Optimizing Cell Culture Conditions for Robust and Reproducible Drug Sensitivity Testing
This article provides a comprehensive guide for researchers and drug development professionals on optimizing cell culture conditions to enhance the accuracy and reproducibility of drug sensitivity testing.
Optimizing Cell Culture Conditions for Robust and Reproducible Drug Sensitivity Testing
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on optimizing cell culture conditions to enhance the accuracy and reproducibility of drug sensitivity testing. It covers foundational principles of cell viability assays and the impact of culture conditions on drug response. The content explores advanced methodological approaches, including 3D culture models and high-throughput screening protocols. A significant focus is given to troubleshooting common experimental pitfalls and optimizing critical parameters like cell seeding density and media composition. Finally, the article examines validated drug response metrics and AI-driven approaches for data analysis, offering a holistic framework for improving preclinical drug screening outcomes.
Laying the Groundwork: Principles and Pitfalls in Cell-Based Drug Screening
The Critical Link Between Cell Culture Conditions and Drug Response Reproducibility
Welcome to the Cell Culture Troubleshooting Hub
This resource center is designed to help researchers identify and resolve common issues that compromise the reproducibility of drug sensitivity testing. The guides and FAQs below are framed within the broader thesis that meticulous optimization of cell culture conditions is not just a preliminary step, but a critical and continuous requirement for generating reliable, translatable data in drug development.
Troubleshooting Guide: Common Cell Culture Issues Affecting Drug Response
| Problem Phenomenon | Potential Causes | Recommended Solutions & Preventive Measures |
|---|---|---|
| High inter-laboratory variability in GR50/IC50 | • Use of different cell viability assays (e.g., image-based count vs. ATP-based) [1]• Variation in cell culture medium composition and serum batches [2]• Differences in cell seeding density and passage number [1] | • Standardize viability assays across all experiments; validate surrogate assays against direct counts for each drug [1].• Use identical, high-quality medium and serum batches from the same supplier for a study series [2].• Optimize and document seeding density to ensure consistent proliferation rates without confluence at endpoint [1]. |
| Inconsistent dose-response curves & high replicate variance | • Evaporation from drug dilution and assay plates, leading to drug concentration spikes [2]• Inappropriate DMSO vehicle control concentration [2]• "Edge effects" from uneven incubator conditions [2] | • Use sealed plates (e.g., parafilm, PCR plate seals) for drug storage; avoid long-term storage of diluted drugs [2].• Use matched DMSO controls for each drug concentration instead of a single control [2].• Humidify incubators properly; use plate layouts that randomize or exclude edge wells [2]. |
| Poor cell growth or viability in control wells | • Microbial contamination (e.g., bacteria, fungi, mycoplasma) [3]• Toxic impurities in media or labware (e.g., endotoxins, detergents) [3] [4]• Incorrect incubation conditions (temperature, CO2, vibration) [4] | • Implement routine mycoplasma testing using PCR-based kits; practice strict aseptic technique [3].• Use qualified, cell culture-grade reagents and consumables; test new media batches [4].• Regularly calibrate incubators; ensure they are level and placed on stable, vibration-free surfaces [4]. |
| Altered cellular morphology or unexpected drug efficacy | • Genetic drift or cell line misidentification [3]• Changes in extracellular matrix (ECM) components in 3D cultures [5]• Drug-induced changes in cell size/metabolism, affecting ATP-based assays [1] | • Authenticate cell lines regularly (e.g., STR profiling); obtain cells from reputable cell banks [3].• Standardize and document the lot of ECM materials like Corning Matrigel matrix [5].• For drugs affecting metabolism, use direct cell counting methods instead of metabolic assays like CellTiter-Glo [1]. |
Frequently Asked Questions (FAQs)
Q1: Why do we observe up to 200-fold differences in drug potency (GR50) when the same protocol is used by different labs? This extreme variability often stems from biological context-sensitive factors rather than just technical pipetting errors. A multi-center study found that the choice of cell viability assay is a major driver. For instance, ATP-based assays (e.g., CellTiter-Glo) and direct image-based cell counts can give vastly different results for drugs like Palbociclib because the drug alters cell size and ATP content, breaking the assumption that ATP is proportional to cell number [1]. Other factors include subtle differences in incubation conditions and the handling of drug stocks [1] [2].
Q2: How can evaporation affect my drug sensitivity results, and how do I prevent it? Evaporation from drug dilution plates or assay plates concentrated your drugs and culture medium, leading to falsely elevated potency estimates (lower IC50/GR50). One study showed that storing diluted drugs in 96-well plates at 4°C or -20°C for just 48 hours significantly altered cell viability readings due to evaporation [2]. Prevention: For drug storage, use sealed PCR plates with aluminum tape instead of standard culture microplates, as they are less prone to evaporation. For long-term assays, ensure incubators are properly humidified and consider using microplates specifically designed to minimize evaporation [2].
Q3: My cell lines are growing poorly, and drug responses are erratic. What are the first things I should check? Begin with these fundamental checks:
- Contamination: Rule out microbial contamination, especially mycoplasma, which can alter cell growth and metabolism without causing visible cloudiness [3].
- Culture Technique: Ensure consistent and gentle mixing of the cell inoculum to avoid foam and bubbles, which can hinder uniform attachment and growth [4].
- Culture Conditions: Verify that your incubator maintains a stable temperature, CO2 level, and humidity. Position cultures away from the door to minimize fluctuations from frequent opening [4].
- Reagents: Check the expiration dates of your media, serum, and supplements. Test a new batch of serum or media to rule out reagent-specific issues [4].
Q4: When testing patient-derived organoids (PDOs), how can I improve the consistency of IC50 calculations between different operators? Recent research highlights several key strategies:
- Calculation Method: For PDOs, IC50 values derived from GraphPad's Dose-response-Inhibition (DRI/logit) and LC-logit methods show minimal variation even when the number of drug concentrations is reduced [6].
