrane Selection Criteria:
- Molecular weight cutoff: 6-100 kDa, typically 20 kDa for neurotransmitters [9]
- Membrane material: Polycarbonate, polysulfone, or CMA designs
- Probe configuration: Concentric, linear, or side-by-side designs for specific applications
- Surface area: Balance between recovery efficiency and tissue disruption
Temporal Resolution Strategies:
- Sample collection intervals typically 5-10 minutes [11]
- Online analysis systems enable sub-minute resolution for rapid processes
- Segmented flow techniques with microfluidic partitioning achieve <15 second resolution [11]
- Balance analytical sensitivity with desired time resolution
Troubleshooting Common Challenges
Poor Analytic Recovery:
- Potential Cause: Surface adsorption or inappropriate flow rate
- Solution: Increase BSA concentration (up to 4%) or decrease flow rate
- Verification: Perform in vitro recovery assessment before in vivo application
Inconsistent Baseline Measurements:
- Potential Cause: Temperature fluctuations or improper pH regulation
- Solution: Maintain perfusate at 37°C and verify pH stability
- Verification: Monitor control analyte with known recovery characteristics
Tissue Response and Inflammation:
- Potential Cause: Probe implantation trauma or osmotic imbalance
- Solution: Incorporate anti-inflammatory agents (e.g., dexamethasone) in perfusate [11]
- Verification: Assess glial markers in subsequent histological analysis
Analytical Interference:
- Potential Cause: BSA or additives interfering with detection methods
- Solution: Modify BSA concentration or switch detection methodology
- Verification: Perform spike-recovery experiments with analytical standards
The strategic formulation of microdialysis perfusate with physiological aCSF and BSA additives represents an essential methodology for valid in vivo neurochemical measurement. By maintaining tissue viability while optimizing analyte recovery, researchers can obtain physiologically relevant data on neurotransmitter dynamics, drug pharmacokinetics, and metabolic processes in the living brain.
This document provides detailed protocols and evidence-based recommendations for mitigating three pervasive technical challenges in in vivo microdialysis for neurotransmitter research: probe backpressure, tissue response to implantation, and analyte sample degradation. The guidance is framed within the context of preclinical research aimed at quantifying dynamic changes in neurotransmitters and is designed to ensure the collection of pharmacologically relevant, high-fidelity data for researchers and drug development professionals.
In vivo microdialysis is a powerful technique for monitoring the unbound concentration of neurotransmitters, drugs, and metabolites in the extracellular fluid of living tissue. The core principle involves implanting a probe with a semi-permeable membrane into the target brain region [12] [54]. A perfusate, isotonic to the extracellular fluid, is pumped through the probe, allowing molecules to diffuse passively across the membrane driven by concentration gradients [29] [15]. The resulting dialysate is collected for analysis.
However, the technique is susceptible to technical artifacts that can compromise data validity. This application note addresses the mitigation of three key challenges:
- Backpressure: Elevated pressure within the system can cause perfusate leakage into the surrounding tissue, altering local physiology and analyte concentration [54].
- Tissue Response: The implantation of a microdialysis probe, a foreign body larger than local blood vessels, causes a penetration injury, triggering ischemia, gliosis, and a progressive loss of neurochemical activity around the probe [55].
- Sample Degradation: Collected analytes, especially labile neurotransmitters or hydrophobic drugs, can degrade or be lost due to adsorption before analysis [29].
The following sections provide targeted protocols and solutions to these challenges.
Challenge 1: Backpressure
Background
Backpressure develops from resistance within the microdialysis system, primarily due to long, narrow outlet tubing and the membrane itself [54]. If the pressure becomes too high, it can force perfusate out through the membrane into the brain tissue. This "leaking" increases intracranial pressure, dilutes the local concentration of analytes, and significantly reduces recovery rates, leading to artificially low measured concentrations [54].
Experimental Protocol: Assessing and Managing Backpressure
Objective: To determine the maximum acceptable outlet tubing length for a specific probe and flow rate without causing perfusate leakage.
Materials:
- Microdialysis probe (e.g., AtmosLM vented probe or equivalent [54])
- Microsyringe pump capable of low flow rates (e.g., 0.1 - 2.0 µL/min)
- Various lengths of outlet tubing
- A small beaker of purified water
- Dissecting microscope
Method:
- Connect the inlet of the probe to the syringe pump via standard inlet tubing, filled with purified water.
- Connect a short length (e.g., 5 cm) of outlet tubing to the probe outlet.
- Immerse the probe tip in the beaker of water and initiate flow at a typical experimental rate (e.g., 1.0 µL/min).
- Observe the probe tip under the dissecting microscope. A small, stable droplet should form at the tip of the outlet tubing. The presence of this droplet indicates a properly functioning, non-leaking probe.
- Gradually increase the length of the outlet tubing in increments (e.g., 10 cm), observing the droplet at the tip after each change.
- Critical Step: If the droplet at the tubing tip disappears, it indicates that backpressure has built up to a point where fluid is now leaking across the membrane instead of exiting through the outlet. The previous tubing length is the maximum usable length for this probe and flow rate.
- Document the maximum acceptable outlet tubing length for your standard setup.
Recommended Solution: Push-Pull System with Vented Probes To eliminate backpressure fundamentally, a push-pull pump system with a vented probe is recommended [54].
- Setup: Use two pumps—one to push perfusate through the inlet and a second to pull dialysate from the outlet.
- Probe: A specially designed vented probe (e.g., AtmosLM) incorporates a vent to the atmosphere between the membrane and the outlet line, which equalizes pressure and prevents any build-up from being transmitted to the membrane [54].
- Outcome: This setup completely decouples the inlet flow from outlet resistance, eliminating the risk of perfusate leakage and ensuring that recovery rates are not artificially suppressed by backpressure.
The workflow for managing backpressure is summarized in the diagram below.
Challenge 2: Tissue Response
Background
Implanting a microdialysis probe causes immediate tissue trauma, damaging blood vessels and cellular structures [55]. This penetration injury initiates a cascade of events: ischemia (restricted blood flow), activation of glial cells (astrocytes and microglia), and ultimately, a progressive loss of neuronal function and neurotransmitter activity around the probe [55]. This compromises the physiological relevance of the collected data, as the sampled environment does not represent healthy brain tissue.
Experimental Protocol: Pharmacological Mitigation of Penetration Injury
Objective: To assess the efficacy of compounds in mitigating tissue damage and preserving neurochemical function following probe implantation, using voltammetry next to a microdialysis probe.
Materials:
- Laboratory rat, anesthetized and prepared for stereotaxic surgery.
- Concentric-style microdialysis probe (e.g., 300 μm diameter, 4 mm membrane [55]).
- Carbon fiber microelectrode for Fast-Scan Cyclic Voltammetry (FSCV).
- Stimulating electrode for the medial forebrain bundle (MFB).
- Syringe pump for retrodialysis.
- Protective compounds: e.g., Dexamethasone (DEX, 7.6 μM in aCSF) or XJB-5-131 (10 μM in aCSF with 1% DMSO) [55].
- Artificial Cerebrospinal Fluid (aCSF) control.
Method:
- Pre-Probe Baseline: Insert the voltammetric electrode into the striatum and the stimulating electrode into the MFB. Record electrically evoked dopamine release via FSCV following MFB stimulation. Repeat to establish a stable, pre-implantation baseline [55].
- Probe Implantation & Drug Retrodialysis: Implant the microdialysis probe in the same coronal plane, approximately 70-100 μm from the microelectrode [55]. Immediately begin perfusing the probe with either:
- Group 1: aCSF (control)
- Group 2: DEX in aCSF
- Group 3: XJB-5-131 in aCSF with 1% DMSO
- Post-Implantation Measurement: Two hours after probe implantation, record evoked dopamine release again using the voltammetric electrode ("voltammetry next to the microdialysis probe") [55].
- Data Analysis: Compare the post-implantation dopamine response between groups. A significantly higher response in DEX or XJB groups compared to the aCSF control indicates successful mitigation of penetration injury.
- Validation: Following in vivo measurements, brain tissue containing the probe track can be examined using immunohistochemistry with markers for ischemia, neuronal nuclei (Neu-N), and dopamine axons (tyrosine hydroxylase, TH) to visually confirm the protective effects [55].
Key Findings from Literature:
- Dexamethasone: An anti-inflammatory glucocorticoid, shown to diminish ischemia, gliosis, and the loss of evoked dopamine activity near the probe [55].
- XJB-5-131: A mitochondrially-targeted reactive oxygen species (ROS) scavenger, shown to be particularly effective in protecting dopamine terminals, which are highly sensitive to oxidative stress [55].
The experimental workflow and key findings are illustrated below.
Challenge 3: Sample Degradation
Background
Sample degradation and loss can occur via two primary mechanisms: chemical instability (e.g., oxidation or enzymatic breakdown) and non-specific binding (NSB) to the surfaces of the collection vials and tubing [29]. This is a pronounced challenge for hydrophobic compounds, which have a high propensity for NSB, leading to low recovery rates and substantial carry-over effects that distort concentration measurements [29].
Experimental Protocol: Evaluating and Preventing Non-Specific Binding
Objective: To identify the extent of NSB for a given analyte and to determine the optimal collection vial material and perfusate additives to minimize analyte loss.
Materials:
- Stock solution of the target analyte (e.g., a hydrophobic drug).
- Perfusate solutions: Ringer's solution or aCSF, with and without additives like Bovine Serum Albumin (BSA, 0.5-1.5%) or low concentrations of organic solvents (e.g., 0.01-0.1% DMSO) [29].
- Different collection vials: Polypropylene, plastic microdialysis tubes, and glass vials [29].
- UPLC-MS/MS system for sensitive quantification.
Method: Part A: Vial Selection Test
- Prepare a solution with a known, precise concentration of your analyte in the chosen perfusate.
- Transfer equal aliquots of this solution into the different types of vials (polypropylene, plastic, glass).
- Let the samples stand for a duration that mimics the experimental collection time.
- Quantify the analyte concentration in each vial using UPLC-MS/MS.
- Calculate the percent recovery for each vial type: (Measured Concentration / Nominal Concentration) * 100%.
- Interpretation: The vial material with a recovery closest to 100% demonstrates the least NSB and should be selected for experiments.
Part B: Perfusate Additive Test
- Prepare perfusate solutions containing different potential blocking agents (e.g., 0.5% BSA, 1.0% BSA, 1.5% BSA, 0.1% DMSO).
- Repeat the Vial Selection Test (Steps 1-5) using the optimal vial material from Part A and each of the modified perfusates.
- Interpretation: The condition yielding the highest recovery rate indicates the most effective formulation for preventing NSB for your specific analyte.
Key Recommendations:
- Surface Coating: Pre-treat the microdialysis system with a solution containing a blocking agent like BSA. BSA acts as a blocking agent by preventing non-specific adsorption of peptides and proteins to the probe and tubing surfaces [54].
- Material Selection: Use surface-modified tubing materials (e.g., fluorinated ethylene propylene, FEP) that exhibit lower binding affinity for hydrophobic molecules [29].
- Stability Conditions: Keep collected samples chilled and analyze them immediately if possible. For certain analytes, protect samples from light and store at -80°C if analysis is not immediate [29].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key materials and their specific functions in addressing the technical challenges discussed in this note.
