LC-MS/MS Method Development and Validation for Quantifying Drug Concentrations in Human Plasma: A Comprehensive Guide for Clinical and Pharmaceutical Research
This article provides a comprehensive guide to the development, optimization, and validation of Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) methods for the precise quantification of drug concentrations in human plasma.
LC-MS/MS Method Development and Validation for Quantifying Drug Concentrations in Human Plasma: A Comprehensive Guide for Clinical and Pharmaceutical Research
Abstract
This article provides a comprehensive guide to the development, optimization, and validation of Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) methods for the precise quantification of drug concentrations in human plasma. Tailored for researchers, scientists, and drug development professionals, it covers foundational principles, practical methodological applications across various drug classes (including antibiotics, antivirals, and anticancer agents), advanced troubleshooting strategies, and rigorous validation protocols per FDA and EMA guidelines. By synthesizing the latest research and practical insights, this resource supports critical activities in therapeutic drug monitoring (TDM), pharmacokinetic studies, and clinical pharmacology, enabling enhanced analytical robustness and patient-specific therapy optimization.
LC-MS/MS Fundamentals: Principles and Role in Modern Bioanalysis
Liquid Chromatography coupled with Tandem Mass Spectrometry (LC-MS/MS) has become an indispensable technique in modern bioanalysis, particularly for the quantification of drugs and their metabolites in biological matrices such as plasma. The power of this technique lies in the synergistic combination of two powerful components: the high-resolution separation capability of High-Performance Liquid Chromatography (HPLC) and the exceptional sensitivity and specificity of the triple quadrupole mass spectrometer. This combination is especially crucial in pharmaceutical and clinical research, where precise measurement of drug concentrations is essential for pharmacokinetic studies, therapeutic drug monitoring, and bioequivalence assessments [1].
The application of LC-MS/MS for quantifying drug concentrations in plasma has revolutionized drug development by enabling researchers to detect and measure minute amounts of analytes amidst complex biological matrices. The triple quadrupole configuration, operating in Multiple Reaction Monitoring (MRM) mode, provides the selectivity required to distinguish target analytes from endogenous compounds in plasma, while the HPLC system effectively separates analytes from potential interferents prior to mass spectrometric detection [2] [3]. This article details the core components of an LC-MS/MS system and provides detailed protocols for its application in plasma drug quantification research.
Core Component 1: High-Performance Liquid Chromatography (HPLC)
Function and Role in LC-MS/MS
The HPLC system serves as the front-end separation component of the LC-MS/MS system, with the primary function of resolving the complex mixture of compounds present in biological samples like plasma. Without effective chromatographic separation, ion suppression or enhancement can occur in the mass spectrometer ion source due to co-eluting matrix components, compromising the accuracy and precision of quantification [1]. The HPLC system delivers the sample to the mass spectrometer in a purified form and in a solvent compatible with the ionization process.
A typical HPLC system for bioanalytical applications includes: a solvent delivery system (pumps), autosampler, column oven, and a analytical column. Modern systems often employ UHPLC (Ultra-High-Performance Liquid Chromatography) technology, which operates at higher pressures and uses smaller particle size columns (<2 μm) to achieve faster analysis times and improved chromatographic resolution [4] [5].
HPLC Method Parameters for Plasma Analysis
Table 1: Typical HPLC Conditions for Plasma Drug Quantification
| Parameter | Typical Specification | Application Example |
|---|---|---|
| Column Type | Reversed-Phase C18 | Ascentis Express AQ-C18 (150 × 3 mm, 5 μm) [5] |
| Column Temperature | 30-40°C | 40°C [5] |
| Mobile Phase | Aqueous buffer + Organic modifier | 0.1% Formic acid in water / Acetonitrile [4] |
| Flow Rate | 0.2-0.6 mL/min | 0.3 mL/min [5] |
| Injection Volume | 5-50 μL | 10 μL [5] |
| Gradient/Isocratic | Gradient or Isocratic elution | 100% Aqueous isocratic method [5] |
| Run Time | 3-10 minutes | 5 minutes [5] |
Core Component 2: Triple Quadrupole Mass Spectrometry
Instrument Configuration and Principle of Operation
The triple quadrupole mass spectrometer forms the detection heart of the LC-MS/MS system and is responsible for the exceptional specificity and sensitivity of the technique. As the name implies, it consists of three consecutive quadrupole mass analyzers, designated Q1 (first quadrupole), Q2 (collision cell), and Q3 (second quadrupole) [2] [3]. Each quadrupole consists of four parallel metal rods that act as mass filters by applying specific DC and RF voltages, allowing only ions of a specific mass-to-charge ratio (m/z) to pass through at any given time [1].
The analytical power of this configuration comes from the two stages of mass filtration separated by a fragmentation stage. In the first quadrupole (Q1), precursor ions (typically the protonated [M+H]+ or deprotonated [M-H]- molecules of the target analyte) are selected. These precursor ions are then transmitted to the second quadrupole (Q2), which functions as a collision cell filled with an inert gas such as nitrogen or argon. Here, the precursor ions undergo Collision-Induced Dissociation (CID), fragmenting into product ions [2] [3]. The resulting fragment ions are then analyzed in the third quadrupole (Q3), where a specific product ion is selected for detection. This two-stage mass filtering process provides unparalleled specificity for quantitative analysis [1].
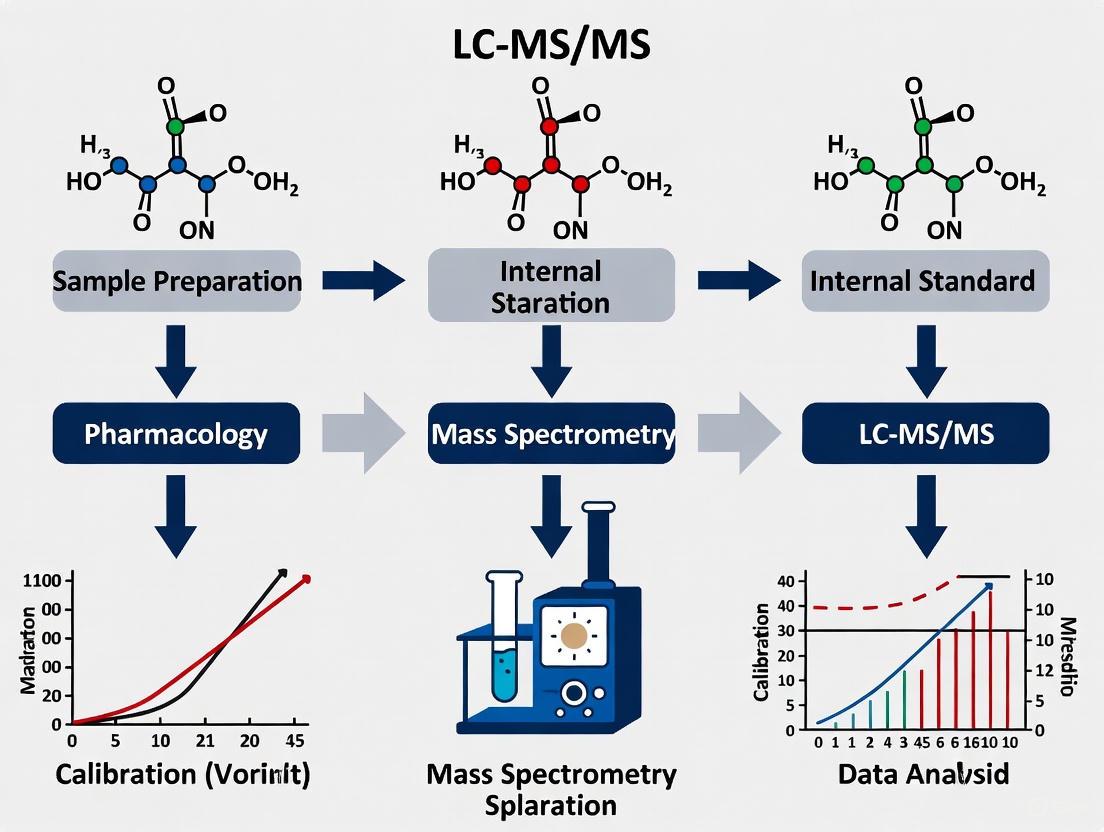
Diagram 1: LC-MS/MS System Workflow. The process begins with sample introduction and LC separation, followed by ionization, two stages of mass selection with intermediate fragmentation, and finally detection.
The interface between the HPLC and the mass spectrometer is the ionization source, which converts analyte molecules into gas-phase ions. The most common ionization techniques for bioanalytical applications are:
Electrospray Ionization (ESI): A "soft" ionization technique where the LC eluent is nebulized and charged at the tip of a metal capillary under high voltage (3-5 kV), creating a fine spray of charged droplets. As the solvent evaporates, the charge is transferred to the analyte molecules. ESI is highly effective for a wide range of polar to moderately polar molecules, including many pharmaceuticals and their metabolites [1]. It can generate both positive ions (M+H)+ and negative ions (M-H)-, with switching between modes possible within milliseconds [2].
Atmospheric Pressure Chemical Ionization (APCI): Similar to ESI, the LC eluent is nebulized, but ionization occurs in the gas phase through interactions with solvent ions created by a corona discharge. APCI is particularly useful for less polar, thermally stable compounds that do not ionize well by ESI [1].
Operational Modes and Multiple Reaction Monitoring (MRM)
The triple quadrupole mass spectrometer can operate in several different modes, but for quantitative bioanalysis of drugs in plasma, the Multiple Reaction Monitoring (MRM) mode is the gold standard [2] [3]. In MRM, both Q1 and Q3 are set to transmit specific m/z values rather than scanning across a mass range. Q1 is set to transmit the precursor ion of the target analyte, while Q3 is set to transmit a specific, characteristic product ion formed in the collision cell [1]. This dual mass filtering dramatically reduces chemical noise from the complex plasma matrix, resulting in significantly improved signal-to-noise ratios and lower limits of quantification.
Table 2: Triple Quadrupole Operational Modes
| Mode | Q1 Function | Q2 Function | Q3 Function | Primary Application |
|---|---|---|---|---|
| MRM (Multiple Reaction Monitoring) | Fixed on precursor ion | CID Fragmentation | Fixed on product ion | High-sensitivity quantification [2] [3] |
| Product Ion Scan | Fixed on precursor ion | CID Fragmentation | Scans all product ions | Structural elucidation [2] |
| Precursor Ion Scan | Scans all precursors | CID Fragmentation | Fixed on product ion | Finding all precursors that form a common fragment [2] |
| Neutral Loss Scan | Scans all precursors | CID Fragmentation | Scans with offset | Finding all precursors that lose a common neutral mass [2] |
The specificity of MRM is demonstrated by the concept of a "mass transition" - the specific precursor ion to product ion pair monitored for each analyte. For example, in a method for quantifying fosmidomycin, the mass transition monitored was m/z 181.9 → 135.9, where 181.9 is the m/z of the precursor ion and 135.9 is the m/z of the characteristic product ion used for quantification [5]. This specific transition provides a unique identifier for the target analyte, distinguishing it from other components in the plasma matrix.
Detailed Protocol: LC-MS/MS Method for Quantifying Drugs in Plasma
This protocol outlines the development and validation of an LC-MS/MS method for quantifying drug concentrations in plasma, based on established approaches in the literature [4] [5] [6].
Sample Preparation: Protein Precipitation
Protein precipitation is a simple and efficient sample clean-up technique for plasma samples.
- Aliquot Plasma Samples: Transfer 20 μL of calibration standard, quality control sample, or unknown patient sample into a microcentrifuge tube.
- Add Internal Standard: Add 80 μL of internal standard (IS) solution. The IS, typically a stable isotope-labeled analog of the analyte, corrects for variability in sample preparation and ionization efficiency [5].
- Precipitate Proteins: Add 50 μL of 10% Trichloroacetic Acid (TCA) in water. Vortex the mixture for 10 seconds to ensure complete protein precipitation [5].
- Centrifuge: Centrifuge the samples at 4°C for 20 minutes at 17,968 × g to pellet the precipitated proteins [5].
- Transfer Supernatant: Carefully transfer 80 μL of the clear supernatant to an HPLC vial for analysis. Store vials at 4°C in the autosampler until analysis.
LC-MS/MS Instrumental Analysis
HPLC Conditions:
- Column: Maintain a reversed-phase column (e.g., Biphenyl or C18, 150 × 3.0 mm, 5 μm) at 40°C [4] [5].
- Mobile Phase: Utilize a binary system. Mobile Phase A: 0.1% formic acid in water; Mobile Phase B: acetonitrile [4].
- Flow Rate: 0.3 mL/min [5].
- Injection Volume: 10 μL [5].
- Gradient Program: Implement an appropriate gradient or isocratic method. For fosmidomycin, a 100% aqueous isocratic method with 10 mM ammonium formate containing 0.1% formic acid was used with a 5-minute run time [5].
Mass Spectrometry Conditions:
- Ionization Mode: Electrospray Ionization (ESI) in positive or negative mode, optimized for the target analyte [5].
- Ion Source Parameters: Optimize temperature, nebulizer gas, and drying gas flows.
- MRM Transitions: Define the specific precursor ion → product ion transitions for the analyte and internal standard. For example, for alvocidib quantification, positive ESI mode was used with MRM [4].
- Collision Energy: Optimize the collision energy for each transition to maximize product ion signal.
Method Validation
According to regulatory guidelines (e.g., EMA), the method must be validated for [5]:
- Selectivity: Demonstrate no significant interference from blank plasma at the retention times of the analyte and IS.
- Linearity and LLOQ: Establish a calibration curve (e.g., 0.25-15 mg/L for fosmidomycin) with a Lower Limit of Quantification (LLOQ) where accuracy and precision are within ±20% [5].
- Accuracy and Precision: Evaluate intra-day and inter-day accuracy (85-115% of nominal values) and precision (CV <15%) [5].
- Matrix Effect: Assess the influence of the plasma matrix on ionization efficiency. The variability should not exceed 15% CV [5].
- Stability: Confirm analyte stability under various conditions (bench-top, freeze-thaw, long-term storage) [4].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for LC-MS/MS Bioanalysis
| Item | Function | Example Application |
|---|---|---|
| HPLC-grade Water/ACN | Mobile phase components | Provides clean baseline and efficient chromatography [5] |
| Formic Acid / Ammonium Formate | Mobile phase additives | Enhances analyte ionization and controls pH [5] |
| Reversed-Phase Column (C18, Biphenyl) | Analytical separation | Separates analytes from matrix interferences [4] [5] |
| Stable Isotope-Labeled Internal Standard | Quantification control | Corrects for sample prep and ionization variability [5] |
| Protein Precipitation Solvent (TCA, ACN) | Sample clean-up | Removes proteins from plasma samples [5] |
| Blank Human/Rat Plasma | Matrix for standards/QC | Maintains consistent matrix effects between samples [5] |
| KM04416 | KM04416, MF:C12H11NO3S, MW:249.29 g/mol | Chemical Reagent |
| ELA-14 (human) | ELA-14 (human), MF:C75H119N25O17S2, MW:1707.0 g/mol | Chemical Reagent |
Application in Pharmacokinetic Studies
The developed and validated LC-MS/MS method can be applied to quantify drug concentrations in plasma samples from pharmacokinetic studies. After administering the drug to subjects (human or animal), blood samples are collected at predetermined time points. The plasma is separated and processed according to the established protocol [4] [5]. The resulting concentration-time data allows researchers to calculate critical pharmacokinetic parameters such as C~max~, T~max~, AUC, and half-life, which are essential for understanding the drug's absorption, distribution, metabolism, and excretion (ADME) profile [4]. For instance, an LC-MS/MS method was successfully applied to study the tissue distribution of alvocidib in rats, revealing differential distribution of the parent drug and its glucuronide metabolite across various tissues [4].
The LC-MS/MS system, with its core components of HPLC for separation and triple quadrupole mass spectrometry for detection, provides an exceptionally powerful platform for the quantification of drugs in plasma. The robustness, sensitivity, and specificity offered by this technology, particularly when operated in MRM mode, make it the method of choice in modern bioanalytical laboratories supporting drug development and clinical research. The detailed protocols and guidelines presented in this application note provide a framework for researchers to develop and implement reliable LC-MS/MS methods for their pharmacokinetic and bioanalysis studies.
This application note details the synergistic combination of Electrospray Ionization (ESI) and Multiple Reaction Monitoring (MRM) for achieving superior sensitivity in the quantification of drug concentrations in plasma. Within the context of LC-MS/MS method development, this targeted proteomics approach provides the high selectivity and robust quantification necessary for critical applications in drug development, such as pharmacokinetic studies and therapeutic drug monitoring. We summarize key performance data, provide detailed experimental protocols, and visualize the underlying mechanisms that make this technology a cornerstone of modern bioanalysis.
The quantification of low-abundance therapeutics and biomarkers in complex biological matrices like plasma presents a significant analytical challenge due to the wide dynamic range of protein concentrations and the presence of interfering substances. While immunoassays have traditionally been used, they are often expensive, time-consuming to develop, and lack multiplexing capabilities [7]. Liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) operating in MRM mode, with ESI as the ionization source, has emerged as a powerful alternative. The dual mass filtering inherent to MRM on a triple quadrupole mass spectrometer, combined with the efficient ion production of ESI for liquid samples, creates a highly specific and sensitive platform for quantitative analysis [8]. This note explores the mechanisms behind this sensitivity and provides a practical framework for its application in plasma drug quantification.
Fundamental Mechanisms and Key Enhancements
Principles of ESI and MRM
The sensitivity of the combined ESI-MRM platform stems from its coherent multi-stage process:
Electrospray Ionization (ESI): ESI functions as a critical front-end, efficiently generating gas-phase ions from the liquid chromatographic eluent at atmospheric pressure. It is particularly adept at ionizing a wide range of biomolecules, including peptides and drugs, making it ideal for bioanalysis [9]. The production of multiple-charged ions further enhances detection capabilities for larger molecules.
Multiple Reaction Monitoring (MRM): MRM on a triple quadrupole mass spectrometer provides exceptional specificity through two stages of mass selection. The first quadrupole (Q1) selects a specific precursor ion corresponding to the target analyte. This ion is then fragmented in the second quadrupole (Q2) via collision-induced dissociation, and a unique product ion is selected in the third quadrupole (Q3) for detection. This specific pair of precursor and product ions is known as a "transition" [7] [8]. By monitoring this transition, the method effectively filters out chemical noise from the complex plasma matrix, leading to a significant gain in signal-to-noise ratio and, consequently, sensitivity.
Technological Advances for Enhanced Sensitivity
A major bottleneck for SRM/MRM technology has been insufficient sensitivity for detecting low-abundance proteins or drugs, which can be present at low ng/mL to pg/mL concentrations in plasma [7]. Recent advances have directly addressed this challenge:
Ion Funnel Technology: The introduction of a multi-capillary inlet/dual-stage electrodynamic ion funnel interface has dramatically enhanced ion transmission efficiency from the ESI source to the mass analyzer. This innovation has been shown to increase average SRM peak intensities by approximately 70-fold and improve the limit of detection for peptides by about 10-fold in complex matrices like mouse plasma [10]. This enhancement allows for the detection of proteins in the 40 to 80 ng/mL range without the need for extensive front-end sample fractionation [10].
Front-End Sample Processing: To further improve sensitivity, various sample preparation strategies are employed to reduce matrix complexity and enrich target analytes. These include:
- Immunoaffinity Depletion: Removal of high-abundance plasma proteins to reveal lower-abundance targets [7].
- Fractionation: Techniques like strong cation exchange (SCX) chromatography to simplify the sample [7].
- Targeted Enrichment: Using antibodies to selectively isolate specific proteins or peptides of interest, which can push quantification limits to the low ng/mL range [7].
The logical relationship and workflow integrating these components for superior sensitivity are illustrated below.
Sensitivity Enhancement Workflow in LC-ESI-MRM
Quantitative Performance Data
The following table summarizes reported limits of quantification (LOQ) for targeted proteins in blood plasma and serum using different SRM/MRM strategies, demonstrating the impact of various sensitivity-enhancement approaches.
Table 1: Reported Limits of Quantification (LOQ) in Plasma/Serum Using SRM/MRM
| Instrumentation Platform | Enrichment Method | Reported LOQ | Reference |
|---|---|---|---|
| NanoLC-SRM with standard interface | None | ~1 μg/mL | [7] |
| NanoLC-SRM with standard interface | None | 15-168 ng/mL | [7] |
| LC-SRM with dual ion funnel interface | None | 40-80 ng/mL | [10] |
| LC-SRM (various platforms) | Immunoaffinity depletion & fractionation | Low ng/mL range | [7] |
Experimental Protocol: MRM-Based Quantification of a Drug in Plasma
This protocol outlines a generalized procedure for developing and applying an LC-ESI-MRM method for quantifying a small molecule drug in plasma, incorporating best practices for achieving high sensitivity.
Sample Preparation
Protein Precipitation:
- Thaw plasma samples on ice and centrifuge at 10,000 × g for 5 minutes.
- Aliquot 100 μL of plasma into a microcentrifuge tube.
- Add 300 μL of ice-cold acetonitrile (containing a stable isotope-labeled internal standard for the target drug) to precipitate proteins.
- Vortex vigorously for 60 seconds and incubate at -20°C for 10 minutes.
- Centrifuge at 15,000 × g for 15 minutes at 4°C.
- Transfer the clear supernatant to a new tube and evaporate to dryness under a gentle stream of nitrogen at 40°C.
- Reconstitute the dried extract in 100 μL of initial LC mobile phase (e.g., 95% water, 5% methanol, 0.1% formic acid). Vortex and centrifuge before transfer to an LC vial.
Alternative/Additional Enrichment (for very low abundances):
- For targets expected to be in the low ng/mL range or lower, implement immunoaffinity enrichment using antibody-coated magnetic beads specific to the target drug or peptide, following the manufacturer's protocol [7].
- Solid-phase extraction (SPE) can also be used for further cleanup and concentration.
LC-ESI-MRM Method Configuration
Liquid Chromatography:
- Column: Reversed-phase C18 column (e.g., 2.1 mm x 100 mm, 1.8 μm particle size).
- Mobile Phase A: Water with 0.1% formic acid.
- Mobile Phase B: Acetonitrile or Methanol with 0.1% formic acid.
- Gradient: Optimize a linear gradient from 5% B to 95% B over 10-15 minutes, followed by a wash and re-equilibration.
- Flow Rate: 0.2 - 0.4 mL/min.
- Column Temperature: 40°C.
Mass Spectrometry (Triple Quadrupole):
- Ion Source: Electrospray Ionization (ESI), positive or negative mode, depending on the analyte.
- Source Parameters: Optimize capillary voltage, cone voltage, desolvation temperature, and gas flows for maximum precursor ion signal.
- Ion Funnel Interface: If available, ensure the dual-stage ion funnel is operational for enhanced sensitivity [10].
- MRM Transitions:
- For the target drug, select 2-3 specific precursor ion > product ion transitions.
- Q1: Select the intact precursor ion ([M+H]+ or [M-H]-) of the drug.
- Q2 (CID): Optimize collision energy for each transition to generate a abundant, characteristic product ion.
- Q3: Select the most intense and specific product ion for quantification, and 1-2 additional ions for qualification.
- Follow the same process for the stable isotope-labeled internal standard.
Table 2: The Scientist's Toolkit - Essential Research Reagents and Materials
| Item/Category | Function and Importance |
|---|---|
| Stable Isotope-Labeled Internal Standards | Corrects for sample prep variability and ion suppression; essential for accurate quantification. |
| Immunoaffinity Depletion Columns | Removes high-abundance plasma proteins (e.g., albumin) to reduce dynamic range and reveal low-abundance targets. |
| Anti-target Antibody Beads | Selectively enriches the specific drug or protein target from plasma, drastically improving LOQ. |
| Triple Quadrupole Mass Spectrometer | The core platform for MRM, providing the two stages of mass selection for high specificity and sensitivity. |
| Ion Funnel Interface | Dramatically improves ion transmission into the mass spectrometer, boosting signal intensity [10]. |
The following diagram maps the logical decision process for method development based on the required sensitivity for the target analyte.
Method Selection Based on Sensitivity Needs
The integration of Electrospray Ionization with Multiple Reaction Monitoring mass spectrometry represents a powerful solution for the sensitive and specific quantification of drugs in plasma. The fundamental mechanisms of MRM provide unparalleled selectivity, while advancements in ESI interface technology, particularly the ion funnel, have driven substantial gains in sensitivity. By following the detailed protocols and strategic method development outlined in this application note, researchers can reliably detect and quantify target analytes at clinically relevant concentrations, thereby accelerating drug development and biomarker validation.
The Critical Role in Therapeutic Drug Monitoring (TDM) and Pharmacokinetic/Pharmacodynamic (PK/PD) Studies
Therapeutic Drug Monitoring (TDM) and Pharmacokinetic/Pharmacodynamic (PK/PD) studies are critical disciplines in modern clinical pharmacology and drug development. TDM is the clinical practice of measuring specific drugs at designated intervals to maintain a constant concentration in a patient's bloodstream, thereby optimizing individual dosage regimens [11]. It is particularly vital for drugs with narrow therapeutic ranges, marked pharmacokinetic variability, medications where target concentrations are difficult to monitor, and drugs known to cause both therapeutic and adverse effects [11]. The process is predicated on the assumption that a definable relationship exists between dose and plasma drug concentration, and between concentration and therapeutic effects [11].
The integration of PK/PD modeling has revolutionized drug development by providing a mathematical approach to study the time course of drug effects and exposure-response relationships [12]. Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS) has emerged as a cornerstone analytical technology in this field, offering the sensitivity, specificity, and versatility required for accurate drug quantification in complex biological matrices like plasma [13] [14]. This article delineates the application of LC-MS/MS within TDM and PK/PD studies, providing detailed protocols and frameworks for researchers and drug development professionals.
Theoretical Foundations of TDM and PK/PD
Pharmacokinetics (PK) and Pharmacodynamics (PD): Core Concepts
Pharmacokinetics (PK) describes the journey of a drug through the body, encompassing the processes of Absorption, Distribution, Metabolism, and Excretion (ADME) [15]. PK parameters such as total drug exposure (Area Under the Curve, AUC), maximum blood concentration (Cmax), half-life (t1/2), and elimination rate (Ke) are fundamental for determining dosing regimens [16].
Pharmacodynamics (PD), in contrast, is the study of the biological and physiological effects of a drug on the body, including its mechanism of action and the relationship between drug concentration and effect [15]. Key PD parameters include the maximum effect (Emax) and the concentration that produces 50% of the maximum effect (EC50) [16].
The interplay between PK and PD is pivotal. PK/PD modeling integrates data from both fields to predict dosing strategies and therapeutic outcomes, ensuring developed drugs have the highest efficacy and lowest risk of adverse effects [15]. The relationship between drug concentration and effect is often described by the sigmoid Emax model, which has its origins in receptor theory and defines a maximal effect (Emax) for a drug [17].
The Essential Role of Therapeutic Drug Monitoring
TDM enables the individualization of therapy by leveraging the relationship between drug exposure and clinical response. Its indications have widened to include assessing efficacy, verifying compliance, detecting drug-drug interactions, avoiding toxicity, and monitoring therapy cessation [11]. The multidisciplinary TDM process, outlined in Table 1, requires excellent communication among team members to ensure best practices.