- Alternative Metrics: Consider using the Area Under the dose-response Curve (AUC), which correlates strongly with IC50 and often demonstrates lower variance between technical replicates [6].
- Technical Consistency: Use opaque-bottom plates instead of transparent-bottom plates for luminescent viability assays, as they yield higher measurement precision [6].
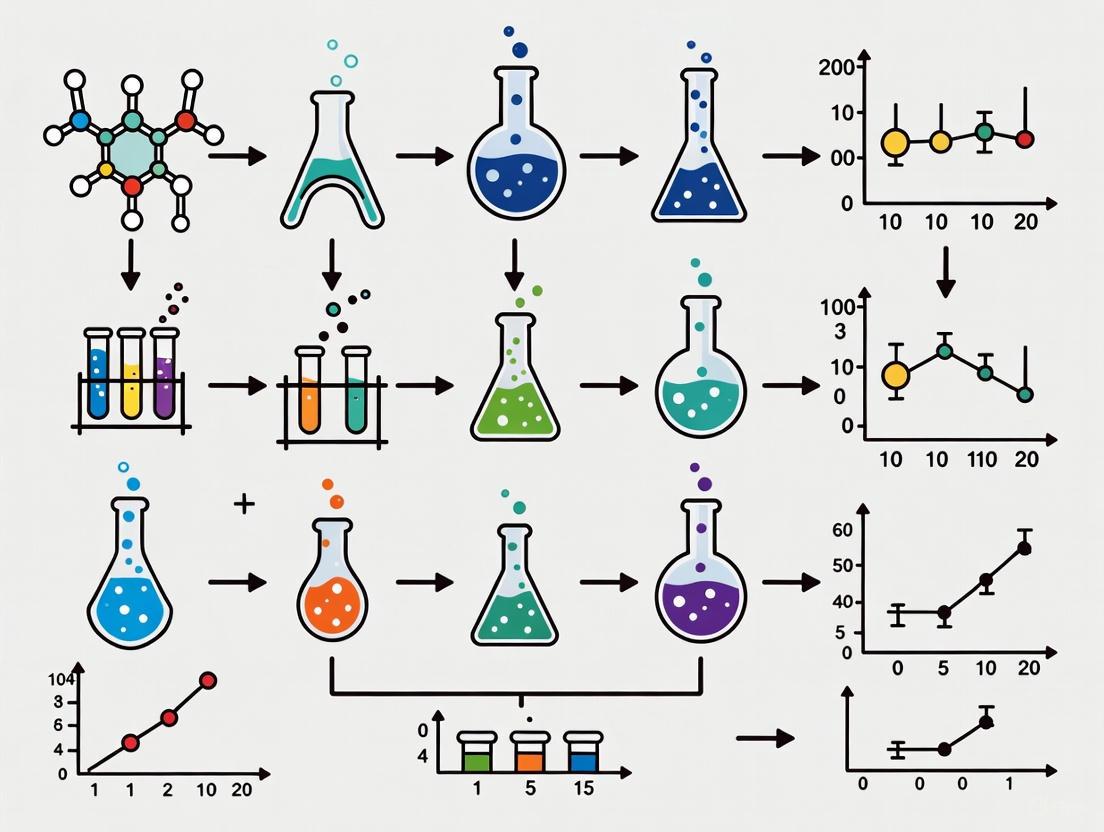
Experimental Protocol: Optimizing a Drug Sensitivity Assay
The following workflow, based on published reproducibility studies [2], provides a detailed methodology for optimizing a 2D cell-based drug sensitivity assay to minimize variability.
Step-by-Step Methodology:
- Define Baseline Protocol: Begin with standard, literature-based parameters. For example, plate cells at a common density (e.g., 1.0 × 10ⴠcells/well in a 96-well plate) in a serum-free medium to avoid serum-induced reduction of drug activity [2].
- Identify Confounders: Systematically test potential sources of error.
- Evaporation: Store diluted drugs in different plate types (e.g., standard culture microplates vs. sealed PCR plates) at 4°C and -20°C for 48-72 hours. Measure volume loss and test the effects on cell viability [2].
- DMSO Toxicity: Treat cells with a range of DMSO concentrations (e.g., 0.1% to 5%) for the assay duration. Cell viability decreases substantially with as little as 1% DMSO, necessitating matched vehicle controls [2].
- Edge Effects: Incolate a plate where all wells contain the same treatment (e.g., DMSO control). Measure the viability in all wells after incubation. Elevated readings in perimeter wells confirm an edge effect [2].
- Test & Optimize Parameters: Implement solutions based on your findings.
- Use sealed plates for drug storage and pre-warm media to reduce condensation-related issues.
- Include a DMSO vehicle control that matches the concentration present in each drug dose.
- Use plate layouts that exclude perimeter wells or fill them with PBS, randomizing the positions of treatments and controls.
- Establish Quality Control (QC) Metrics: Calculate metrics like the Z-factor to ensure your optimized assay is robust. A Z-factor > 0.5 indicates an excellent assay suitable for screening [2].
- Validate with Controls: Finally, run the fully optimized assay using a well-characterized cell line (e.g., MCF7) and a control drug (e.g., Bortezomib) to generate reference dose-response curves and potency values (IC50, GR50) [2].