Table 1: Essential Research Reagents and Materials for Microdialysis
| Item | Function/Application in Mitigation | Key Consideration |
|---|---|---|
| Vented Microdialysis Probe (e.g., AtmosLM) | Prevents backpressure build-up by incorporating a vent to atmosphere [54]. | Essential for push-pull systems to eliminate leakage risk. |
| Push-Pull Pump System | Uses separate pumps for inlet (push) and outlet (pull) to eliminate system backpressure [54]. | Requires a compatible vented probe. |
| Dexamethasone | Potent anti-inflammatory retrodialyzed to suppress gliosis and preserve neurochemical activity post-implantation [55]. | Typical concentration: 7.6 µM in aCSF [55]. |
| XJB-5-131 | Mitochondrially-targeted reactive oxygen species (ROS) scavenger; mitigates oxidative stress from penetration injury [55]. | Requires dissolution in aCSF with 1% DMSO [55]. |
| Bovine Serum Albumin (BSA) | Added to perfusate (0.5-1.5%) to block non-specific binding sites on tubing and probes, crucial for hydrophobic compounds [29]. | Also serves as an osmotic agent for large-pore membranes [54]. |
| Low-Binding Collection Vials (e.g., Glass, specific polymers) | Minimizes analyte loss via adsorption after sample collection [29]. | Material should be validated for each specific analyte. |
| Fluorinated Ethylene Propylene (FEP) Tubing | Tubing material with lower propensity for non-specific binding of hydrophobic analytes compared to other plastics [29]. | Use in the outlet line to minimize analyte loss post-probe. |
The following tables consolidate quantitative data from the cited literature and protocols to guide experimental design.
Table 2: Pharmacological Mitigation of Tissue Damage - Key Experimental Parameters and Outcomes [55]
| Parameter / Finding | Dexamethasone (DEX) Group | XJB-5-131 (XJB) Group | Control (aCSF) Group |
|---|---|---|---|
| Perfusion Concentration | 7.6 µM in aCSF | 10 µM in aCSF + 1% DMSO | aCSF alone |
| Key Mechanism of Action | Anti-inflammatory | Mitochondrial ROS Scavenging | N/A |
| Impact on Evoked DA Release | Diminished loss | Diminished loss | Significant loss |
| Histological Outcome | Diminished ischemia, gliosis, and loss of DA axons/terminals | Diminished ischemia, gliosis, and loss of DA axons/terminals | Pronounced tissue damage |
Table 3: Impact of Perfusate Additives on Recovery of Challenging Analytes [29]
| Analyte Property | Technical Challenge | Recommended Mitigation Strategy | Documented Effect |
|---|---|---|---|
| Hydrophobicity (e.g., Actinomycin D, Selinexor) | Pronounced non-specific binding (NSB) to system components; low recovery [29]. | Perfusate addition of BSA (0.5-1.5%) and/or low-concentration DMSO (0.01-0.1%) [29]. | Significantly reduced NSB and increased relative recovery rates [29]. |
| Lipophilicity (e.g., Endocannabinoids AEA, 2-AG) | Low in vivo recovery due to membrane interactions and hydrophobicity [56]. | Optimization of perfusate with LC-MS compatible additives to stabilize analytes [56]. | Enabled successful measurement of extracellular levels in amygdala [56]. |
Microdialysis is a powerful technique for monitoring neurotransmitter dynamics and drug distribution in the living brain, providing critical insights into neurochemical processes and pharmacokinetics in preclinical research. However, the successful application of in vivo microdialysis hinges on rigorous in vitro pre-testing to validate methods, optimize recovery, and prevent experimental artifacts. This document outlines essential in vitro protocols and considerations to ensure the generation of reliable, reproducible, and quantitatively accurate data from in vivo microdialysis studies, with a specific focus on neurotransmitter measurement.
The core principle of microdialysis involves implanting a probe with a semi-permeable membrane into the tissue of interest, which is then perfused with a solution that mimics extracellular fluid [29] [57]. The unbound fraction of analytes diffuses across the membrane into the dialysate, which is collected for analysis. A critical challenge is that the concentration in the dialysate (Cd) is only a fraction of the true extracellular concentration (CECF), and this fraction—the recovery—must be accurately determined through calibration [57]. This process is complicated by factors such as non-specific binding, probe design, and the physicochemical properties of the target analytes [29].
The Critical Role of In Vitro Pre-Testing
Comprehensive in vitro characterization is a prerequisite for any meaningful in vivo microdialysis experiment. It directly addresses several key challenges.
Defining Recovery and its Importance
Recovery is the efficiency with which an analyte crosses the microdialysis membrane and is collected in the dialysate. Quantitative microdialysis requires precise knowledge of recovery to calculate true extracellular concentrations from dialysate measurements [57]. The fundamental relationship is expressed as CECF = Cd / Recovery.
Overcoming Drug-Specific and Method-Related Challenges
Hydrophobic compounds, including many central nervous system (CNS) drugs, are particularly prone to non-specific binding (NSB) to the surfaces of the microdialysis apparatus (e.g., tubing, membrane, collection vials) [29]. This binding leads to low recovery rates, substantial carry-over effects, and an underestimation of true concentrations. In vitro testing is indispensable for identifying and mitigating these issues.
Essential In Vitro Characterization Protocols
The following protocols form the core of a robust in vitro pre-testing strategy.
Protocol 1: Determination of Relative Recovery
This protocol establishes the baseline performance of your microdialysis system for a specific analyte.
3.1.1 Materials
- Microdialysis pump and fraction collector
- Microdialysis probe
- Artificial Cerebrospinal Fluid (aCSF)
- Standard solution of the target analyte
- Analytical instrument for quantification (e.g., UPLC-MS/MS)
3.1.2 Methodology
- Immerse the microdialysis probe in a stirred solution of aCSF containing a known concentration of your analyte (Cmedium).
- Perfuse the probe with blank aCSF at a physiological flow rate (e.g., 0.5 - 2.0 µL/min).
- After an equilibration period, collect dialysate fractions.
- Quantify the analyte concentration in the dialysate (Cd).
- Calculate relative recovery as: Recovery = (Cd / Cmedium) × 100% [29].
Protocol 2: Assessing and Mitigating Non-Specific Binding
This protocol quantifies analyte loss due to adsorption to system components [29].
3.2.1 Materials
- Microdialysis tubing (e.g., FEP, PEEK)
- Syringes
- Collection vials (e.g., polypropylene, glass)
3.2.2 Methodology
- Prepare a solution with a known concentration of the analyte.
- Transfer the solution through the entire fluid path: syringe → tubing → collection vial.
- Measure the final concentration after each transfer step using a highly sensitive analytical technique.
- Calculate recovery at each stage: Recovery = (Cmeasured / Cnominal) × 100%.
- Mitigation Strategies: If significant loss is observed, employ strategies such as:
- Surface Coating: Using tubing and membranes coated with inert materials.
- Additives: Adding carriers like bovine serum albumin (BSA, 0.5-1.5%) or low concentrations of organic solvents (e.g., 0.01-0.1% DMSO) to the perfusate to compete for binding sites [29].
- Material Selection: Using glass injection syringes and low-binding polymer tubing.
Protocol 3: Probe Calibration via Retrodialysis
This method is a key in vitro calibration technique that can also be applied in vivo.
3.3.1 Principle The probe is perfused with a known concentration of the analyte (Cperfusate), and the disappearance of the analyte across the membrane (due to diffusion into the surrounding medium) is measured. The relative loss is used to calculate the delivery recovery (EED), which is assumed to be equal to the relative recovery during sampling [57].
3.3.2 Methodology
- Immerse the probe in a stirred blank aCSF solution.
- Perfuse the probe with a solution containing a known concentration of the analyte or a very similar internal standard.
- Collect dialysate fractions and measure the analyte concentration (Cdialysate).
- Calculate recovery by delivery: EED = (Cperfusate - Cdialysate) / Cperfusate [29] [57].
Table 1: Comparison of Key In Vitro Calibration Methods
| Calibration Method | Key Principle | Advantages | Key Limitations |
|---|---|---|---|
| Relative Recovery (Dialysis) [29] | Probe in analyte solution; measures gain in dialysate. | Simple; no animals needed. | Does not account for in vivo mass transfer resistance. |
| Retrodialysis [29] [57] | Probe perfused with analyte; measures loss to medium. | Accounts for some mass transfer; uses the actual drug. | Cannot be performed simultaneously with in vivo sampling. |
| Retrodialysis with Internal Standard [57] | Uses an analog compound during in vivo sampling. | Allows for continuous, simultaneous in vivo calibration. | Requires a standard with near-identical properties to the analyte. |
Experimental Workflow and Data Interpretation
The relationship between in vitro pre-testing and the final in vivo experiment can be visualized as a logical, sequential workflow.
From In Vitro Data to In Vivo Application
A critical consideration is that recovery determined in a beaker (in vitro) is often higher than the actual recovery in tissue (in vivo) [57]. This difference arises because transport through the tortuous extracellular space of tissue, not just the membrane, can be the rate-limiting step. Therefore, while in vitro recovery provides a crucial performance baseline and allows for system optimization, the absolute value should not be directly applied to in vivo data without further validation (e.g., via in vivo retrodialysis).
Troubleshooting and Material Selection
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the appropriate materials is fundamental to experimental success.
Table 2: Essential Materials for Microdialysis Experiments
| Item | Function / Purpose | Key Considerations & Examples |
|---|---|---|
| Perfusate | Mimics ionic composition of extracellular fluid to minimize osmotic shock. | Artificial Cerebrospinal Fluid (aCSF) or Ringer's solution [29] [58]. |
| Binding Mitigators | Reduce non-specific binding of hydrophobic analytes to the system. | Bovine Serum Albumin (BSA, 0.5-1.5%) [29]; Pluronic F-127 [59]; low-concentration DMSO (0.01-0.1%) [29]. |
| Probe Membrane | The semi-permeable interface for molecular diffusion. | Material (e.g., Polyacrylonitrile, Cuprophan, Polyethersulfone) and Molecular Weight Cut-Off (MWCO, e.g., 6-20 kDa) must be selected for the target analyte [58] [15]. |
| Tubing Material | Conduit for perfusate/dialysate. | Material choice affects binding. Fluorinated Ethylene Propylene (FEP) and Polyetheretherketone (PEEK) are common; test for NSB [29]. |
| Analytical Instrumentation | Quantifies low analyte concentrations in small-volume dialysate. | Requires high sensitivity. Common techniques: UPLC-MS/MS [29], LC-MS [59], GC-FID [58]. |
Advanced Calibration Methods
For complex experiments, more sophisticated calibration methods may be required.
Table 3: Advanced In Vivo Applicable Calibration Methods
| Method | Calculation | Application Context |
|---|---|---|
| No-Net-Flux (NNF) | Finds CECF at x-intercept of (Cin - Cout) vs. Cin plot. | Gold standard for steady-state conditions; time-consuming [57]. |
| Dynamic No-Net-Flux | Modification of NNF for changing concentrations. | Less time-consuming than NNF; requires fewer samples [29]. |
| Retrodialysis by Drug | Recovery (EED) = (Cperfusate - Cdialysate) / Cperfusate | Performed before/after in vivo experiment with the actual drug [29] [57]. |
In vitro pre-testing is not an optional preliminary step but a critical, integral component of rigorous in vivo microdialysis research. By systematically characterizing probe recovery, quantifying and mitigating non-specific binding, and validating calibration approaches, researchers can avoid costly in vivo failures and generate pharmacokinetic and neurochemical data that are both reliable and reproducible. The protocols and guidelines provided here offer a concrete framework for strengthening experimental design, ultimately accelerating drug development and enhancing our understanding of brain function and dysfunction.