Table 1: Key Indications for Therapeutic Drug Monitoring
| Indication | Clinical Application Example |
|---|---|
| Optimizing Efficacy | Tailoring dosage of prophylactic drugs like lithium or cyclosporine to prevent disease recurrence or transplant rejection [11]. |
| Avoiding Toxicity | Diagnosing digoxin toxicity, which can mimic heart disease symptoms, by confirming elevated plasma concentrations [11]. |
| Assessing Compliance | Differentiating between poor compliance and undertreatment when a low drug concentration is observed [11]. |
| Managing Drug Interactions | Adjusting lithium dosage when a thiazide diuretic is co-administered, or adjusting theophylline when erythromycin is added [11]. |
| Dosing in Special Populations | Optimizing doses in critically ill patients or those with organ dysfunction where PK parameters are altered [14] [11]. |
LC-MS/MS as the Analytical Gold Standard
The choice of analytical technique is fundamental to successful TDM and PK/PD studies. LC-MS/MS offers increased sensitivity and specificity compared to other methods like immunoassays, and is often the only viable method for quantifying drugs without natural chromophores or fluorophores [13].
Advantages of LC-MS/MS in Bioanalysis
- High Sensitivity and Specificity: The combination of chromatographic separation with mass spectrometric detection minimizes interference from matrix effects and drug metabolites, leading to highly accurate measurements [13] [14].
- Wide Applicability: LC-MS/MS can be applied to a vast range of small molecules and some large molecules, making it suitable for monitoring diverse drug classes, from antibiotics to oral antitumor agents [14] [18].
- Multiplexing Capability: Methods can be developed to simultaneously quantify dozens of drugs, as demonstrated by an assay that measures 57 oral antitumor agents in a single run, improving efficiency for clinical studies [18].
- Rapid Analysis: Modern LC-MS/MS systems can achieve total run times as low as 5 minutes per sample, facilitating high-throughput analysis crucial for clinical decision-making [14].
Application Notes: Implementing LC-MS/MS in TDM and PK/PD Studies
Protocol: LC-MS/MS Method Development and Validation for Omadacycline
The following detailed protocol, adapted from a recent study, outlines the steps for developing and validating a robust LC-MS/MS method for quantifying the antibiotic omadacycline in human plasma [14].
Instruments and Reagents
- Liquid Chromatograph: Agilent 1260 series HPLC system.
- Mass Spectrometer: API 4000 triple quadrupole tandem mass spectrometer.
- Chromatography Column: Phenomenex KINETEX XB-C18 (2.6 μm, 3 × 50 mm).
- Mobile Phases: (A) 0.1% formic acid in water; (B) pure acetonitrile.
- Chemicals: Omadacycline benzenesulfonate (reference standard), fexofenadine-d6 (Internal Standard), HPLC-grade methanol, acetonitrile, and formic acid.
Sample Preparation Procedure
- Protein Precipitation: Add 200 μL of protein precipitant (acetonitrile containing internal standard, fexofenadine-d6 at 50 ng/mL) to 50 μL of plasma sample.
- Mixing and Centrifugation: Vortex the mixture vigorously for 5 minutes and centrifuge at 13,000 rpm for 5 minutes at 4°C.
- Dilution: Transfer 50 μL of the supernatant to 200 μL of 0.1% formic acid in water and vortex to mix.
- Injection: Transfer 100 μL of the final supernatant to an injection vial and inject 5 μL into the LC-MS/MS system.
Chromatographic and Mass Spectrometric Conditions
- Gradient Elution: Total run time of 5 minutes at a flow rate of 0.4 mL/min.
- Gradient Program:
- 0-0.5 min: 10% B
- 0.5-3.5 min: 10% B → 90% B
- 3.5-4.0 min: 90% B
- 4.0-5.0 min: 10% B
- Ionization: Electrospray Ionization (ESI) in positive ion mode.
- Detection: Multiple Reaction Monitoring (MRM) with transitions:
- Omadacycline: m/z 557.4 → 453.4
- Internal Standard (fexofenadine-d6): m/z 508.4 → 472.8
Method Validation Results
The method was rigorously validated according to scientific guidelines, with key results summarized in Table 2 below.
Table 2: LC-MS/MS Method Validation Parameters for Omadacycline Quantification
| Validation Parameter | Result / Acceptance Criterion |
|---|---|
| Linear Range | 20 - 2000 ng/mL (effectively covers >98% of clinical samples) [14] |
| Intra-day & Inter-day Precision | Relative Standard Deviation (RSD) < 10% [14] |
| Accuracy | Relative Error (RE) within ± 10.00% [14] |
| Selectivity | No interference from blank plasma matrices at analyte retention times [14] |
| Carryover | Peak area at analyte position <20% of the LLOQ [14] |
Workflow Diagram: LC-MS/MS in TDM and PK/SD
The following diagram illustrates the integrated workflow of TDM and PK/PD studies, from clinical assessment to data-informed dosing recommendations.
Integrating PK/PD Modeling in Drug Development
PK/PD modeling is an indispensable tool that evolves throughout the drug discovery and development process [19] [12]. Its primary objective is to select promising compounds and identify safe, effective doses and dosing regimens [19].
A Framework for PK/PD Study Design
Effective implementation requires a strategic, iterative approach, as outlined below.
Key Considerations for PK/PD Study Design
- Effective Partnerships: A core partnership between pharmacologists and DMPK (Drug Metabolism and Pharmacokinetics) scientists must be established early in a discovery program [19].
- Pilot Studies: Initial studies with a reference compound help establish fundamental PK/PD principles, optimize the study design, and build confidence before testing novel compounds [19].
- Study Types: Studies progress from simple, acute models (single dose, sparse sampling) to complex, chronic disease models (repeated dosing, multiple biomarkers) as the program matures [19].
- Graphical Data Evaluation: Plotting concentration and response versus time, and response versus concentration, is crucial for identifying relationships, delays (hysteresis), and potential biases from dropout [17].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of LC-MS/MS-based TDM and PK/PD studies relies on a suite of essential materials and reagents. The following table details key components.
Table 3: Essential Research Reagents and Materials for LC-MS/MS-based TDM/PK/PD
| Item | Function & Application |
|---|---|
| Triple Quadrupole Mass Spectrometer | Gold standard for quantitative LC-MS/MS; enables highly specific Multiple Reaction Monitoring (MRM) for precise drug quantification [13] [14]. |
| U/HPLC System with C18 Column | Provides high-resolution chromatographic separation of the analyte from matrix components, reducing ion suppression and improving data quality [14] [18]. |
| Certified Reference Standard | The authentic drug substance of known purity and identity; essential for accurate calibration and quantification [14]. |
| Stable Isotope-Labeled Internal Standard | (e.g., fexofenadine-d6, deuterated analogs). Corrects for variability in sample preparation and ionization efficiency, improving precision and accuracy [13] [14]. |
| HPLC-Grade Solvents & Modifiers | (e.g., Acetonitrile, Methanol, Formic Acid). Used for mobile phases and sample preparation; high purity is critical to minimize background noise and contamination [14]. |
| Blank Control Matrix | (e.g., Drug-free human plasma). Used to prepare calibration standards and quality control samples for method development and validation [14] [18]. |
| Protein Precipitation Plates/Tubes | Facilitate high-throughput sample preparation by removing proteins from plasma samples, clarifying the extract for LC-MS/MS analysis [14]. |
| MMV665916 | MMV665916, MF:C19H19N3O4, MW:353.4 g/mol |
| BMS-986020 sodium | BMS-986020 sodium, MF:C29H25N2NaO5, MW:504.5 g/mol |
The synergy between robust LC-MS/MS analytical methods, principled Therapeutic Drug Monitoring, and sophisticated PK/PD modeling forms the bedrock of modern precision medicine in pharmacology. The protocols and frameworks detailed in this article provide a roadmap for researchers to generate high-quality, clinically actionable data. As drug therapies become more complex and targeted, the role of LC-MS/MS in elucidating exposure-response relationships and guiding individualized treatment will only grow in importance, ultimately contributing to the development of safer and more effective pharmaceuticals.
Liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) has emerged as a cornerstone technology in bioanalytical chemistry, particularly for the precise quantification of drug concentrations in plasma. This application note delineates the distinct advantages of LC-MS/MS over traditional High-Performance Liquid Chromatography (HPLC) with conventional detectors (e.g., UV, fluorescence) in the context of modern drug development. We focus on three pivotal areas where LC-MS/MS offers transformative benefits: superior selectivity, enhanced sensitivity, and powerful multiplexing capability. Supported by experimental data and detailed protocols, this document provides a framework for researchers and scientists to leverage these advantages in pharmacokinetic studies, therapeutic drug monitoring, and bioequivalence assessments.
Comparative Advantages of LC-MS/MS
The transition from HPLC to LC-MS/MS represents a significant evolution in analytical capabilities, driven by the mass spectrometer's role as a highly specific detector.
Table 1: Key Advantages of LC-MS/MS over Traditional HPLC
| Feature | Traditional HPLC | LC-MS/MS | Impact on Plasma Drug Analysis |
|---|---|---|---|
| Selectivity | Relies on retention time and spectral matching; susceptible to co-eluting interferents from complex matrices. | Uses mass-to-charge ratio (m/z) and unique fragmentation patterns; effectively distinguishes analytes from matrix components. [1] [20] | Reduces false positives/negatives; enables accurate quantification in complex biomatrices like plasma without complete baseline separation. |
| Sensitivity | Typically in the ng-µg/mL range (e.g., UV detection). | Routinely achieves pg-ng/mL levels (e.g., 0.004-0.01 ng/injection LLOQ reported). [21] [22] | Essential for quantifying low-dose drugs, metabolites, and drugs with low circulating plasma concentrations. |
| Multiplexing | Limited; typically requires separate methods or compromised conditions for multiple analytes. | Enables simultaneous quantification of dozens of analytes in a single run via Multiple Reaction Monitoring (MRM). [1] [23] | Dramatically increases throughput for therapeutic drug monitoring (TDM) and pharmacokinetic studies; allows for comprehensive cocktail analysis. |
The following diagram illustrates the core logical relationship underpinning the superior performance of LC-MS/MS in bioanalysis.
LC-MS/MS Specificity Logic
Enhanced Selectivity via Tandem MS
The selectivity of LC-MS/MS stems from its use of tandem mass spectrometry. The first mass analyzer (MS1) selects the intact ion (precursor ion) of the target analyte. This ion is then fragmented in a collision cell, and a second mass analyzer (MS2) selects a unique product ion. This two-stage filtering process, monitored as a precursor-product ion transition, provides a high degree of certainty in analyte identity that is unattainable with HPLC retention time alone. [1] This is crucial in plasma analysis, where endogenous compounds can co-elute and interfere with the analyte of interest.
Superior Sensitivity
LC-MS/MS offers significantly lower limits of quantification (LLOQ) compared to HPLC. This is due to the high efficiency of modern ionization sources like electrospray ionization (ESI) and the reduced chemical noise inherent in the MRM detection mode. [1] [22] For instance, a recently developed method for vonoprazan, amoxicillin, and clarithromycin in human plasma achieved LLOQs of 2-5 ng/mL, with detection limits (LOD) as low as 0.0013 ng/injection, demonstrating sensitivity suitable for rigorous pharmacokinetic studies. [21] Furthermore, techniques like micro-flow LC-MS/MS can offer additional sensitivity gains by improving ionization efficiency. [24]
High-Throughput Multiplexing
The MRM capability of triple quadrupole mass spectrometers allows for the rapid toggling between dozens, or even hundreds, of specific ion transitions within a single chromatographic run. [1] This enables the simultaneous quantification of a vast panel of drugs. A prominent example is a multiplex assay for 14 antibacterial and antifungal agents in patient serum, which streamlines therapeutic drug monitoring in intensive care units without compromising accuracy or precision. [23] This multiplexing capability drastically improves laboratory efficiency and reduces sample volume requirements.
Application Protocol: Multiplex Quantification of Antibacterial Agents in Plasma
The following detailed protocol is adapted from a validated method for the simultaneous quantification of 14 antibacterial/antifungal drugs in human serum, exemplifying the practical application of LC-MS/MS advantages in a clinical research setting. [23]
Research Reagent Solutions
Table 2: Essential Materials and Reagents
| Item | Function/Description | Example |
|---|---|---|
| Analytical Column | Core separation unit; a reversed-phase C8 column (e.g., 1.7 µm, 2.1 x 50 mm) provides robust separation for a diverse drug panel. [23] | Waters Acquity UPLC C8 |
| Mass Spectrometer | Detection and quantification; a triple quadrupole mass spectrometer operated in MRM mode is the industry standard. [1] [23] | Shimadzu LCMS-8050 |
| Internal Standards | Correct for variability in sample preparation and ionization; stable isotope-labeled analogs of the analytes are ideal. [23] | d5-piperacillin, 13C2,2H3-voriconazole |
| Sample Solvent | Protein precipitation agent; organic solvent with acid modifier to efficiently denature and precipitate plasma proteins. [23] | Methanol with 0.1% Formic Acid |
| Mobile Phase | A: Aqueous buffer with volatile modifier (e.g., 0.1% formic acid). B: Organic solvent with same modifier (e.g., acetonitrile with 0.1% formic acid). [21] [23] | 0.1% Formic Acid in Water / 0.1% Formic Acid in Acetonitrile |
Experimental Workflow
The following diagram outlines the end-to-end workflow for the multiplex assay, from sample collection to data analysis.
Multiplex Assay Workflow
Sample Preparation Protocol
- Protein Precipitation: Transfer 100 µL of thawed plasma or serum into a polypropylene tube.
- Internal Standard Addition: Add 20 µL of a mixed internal standard solution.
- Precipitation: Add 480 µL of ice-cold methanol containing 0.1% formic acid to precipitate proteins.
- Vortex and Centrifuge: Vortex the mixture vigorously for 1 minute, then centrifuge at 13,780 × g for 8 minutes.
- Supernatant Collection: Transfer 500 µL of the clear supernatant to an LC vial for analysis.
Chromatographic Conditions
- Column: Waters Acquity UPLC C8 (1.7 µm, 2.1 mm × 50 mm)
- Column Temperature: 40 °C
- Mobile Phase: A: 0.1% Formic acid in water; B: 0.1% Formic acid in acetonitrile
- Flow Rate: 0.4 mL/min
- Injection Volume: 2 µL
- Gradient Program:
Time (min) %B 0.0 5 0.5 5 4.0 65 4.2 5 5.0 5
Mass Spectrometric Conditions
- Ionization Source: Electrospray Ionization (ESI)
- Ion Mode: Positive
- Detection Mode: Multiple Reaction Monitoring (MRM)
- Operation: The mass spectrometer is configured to monitor specific precursor ion → product ion transitions for each of the 14 target analytes and their internal standards. Source temperature, desolvation gas, and collision energies are optimized for maximum response.
Method Validation Data
The described method was rigorously validated, yielding the following performance characteristics for key analytes. [23]
Table 3: Validation Data for Select Antibacterial Agents
| Analyte | Linear Range (µg/mL) | LLOQ (µg/mL) | Intra-day Precision (%RSD) | Inter-day Precision (%RSD) | Accuracy (%RE) | Absolute Recovery (%) |
|---|---|---|---|---|---|---|
| Linezolid | 0.1 - 100 | 0.1 | < 6.2 | < 8.5 | ± 8.9 | > 95 |
| Vancomycin | 0.3 - 100 | 0.3 | < 7.1 | < 9.3 | ± 11.2 | > 93 |
| Meropenem | 0.1 - 50 | 0.1 | < 8.5 | < 10.1 | ± 9.8 | > 94 |
| Voriconazole | 0.1 - 100 | 0.1 | < 5.9 | < 7.7 | ± 7.5 | > 96 |
LC-MS/MS solidly outperforms traditional HPLC for the quantification of drugs in plasma by providing unmatched selectivity to eliminate matrix interferences, exceptional sensitivity to monitor low-abundance analytes, and unparalleled multiplexing capability for high-throughput analysis. The detailed protocol for a 14-plex antibacterial assay serves as a practical template for researchers to implement this powerful technology. As instrument innovation continues, with trends toward miniaturization, increased automation, and greener chemistry, the role of LC-MS/MS as an indispensable tool in drug development and clinical research is poised for further growth. [25] [26] [22]
From Theory to Practice: Developing Robust LC-MS/MS Methods for Diverse Drug Classes
The development of robust, sensitive, and selective bioanalytical methods is a critical pillar in pharmaceutical research, particularly for the quantification of drug concentrations in plasma using Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS). The reliability of pharmacokinetic data, essential for therapeutic drug monitoring and dose regimen optimization, hinges directly on the meticulous optimization of two foundational elements: the chromatographic column and the mobile phase [27] [14]. Within the complex matrix of plasma, where analytes are present at trace levels amidst a host of interfering compounds, a well-designed chromatographic separation is the first and most crucial step in ensuring data integrity. This application note provides a detailed, practical framework for the selection and optimization of columns and mobile phases, framed within the context of developing an LC-MS/MS method for drug quantification in plasma.
Core Principles and Systematic Protocol
A structured approach to method development significantly reduces the time and resources required to achieve a validated method. The following sections outline a step-by-step protocol for column screening and mobile phase optimization.
Step-by-Step Column Selection Protocol
The choice of column dictates the primary interaction mechanism with your analyte and is the starting point for method development.
1. Define the Goal: Clearly outline the method's requirements, including desired resolution of critical pairs, sensitivity (LLOQ), analysis time, and robustness. 2. Analyze Analyte Structure: Determine the analyte's hydrophobicity, ionization constants (pKa), and presence of specific functional groups to guide the selection of separation mode [28]. 3. Select the Chromatographic Mode: - Reversed-Phase (RPLC): The most common mode for LC-MS/MS of small molecule drugs. Ideal for neutral and non-polar to moderately polar compounds [27] [29]. - Hydrophilic Interaction Liquid Chromatography (HILIC): Employ for highly polar and hydrophilic compounds that are not retained in RPLC [29]. 4. Screen Initial Columns: Begin with 3-4 columns featuring different stationary phase chemistries. A typical screening set may include: - A C18 column (e.g., Phenomenex KINETEX XB-C18 [14] or equivalent). - A Phenyl-Hexyl or equivalent for potential π-π interactions. - A Polar-embedded phase (e.g., amide) for improved retention of polar compounds. - A HILIC column (e.g., silica or amide) if RPLC retention is insufficient. 5. Evaluate Performance: Assess columns based on peak shape (asymmetry factor), retention factor (k), and resolution of critical analyte pairs from potential interferences. The column providing the best compromise of these factors is selected for further mobile phase optimization.
Table 1: Guide to Reversed-Phase Column Selection Based on Analyte Properties
| Analyte Property | Recommended Stationary Phase | Rationale |
|---|---|---|
| Non-polar to moderate polarity | C18 or C8 | Provides strong hydrophobic retention; the workhorse for most drug analyses [14] [30]. |
| Polar compounds | Polar-embedded (e.g., amide, ether) | Offers mixed-mode retention; can improve peak shape for bases [28]. |
| Aromatic compounds | Phenyl or Phenyl-Hexyl | Potential for π-π interactions, offering different selectivity versus C18. |
| Basic compounds | * charged surface hybrid (CSH) * or base-deactivated | Minimizes silanol interactions, reducing peak tailing and improving sensitivity [28]. |
| Very Polar/ Hydrophilic | HILIC | Provides complementary retention mechanism to RPLC; uses organic-rich mobile phases [29]. |
Comprehensive Mobile Phase Optimization
The mobile phase serves not only to elute analytes but also to control ionization, selectivity, and compatibility with the MS detector.
1. Select Organic Modifier: Choose between acetonitrile (ACN) and methanol (MeOH). Acetonitrile is generally preferred for LC-MS due to its lower viscosity (reducing backpressure), better UV transparency, and superior peak shape. Methanol is a cost-effective alternative but can generate higher backpressure [28] [31]. 2. Adjust pH with Volatile Buffers: The mobile phase pH is critical for controlling the ionization state of ionizable analytes, thereby modulating retention and selectivity. For LC-MS, always use volatile buffers such as ammonium formate or ammonium acetate, typically in a concentration range of 2-10 mM [32] [28] [30]. Set the pH at least 1.5–2.0 units away from the analyte's pKa to ensure a consistent ionization state and minimize retention time drift [28]. 3. Incorporate Additives: Small amounts of acidic or basic modifiers can significantly enhance ionization efficiency and peak shape. - Formic Acid (0.05-0.1%): Standard additive for positive electrospray ionization (ESI+), promotes [M+H]+ formation [14] [32]. - Ammonium Hydroxide / Ammonia Solution: Used for negative electrospray ionization (ESI-) to promote [M-H]- formation. - Trifluoroacetic Acid (TFA): Avoid if possible in LC-MS. While it excellent for peak shape of basic compounds, it causes severe ion suppression in the MS detector [28]. 4. Optimize Elution Mode: - Isocratic Elution: Suitable for simple mixtures where the retention of all components is similar. - Gradient Elution: Essential for complex samples or when analytes have a wide range of polarities. A gradient, typically from a low to a high percentage of organic solvent, ensures all compounds are eluted with sharp peaks and in a reasonable time [27] [14] [30]. 5. Fine-tune Flow Rate and Temperature: The flow rate (e.g., 0.3-0.6 mL/min for standard 2.1 mm i.d. columns) and column temperature (e.g., 40-50°C) are final parameters for fine-tuning resolution and cycle time. Higher temperatures can reduce backpressure and improve efficiency [14] [30].
Table 2: Optimization of Mobile Phase Additives for LC-MS/MS Applications
| Additive | Typical Concentration | Primary Function & ESI Mode | Advantages | Considerations |
|---|---|---|---|---|
| Formic Acid | 0.05 - 0.1% | Promotes protonation; ESI+ [14] [32] | Volatile, excellent for [M+H]+ signal, widely used. | Can suppress signal in ESI-; may not be strong enough for some basic compounds. |
| Ammonium Formate | 2 - 10 mM | pH control; ESI+ & ESI- [32] [30] | Volatile, good buffer capacity at ~pH 3-4. | Can form [M+NH4]+ adducts in ESI+, complicating spectra. |
| Ammonium Acetate | 2 - 10 mM | pH control; ESI+ & ESI- [32] | Volatile, good buffer capacity at ~pH 4.5-5.5. | Less common for ESI+; suitable for neutral molecules and ESI-. |
| Acetic Acid | 0.05 - 0.5% | Promotes protonation; ESI+ [32] | Weaker acid than formic acid; can offer different selectivity. | May provide lower sensitivity for some compounds compared to formic acid. |
| Ammonia / Ammonium Hydroxide | 0.05 - 0.2% | Promotes deprotonation; ESI- [30] | Volatile, essential for many ESI- applications. | Highly volatile, requires careful mobile phase preparation. |
Experimental Protocols and Methodologies
Detailed Protocol: Mobile Phase Optimization for a Novel Drug Compound
This protocol outlines the experimental workflow for optimizing the mobile phase to achieve maximum MS sensitivity and chromatographic resolution for a hypothetical drug in plasma.
Objective: To establish the optimal mobile phase composition (organic modifier, buffer pH, and additive) for the LC-MS/MS quantification of [Drug Name] in human plasma. Materials:
- Chemicals: HPLC-grade water, acetonitrile, methanol, ammonium formate, ammonium acetate, formic acid, acetic acid, ammonia solution.
- Equipment: LC-MS/MS system with electrospray ionization (ESI) and binary pump, analytical columns (as per Table 1).
- Standards: Pure analyte standard, internal standard.
Procedure:
- Standard Solution Preparation: Prepare a stock solution of the analyte at 1 mg/mL in an appropriate solvent (e.g., DMSO, methanol). Further dilute with a 50:50 mixture of water and organic solvent to a working concentration of 1 µg/mL for direct infusion and LC-MS testing [33].
- Initial MS/MS Optimization (Direct Infusion):
- Directly infuse the standard solution into the MS to determine the precursor ion ([M+H]+ or [M-H]-) and optimize fragmentor voltage.
- Select multiple reaction monitoring (MRM) transitions, optimizing collision energy (CE) for at least two fragments per compound [33].
- Initial Chromatographic Screening:
- Column: Install a C18 column (e.g., 50-100 mm length, 2.1 mm i.d., sub-3µm particles).
- Mobile Phase A: Test 0.1% formic acid in water.
- Mobile Phase B: Test 0.1% formic acid in acetonitrile.
- Perform a fast gradient (e.g., 5% to 95% B in 3-5 minutes) to assess retention and peak shape.
- Systematic Mobile Phase Comparison:
- Using the same column and standard, test the following mobile phase systems in an identical gradient:
- Data Analysis: For each system, record and compare the peak area (indicator of ionization efficiency), peak asymmetry factor, signal-to-noise ratio at the lower limit of quantification (LLOQ), and retention time stability.
The following workflow diagram summarizes this experimental protocol for mobile phase optimization:
Case Study: LC-MS/MS Method for Omadacycline in Human Plasma
A recent study developed an LC-MS/MS method for quantifying omadacycline, an antibiotic, in human plasma, providing an excellent real-world application of these principles [14].
Chromatographic Conditions:
- Column: Phenomenex KINETEX XB-C18 (50 x 3.0 mm, 2.6 µm).
- Mobile Phase: A: 0.1% Formic acid in water; B: Acetonitrile.
- Gradient Elution:
- 0-0.5 min: 10% B
- 0.5-3.5 min: 10% B → 95% B
- 3.5-4.0 min: 95% B
- 4.0-4.1 min: 95% B → 10% B
- 4.1-5.0 min: 10% B (re-equilibration)
- Flow Rate: 0.4 mL/min.
- Column Temperature: 40°C.
- Injection Volume: 5 µL.
- Total Run Time: 5 minutes.
Mass Spectrometry Conditions:
- Ionization: Electrospray Ionization (ESI), Positive Ion Mode.
- MRM Transitions:
- Omadacycline: m/z 557.4 → 453.4
- Internal Standard (Fexofenadine-d6): m/z 508.4 → 472.8
Sample Preparation: Protein precipitation was employed using 200 µL of acetonitrile (containing the internal standard) added to 50 µL of plasma. After vortexing and centrifugation, the supernatant was diluted with 0.1% formic acid in water and injected [14].
Key Outcomes: The method demonstrated linearity from 20-2000 ng/mL, with precision (RSD) <10% and accuracy (RE) within ±10%, successfully applied to clinical therapeutic drug monitoring.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for successful LC-MS/MS method development for plasma analysis.
Table 3: Essential Research Reagents and Materials for LC-MS/MS Plasma Method Development
| Item Category | Specific Examples | Function & Application Notes |
|---|---|---|
| HPLC Columns | C18, C8, Phenyl-Hexyl, HILIC (e.g., silica, amide) | Stationary phase for chromatographic separation; selection is critical for retention and selectivity [14] [29]. |
| Organic Solvents | Acetonitrile, Methanol (HPLC-MS Grade) | Mobile phase organic modifiers; high-purity grade is essential to minimize background noise [27] [31]. |
| Volatile Buffers | Ammonium Formate, Ammonium Acetate | Provide pH control and buffering capacity in the mobile phase while being compatible with MS detection [32] [28]. |
| Ionization Additives | Formic Acid, Acetic Acid, Ammonia Solution | Enhance analyte ionization in the ESI source and can improve chromatographic peak shape [14] [32] [30]. |
| Sample Prep Sorbents | C18, Mixed-Mode Cation/Anion Exchange | Used in Solid-Phase Extraction (SPE) for clean-up and concentration of analytes from complex plasma matrix [29]. |
| Protein Precipitants | Acetonitrile, Methanol, Trichloroacetic Acid | Used in protein precipitation to remove proteins from plasma samples prior to analysis [14] [5]. |
| Internal Standards | Stable Isotope-Labeled Analogs (e.g., d6, 13C) | Correct for variability in sample preparation and ionization efficiency; ideal for quantification [14] [30]. |
| KB02-JQ1 | KB02-JQ1, CAS:2384184-44-3, MF:C38H43Cl2N7O6S, MW:796.77 | Chemical Reagent |
| Cyclo(his-pro) TFA | Cyclo(his-pro) TFA, MF:C13H15F3N4O4, MW:348.28 g/mol | Chemical Reagent |
Troubleshooting and Best Practices
Even with a systematic protocol, challenges can arise. The following diagram illustrates a logical troubleshooting path for common chromatographic issues, linking them back to potential root causes in column or mobile phase selection.