Table 1: Impact of Assay Parameters on Cell Viability Measurements. Data synthesized from systematic investigations into replicability of drug screens [2].
| Parameter Tested | Condition 1 | Condition 2 | Effect on Cell Viability (IC50/AUC) | Key Finding |
|---|---|---|---|---|
| Drug Storage & Evaporation | 48h at 4°C in culture plate | 48h at -20°C in culture plate | Significant decrease in IC50 for both | Location (4°C vs. -20°C) had no effect, but evaporation occurred in both, concentrating the drug [2]. |
| Drug Storage & Evaporation | 72h in culture plate (Parafilm) | 72h in PCR plate (Aluminum tape) | N/A | Evaporation rate was significantly faster in standard culture microplates compared to sealed PCR plates [2]. |
| DMSO Vehicle Control | Single 1% DMSO control | Matched DMSO controls | Viability >100% at start of curve with single control | Using a single, high-concentration DMSO control for all doses led to artifactual dose-response curves [2]. |
| Viability Assay Method | Image-based cell count | ATP-based (CellTiter-Glo) | GRmax differed by 0.57 for Palbociclib | Discrepancy is drug-dependent; ATP assays are unreliable for drugs that alter cell size or metabolism [1]. |
| Plate Type for Luminescence | Transparent-bottom plate | Opaque-bottom plate | N/A | Opaque-bottom plates yielded higher precision in cell viability measurements for PDO-based assays [6]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials and Reagents for Reproducible Drug Sensitivity Assays.
| Item | Function & Importance in Drug Screens |
|---|---|
| Corning Matrigel Matrix | A basement membrane extract used for establishing 3D organoid and spheroid cultures. It provides a physiologically relevant microenvironment for studying tumor biology and drug response [5]. |
| Validated Cell Line Stock | Authenticated, low-passage cell stocks obtained from reputable banks (e.g., ECACC). Critical for preventing genetic drift and misidentification, which are major sources of irreproducible data [3]. |
| Characterized Fetal Bovine Serum (FBS) | A complex supplement providing growth factors and nutrients. Batch-to-batch variability can significantly alter cell growth and drug response; therefore, testing and using large, single batches for a study is essential [3] [2]. |
| DMSO (Cell Culture Grade) | A common solvent for water-insoluble drugs. Must be used at the lowest possible concentration (typically <0.5%) with matched vehicle controls for each dose to avoid solvent toxicity confounding results [2]. |
| Spheroid Microplates / ULA Plates | Microplates with ultra-low attachment (ULA) surfaces or specialized geometry to promote the formation and maintenance of 3D spheroids and organoids for more predictive screening models [5]. |
| Quality Control Assays (e.g., Mycoplasma Tests) | Routine use of PCR- or enzyme-based kits to detect microbial contamination, particularly mycoplasma, which can alter cell physiology and drug sensitivity without visible signs [3]. |
| Silibinin | Silibinin, CAS:1265089-69-7, MF:C25H22O10, MW:482.4 g/mol |
| DL-alpha-Tocopherol | Alpha-Tocopherol |
Core Principles and Mechanisms
What are the fundamental principles behind WST-1 and resazurin assays?
Both WST-1 and resazurin assays are colorimetric methods that measure cellular metabolic activity as a proxy for cell viability. Despite this common goal, they operate through distinct biochemical mechanisms.
WST-1 Assay Principle: The WST-1 assay utilizes a tetrazolium salt that is cleaved by mitochondrial dehydrogenases in metabolically active cells. This reaction requires an intermediate electron acceptor to shuttle electrons from the cellular metabolic pathways to the WST-1 molecule, resulting in the production of a water-soluble formazan dye. The amount of formazan produced is directly proportional to the number of viable cells and can be quantified by measuring absorbance at 440-450 nm using a microplate reader [7].
Resazurin Assay Principle: Also known as the Alamar Blue assay, the resazurin assay employs a cell-permeable blue dye that is reduced primarily by mitochondrial enzymes within viable cells. This reduction converts resazurin to resorufin, a highly fluorescent pink compound that is released back into the culture medium. The fluorescence intensity, measured with excitation at 530-570 nm and emission at 580-620 nm, provides a reliable estimate of viable cell numbers [8].
The diagram below illustrates the key differences in the biochemical pathways of these two assays:
Comparative Analysis of Cell Viability Assays
How do different cell viability assays compare in performance characteristics?
The selection of an appropriate cell viability assay depends on multiple factors including sensitivity, detection method, and experimental requirements. The table below provides a comprehensive comparison of key assay types:
| Assay Type | Detection Method | Sensitivity | Incubation Time | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| WST-1 | Absorbance (440-450 nm) | Generally higher than MTT, MTS [7] | 0.5-4 hours [7] | Water-soluble product; no solubilization required; suitable for time-course studies [7] | May require intermediate electron acceptor; higher background than MTT [7] |
| Resazurin | Fluorescence (Ex/Em: ~535/590 nm) | More sensitive than tetrazolium assays [8] | 30 min-4 hours (cell type dependent) [8] | Non-toxic at low concentrations; wide dynamic range; suitable for time-lapse experiments [8] | Fluorescence interference possible; incubation time critical [8] |
| MTT | Absorbance (570 nm) | Lower than WST-1 [7] | 1-4 hours [9] | Simple; widely used; inexpensive [9] | Formazan insoluble (requires solubilization); toxic to cells [9] |
| MTS | Absorbance (490-500 nm) | Intermediate between MTT and WST-1 [7] | 1-4 hours [10] | Water-soluble product; no solubilization required [10] | Requires intermediate electron acceptor [10] |
| ATP Assay | Luminescence | Excellent sensitivity and broad linearity [10] | 10 minutes [10] | Fast; sensitive; less prone to artifacts [10] | Requires cell lysis; endpoint measurement only [10] |
Troubleshooting Common Experimental Issues
Why might my viability assay show inconsistent results between replicates?
Inconsistent results often stem from improper assay optimization or technical artifacts. The following table addresses common issues and their solutions:
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| High background signal | Culture medium components interfering with detection; incorrect wavelength settings; contaminated reagents [7] [8] | Include proper blank controls (medium + reagent only); optimize excitation/emission wavelengths for your cell type [8]; use fresh, filtered reagents [11] |
| Poor linearity with cell concentration | Incorrect incubation time; over- or under-confluent cells; depleted resazurin in high-density wells [8] | Optimize incubation time for each cell line; ensure cells are in log phase growth; perform cell titration experiments [8] [11] |
| Unexpectedly high signal in treated groups | Chemical interference from test compounds (antioxidants, reducing agents) [7] [9] | Include compound-only controls (no cells); consider alternative detection methods (e.g., ATP assay) [9] |
| Low signal-to-noise ratio | Suboptimal cell density; incorrect assay parameters; low metabolic activity [8] | Determine optimal seeding density empirically; validate wavelength selection for your cell type [11]; ensure healthy cell cultures |
| Inconsistent reduction in spheroids | Limited dye penetration due to tight cell-cell interactions [12] | Disrupt tight junctions mechanically or chemically; consider alternative viability assays for 3D models [12] |
How can I optimize resazurin assay parameters for my specific cell type?