Validating Microdialysis Data and Comparative Analysis with Other Techniques
{#topic} {.graf .graf--h3 .graf--leading .graf--title}
Benchmarking Against Tradition: Comparisons with Equilibrium Dialysis and Push-Pull Cannulas
Application Notes & Protocols
The accurate measurement of neurotransmitter dynamics in the living brain is a cornerstone of neuroscience and neuropharmacology. For in vivo research, two perfusion-based sampling techniques have been historically pivotal: the traditional push-pull cannula method and the more contemporary cerebral microdialysis. This application note provides a structured comparison of these two techniques, framing them within a modern research context. We detail experimental protocols, provide quantitative comparisons of key performance data, and list essential research reagents to guide scientists in selecting and implementing the most appropriate method for their investigative goals. The core distinction lies in the presence of a semipermeable membrane; microdialysis incorporates this membrane to contain fluid flow and filter molecules, whereas push-pull perfusion involves the direct, open exchange of fluid with the brain extracellular space [60] [61].
Technical Comparison & Quantitative Data
The choice between microdialysis and push-pull perfusion involves trade-offs between sample purity, temporal resolution, practical handling, and potential tissue perturbation. The table below summarizes a direct, quantitative comparison from key studies.
Table 1: Quantitative Comparison of Microdialysis and Push-Pull Perfusion
| Parameter | Microdialysis | Push-Pull Perfusion | Experimental Context & Citation |
|---|---|---|---|
| Dopamine (DA) Basal Recovery | Almost undetectable [62] | 7.0–10.0 pg/min [62] | Rat caudate nucleus, artificial CSF perfusion [62] |
| DA Recovery with K+ Stimulation | Lower (benchmark = 1x) [62] | 2–4x higher than microdialysis [62] | 30/60 mM K+ in CSF; simultaneous implantation [62] |
| Serotonin & Norepinephrine | No basal levels detected; no change to noxious pinch [63] | Significant increase in response to noxious pinch [63] | Spinal cord dorsal horn; sample collection without perchloric acid [63] |
| Typical Perfusion Flow Rate | 0.1 - 5.0 µL/min (low) [9] [60] | 10 - 20 µL/min (high, to prevent clogging) [64] [61] | Standard operational parameters [9] [60] [64] |
| Mechanical Setup | Single "push" pump [60] | Two precisely calibrated "push" and "pull" pumps [60] [61] | Required system configuration [60] [61] |
| Tissue Damage & Gliosis | Minimal fluidynamic disturbance; damage localized to track [60] | Potentially greater due to open flow and higher perfusion rates [62] [61] | Acute experiments show more damage with push-pull; gliosis occurs with chronic cannula placement [62] [61] |
| Sample Clean-up | Automatic; membranes exclude large molecules and proteins [61] | None; samples contain all molecules from extracellular fluid [60] | Beneficial for analyzing easily degradable molecules like acetylcholine [61] |
Experimental Protocols
Protocol: Simultaneous Comparison of Neurotransmitter Efflux
This protocol is adapted from a direct comparison study and is designed to benchmark microdialysis performance against push-pull perfusion in the same animal [62].
1. Probe Implantation and Preparation:
- Animals: Use anesthetized rats.
- Stereotaxic Surgery: Implant a miniaturized push-pull needle (e.g., 33/26 ga) into the left caudate nucleus and a dialysis probe (e.g., 24 ga) into the right caudate nucleus.
- Perfusate: Use an artificial cerebrospinal fluid (aCSF). A common formulation is: 123 mM NaCl, 4.8 mM KCl, 1.22 mM MgSO₄, 13.9 mM Na₂HPO₄, 2.45 mM NaH₂PO₄, 1 mM CaCl₂, pH 7.4 [62] [61]. Add an enzyme inhibitor like bacitracin (58 µg/mL) if sampling peptides [61].
- Flow Rates: Perfuse the push-pull cannula at 10 µL/min and the dialysis probe at 1.0 or 2.0 µL/min [62].
2. Sample Collection and Stimulation:
- Baseline Collection: Collect 8-10 sequential perfusate and dialysate samples to establish baseline levels.
- Stimulated Release: Incorporate a high-K⺠solution (e.g., 30 or 60 mM) into the aCSF to evoke neurotransmitter release. Deliver this solution simultaneously to both probes.
- Sample Handling: Collect samples on ice in a fraction collector. Aliquot and immediately freeze on dry ice, storing at -70°C until analysis [61].
3. Analytical Quantification:
- Analysis: Quantify neurotransmitters and metabolites using High-Performance Liquid Chromatography (HPLC) with appropriate detection (e.g., coulometric electrochemical detection for catecholamines).
- Data Calculation: Express efflux in absolute terms (e.g., pg/min) [62].
4. Histological Validation:
- Perfusion and Sectioning: Upon experiment completion, transcardially perfuse the animal with fixative. Remove the brain and prepare frozen or paraffin sections.
- Staining: Stain sections (e.g., Cresyl Violet) to localize probe placement and assess cytological damage at both implantation sites [62] [5].
Protocol: Assessing Pharmacologically-Induced Changes in Monoamines
This protocol, derived from spinal cord studies, highlights the capability to detect stimulus-evoked changes in monoamines, which can be more readily measured with push-pull perfusion under certain conditions [63].
1. Probe Implantation:
- Implant a transverse push-pull or microdialysis catheter into the target region (e.g., spinal cord dorsal horn).
2. Sample Collection and Pharmacological Challenge:
- Baseline: Collect samples for at least 60 minutes prior to intervention.
- Stimulus Application: Apply a noxious stimulus (e.g., 20s pinch/min for 10 minutes) or a pharmacological agent.
- Post-Stimulus: Continue sampling for a recovery period.
- Critical Note on Sample Stability: Collect samples without perchloric acid for monoamine stability. Analyze samples via HPLC within 24 hours to prevent significant analyte degradation [63].
Workflow and Mechanism Visualization
The following diagram illustrates the fundamental operational principles and key differentiating factors of the two sampling techniques.
Diagram 1: Comparative workflow of Microdialysis and Push-Pull Perfusion, highlighting key technical distinctions and their practical implications.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of these in vivo sampling techniques requires carefully selected reagents and materials. The table below details essential components and their functions.
Table 2: Essential Materials for Perfusion-Based Sampling
| Item | Function / Description | Application Notes |
|---|---|---|
| Artificial Cerebrospinal Fluid (aCSF) | Isotonic perfusion solution mimicking the ionic composition of brain extracellular fluid. [29] [61] | Base for perfusate; can be modified with K⺠for stimulation or drugs for local application. |
| Bovine Serum Albumin (BSA) / Human Serum Albumin (HSA) | Perfusate additive to reduce nonspecific binding of hydrophobic drugs to the apparatus. [29] [65] | Critical for accurate sampling of hydrophobic compounds (e.g., ulixertinib, selinexor). Concentrations of 0.5-1.5% are common. [29] |
| Microdialysis Probe | Device featuring a semipermeable membrane with a defined molecular weight cutoff (MWCO). [9] [60] | MWCO (e.g., 20 kDa) determines size of collectable molecules. Probe size and membrane length are tissue-dependent. |
| Push-Pull Cannula | Concentric cannula system where an inner "push" tube is slightly extruded from an outer "pull" tube. [64] [61] | Typically custom-fabricated. Precise length matching between inner cannula and stylet is critical to minimize tissue damage on insertion. [61] |
| Precision Perfusion Pumps | Syringe or peristaltic pumps for controlling fluid flow. [60] | Microdialysis requires one pump. Push-pull perfusion requires two precisely calibrated pumps to maintain balanced flow and prevent fluid buildup. [60] [61] |
| Bacitracin | Protease inhibitor added to the perfusate. [61] | Stabilizes neuropeptides in collected samples (e.g., LHRH, NPY) by inhibiting enzymatic degradation. |
| Fraction Collector | Instrument for automated collection of perfusate/dialysate samples at defined time intervals. [29] [61] | Allows for high temporal resolution monitoring of neurotransmitter dynamics. Samples are typically collected on ice. |
In vivo neuropharmacology research requires precise methods to correlate the concentration of neurotransmitters in the brain extracellular space with their resulting pharmacological effects. Microdialysis sampling has emerged as a preeminent technique for monitoring these extracellular chemical dynamics in living organisms [66]. This application note details integrated protocols for measuring neurotransmitter levels via microdialysis and constructing mechanism-based pharmacokinetic-pharmacodynamic (PK-PD) models to quantitatively link these concentrations to observed effects. The approaches outlined herein are framed within a broader thesis on utilizing advanced microdialysis techniques to elucidate the chemical underpinnings of brain function and dysfunction, providing researchers with practical methodologies for advancing neuropharmacological drug development.
Quantitative Analysis of Neurotransmitter Dynamics
Microdialysis enables the collection of small molecules from the brain extracellular space, allowing researchers to monitor changes in neurotransmitter levels during various physiological and pharmacological manipulations. The following table summarizes key quantitative findings from recent studies employing these techniques:
Table 1: Key Quantitative Findings on Neurotransmitter Dynamics from Microdialysis Studies
| Neurotransmitter/Parameter | Quantitative Finding | Experimental Context | Citation |
|---|---|---|---|
| Extracellular Dopamine (NAc) | 20-30 nM (basal) | Awake, freely moving rats measured by FSCV | [67] |
| Extracellular Dopamine (NAc) | ~500 nM (after VMAT2 inhibition) | Following tetrabenazine (1 mg/kg i.v.) | [67] |
| Identified Compounds in Dialysate | 479 unique compounds | Rat striatum using LC-MS/MS | [5] |
| Benzoylated Features Detected | 872 non-degenerate features | Including most small molecule neurotransmitters | [5] |
| Neuronal Glutamate | 144 ± 35 nM | From 2.5 μM 13C5-glutamine infusion in rat cortex | [68] |
| DAT Dissociation Constant (Kd) | 0.248 μM | Methylphenidate binding in vitro | [69] |
Experimental Protocols
In Vivo Microdialysis for Deep Metabolome Coverage
This protocol describes an approach for identifying hundreds of compounds in brain dialysate, enabling deep monitoring of brain chemistry in time-resolved studies [5].
Materials
- CMA 12 Elite microdialysis probes (4 mm membrane, 20,000 MWCO)
- Male Sprague-Dawley rats (75 days old, 340-375 g)
- LC-MS grade acetonitrile, methanol, and water
- Benzoyl chloride (light and 13C6-labeled)
- Artificial cerebrospinal fluid (aCSF: 145 mM NaCl, 2.68 mM KCl, 1.40 mM CaClâ‚‚, 1.01 mM MgSOâ‚„, 1.55 mM Naâ‚‚HPOâ‚„, 0.45 mM NaHâ‚‚POâ‚„, 0.25 mM ascorbic acid)
- Thermo Fisher Scientific Vanquish Horizon LC system coupled to Orbitrap ID-X mass spectrometer
Procedure
- Surgical Implantation: Anesthetize rats with ketamine (65 mg/kg) and dexdomitor (0.25 mg/kg). Position in stereotaxic frame and implant microdialysis probes in target brain region (e.g., striatum: +0.2 mm anterior, ±2.3 mm lateral from bregma, 3 mm ventral).
- Dialysate Collection: Connect probes to syringe pump and perfuse with aCSF at 1 μL/min. Collect samples from awake animals over 12 hours. Pool samples from multiple animals if necessary for increased detection sensitivity.
- Sample Preparation - Underivatized:
- Transfer 750 μL aliquots to tapered glass HPLC vials.