Additional Best Practices:
- Mobile Phase Preparation: Always use the highest purity water and solvents. Measure pH of the aqueous buffer before adding the organic solvent. Filter and degas all mobile phases to prevent blockages and baseline noise [27].
- Column Care: Use a guard column to protect the analytical column. Flush and store columns according to the manufacturer's instructions to maximize their lifetime.
- System Suitability: Always perform system suitability tests before a batch run to ensure the method is performing as expected in terms of retention, resolution, peak shape, and sensitivity.
The path to a robust and sensitive LC-MS/MS method for quantifying drugs in plasma is a deliberate process of optimization. It begins with a rational selection of the chromatographic column based on analyte chemistry, followed by meticulous optimization of the mobile phase—its organic modifier, pH, and additives—to achieve the trifecta of strong retention, excellent peak shape, and maximum MS signal intensity. By adhering to the structured protocols, case study examples, and troubleshooting guidance provided in this application note, researchers and drug development professionals can enhance the efficiency and success of their bioanalytical method development, thereby generating high-quality data that is critical for advancing pharmaceutical science.
In the development of LC-MS/MS methods for quantifying drug concentrations in plasma, sample preparation is a critical first step to ensure the accuracy, sensitivity, and reliability of bioanalytical results. Effective sample preparation removes interfering matrix components, concentrates the analyte, and protects the instrumentation, thereby enhancing data quality [34] [29]. For researchers and drug development professionals, selecting the appropriate sample preparation technique is paramount for obtaining meaningful pharmacokinetic and toxicokinetic data.
Among the various available methods, protein precipitation (PP) and liquid-liquid extraction (LLE) are two widely used approaches for processing biological samples like plasma and serum. This application note provides a detailed comparison of these two techniques, framed within the context of developing a robust LC-MS/MS method for drug quantification in plasma. We summarize quantitative performance data, provide detailed experimental protocols, and offer guidance for method selection to support your bioanalytical workflows.
Core Principles and Comparative Analysis
Protein Precipitation is a straightforward and rapid deproteinization method. It involves adding a miscible organic solvent (e.g., methanol, acetonitrile, or acetone) to the plasma sample. The solvent disrupts the hydration shell around proteins, causing them to denature and aggregate, after which they are removed by centrifugation [34] [35]. This technique is characterized by its simplicity, minimal method development requirements, and high-throughput capability, making it particularly suitable for the early stages of drug discovery [34] [36].
Liquid-Liquid Extraction, in contrast, is a more selective technique that separates analytes based on their differential solubility between two immiscible liquid phases, typically an aqueous phase (the plasma sample) and an organic solvent [35]. The success of LLE depends on the careful selection of an organic solvent that provides optimal partitioning of the target analyte away from matrix interferences. This method often results in cleaner extracts and can significantly reduce matrix effects, which is crucial for achieving lower limits of quantification [37] [38].
Table 1: Comparative Analysis of Protein Precipitation and Liquid-Liquid Extraction
| Feature | Protein Precipitation (PP) | Liquid-Liquid Extraction (LLE) |
|---|---|---|
| Basic Principle | Denaturation and removal of proteins via organic solvents [34] | Partitioning of analyte between immiscible aqueous and organic phases [35] |
| Complexity & Workflow | Simple and fast; minimal method development [34] | More complex; requires solvent selection and optimization [37] |
| Typical Solvents | Acetonitrile, Methanol, Acetone [34] [39] | Methyl tert-butyl ether (MTBE), Ethyl acetate, Chloroform, Hexane [37] [40] |
| Matrix Removal | Moderate; some phospholipids and salts may remain [41] | Excellent for removing polar matrix interferences and phospholipids [37] |
| Recovery | Generally high and consistent for small molecules [34] | Can be very high, but highly dependent on analyte and solvent choice [37] |
| Throughput | High, easily automated in 96-well plates [36] | Lower, though automation with 96-well plates is possible [40] |
| Ideal Use Case | High-throughput screening, early drug discovery [34] | Targeted quantification requiring high sensitivity and low matrix effects [37] |
Detailed Methodologies and Protocols
Protein Precipitation Protocol
This protocol for protein precipitation using acetonitrile is adapted for a high-throughput 96-well format and is suitable for processing plasma samples in pharmacokinetic studies [36].
Materials and Reagents:
- Acetonitrile (LC-MS grade)
- Formic acid (LC-MS grade)
- Internal Standard working solution
- Plasma samples
- 96-well protein precipitation or filtration plate (e.g., PTFE membrane)
- 96-well collection plates
- Centrifuge capable of handling microplates
- Positive displacement liquid handler (optional, for automation)
Procedure:
- Aliquot Samples: Pipette 50 µL of acidified acetonitrile (containing 0.1% formic acid and the internal standard) into each well of a 96-well filtration plate.
- Add Plasma: Add 25 µL of plasma sample to the corresponding wells.
- Mix: Seal the plate and vortex mix for 3-5 minutes to ensure complete protein precipitation.
- Separate: Centrifuge the stacked plate (filtration plate on top of a collection plate) at approximately 1,500 × g for 5-10 minutes. The vacuum or centrifugal force will drive the deproteinized supernatant through the filter into the collection plate.
- Analyze: Transfer an aliquot (e.g., 10 µL) of the clear supernatant from the collection plate directly to an LC-MS/MS system for analysis [36].
Variations: Methanol and acetone are also commonly used precipitating solvents. A study comparing five different precipitation methods found that methanol and methanol/acetonitrile mixtures provided broad specificity and outstanding accuracy for metabolomics applications, a finding that is often transferable to small-molecule drug analysis [41]. For urine proteomics, methanol/chloroform precipitation has been shown to provide high protein recovery rates and a large number of protein identifications in LC-MS/MS analysis [39].
Liquid-Liquid Extraction Protocol
This LLE protocol uses methyl tert-butyl ether (MTBE) for the extraction of a pharmaceutical compound from whole blood, which can be readily adapted for plasma samples [40].
Materials and Reagents:
- Methyl tert-butyl ether (MTBE, HPLC grade)
- Internal Standard working solution in methanol/water
- Plasma samples
- 2 mL 96-well deep-well plates
- Centrifuge
- Liquid handler (recommended for automation)
- Nitrogen evaporator
Procedure:
- Internal Standard & Lysis: Add 60 µL of internal standard working solution to a 2 mL 96-well plate. The aqueous-organic mixture helps to lyse any blood cells if present. Add 40 µL of plasma sample to each well and vortex for 10 minutes.
- Extraction: Add 500 µL of MTBE to each well. Seal the plate securely and mix thoroughly by vortexing for 10-20 minutes to achieve efficient partitioning of the analyte into the organic phase.
- Phase Separation: Centrifuge the plate at a sufficient speed (e.g., 3,000 × g) for 10 minutes to achieve clear phase separation.
- Collection: Carefully collect 450 µL of the upper organic layer and transfer it to a new 96-well plate. Take care not to disturb the interface or the lower aqueous layer.
- Evaporation and Reconstitution: Evaporate the organic solvent to dryness under a gentle stream of nitrogen. Reconstitute the dried extract with 180 µL of a solvent compatible with your LC-MS/MS mobile phase (e.g., 20/80 acetonitrile/water) with vortex mixing.
- Analyze: Inject an aliquot (e.g., 20-30 µL) into the LC-MS/MS system [40].
Notes on Solvent Selection: The choice of organic solvent is critical. Dibutyl phthalate has been shown to provide complete extraction of compounds like testosterone and phenytoin from buffer solutions, though recovery from protein-containing matrices like albumin may be partial [37]. For extracting diverse compounds from traditional Chinese medicine, an ethyl acetate:acetone (10:1) system has proven effective [38].
Workflow Visualization
The following diagram illustrates the key decision points and procedural steps involved in selecting and executing PP or LLE for plasma sample preparation.
Essential Research Reagent Solutions
The selection of appropriate reagents is fundamental to the success of any sample preparation method. The following table details key materials and their functions in PP and LLE protocols.
Table 2: Key Reagents and Materials for Sample Preparation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Acetonitrile (LC-MS Grade) | Protein precipitating agent. Denatures and aggregates plasma proteins for easy removal [34]. | Most common precipitant; provides clean backgrounds. Acidification with 0.1% formic acid can improve recovery for some analytes [36]. |
| Methanol (LC-MS Grade) | Protein precipitating agent and solvent for standards/reconstitution [34] [40]. | Especially valuable for supporting preclinical pharmacokinetic studies during lead optimization [34]. |
| Methyl tert-butyl ether (MTBE) | Organic extraction solvent for LLE [40]. | A volatile and relatively safe solvent. Provides high recovery for non-polar to moderately polar analytes [40]. |
| Formic Acid (LC-MS Grade) | Mobile phase additive and solvent acidifier. Enhances protonation of analytes in positive ESI mode [36]. | Improves ionization efficiency and peak shape. Commonly used at 0.1-0.2% in mobile phases and sample solvents [36]. |
| Internal Standards | Isotope-labeled analogs of the analyte(s). Correct for variability in sample preparation and ionization [40]. | Crucial for achieving accurate and precise quantification. Should be added at the very beginning of the sample preparation process. |
| 96-Well Filtration Plates (PTFE) | For high-throughput protein precipitation. Membrane retains precipitated proteins during filtration [36]. | Enables parallel processing of 96 samples, eliminating the need for manual supernatant transfer and increasing reproducibility [36]. |
| Ammonium Acetate/Formate | Buffering agents for mobile phases. Can promote adduct formation ([M+NHâ‚„]âº) [40]. | Useful for stabilizing certain analytes. Concentration (e.g., 5-10 mM) and compatibility with MS detection should be optimized. |
Both protein precipitation and liquid-liquid extraction are indispensable techniques in the bioanalytical toolkit for LC-MS/MS-based drug quantification in plasma. The choice between them is not a matter of superiority but of strategic fit. Protein precipitation offers unmatched speed and simplicity, ideal for high-throughput environments like early drug discovery. Liquid-liquid extraction, while more labor-intensive, provides superior sample clean-up and reduced matrix effects, making it the method of choice for assays requiring high sensitivity and rigorous validation, such as those supporting late-stage development and clinical trials.
Researchers are advised to base their selection on key project parameters, including the number of samples, required throughput, physicochemical properties of the analyte, and the desired level of sensitivity. In many cases, a complementary use of both techniques—employing PP for rapid screening and LLE for definitive analysis—can provide an efficient and effective strategy across the drug development pipeline.
In the development of a robust Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) method for quantifying drug concentrations in plasma, the optimization of mass spectrometric parameters is a critical step that directly impacts method sensitivity, selectivity, and reproducibility. The process specifically focuses on two key areas: the ion source, where analyte molecules are converted into gas-phase ions, and the collision cell, where precursor ions are fragmented into product ions for detection [42] [43]. This application note provides detailed protocols and strategic frameworks for systematically optimizing these parameters to enhance bioanalytical performance in pharmaceutical research and development.
Efficient method development requires understanding the role of each parameter in the MS workflow. The figure below illustrates the key optimization parameters in a triple quadrupole mass spectrometer and their locations within the system.
Figure 1. LC-MS/MS optimization parameters. This workflow shows the key parameters for ion source and collision cell optimization in a triple quadrupole mass spectrometer.
Ion Source Parameter Optimization
The ion source converts analyte molecules into gas-phase ions, with efficiency determined by multiple interdependent parameters. Systematic optimization of these parameters significantly enhances ionization efficiency and overall signal response [44] [43].
Critical Ion Source Parameters and Their Functions
Table 1. Key Ion Source Parameters for Optimization in ESI Mode
| Parameter | Symbol | Function | Typical Range | Optimization Impact |
|---|---|---|---|---|
| IonSpray Voltage | IS | Creates strong electric field for droplet charging and ion emission | 2000-6000 V | Dramatically affects ionization efficiency; optimal voltage is compound-dependent [43] |
| Nebulizer Gas | GS1 | Shears liquid stream into fine droplets for efficient desolvation | 0-150 psi | Higher values create smaller droplets but excessive flow can cool spray [43] |
| Heating Gas | GS2 | Promotes desolvation of charged droplets through heated nitrogen flow | 0-150 psi | Prevents solvent clusters; temperature should be optimized with TEM [43] |
| Source Temperature | TEM | Controls heating of auxiliary gas for enhanced desolvation | 100-700°C | Critical for highly aqueous mobile phases; prevents premature vaporization [43] |
| Curtain Gas | CUR | Forms barrier between source and analyzer; prevents contamination | 0-50 psi | Higher values reduce chemical noise; optimize without significant sensitivity loss [43] |
| Declustering Potential | DP | Accelerates ions to remove solvent adducts and clusters | 20-200 V | Balances between adduct removal and unwanted in-source fragmentation [43] |
| Entrance Potential | EP | Guides and focuses ions through Q0 region | 5-15 V | Minor effect on optimization; typically set at ±10 V [43] |
Experimental Protocol for Ion Source Optimization
Sample Preparation for Optimization
- Prepare a pure chemical standard of the target analyte at concentrations typically ranging from 50 ppb to 2 ppm in an appropriate solvent [33]. For drug quantification in plasma, omadacycline was optimized using standards at 20-2000 ng/mL in blank plasma [45].
- Use a solvent composition that matches the anticipated mobile phase (typically 50:50 organic:aqueous ratio) to maintain consistency between optimization and final method conditions [33] [43].
- For plasma-based methods, include matrix-matched quality control samples at low, medium, and high concentrations to monitor matrix effects during optimization [45].
Systematic Optimization Procedure
- Step 1: Sample Introduction: Utilize either infusion (5-25 μL/min via syringe pump) or flow injection analysis (FIA) (25-1000 μL/min via LC system) to introduce the standard to the mass spectrometer without chromatographic separation [43].
- Step 2: IonSpray Voltage and Gas Optimization: Using MRM mode, systematically vary IS voltage while monitoring signal response. Subsequently, optimize GS1, GS2, TEM, and CUR parameters using a multivariate approach [44] [43].
- Step 3: Declustering Potential Optimization: Introduce the standard and perform a Q1 scan to determine the optimal DP value (typically 20-100 V) that maximizes precursor ion intensity while minimizing fragmentation [43].
- Step 4: Response Surface Methodology (RSM): For advanced optimization, employ design of experiments (DoE) approaches to model interaction effects between parameters. This has been shown to improve signal-to-noise ratios 2-4 fold for challenging analytes [46].
Collision Energy Optimization
Collision energy optimization determines the efficiency of precursor ion fragmentation into characteristic product ions, directly impacting the selectivity and sensitivity of MRM-based quantification methods [33] [43].
Collision Cell Parameters and Functions
Table 2. Key Collision Cell Parameters for MRM Optimization
| Parameter | Symbol | Function | Optimization Consideration |
|---|---|---|---|
| Collision Energy | CE | Accelerates precursor ions into collision gas; determines degree of fragmentation | Compound-specific; must be optimized for each MRM transition [43] |
| Collision Gas | CAD | Inert gas (typically argon or nitrogen) for collision-induced dissociation | Sufficient pressure needed for fragmentation; typically 1-5 mTorr [43] [46] |
| Collision Cell Exit Potential | CXP | Focuses and transmits fragment ions from collision cell to Q3 | Affects transmission efficiency; typically optimized for each transition [43] |
Experimental Protocol for Collision Energy Optimization
Product Ion Scan and MRM Development
- Step 1: Precursor Ion Selection: Using the optimized ion source parameters, introduce the standard and confirm the precursor ion mass (typically [M+H]+ or [M-H]-). Account for possible adduct formation with mobile phase additives [33].
- Step 2: Product Ion Scan: Perform product ion scans across a range of collision energies (e.g., 5-50 eV) to identify the most abundant fragment ions [43]. The example of omadacycline quantification identified the transition m/z 557.4→453.4 as optimal [45].
- Step 3: MRM Transition Selection: Select at least two MRM transitions per compound - one for quantification and another for confirmation. The ratio between these transitions should remain constant and serve as a confirmatory criterion [33].
Collision Energy Fine-Tuning
- Step 4: CE Optimization: For each MRM transition, systematically vary CE in 2-5 eV increments while monitoring product ion intensity. Optimal CE typically falls between 10-40 eV, depending on the compound and instrument [43].
- Step 5: Advanced DoE Approaches: For methods quantifying multiple analytes, employ fractional factorial designs to efficiently optimize CE across all compounds. This approach revealed distinct fragmentation behaviors between polar and apolar oxylipins, requiring class-specific optimization [46].
- Step 6: CXP Optimization: Fine-tune CXP (typically 5-25 V) to maximize transmission of product ions to the detector [43].
Integrated Workflow for Comprehensive Optimization
A systematic approach to LC-MS/MS method development ensures optimal performance for drug quantification in plasma matrices. The following workflow integrates both ion source and collision energy optimization steps.
Figure 2. LC-MS/MS parameter optimization workflow. This integrated approach systematically addresses both ion source and collision cell parameters for robust method development.
Case Studies and Applications
Omadacycline Quantification in Human Plasma
A recently developed LC-MS/MS method for omadacycline quantification exemplifies proper parameter optimization [45]. Key optimized parameters included:
- Ion source: Positive ESI mode with specific desolvation temperature and gas flows
- MRM transition: m/z 557.4→453.4 with compound-specific collision energy
- Chromatography: Gradient elution with 0.1% formic acid-water and acetonitrile The method demonstrated excellent linearity (20-2000 ng/mL), precision (RSD <10%), and accuracy (RE within ±10%), making it suitable for therapeutic drug monitoring [45].
LXT-101 Sustained-Release Suspension Bioanalysis
For the novel prostate cancer drug LXT-101, researchers developed a validated LC-MS/MS method with the following optimized parameters [47]:
- Collision energy: 43 eV specifically optimized for the transition m/z 472.13+→587.8
- Ion source settings: Spray voltage 4800 V, source temperature 300°C, sheath gas 10 psi
- Sample preparation: Protein precipitation followed by evaporation and reconstitution The method showed good linearity (2-600 ng/mL) and was successfully applied to pharmacokinetic studies in beagle dogs [47].
Design of Experiments for Oxylipin Analysis
A systematic DoE approach for oxylipin analysis demonstrated that response surface methodology could significantly improve sensitivity [46]:
- Polar oxylipins (prostaglandins, lipoxins) benefited from higher CID gas pressure and lower interface temperatures
- Apolar oxylipins (HETEs, HODEs) required different optimal conditions
- Results: 2-fold S/N improvement for lipoxins and resolvins; 3-4 fold improvement for leukotrienes and HETEs This systematic approach outperformed traditional one-factor-at-a-time optimization [46].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3. Essential Research Reagents and Materials for LC-MS/MS Method Development
| Item | Function | Application Notes |
|---|---|---|
| HPLC-grade solvents (methanol, acetonitrile, water) | Mobile phase components; standard preparation | Minimize contamination; use LC-MS grade for sensitivity-critical applications [45] [47] |
| Volatile buffers (ammonium formate, ammonium acetate) | Mobile phase additives; pH control | Preferred over non-volatile salts; concentration typically 2-10 mM [42] [48] |
| Formic acid, acetic acid | Ion pairing agents; pH modification | Typically used at 0.05-0.1% in mobile phase; enhances positive ion mode sensitivity [45] [47] |
| Chemical standards (pure analytes) | Method development and calibration | ≥98% purity; prepare stock solutions in appropriate solvents [45] [33] |
| Stable isotope-labeled internal standards | Normalization; quantification accuracy | Correct for matrix effects and recovery variations; essential for bioanalysis [45] [47] |
| Blank plasma matrix | Method development; quality control | Should be from appropriate species; used for matrix-matched calibration [45] [47] |
| Solid-phase extraction cartridges | Sample clean-up; analyte concentration | C8 or C18 chemistry commonly used; improves sensitivity by reducing matrix effects [42] [48] |
| Chromatographic columns (C18, C8) | Analyte separation | 50-100 mm length, 2.1 mm ID; sub-3μm particles for improved separation [45] [47] |
| mogroside IE | mogroside IE, CAS:88901-39-7, MF:C36H62O9, MW:638.9 g/mol | Chemical Reagent |
| (R)-BRD3731 | (R)-BRD3731, CAS:2056262-08-7, MF:C24H31N3O, MW:377.532 | Chemical Reagent |
The rise of antimicrobial resistance necessitates precision medicine approaches to antibiotic therapy, particularly for last-resort treatments. Therapeutic Drug Monitoring (TDM) via Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) provides the analytical rigor required to optimize dosing regimens for critically ill patients. This application note details validated LC-MS/MS methodologies for quantifying two essential antibiotic classes: the novel tetracycline omadacycline and the oxazolidinones (linezolid, tedizolid, and contezolid). Framed within broader research on LC-MS/MS for plasma drug quantification, these protocols support pharmacokinetic/pharmacodynamic (PK/PD) studies and clinical TDM to improve patient outcomes.
The Clinical Imperative for Precision Dosing
Omadacycline
Omadacycline, a third-generation tetracycline, demonstrates time-dependent pharmacokinetics. Its efficacy is best correlated with the ratio of the 24-hour area under the concentration-time curve to the minimum inhibitory concentration (AUC0–24/MIC) [14] [45]. In critically ill patients, pathophysiological changes can significantly alter drug pharmacokinetics, making TDM essential for ensuring adequate drug exposure [14]. For tuberculosis treatment, the PK/PD target (EC80) has been identified as an AUC0–24/MIC of 26.93 [49].
Oxazolidinones
The oxazolidinone class, including linezolid, tedizolid, and contezolid, exhibits concentration-dependent antibacterial activity. The primary PK/PD index for efficacy is the time that free drug concentration exceeds the MIC (fT>MIC) [50]. These drugs also possess a narrow therapeutic index, with potential for hematological toxicity (e.g., thrombocytopenia) and neurotoxicity at elevated concentrations, creating a critical need for TDM to balance efficacy and safety [50].
Analytical Methodologies
LC-MS/MS Platform and Reagent Solutions
The following table catalogs essential reagents and instrumentation common to the described methods.
Table 1: Research Reagent Solutions for LC-MS/MS Quantification
| Component | Specific Examples & Specifications | Function in Protocol |
|---|---|---|
| Chromatography System | Agilent 1260 series HPLC [14] | Solvent delivery and sample introduction |
| Mass Spectrometer | API-4000 Triple Quadrupole [14]; SCIEX QSight 210 [50] | Analyte detection and quantification |
| Analytical Column | Phenomenex KINETEX XB-C18 (50 x 2.1 mm, 2.6 µm) [14] | Chromatographic separation of analytes |
| Internal Standards | Fexofenadine-d6 [14]; Voriconazole-d3 [50] | Normalization for sample prep and injection variability |
| Protein Precipitant | Acetonitrile (with or without 0.1-0.2% formic acid) [50] [51] | Plasma protein precipitation and analyte extraction |
| Mobile Phase A | Water with 0.1% Formic Acid [14] [51] | Aqueous component for gradient elution |
| Mobile Phase B | Acetonitrile with 0.1% Formic Acid [14] [51] | Organic component for gradient elution |
Omadacycline Quantification Protocol
Sample Preparation
A simple protein precipitation protocol ensures high-throughput analysis.
- Precipitant Preparation: Dilute fexofenadine-d6 internal standard (IS) stock solution in pure acetonitrile to a concentration of 50 ng/mL [14] [45].
- Precipitation: Add 200 µL of the precipitant/IS solution to 50 µL of calibrator, quality control (QC), or patient plasma sample in a 1.5 mL centrifuge tube [14] [45].
- Mixing and Centrifugation: Vortex the mixture for 1 minute and centrifuge at 13,000 rpm for 5 minutes at 4°C [14].
- Dilution and Injection: Transfer 50 µL of the supernatant to 200 µL of 0.1% formic acid in water, vortex to mix, and inject 5 µL into the LC-MS/MS system [14].
Instrumental Analysis
- Chromatography: Separation is achieved using a gradient elution at 0.4 mL/min over a 5-minute run time [14]. The gradient profile is detailed in the table below.
- Mass Spectrometry: Detection employs positive electrospray ionization (ESI+) and Multiple Reaction Monitoring (MRM). The transition for omadacycline is m/z 557.4 → 453.4, and for the IS (fexofenadine-d6) is m/z 508.4 → 472.8 [14] [45].
Table 2: Optimized Gradient for Omadacycline Separation
| Time (min) | Mobile Phase A (%) | Mobile Phase B (%) |
|---|---|---|
| 0.0 | 90 | 10 |
| 0.5 | 90 | 10 |
| 1.5 | 3 | 97 |
| 3.0 | 3 | 97 |
| 3.5 | 90 | 10 |
| 5.0 | 90 | 10 |
Oxazolidinone Quantification Protocol
Sample Preparation
A similar precipitation method is used for the simultaneous extraction of multiple oxazolidinones.
- Precipitation: Add 200 µL of IS working solution (voriconazole-d3 in methanol:ACN) to 50 µL of plasma sample [50].
- Mixing and Centrifugation: Vortex to homogenize and centrifuge at 14,000 rpm for 10 minutes at 4°C [50].
- Dilution and Injection: Mix 100 µL of the supernatant with 200 µL of 50% ACN containing 0.1% formic acid. Transfer to an autosampler vial for injection [50].
Instrumental Analysis
- Chromatography: A C18 column (100 × 2.1 mm, 3.5 µm) with a gradient elution is used for separation [50].
- Mass Spectrometry: ESI+ and MRM are used with the following transitions: linezolid m/z 338.14→162.8, tedizolid m/z 371→343.1, and contezolid m/z 409.15→269.14 [50].
Key Analytical Performance Data
Both methods have been rigorously validated according to international guidelines, demonstrating reliability for clinical and research applications.
Table 3: Analytical Method Performance Data
| Parameter | Omadacycline Method [14] | Oxazolidinones Method [50] |
|---|---|---|
| Linear Range | 20 - 2,000 ng/mL | Linezolid/Contezolid: 50.0 - 15,000.0 ng/mL; Tedizolid: 25.0 - 7,500.0 ng/mL |
| Precision (RSD) | Intra- and inter-day RSD < 10% | Intra- and inter-day RSD within acceptable limits (<11.9%) |
| Accuracy (RE) | Within ± 10% | 94.4% to 104.2% |
| Internal Standard | Fexofenadine-d6 | Voriconazole-d3 |
| Run Time | 5 minutes | Not specified |
Experimental Workflow and Data Interpretation
TDM Workflow Diagram
The following diagram illustrates the logical flow from sample collection to clinical decision-making in a TDM program.
Applying PK/PD Targets in Practice
The quantitative data from LC-MS/MS analysis must be interpreted using established PK/PD targets to guide therapy.
- For Omadacycline: The goal is to achieve a plasma AUC0–24/MIC ratio of ≥ 26.93 for maximal kill against M. tuberculosis [49]. For other pathogens, the clinical MIC and patient-specific factors determine the target.
- For Linezolid: The PK/PD target associated with efficacy is an AUC/MIC ratio of > 100 [50]. TDM is also crucial to maintain trough concentrations below a toxicity threshold, often cited as 2-8 mg/L, to minimize the risk of thrombocytopenia.
The LC-MS/MS protocols detailed herein provide robust, sensitive, and specific methods for quantifying omadacycline and oxazolidinones in human plasma. Their application in clinical TDM and PK/PD research is instrumental for moving beyond empirical dosing towards personalized antimicrobial therapy. By ensuring optimal drug exposure, these analytical strategies maximize therapeutic efficacy and minimize toxicity, ultimately combating treatment failure and the progression of antimicrobial resistance.