Optimizing resazurin assays requires systematic evaluation of key parameters. Recent research demonstrates that applying standardized operating procedures can achieve measurement uncertainty of less than 10% [11]. Follow this workflow for optimal results:
Implementation Notes:
- Wavelength Optimization: Test various excitation/emission combinations within the resazurin spectra (e.g., λEx: 530, 535, 540, 545 nm paired with λEm: 585, 590, 595 nm) and select the combination providing the highest fluorescence intensity with minimal background [11].
- Incubation Time Determination: Evaluate different incubation periods (1-6 hours) across a range of cell densities. Optimal time provides linear response (R² > 0.99) between fluorescence intensity and cell number [8] [11].
- Assay Limits Establishment: Calculate Limit of Blank (LoB), Limit of Detection (LoD), and Limit of Quantification (LoQ) to define the reliable working range of your assay [11].
Experimental Protocols for Drug Sensitivity Testing
What is a standardized protocol for conducting drug sensitivity testing using viability assays?
The following protocol provides a robust framework for drug sensitivity testing (DST) applicable to both single-agent and combination therapy screening [13].
Materials Required:
- Cell line of interest (e.g., HeLa cells for cervical cancer studies)
- 96-well flat-bottom tissue culture plates
- WST-1 or resazurin assay reagent
- Test compounds at appropriate concentrations
- Microplate reader capable of absorbance/fluorescence detection
- Cell culture incubator (37°C, 5% CO₂)
Procedure:
- Cell Seeding: Harvest exponentially growing cells and seed into 96-well plates at optimized density. For adherent cells, typical densities range from 3,000-10,000 cells/well depending on growth rate.
- Pre-incubation: Incubate plates for 24 hours under standard culture conditions to allow cell attachment and recovery.
- Drug Treatment:
- Prepare serial dilutions of test compounds in culture medium.
- For combination studies, use checkerboard designs to evaluate multiple concentration ratios.
- Include vehicle controls and blank wells (medium only).
- Treatment Incubation: Incubate plates for desired exposure period (typically 48-72 hours for cytotoxicity assessment).
- Viability Assessment:
- WST-1 Method: Add 10 μL WST-1 reagent per 100 μL culture medium. Incubate for 0.5-4 hours until color development is sufficient. Measure absorbance at 440-450 nm with reference wavelength >600 nm [7].
- Resazurin Method: Add resazurin working solution (final concentration 10-44 μM). Incubate for optimized duration (1-6 hours based on cell type). Measure fluorescence at optimal wavelengths (e.g., λEx 535 nm/λEm 590 nm) [11].
- Data Analysis: Calculate percentage viability relative to untreated controls. Generate dose-response curves and determine ICâ‚…â‚€ values using appropriate software (e.g., SynergyFinder for combination studies) [13].
Research Reagent Solutions
What essential materials are required for implementing these viability assays?
The table below outlines key reagents and their functions in cell viability assessment:
| Reagent/Material | Function | Application Notes |
|---|---|---|
| WST-1 Assay Reagent | Tetrazolium salt cleaved by mitochondrial dehydrogenases to soluble formazan [7] | Use at 10 μL per 100 μL medium; requires intermediate electron acceptor for some formulations [7] |
| Resazurin Sodium Salt | Cell-permeable blue dye reduced to fluorescent resorufin by metabolically active cells [8] | Prepare fresh working solution (e.g., 44 μM); protect from light; filter-sterilize [11] |
| 96-well Tissue Culture Plates | Platform for cell growth and treatment | Use flat-bottom plates for adherent cells; ensure uniform cell seeding |
| Intermediate Electron Acceptors | Facilitate electron transfer for WST-1 reduction (e.g., 1-methoxy PMS) [7] | May be toxic to cells at high concentrations; requires optimization [7] |
| Microplate Reader | Detection of absorbance/fluorescence signals | Ensure appropriate filters/wavelengths; validate instrument performance regularly |
| Cell Culture Medium | Supports cell growth during treatment | Phenol-red free medium may reduce background for absorbance assays [7] |
Frequently Asked Questions
Can these viability assays be used for 3D cell culture models?
The application of viability assays to 3D cultures requires careful consideration. While resazurin assays are widely used for 3D models, recent research indicates that compact spheroids with tight cell-cell interactions may hamper resazurin uptake and reduction, potentially leading to underestimated viability [12]. Disruption of tight junctions through trypsinization or EDTA treatment can restore accurate measurement correlation [12]. For complex 3D models, consider validating results with multiple assay types or using ATP-based assays which may provide more reliable quantification.
How can I distinguish between cytotoxic and cytostatic effects in my experiments?
Distinguishing between these mechanisms requires complementary approaches:
- Time-course Analysis: Monitor viability at multiple time points. Cytotoxic compounds show progressive cell death, while cytostatic agents typically maintain viability at initial levels without progression to death.
- Multiplexing Approaches: Combine viability assays with direct cytotoxicity markers (e.g., LDH release, dead-cell proteases) [10]. This allows simultaneous assessment of viable and dead cell populations.
- Morphological Assessment: Complement quantitative data with visual inspection of cellular morphology.
- Recovery Experiments: Wash out compounds after treatment and monitor whether cells resume proliferation, indicating cytostatic rather than cytotoxic effects.
What are the critical considerations for assay validation in drug sensitivity testing?
Robust validation of viability assays for drug screening should address:
- Linearity and Range: Establish the linear range of the assay for your specific cell line through cell titration experiments [11].
- Precision: Determine repeatability (intra-assay) and reproducibility (inter-assay) variability, aiming for less than 20% imprecision [8].