- Dry in vacuum centrifuge at ambient temperature for >3 hours.
- Reconstitute with 75 μL of 9:1 water:methanol (for RPLC) or 85:15 acetonitrile:water (for HILIC).
- Sample Preparation - Derivatized:
- Mix dialysate with 100 mM sodium tetraborate.
- Add benzoyl chloride (2% in acetonitrile, v/v).
- Include internal standard (13C6-benzoyl chloride in sodium tetraborate).
- LC-MS/MS Analysis:
- HILIC: Use BEH Amide column (2.1 × 100 mm, 1.7 μm) with positive/negative mode MS.
- RPLC: Use HSST3 column (2.1 × 100 mm, 1.8 μm).
- Set MS parameters: sheath gas 40, aux gas 10, ion transfer tube temp 325°C, vaporizer temp 300°C, orbitrap resolution 120,000.
- For MS/MS: resolution 60,000, intensity threshold 1.0×10â´, collision energies 20, 40, and 80%.
- Data Processing: Use MetIDTracker software to search MS/MS spectra against NIST20, MONA, and MS-Dial libraries.
Metabolic Labeling for Source-Specific Glutamate Measurement
This protocol enables differentiation of neuronal versus astrocytic glutamate sources using metabolic labeling [68].
Materials
- Custom-built microdialysis probes (40/100 μm i.d./o.d. fused silica) or CMA12 Elite probes
- 13C5-glutamine
- Tetrodotoxin (TTX)
- α-(methylamino)isobutyric acid
- Riluzole
- (1S,3R)-1-aminocyclopentane-1,3-dicarboxylic acid (ACPD)
- l-trans-pyrrolidine-2,4-dicarboxylic acid (PDC)
Procedure
- Probe Implantation: Implant microdialysis probes into target region (e.g., cortex).
- Metabolic Labeling: Add 2.5 μM 13C5-glutamine to perfusate aCSF.
- Pharmacological Manipulations:
- To inhibit neuronal activity: Add 20 μM TTX to perfusate.
- To block glutamine transport: Add 20 mM α-(methylamino)isobutyric acid or 500 mM riluzole.
- To activate metabotropic glutamate receptors: Add 100 μM ACPD.
- To inhibit glutamate uptake: Add 100 μM PDC.
- Sample Collection: Collect dialysate at 1 μL/min in 10-30 minute intervals.
- Stress Induction: Apply tail pinch for 2-5 minutes while collecting dialysate to evoke neuronal glutamate release.
- Analysis: Derivatize samples with benzoyl chloride and analyze via UPLC-MS/MS.
PK-PD Modeling of Dopamine Based on DAT Occupancy
This protocol describes a mechanism-based approach to model dopamine levels based on dopamine transporter occupancy [69].
Materials
- Methylphenidate hydrochloride
- Cocaine
- Fluorescent-based neurotransmitter transporter uptake assay dye
- Rat striatal synaptosomes
Procedure
- In Vitro DAT Binding Assay:
- incubate rat striatal synaptosomes with fluorescent DAT substrate.
- Apply methylphenidate (0.0781-2.50 μM) to inhibit DAT uptake.
- Monitor fluorescence intensity over time.
- Fit data to determine association (kâ‚’â‚™) and dissociation (kâ‚’ff) rate constants.
- In Vivo Microdialysis:
- Administer methylphenidate (1-10 mg/kg i.v.) to rats.
- Collect striatal dialysate at regular intervals.
- Analyze dopamine content using HPLC-EC or LC-MS.
- Plasma and Brain Concentration Measurement:
- Collect blood samples at multiple time points.
- Extract and analyze methylphenidate concentrations using LC-MS.
- Measure brain tissue concentrations where possible.
- Model Development:
- Develop pharmacokinetic model for methylphenidate plasma and brain concentrations.
- Incorporate kâ‚’â‚™ and kâ‚’ff values to estimate DAT occupancy.
- Link DAT occupancy to changes in extracellular dopamine levels using an Emax model.
Signaling Pathways and Experimental Workflows
Neuronal Glutamate Measurement Through Metabolic Labeling
Diagram 1: Metabolic labeling of neuronal glutamate via the glutamine-glutamate shuttle. 13C5-glutamine delivered via microdialysis perfusate is taken up by neurons, converted to 13C5-glutamate, and released synaptically, allowing differentiation from non-neuronal glutamate sources [68].
Dopamine Dynamics and DAT Occupancy PK-PD Modeling
Diagram 2: PK-PD model linking methylphenidate concentrations to dopamine increases via DAT occupancy. The model incorporates binding kinetics (kâ‚’â‚™/kâ‚’ff) to predict dopamine increases based on transporter occupancy [69] [67].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Microdialysis and Neurotransmitter Analysis
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| CMA 12 Elite Microdialysis Probes | Sampling brain extracellular fluid | 4 mm membrane, 20,000 MWCO, 0.5 mm O.D. |
| Benzoyl Chloride (and 13C6-labeled) | Chemical derivatization for enhanced LC-MS detection of amines | 2% in acetonitrile (v/v) |
| Artificial Cerebrospinal Fluid (aCSF) | Physiological perfusion fluid for microdialysis | 145 mM NaCl, 2.68 mM KCl, 1.40 mM CaClâ‚‚, 1.01 mM MgSOâ‚„, 1.55 mM Naâ‚‚HPOâ‚„, 0.45 mM NaHâ‚‚POâ‚„, 0.25 mM ascorbic acid |
| 13C5-Glutamine | Metabolic precursor for labeling neuronal glutamate | 2.5 μM in perfusate for neuronal glutamate tracing |
| Tetrodotoxin (TTX) | Sodium channel blocker to inhibit neuronal activity | 20 μM in perfusate to identify neuronal vs. non-neuronal release |
| α-(Methylamino)isobutyric Acid | Inhibitor of glutamine transport into neurons | 20 mM in perfusate to block Gln-Glu shuttle |
| GBR 12909 | Dopamine transporter inhibitor | 1.5 mg/kg i.v. to probe DAT contribution to extracellular dopamine |
| Tetrabenazine | Vesicular monoamine transporter (VMAT2) inhibitor | 1 mg/kg i.v. to deplete dopamine storage and induce reverse transport |
Data Analysis and Interpretation
Pattern Recognition in Pharmacodynamic Response
The time course of pharmacodynamic responses often differs markedly from plasma drug concentrations due to complex interactions including transport to the biophase, target binding, activation of downstream mediators, and homeostatic feedback mechanisms [70]. When analyzing response-time data:
- Identify baseline behavior and determine if it is stable, oscillating, or drifting
- Note the number of phases in the response-time course
- Look for time delays between concentration and response peaks
- Check for peak shifts in response with increasing doses
- Identify saturation phenomena and other nonlinearities
Turnover Modeling Approaches
The basic turnover model (also known as the indirect response model) provides a framework for interpreting pharmacodynamic data [70]. Key variants include:
- Inhibition of production (declining response)
- Inhibition of loss (increasing response)
- Stimulation of production (increasing response)
- Stimulation of loss (declining response)
These models can be extended to incorporate complex phenomena such as tolerance, rebound, and oscillatory behavior through the addition of feedback mechanisms.
The integration of advanced microdialysis techniques with mechanism-based PK-PD modeling provides a powerful framework for correlating extracellular neurotransmitter levels with pharmacodynamic outcomes. The protocols outlined in this application note enable researchers to obtain deep coverage of the brain extracellular metabolome, differentiate neurotransmitter sources through metabolic labeling, and develop quantitative models that link target engagement to functional responses. These approaches facilitate the translation of preclinical findings to human therapeutic applications by providing a mechanistic basis for understanding central nervous system drug action.
Microdialysis is a pivotal in vivo sampling technique that enables researchers to monitor extracellular concentrations of neurotransmitters in the brain of living animals, providing critical insights into neurochemical dynamics under physiological and pathological conditions. This technique involves implanting a semi-permeable membrane into a discrete brain region, perfusing it with a solution mimicking cerebrospinal fluid, and collecting dialysates for analysis of their chemical content, typically via high-performance liquid chromatography (HPLC) [71]. The application of microdialysis has dramatically advanced our understanding of neurochemical mechanisms in various brain disorders. This application note presents detailed case studies validating the use of microdialysis in three distinct research domains: addiction, Attention Deficit Hyperactivity Disorder (ADHD), and Parkinson's disease, providing standardized protocols and analytical frameworks for researchers investigating these conditions.
Case Study 1: Psychostimulant Addiction and Neuroplasticity
Background and Experimental Validation
Drug addiction is characterized by compulsive drug-seeking despite negative consequences, a behavior driven by long-lasting neuroplastic changes in mesocorticolimbic circuitry. Microdialysis studies have been instrumental in mapping the neurotransmitter alterations that occur during different phases of addiction, from initial exposure to relapse. Research has demonstrated that chronic exposure to drugs of abuse like cocaine induces significant neuroplasticity in multiple neurotransmitter systems including glutamate, GABA, dopamine, and serotonin [71]. These studies typically employ animal models such as psychomotor sensitization, conditioned place preference (CPP), and self-administration paired with microdialysis to correlate neurochemical changes with behavioral output.
Key validated findings include the discovery that chronic cocaine administration produces time-dependent changes in glutamate neurotransmission. After extended withdrawal periods (21 days), cocaine-sensitized rats exhibit increased glutamate efflux in the nucleus accumbens (NAc) core following a cocaine challenge compared to saline-treated controls [71]. Similarly, dopamine release patterns shift dramatically throughout addiction stages, with early withdrawal showing increased basal extracellular dopamine in the NAc, while late withdrawal shows decreased basal release [71].
Key Neurochemical Findings in Addiction
Table 1: Neurochemical Changes After Chronic Cocaine or Amphetamine Measured by Microdialysis
| Drug Administration/ Behavioral Paradigm | Neurotransmitter | Brain Region | Effect | Reference |
|---|---|---|---|---|
| Psychomotor Sensitization (early withdrawal) | Glutamate | mPFC | ↑ | Williams and Steketee, 2004 |
| GABA | mPFC | ↑ | Jayaram and Steketee, 2005 | |
| Dopamine | NAc | NC | Wolf et al., 1993 | |
| Psychomotor Sensitization (late withdrawal) | Glutamate | NAc | ↑ | Pierce et al., 1996 |
| Dopamine | NAc | ↑ | Robinson et al., 1998 | |
| Basal Extracellular Concentration after Withdrawal | Glutamate | NAc | ↓ | Baker et al., 2003 |
| GABA | NAc | ↑ | Xi et al., 2003 | |
| Drug-primed Reinstatement | Glutamate | NAc core | ↑ | McFarland et al., 2003 |
| GABA | VP | ↓ | Tang et al., 2005 | |
| Dopamine | NAc | ↑ | Neisewander et al., 1996 |
Key: ↑ = increased extracellular concentration; ↓ = decreased extracellular concentration; NC = no change; NAc = nucleus accumbens; mPFC = medial prefrontal cortex; VP = ventral pallidum
Signaling Pathways in Addiction Neuroplasticity
The following diagram illustrates the key neurotransmitter pathways involved in addiction neuroplasticity and their interactions:
Case Study 2: ADHD and Catecholaminergic Dysregulation
Experimental Approach and Validation
The spontaneously hypertensive (SH) rat has been extensively validated as an animal model displaying core behavioral and cognitive deficits relevant to ADHD, including hyperactivity, impulsivity, and attentional impairments. Microdialysis studies in freely-moving SH rats have revealed distinctive neurochemical deficits that mirror proposed catecholaminergic dysregulation in human ADHD [72] [73]. These studies typically involve implanting microdialysis probes in brain regions central to ADHD pathology, including the prefrontocortex (PFC), striatum, and nucleus accumbens, followed by collection of dialysates during baseline conditions and after pharmacological challenges with ADHD medications.