Therapeutic drug monitoring (TDM) and pharmacokinetic (PK) studies are critical components of modern precision medicine, particularly for drugs with narrow therapeutic windows or significant interindividual variability. In the intersecting fields of oncology and virology, the development of analytical methods for simultaneous drug quantification presents unique challenges and opportunities. The combination of venetoclax, a B-cell lymphoma-2 (BCL-2) inhibitor used in hematological malignancies, and cobicistat, a pharmacokinetic enhancer primarily used in antiretroviral therapy, represents a compelling case study in cross-disciplinary assay development [52]. This application note details the establishment and validation of a rapid, reliable liquid chromatography-tandem mass spectrometry (LC-MS/MS) method for the simultaneous quantification of these therapeutically distinct compounds, framed within broader research on LC-MS/MS methods for quantifying drug concentrations in plasma.
The clinical imperative for this simultaneous assay stems from ongoing investigative therapeutic strategies. Venetoclax, while effective for treating acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL), is primarily metabolized by CYP3A4, making it susceptible to pharmacokinetic boosting [52]. Cobicistat, a potent irreversible CYP3A4 inhibitor, is being explored in clinical trials like the HOVON 171 trial (NCT06014489) to reduce venetoclax dosing requirements, thereby potentially enhancing cost-effectiveness while maintaining therapeutic efficacy [52]. This combination necessitates analytical methods capable of monitoring both compounds concurrently to support dose optimization, adherence monitoring, and interaction management.
Background and Clinical Significance
Pharmacological Profiles
Venetoclax is an oral inhibitor of the anti-apoptotic protein BCL-2 that has demonstrated significant efficacy in CLL and, in combination with azacitidine, as a first-line treatment for unfit AML patients [52]. Despite its clinical benefits, venetoclax exhibits wide interindividual pharmacokinetic variability and is associated with dose-dependent toxicities, necessitating careful dose management [53] [54]. As a substrate of CYP3A4, its metabolism is significantly influenced by concomitant administration of CYP3A4 inhibitors or inducers, and by genetic polymorphisms in CYP3A4/3A5 enzymes [54].
Cobicistat is a mechanism-based CYP3A4 inhibitor primarily employed as a pharmacokinetic enhancer in antiretroviral regimens for HIV treatment [52]. By irreversibly inhibiting CYP3A4, cobicistat increases systemic exposure to co-administered drugs that are CYP3A4 substrates. This property has been leveraged in oncology to boost the exposure of several antineoplastic agents, potentially allowing for dose reduction of expensive targeted therapies while maintaining therapeutic concentrations [52].
Therapeutic Drug Monitoring Rationale
Therapeutic drug monitoring of these agents serves distinct but complementary purposes. For cobicistat, TDM can guide therapy in special populations and serve as an adherence monitor, which is particularly valuable when it is used to boost oncology drugs [52]. While TDM of venetoclax is not routinely recommended for efficacy optimization, it plays a crucial role in toxicity management and interaction assessment, especially when combined with strong CYP3A4 inhibitors like cobicistat [52] [54]. Clinical evidence demonstrates that venetoclax plasma concentrations correlate with treatment efficacy, with one study identifying a 6-hour post-dose concentration (C6h) cut-off value of 0.2868 μg/mL (286.8 ng/mL) that significantly correlates with response in leukemia patients with good or intermediate prognosis [54].
Materials and Methods
Reagents and Chemicals
Table 1: Key Research Reagent Solutions
| Reagent/Component | Specification/Source | Primary Function in Assay |
|---|---|---|
| Cobicistat reference standard | Alsachim, France | Primary analyte for quantification |
| Venetoclax reference standard | Alsachim, France | Primary analyte for quantification |
| [13C4,2H3] Cobicistat (IS) | Alsachim, France | Internal standard for cobicistat |
| [2H7] Venetoclax (IS) | Alsachim, France | Internal standard for venetoclax |
| Acetonitrile (HPLC grade) | Biosolve, Netherlands | Mobile phase component and protein precipitation |
| Ammonium formate | Thermo Scientific, USA | Mobile phase buffer component |
| Formic acid | Not specified in sources | Mobile phase pH modifier |
| Dimethyl sulfoxide (DMSO) | Merck, Netherlands | Solvent for stock solutions |
| Blank human EDTA plasma | BioIVT, USA | Matrix for calibration standards |
| Blank human serum | Merck Millipore | Alternative matrix for validation |
Instrumentation and Analytical Conditions
The simultaneous quantification method employs an ultra-high-performance liquid chromatography (UHPLC) system coupled to a triple quadrupole mass spectrometer (TSQ Quantiva, Thermo Fisher Scientific) [52]. Key instrumental parameters are summarized below:
Chromatographic Conditions:
- Column: C18 column (2.6 μm, 50 × 2.1 mm, Accucore, Thermo Fisher Scientific)
- Column Temperature: 60°C
- Autosampler Temperature: 10°C
- Injection Volume: 0.5 μL
- Mobile Phase A: 20 mmol/L ammonium formate (pH 3.5 with formic acid)
- Mobile Phase B: Acetonitrile
- Flow Rate: 1.000 mL/min
- Gradient Program: 0.00 min (30.0% B), 0.000-0.300 min (47.5% B), 0.300-0.950 min (75% B), 0.950-1.400 min (100% B), 1.400-1.500 min (30% B), 1.500 min (30.0% B)
Mass Spectrometric Conditions:
- Ionization Source: Heated electrospray ionization (H-ESI) with positive polarity
- Spray Voltage: 1500 V (static)
- Ion Transfer Tube Temperature: 140°C
- Vaporizer Temperature: 350°C
- Sheath Gas Pressure: 60 arbitrary units (a.u.)
- Auxiliary Gas Pressure: 25 a.u.
- Sweep Gas Pressure: 0 a.u.
- Detection Mode: Selected reaction monitoring (SRM)
- Q1 and Q3 Resolutions: 0.7 full width at half maximum (FWHM)
Table 2: SRM Transitions and Parameters
| Analyte | Retention Time (min) | Precursor Ion (m/z) | Product Ion (m/z) | Collision Energy (V) |
|---|---|---|---|---|
| Cobicistat | 0.45 | 776.4 | 545.3 | 36 |
| [13C4,2H3] Cobicistat (IS) | 0.45 | 783.4 | 552.3 | 36 |
| Venetoclax | 0.85 | 868.4 | 321.1 | 41 |
| [2H7] Venetoclax (IS) | 0.85 | 875.4 | 321.1 | 41 |
Sample Preparation Protocol
The method employs a simple protein precipitation procedure suitable for high-throughput analysis:
- Aliquot 50 μL of plasma or serum sample into a microcentrifuge tube.
- Add internal standard working solution containing 20 μg/L of each stable isotope-labeled internal standard.
- Precipitate proteins by adding an appropriate volume of acetonitrile (typically 150-200 μL) and vortex mixing vigorously for 60 seconds.
- Centrifuge at high speed (≥13,000 × g) for 10 minutes to pellet precipitated proteins.
- Transfer supernatant to autosampler vials for analysis.
- Inject 0.5 μL onto the LC-MS/MS system.
For alternative methods, solid-phase extraction (SPE) using C18 cartridges has been successfully employed for venetoclax in combination with other drugs, providing high recovery rates (90.68-97.56%) with minimal interference from plasma endogenous components [55].
Calibration Standards and Quality Controls
Stock solutions of cobicistat and venetoclax are prepared in DMSO and serially diluted to create working solutions. Calibration standards are prepared by spiking blank human plasma or serum:
- Cobicistat calibration range: 5-500 μg/L (5, 10, 25, 50, 100, 200, 400, and 500 μg/L)
- Venetoclax calibration range: 50-5000 μg/L (50, 100, 250, 500, 1000, 2000, 4000, and 5000 μg/L)
Quality control (QC) samples are prepared at four concentration levels:
- Lower limit of quantification (LLQ): 5 μg/L (cobicistat), 50 μg/L (venetoclax)
- Low QC: 10 μg/L (cobicistat), 100 μg/L (venetoclax)
- Medium QC: 200 μg/L (cobicistat), 2000 μg/L (venetoclax)
- High QC: 400 μg/L (cobicistat), 4000 μg/L (venetoclax)
Method Validation
The simultaneous assay was validated according to both European Medicines Agency (EMA) and U.S. Food and Drug Administration (FDA) guidelines for bioanalytical method validation [52].
Analytical Performance
Table 3: Method Validation Results
| Validation Parameter | Cobicistat Performance | Venetoclax Performance |
|---|---|---|
| Calibration Range | 5-500 μg/L | 50-5000 μg/L |
| Accuracy (%) | -5.9% to 2.4% | Within acceptance criteria |
| Within-day Precision (% RSD) | 1.2% to 4.8% | 1.2% to 4.8% |
| Between-day Precision (% RSD) | 0.4% to 4.3% | 0.4% to 4.3% |
| Stability | ≥8 days under various conditions | ≥8 days under various conditions |
| Carry-over | <20% of LLOQ after HLOQ sample | <20% of LLOQ after HLOQ sample |
The validation demonstrated excellent linearity across the specified concentration ranges for both analytes, with correlation coefficients (r²) exceeding 0.998 for both cobicistat and venetoclax [52] [55]. The method exhibited sufficient sensitivity to quantify trough concentrations observed in clinical settings, with lower limits of quantification adequate for TDM purposes.
Specificity and Selectivity
The method demonstrated high specificity with no significant interference from endogenous plasma components at the retention times of cobicistat (0.45 min) or venetoclax (0.85 min) [52]. The use of stable isotope-labeled internal standards for both analytes compensated for any potential matrix effects or variability in sample preparation.
Stability
Stability studies confirmed that both cobicistat and venetoclax remained stable in plasma and serum for at least 8 days under various storage and handling conditions, including freeze-thaw cycles, benchtop stability, and processed sample stability in the autosampler [52].
Experimental Workflow and Clinical Application
The following diagram illustrates the complete workflow from sample collection to data analysis for the simultaneous LC-MS/MS assay:
Clinical Applications and Representative Data
Therapeutic Drug Monitoring Experience
In clinical applications, the validated method has been successfully applied to patient samples from therapeutic drug monitoring programs. Analysis of clinical TDM samples revealed mean concentrations (± standard deviation) of 138.8 ± 123.3 μg/L for cobicistat and 1497.1 ± 1285.9 μg/L for venetoclax [52]. The substantial variability observed in venetoclax concentrations underscores the importance of TDM, particularly when co-administered with CYP3A4 inhibitors like cobicistat.
Independent studies in Chinese AML patients reported a venetoclax peak plasma concentration (Cmax) of 2966.0 ± 1595.0 ng/mL and trough concentration (Cmin) of 1018.0 ± 729.4 ng/mL [53]. These concentrations showed positive correlation with aspartate aminotransferase (AST) levels and were significantly higher in older patients, highlighting patient-specific factors that influence drug exposure [53].
Pharmacogenomic Considerations
The relationship between pharmacogenetics and venetoclax exposure has clinical implications for personalized dosing. Patients carrying CYP3A5 rs776746 AA/AG genotypes were prone to higher venetoclax plasma concentrations regardless of dose reductions [54]. This finding supports the integration of pharmacogenetic testing with TDM to optimize venetoclax therapy, particularly when used in combination with CYP3A4 inhibitors like cobicistat.
The following diagram illustrates the key factors influencing venetoclax pharmacokinetics and their clinical implications:
The validated LC-MS/MS method for simultaneous quantification of cobicistat and venetoclax represents a significant advancement in supporting innovative therapeutic strategies that cross traditional disciplinary boundaries between virology and oncology. The assay's performance characteristics—including wide dynamic range, excellent precision and accuracy, and rapid analysis time (less than 1.5 minutes per sample)—make it ideally suited for both therapeutic drug monitoring and pharmacokinetic studies in clinical trials [52].
The clinical implementation of this assay supports the rational development of venetoclax dosing strategies in combination with cobicistat, potentially addressing the high cost of venetoclax-based regimens through pharmacokinetic boosting [52]. Furthermore, the ability to simultaneously monitor both compounds provides valuable insights into exposure-response relationships and interaction management, ultimately contributing to improved patient outcomes.
This application note demonstrates that the simultaneous LC-MS/MS assay for cobicistat and venetoclax is robust, reproducible, and fit-for-purpose in clinical and research settings. The method efficiently supports therapeutic drug monitoring, adherence assessment, and pharmacokinetic studies, providing a valuable tool for optimizing combination therapies that leverage pharmacokinetic enhancement strategies.
The eradication of Helicobacter pylori (H. pylori), a primary cause of peptic ulcers and a significant risk factor for gastric cancer, relies on effective combination therapy [21] [56]. A novel triple therapy regimen, recently approved by the U.S. FDA, combines vonoprazan (VPN)—a potassium-competitive acid blocker (P-CAB)—with the antibiotics amoxicillin (AMX) and clarithromycin (CMN) [21] [57] [56]. Profound and sustained acid suppression is critical for successful eradication, as it enhances the stability and efficacy of the co-administered antibiotics [56]. Vonoprazan provides a superior pharmacological profile compared to traditional proton pump inhibitors (PPIs), including faster onset, more potent acid suppression, and less influence from genetic metabolic differences [21] [56].
Therapeutic Drug Monitoring (TDM) and pharmacokinetic (PK) studies are essential for optimizing dosing regimens, ensuring efficacy, and minimizing toxicity. For these purposes, a robust, specific, and sensitive bioanalytical method is required to simultaneously quantify the three drugs in human plasma [21]. This case study details the development and validation of a rapid LC-MS/MS method for the simultaneous quantification of vonoprazan, amoxicillin, and clarithromycin, framed within broader research on quantifying drug concentrations in plasma.
Method Development
Objectives and Challenges
The primary objective was to develop a single, rapid LC-MS/MS method capable of simultaneously quantifying VPN, AMX, and CMN in spiked human plasma [21]. A significant challenge was the lack of any previously validated LC-MS/MS method for this specific ternary combination in human plasma [21]. Existing methods often involved laborious sample preparation or were not applicable to all three analytes simultaneously [21]. The new method needed to address this gap by being rapid, sensitive, selective, and suitable for high-throughput clinical and pharmacokinetic studies.
Chromatographic Optimization
Achieving optimal chromatographic separation was a critical step in the method development process, requiring careful selection of the stationary phase and mobile phase composition.
- Stationary Phase: Initial tests with C8, phenyl, and polar-embedded columns did not yield satisfactory resolution or peak shapes for all analytes. The Phenomenex Kinetex C18 column (100 × 4.6 mm, 2.6 µm) was ultimately selected for its superior performance in providing excellent retention, peak symmetry, and resolution for VPN, AMX, and CMN [21].
- Mobile Phase and Gradient Elution: The best separation was achieved using a gradient elution system. Mobile Phase A consisted of 0.1% formic acid in water, and Mobile Phase B was 0.1% formic acid in acetonitrile [21]. The gradient program was optimized as follows:
Time (min) % Mobile Phase B 0.0 5 0.5 5 1.5 65 4.0 65 4.2 5 5.0 5
This gradient program successfully eluted all three analytes and the internal standard within a total run time of 5.0 minutes, facilitating high-throughput analysis [21].
Mass Spectrometric Detection
Detection was performed using a mass spectrometer operated in Multiple Reaction Monitoring (MRM) mode with positive electrospray ionization (ESI+) [21]. This mode offers high specificity and sensitivity for quantifying analytes in complex matrices like plasma. Diazepam was used as the internal standard (IS) to correct for variations during sample preparation and analysis [21].
Sample Preparation
A simple and efficient liquid-liquid extraction (LLE) technique was employed for sample preparation [21]. This method was chosen over more complex procedures like solid-phase extraction to enhance practicality and cost-effectiveness for routine analysis. The LLE protocol provided high and consistent recoveries for all analytes with negligible matrix effects [21].
Experimental Protocol
This section provides a detailed, step-by-step protocol for the quantitative analysis of vonoprazan, amoxicillin, and clarithromycin in human plasma.
Materials and Reagents
Table: Research Reagent Solutions
| Item | Specification / Function |
|---|---|
| Analytical Standards | Vonoprazan fumarate, Amoxicillin, Clarithromycin (all with purity ≥99%) |
| Internal Standard | Diazepam |
| HPLC Column | Phenomenex Kinetex C18 (100 × 4.6 mm, 2.6 µm) |
| Mobile Phase A | 0.1% (v/v) Formic Acid in Water |
| Mobile Phase B | 0.1% (v/v) Formic Acid in Acetonitrile |
| Extraction Solvent | Xylene (for Liquid-Liquid Extraction) |
| Matrix | Spiked Human Plasma |
Sample Preparation Procedure
- Spike Plasma Samples: Pipette 500 µL of human plasma into a microcentrifuge tube. Spike with appropriate volumes of VPN, AMX, and CMN working standard solutions and the internal standard (diazepam) solution.
- Protein Precipitation and Extraction: Add a predetermined volume of xylene (e.g., 1 mL) to the plasma sample.
- Vortex and Centrifuge: Vortex the mixture vigorously for 5 minutes to ensure complete extraction. Then, centrifuge at 10,000 × g for 10 minutes to separate the organic and aqueous layers.
- Collect Organic Layer: Carefully transfer the upper organic layer into a new, clean tube.
- Evaporate and Reconstitute: Evaporate the organic layer to dryness under a gentle stream of nitrogen. Reconstitute the dried residue with 200 µL of the initial mobile phase (e.g., 5% Mobile Phase B).
- Inject into LC-MS/MS: Transfer the reconstituted solution to an autosampler vial for analysis.
Instrumental Analysis
- LC System: Agilent 1200 Series HPLC system or equivalent.
- Mass Spectrometer: Triple quadrupole mass spectrometer capable of MRM detection.
- Column Oven Temperature: Maintained at 40°C.
- Injection Volume: 5 µL.
- Flow Rate: 0.8 mL/min.
- Autosampler Temperature: 4°C.
The experimental workflow from sample to result is summarized in the diagram below.
Method Validation
The developed LC-MS/MS method was subjected to a full validation according to FDA bioanalytical method validation guidelines. The key validation parameters and results are summarized below.
Table: Summary of Method Validation Parameters
| Validation Parameter | Result for AMX | Result for CMN | Result for VPN |
|---|---|---|---|
| Linear Range (ng/mL) | 2 - 100 | 2 - 100 | 5 - 100 |
| Lower Limit of Quantification (LLOQ) | 2 ng/mL | 2 ng/mL | 5 ng/mL |
| Intra-day Precision (RSD%) | < 15% | < 15% | < 15% |
| Inter-day Precision (RSD%) | < 15% | < 15% | < 15% |
| Accuracy (Relative Error %) | < 15% | < 15% | < 15% |
| Mean Absolute Recovery | > 93% | > 93% | > 93% |
| Matrix Effect | Negligible | Negligible | Negligible |
Specificity and Selectivity
The method demonstrated high specificity, with no significant interference from endogenous plasma components at the retention times of VPN, AMX, CMN, or the internal standard [21].
Sensitivity
The method proved highly sensitive, with Lower Limits of Quantification (LLOQs) of 2 ng/mL for AMX and CMN and 5 ng/mL for VPN [21]. These LLOQs are substantially lower than those reported in some earlier HPLC methods, ensuring the method's suitability for detecting low plasma concentrations in pharmacokinetic studies [21].
Greenness Assessment
The environmental impact of the analytical method was assessed using the AGREE tool [21]. The method scored highly, confirming its alignment with the principles of green analytical chemistry due to factors such as minimal solvent consumption and reduced waste generation [21].
Application in Pharmacokinetic Research
The validated method is ideally suited for applications in clinical pharmacology and drug development.
- Therapeutic Drug Monitoring (TDM): This rapid and sensitive method allows for the routine monitoring of plasma drug levels in patients undergoing H. pylori eradication therapy. This is crucial for ensuring therapeutic concentrations are maintained, checking patient adherence, and potentially managing toxicity [21].
- Pharmacokinetic and Bioequivalence Studies: The method's ability to simultaneously quantify all three drugs with a short run time makes it highly efficient for generating rich pharmacokinetic data (e.g., AUC, C~max~, T~max~, t~1/2~) in clinical trials, including bioequivalence studies of new formulations [21] [57].
- Correlating Concentration and Effect: Understanding the relationship between plasma drug concentrations and clinical effect is a cornerstone of pharmacology [58]. For systemically acting drugs like vonoprazan and its accompanying antibiotics, plasma concentration is often a useful surrogate for exposure at the site of action. The following diagram illustrates the central role of plasma concentration measurement in linking dose to effect, while also acknowledging scenarios where this relationship can be complex.
It is important to note that the free (unbound) drug fraction is generally considered the pharmacologically active species, as it is available to cross membranes and reach the site of action [59]. For drugs with high or variable protein binding, measuring the free concentration may provide a better correlation with the therapeutic effect [59]. Vonoprazan has a reported plasma protein binding of 85-88% [56].
This case study presents a fully validated, rapid, selective, and sensitive LC-MS/MS method for the simultaneous quantification of vonoprazan, amoxicillin, and clarithromycin in human plasma. The method addresses a critical gap in bioanalytical support for the novel vonoprazan-based triple therapy. Its validation in accordance with regulatory guidelines, combined with its high throughput and green chemistry attributes, makes it an ideal tool for advancing pharmacokinetic research, therapeutic drug monitoring, and the clinical development of this promising H. pylori eradication regimen.
Troubleshooting LC-MS/MS Assays: Solving Common Problems for Enhanced Performance
Diagnosing and Resolving Sensitivity and Accuracy Issues
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) is a powerful technique for the quantitative analysis of drug concentrations in plasma, prized for its high selectivity, sensitivity, and specificity [60]. However, developing a robust bioanalytical method is a complex process, and scientists often encounter challenges related to sensitivity (the ability to detect and quantify low analyte levels) and accuracy (the closeness of the measured value to the true value) [60]. These issues can stem from multiple factors within the sample preparation, chromatographic separation, and mass spectrometric detection stages. This application note provides a structured framework for diagnosing and resolving these critical issues, ensuring the generation of reliable and reproducible data for pharmaceutical research and development.
Troubleshooting Guide: Common Issues and Solutions
The following table summarizes common symptoms, their potential causes, and recommended corrective actions for sensitivity and accuracy issues in LC-MS/MS assays.
Table 1: Troubleshooting Guide for Sensitivity and Accuracy in LC-MS/MS
| Observed Symptom | Potential Root Cause | Diagnostic Experiments | Recommended Corrective Actions |
|---|---|---|---|
| Low Sensitivity | Inefficient ionization | Compare ionization modes (ESI vs. APCI); infuse analyte to optimize voltages and gas flows [61]. | Switch ionization mode (e.g., ESI for polar/ionizable compounds); manually tune source parameters for maximum signal [61]. |
| High matrix effect | Post-column infuse analyte and inject blank matrix extract; analyze spiked samples in different matrix lots [60]. | Improve sample clean-up (e.g., switch from PPT to SPE or LLE); optimize chromatography to separate analyte from ion suppressors; use a stable isotope-labeled internal standard [62]. | |
| Analyte loss during sample prep | Perform recovery experiments by comparing extracted samples to post-extraction spiked samples [60]. | Modify extraction protocol (pH, solvent); change extraction technique (e.g., LLE to SLE); use a different sorbent for SPE [62]. | |
| Poor Accuracy/Incorrect Quantification | Inadequate chromatographic separation | Inject a representative sample and acquire a full-scan mass spectrum to check for co-eluting peaks [61]. | Optimize the LC gradient and mobile phase; change the column chemistry (e.g., C18 to phenyl); increase column length or decrease particle size [62] [61]. |
| Instability of the analyte | Analyze QC samples over a single run; perform bench-top and freeze-thaw stability tests [60]. | Adjust sample pH; use specific collection tubes (e.g., K2EDTA); add stabilizers to the matrix; ensure samples are stored at correct temperature [63]. | |
| Insufficient method specificity | Analyze blank matrix samples from at least six different sources to check for interferences [64]. | Select a more specific MRM transition; improve sample cleanup; use a high-resolution mass analyzer for additional selectivity [64] [22]. |
Core Experimental Protocols for Issue Diagnosis
Protocol: Assessing and Mitigating Matrix Effects
Matrix effects occur when co-eluting compounds from the sample suppress or enhance the ionization of the analyte, leading to inaccurate quantification [60].
Materials:
- Test Solutions: Blank human plasma or serum from at least six different individuals [64].
- Working Solutions: Analyte and internal standard (IS) at medium QC concentration.
- Equipment: LC-MS/MS system with infusion capability.
Procedure:
- Post-Column Infusion Assay:
- Prepare a neat solution of the analyte at a concentration that produces a stable signal.
- Connect a tee-union between the LC column outlet and the MS source.
- Continuously infuse the analyte solution via a syringe pump while injecting a blank, extracted plasma sample onto the LC column.
- Monitor the MRM transition for the analyte. A dip or peak in the baseline signal at the retention time of the analyte indicates ion suppression or enhancement from the matrix [60].
- Calculation of Matrix Factor (MF):
- Prepare two sets of samples in triplicate:
- Set A (Post-extraction spiked): Spike the analyte and IS into the supernatant of extracted blank plasma.
- Set B (Neat solution): Prepare the analyte and IS in mobile phase or reconstitution solvent at the same concentration.
- Inject all samples and record the peak areas for the analyte and IS.
- Calculate the Matrix Factor (MF) using the formula:
MF = (Peak Area of Post-extraction Spiked Sample / Peak Area of Neat Solution) - An MF significantly different from 1.0 indicates a matrix effect. The internal standard should correct for this if its MF is similar to the analyte's. The precision of the MF across different matrix lots should be ≤15% [60].
- Prepare two sets of samples in triplicate:
Protocol: Optimizing Ionization and MS Parameters
Sensitivity is highly dependent on the efficient generation and transmission of gas-phase ions.
Materials:
- Test Solutions: Standard solution of the analyte (e.g., 1 µg/mL) in a 50:50 mixture of organic mobile phase and 10 mM ammonium formate buffer at pH 2.8 and 8.2 [61].
- Equipment: LC-MS/MS system with autotune and manual tuning capabilities.
Procedure:
- Ionization Mode and Polarity Selection:
- Infuse the analyte solution directly into the mass spectrometer.
- Acquire spectra in both positive and negative ion modes using the autotune routine.
- Select the ionization polarity that yields the highest and most stable signal for the protonated
[M+H]+or deprotonated[M-H]-molecular ion.
- Source Parameter Optimization:
- Using the selected polarity, perform a manual tune. Key parameters to optimize include ion spray voltage, source temperature, and nebulizer and desolvation gas flows.
- Adjust these parameters while monitoring the signal intensity of the precursor ion. Critical Tip: Set the value on a maximum plateau where small changes do not produce a large change in response, ensuring method robustness [61].
- MRM Optimization:
- Using the optimized source conditions, infuse the analyte and select the precursor ion.
- Introduce collision gas and systematically vary the collision energy (CE) voltage.
- Identify 2-3 abundant product ions and optimize the CE for each to achieve 10-15% of the precursor ion remaining, maximizing product ion signal [61].
- For large molecules that form multiple charge states, consider using Sum of MRM (SMRM), which sums the signals from multiple precursor-product ion pairs to boost sensitivity [65].
Workflow Visualization
The following diagram illustrates the logical workflow for diagnosing and resolving sensitivity and accuracy issues.
The Scientist's Toolkit: Essential Research Reagent Solutions
The selection of appropriate reagents and materials is fundamental to developing a successful LC-MS/MS method. The table below details key solutions used in the featured protocols and the broader field.