- Specificity: Verify that assay signals specifically reflect viable cell metabolism through appropriate controls.
- Limits of Detection and Quantification: Define the minimum number of detectable and quantifiable cells [11].
- Interference Testing: Evaluate potential interference from test compounds, especially in fluorescence-based assays [8].
Implementing these validation parameters will enhance the reliability of your drug sensitivity data and facilitate comparisons across studies and laboratories.
How Cellular Metabolism and Microenvironment Influence Drug Efficacy
FAQs: Core Concepts and Troubleshooting
FAQ 1: Why do cancer cells in traditional 2D culture often show different drug sensitivity compared to in vivo tumors?
The primary reason is that traditional 2D culture fails to replicate the complex three-dimensional architecture and cellular interactions of the tumor microenvironment (TME). In 2D cultures [14]:
- Cells adopt a flat, unnatural morphology and exhibit rapid, uncontrolled proliferation.
- They lack cell-cell and cell-matrix communication, which are critical for maintaining proper cell polarity, differentiation, and function.
- This leads to altered gene expression and metabolism patterns, which are key determinants of drug sensitivity.
Consequently, drug responses observed in 2D-cultured cancer cells may not accurately reflect the behavior of tumors in vivo, where the TME imposes intense metabolic stress through nutrient competition and lactate-driven acidification [15].
FAQ 2: What are the key metabolic interactions in the TME that can lead to drug resistance?
The TME is an ecosystem where different cell types compete for resources and engage in metabolic crosstalk, often creating an immunosuppressive milieu that promotes drug resistance. Key interactions include [16]:
- Nutrient Competition: Tumor cells and immune cells, particularly T cells, compete for essential nutrients like glucose and amino acids. Tumor cells often outcompete T cells, leading to T cell dysfunction and impaired anti-tumor immunity.
- Lactate-Driven Acidification: Tumor cells preferentially use glycolysis, producing large amounts of lactate. This creates an acidic TME that suppresses the function of cytotoxic T cells and can promote the polarization of tumor-associated macrophages (TAMs) towards a pro-tumor, M2-like state.
- Metabolic Support: Cancer-associated fibroblasts (CAFs) can undergo metabolic reprogramming to produce energy-rich metabolites (like lactate and ketones) that are then used as fuel by cancer cells, a phenomenon known as the "reverse Warburg effect."
FAQ 3: Our lab is transitioning to 3D models. What are the common challenges in maintaining physiological relevance in 3D cultures for drug testing?
Successfully leveraging 3D models requires careful attention to culture conditions. Common challenges and their solutions include [14]:
- Challenge: Reproducibility and standardization of 3D spheroid/organoid formation.
- Solution: Utilize scaffold-based methods with defined extracellular matrix (ECM) substitutes like Corning Matrigel and employ automated liquid handling systems to improve consistency.
- Challenge: Inadequate nutrient and oxygen diffusion to the core of 3D structures, leading to necrotic centers that do not reflect viable tumor regions.
- Solution: Optimize the size of spheroids and consider dynamic culture systems (like bioreactors) to improve perfusion.
- Challenge: Failure to recapitulate the native tumor's cellular heterogeneity and stromal components.
- Solution: Develop co-culture systems that incorporate patient-derived cancer cells with relevant stromal and immune cells to better mimic the interactive TME.
Technical Guides: Methodologies and Protocols
Protocol: Establishing a Patient-Derived Tumor Organoid (PDTO) Model for Drug Sensitivity Testing
Patient-derived tumor organoids (PDTOs) preserve the genetic and phenotypic heterogeneity of the original tumor, making them a superior model for predictive drug testing [14].
Workflow Overview:
Detailed Methodology:
- Sample Processing: Obtain fresh tumor tissue from surgical resection or biopsy. Mechanically mince the tissue and digest it with a collagenase/hyaluronidase solution to create a single-cell suspension or small cell clusters [14].
- 3D Embedding: Mix the cell suspension with a basement membrane extract, such as Corning Matrigel, which provides a scaffold that mimics the native extracellular matrix. Plate the mixture as droplets in pre-warmed culture dishes.
- Culture Conditions: Overlay the solidified Matrigel droplets with a specialized, bespoke growth factor media tailored to the specific tumor type. This media typically contains factors like R-spondin 1, Noggin, and Wnt3a to support stem cell expansion and organoid growth.
- Passaging and Biobanking: Once organoids are established and reach a sufficient size (typically after 1-3 weeks), they can be enzymatically dissociated and re-embedded in Matrigel for expansion. Aliquots can be cryopreserved to create a biobank.
- Drug Sensitivity Testing (Pharmacotyping): Harvest and dissociate organoids into single cells or small fragments. Re-embed them in Matrigel in a 96-well plate. After 3-5 days, treat with a concentration gradient of the anti-tumor drugs of interest. Incubate for a predetermined period (e.g., 5-7 days).
- Viability Assessment: Measure cell viability using assays like CellTiter-Glo 3D, which quantifies ATP levels as a proxy for metabolically active cells. Calculate the half-maximal inhibitory concentration (IC50) for each drug.
Protocol: Analyzing Drug-Induced Metabolic Changes Using Constraint-Based Modeling
Genome-scale metabolic models (GEMs) can be used to infer changes in metabolic pathway activity from transcriptomic data following drug treatment, providing insight into mechanisms of drug synergy [17].
Workflow Overview:
Detailed Methodology:
- Cell Treatment and RNA Sequencing: Treat cancer cells (e.g., the gastric cancer line AGS) with individual kinase inhibitors (e.g., PI3Ki, MEKi) and their synergistic combinations. Include a DMSO vehicle control. Extract total RNA and perform RNA-sequencing.
- Bioinformatic Analysis: Identify differentially expressed genes (DEGs) for each treatment condition compared to control using a standard pipeline with tools like the DESeq2 package. Perform gene set enrichment analysis (GSEA) to understand broad functional changes.