A key validation finding is that SH rats exhibit attenuated basal norepinephrine efflux in the PFC alongside hyperfunctional dopaminergic neurotransmission in striatal and mesolimbic regions [72] [73]. This neurochemical profile aligns with the hyperactive phenotype of SH rats and informs our understanding of ADHD pathophysiology. Furthermore, microdialysis has revealed that the most efficacious ADHD medications powerfully increase both norepinephrinergic and dopaminergic neurotransmission, providing a neurochemical basis for treatment efficacy [73].
Pharmacological Profiling of ADHD Medications
Table 2: Effects of ADHD Medications on Catecholamines Measured by Microdialysis in SH Rats
| Drug | Mechanism | Effect on NE in PFC | Effect on DA in Striatum/NAc | Clinical Efficacy Correlation |
|---|---|---|---|---|
| d-amphetamine | Monoamine releasing agent | ↑↑↑ | ↑↑↑ | High efficacy |
| dl-threo-methylphenidate | DA/NE reuptake inhibitor | ↑↑ | ↑↑ | High efficacy |
| d-threo-methylphenidate | DA/NE reuptake inhibitor | ↑↑ | ↑↑ | High efficacy |
| l-threo-methylphenidate | DA/NE reuptake inhibitor | ↑ | ↑ | Moderate efficacy |
| Atomoxetine | Selective NE reuptake inhibitor | ↑↑ | ↓/NC | Moderate efficacy |
Key: ↑ = mild increase; ↑↑ = moderate increase; ↑↑↑ = strong increase; NE = norepinephrine; DA = dopamine; PFC = prefrontal cortex; NAc = nucleus accumbens; NC = no change
Experimental Protocol: Microdialysis in SH Rats for ADHD Drug Screening
Materials:
- Freely-moving spontaneously hypertensive rats (8-12 weeks old)
- Microdialysis guide cannulae targeting PFC, striatum, and/or NAc
- Ringer's solution (147 mM NaCl, 2.2 mM CaClâ‚‚, 4 mM KCl)
- Syringe pump with liquid swivel system
- Fraction collector
- HPLC-EC or LC-MS systems for catecholamine analysis
- ADHD medications (amphetamine, methylphenidate, atomoxetine)
Procedure:
- Implant microdialysis guide cannulae stereotaxically into target regions under anesthesia.
- Allow 48-hour recovery period post-surgery.
- Insert microdialysis probes (2-4 mm membrane length, depending on target region) 12-16 hours before experiment.
- Perfuse with Ringer's solution at 1.0-1.5 μL/min overnight.
- On experiment day, adjust flow rate to 2.0 μL/min and allow 60-minute stabilization.
- Collect baseline samples every 15-20 minutes for at least 2 hours to establish stable baseline.
- Administer ADHD medication (systemically or locally via reverse dialysis).
- Continue sample collection for 3-5 hours post-administration.
- Analyze samples for norepinephrine, dopamine, and metabolites using HPLC-EC.
- Verify probe placement histologically post-experiment.
Validation Notes:
- SH rats show different pharmacodynamic responses compared to outbred Sprague-Dawley rats, highlighting the importance of using validated disease models [73].
- Basal catecholamine levels differ significantly between SH rats and controls, with PFC norepinephrine notably lower in SH rats [73].
- Drug responses are dose-dependent and enantiomer-specific, requiring careful pharmacological characterization.
Case Study 3: Parkinson's Disease and Dopaminergic Restoration
Background and Mechanistic Insights
Parkinson's disease involves the progressive degeneration of nigrostriatal dopaminergic neurons, leading to characteristic motor symptoms. L-DOPA remains the most effective treatment, but its mechanism of action has been clarified through microdialysis studies, particularly in the 6-hydroxydopamine (6-OHDA) lesioned rat model of Parkinson's disease [74]. Microdialysis has been essential in demonstrating that L-DOPA's therapeutic effects involve conversion to dopamine primarily within serotonergic (5-HT) neurons rather than remaining dopaminergic neurons in severely lesioned states [74].
Multisite intracerebral microdialysis, with probes simultaneously implanted in multiple brain regions, has revealed that L-DOPA-induced dopamine release occurs widely throughout the brain in regions receiving serotonergic innervation, not just the striatum [74]. This widespread release pattern may contribute to both therapeutic effects and side effects like dyskinesias and psychosis. Additionally, microdialysis in parkinsonian patients during deep brain stimulation surgery has provided direct human validation, showing stable basal release of amino acid neurotransmitters but limited acute changes in response to apomorphine administration [75].
Key Findings in Parkinson's Disease Models
Table 3: Microdialysis Findings in Parkinson's Disease Models and Patients
| Experimental Condition | Neurotransmitter | Brain Region | Effect | Significance |
|---|---|---|---|---|
| L-DOPA in 6-OHDA rats | Dopamine | Striatum | ↑↑↑ (5-HT dependent) | 5-HT neurons mediate DA release after severe DA depletion [74] |
| Dopamine | Extrastriatal regions | ↑ (widespread) | Explains broader L-DOPA effects beyond motor symptoms [74] | |
| Basal measurements in PD patients | GABA | GPi vs. GPe | Higher in GPi | Reflects altered basal ganglia output in OFF state [75] |
| Apomorphine in PD patients | Amino acids (GABA, glutamate) | GPe/GPi, STN | No change | Clinical effects not mediated by acute amino acid release changes [75] |
| Transplantation in 6-OHDA rats | Dopamine | Striatum | Phasic release during swimming | Transplant integration restores context-dependent DA release [76] |
Key: 6-OHDA = 6-hydroxydopamine; 5-HT = serotonin; GPi = internal globus pallidus; GPe = external globus pallidus; STN = subthalamic nucleus
L-DOPA Mechanism of Action Pathway
The following diagram illustrates the mechanism of L-DOPA-induced dopamine release in the parkinsonian brain:
Experimental Protocol: Multisite Microdialysis in 6-OHDA Lesioned Rats
Materials:
- Unilateral 6-OHDA lesioned rats (≥90% striatal DA depletion)
- Microdialysis probes with 2-4 mm membranes
- L-DOPA with benserazide or carbidopa (peripheral decarboxylase inhibitor)
- Artificial cerebrospinal fluid (aCSF)
- HPLC-EC with catecholamine analysis capability
- Tetrodotoxin (TTX), reserpine, 5-HT neuron toxins for pharmacological validation
Procedure:
- Establish 6-OHDA lesions 2-4 weeks prior to microdialysis experiments.
- Verify lesion extent by monitoring contralateral rotation to apomorphine.
- Implant microdialysis guide cannulae in multiple regions (e.g., striatum, prefrontal cortex, substantia nigra).
- On experiment day, insert probes and perfuse with aCSF at 1.5-2.0 μL/min.
- After 2-hour stabilization, collect baseline samples every 15-20 minutes.
- Administer L-DOPA (50-100 mg/kg i.p. with peripheral decarboxylase inhibitor).
- Continue sample collection for 3-6 hours post-administration.
- For mechanism studies, include pharmacological challenges:
- TTX (1 μM) via reverse dialysis to assess impulse-dependence
- Reserpine pre-treatment to deplete vesicular stores
- 5-HT1A agonists to inhibit 5-HT neuron firing
- Analyze samples for dopamine, serotonin, and metabolites.
- For behavioral correlation, monitor rotational behavior or locomotor activity during dialysis.
Validation Notes:
- L-DOPA-induced dopamine release in severely lesioned rats is:
- Multisite probes reveal region-dependent release patterns explaining both therapeutic and side effects.
General Microdialysis Protocol Considerations
Technical Specifications and Methodological Standards
Probe Construction and Selection:
- Membrane materials: Commonly used membranes include cuprophane, polycarbonate, or polysulfone with 2-4 mm length and 200-300 kDa molecular weight cut-off
- Flow rates: Typically 1.0-2.0 μL/min for optimal recovery without tissue damage
- Recovery calibration: Determine in vitro recovery for each probe before implantation
Analytical Methods:
- HPLC with electrochemical detection (HPLC-EC): Preferred for monoamines (dopamine, norepinephrine, serotonin)
- HPLC with fluorescence detection: Suitable for amino acid neurotransmitters (glutamate, GABA) after derivatization
- LC-MS/MS: Emerging as gold standard for simultaneous analysis of multiple neurotransmitter classes with high sensitivity [14]
Validation Requirements:
- Histological verification of probe placement post-experiment
- Determination of extraction fraction for each analyte
- Stability testing of analytes in collection vials
- In vitro recovery assessment for each probe
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Microdialysis Studies in Neurological Disorders
| Reagent/Category | Specific Examples | Function/Application | Notes |
|---|---|---|---|
| Neurotoxins for Modeling | 6-OHDA, MPTP | Selective lesioning of dopaminergic neurons | 6-OHDA used in rats, MPTP in primates; require proper safety protocols |
| Pharmacological Agents | Apomorphine, L-DOPA, Amphetamine, Ro 60-0175 (5-HT2C agonist) | Challenge tests, mechanism studies | Dose-response critical; species/strain differences important |
| Transporter Inhibitors | Nomifensine (DA), Desipramine (NE), Citalopram (5-HT) | Enhance neurotransmitter detection, mechanism studies | Nomifensine increases basal DA detection in microdialysis [76] |
| Enzyme Inhibitors | Benserazide, Carbidopa | Peripheral DOPA decarboxylase inhibition for L-DOPA studies | Enhance central L-DOPA delivery; standard in Parkinson's studies |
| Analytical Standards | Dopamine, DOPAC, HVA, 5-HIAA, Glutamate, GABA | HPLC/LC-MS calibration | Essential for quantitative analysis; prepare fresh daily |
| Perfusion Solutions | Ringer's solution, Artificial CSF | Microdialysis perfusion medium | Ionic composition critical for neuronal viability and baseline measures |
Microdialysis has proven to be an invaluable technique for validating disease mechanisms and treatment strategies in models of addiction, ADHD, and Parkinson's disease. Through the case studies presented, we demonstrate how this technique provides unique insights into neurochemical dynamics in vivo, revealing neurotransmitter-specific alterations that underlie behavioral phenotypes and treatment responses. The standardized protocols and validation criteria outlined here provide researchers with robust frameworks for applying microdialysis to these research domains, ensuring reliable and interpretable results that advance our understanding of complex neurological disorders and facilitate the development of more effective therapeutics.
In vivo neuroscience research and central nervous system (CNS) drug development require precise measurement of neurotransmitter dynamics. No single technique provides a complete picture; microdialysis, positron emission tomography (PET), and fluorescence methods each offer unique advantages and limitations. Cross-technique validation, the process of integrating data from these complementary methodologies, is therefore critical for obtaining a holistic and accurate understanding of neurochemical processes in the living brain. This Application Note provides a detailed framework for designing and executing studies that synergistically combine quantitative microdialysis with PET imaging and fluorescence-based detection. We outline specific experimental protocols, data analysis procedures, and reagent solutions to enable researchers to robustly validate findings across technological platforms, thereby strengthening the reliability of neurochemical data for both basic research and drug development applications.