Table 2: Key Research Reagent Solutions for LC-MS/MS Method Development
| Item | Function/Application | Brief Explanation & Example |
|---|---|---|
| Stable Isotope-Labeled Internal Standard (IS) | Corrects for analyte loss during preparation and matrix effects [62]. | An isotopically labeled version of the analyte (e.g., ABZ-d3) behaves identically but is distinguished by the MS, normalizing for variability [66]. |
| Solid-Phase Extraction (SPE) | Sample clean-up and pre-concentration for complex matrices [62]. | Uses a sorbent (e.g., C18) to retain analytes while washing away matrix components, yielding cleaner extracts and reduced ion suppression compared to protein precipitation [66]. |
| Supported Liquid Extraction (SLE) | High-throughput alternative to liquid-liquid extraction (LLE) [62]. | Sample is dispersed into a diatomaceous earth bed; analytes are eluted with organic solvent, offering cleaner extracts than PPT with better reproducibility than LLE [62]. |
| LC-MS Grade Mobile Phase Additives | Ensures sensitivity and prevents source contamination. | High-purity acids (e.g., formic acid) and volatile buffers (e.g., ammonium acetate/formate) promote ionization and are compatible with MS, unlike non-volatile buffers [64] [63]. |
| UPLC BEH C18 Column | High-efficiency chromatographic separation [63] [66]. | Columns with small, uniform particles (e.g., 1.7 µm) provide superior resolution, sharper peaks, and increased sensitivity, effectively separating analytes from matrix interferences [63]. |
| DJ001 | (Z)-3-(3-nitroanilino)-1-phenylprop-2-en-1-one|RUO | |
| GLUT1-IN-2 | N-(3-(1H-Benzo[d]imidazol-2-yl)phenyl)-3-methylbenzamide |
Sensitivity and accuracy issues in LC-MS/MS bioanalysis are multifactorial but can be systematically diagnosed and resolved. A methodical approach—investigating sample preparation efficiency, quantitatively assessing matrix effects, ensuring optimal chromatographic separation, and fine-tuning mass spectrometric detection—is key to success. By adhering to the detailed protocols and utilizing the essential tools outlined in this document, scientists can enhance the robustness of their methods, ensuring the generation of high-quality, reliable data crucial for advancing drug development.
Mitigating Matrix Effects and Ion Suppression in Complex Plasma Samples
Matrix effects and ion suppression represent significant challenges in the quantitative analysis of drugs in plasma using liquid chromatography-tandem mass spectrometry (LC-MS/MS). These phenomena occur when co-eluting matrix components from the sample interfere with the ionization process of the target analytes in the mass spectrometer source, leading to diminished or enhanced signal response and compromising analytical accuracy, precision, and sensitivity [67]. In electrospray ionization (ESI), which is capacity-limited, an excess of competing ions within the droplet can reduce ionization efficiency, negatively impacting the reliability of analytical results [68]. When matrix components and analytes co-elute, they compete for the limited charge available during ionization, resulting in reduced ion formation for the analyte (ion suppression) [67]. Conversely, suppression of the analyte itself can produce a negative bias, while suppression of internal standards can lead to overestimation of analyte concentration [68]. Neither scenario is acceptable in pharmaceutical research and bioanalysis, where quantitative measurements inform critical decisions in drug development and therapeutic monitoring.
Detection and Assessment of Matrix Effects
Established Detection Methodologies
Researchers employ several experimental techniques to identify and quantify matrix effects during method development and validation:
Post-Extraction Spiking: This method evaluates matrix effects by comparing the signal response of an analyte in neat mobile phase with the signal response of an equivalent amount of the analyte in a blank matrix sample spiked post-extraction. The difference in response indicates the extent of the matrix effect [69]. A significant challenge with this approach is that for endogenous analytes, a truly blank matrix is not available.
Post-Column Infusion: This technique qualitatively assesses matrix effects by infusing a constant flow of analyte into the HPLC eluent while injecting a blank sample extract. Variations in the signal response of the infused analyte caused by co-eluting interfering compounds indicate regions of ionization suppression or enhancement in the chromatogram [69] [68]. While valuable for identifying problematic retention time windows, this process is time-consuming, requires additional hardware, and presents challenges for multi-analyte methods.
A Simplified Recovery-Based Approach
A simpler, recovery-based method has been proposed for detecting matrix effects that can be applied to any analyte, including endogenous compounds, without requiring specialized equipment [69]. This approach involves comparing the measured concentration in a prepared sample against the expected value, with discrepancies indicating potential matrix effects. This practical method facilitates routine assessment of matrix effects in complex samples like plasma.
Strategic Approaches for Mitigation
Multiple strategies exist to mitigate the impact of matrix effects, ranging from sample preparation techniques to sophisticated calibration methods.
Sample Preparation and Chromatographic Optimization
Table 1: Sample Preparation Techniques for Mitigating Matrix Effects
| Technique | Mechanism of Action | Key Considerations |
|---|---|---|
| Solid Phase Extraction (SPE) | Selectively extracts analytes while removing salts, phospholipids, and other non-specific matrix compounds that contribute to ion suppression [70] [67]. | Can be optimized to retain target analytes and wash away interferences. May require method development for different analyte classes. |
| Liquid-Liquid Extraction (LLE) | Partitions analytes away from hydrophilic matrix components based on solubility differences, effectively reducing ionizable interferents [21] [68]. | High and consistent recoveries (e.g., >93%) can be achieved with minimal matrix effects [21]. |
| Protein Precipitation | Removes proteins from plasma samples via organic solvent addition. | A simple and fast technique, but may be less effective at removing other ion-suppressing compounds compared to SPE or LLE [67]. |
| Sample Dilution | Reduces the absolute amount of matrix components entering the LC-MS system. | Only feasible when the assay sensitivity is sufficiently high to accommodate the dilution [69]. |
Optimizing chromatographic conditions is equally critical. Adjusting the mobile phase composition, gradient profile, and flow rate can improve the separation of analytes from matrix components, thereby reducing co-elution and the associated ion suppression [67] [69]. The goal is to achieve chromatographic resolution that shifts the analyte retention time away from regions with severe ion suppression, as identified by post-column infusion.
Internal Standardization and Calibration Techniques
Table 2: Calibration and Standardization Strategies
| Strategy | Principle | Advantages and Limitations |
|---|---|---|
| Stable Isotope-Labeled Internal Standards (SIL-IS) | Uses a chemically identical but isotopically heavy version of the analyte that co-elutes with the native compound, experiencing nearly identical matrix effects and compensating for them in quantification [70] [71] [68]. | Considered the gold standard. However, deuterated standards ((^{2}\text{H})) may exhibit slight retention time shifts; (^{13}\text{C}) or (^{15}\text{N})-labeled standards are ideal for perfect co-elution [71]. Can be expensive or unavailable for novel compounds. |
| Matrix-Matched Calibration | Prepares calibration standards in the same biological matrix as the study samples (e.g., plasma) to mirror the matrix effects experienced by unknown samples. | Accounts for matrix-induced changes. Requires a significant volume of blank matrix, which may not be available, and it is impossible to exactly match the matrix of every individual sample [67] [69]. |
| Standard Addition | Spikes known concentrations of the analyte directly into the sample aliquot. This method is particularly useful for endogenous analytes where a blank matrix is unavailable [69]. | Does not require a blank matrix. However, it is more labor-intensive and requires a larger sample volume, making it less suitable for high-throughput analyses. |
The following workflow diagram illustrates the decision process for selecting and applying these key mitigation strategies:
Detailed Experimental Protocols
Protocol 1: Evaluating Matrix Effects via Post-Extraction Spiking
Objective: To quantitatively assess the magnitude of ion suppression/enhancement for a target analyte in a specific plasma matrix.
Materials and Reagents:
- Blank plasma matrix (from at least 6 different sources)
- Stock solutions of target analyte and internal standard
- Appropriate solvents and reagents for sample preparation (e.g., methanol, acetonitrile, formic acid)
- LC-MS/MS system
Procedure:
- Prepare Neat Solutions: Prepare a set of analyte solutions in a neat solvent (e.g., mobile phase) at low, medium, and high concentrations within the calibration range.
- Prepare Post-Extraction Spiked Samples: a. Extract blank plasma samples from multiple donors using your optimized sample preparation protocol. b. Spike the same concentrations of analyte from Step 1 into the final extracts of the blank matrix.
- LC-MS/MS Analysis: Analyze both the neat solutions and the post-extraction spiked samples.
- Calculation: For each concentration, calculate the matrix effect (ME) as:
ME (%) = (Peak Area of Post-Extraction Spiked Sample / Peak Area of Neat Solution) × 100 - Interpretation: An ME of 100% indicates no matrix effect. Values <85% or >115% typically signify significant ion suppression or enhancement, respectively. The coefficient of variation of ME across different plasma lots should be <15% [69].
Protocol 2: Implementing Stable Isotope-Labeled Internal Standards
Objective: To incorporate a SIL-IS for correcting matrix effects, instrument variability, and preparation losses.
Materials and Reagents:
- (^{13}\text{C}) or (^{15}\text{N})-labeled internal standard (optimal for co-elution)
- Calibration standards and quality control samples in plasma
- Sample preparation materials
Procedure:
- Addition of SIL-IS: Add a fixed, appropriate concentration of the SIL-IS to all samples, calibration standards, and quality control (QC) samples before the sample preparation step begins.
- Sample Preparation and Analysis: Proceed with the routine sample preparation and LC-MS/MS analysis.
- Calibration and Quantification: a. Construct a calibration curve by plotting the peak area ratio (analyte / SIL-IS) against the nominal concentration of the calibration standards. b. Use the linear regression of this curve to calculate the concentration of the analyte in unknown and QC samples based on their measured peak area ratio.
- Verification: The internal standard corrects for variability by mirroring the behavior of the analyte. Its effectiveness relies on its co-elution with the analyte, ensuring it experiences identical matrix effects [70] [71].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Mitigating Matrix Effects in Plasma Analysis
| Research Reagent | Function & Rationale | Application Example |
|---|---|---|
| Stable Isotope-Labeled Internal Standards (SIL-IS) | Corrects for matrix effects, extraction efficiency, and instrument variability by behaving almost identically to the native analyte [70] [71] [68]. | Quantification of ethanolamines in complex wastewaters was achieved using one SIL-IS per target compound to correct for severe ion suppression from salts and organic matter [70]. |
| Mixed-Mode Solid Phase Extraction (SPE) Sorbents | Provide multiple mechanisms (e.g., reversed-phase, ion-exchange) for selective cleanup, effectively removing diverse matrix interferences like salts and phospholipids from plasma [70]. | A mixed-mode LC column (Acclaim Trinity P1) was deployed to help separate and analyze ethanolamines in high-salinity produced water [70]. |
| High-Purity Mobile Phase Modifiers | Acids (e.g., formic acid) and volatile salts in the mobile phase improve chromatographic peak shape and ionization efficiency without causing persistent source contamination or suppression. | 0.1% formic acid in both water and acetonitrile was used as the mobile phase for rapid separation of drugs in human plasma within a 5-minute run time [21] [14]. |
| Liquid-Liquid Extraction (LLE) Solvents | Organic solvents (e.g., ethyl acetate, methyl tert-butyl ether) partition analytes away from hydrophilic plasma matrix components, offering a clean extract with minimal ion suppression. | A simple and efficient LLE technique using xylene provided high recoveries (93–104%) for a triple therapy regimen in plasma with negligible matrix effects [21]. |
| hDHODH-IN-7 | DHODH-IN-9|Human DHODH Inhibitor|CAS 1644156-41-1 | DHODH-IN-9 is a potent human dihydroorotate dehydrogenase (DHODH) inhibitor for antiviral research. For Research Use Only. Not for human use. |
| PF-06952229 | PF-06952229, CAS:1801333-55-0, MF:C23H24ClFN4O3, MW:458.9 g/mol | Chemical Reagent |
Effectively mitigating matrix effects and ion suppression is not merely a validation requirement but a fundamental aspect of developing robust, accurate, and reliable LC-MS/MS methods for quantifying drugs in complex plasma samples. A multi-faceted approach is most effective, beginning with optimized sample preparation to remove interferents, followed by chromatographic separation to avoid co-elution. The use of a well-chosen stable isotope-labeled internal standard remains the most powerful tool for compensating any residual matrix effects. By systematically implementing these strategies—detection, mitigation, and correction—researchers can ensure the generation of high-quality data that reliably supports drug development and therapeutic monitoring.
In the development of robust and sensitive Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) methods for quantifying drug concentrations in plasma, the optimization of the ion source parameters is a critical step. The ionization process is the fundamental bridge where analytes in the liquid chromatographic eluent are converted into gas-phase ions, making them amenable to mass analysis. The efficiency of this process directly dictates the sensitivity, reproducibility, and overall success of a bioanalytical method. Within the ion source, the capillary voltage (also referred to as sprayer voltage or ion spray voltage) and the gas settings (nebulizing, drying, and heater gases) are among the most influential parameters. Their careful optimization ensures stable electrospray operation, maximizes ion yield, and minimizes signal suppression, which is paramount for detecting low-abundance analytes in complex matrices like human plasma. This application note provides a detailed, practical framework for systematically optimizing these key parameters to achieve maximum ionization efficiency in quantitative LC-MS/MS assays.
Theoretical Foundations of Electrospray Ionization
Electrospray Ionization (ESI) is a soft ionization technique that operates at atmospheric pressure and is exceptionally well-suited for the analysis of thermolabile and high-molecular-weight compounds, including many pharmaceuticals and their metabolites [72] [73]. The mechanism involves multiple stages:
- Droplet Formation: The LC eluent, containing the analyte, is pumped through a metal or metallized capillary held at a high voltage (typically 2.5–6.0 kV). This high potential charges the surface of the liquid, leading to the formation of a Taylor cone at the capillary tip, from which a fine mist of charged droplets is emitted [74] [73].
- Droplet Desolvation: The charged droplets travel towards the mass spectrometer's orifice, assisted by a flow of nebulizing gas and a stream of heated drying gas. These gases facilitate the evaporation of the solvent, causing the droplets to shrink and significantly increase their surface charge density [75] [73].
- Ion Emission: When the Rayleigh limit is reached, the Coulombic repulsion within the droplet overcomes its surface tension, leading to Coulombic fissions and the eventual release of gas-phase analyte ions [74] [73].
The stability and efficiency of this entire process are governed by the source parameters. The capillary voltage provides the primary electrostatic force for droplet dispersal and charging. In contrast, the gas settings control the initial droplet size and the efficiency of solvent evaporation, which are critical for producing a stable ion plume and preventing the introduction of solvent clusters into the high-vacuum region of the mass spectrometer [75] [76].
Systematic Parameter Optimization
Capillary Voltage Optimization
The capillary voltage is the primary driver for the electrospray process. Its optimal setting is a balance between achieving sufficient ionization and avoiding non-ideal spray modes.
- Principle: The applied voltage must be high enough to form a stable Taylor cone and produce a fine aerosol of charged droplets. However, excessively high voltages can lead to corona discharge, characterized by the formation of protonated solvent clusters (e.g., H3O+(H2O)n in aqueous mobile phases), which causes an unstable signal and increased chemical noise [77] [75]. Operation at voltages that are too low, on the other hand, fails to achieve a stable electrospray, leading to poor sensitivity.
- Gradient Elution Consideration: During a reversed-phase LC gradient, the eluent composition changes from aqueous to organic. The optimum capillary voltage decreases as the concentration of organic solvent increases because organic solvents have lower surface tension and are more easily ionized [77]. Therefore, a voltage set at the beginning of a gradient may not be optimal for analytes eluting later. For methods requiring ultimate sensitivity, one may need to optimize the voltage at the specific organic solvent concentration at which the analyte elutes [74].
- Protocol for Optimization:
- Infusion Setup: Connect a syringe pump to the LC flow path via a T-union, allowing a standard solution of the analyte (e.g., 100-500 ng/mL in the starting mobile phase composition) to be infused post-column at the method's flow rate.
- Initial Conditions: Set the source temperature and gas flows to estimated values (see Section 3.2). Begin with a capillary voltage of 3.0 kV for positive mode or 2.5 kV for negative mode.
- Data Acquisition: Monitor the signal of the protonated or deprotonated analyte molecule ([M+H]+ or [M-H]-) in Selected Ion Recording (SIR) or Multiple Reaction Monitoring (MRM) mode.
- Voltage Ramp: Incrementally increase the capillary voltage (e.g., in steps of 0.1-0.2 kV) and record the analyte response at each step. A typical optimization range is 2.0–5.0 kV.
- Identify Optimum: Plot the signal intensity against the applied voltage. The optimum voltage is typically at the plateau region just before the signal becomes unstable or begins to decrease due to discharge or adverse side reactions [75]. For open-access systems, using a slightly lower voltage is often advised to promote long-term stability [75].
Table 1: Troubleshooting Capillary Voltage-Related Issues
| Observation | Potential Cause | Corrective Action |
|---|---|---|
| Unstable signal, high baseline noise | Corona discharge | Reduce capillary voltage; consider adding 1-2% organic solvent to highly aqueous mobile phases [75] |
| Low signal for all analytes | Voltage too low; unstable spray | Increase capillary voltage incrementally |
| Signal intensity highly variable between runs | Rim emission or erratic spray | Optimize nebulizing gas flow and capillary voltage; ensure mobile phases contain volatile additives [77] [75] |
| Formation of sodium/potassium adducts | Metal ion contamination | Use LC-MS grade solvents and additives; use plastic vials instead of glass; include a chelating agent in sample prep [75] |
Gas Settings Optimization
The gas flows work in concert with the capillary voltage to desolvate the analyte and stabilize the electrospray.
- Nebulizing Gas (N2): This gas shears the liquid stream at the capillary tip, constraining the initial droplet size and helping to form a finer aerosol. Higher flows generally produce smaller initial droplets, which can improve desolvation efficiency, especially at higher LC flow rates or with aqueous mobile phases [44] [75].
- Drying/Desolvation Gas (N2): This is a heated stream of nitrogen that flows coaxially around the spray to accelerate solvent evaporation from the charged droplets. Efficient desolvation is critical for generating gas-phase ions and preventing solvent clusters from entering the mass analyzer [74].
- Source Temperature: This parameter aids the desolvation process. However, for thermally labile analytes, excessive temperatures can cause degradation before ionization, as was observed for emamectin benzoate B1a when the desolvation temperature was increased beyond 500°C [74].
Table 2: Typical Ranges and Functions of ESI Gas Parameters
| Parameter | Function | Typical Range | Optimization Guideline |
|---|---|---|---|
| Nebulizing Gas | Constricts droplet size at the tip for a stable spray. | 20-80 psi (or arbitrary units 5-10) | Increase for higher flow rates and highly aqueous mobile phases [44] [75]. |
| Drying Gas | Evaporates solvent from charged droplets. | 30-70 psi (or L/min, instrument-dependent) | Increase flow and temperature for efficient desolvation; balance with analyte thermal stability [74]. |
| Source Temperature | Provides heat to assist solvent evaporation. | 200°C - 600°C | Set as high as possible without degrading thermally labile analytes [74]. |
Table 3: Exemplary Optimized Source Parameters from Clinical LC-MS/MS Methods
| Analyte | Capillary Voltage | Nebulizing Gas | Drying Gas | Temperature | Mobile Phase | Citation |
|---|---|---|---|---|---|---|
| Omadacycline | Not Specified | Not Specified | Not Specified | Not Specified | 0.1% Formic Acid in Water / Acetonitrile | [14] |
| Clonidine | 4000 V | 10 (arb. units) | 8 (arb. units) | 250°C | Acetonitrile-Water (60:40) + 0.2% Formic Acid | [78] |
Protocol for Gas Optimization:
- Initial Setup: Begin with the capillary voltage at the previously optimized value or a manufacturer's default. Infuse an analyte standard.
- Nebulizing Gas: With the drying gas and temperature set to mid-range values, incrementally increase the nebulizing gas flow while monitoring the analyte signal. The signal will typically increase to a maximum and then plateau or slightly decrease.
- Drying Gas and Temperature: With the optimized nebulizing gas, now incrementally increase the drying gas flow and temperature. These two parameters are often interrelated and can be optimized together. The goal is to find the setting where the signal is maximized.
- Final Fine-Tuning: Once all parameters have been roughly optimized, a final fine-tuning round may be conducted, as interactions between parameters can sometimes occur.
Integrated Optimization Workflow
The following diagram illustrates the logical sequence for a systematic approach to source optimization, integrating both capillary voltage and gas settings.
The Scientist's Toolkit: Essential Research Reagents and Materials
The reliability of LC-MS/MS data is heavily dependent on the quality of materials used throughout the workflow.
Table 4: Essential Materials for Robust LC-MS/MS Method Development
| Item | Function | Key Considerations |
|---|---|---|
| LC-MS Grade Water | Aqueous mobile phase component. | Use bottled hypergrade water or water from a Milli-Q purification system to minimize ionic contaminants and organic impurities [76]. |
| LC-MS Grade Acetonitrile & Methanol | Organic mobile phase components. | Use hypergrade solvents labeled for LC-MS to reduce background noise and prevent ghost peaks [76]. |
| Volatile Additives | Promote analyte protonation/deprotonation. | Formic acid, acetic acid, ammonium acetate, and ammonium formate are standard. Avoid non-volatile buffers (e.g., phosphates) and ion-pairing reagents like TFA, which cause signal suppression [44] [76]. |
| Protein Precipitant | Clean up plasma samples. | Methanol or acetonitrile are commonly used. Perchloric acid was used successfully for clonidine [78]. |
| Plastic Vials & Containers | Store samples and solvents. | Preferred over glass to avoid leaching of metal ions that form adducts (e.g., [M+Na]+). Ensure they are tested for leachables [75] [76]. |
| Internal Standard | Normalize for variability. | Stable isotope-labeled analogs of the analyte (e.g., fexofenadine-d6) are ideal for correcting for matrix effects and injection variability [14] [78]. |
| Osimertinib D6 | Osimertinib D6, MF:C28H33N7O2, MW:505.6 g/mol | Chemical Reagent |
| IDE-IN-1 | IDE-IN-1, CAS:1417537-93-9, MF:C41H55N7O7, MW:757.933 | Chemical Reagent |
The meticulous optimization of ion source parameters is non-negotiable for developing sensitive and reliable LC-MS/MS methods for drug quantification in plasma. A systematic approach, beginning with the capillary voltage to establish a stable electrospray, followed by the optimization of nebulizing and drying gas flows and temperatures to ensure efficient desolvation, yields significant dividends in method performance. This process is greatly aided by infusing the analyte of interest and monitoring the signal response while varying one parameter at a time. Furthermore, the use of high-purity reagents and appropriate materials is fundamental to maintaining low background noise and preventing adduct formation. By adhering to the detailed protocols and guidelines outlined in this application note, researchers and drug development professionals can consistently maximize ionization efficiency, thereby lowering detection limits and enhancing the quality of their pharmacokinetic and therapeutic drug monitoring data.
Improving Chromatographic Peak Shape and Retention
In the development of robust and sensitive LC-MS/MS methods for quantifying drug concentrations in plasma, the quality of chromatographic peaks is paramount. Optimal peak shape and consistent retention are critical for achieving reliable separation, accurate identification, and precise quantification, especially when dealing with complex biological matrices [79] [14]. Peak distortions, such as tailing, fronting, or broadening, can severely compromise data integrity, leading to reduced sensitivity, poor reproducibility, and inaccurate pharmacokinetic conclusions [80] [81]. This application note provides a detailed framework for diagnosing and resolving common peak shape and retention issues within the specific context of LC-MS/MS bioanalysis for drug quantification in plasma, featuring structured protocols, key reagent solutions, and visual guides for method optimization.
The Critical Role of Peak Shape in Bioanalytical Method Validation
In regulated bioanalysis, peak quality directly impacts method validation parameters. Well-shaped, symmetrical Gaussian peaks are ideal as they facilitate more accurate integration, improve detection sensitivity, and allow for a higher peak capacity within a given chromatographic run time [81]. Non-ideal peak shapes can indicate underlying problems such as column packing issues, secondary chemical interactions, or suboptimal instrument settings [81].
Table 1: Impact of Peak Shape on Method Performance
| Peak Characteristic | Ideal Outcome | Consequence of Poor Performance |
|---|---|---|
| Symmetry | Gaussian, symmetrical shape (Tailing Factor ~1) | Inaccurate integration, reduced resolution between peaks |
| Efficiency (Theoretical Plates, N) | High plate number | Broad peaks, lower sensitivity, and poor separation |
| Retention Time | Consistent and reproducible | Inaccurate analyte identification and quantification |
| Peak Width | Narrow and consistent | Decreased signal-to-noise ratio, higher limit of quantification |
For LC-MS/MS assays, such as those developed for drugs like omadacycline or contezolid in plasma, a consistent retention time is vital for correct analyte identification using multiple reaction monitoring (MRM), while a narrow peak width concentrates the analyte signal, enhancing the lower limit of quantification (LLOQ) [79] [14]. The U.S. Food and Drug Administration (FDA) often recommends a tailing factor of ≤2 for acceptance of analytical methods [81].
A Systematic Approach to Diagnosing and Improving Peak Shape
Troubleshooting peak shape issues requires a structured methodology, changing only one parameter at a time to isolate the root cause [80]. The following workflow provides a logical sequence for investigation and optimization.
Sample and System Preparation
The journey to optimal peaks begins with sample integrity and system cleanliness.
- Sample Preparation: Plasma samples require deproteinization to prevent column fouling and interference. Protein precipitation (PP) using organic solvents like acetonitrile or methanol is a common and effective approach [79] [14]. For the analysis of contezolid, protein precipitation provided satisfactory recovery with minimal matrix effect, simplifying the extraction process [79]. However, PP may not remove salts and lipids completely, which can interfere with analysis [79].
- Mobile Phase Composition: The choice of mobile phase additives significantly impacts peak shape. For basic analytes analyzed in positive ion mode LC-MS/MS, the addition of 0.1% formic acid is common. This additive improves protonation, enhances signal response in the MS, and reduces peak tailing by masking silanol interactions on the stationary phase [79] [14]. Buffer ionic strength and pH are also critical for controlling analyte retention and selectivity [80].
- Column Selection: The stationary phase is the heart of the separation. C18 columns are the workhorse for reversed-phase LC-MS/MS [79] [14]. Columns packed with smaller particles (e.g., sub-2µm) provide higher efficiency and better resolution but require instruments that can handle higher backpressures [80]. The selection of a column with appropriate selectivity for the analyte is crucial.
Instrumental Parameters and Data Acquisition
After addressing preparation and chemistry, fine-tuning the instrument is essential.
- Flow Rate and Column Temperature: In most cases, lowering the flow rate will decrease the retention factor, making peaks narrower and improving response [80]. Higher column temperatures allow for faster analysis but can risk sample degradation and lower resolution, while lower temperatures improve retention and peak shape at the cost of longer run times [80].
- Injection Volume: Overloading the column with too much sample (mass overload) causes peak fronting and decreased retention time, negatively impacting resolution [80]. A general rule is to inject 1-2% of the total column volume for sample concentrations around 1 µg/µL [80].
- Detector Settings: For modern mass spectrometers acting as detectors, ensuring sufficient data acquisition rate is vital. A minimum of 20-40 data points across a peak is required for optimal peak shape representation and accurate quantification [80].
Experimental Protocol: Optimizing an LC-MS/MS Method for Plasma Analysis
This protocol outlines the key experiments for optimizing peak shape and retention during the development of an LC-MS/MS method for drug quantification in plasma, using principles applied in recent studies [79] [14].