- Metabolic Modeling with TIDE: Use the Tasks Inferred from Differential Expression (TIDE) algorithm. This constraint-based method maps the DEGs onto a genome-scale metabolic model (GEM) like Recon3D.
- TIDE evaluates the ability of the context-specific metabolic network to carry out defined metabolic tasks (e.g., "ornithine biosynthesis") based on the expression of associated genes.
- It calculates a score for each task, indicating whether its activity is increased, decreased, or unchanged upon drug treatment.
- Synergy Scoring: Introduce a metabolic synergy score that compares the pathway activity changes in the combination treatment to those observed in the individual drug treatments. This helps identify metabolic processes specifically and strongly altered by the drug synergy, such as downregulation of ornithine and polyamine biosynthesis in the case of PI3Ki–MEKi combination [17].
Data Presentation: Quantitative Comparisons
Table 1: Comparison of 2D vs. 3D Cell Culture Models for Drug Sensitivity Testing
| Parameter | 2D Culture | 3D Culture |
|---|---|---|
| Cell Morphology | Flat, stretched | In vivo-like, 3D structure [14] |
| Cell Proliferation | Rapid, contact-inhibited | Slower, more physiologically relevant [14] |
| Cell Function & Differentiation | Simplified, incomplete | Maintains polarity and normal differentiation [14] |
| Cell-Cell & Cell-Matrix Communication | Limited | Extensive, mimics in vivo interactions [14] |
| Gene Expression & Metabolism | Altered patterns | Closer to native tumor profiles [14] |
| Predictive Value for Drug Efficacy | Lower, often overestimates | Higher, better correlates with clinical response [14] |
| Suitability for High-Throughput Screening | High | Moderate (improving with new technologies) [14] |
Table 2: Metabolic Pathways in Key TME Cell Types and Potential Therapeutic Targets
| Cell Type | Key Metabolic Features | Associated Drug Targets & Experimental Reagents |
|---|---|---|
| Tumor-Associated Macrophages (TAMs) | M1-like: Glycolysis; M2-like: Oxidative Phosphorylation (OXPHOS), Fatty Acid Oxidation (FAO) [16] | CSF-1R inhibitors (e.g., Emactuzumab), Glutaminase (GLS) inhibitors, drugs targeting Fatty Acid Synthase (FASN) [16] |
| Cancer-Associated Fibroblasts (CAFs) | "Reverse Warburg": Glycolysis, lactate production; Autophagy; Glutamine metabolism [16] | Monocarboxylate Transporter inhibitors (MCTi), CB-839 (Telaglenastat - GLS inhibitor), Chloroquine (autophagy inhibitor) [16] |
| T Cells (TILs) | Effector T cells: Glycolysis, OXPHOS; Dysfunctional T cells: Mitochondrial defects, lipid accumulation [15] [16] | Immune checkpoint blockers (anti-PD-1, anti-CTLA-4), DRP-104 (a prodrug of the glutamine antagonist DON), L-arginine to enhance T cell function [16] |
| Tumor Endothelial Cells (TECs) | Glycolysis, Fatty Acid Oxidation [16] | PFKFB3 inhibitors, VEGF/VEGFR inhibitors (anti-angiogenics) [16] |
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Materials for Advanced TME and Metabolism Research
| Research Reagent / Solution | Primary Function in Experiment |
|---|---|
| Corning Matrigel Matrix | A basement membrane extract used as a scaffold for 3D cell culture, enabling the formation of organoids and spheroids by providing a physiologically relevant environment for cell growth and signaling [14] [5]. |
| Seahorse XF Analyzer Consumables | Cartridges and culture plates designed for real-time, live-cell analysis of metabolic function, specifically measuring glycolysis and mitochondrial respiration (OXPHOS) rates [14]. |
| CellTiter-Glo 3D Cell Viability Assay | A luminescent assay optimized for 3D models that measures ATP content, providing a reliable indicator of cell viability and compound cytotoxicity in complex microtissues [14]. |
| CRISPR/Cas9 Systems | Tools for precise genome editing (e.g., knockout of metabolic genes) in cell lines or patient-derived organoids to identify novel metabolic vulnerabilities and validate drug targets [5]. |
| Lactate Assay Kits | Colorimetric or fluorometric kits for quantifying lactate concentration in cell culture media, a key readout for glycolytic flux in cancer cells and the TME [16]. |
| Recombinant Human IL-15 | A cytokine used in co-culture experiments to augment T-cell proliferation and activation, thereby improving the efficacy of therapies like CDK4/6 inhibitors in an immunosuppressive TME [18]. |
| beta-Damascenone | beta-Damascenone, CAS:23726-93-4, MF:C13H18O, MW:190.28 g/mol |
| 2-Furancarboxylic acid | 2-Furoic Acid|Furan-2-carboxylic Acid Supplier |
Signaling Pathways and Metabolic Crosstalk
Metabolic Crosstalk in TME
Diagram illustrating the key metabolic interactions between cells in the Tumor Microenvironment (TME). Cancer cells outcompete T cells for nutrients, while both cancer cells and Cancer-Associated Fibroblasts (CAFs) secrete lactate, further suppressing immune function. Tumor-Associated Macrophages (TAMs) polarized to an M2-state contribute to an immunosuppressive milieu [15] [16].
Frequently Asked Questions (FAQs)
FAQ 1: What are the most common sources of variability in 2D drug sensitivity screens? The most common sources of variability are often related to cell culture conditions, drug storage and preparation, and assay protocol design. Specifically, evaporation of drug solutions, DMSO solvent cytotoxicity, and suboptimal cell seeding density can significantly impact the replicability and reproducibility of your results [2].
FAQ 2: How can I improve the consistency of my dose-response curves? To improve consistency, optimize and standardize your cell culture and assay protocols. This includes using matched DMSO controls for each drug concentration to correct for solvent cytotoxicity, ensuring proper sealing of plates to prevent evaporation, and determining the optimal cell seeding density for your specific cell line to avoid overgrowth or poor signal dynamic range [2].