Quantitative Microdialysis
Quantitative microdialysis (qµD) is a well-established biophysical technique for determining the affinity of small molecules for target proteins and for analyzing their diffusibility in vivo [59]. The core principle involves incubating a target protein and test compound in a chamber partitioned by a semipermeable membrane that allows only small molecules to pass through. Following incubation, techniques like reversed-phase high performance liquid chromatography (RP-HPLC) or liquid chromatography–mass spectrometry (LC–MS) are used to determine compound abundance in each chamber. A higher concentration in the protein-containing chamber indicates binding, from which the dissociation constant (KD) can be calculated [59]. A significant advantage of qµD is its ability to reliably determine very low-affinity interactions, with KD values up to 500 µM [59]. Beyond in vitro binding studies, in vivo brain microdialysis is the preferred method for monitoring neurotransmitters like glutamate, GABA, and acetylcholine in the extracellular space of behaving animals, typically coupled with HPLC for analysis [77]. However, a key limitation is its poor temporal resolution (on the order of minutes), which can miss rapid, phasic neurotransmitter release events [77].
Positron Emission Tomography (PET) Imaging
PET neuroimaging is a powerful, non-invasive tool for quantifying molecular targets in the human brain. It is particularly useful for measuring dynamic changes in endogenous neurotransmitter levels, such as dopamine, serotonin, and opioids, in response to pharmacological or behavioral challenges [78]. The most common approach involves administering a radioactive tracer that competes with the endogenous neurotransmitter for receptor binding sites. A decrease in the tracer's binding potential (BPND) between a rest state and a stimulated state is used as an index of neurotransmitter release [78]. While traditional "time-invariant" models assume constant neurotransmitter levels during the scan, newer "time-varying" models like the linearized simplified reference tissue model (LSRTM) and linear parametric neurotransmitter PET (lp-ntPET) are better configured to capture transient neurotransmitter responses during a single scanning session [78]. Recent efforts have culminated in comprehensive normative atlases of neurotransmitter receptors and transporters across the human brain, providing an invaluable reference for interpreting neurochemical patterns in health and disease [79] [80].
Fluorescence and Optical Methods
Fluorescence-based detection, while not covered in depth in the provided search results, is a cornerstone of in vitro assay development and is increasingly used in vivo with biosensors. These methods often provide high temporal and spatial resolution. As part of a cross-technique validation framework, fluorescence can be used in benchtop assays to confirm binding interactions or compound properties before moving to more complex in vivo microdialysis or PET studies. The development of micro-instruments based on microfluidics, micro-optics, and microelectronics promises future opportunities for highly sensitive, real-time monitoring of neurotransmitters in compact formats [81].
Table 1: Key Characteristics of Neurotransmitter Measurement Techniques
| Technique | Key Measured Parameters | Temporal Resolution | Spatial Resolution | Primary Applications |
|---|---|---|---|---|
| Quantitative Microdialysis | Extracellular fluid concentration, KD, extraction fraction [59] [77] | Minutes to hours (Poor) [77] | Millimetre (probe-dependent) | In vivo sampling in animals, affinity determination, pharmacokinetics |
| PET Imaging | Binding potential (BPND), receptor/transporter availability, ΔBPND [78] | Minutes to tens of minutes | Millimetre | Non-invasive human brain imaging, neurotransmitter release, receptor occupancy |
| Fluorescence/Biosensors | Real-time concentration changes, kinetic binding parameters | Sub-second to seconds (High) [77] | Micrometre | In vitro binding assays, in vivo real-time monitoring with implanted sensors |
Integrated Experimental Protocols
Protocol 1: Validating PET-Derived Dopamine Release with Microdialysis
This protocol is designed to cross-validate changes in striatal dopamine release measured non-invasively with PET in a pre-clinical rodent model using the gold-standard of in vivo microdialysis.
A. PET Imaging of Amphetamine-Induced Dopamine Release
- Radiotracer Injection: Anesthetize the animal and administer a bolus of a dopamine D2/D3 receptor radioligand (e.g.,
[11C]Racloprideor[18F]Fallypride) intravenously. - Dynamic PET Scan: Initiate a 90-minute dynamic PET scan to establish a baseline binding curve for the radiotracer.
- Pharmacological Challenge: At a predetermined time (e.g., 30 minutes post-injection), administer a dose of d-amphetamine (e.g., 0.5 mg/kg, i.p.) known to evoke substantial dopamine release.
- Image Reconstruction and Analysis: Reconstruct dynamic PET images and co-register them with an anatomical MRI template. Using the simplified reference tissue model (SRTM) or LSRTM, generate parametric maps of BPND.
- Quantification: Calculate the percentage change in BPND (ΔBPND) in the striatum between the pre-amphetamine and post-amphetamine periods using the standard endpoint: ΔBPND = (BPNDpost - BPNDpre) / BPNDpre [78].
B. Post-PET Microdialysis Validation
- Guide Cannula Implantation: In a separate cohort of animals, surgically implant a guide cannula targeting the striatum (coordinates: AP +1.0 mm, ML ±2.5 mm from bregma; DV -3.0 mm from dura) and allow for a post-surgical recovery period of at least 48 hours.
- Microdialysis Probe Insertion and Perfusion: On the experimental day, insert a microdialysis probe with a 4-mm active membrane (e.g., 220 µm o.d., 13-kDa MWCO) through the guide cannula. Perfuse with artificial cerebrospinal fluid (aCSF: 145 mM NaCl, 2.8 mM KCl, 1.2 mM CaCl2, 1.2 mM MgCl2, 0.25 mM ascorbic acid, 5.4 mM D-glucose, pH 7.4) at a constant flow rate of 1.0 µL/min [82].
- Baseline Sample Collection: After a 2-hour equilibration period, collect dialysate samples every 10-20 minutes to establish a stable baseline of extracellular dopamine.
- Amphetamine Challenge and Sample Collection: Administer the same dose of d-amphetamine (0.5 mg/kg, i.p.) used in the PET experiment and continue collecting dialysate samples for at least 2 hours.
- Dialysate Analysis: Analyze dopamine content in the dialysate samples using HPLC coupled with electrochemical detection (HPLC-ECD) or LC-MS.
- Data Correlation: Correlate the percentage increase in extracellular dopamine concentration measured by microdialysis with the percentage decrease in
[11C]RacloprideBPND measured by PET.
Protocol 2: Using Fluorescence and qµD for In Vitro Binding Affinity (KD) Determination
This protocol uses fluorescence-based assays as a high-throughput initial screen to inform and validate subsequent quantitative microdialysis experiments for precise KD determination.
A. Fluorescence Polarization (FP) Binding Assay
- Plate Setup: Prepare a dilution series of the target protein in an assay buffer compatible with both fluorescence and dialysis.
- Incubation: To each well, add a constant, low-nanomolar concentration of a fluorescently labelled ligand and varying concentrations of the unlabeled test compound. Include controls for total binding (no competitor) and non-specific binding (NSB, with a high concentration of a known competitive inhibitor).
- Measurement: Incubate the plate to equilibrium, then measure fluorescence polarization.
- Analysis: Plot the FP signal against the logarithm of the competitor concentration and fit the data with a sigmoidal dose-response curve to determine the IC50 value.
B. Quantitative Microdialysis Validation
- Concentration Determination: Establish the appropriate concentration for the test compound using RP-HPLC or LC-MS. For LC-MS, a concentration range of 50-1500 nM is often suitable [59].
- Simulation: Simulate the dialysis process to determine the optimal target protein concentration that will maximize the concentration difference between chambers for accurate KD calculation [59].
- Equilibration in Absence of Protein: Using a rapid equilibrium dialysis (RED) device, incubate the test compound in assay buffer to confirm it equilibrates uniformly between chambers (partition coefficient, pc ~1.0) in the absence of protein over 6 hours [59].
- Binding Experiment: Load one chamber of the RED device with the target protein (at the predetermined concentration) and the test compound. Load the other chamber with buffer and compound only. Seal the device and incubate with orbital shaking for 6 hours at a controlled temperature.
- Sample Analysis: Collect samples from both chambers and analyze compound abundance using RP-HPLC or LC-MS. No protein precipitation is required prior to RP-HPLC analysis [59].
- KD Calculation: Use the provided software and equations to calculate the KD based on the measured compound concentrations in each chamber and the known total protein concentration [59].
Figure 1: A sequential workflow for cross-technique validation, beginning with high-throughput fluorescence assays and progressing to rigorous quantitative microdialysis and in vivo PET imaging for the most promising compounds.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Cross-Technique Experiments
| Item | Specification / Example (Catalog Number) | Function / Application |
|---|---|---|
| Rapid Equilibrium Dialysis (RED) Device | Reusable base plate (Thermo Fisher, Cat. no. 89811) & Inserts, 8.0 kDa (Thermo Fisher, Cat. no. 89809) [59] | Core device for performing quantitative microdialysis in vitro for protein-binding studies. |
| Microdialysis Probes | Custom-built with 4-mm active membrane (13-kDa MWCO, ~220 µm o.d.) [82] or commercial equivalents. | For in vivo sampling of neurotransmitters from specific brain regions in animal models. |
| PET Radiotracers | [11C]Raclopride, [18F]Fallypride (for dopamine D2/3 receptors); [11C]CIMBI-36 (for serotonin) [78] [79]. |
Radioactive ligands used to image and quantify receptor availability and neurotransmitter release in PET studies. |
| Assay Buffer | 145 mM NaCl, 2.8 mM KCl, 1.2 mM CaCl2, 1.2 mM MgCl2, 0.25 mM ascorbic acid, 5.4 mM D-glucose, pH 7.4 [82]. | Physiologically compatible buffer for in vivo microdialysis and in vitro assays to maintain biological activity. |
| Pluronic F127 | Low UV absorbance (Thermo Fisher, Cat. no. P6867) [59]. | Surfactant used to prevent nonspecific binding of compounds to equipment surfaces in microdialysis. |
| HPLC/MS Solvents | HPLC grade H2O and Acetonitrile (Sigma Aldrich, Cat. no. 34998); Formic acid (FA) for LCMS (Sigma Aldrich, Cat no. 5.33002) [59]. | High-purity solvents and additives for chromatographic separation and mass spectrometric detection of analytes. |
Data Integration and Analysis Framework
Successfully integrating data from multiple techniques requires a thoughtful analytical approach. The workflow diagram in Figure 1 outlines a logical progression. Key considerations for data integration include:
- Temporal Alignment: When correlating microdialysis and PET data, it is critical to align the time courses based on the pharmacokinetics of the challenge agent (e.g., amphetamine). The temporal resolution of each method must be accounted for, with PET providing a integrated measure over minutes and microdialysis offering discrete time points.
- Quantitative Bridging: Use parameters that are common across techniques. For example, the KD value determined by qµD in vitro [59] can be used to inform the interpretation of receptor occupancy measures derived from PET imaging in vivo [78].
- Spatial Concordance: When comparing microdialysis data from animals with PET data from humans or animals, ensure anatomical homology between the sampled brain regions. The recently published neurotransmitter atlas provides a crucial reference for comparing receptor densities and lesion locations across studies and modalities [79] [80].