Materials and Reagents
Table 2: Key Research Reagent Solutions for LC-MS/MS Bioanalysis
| Item | Function/Application | Example from Literature |
|---|---|---|
| C18 Chromatographic Column | Reversed-phase separation of analytes. | Phenomenex KINETEX XB-C18 [14], Agilent Eclipse Plus C18 [79] |
| Acetonitrile (HPLC grade) | Organic solvent for mobile phase and protein precipitation. | Used in mobile phase and sample prep for omadacycline and contezolid [79] [14] |
| Formic Acid (HPLC grade) | Mobile phase additive to improve ionization and peak shape. | 0.1% Formic acid in water and/or acetonitrile [79] [14] |
| Ammonium Acetate | Buffer salt for controlling mobile phase pH and ionic strength. | 10 mM aqueous ammonium acetate used for contezolid [79] |
| Internal Standard | Corrects for variability in sample prep and ionization. | Fexofenadine-d6 for omadacycline [14], Linezolid for contezolid [79] |
Step-by-Step Optimization Procedure
Initial Column and Mobile Phase Scouting
- Select 2-3 different C18 columns (e.g., from different manufacturers, with varying particle sizes like 3.5µm and 1.7-2.6µm) [80] [79] [14].
- Prepare a standard solution of the analyte in a compatible solvent (e.g., acetonitrile/water) at a mid-range concentration.
- Start with a simple, generic gradient (e.g., 5-95% acetonitrile in water, both with 0.1% formic acid, over 10 minutes) at a flow rate of 0.3-0.6 mL/min [14].
- Inject the standard and evaluate the chromatogram for retention factor, peak symmetry, and signal intensity.
Mobile Phase Additive and pH Screening
- If peak tailing is observed (common for basic compounds), test different acidic additives. Compare 0.1% formic acid against alternatives like 10 mM ammonium formate, adjusting the pH if necessary [79].
- For each condition, inject the analyte standard and note the impact on peak shape and MS signal response.
Fine-Tuning Chromatographic Conditions
- Once a promising column/additive combination is found, optimize the gradient profile to achieve the desired retention time (typically 1.5-3 times the void volume) and separation from potential interferences.
- Experiment with column temperature (e.g., 30°C, 40°C, 50°C) to improve efficiency and reduce backpressure [80].
- Evaluate the effect of flow rate on backpressure and peak width. A lower flow rate often yields narrower peaks but increases run time [80].
Sample Preparation Optimization in Plasma Matrix
- Spike the analyte into blank plasma to create quality control (QC) samples.
- Precipitate proteins by adding a volume of internal standard solution in acetonitrile (e.g., 200 µL to 50 µL of plasma) [14]. Vortex and centrifuge.
- Inject the processed plasma sample and compare the peak shape and ion suppression/enhancement (matrix effect) to a neat standard at the same concentration. A significant difference indicates a need for further sample clean-up or adjustment of the precipitation protocol.
Final Method Validation with Plasma Samples
- Once optimal conditions are established, validate the method by analyzing a calibration curve and QC samples in replicates across different batches.
- Assess critical validation parameters including linearity, precision, accuracy, and lower limit of quantification (LLOQ), ensuring the peak shape and retention time are consistent and reliable for all samples [79] [14].
Achieving and maintaining ideal chromatographic peak shape and retention is a foundational element in developing a robust LC-MS/MS method for plasma drug analysis. By adhering to a systematic troubleshooting workflow that meticulously examines sample preparation, mobile phase chemistry, column selection, and instrument parameters, scientists can effectively diagnose and resolve common issues. The experimental protocols and reagent solutions detailed in this application note provide a practical roadmap for optimizing bioanalytical methods, ultimately leading to more reliable data, successful method validation, and confident decision-making in drug development and therapeutic drug monitoring.
Preventive Maintenance and LC Hygiene for Long-Term System Stability
Within the context of developing and validating an LC-MS/MS method for quantifying drug concentrations in plasma, the stability and reliability of the liquid chromatography (LC) system are paramount. Consistent performance is a cornerstone for generating accurate, reproducible pharmacokinetic data in drug development research. This document outlines essential preventive maintenance and hygiene practices to ensure long-term system stability, directly impacting the integrity of your analytical results.
Essential LC System Hygiene Practices
Proper daily hygiene extends the operational life of your LC system and minimizes downtime.
Mobile Phase Management
Mobile phase preparation is a critical first step in ensuring data quality.
- Degassing: Bubbles in the mobile phase can cause pressure fluctuations, irregular flow, and baseline instability in the UV/VIS detector. Effective degassing methods include online degassers (preferred), helium sparging, or sonication [82].
- Filtration: While HPLC-grade solvents typically do not require filtration, any mobile phase containing buffer salts or additives should be filtered through a 0.45 µm (or 0.2 µm) membrane to remove particulate matter that could clog the system [82]. Consistently use high-purity solvents and reagents to prevent column contamination and ion source fouling in the mass spectrometer.
System Flushing and Cleaning
Maintaining system cleanliness prevents the accumulation of salts and contaminants.
- Buffer Removal: At the end of each day, or after running buffer-containing mobile phases, flush the entire system (pump, injector, column) with a high-purity water/organic solvent mixture (e.g., 50:50 water/methanol) to completely remove salts. Never allow buffer solutions to stand in the HPLC system [82].
- Solvent Line Cleaning: Regularly check and clean the solvent inlet lines and sinker frits located in the mobile phase reservoirs [82].
- Column Storage: When not in use, store columns as recommended by the manufacturer, typically in an organic-rich solvent like 80% methanol or acetonitrile.
Scheduled Preventive Maintenance Protocol
A proactive maintenance schedule is indispensable for preventing unexpected system failures. The following table outlines a recommended regimen for key LC system components.
Table 1: Scheduled Preventive Maintenance Protocol for LC Systems
| Component | Frequency | Maintenance Action | Purpose & Rationale |
|---|---|---|---|
| Pump Seal | Every 3-6 months or as per instrument manual | Replace | Prevents leaks and protects the pump from abrasion by salt crystals. Worn seals are a major source of particulates [82]. |
| In-line Filter | Weekly or when pressure increases by 25% or 500 psi | Clean or replace | Protects the analytical column by trapping particulates from the mobile phase and pump seal wear [82]. |
| Autosampler Needle | Weekly | Inspect and clean with solvent | Prevents cross-contamination and ensures accurate injection volumes. |
| Autosampler Rotor Seal | When leakage occurs or after ~20,000 injections | Replace | Prevents leaks in the flow path that cause retention time shifts and peak area inconsistencies [82]. |
| Backpressure Regulator | Annually | Inspect and service | Ensures consistent pressure application post-detector, which helps prevent bubble formation in the flow cell [82]. |
Impact of LC Hygiene on Analytical Method Performance
Neglecting LC hygiene and maintenance directly compromises key validation parameters of an LC-MS/MS method.
- Retention Time Stability: Contamination or blockages in the column or tubing can alter the chromatographic bed, leading to retention time drift.
- Peak Shape & Resolution: A contaminated system, especially at the column head, can cause peak broadening, tailing, and loss of resolution, affecting the ability to integrate peaks accurately [82].
- Detection Sensitivity: Contamination that reaches the MS ion source can cause significant ion suppression, reducing signal intensity and increasing the limit of quantification.
- System Pressure: Particulate accumulation is the primary cause of steadily increasing system pressure, which can lead to complete system shutdown and column failure [82].
Experimental Protocol: Verification of System Cleanliness
This procedure provides a quantitative assessment of LC system hygiene, suitable for periodic performance verification.
Materials and Reagents
- Mobile Phase A: High-purity water with 0.1% formic acid.
- Mobile Phase B: Methanol or acetonitrile with 0.1% formic acid.
- Test Column: A standard C18 column (e.g., 50 mm x 2.1 mm, 1.7 µm).
- System Suitability Standard: A solution of a known, stable compound appropriate for your column chemistry.
Methodology
- System Equilibration: Purge the system and equilibrate the test column with a mixture of 10% B for 10 minutes, followed by 5 minutes at the starting method condition (e.g., 5% B).
- Blank Injection: Inject a sample of pure Mobile Phase A.
- System Suitability Injection: Inject the system suitability standard.
- Gradient Run: Execute a shallow gradient (e.g., 5% B to 95% B over 20 minutes) while monitoring the baseline.
- Data Analysis:
- Examine the blank injection chromatogram for the absence of extraneous peaks.
- From the system suitability injection, calculate the %RSD of retention time (target <1%) and peak area (target <2%), and measure the peak asymmetry factor (target 0.8-1.5).
- From the gradient blank, assess the baseline noise and drift.
Data Interpretation and Acceptance Criteria
The following table summarizes the key acceptance criteria for verifying system cleanliness and performance.
Table 2: Acceptance Criteria for LC System Performance Verification
| Performance Parameter | Acceptance Criterion | Impact of Non-Conformance |
|---|---|---|
| Retention Time %RSD | < 1.0% (n=5) | Indicates pump flow rate inaccuracy or column degradation. |
| Peak Area %RSD | < 2.0% (n=5) | Suggests injector malfunctions or detection instability. |
| Peak Asymmetry (Tailing Factor) | 0.8 - 1.5 | Values outside this range indicate column contamination or damage [82]. |
| Baseline Noise (Blank Run) | No significant ghost peaks | Ghost peaks are a direct indicator of system contamination. |
| System Pressure | Stable, within ±10% of baseline | Rising pressure indicates a blockage or particulate buildup [82]. |
The Scientist's Toolkit: Key Research Reagent Solutions
The following reagents and materials are essential for maintaining an LC-MS/MS system used for plasma drug analysis.
Table 3: Essential Research Reagents and Materials for LC-MS/MS Maintenance
| Item | Function & Application |
|---|---|
| HPLC-Grade Solvents (MeOH, ACN, Water) | Used for mobile phase preparation and system flushing to minimize UV absorption and MS chemical noise. |
| High-Purity Volatile Acids & Buffers (Formic, Acetic Acid, Ammonium Acetate) | Mobile phase additives to control pH and improve ionization efficiency in the MS source [83] [84]. |
| In-line Filters (0.5 µm) | Placed between the autosampler and column to trap particulates, protecting the analytical column [82]. |
| Pump Seals & Frit Kits | Replacement parts for scheduled preventive maintenance of the LC pump and fluidic paths. |
| Protein Precipitation Reagents (e.g., ACN, MeOH) | Used in sample pre-treatment for plasma analysis to remove proteins and other macromolecules, preventing column and system contamination [83]. |
| Stable Isotope-Labeled Internal Standards | Added to samples and calibrators to correct for variability in sample preparation and ionization efficiency [83] [84]. |
System Hygiene and Maintenance Workflow
The following diagram illustrates the logical workflow for maintaining LC hygiene and its direct impact on analytical data quality within the context of a plasma drug assay.
Ensuring Data Integrity: A Practical Guide to Method Validation and Comparison
The reliability of data generated by a liquid chromatography-tandem mass spectrometry (LC-MS/MS) method for quantifying drug concentrations in plasma is paramount in drug development research. For a method to be considered valid and yield trustworthy results suitable for supporting regulatory submissions, it must undergo a rigorous validation process. This process demonstrates that the method is consistently reliable for its intended purpose. This application note details the experimental protocols and acceptance criteria for four key validation parameters—Selectivity, Linearity, Lower Limit of Quantification (LLOQ), and Carryover—within the context of developing a robust LC-MS/MS method for plasma analysis [85].
Parameter Definitions and Acceptance Criteria
The table below summarizes the core objectives and standard acceptance criteria for each key validation parameter, as derived from industry practices and regulatory guidance [85] [86] [87].
Table 1: Key Validation Parameters and Their Acceptance Criteria
| Parameter | Core Objective | Standard Acceptance Criteria |
|---|---|---|
| Selectivity/Specificity | To confirm the method accurately measures the analyte in the presence of other components. | Signal in blank matrix from 6-10 individual sources should be <20% of LLOQ response and <5% from internal standard [85] [86]. |
| Linearity | To demonstrate that the method provides results directly proportional to the analyte concentration. | A calibration curve with a minimum of 6 concentration levels. Regression coefficient (r²) > 0.99 (or 0.995 for some applications) [64] [88]. Calibration standards should be within ±15% of nominal (±20% at LLOQ) [85]. |
| Lower Limit of Quantification (LLOQ) | The lowest concentration that can be measured with acceptable accuracy and precision. | Signal-to-noise ratio ≥ 10:1 [64]. Accuracy and Precision (CV) within ±20% [85] [86]. |
| Carryover | To ensure a sample does not affect the analysis of a subsequent sample. | Peak area in blank sample after a high-concentration standard should be <20% of the LLOQ response [85] [86]. |
Experimental Protocols
Selectivity and Specificity
Purpose: To verify that the method can unequivocally quantify the analyte without interference from endogenous matrix components, metabolites, or concomitant medications [85] [86].
Detailed Procedure:
- Sample Preparation: Collect blank plasma from at least six individual sources [85]. For each source, prepare:
- A blank sample (no analyte, no internal standard).
- A blank sample spiked with the internal standard (IS) only.
- A sample spiked with the analyte at the LLOQ concentration and the IS.
- Analysis: Inject and analyze all samples using the developed LC-MS/MS method.
- Interference Check: Systematically inspect the chromatograms of the blank and IS-only samples for any co-eluting peaks at the same retention time as the analyte or IS.
- Assessment: The response of any interfering peak in the blank matrix at the analyte's retention time must be less than 20% of the LLOQ response. The response of any interfering peak at the IS's retention time must be less than 5% of the IS response [86].
Linearity and LLOQ
Purpose: To establish the concentration range over which the method provides accurate and precise results and to define the lowest measurable concentration.
Detailed Procedure:
- Calibration Curve Preparation: Prepare a calibration curve using a minimum of six non-zero concentration levels, spanning the expected range in study samples (e.g., from LLOQ to Upper Limit of Quantification, ULOQ) [85]. Each level should be prepared in the biological matrix (plasma) and processed according to the method.
- Analysis: Analyze the calibration standards in a single run.
- Regression Analysis: Plot the peak area ratio (Analyte/IS) against the nominal concentration. Use a weighted least-squares regression model (e.g., 1/x or 1/x²) to fit the data [86].
- Acceptance: The correlation coefficient (r²) should typically be greater than 0.99 [64] [88]. The calculated back-concentration of each calibration standard should be within ±15% of the nominal value (±20% at the LLOQ) [85].
- LLOQ Confirmation: The LLOQ is validated by analyzing at least five replicates at the proposed LLOQ concentration. The precision (Coefficient of Variation, CV) and accuracy (Relative Error, RE) for these replicates must be within ±20% [85] [86]. A signal-to-noise ratio of 10:1 is a common additional criterion [64].
Carryover
Purpose: To evaluate and minimize the contribution of a high-concentration sample to the signal of a subsequent sample.
Detailed Procedure:
- Sample Sequence: Inject the following sequence into the LC-MS/MS system:
- A blank plasma sample.
- A solvent blank.
- The highest calibration standard (ULOQ).
- A blank plasma sample.
- A solvent blank.
- Analysis: Analyze all samples and examine the chromatograms of the blanks injected after the ULOQ standard.
- Assessment: The peak response in the blank sample at the retention time of the analyte must be less than 20% of the LLOQ response [85] [86]. If carryover exceeds this limit, the autosampler wash protocol and injection needle must be optimized, for example, by using multiple wash solvents and extended needle wash procedures [89].
Workflow and Logical Relationships
The following diagram illustrates the logical sequence and decision-making process involved in validating these four key parameters. The process is iterative; failure at any stage requires troubleshooting and re-evaluation before proceeding.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and materials critical for successfully executing the validation protocols described above.
Table 2: Essential Research Reagents and Materials for LC-MS/MS Method Validation
| Item | Function / Purpose | Exemplary Use in Protocol |
|---|---|---|
| Blank Biological Matrix | Serves as the foundation for preparing calibration standards and QC samples, assessing matrix effects and selectivity. | Sourced from at least 6-10 individual donors to test for endogenous interferences [85] [90]. |
| Certified Reference Standard | The pure, well-characterized analyte used to prepare stock solutions, ensuring accurate and traceable quantification. | Used to prepare primary stock solutions for spiking calibration curves and QC samples [86] [87]. |
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Accounts for variability in sample preparation and ionization efficiency; improves accuracy and precision. | Added in a constant amount to all samples, calibrators, and QCs before processing; analyte/IS peak area ratio is used for quantification [85] [90]. |
| Protein Precipitation Solvent | A solvent (e.g., acetonitrile, methanol) used to remove proteins from plasma samples, clarifying the sample for analysis. | Added to plasma samples, vortex-mixed, and centrifuged to precipitate proteins; supernatant is injected or processed further [86] [91]. |
| LC-MS/MS System with UHPLC | The core instrument platform for chromatographic separation (UHPLC) and highly specific and sensitive detection (MS/MS). | Separates the analyte from matrix components; detects and quantifies the analyte via Multiple Reaction Monitoring (MRM) [88] [89]. |
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) has become the gold standard for the quantitative analysis of drugs and their metabolites in biological matrices, playing a pivotal role in therapeutic drug monitoring (TDM), pharmacokinetic studies, and bioequivalence research [14] [92]. The reliability of data generated by these methods is paramount, as conclusions regarding drug safety and efficacy depend on it. Accuracy and precision are two fundamental pillars in validating any bioanalytical method, serving as the primary indicators of its performance and robustness [14] [93] [94]. Accuracy reflects the closeness of agreement between a measured value and its true concentration, while precision describes the closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample under prescribed conditions [14]. Within precision assessment, intra-day (within a single analytical run) and inter-day (across different runs over multiple days) performance are critically evaluated to ensure a method's consistency over time [93]. This document, framed within broader thesis research on LC-MS/MS method development for quantifying anticancer drugs in plasma, provides detailed application notes and protocols for assessing these essential validation parameters, supported by experimental data and standardized procedures.
Experimental Protocols
Materials and Reagents
- Chemicals and Reagents: LC-MS/MS grade solvents are essential. This includes water, methanol, and acetonitrile [95] [14]. Formic acid or ammonium formate is typically used as a mobile phase additive. Analytes of interest and their deuterated or otherwise isotopically labeled internal standards should be sourced from reputable suppliers [95] [92].
- Biological Matrix: Blank human plasma, typically with Kâ‚‚EDTA as an anticoagulant, is required for the preparation of calibration standards and quality control (QC) samples [95].
- Solution Preparation:
- Stock Solutions: Prepare separate stock solutions of the analyte and internal standard in a suitable solvent such as methanol or dimethyl sulfoxide (DMSO) at a concentration of approximately 1 mg/mL [95] [14].
- Working Solutions: Serially dilute stock solutions with methanol or acetonitrile to create working solutions for spiking into plasma to generate calibration standards and QC samples at desired concentrations [14] [92].
- Internal Standard Working Solution: Dilute the internal standard stock solution to an appropriate concentration for use in the sample preparation procedure [14].
Sample Preparation for Calibration and Quality Controls
- Preparation of Calibration Standards and QC Samples: Spike appropriate volumes of analyte working solutions into blank human plasma to generate a calibration curve (e.g., 6-8 non-zero concentrations) and at least three levels of QC samples (Low, Medium, High) covering the expected range [92]. The lower limit of quantification (LLOQ) serves as the lowest calibration standard [14].
- Sample Pre-treatment: For each sample (calibrators, QCs, and study samples), aliquot a defined volume (e.g., 50-100 µL) of plasma into a tube [95] [14].
- Protein Precipitation: Add a volume of internal standard working solution in an organic solvent (e.g., methanol or acetonitrile) to the plasma aliquot. Vortex mix vigorously for several minutes to ensure complete protein precipitation and analyte extraction [95] [92].
- Centrifugation: Centrifuge the samples at high speed (e.g., 10,000-14,000× g) for 5-10 minutes at a controlled temperature (e.g., 4°C) to pellet the precipitated proteins [95].
- Sample Reconstitution: Transfer a portion of the supernatant to a new vial. It may be diluted with an aqueous solvent [95] [14] before injection into the LC-MS/MS system.
LC-MS/MS Instrumental Analysis
- Chromatography:
- Column: A reversed-phase C18 column is commonly used [14] [96].
- Mobile Phase: Typically consists of an aqueous phase (e.g., 0.1% formic acid in water) and an organic phase (e.g., acetonitrile or methanol) [14].
- Gradient: A gradient elution is often employed to achieve optimal separation of analytes from matrix interferences. The total run time can vary but modern methods aim for 5-9 minutes [95] [14].
- Temperature: The column temperature is often maintained at 40-50°C [14].
- Injection Volume: Typically 5-10 µL [14] [92].
- Mass Spectrometry:
- Ionization: Electrospray Ionization (ESI) in positive or negative mode is standard [14] [93].
- Detection: Multiple Reaction Monitoring (MRM) is used for highly selective and sensitive detection. Specific precursor-to-product ion transitions are monitored for each analyte and its internal standard [14] [94].
Experimental Procedure for Intra-day and Inter-day Assessment
- Analytical Batch Design: The validation batch for precision and accuracy should include a blank plasma sample (without analyte and internal standard), a zero sample (with internal standard only), calibration standards, and replicate QC samples at a minimum of three concentration levels (Low, Medium, High) [14].
- Intra-day (Within-run) Assessment: On a single day, prepare and analyze a minimum of five (n≥5) replicates of each QC level (LQC, MQC, HQC) within one analytical batch [14] [93].
- Inter-day (Between-run) Assessment: Repeat the analysis described in Step 2 on at least three different days (n≥3 batches). The replicates for each QC level on each day should be prepared independently from fresh stock/solutions if possible, to capture total method variability [14].
- Data Analysis: For both intra-day and inter-day data, calculate the mean measured concentration, standard deviation (SD), and relative standard deviation (RSD %) for each QC level. The RSD (%) is calculated as (SD / Mean) × 100. Accuracy is calculated as (Mean Measured Concentration / Nominal Concentration) × 100 [14].
The following workflow diagram illustrates the key stages of this assessment procedure:
Data Presentation and Analysis
The tables below summarize intra-day and inter-day accuracy and precision data for various drugs quantified in human plasma using LC-MS/MS, as reported in recent scientific literature.
Table 1: Intra-day and Inter-day Performance of LC-MS/MS Methods for Anticancer Drugs
| Analyte | Matrix | QC Level | Intra-day Precision (RSD%) | Intra-day Accuracy (%) | Inter-day Precision (RSD%) | Inter-day Accuracy (%) | Citation |
|---|---|---|---|---|---|---|---|
| Dabrafenib | Plasma | Across AMR* | 1.3–6.5% | Not Specified | Not Specified | Not Specified | [95] |
| Trametinib | Plasma | Across AMR* | 1.3–5.1% | Not Specified | Not Specified | Not Specified | [95] |
| Sunitinib | Plasma | LQC, MQC, HQC | < 8.8% | -14.8% to 11.3% | < 10.5% | -14.8% to 11.3% | [92] |
| N-Desethyl Sunitinib | Plasma | LQC, MQC, HQC | < 8.8% | -14.8% to 11.3% | < 10.5% | -14.8% to 11.3% | [92] |
| Abemaciclib | Cell Lysate | QC-L, M, H | 2.7–6.2% | 94.4–104.0% | 4.4–8.7% | 95.2–104.2% | [94] |
| Tazemetostat | Cell Lysate | QC-L, M, H | 3.5–7.9% | 93.8–105.5% | 6.3–9.4% | 95.8–105.8% | [94] |
*AMR: Analytical Measurement Range
Table 2: Intra-day and Inter-day Performance of LC-MS/MS Methods for Other Drug Classes
| Analyte | Matrix | QC Level | Intra-day Precision (RSD%) | Intra-day Accuracy (%) | Inter-day Precision (RSD%) | Inter-day Accuracy (%) | Citation |
|---|---|---|---|---|---|---|---|
| Omadacycline | Plasma | LQC, MQC, HQC | < 10% | Within ± 10% | < 10% | Within ± 10% | [14] |
| Homovanillic Acid (HVA) | Urine | QC Low, High | 7–8% | Not Specified | 3–7% | Not Specified | [93] |
| Vanillylmandelic Acid (VMA) | Urine | QC Low, High | 5–6% | Not Specified | 2–7% | Not Specified | [93] |
| Metolazone | Plasma | Across Range | 0.9–4.8% | 97.5–102.3% | 4.2–6.3% | 99.2–104.0% | [96] |
Acceptance Criteria and Data Interpretation
For a bioanalytical method to be considered valid, the accuracy and precision data must fall within predefined acceptance criteria, typically guided by international guidelines like the ICH M10 [94].
- Precision: The RSD for each QC level should generally be ≤15%, except for the LLOQ, for which it can be ≤20% [14].
- Accuracy: The mean accuracy for each QC level should be within ±15% of the nominal concentration, except for the LLOQ, which can be within ±20% [14].
Data presented in the tables above consistently meet these stringent criteria, demonstrating the robustness of well-developed LC-MS/MS methods. The high precision (low RSD%) across different days and runs indicates minimal random error, while the high accuracy (close to 100%) indicates minimal systematic error. The slightly higher inter-day RSD% values compared to intra-day, as seen with abemaciclib and tazemetostat [94], reflect the additional variables introduced over time, such as fresh reagent preparation and minor instrumental fluctuations.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for LC-MS/MS Method Validation
| Item | Function / Application | Specific Examples |
|---|---|---|
| Triple Quadrupole Mass Spectrometer | The core detection instrument; provides highly selective and sensitive quantification via Multiple Reaction Monitoring (MRM). | API 4000, LCMS-8050 [14] [92] |
| U/HPLC System | Provides high-resolution chromatographic separation of analytes from matrix components, reducing ion suppression. | Agilent 1260 series, Thermo Vanquish Flex, Shimadzu Nexera X2 [95] [14] [92] |
| C18 Reversed-Phase LC Column | The standard stationary phase for separating moderately hydrophobic to hydrophobic analytes in complex biological samples. | Phenomenex KINETEX XB-C18, Thermo Hypersil GOLD aQ [95] [14] |
| Isotopically Labeled Internal Standards (IS) | Corrects for analyte loss during sample preparation and for variability in ionization efficiency, improving accuracy and precision. | Dabrafenib-D9, Trametinib-13C6, Fexofenadine-d6 [95] [14] |
| LC-MS Grade Solvents | High-purity solvents minimize background noise and contamination, ensuring optimal chromatographic performance and signal stability. | Water, Methanol, Acetonitrile [95] [14] |
| Protein Precipitation Plates/Tubes | Used in the sample preparation workflow to remove proteins from plasma, yielding a clean supernatant for injection. | 1.5 mL microtubes, 96-well plates [14] [92] |
The role of internal standards in ensuring method accuracy and precision is so critical that their selection and use can be conceptualized as a key decision pathway within the validation process, as shown in the following diagram:
Evaluating Extraction Recovery and Matrix Effects
In the development of bioanalytical methods using Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) for quantifying drug concentrations in plasma, two parameters are critical for ensuring data reliability: extraction recovery and matrix effects. These elements form part of the essential characteristics required for method validation, as they directly impact the accuracy, sensitivity, and reproducibility of the results [60]. Within the broader context of thesis research on LC-MS/MS method development, a thorough investigation of these factors is indispensable for transforming a theoretical assay into a robust, clinically applicable tool for drug development and therapeutic drug monitoring.
This application note provides detailed protocols and data evaluation techniques to accurately assess extraction recovery and matrix effects, utilizing real-world case studies from recent scientific literature.
Theoretical Background and Definitions
The Eight Essential Characteristics of LC-MS/MS Validation
The validation of an LC-MS/MS method is a comprehensive process. To ensure a method is reliable and accurate, it is essential to validate it against eight key characteristics [60]:
- Accuracy
- Precision
- Specificity
- Quantification Limit
- Linearity
- Recovery
- Matrix Effect
- Stability
This document focuses specifically on the experimental determination of Recovery and Matrix Effect, which are often interconnected.