FAQ 3: Why do I get inconsistent IC50 values between replicate experiments? Inconsistent IC50 values can stem from suboptimal drug storage conditions or unaccounted-for edge effects in microplates. Storing diluted drugs for extended periods, even at -20°C, can lead to evaporation and drug concentration, altering the effective dose. Furthermore, an "edge effect"—where cells in perimeter wells show different viability—can introduce bias if not controlled for by excluding these wells or using plate layouts that account for it [2].
FAQ 4: What drug response metrics are more robust for interlaboratory comparison? While IC50 and Emax are common, metrics for growth rate inhibition (GR) have been shown to produce more consistent interlaboratory results. These include GR50, GRmax, and GRAOC (Area Over the Curve), as they account for differences in cellular division rates better than conventional metrics [2].
Troubleshooting Guides
Issue 1: High Background or Inconsistent Signal in Viability Assays
Potential Causes and Solutions:
- Cause: Evaporation from drug and assay plates, leading to increased concentration of compounds and DMSO, which can be cytotoxic [2].
- Solution: Seal plates properly during storage and incubation. For long-term storage of diluted drugs, use sealed PCR plates instead of culture microplates, and avoid storing diluted drugs for more than 48 hours [2].
- Cause: Incorrect DMSO concentration across wells, leading to variable solvent toxicity [2].
- Solution: Use a matched DMSO vehicle control for each drug concentration rather than a single control for the entire plate. This ensures the DMSO concentration is consistent in all comparative wells [2].
- Cause: Suboptimal cell seeding density. Too few cells yield a weak signal; too many cells can lead to over-confluency and nutrient depletion by the end of the assay [2].
- Solution: Perform a cell titration experiment to determine the optimal cell number that keeps cells in the exponential growth phase throughout the assay duration without overgrowth. For example, for MCF7 cells in a 96-well format, a density of 7.5 × 10³ cells/well may be optimal [2].
Issue 2: Poor Replicability Between Technical Replicates
Potential Causes and Solutions:
- Cause: Edge effects in microplates, where cells in outer wells exhibit different growth and viability due to increased evaporation [2].
- Solution: Use only the inner 60 wells of a 96-well plate for critical assays. Fill the perimeter wells with sterile PBS or medium to create a humidified buffer zone [2].
- Cause: Instability of the drug compound in the chosen storage condition or medium [2].
- Solution: Prepare fresh drug dilutions for each experiment. If this is not feasible, validate the stability of your compounds under your specific storage conditions (e.g., -20°C in sealed PCR tubes) over the intended storage period [2].
- Cause: Inconsistent cell health or passage number.
- Solution: Use cells at a consistent, low passage number. Ensure cells are healthy and not contaminated. Use standardized culture conditions, including the same batch of growth medium and serum [19].
Issue 3: Lack of Reproducibility Between Different Analysts or Labs
Potential Causes and Solutions:
- Cause: Use of different drug response metrics that are sensitive to cellular growth rates [2].
- Solution: Adopt more robust growth rate-based metrics (GR) like GR50 and GRAOC instead of, or in addition to, traditional IC50 and AUC metrics [2].
- Cause: Variation in core cell culture protocols, such as medium composition (e.g., serum-free vs. serum-containing), assay incubation time, or the method of resorufin detection (absorbance vs. fluorescence) [2].
- Solution: Fully optimize and document all experimental parameters. Once optimized, create a Standard Operating Procedure (SOP) to be followed by all analysts. For example, using growth medium with 10% FBS and a defined resazurin incubation time can improve reproducibility [2].
The table below summarizes key experimental parameters and their impact on cell viability data, based on variance component analysis [2].
Table 1: Major Sources of Experimental Variability in Pharmacogenomic Screens
| Source of Variability | Impact on Data | Recommended Optimization Strategy |
|---|---|---|
| Pharmaceutical Drug & Cell Line | High impact on viability. Primary factors in variability [2]. | Use well-characterized cell lines and drugs. Validate each new model system. |
| Drug Storage (Evaporation) | Significant. Alters effective drug concentration, affecting IC50 and AUC [2]. | Store diluted drugs at -20°C in sealed PCR plates for ≤48 hours; avoid 4°C storage [2]. |
| DMSO Solvent Concentration | High cytotoxicity at ≥1% v/v. Causes dose-response curves to start >100% viability [2]. | Use matched DMSO vehicle controls for each drug dose [2]. |
| Cell Seeding Density | Medium. Affects dynamic range and can lead to overgrowth [2]. | Titrate cell number; e.g., use 7.5 x 10³ cells/well for MCF7 in 96-well format [2]. |
| Assay Incubation Time & Growth Medium | Lower impact, but can be cell line-specific [2]. | Standardize medium (e.g., with 10% FBS) and incubation time across experiments [2]. |
Experimental Protocols
This protocol provides a step-by-step guide to optimize a common cell viability assay to minimize variability.
1. Determine Optimal Cell Seeding Density:
- Seed cells in a 96-well plate at a range of densities (e.g., from 2.5 x 10³ to 2.0 x 10ⴠcells/well) in 100 µL of growth medium supplemented with 10% FBS. Avoid antibiotics to prevent unintended effects on cell viability.
- Incubate the plate for 24, 48, and 72 hours at 37°C in a humidified 5% CO₂ incubator.
- At each time point, add 10 µL of 10% (w/v) resazurin solution directly to the wells. Incubate for 2-4 hours.
- Measure fluorescence (Ex/Em ~560/590 nm) or absorbance (~570 nm and ~600 nm as a reference).
- Calculate the signal-to-background ratio. The optimal density is the one that provides a robust signal (e.g., >3-fold over background) while ensuring cells remain in the exponential growth phase throughout the entire assay duration.
2. Mitigating Evaporation and Edge Effects:
- Drug Preparation: Prepare drug working solutions fresh on the day of the experiment. If storage is necessary, aliquot and store at -20°C in a tightly sealed PCR plate for no more than 48 hours.