Table 3: Addressing Technical Challenges in Cross-Technique Validation
| Challenge | Impact on Data | Mitigation Strategy |
|---|---|---|
| Microdialysis Probe Implantation Trauma | Can alter local neurotransmitter release and uptake, leading to underestimation of true extracellular concentrations [82]. | Allow for a sufficient post-surgical recovery period (e.g., 24-48 hrs). Use mathematical models that incorporate a "trauma layer" in data analysis [82]. |
| Differing Temporal Resolutions | Makes direct, moment-to-moment correlation of dynamic processes difficult. | Compare integrated responses over comparable time windows (e.g., area-under-the-curve for a pharmacological challenge). |
| Radiotracer vs. Endogenous Transmitter | PET measures displacement of a tracer, not the endogenous neurotransmitter concentration directly. | Use challenge paradigms with well-characterized mechanisms (e.g., amphetamine for dopamine). Validate with microdialysis in pre-clinical models. |
The integration of microdialysis, PET imaging, and fluorescence methods represents a powerful paradigm for advancing neuroscience research and CNS drug development. This Application Note provides a concrete foundation for researchers to design and implement cross-technique validation studies. By systematically combining the high temporal resolution of fluorescence, the precise biophysical data from quantitative microdialysis, and the non-invasive neurochemical mapping capabilities of PET, scientists can overcome the limitations inherent in any single method. This multi-faceted approach leads to a more robust, validated, and comprehensive understanding of brain chemistry, ultimately de-risking drug discovery and deepening our knowledge of brain function in health and disease.
Cerebral microdialysis is a cornerstone in vivo sampling technique in neuroscience research, enabling the monitoring of neurotransmitter dynamics and brain metabolism in live subjects [11]. By implanting a probe with a semi-permeable membrane into brain tissue, researchers can collect samples from the extracellular fluid to quantify the unbound, pharmacologically active fraction of neurochemicals and drugs [29] [83]. This technique provides critical insights for understanding brain function and developing central nervous system (CNS) therapeutics. However, its application is bound by several inherent methodological constraints. This Application Note delineates three principal limitations—temporal resolution, molecular size constraints, and tissue perturbation—within the context of neurotransmitter research. We provide a detailed analysis of these challenges, supported by quantitative data, and present validated experimental protocols and modern solutions to enhance the reliability and scope of microdialysis studies.
Limitations and Experimental Analysis
Temporal Resolution
Definition and Impact: Temporal resolution refers to the shortest time interval over which a meaningful change in analyte concentration can be detected. Traditional microdialysis systems are limited by the time required to collect sufficient sample volume for analysis, typically resulting in resolutions of 5-10 minutes, and often longer [11] [32]. This is insufficient for capturing the rapid, second-scale dynamics of neurotransmitter release and signaling that underlie fast cognitive processes and behaviors [32].
Key Factors and Optimization Data: The resolution is governed by perfusion flow rate, sample volume requirements of the analytical system, and the recovery efficiency of the probe. The table below summarizes the relationship between flow rate, recovery, and temporal resolution, and outlines modern approaches for improvement.
Table 1: Factors Affecting Temporal Resolution and Optimization Strategies
| Factor | Traditional Challenge | Optimization Strategy | Achievable Improvement |
|---|---|---|---|
| Flow Rate | Low flow (~0.3-1.0 µL/min) for high relative recovery; increases sample collection time [83]. | Use of segmented flow/droplet microfluidics to partition dialysate into nanoliter droplets [32]. | Enables collection of smaller volumes (3 nL) at rates up to 3 fractions per second [32]. |
| Analytical Method | Off-line analysis (e.g., HPLC) requires µL-volume samples, forcing longer collection intervals [11]. | Coupling to rapid, sensitive on-line analysis (e.g., direct ESI-MS/MS, capillary electrophoresis) [11] [32]. | Temporal resolution of seconds (e.g., 11 s) for multiplexed neurotransmitter monitoring [32]. |
| Recovery Efficiency | Analyte recovery is variable and flow-rate dependent, complicating quantification [11]. | System calibration (e.g., retrodialysis) for each experimental setup to define exact recovery [29]. | Ensures accurate quantification despite rapid sampling, validating high-resolution data [29]. |
Molecular Size Constraints
Definition and Impact: The molecular weight cut-off (MWCO) of the probe's membrane dictates the size range of molecules that can be sampled. While standard membranes (e.g., 20 kDa) are adequate for classic neurotransmitters (e.g., glutamate, dopamine), they exclude larger neuropeptides, cytokines, and growth factors critical for understanding neuroinflammation and other complex processes [84] [85].
Key Factors and Optimization Data: The recovery of large molecules is challenged by their low aqueous diffusion coefficients, high mass transport resistance, and nonspecific binding to the microdialysis system components (tubing, membrane) [29] [85]. The following table compares probe types and solutions for large molecule microdialysis.
Table 2: Microdialysis Setups for Different Molecular Sizes
| Target Analyte Size | Recommended Probe MWCO | Key Challenges | Recommended Solutions |
|---|---|---|---|
| Small Molecules (e.g., Glucose, Lactate, Glutamate) | 6 - 20 kDa [83] [11] | Limited primarily by temporal resolution. | Standard setups with artificial cerebrospinal fluid (aCSF) perfusate and low flow rates (0.3 µL/min) [83]. |
| Hydrophobic Drugs (e.g., Selinexor, Ulixertinib) | 20 - 100 kDa | Pronounced non-specific binding (NSB) to system components, leading to low recovery and carry-over [29]. | Use of surface-coated tubing/membranes; adding carriers like BSA (0.5-1.5%) or DMSO (0.01-0.1%) to perfusate to minimize NSB [29]. |
| Large Molecules (e.g., Cytokines, Neuropeptides, Amyloid-β) | 55 kDa - 3 MDa [84] [85] | Low relative recovery; ultrafiltration causing net fluid loss [84] [85]. | For 55-100 kDa: Use dextran (500 kDa, 3%) in perfusate to stabilize pressure [84]. For 500 kDa-2 MDa: Use push-pull peristaltic pump set-ups to manage flow and pressure [84]. |
Tissue Perturbation
Definition and Impact: The implantation of a microdialysis probe (200-300 µm in diameter) causes inevitable physical damage to the brain parenchyma [11]. This trauma initiates a series of events—including the rupture of blood vessels and the blood-brain barrier (BBB), triggering of inflammatory responses, and reactive gliosis—which can confound experimental findings by altering the local neurochemical environment being measured [11].
Key Factors and Optimization Data: The foreign body response creates a concentric gradient of damaged cells extending up to 250 µm from the probe track, which can significantly distort measurements, especially in the delicate structures of rodent brains [11]. The following table outlines the causes and mitigation strategies.
Table 3: Tissue Perturbation and Mitigation Strategies
| Aspect of Perturbation | Consequence | Evidence-Based Mitigation Strategy |
|---|---|---|
| Initial Physical Trauma | Direct tissue damage and BBB disruption during insertion [11]. | Allow for a postsurgical equilibration period (often 24 hours); discard the first hour of sample post-insertion to avoid acute insertion artifacts [83]. |
| Chronic Foreign Body Response | Gliosis forms a physical barrier around the probe, impeding analyte diffusion and reducing recovery over time [11]. | Miniaturization of probes; local administration of anti-inflammatory agents (e.g., retrodialysis of dexamethasone) to suppress glial scarring [11]. |
| Probe Size vs. Brain Anatomy | Standard probes greatly exceed the intercapillary distance in rodent brains (~30 µm), causing widespread vascular damage [11]. | Use of flexible, miniaturized probes to minimize tissue displacement and damage, thereby improving long-term signal stability [86]. |
Detailed Experimental Protocols
Protocol: Retrodialysis for Recovery Calibration of Hydrophobic Compounds
This protocol is critical for obtaining accurate quantitative data, especially for drugs prone to non-specific binding [29].
- Probe Preparation: Immerse the microdialysis probe (e.g., CMA7 or CMA8) in a stirred blank Ringer's solution maintained at 37°C. The solution should be supplemented with 0.5%–1.5% Bovine Serum Albumin (BSA). For extremely hydrophobic compounds like ulixertinib, 0.01% or 0.1% DMSO may be added [29].
- Perfusion with Drug Solution: Perfuse the probe with a solution of the drug of interest (e.g., at 100 ng/mL) at a low flow rate of 0.5 µL/min using a precision syringe pump [29].
- Equilibration: Allow the system to equilibrate for a sufficient period to ensure stable diffusion.
- Sample Collection: Collect three consecutive dialysate fractions at defined intervals (e.g., 1 hour). Immediately store the samples at -80°C to prevent degradation prior to analysis [29].
- Calculation of Relative Recovery (RR): Calculate the recovery using the retrodialysis formula, which assumes the diffusion rate out of the probe is equivalent to the diffusion rate into the probe [29].
> RR = (Cperfusate - Cdialysate) / C_perfusate
> Where
C_perfusateis the known concentration of the drug in the perfusate, andC_dialysateis the measured concentration in the collected sample. The actual extracellular concentration (C_ECF) can then be estimated as:C_ECF = C_dialysate / RR[29].
Protocol: Assessing Non-Specific Binding (NSB) to System Components
This preparatory experiment is essential before in vivo studies with hydrophobic molecules [29].
- Solution Preparation: Prepare a solution with a known concentration of the drug (e.g., 100 ng/mL) in Ringer's solution [29].
- Tubing Adsorption Test:
- Load the solution into a glass syringe.
- Pump the solution through a 1-meter long tubing system (e.g., FEP or PEEK) at 0.5 µL/min.
- Collect samples at the outlet at three time points over 3 hours (T1-T3). Also, collect samples directly from the syringe before (S1) and after (S2) perfusing the tubing [29].
- Carry-Over Test:
- Clean the syringes and refill with blank Ringer's solution (without drug).
- Repeat the pumping and sampling process (T4-T6, S3, S4) [29].
- Analysis and Calculation:
- Quantify drug concentrations in all samples using UPLC-MS/MS.
- Calculate recovery rates for the adsorption test:
Recovery = (C_sample / C_S1) * 100. - The presence of the drug in T4-T6 samples indicates significant carry-over effect [29].
The workflow below illustrates the logical decision process for selecting appropriate materials and methods to overcome the key limitations discussed.
The Scientist's Toolkit: Research Reagent Solutions
Selecting the appropriate materials is fundamental to designing a successful microdialysis experiment. The following table lists key solutions and their specific functions in addressing common methodological challenges.
Table 4: Essential Research Reagents and Materials for Microdialysis
| Item Name | Function & Application |
|---|---|
| Perfusion Fluid CNS with Dextran 500 kDa 3% | Sterile, non-buffered perfusate additive. Used with high cut-off probes (55-100 kDa) to stabilize intracapillary pressure via osmosis, thereby limiting ultrafiltration and improving fluid recovery close to 100% [84]. |
| CMA 7 / CMA 11 Probes (2 MDa) | Ultra-high cut-off microdialysis probes for rats and mice. Designed for sampling very large molecules like proteins, cytokines, and antibodies. Require specialized push-pull set-ups to function optimally [84]. |
| REGLO ICC Digital Peristaltic Pump | A 12-roller peristaltic pump capable of accurate flow rates as low as 0.1 µL/min. Essential for push-pull set-ups with ultra-high cut-off probes to ensure smooth flow and prevent backpressure-related ultrafiltration [84]. |
| Bovine Serum Albumin (BSA) | A protein carrier added to the perfusate (at 0.5%-1.5%) to saturate non-specific binding sites on tubing and the membrane. Critical for improving the recovery of hydrophobic drugs [29]. |
| Anti-Inflammatory Agents (e.g., Dexamethasone) | Administered via retrodialysis (reverse delivery through the probe) to locally suppress the glial scar formation around the implanted probe, thereby extending its functional lifespan and improving recovery stability [11]. |
| Flexible, Multifunctional Fiber Probes | Innovative probes that integrate microdialysis with electrophysiological recording capabilities. Their flexibility minimizes tissue damage during implantation and ensures longer-term stability for chronic studies [86]. |
The limitations of temporal resolution, molecular size constraints, and tissue perturbation are inherent to the microdialysis technique but not insurmountable. As detailed in this application note, a mechanistic understanding of these challenges allows researchers to select appropriate strategies—such as adopting droplet microfluidics for second-scale resolution, employing dextran-containing perfusate for large molecules, and utilizing flexible probes with anti-inflammatory treatments to mitigate tissue damage. The experimental protocols and toolkit provided herein offer a practical framework for optimizing microdialysis set-ups. By systematically addressing these limitations, scientists can enhance the quality and translational value of their in vivo neurotransmitter research, thereby accelerating drug development for CNS disorders.