Key Definitions
- Extraction Recovery refers to the efficiency of the sample preparation process in extracting the analyte from a biological matrix. It is a measure of the ability of the method to accurately measure the analyte in the sample after the sample has undergone extraction or other sample preparation procedures [60]. High recovery indicates a efficient sample clean-up and minimal loss of the analyte.
- Matrix Effect is the interference caused by the sample matrix on the ionization and detection of the analyte in the mass spectrometer. It is evaluated by extracting individual matrix sources/lots spiked with known concentrations of analyte and internal standard [60]. Matrix effects can cause either suppression or enhancement of the analyte signal, leading to inaccurate quantification.
The following diagram illustrates the logical relationship and assessment focus of these two key parameters within the method validation workflow.
Experimental Protocols
Protocol for Determining Extraction Recovery
Principle: Recovery is assessed by comparing the MS response of an analyte spiked into a matrix before extraction with the response of the same amount of analyte spiked into a blank matrix extract after extraction (post-extraction spike) [97].
Procedure:
- Prepare Post-Extraction Spiked Samples (Set A): Take a volume of blank, processed matrix (the supernatant after protein precipitation or extraction). Spike this clean matrix with a known concentration of the analyte and internal standard. This set represents the 100% reference.
- Prepare Pre-Extraction Spiked Samples (Set B): Take the same volume of blank matrix and spike it with the identical known concentration of analyte and internal standard. Then, subject this sample to the entire sample preparation procedure (e.g., protein precipitation).
- Analysis and Calculation: Analyze both sample sets (A and B) using the developed LC-MS/MS method. The extraction recovery (%RE) is calculated using the formula:
% Recovery = (Peak Area of Set B / Peak Area of Set A) × 100% [97]
This protocol should be replicated at a minimum of three concentration levels (Low, Medium, High) across multiple validation runs to establish consistency.
Protocol for Determining Matrix Effects
Principle: The matrix effect is evaluated by comparing the MS response of an analyte in a post-extraction spiked sample to the response of the same pure analyte in a neat solution (e.g., mobile phase) [97]. Using a stable isotope-labeled internal standard (SIL-IS) is highly recommended as it can correct for these effects.
Procedure:
- Prepare Neat Solution (Set C): Spike a known concentration of the analyte and internal standard into a pure solvent (e.g., mobile phase). This set is devoid of any matrix.
- Prepare Post-Extraction Spiked Samples (Set A): As described in Section 3.1, spike the same known concentration of analyte and internal standard into a blank, processed matrix.
- Analysis and Calculation: Analyze both sample sets (A and C). The matrix effect (ME) is calculated as:
% Matrix Effect = (Peak Area of Set A / Peak Area of Set C) × 100% - ME = 100%: Indicates no matrix effect. - ME < 100%: Indicates ion suppression. - ME > 100%: Indicates ion enhancement.
The precision (relative standard deviation, RSD) of the matrix effect measured across different lots of matrix should also be calculated. An RSD of less than 15% is typically acceptable [30].
Data Presentation and Analysis
The following tables summarize quantitative data for extraction recovery and matrix effects from published, validated LC-MS/MS methods, providing benchmarks for expected performance.
Table 1: Reported Extraction Recovery and Matrix Effect Data from Validated Methods
| Analyte | Biological Matrix | Extraction Method | Recovery (%) | Matrix Effect (% RSD) | Citation |
|---|---|---|---|---|---|
| Ciprofol | Human Plasma | Protein Precipitation (Methanol) | 87.24 - 97.77 | < 15% | [30] |
| Omadacycline | Human Plasma | Protein Precipitation (Acetonitrile) | Acceptable (Full data in text) | Acceptable (Full data in text) | [14] |
| Immunosuppressants (Tac, MPA, etc.) | Whole Blood | Protein Precipitation | - | - | [88] |
| Usnic Acid | Lichen Extract | Liquid-Liquid Extraction | High (Validated) | Minor levels reported | [97] |
Table 2: Experimental QC Results for Precision and Accuracy from a Validated Immunosuppressant Method
| Analyte | Concentration Level | Precision (RSD, %) | Accuracy (%, within ±15%) |
|---|---|---|---|
| Mycophenolic Acid (MPA) | Low QC | < 10% | Within ±15% |
| Medium QC | < 10% | Within ±15% | |
| High QC | < 10% | Within ±15% | |
| Tacrolimus (Tac) | Low QC | < 10% | Within ±15% |
| Medium QC | < 10% | Within ±15% | |
| High QC | < 10% | Within ±15% |
Data adapted from a simultaneous quantification method for immunosuppressants in microvolume whole blood [88].
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and reagents commonly used in these experiments, based on the protocols found in the search results.
Table 3: Essential Reagents and Materials for Recovery and Matrix Effect Studies
| Item | Function / Purpose | Example from Literature |
|---|---|---|
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Corrects for variability in sample preparation and ionization efficiency; crucial for compensating matrix effects. | Ciprofol-d6 used in UHPLC-MS/MS method [30]. Fexofenadine-d6 used for omadacycline quantification [14]. |
| Blank Biological Matrix | Sourced from multiple donors to assess inter-individual variability in matrix effects. | Blank human plasma from multiple lots [30] [14]. Use of Cladonia ochrochlora extract as a blank matrix for usnic acid analysis [97]. |
| High-Purity Solvents | Used for mobile phase, sample reconstitution, and protein precipitation to minimize background interference. | Methanol, Acetonitrile (HPLC grade) [30] [14]. |
| Protein Precipitant | Removes proteins from plasma/serum samples, cleaning up the matrix for analysis. | Methanol or Acetonitrile, often used with an internal standard solution [30] [14]. |
| Analytical Reference Standard | The pure, known quantity of the analyte used to prepare calibration standards and QC samples. | Ciprofol standard [30], Omadacycline benzenesulfonate [14]. |
Workflow Visualization
The entire experimental process for evaluating both extraction recovery and matrix effects is summarized in the integrated workflow below.
Rigorous evaluation of extraction recovery and matrix effects is a non-negotiable component of a robust LC-MS/MS method validation for plasma drug quantification. By adhering to the detailed protocols outlined in this document—using a stable isotope-labeled internal standard, testing multiple lots of matrix, and employing the standard calculations—researchers can confidently identify and mitigate sources of analytical inaccuracy. Mastering these concepts and techniques ensures the generation of reliable, high-quality data that is fit for purpose in advanced pharmacokinetic studies and therapeutic drug monitoring, forming a solid foundation for any thesis in the field of bioanalytical chemistry.
Stability testing constitutes a critical component of bioanalytical method validation for liquid chromatography-tandem mass spectrometry (LC-MS/MS) methods quantifying drug concentrations in plasma. These studies provide essential data on the integrity of analyte(s) under various conditions that samples may encounter during handling, storage, and processing, thereby ensuring the reliability of pharmacokinetic, toxicokinetic, and therapeutic drug monitoring data [98] [99]. The establishment of proper stability conditions is particularly crucial for supporting clinical trials and routine therapeutic drug monitoring, where inaccurate concentration measurements could lead to incorrect dosing recommendations or misinterpretation of study outcomes [98] [14].
Within the framework of LC-MS/MS method validation for plasma analysis, three types of stability studies are particularly fundamental: bench-top stability, which assesses sample integrity at room temperature during processing; freeze-thaw stability, which evaluates the effects of cyclic freezing and thawing that may occur during analysis; and long-term stability, which determines appropriate storage conditions and durations for biological samples [99] [100]. These evaluations are performed in accordance with regulatory guidelines from the Food and Drug Administration (FDA) and the International Council for Harmonisation (ICH) to ensure data integrity and regulatory acceptance [101] [102] [100].
The recent draft ICH Q1 guideline (2025) consolidates previous stability guidances and emphasizes a science- and risk-based approach to stability testing, encouraging continuity from development through post-approval stages [102] [103]. This modernized framework supports the implementation of stability procedures throughout the product lifecycle, aligning with contemporary Quality-by-Design principles [102] [103].
Regulatory Framework and Guidelines
Stability testing for bioanalytical methods operates within a well-defined regulatory framework designed to ensure the generation of reliable and reproducible data. The FDA bioanalytical method validation guidance provides the foundational requirements for stability testing, while ICH guidelines offer complementary international standards for drug substance and product stability [101] [100]. The recent consolidation of the ICH Q1A(R2) through Q1F and Q5C guidelines into a single comprehensive document represents a significant advancement in harmonizing stability testing requirements globally [101] [102].
The 2025 ICH Q1 draft guideline emphasizes a more systematic, knowledge-driven approach to stability study design, encouraging the use of risk management principles and scientific justification throughout the product lifecycle [102] [103]. This updated guidance specifically addresses stability considerations for advanced therapy medicinal products and other complex biologics, which were not comprehensively covered in previous versions [101] [102]. For small molecule drugs quantified in plasma using LC-MS/MS, the guidelines require demonstration of stability under conditions that mimic actual sample handling, storage, and processing environments.
Regulatory guidelines mandate that stability testing should evaluate the stability of analytes in the biological matrix at relevant temperatures and after a specific number of freeze-thaw cycles [99] [100]. The acceptance criteria for stability experiments typically require that the mean concentration at each level should be within ±15% of the nominal concentration, with a relative standard deviation not exceeding 15% [99] [14] [100]. These criteria ensure that analyte degradation does not significantly impact the accuracy and precision of the quantitative measurements.
Table 1: Key Regulatory Guidelines for Stability Testing
| Guideline | Issuing Authority | Scope | Key Requirements |
|---|---|---|---|
| FDA Bioanalytical Method Validation | U.S. Food and Drug Administration | Bioanalytical methods supporting clinical studies | Demonstration of analyte stability in matrix under storage, processing, and handling conditions |
| ICH Q1 (Draft 2025) | International Council for Harmonisation | Stability testing of drug substances and products | Consolidated guidance applying risk-based approaches across product lifecycle |
| EMA Bioanalytical Method Validation | European Medicines Agency | Bioanalytical methods in clinical research | Requirements similar to FDA with some regional variations |
Experimental Design for Stability Studies
General Principles
The design of stability studies for LC-MS/MS bioanalytical methods requires careful consideration of multiple factors to ensure scientifically valid results. Stability experiments should be conducted using quality control (QC) samples prepared at low, mid, and high concentrations within the calibration curve range, typically in replicates of at least three to five at each level [99] [14] [100]. These QC samples should be prepared from independently prepared stock solutions rather than from calibration standards to ensure unbiased evaluation.
A critical aspect of stability study design is the use of appropriate controls. Freshly prepared calibration standards and QC samples are analyzed alongside stability samples to establish baseline responses [99] [100]. The comparison of stability samples against these freshly prepared standards allows for accurate quantification of any degradation that may have occurred. Additionally, the use of stable isotope-labeled internal standards, when available, can correct for minor variations during sample processing and analysis, thereby improving the reliability of stability assessments [99].
The design of stability studies should reflect actual sample handling conditions anticipated during clinical sample collection, storage, and analysis. This includes considering the maximum expected time between sample collection and processing, the number of freeze-thaw cycles samples might undergo during reanalysis, and the long-term storage duration necessary for supporting clinical trials [99] [100]. Documentation of stability testing conditions, including temperature monitoring records and sample handling procedures, is essential for regulatory compliance and data integrity.
Stability Study Workflow
The following diagram illustrates the systematic workflow for conducting comprehensive stability studies in bioanalytical method validation:
Figure 1: Comprehensive Stability Study Workflow for Bioanalytical Method Validation
Protocols for Stability Assessments
Bench-Top Stability
Bench-top stability evaluates the integrity of analytes in plasma samples when maintained at room temperature for durations reflecting typical sample processing periods. This assessment is crucial as plasma samples may remain at ambient temperature during centrifugation, aliquoting, and preliminary preparation steps before analysis or storage [99] [14].
Protocol:
- Prepare QC samples at low and high concentrations (minimum of three replicates each) in the appropriate biological matrix (plasma)
- Keep samples undisturbed at room temperature (typically 20-25°C) for a predetermined duration (e.g., 4, 8, 12, or 24 hours) [99] [14]
- Process and analyze these samples alongside freshly prepared calibration standards and QC samples
- Calculate the percentage of nominal concentration remaining by comparing the measured concentrations of stability samples with nominal concentrations
- Accept results if mean measured concentrations are within ±15% of nominal values with RSD ≤15% [99] [100]
Recent applications of this protocol include the validation of methods for tazemetostat, where bench-top stability was confirmed for 24 hours at room temperature [99], and for omadacycline, where similar stability was demonstrated [14]. The specific duration for bench-top stability should reflect the maximum anticipated sample processing time in the clinical or analytical setting.
Freeze-Thaw Stability
Freeze-thaw stability investigations determine the effects of repeated freezing and thawing cycles on analyte integrity, simulating scenarios where samples may undergo multiple cycles due to reanalysis, repeat testing, or aliquoting for different assays [99] [100].
Protocol:
- Prepare QC samples at low and high concentrations (minimum of three replicates each)
- Subject samples to a minimum of three complete freeze-thaw cycles [99] [100]
- Each cycle consists of:
- Freezing at the intended storage temperature (typically -20°C or -80°C) for at least 12 hours
- Thawing unassisted at room temperature (approximately 20-25°C)
- Maintaining in the thawed state for 1-4 hours before refreezing
- After the final cycle, process and analyze samples alongside freshly prepared calibration standards and QC samples
- Calculate the percentage of nominal concentration remaining after freeze-thaw cycles
- Accept results if mean measured concentrations are within ±15% of nominal values with RSD ≤15% [99] [100]
This protocol has been successfully applied in the validation of methods for drugs including tazemetostat, which demonstrated stability after three freeze-thaw cycles [99], and SGR-1505, which also showed appropriate stability under similar conditions [100].
Long-Term Storage Stability
Long-term stability assessments establish appropriate storage conditions and durations for biological samples, ensuring that analyte concentrations remain unchanged during the storage period between sample collection and analysis, which can extend for months or years in large clinical trials [99] [100].
Protocol:
- Prepare QC samples at low and high concentrations (minimum of three replicates each)
- Store samples at the intended storage temperature(s) (typically -20°C or -80°C)
- Remove and analyze samples at predetermined time intervals (e.g., 1, 3, 6, 9, 12 months) alongside freshly prepared calibration standards and QC samples [99] [100]
- For each time point, calculate the percentage of nominal concentration remaining
- Accept results if mean measured concentrations are within ±15% of nominal values with RSD ≤15%
- The longest time point for which stability is demonstrated establishes the acceptable storage duration [99] [100]
Recent applications include the tazemetostat method validation, which confirmed 4-month stability at -80°C [99], and the SGR-1505 validation, which demonstrated long-term stability under frozen storage conditions [100]. Storage temperature should be selected based on the analyte's properties and the anticipated storage duration, with -80°C generally providing enhanced stability for labile compounds.
Data Interpretation and Acceptance Criteria
The interpretation of stability data follows standardized acceptance criteria established by regulatory guidelines. For all stability experiments, the mean calculated concentration of the stability samples should be within ±15% of the nominal concentration, with the relative standard deviation (RSD) not exceeding 15% for QC samples at each concentration level [99] [14] [100]. These criteria ensure that any degradation occurring during storage or processing does not significantly impact the accuracy and precision of the quantitative method.
When evaluating stability data, it is essential to consider both systematic trends and random variations. A gradual decrease in measured concentrations over time or with increasing freeze-thaw cycles may indicate progressive degradation, while substantial variability without a clear trend might suggest issues with sample handling or analytical precision. Statistical analysis, including regression analysis of concentration versus time, can provide additional insights into degradation kinetics and help establish appropriate storage expiration dates [102].
Stability results should be presented in comprehensive tables that include nominal concentrations, measured concentrations, accuracy (percentage of nominal), precision (RSD), and the number of replicates for each test condition. This organized presentation facilitates regulatory review and provides clear evidence of method robustness [99] [14] [100].
Table 2: Stability Results from Recent Bioanalytical Method Validations
| Drug Compound | Matrix | Bench-Top Stability | Freeze-Thaw Stability | Long-Term Stability | Reference |
|---|---|---|---|---|---|
| Tazemetostat | Human plasma | 24 hours at room temperature | 3 cycles (-80°C) | 4 months at -80°C | [99] |
| SGR-1505 | Human plasma | Established per protocol | Established per protocol | Established for short-term and long-term frozen storage | [100] |
| Omadacycline | Human plasma | Implied by validation | Implied by validation | Implied by validation | [14] |
| Cystic Fibrosis Drugs (Caftors) | Human plasma | Assessed during validation | Assessed during validation | Assessed during validation | [98] |
Case Studies and Applications
Case Study: Tazemetostat Stability in Human Plasma
The LC-MS/MS method validation for tazemetostat provides an exemplary case study in comprehensive stability assessment. During method validation, stability experiments demonstrated that tazemetostat remained stable in human plasma through three freeze-thaw cycles when stored at -80°C and thawed to room temperature [99]. Additionally, bench-top stability was confirmed for 24 hours at room temperature, covering typical sample processing durations. Long-term stability evaluations established that plasma samples could be stored for at least 4 months at -80°C without significant degradation [99]. These stability findings were crucial for supporting a phase I clinical trial in patients with lymphomas, where reliable quantification of tazemetostat was essential for pharmacokinetic characterization and dose optimization.
Case Study: Cystic Fibrosis Drugs (Caftors) Stability Assessment
The LC-MS/MS method for quantifying cystic fibrosis drugs (ivacaftor, lumacaftor, tezacaftor, and elexacaftor) included rigorous stability testing to support therapeutic drug monitoring and pharmacokinetic studies [98]. The validated method demonstrated excellent precision and accuracy while establishing stability profiles for these compounds under various storage and handling conditions [98]. The comprehensive stability data enabled the application of this method to characterize the pharmacokinetic variability of caftors and monitor potential drug-drug interactions, ultimately supporting personalized dosing strategies for cystic fibrosis patients. This case highlights the critical role of stability assessments in precision medicine applications.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of stability studies requires careful selection of appropriate reagents, materials, and equipment. The following table details essential components of the stability testing toolkit:
Table 3: Essential Research Reagents and Materials for Stability Studies
| Item | Specification | Function in Stability Studies |
|---|---|---|
| Quality Control Materials | Drug substance with certified purity (>98%) | Preparation of QC samples for stability assessments |
| Biological Matrix | Human plasma (typically from drug-free volunteers) | Matrix-matched stability evaluation under relevant conditions |
| Internal Standard | Stable isotope-labeled analog (when available) | Correction for variability during sample processing and analysis |
| Storage Containers | Cryogenic vials with secure seals | Maintenance of sample integrity during storage at various temperatures |
| Solvents | LC-MS grade methanol, acetonitrile, water | Mobile phase preparation and sample processing |
| Additives | HPLC-grade formic acid, ammonium salts | Mobile phase modification for optimal chromatography |
| Freezers | -20°C and -80°C with temperature monitoring | Controlled storage conditions for long-term stability assessments |
| LC-MS/MS System | Triple quadrupole mass spectrometer with HPLC | Quantitative analysis of stability samples |
Stability studies—encompassing bench-top, freeze-thaw, and long-term storage evaluations—form an indispensable component of bioanalytical method validation for LC-MS/MS methods quantifying drug concentrations in plasma. These systematic assessments provide critical data that ensure the reliability of analytical results under conditions mimicking actual sample handling, processing, and storage scenarios. The experimental protocols outlined in this document, aligned with current regulatory expectations, offer a standardized approach for demonstrating analyte stability in biological matrices.
The continuous evolution of regulatory guidelines, particularly the recent ICH Q1 draft guidance, emphasizes a science- and risk-based approach to stability testing throughout the product lifecycle [102] [103]. This modernized framework encourages the application of knowledge gained during method development to design efficient yet comprehensive stability protocols. By implementing robust stability assessments during method validation and monitoring stability throughout the analytical lifecycle, researchers can generate high-quality, reliable data to support drug development and therapeutic monitoring decisions, ultimately contributing to improved patient care through precise pharmacokinetic characterization and optimized dosing regimens.
The reliability of bioanalytical data is paramount in making informed regulatory decisions regarding the safety and efficacy of drug products. Regulatory submissions for new drugs depend heavily on accurate concentration measurements of chemical and biological drug substances and their metabolites in biological matrices [104]. To ensure data integrity, regulatory agencies including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have established harmonized guidelines for bioanalytical method validation. The ICH M10 guideline, finalized in 2022 and implemented in early 2023, provides a unified framework for method validation and study sample analysis, replacing previous regional guidelines including the FDA's 2018 guidance and EMA's earlier requirements [105] [106] [107]. This document provides detailed application notes and protocols for adhering to these standards, specifically within the context of developing and validating LC-MS/MS methods for quantifying drug concentrations in plasma.
Regulatory Framework: ICH M10 Harmonization
The ICH M10 guideline, titled "Bioanalytical Method Validation and Study Sample Analysis," represents a significant achievement in global regulatory harmonization. It provides comprehensive recommendations for validating bioanalytical assays used in nonclinical and clinical studies that generate data to support regulatory submissions [105]. The scope encompasses both chromatographic methods (like LC-MS/MS) and ligand-binding assays for measuring chemical and biological drugs and their metabolites [104].
Guideline Status: ICH M10 reached Step 4 of the ICH process in May 2022. The FDA implementation date was November 7, 2022, while the EMA date of coming into effect was January 21, 2023 [107]. This guideline now supersedes the FDA's 2018 Bioanalytical Method Validation guidance and EMA's previous guideline (EMEA/CHMP/EWP/192217/2009 Rev. 1 Corr. 2) [106] [108].
Objective: The primary objective of validation is to demonstrate that a bioanalytical method is suitable for its intended purpose and can generate reliable results for regulatory decision-making [104]. The guidance covers procedures for both method validation and the subsequent application of the validated method to the analysis of study samples.
Q&A Document: An accompanying Frequently Asked Questions (FAQ) document provides further clarification on specific topics, such as procedures for investigating "Trends of Concern," which should be driven by a Standard Operating Procedure (SOP) and encompass the entire process from sample handling to analysis [104] [107].
Critical Validation Parameters for LC-MS/MS Methods
For an LC-MS/MS method quantifying drugs in plasma to be considered validated, specific performance parameters must be rigorously demonstrated. The following sections and corresponding tables detail these parameters and their acceptance criteria as per ICH M10, illustrated with examples from recent research.
Table 1: Key Validation Parameters and Acceptance Criteria for LC-MS/MS Methods according to ICH M10
| Validation Parameter | Evaluation Purpose | Typical Acceptance Criteria |
|---|---|---|
| Accuracy and Precision | To measure closeness to true value (accuracy) and degree of scatter (precision) [109] | Accuracy: ±15% (±20% at LLOQ); Precision: ≤15% CV (≤20% CV at LLOQ) [52] |
| Selectivity/Specificity | To confirm the assay unequivocally quantifies the analyte in the presence of matrix components | No significant interference (<20% of LLOQ for analyte, <5% for IS) from at least 6 different matrix sources |
| Linearity & Range | To demonstrate a proportional relationship between concentration and response | A defined concentration range where accuracy, precision, and linearity criteria are met (e.g., using ≥6 calibration levels) [52] |
| Lower Limit of Quantification (LLOQ) | The lowest concentration that can be measured with acceptable accuracy and precision | Signal-to-noise ratio ≥5; Accuracy and precision within ±20% [52] |
| Stability | To ensure analyte integrity under various storage and handling conditions | Stable for at least 8 days under various storage and handling conditions [52] |
Recent research on a validated LC-MS/MS method for anti-tuberculosis drugs in human lung tissue demonstrated the application of these parameters, proving the method to be "precise, accurate, and robust with no significant influence of matrix components" after validation according to FDA and EMA guidelines [109]. Similarly, an assay for cobicistat and venetoclax in plasma and serum reported accuracy within -5.9% to 2.4%, within-day precision from 1.2% to 4.8%, and between-day precision from 0.4% to 4.3%, all well within the required limits [52].
Table 2: Example Validation Data from a Published LC-MS/MS Method for Cobicistat and Venetoclax
| Analyte | Concentration Range (μg/L) | Accuracy Range (%) | Within-Day Precision (% CV) | Between-Day Precision (% CV) |
|---|---|---|---|---|
| Cobicistat | 5 - 500 [52] | -5.9 to 2.4 [52] | 1.2 to 4.8 [52] | 0.4 to 4.3 [52] |
| Venetoclax | 50 - 5000 [52] | -5.9 to 2.4 [52] | 1.2 to 4.8 [52] | 0.4 to 4.3 [52] |
Experimental Protocol: A Case Study in LC-MS/MS Method Validation
This protocol outlines the development and validation of an LC-MS/MS method for the simultaneous quantification of Cobicistat and Venetoclax in human plasma, based on a study that adhered to EMA and FDA (ICH M10) guidelines [52].
Materials and Reagents
- Analytes and Internal Standards (IS): Cobicistat, [^13C4,^2H3] Cobicistat (IS), Venetoclax, [^2H7] Venetoclax (IS).
- Matrices: Blank human EDTA plasma and blank human serum.
- Solvents and Chemicals: Acetonitrile, methanol, dimethyl sulfoxide (DMSO), ammonium formate, formic acid.
Chromatographic Conditions
- System: Ultra-high-performance liquid chromatography (UHPLC) system.
- Column: C18 column (e.g., 2.6 μm, 50 × 2.1 mm).
- Mobile Phase: A) 20 mmol/L ammonium formate (pH 3.5), B) Acetonitrile.
- Gradient Elution:
- 0.00 min: 30% B
- 0.000-0.300 min: 47.5% B
- 0.300-0.950 min: 75% B
- 0.950-1.400 min: 100% B
- 1.400-1.500 min: 30% B (re-equilibration)
- Flow Rate: 1.000 mL/min.
- Injection Volume: 0.5 μL.
- Column Oven Temperature: 60°C.
- Autosampler Temperature: 10°C [52].
Mass Spectrometric Conditions
- System: Triple quadrupole mass spectrometer with heated electrospray ionization (H-ESI) in positive mode.
- Ion Source Parameters: Spray voltage: 1500 V; Vaporizer temperature: 350°C; Sheath gas: 60 arb; Auxiliary gas: 25 arb.
- Detection: Selected reaction monitoring (SRM).
- SRM Transitions:
- Cobicistat: m/z 776.4 → 545.3 (Collision Energy (CE): 36 V)
- Cobicistat IS: m/z 783.4 → 552.3 (CE: 36 V)
- Venetoclax: m/z 868.4 → 321.1 (CE: 41 V)
- Venetoclax IS: m/z 875.4 → 321.1 (CE: 41 V) [52].
Sample Preparation
- Preparation of Standards and QCs: Prepare stock solutions of analytes in DMSO. Perform serial dilution in DMSO to create working solutions. Spike working solutions into blank plasma/serum to generate calibration standards and quality control (QC) samples. Final DMSO concentration should be <5% [52].
- Calibration Curve: Eight-point calibration curve for Cobicistat (5–500 μg/L) and Venetoclax (50–5000 μg/L) [52].
- Quality Controls: QC levels at LLQ, Low, Medium, and High concentrations for both analytes.
- Extraction: Homogenize samples followed by protein precipitation. A stable isotope-labelled IS is added to all samples (calibrators, QCs, and unknowns) to correct for variability [52].
Validation Experiments
The following workflow outlines the key stages in the bioanalytical method validation process:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of a validated LC-MS/MS method requires specific, high-quality materials. The following table details key reagents and their critical functions based on the cited protocols.