Conclusion
In vivo microdialysis stands as an indispensable, versatile technique that provides direct access to pharmacologically active, unbound neurotransmitter concentrations in the brain, offering unparalleled insights for neuropharmacology and drug discovery. Its unique capability for continuous monitoring in behaving animals, combined with advanced analytical methods like LC-MS/MS, allows for a sophisticated understanding of drug mechanisms and disease pathophysiology. Future directions point toward more integrated, multi-omics approaches using microdialysis for metabolomic fingerprints, further miniaturization for probing smaller brain nuclei, and expanded clinical translation to monitor neurochemistry in human patients, solidifying its role in the development of next-generation neurotherapeutics.
References
- 1. The principle of microdialysis [https://www.mdialysis.com/us/about-us/the-principle-of-microdialysis/]
- 2. Microdialysis - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/microdialysis]
- 3. 1.1. Basic Principles and Advantages of microdialysis [https://bio-protocol.org/exchange/minidetail?id=18911138&type=30]
- 4. Microdialysis Education [https://microdialysis.com/microdialysis-education.html]
- 5. In Depth Chemical Analysis of Brain Extracellular Space using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12117515/]
- 6. 2.5. Measurement of brain monoaminergic ... [https://bio-protocol.org/exchange/minidetail?id=87419&type=30]
- 7. Benefits of Using an Autosampler in Microdialysis [https://www.news-medical.net/life-sciences/Benefits-of-Using-an-Autosampler-in-Microdialysis.aspx]
- 8. What Is Brain Microdialysis and Its Application in PK ... [https://dmpkservice.wuxiapptec.com/articles/467-what-is-brain-microdialysis-and-its-application-in-pk-studies-for-cns-drugs/]
- 9. Microdialysis [https://en.wikipedia.org/wiki/Microdialysis]
- 10. Microdialysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1122512/]
- 11. Microdialysis - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/microdialysis]
- 12. Overview of Brain Microdialysis - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2953244/]
- 13. Microdialysis - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/chemistry/microdialysis]
- 14. Establishing In-vivo brain microdialysis for comparing ... [https://pubmed.ncbi.nlm.nih.gov/39798806/]
- 15. Analytical considerations for microdialysis sampling [https://www.sciencedirect.com/science/article/abs/pii/S0169409X00001149]
- 16. Microdialysis as a tool in local pharmacodynamics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3231563/]
- 17. In vivo brain microdialysis: advances in ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3083031/]
- 18. Systems Pharmacology: Network Analysis to Identify ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3619403/]
- 19. Estimating neurotransmitter kinetics with ntPET - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2271120/]
- 20. A Systems-Based Paradigm-DrivenMulti-Target Drug ... [https://www.healthcare-bulletin.co.uk/article/network-pharmacology-a-systems-based-paradigm-drivenmulti-target-drug-discovery-development-3872/]
- 21. Recent trends in microdialysis sampling integrated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3744124/]
- 22. Dialysis Membrane - an overview [https://www.sciencedirect.com/topics/materials-science/dialysis-membrane]
- 23. Separation Characteristics of Dialysis Membranes [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/protein-biology-application-notes/separation-characteristics-dialysis-membranes.html]
- 24. Molecular weight cut-off [https://en.wikipedia.org/wiki/Molecular_weight_cut-off]
- 25. Protocol for evaluating neuronal activity and ... [https://pubmed.ncbi.nlm.nih.gov/40131934/]
- 26. Protocol for evaluating neuronal activity and ... [https://www.sciencedirect.com/science/article/pii/S2666166725001182]
- 27. 2.2. Guide cannula implantation and intra-BNST drug ... [https://bio-protocol.org/exchange/minidetail?id=7180130&type=30]
- 28. Intracranial Cannular Implantation in a Mouse to Deliver ... [https://www.jove.com/v/30937/intracranial-cannular-implantation-mouse-to-deliver-therapeutic]
- 29. Experimental Insights and Recommendations for Successfully ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12033007/]
- 30. Microdialysis Calibration Using Retrodialysis and Zero-Net ... [https://link.springer.com/article/10.1023/A:1018906821725]
- 31. Quantitative monitoring and modelling of retrodialysis drug ... [https://www.nature.com/articles/s41598-023-28915-3]
- 32. Microdialysis coupled with droplet microfluidics and mass ... [https://pubs.rsc.org/en/content/articlelanding/2024/an/d4an00112e]
- 33. The High-Precision Liquid Chromatography with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10818480/]
- 34. Electrochemical detection for HPLC [https://antecscientific.com/products/techniques/electrochemical-detection/]
- 35. Benefits of using HPLC-ECD for Neurotransmitter Detection [https://www.amuzainc.com/blog/benefits-of-using-hplc-ecd-for-neurotransmitter-detection/?srsltid=AfmBOorpiNg8REI6ako2gfHjxQS2rN3lbSY3KhdzlnRaMZ0YJrhFZLpM]
- 36. LC-MS-MS | Liquid Chromatography [https://www.eag.com/app-note/liquid-chromatography-tandem-mass-spectrometry-lc-ms-ms/]
- 37. LC-MS Sample Preparation [https://www.thermofisher.com/us/en/home/industrial/mass-spectrometry/mass-spectrometry-learning-center/liquid-chromatography-mass-spectrometry-lc-ms-information/lc-ms-sample-preparation.html]
- 38. A practical guide to sample preparation for liquid ... [https://www.spectroscopyeurope.com/article/practical-guide-sample-preparation-liquid-chromatography-tandem-mass-spectrometry-clinical]
- 39. A derivatization and validation strategy for determining the ... [https://pubmed.ncbi.nlm.nih.gov/25044893/]
- 40. Microdialysis Techniques in Neuroscience [https://link.springer.com/book/10.1007/978-1-62703-173-8]
- 41. A soft neural interface with a tapered peristaltic micropump ... [https://www.nature.com/articles/s41528-025-00463-y]
- 42. Impact of Neurodegenerative Diseases on Drug Binding to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6095788/]
- 43. Animal Models of Neurodegenerative Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6615039/]
- 44. Emerging hiPSC Models for Drug Discovery in ... [https://www.mdpi.com/1422-0067/22/15/8196]
- 45. Antidepressant activity: contribution of brain microdialysis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3737470/]
- 46. Methods and issues in microdialysis calibration [https://www.sciencedirect.com/science/article/abs/pii/S0003267098005984]
- 47. Adsorption of xenobiotics to plastic tubing incorporated into ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961200003896]
- 48. Sorption and release of small molecules in PDMS ... [https://www.nature.com/articles/s41598-025-97111-2]
- 49. Loss of lipid to plastic tubing [https://www.sciencedirect.com/science/article/pii/S0022227520394840]
- 50. Cerebral microdialysis in clinical studies of drugs [https://pmc.ncbi.nlm.nih.gov/articles/PMC3663257/]
- 51. Use of osmotic agents in microdialysis studies to improve ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354916312825]
- 52. An In Vivo Microdialysis Study of FLZ Penetration through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4090575/]
- 53. Physiology, Cerebral Spinal Fluid - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK519007/]
- 54. Microdialysis - In Vivo System for Neurotransmitter Recovery [https://www.amuzainc.com/what-is-microdialysis/?srsltid=AfmBOooCU8tNLL4urxosQeTLxMwnduwbUICG6dt_rGWJjjQLia7KwKI9]
- 55. Pharmacological Mitigation of Tissue Damage During ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3799822/]
- 56. Neurochemical in vivo microdialysis and postmortem tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S0197018625000798]
- 57. Calibration methods for microdialysis sampling in vivo [https://www.sciencedirect.com/science/article/abs/pii/S0003267099006133]
- 58. Experimental and numerical investigation of microdialysis ... [https://pubs.rsc.org/en/content/articlehtml/2024/ay/d4ay00699b]
- 59. Quantitative Microdialysis: Experimental Protocol and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7563421/]
- 60. Microdialysis and microperfusion electrodes in neurologic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8638547/]
- 61. Push-Pull Perfusion - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/push-pull-perfusion]
- 62. Simultaneous comparison of cerebral dialysis and push-pull ... [https://pubmed.ncbi.nlm.nih.gov/9579326/]
- 63. Comparison of microdialysis and push-pull perfusion for ... [https://pubmed.ncbi.nlm.nih.gov/12814843/]
- 64. Push-Pull Perfusion - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/push-pull-perfusion]
- 65. Impact of protein binding on drug sampling by ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725004411]
- 66. Changes in Neurotransmitter Extracellular Levels during ... [https://www.ncbi.nlm.nih.gov/books/NBK3921/]
- 67. Sources Contributing to the Average Extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3323736/]
- 68. Detection of Neuronal Glutamate in Brain Extracellular Space ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418293/]
- 69. Pharmacokinetic-Pharmacodynamic Modeling of Brain ... [https://www.sciencedirect.com/science/article/abs/pii/S0022356524259656]
- 70. Pattern Recognition in Pharmacodynamic Data Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7583549/]
- 71. Microdialysis and the Neurochemistry of Addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2659871/]
- 72. New perspectives from microdialysis studies in freely- ... [https://pubmed.ncbi.nlm.nih.gov/18456311/]
- 73. New perspectives from microdialysis studies in freely ... [https://www.sciencedirect.com/science/article/abs/pii/S0091305708001032]
- 74. Multisite Intracerebral Microdialysis to Study the Mechanism of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3656765/]
- 75. Microdialysis in Parkinsonian Patient Basal Ganglia [https://pubmed.ncbi.nlm.nih.gov/11161624/]
- 76. Using microdialysis to monitor dopaminergic support of ... [https://www.sciencedirect.com/science/article/abs/pii/S0166432824002778]
- 77. An Update of the Classical and Novel Methods Used for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4428024/]
- 78. Methods for Quantifying Neurotransmitter Dynamics in the ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2020.00792/full]
- 79. Mapping neurotransmitter systems to the structural and ... [https://www.nature.com/articles/s41593-022-01186-3]
- 80. Neurotransmitters' white matter mapping unveils the ... [https://www.nature.com/articles/s41467-025-57680-2]
- 81. Exploring Neurotransmitters through In Vivo vs. In Vitro ... [https://www.mdpi.com/1424-8220/24/2/647]
- 82. Microdialysis of dopamine interpreted with quantitative model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2386091/]
- 83. An overview of clinical cerebral microdialysis in acute brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9989027/]
- 84. NEW! Solutions for Microdialysis of Large Molecules [https://microdialysis.com/new-solution-microdialysis-large-molecule-1309.html]
- 85. Microdialysis of Large Molecules [https://www.sciencedirect.com/science/article/abs/pii/S0022354916416795]
- 86. Physics of Neural Systems III | APS SMT 2025 Meeting [https://schedule.aps.org/smt/2025/events/MAR-M73/13]