Table 3: Essential Research Reagents and Materials for LC-MS/MS Bioanalysis
| Item | Function / Purpose | Example from Protocol |
|---|---|---|
| Stable Isotope-Labeled Internal Standards (IS) | Corrects for analyte loss during sample preparation and ion suppression/enhancement in the mass spectrometer. Critical for achieving high accuracy and precision. | [^13C4,^2H3] Cobicistat and [^2H7] Venetoclax [52]. |
| Chromatography Column | Separates the analytes of interest from each other and from matrix components, reducing ion suppression and improving sensitivity. | C18 column (e.g., 2.6 μm, 50 × 2.1 mm) [52]. |
| Mass Spectrometry Solvents | High-purity solvents are essential for mobile phase preparation to minimize background noise and contamination, ensuring consistent analyte ionization. | LC-MS grade Acetonitrile and Methanol [52]. |
| Blank Biological Matrix | Serves as the foundation for preparing calibration standards and QCs. It is crucial for assessing selectivity and demonstrating the absence of interfering substances. | Blank human EDTA plasma and blank human serum [52]. |
| Buffer Salts | Used in the mobile phase to control pH and improve chromatographic peak shape and reproducibility. | Ammonium formate, buffered at pH 3.5 with formic acid [52]. |
Analysis of Study Samples and Incurred Sample Reanalysis (ISR)
Once a method is validated, it is applied to the analysis of actual study samples. ICH M10 provides recommendations for this phase to ensure continued reliability.
Acceptance Criteria for Run Acceptance: A bioanalytical run typically consists of a set of calibration standards, QCs (at least at three concentration levels), and the unknown study samples. The run is acceptable if a pre-specified number of QCs (e.g., ≥67%) fall within ±15% of their nominal concentration [104].
Incurred Sample Reanalysis (ISR): ISR is a critical component where a portion of study samples are reanalyzed to demonstrate the reproducibility of the method in the actual study matrix. ISR assesses the method's performance with samples containing metabolites and other components that may not be fully represented in spiked QCs. The investigation of any trends should be driven by an SOP and cover the entire process from sample handling to analysis [104] [107].
The application of a validated method to clinical samples, as demonstrated with the anti-tuberculosis drug assay, confirms the method's feasibility for its intended purpose and its potential to provide critical insights for drug development [109].
Adherence to the harmonized ICH M10 guideline is imperative for generating robust and reliable bioanalytical data that regulatory agencies will accept. The guidelines set forth a comprehensive framework for validating LC-MS/MS methods, from establishing fundamental parameters like accuracy, precision, and sensitivity to governing the analysis of study samples. As demonstrated through the cited examples, meticulous protocol design and execution, supported by high-quality reagents and materials, are the cornerstones of successful bioanalytical method validation. By following these structured application notes and protocols, researchers and drug development professionals can ensure their bioanalytical data meets the stringent standards required for regulatory submissions to both the FDA and EMA.
Comparative Analysis of Published Methods for Different Drug Categories
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) has become the cornerstone technique for the precise quantification of drug concentrations in plasma, playing a critical role in therapeutic drug monitoring (TDM), pharmacokinetic studies, and personalized medicine [14] [88]. The technology's superior sensitivity, specificity, and ability to simultaneously analyze multiple analytes makes it particularly valuable for optimizing dosing regimens for drugs with narrow therapeutic windows [52]. This application note provides a comprehensive comparative analysis of recently published LC-MS/MS methods across diverse therapeutic categories, highlighting standardized approaches and method-specific adaptations that ensure reliable analytical performance in clinical research and routine monitoring.
Comparative Methodologies for Diverse Drug Classes
The analysis of published methods reveals both universal principles and specific adaptations required for accurate drug quantification. The table below summarizes key analytical parameters for five recently developed LC-MS/MS methods.
Table 1: Comparative Analysis of Published LC-MS/MS Methods for Different Drug Categories
| Drug Category & Analytes | Sample Volume & Preparation | Chromatographic Column; Mobile Phase | Linear Range | Key MS Parameters (Ion Transitions) | Clinical/Research Application |
|---|---|---|---|---|---|
| Antibiotic [14]Omadacycline | 50 µL plasma;Protein precipitation | Phenomenex KINETEX XB-C18 (50 x 3.0 mm, 2.6 µm);0.1% FA in water / ACN (Gradient) | 20 - 2,000 ng/mL | ESI+; MRM;Omadacycline: 557.4 → 453.4IS (Fexofenadine-d6): 508.4 → 472.8 | TDM in critically ill patients |
| Oncology [110]Osimertinib, AZ7550, AZ5104 | Not Specified;Protein precipitation | Kinetex EVO C18 (150 x 2.1 mm, 2.6 µm);Not Specified | 1.25 - 3,000 ng/mL | ESI+; MRM(Ion transitions not specified) | TDM and PK studies in NSCLC patients |
| Oncology [111]Tepotinib | 1 mL plasma;Protein precipitation | Zorbax C18 (100 x 2.1 mm, 3 µm);0.1% HCOOH / ACN (85:15) | 1.5 - 1,200 ng/mL | ESI+; MRM;Tepotinib: 493.23 → 296.17IS (Axitinib): 387.12 → 220.08 | Bioequivalence and bioavailability studies |
| Antiviral/Oncology [52]Cobicistat, Venetoclax | Not Specified;Dilution in solvent | Accucore C18 (50 x 2.1 mm, 2.6 µm);Ammonium formate (pH 3.5) / ACN (Gradient) | Cobicistat: 5-500 µg/LVenetoclax: 50-5,000 µg/L | H-ESI+; SRM;Cobicistat: 776.4 → 545.3Venetoclax: 868.4 → 321.1 | TDM and PK boosting studies |
| Immunosuppressants [88]Tacrolimus, Everolimus, Sirolimus, Cyclosporine A, Mycophenolic acid (MPA) | 2.8 µL whole blood;Micro-sampling & protein precipitation | Not Specified | MPA: 0.1-50 µg/mLTac/Eve/Sir: <2-35 ng/mLCycA: 26-1866 ng/mL | MPA/MPAG: ESI-CIs: ESI+ | TDM in transplant patients with limited venous access |
Critical Insights from Comparative Data
Sample Preparation Universality: Protein precipitation is the most prevalent sample preparation technique across all drug categories due to its simplicity and effectiveness in removing phospholipids and other interfering compounds from plasma proteins [14] [110] [111]. This is crucial for minimizing matrix effects in mass spectrometric detection.
Chromatographic Consistency: Reversed-phase chromatography using C18 columns is the universal choice for compound separation. Mobile phases typically consist of a combination of aqueous acid (formic acid or ammonium formate) and acetonitrile, with gradient elution being preferred for resolving multiple analytes with different polarities [14] [52] [111].
Mass Spectrometric Detection: Electrospray ionization in positive mode (ESI+) is employed for the vast majority of small molecule drugs. The use of Multiple Reaction Monitoring (MRM) is universal, providing the high specificity required for quantifying drugs in complex biological matrices by monitoring specific precursor-to-product ion transitions [14] [52] [111].
Detailed Experimental Protocols
Sample Preparation Workflow
The following diagram illustrates the generalized sample preparation workflow common to the cited methods, with specific variations noted for different drug categories.
Generalized Sample Preparation Protocol:
Aliquot Plasma Sample: Pipette the specified volume of plasma (typically 50 μL) into a 1.5 mL microcentrifuge tube [14].
Add Internal Standard (IS): Add the appropriate volume of IS working solution. Stable isotope-labeled analogs (e.g., fexofenadine-d6 for omadacycline, [2H7] venetoclax) are preferred for optimal compensation of matrix effects and recovery variations [14] [52].
Protein Precipitation: Add a minimum of 3-4 volumes of ice-cold organic solvent (typically acetonitrile or methanol) to the sample. Vortex vigorously for 30-60 seconds to ensure complete mixing and protein denaturation [14] [111].
Centrifugation: Centrifuge samples at 13,000-15,000 rpm for 5-10 minutes at 4°C to pellet precipitated proteins [14] [111].
Supernatant Collection & Reconstitution: Transfer the clear supernatant to a new tube. For the omadacycline method, 50 μL of supernatant is diluted with 200 μL of 0.1% formic acid in water before analysis [14]. Alternatively, the supernatant may be evaporated to dryness under a gentle nitrogen stream at 45°C and reconstituted in a smaller volume of initial mobile phase to enhance sensitivity [111].
LC-MS/MS Analysis Conditions
Chromatographic Separation:
- Column Oven Temperature: Maintained between 40-60°C to ensure retention time reproducibility and optimal peak shape [14] [52].
- Flow Rate: Typically 0.4-1.0 mL/min depending on column dimensions and system configuration [14] [52].
- Injection Volume: Ranges from 0.5-10 μL, optimized to balance sensitivity and system carryover [14] [52].
- Gradient Elution: Essential for resolving multiple analytes. For example, the omadacycline method uses a 5-minute gradient from 10% to 95% organic phase, while the cobicistat/venetoclax method achieves rapid separation in under 1.5 minutes [14] [52].
Mass Spectrometric Detection:
- Ion Source: Electrospray Ionization (ESI) is universally employed. Source temperatures typically range from 150-450°C [14] [111].
- Ion Mode: Positive ionization (ESI+) is used for most small molecule drugs. Negative mode (ESI-) is reserved for specific analytes like mycophenolic acid and its glucuronide metabolite [88].
- Detection Mode: Multiple Reaction Monitoring (MRM) is the standard for quantification, monitoring specific precursor → product ion transitions for each analyte and IS [14].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagents and Materials for LC-MS/MS Method Development
| Reagent/Material | Function & Importance | Examples from Literature |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Corrects for analyte loss during sample prep and matrix effects during ionization; essential for accuracy and precision. | Fexofenadine-d6 [14], [13C4,2H3] Cobicistat, [2H7] Venetoclax [52], [2H7] Venetoclax [52] |
| LC-MS Grade Solvents | High-purity solvents minimize background noise and ion suppression, ensuring method sensitivity and robustness. | Acetonitrile, Methanol (HPLC grade) [14] [111] |
| Chromatographic Columns | C18 columns provide the primary separation mechanism; sub-3μm particle sizes offer high efficiency. | Phenomenex KINETEX XB-C18 [14], Zorbax C18 [111], Kinetex EVO C18 [110] |
| Mobile Phase Additives | Volatile acids (e.g., formic acid) enhance analyte ionization; volatile buffers (e.g., ammonium formate) aid separation. | 0.1% Formic Acid [14] [111], Ammonium Formate [52] |
| Quality Control Materials | Pooled human plasma from drug-free volunteers used to prepare calibration standards and QCs for validation. | Blank human EDTA plasma [52] [111] |
Method Validation & Regulatory Considerations
All cited methods were validated according to international guidelines (e.g., FDA, EMA), demonstrating that the fundamental validation parameters are consistent across drug categories [52]. Key validation parameters include:
- Selectivity and Specificity: Confirmed by analyzing blank plasma from at least six different sources to demonstrate no interference at the retention times of the analytes and IS [14].
- Linearity and Calibration: A minimum of six to eight calibration standards are used to construct a linear calibration curve using a weighted (1/x or 1/x²) least squares regression model [14] [111].
- Precision and Accuracy: Assessed by analyzing quality control (QC) samples at multiple concentrations (LLOQ, Low, Medium, High) in replicates across different runs. Acceptance criteria typically require precision (RSD) ≤15% and accuracy (RE) within ±15% for all QCs [14] [110].
- Carryover: Must be ≤20% of the LLOQ response for the analyte and ≤5% for the IS, ensuring that a high-concentration sample does not affect the subsequent analysis [14].
- Stability: Evaluated under various conditions including benchtop, processed sample (autosampler), freeze-thaw, and long-term storage. For instance, osimertinib and its metabolites were shown to be stable for over 3 years at -80°C [110].
This comparative analysis demonstrates that while LC-MS/MS method development for drug quantification follows a standardized framework, specific adaptations are required for different drug categories based on their physicochemical properties and clinical application requirements. The consistent use of protein precipitation for sample cleanup, C18 chromatography for separation, and ESI+/MRM for detection forms the foundation of robust bioanalytical methods. The detailed protocols and reagent solutions outlined herein provide a valuable resource for researchers and drug development professionals aiming to develop or implement LC-MS/MS methods for therapeutic drug monitoring and pharmacokinetic studies, ultimately supporting the advancement of personalized medicine.
Conclusion
The development and validation of robust LC-MS/MS methods are fundamental to advancing precision medicine, particularly in therapeutic drug monitoring and pharmacokinetics. This synthesis of foundational principles, practical applications, optimization strategies, and rigorous validation underscores the technique's indispensable role in generating reliable data for clinical decision-making. Future directions will likely involve increased automation, the integration of machine learning for data processing, and the expansion into novel biological matrices, further solidifying LC-MS/MS as a cornerstone technology for optimizing drug therapy and improving patient outcomes in biomedical research.
References
- 1. Principles and Applications of Liquid Chromatography ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2643089/]
- 2. Triple Quadrupole LC-MS/MS [https://www.shimadzu.com/an/products/liquid-chromatograph-mass-spectrometry/triple-quadrupole-lc-msms/index.html]
- 3. Triple Quadrupole Mass Spectrometry - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/triple-quadrupole-mass-spectrometry]
- 4. Development and validation of a novel LC-MS/MS method for ... [https://pubs.rsc.org/en/content/articlehtml/2025/ay/d5ay01143d]
- 5. Development and application of an LC–MS/MS method ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12297723/]
- 6. Development and validation of an LC-MS/MS method for ... [https://www.sciencedirect.com/science/article/pii/S1570023224004483]
- 7. Advancing the sensitivity of selected reaction monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3375056/]
- 8. 质谱MRM技术的原ç†å’Œä¼˜åŠ¿ [http://www.biotech-pack.com/lqa73.html]
- 9. 常压电喷雾离å化的机ç†åŠåº”用 [https://manu56.magtech.com.cn/progchem/CN/lexeme/showArticleByLexeme.do?articleID=12173]
- 10. Enhanced Sensitivity for Selected Reaction Monitoring ... [https://www.sciencedirect.com/science/article/pii/S1535947620327833]
- 11. Overview of Therapeutic Drug Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2687654/]
- 12. Application of Pharmacokinetic-Pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00997/full]
- 13. Therapeutic drug monitoring and LC-MS/MS [https://pubmed.ncbi.nlm.nih.gov/21992751/]
- 14. LC-MS/MS quantification of omadacycline in human ... [https://www.nature.com/articles/s41598-025-13396-3]
- 15. The Crucial Role of Pharmacodynamic and ... [https://arelabs.com/publications/the-crucial-role-of-pharmacodynamic-and-pharmacokinetic-studies-in-drug-development]
- 16. What You Need to Know about PK/PD for a Job in Pharma [https://grad.rutgers.edu/news/ijobs-primer-what-you-need-know-about-pkpd-job-pharma]
- 17. Part 3—Introduction to Pharmacodynamic Modeling Methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC3917320/]
- 18. An Easily Expandable Multi-Drug LC-MS Assay for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8699473/]
- 19. Implementation of pharmacokinetic and pharmacodynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4112793/]
- 20. Liquid Chromatography Coupled with Tandem Mass ... [https://www.spectroscopyonline.com/view/liquid-chromatography-coupled-tandem-mass-spectrometry-clinical-applications]
- 21. LC-MS/MS Method Development and Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567155/]
- 22. Recent Advances in Liquid Chromatography–Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204688/]
- 23. LC–MS/MS-based multiplex antibacterial platform for ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1116071/full]
- 24. Comparison of Traditional HPLC-MS/MS Sensitivity to the ... [https://alturasanalytics.com/resource/eksigentposter/]
- 25. New HPLC, MS, and CDS Products from 2024–2025 [https://www.chromatographyonline.com/view/new-hplc-ms-and-cds-products-from-2024-2025-a-brief-review]
- 26. Advantages, Limitations, And Future Trends Of High- ... [https://www.alwsci.com/news/advantages-limitations-and-future-trends-of-85237687.html]
- 27. Mobile Phase Optimization: A Critical Factor in HPLC [https://www.phenomenex.com/knowledge-center/hplc-knowledge-center/mobile-phase-in-chromatography?srsltid=AfmBOop2Q_Hp-XiX91V5I30nE4SY2d0UdnCfGbFg5pGpmiccGDCwFChv]
- 28. Mobile Phase Selection in Method Development [https://www.welch-us.com/blogs/knowleage-base/mobile-phase-selection-in-method-development-how-to-optimize]
- 29. LC-MS Sample Preparation [https://www.thermofisher.com/us/en/home/industrial/mass-spectrometry/mass-spectrometry-learning-center/liquid-chromatography-mass-spectrometry-lc-ms-information/lc-ms-sample-preparation.html]
- 30. Development and Validation of a UHPLC-MS/MS Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255265/]
- 31. Optimizing Mobile Phase Composition: A Practical Approach ... [https://www.mastelf.com/optimizing-mobile-phase-composition-a-practical-approach-to-enhancing-hplc-performance/]
- 32. Optimization of Mobile Phase Modifiers for Fast LC-MS ... [https://pubmed.ncbi.nlm.nih.gov/36768308/]
- 33. 4 Steps to Successful Compound Optimization on LC-MS/MS [https://www.technologynetworks.com/analysis/how-to-guides/4-steps-to-successful-compound-optimization-on-lc-msms-311382]
- 34. Comparison of different serum sample extraction methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4669428/]
- 35. LC-MS Sample Preparation: Techniques & Challenges [https://opentrons.com/applications/lc-ms-sample-preparation?srsltid=AfmBOorRqfSwcceHK45gdjqd73H5MdkUOwWrqC7asYWCnzi0fw802oyR]
- 36. LC–MS-MS Total Drug Analysis of Biological Samples ... [https://www.chromatographyonline.com/view/lc-ms-ms-total-drug-analysis-biological-samples-using-high-throughput-protein-precipitation-method]
- 37. Comparison of liquid–liquid extraction, microextraction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8830356/]
- 38. Liquid-liquid extraction pretreatment samples method used ... [https://www.sciencedirect.com/science/article/pii/S2095754817301242]
- 39. The Optimized Workflow for Sample Preparation in LC-MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6632171/]
- 40. Strategies for Developing Sensitive and Automated LC-MS/ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3986713/]
- 41. Comparison between 5 extractions methods in either ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10200056/]
- 42. Optimizing LC‑MS/MS Sensitivity: Strategies to Overcome ... [https://biotech-spain.com/en/articles/optimizing-lc-ms-ms-sensitivity-strategies-to-overcome-ion-suppression-and-boost-robustness-in-bioanalysis/]
- 43. Learn with Lin about LC–MS bioanalysis: part III tune ... [https://www.bioanalysis-zone.com/learn-with-lin-about-lc-ms-bioanalysis-part-iii-tune-the-triple-quadrupole-system_covance/]
- 44. Optimizing LC–MS and LC–MS-MS Methods [https://www.chromatographyonline.com/view/optimizing-lc-ms-and-lc-ms-ms-methods-1]
- 45. LC-MS/MS quantification of omadacycline in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307862/]
- 46. Species-specific optimization of oxylipin ionization in LC–MS [https://pmc.ncbi.nlm.nih.gov/articles/PMC11913994/]
- 47. Development and validation of an LC–MS/MS method ... [https://www.nature.com/articles/s41598-025-96764-3]
- 48. Preparation and pharmacokinetic evaluation of a sertraline ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d4ra08357a]
- 49. Omadacycline pharmacokinetics/pharmacodynamics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10848755/]
- 50. LC-MS/MS Method for Simultaneous Quantification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497388/]
- 51. tandem mass spectrometry assay for monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11625210/]
- 52. Validation of a LCâ€MS/MS Assay for Rapid and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12303788/]
- 53. Quantification of Venetoclax for Therapeutic Drug ... [https://pubmed.ncbi.nlm.nih.gov/35268708/]
- 54. Plasma concentrations of venetoclax and ... [https://www.nature.com/articles/s41397-024-00359-6]
- 55. LC–MS/MS method for the quantitation of decitabine and ... [https://www.sciencedirect.com/science/article/pii/S1319016423001883]
- 56. Vonoprazan: A Review in Helicobacter pylori Infection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11090951/]
- 57. LC-MS/MS Method Development and Validation for ... [https://pubmed.ncbi.nlm.nih.gov/41155622/]
- 58. Are plasma drug concentrations still necessary? Rethinking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341389/]
- 59. Recent advances in the determination of unbound ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914020313436]
- 60. 8 Essential Characteristics of LC-MS/MS Method Validation [https://www.resolian.com/bioanalytics/8-essential-characteristics-of-lc-ms-ms-method-validation/]
- 61. Tips for Optimizing Key Parameters in LC–MS [https://www.chromatographyonline.com/view/tips-optimizing-key-parameters-lc-ms]
- 62. Liquid chromatography–tandem mass spectrometry for clinical diagnostics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9735147/]
- 63. Development and Validation of Bioanalytical LC–MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300523/]
- 64. Development and validation of an LC-MS/MS method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3659617/]
- 65. Enhancement of Sensitivity and Quantification Quality in the LC-MS/MS Measurement of Large Biomolecules with Sum of MRM (SMRM) - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8804067/]
- 66. Simultaneous LC-MS/MS Method for the Quantitation of Probenecid, Albendazole, and Its Metabolites in Human Plasma and Dried Blood Spots | MDPI [https://www.mdpi.com/2297-8739/11/7/197]
- 67. Matrix Effects and Ion Suppression in LC-MS [https://www.longdom.org/open-access/matrix-effects-and-ion-suppression-in-lcms-essential-strategies-for-research-1100713.html]
- 68. Drug-mediated ion suppression and mitigation of ... [https://www.sciencedirect.com/science/article/abs/pii/S1570023219315223]
- 69. Strategies for the Detection and Elimination of Matrix ... [https://www.chromatographyonline.com/view/strategies-detection-and-elimination-matrix-effects-quantitative-lc-ms-analysis]
- 70. Mitigating matrix effects in oil and gas wastewater analysis [https://pubs.rsc.org/en/content/articlehtml/2025/em/d4em00716f]
- 71. Mitigating Matrix Effects in LC–ESI–MS/MS Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10949524/]
- 72. Ionization Methods in Mass Spec: Making Molecules Fly [https://bitesizebio.com/82650/ionization-methods-mass-spec/]
- 73. Electrospray Ionisation Mass Spectrometry: Principles and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1853331/]
- 74. LC–MS Sensitivity: Practical Strategies to Boost Your ... [https://www.chromatographyonline.com/view/lc-ms-sensitivity-practical-strategies-boost-your-signal-and-lower-your-noise]
- 75. 10 Great Tips for Electrospray Ionization LC–MS [https://www.chromatographyonline.com/view/the-lcgc-blog-10-great-tips-for-electrospray-ionization-lc-ms]
- 76. How to Maximize Sensitivity in LC-MS [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/analytical-chemistry/small-molecule-hplc/tips-and-tricks-sensitivity-gains-in-lcms?srsltid=AfmBOopw4EAd2EAdmhEy-B0JaRScsnqyCJu6DXRmps997Py5f33qIMu6]
- 77. Selection of the Optimum Electrospray Voltage for Gradient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2692488/]
- 78. LC-MS Method for Studying the Pharmacokinetics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4842247/]
- 79. Development and Validation of an LC-MS/MS Method for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9860615/]
- 80. Real Solutions to Improve Your HPLC Peak Resolution [https://www.thermofisher.com/blog/analyteguru/real-solutions-to-improve-your-hplc-peak-resolution/]
- 81. Peak Shapes and Their Measurements [https://www.chromatographyonline.com/view/peak-shapes-and-their-measurements-need-and-concept-behind-total-peak-shape-analysis-0]
- 82. 高效液相色谱仪æ“作“三è¦ç‚¹â€-环境检测 [https://www.shiyanjia.com/knowledge-articleinfo-1974.html]
- 83. CN114814018A - 通过lc-ms/ms测定人血浆ä¸å¤šè¥¿æ‹‰æ•çš„方法 [https://patents.google.com/patent/CN114814018A/zh]
- 84. 基于LC-MS/MS技术的ä¹ç§æ–°åž‹é¶å‘抗癌è¯ç‰©è¡€æµ†æµ“度监测 ... [https://www.ebiotrade.com/newsf/2025-7/20250724133752801.htm]
- 85. Recommendations for Validation of LC-MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4287296/]
- 86. A Validated HPLC-MS/MS Method for Quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8577619/]
- 87. Development and Validation of a Novel LC-MS/MS Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9953620/]
- 88. Analytical Validation of an LC-MS/MS Method for ... [https://www.mdpi.com/1422-0067/26/13/6358]
- 89. Investigating the performance attributes of an ultra-high ... [https://sciex.com/tech-notes/technology/investigating-the-performance-attributes-of-an-ultra-high-pressu]
- 90. A highâ€throughput LC–MS/MS method for simultaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9787364/]
- 91. Development and validation of an LC–MS/MS method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9332635/]
- 92. Development of Simultaneous Drug Concentration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11435224/]
- 93. Validation of an LC-MS/MS method for urinary homovanillic ... [https://www.sciencedirect.com/science/article/pii/S2667145X25000148]
- 94. Validation of an LC-MS/MS Method for the Simultaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030624/]
- 95. Performance Comparison of Liquid Chromatography and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11834250/]
- 96. Development of a LC–MS/MS-based method for ... [https://www.sciencedirect.com/science/article/pii/S1021949813000057]
- 97. Development and validation of a reliable LC–MS/MS method ... [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-019-4580-x]
- 98. A Liquid Chromatography-Tandem Mass Spectrometry ... [https://pubmed.ncbi.nlm.nih.gov/40363673/]
- 99. Quantitation of tazemetostat in human plasma by LC-MS/MS [https://pmc.ncbi.nlm.nih.gov/articles/PMC11816758/]
- 100. Development and Validation of a Sensitive LC-MS/MS Method for ... [https://aaps2025.eventscribe.net/ajaxcalls/PosterInfo.asp?efp=SFZPSE9XSVEyNTE0Ng&PosterID=742241&rnd=0.6287519]
- 101. Q1 Stability Testing of Drug Substances and Drug Products [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q1-stability-testing-drug-substances-and-drug-products]
- 102. ICH Q1 Draft Guideline Marks a New Era for Stability Testing [https://stabilityhub.com/2025/09/07/ich-q1-draft-guideline-marks-a-new-era-for-stability-testing/]
- 103. Protocol Design and Lifecycle Following the Draft ICH ... [https://www.lachmanconsultants.com/2025/08/protocol-design-and-lifecycle-following-the-draft-ich-stability-guidance/]
- 104. ICH M10 on bioanalytical method validation - Scientific guideline [https://www.ema.europa.eu/en/ich-m10-bioanalytical-method-validation-scientific-guideline]
- 105. M10 Bioanalytical Method Validation and Study Sample ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m10-bioanalytical-method-validation-and-study-sample-analysis]
- 106. Bioanalytical method validation - Scientific guideline [https://www.ema.europa.eu/en/bioanalytical-method-validation-scientific-guideline]
- 107. ICH M10 Guideline on Bioanalytical Method Validation and ... [https://www.gmp-compliance.org/gmp-news/ich-m10-guideline-on-bioanalytical-method-validation-and-study-sample-analysis]
- 108. Bioanalytical Method Validation Guidance for Industry [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioanalytical-method-validation-guidance-industry]
- 109. Validation and clinical application of an LC-MS/MS method ... [https://www.sciencedirect.com/science/article/pii/S0731708525004340]
- 110. Development and validation of an LC-MS/MS method ... [https://pubmed.ncbi.nlm.nih.gov/39787847/]
- 111. Liquid chromatography and tandem mass spectrometric ... [https://japsonline.com/abstract.php?article_id=4597&sts=2]