- Assay Plate Setup: When setting up the drug treatment assay, use only the inner 60 wells. Fill the perimeter wells with 100-200 µL of sterile PBS to create a humidified chamber, minimizing the "edge effect."
3. Controlling for DMSO Cytotoxicity:
- Prepare a master plate of drug dilutions in a way that the DMSO concentration is serially diluted alongside the drug.
- For each concentration of the drug tested, include a vehicle control well that contains the same concentration of DMSO but no drug. This "matched control" is used to calculate 100% viability for that specific DMSO concentration.
4. Data Acquisition and Analysis:
- After adding resazurin and incubating, measure the signal.
- For each drug concentration, calculate the percentage of cell viability relative to its matched DMSO vehicle control.
- Use nonlinear regression to fit the dose-response curve and calculate metrics like IC50, GR50, or AUC. The use of GR metrics is encouraged for screens where cell proliferation rates may vary [2].
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for Robust Drug Screens
| Item | Function | Key Considerations |
|---|---|---|
| Resazurin Sodium Salt | A cell-permeable, blue dye reduced to pink, fluorescent resorufin in viable cells. Used as a viability indicator [2] [19]. | Prepare a 10% (w/v) stock solution in PBS. It is light-sensitive; store aliquots in the dark. Incubation time (2-4 hours) must be optimized. |
| Matched DMSO Vehicle Controls | Control wells containing the exact concentration of DMSO used in the corresponding drug test well. Corrects for solvent-specific cytotoxicity [2]. | Critical for accurate baseline (100% viability) measurement. Eliminates artifacts of variable DMSO concentration. |
| Sealed PCR Plates | For the short-term storage of diluted drug solutions. Superior seal to prevent evaporation compared to standard culture microplates [2]. | Use for storing drug working solutions at -20°C for no more than 48 hours. |
| Cell Line-Specific Growth Medium | Provides nutrients and factors for cell growth. The composition (e.g., serum content) can affect drug activity and cell health [2]. | Standardize the medium recipe and serum batch across experiments. Note that serum-free medium may enhance cytotoxicity for some drugs like Bortezomib [2]. |
| L-Cysteine hydrochloride hydrate | L-Cysteine Hydrochloride Monohydrate | High-purity L-Cysteine Hydrochloride Monohydrate for research. Used in food, feed, and plant studies. For Research Use Only. Not for human consumption. |
| Metoprolol | Metoprolol | High-purity Metoprolol, a selective β1-adrenergic receptor antagonist. For Research Use Only. Not for diagnostic, therapeutic, or personal use. |
Experimental Workflow and Variability Analysis
The following diagram illustrates the workflow for identifying and controlling major sources of variability in pharmacogenomic screens.
Workflow for Identifying Experimental Variability
The diagram below shows the relative impact of different factors on cell viability based on variance analysis.
Relative Impact of Variability Sources
The Global Challenge of Antibiotic Resistance and Its Implications for Sensitivity Testing
Frequently Asked Questions (FAQs)
Q1: What are the recognized standards for antibacterial susceptibility testing, and why are they critical for my research? The U.S. Food and Drug Administration (FDA) recognizes specific consensus standards to ensure the accuracy and reproducibility of susceptibility testing. The primary standard is the Clinical and Laboratory Standards Institute (CLSI) M100 document, "Performance Standards for Antimicrobial Susceptibility Testing," which is updated annually [20] [21]. These standards provide the official susceptibility test interpretive criteria (STIC), or "breakpoints," which are the minimum inhibitory concentration (MIC) values used to categorize bacterial isolates as susceptible, intermediate, or resistant to an antibacterial agent [20]. Adhering to these recognized standards is mandatory for generating clinically relevant data, ensuring consistency across laboratories, and satisfying regulatory requirements for drug development [21].
Q2: What is the difference between high-throughput screening (HTS) and high-content screening (HCS) in drug sensitivity testing? While both are automated screening methods, they serve different purposes:
- High-Throughput Screening (HTS) is optimized for speed, testing thousands of compounds in parallel, typically using a single readout (e.g., cell viability via luminescence) [22] [23].
- High-Content Screening (HCS), also known as high-content analysis (HCA), is slightly slower but provides a deeper, multi-parameter analysis of cellular phenotypes. It uses automated microscopy and image analysis to simultaneously assess multiple parameters, such as cell morphology, protein localization, and organelle function, in response to treatment [22] [23]. This makes HCS invaluable for understanding the complex mechanisms of drug action and resistance beyond simple cell death.
Q3: What are the primary mechanisms by which bacteria become resistant to antibiotics? Bacteria evolve through several mechanisms to evade antibiotics [24]:
- Intrinsic Resistance: Natural evolution leads to structural or functional changes, such as the absence of a drug's target (e.g., bacteria without cell walls are resistant to penicillin) [24].
- Acquired Resistance: Bacteria can become resistant through new genetic mutations or by acquiring resistance genes from other bacteria via horizontal gene transfer. This occurs through:
- Transformation: Uptake of naked DNA from the environment.
- Transduction: Transfer of DNA via bacteriophages (viruses that infect bacteria).
- Conjugation: Direct cell-to-cell transfer of genetic material [24]. These mechanisms can lead to specific resistance strategies, including neutralizing the antibiotic, pumping it out of the cell (efflux), or modifying the antibiotic's target site [24].
Troubleshooting Guides
Table 1: Common Cell Culture Issues in Drug Sensitivity Assays
| Problem | Potential Cause | Solution |
|---|---|---|
| High variability in IC50 values | Inconsistent culture conditions (pH, temperature), contamination, or low cell viability at seeding. | Standardize culture protocols; implement strict quality control for reagents; ensure >95% cell viability at the start of experiments [25]. |
| Unusual charge heterogeneity in recombinant protein products (e.g., mAbs) | Post-translational modifications (deamidation, oxidation) driven by suboptimal culture conditions like elevated pH or temperature [25]. | Systematically optimize culture parameters (pH, temperature, feed components) using Design of Experiments (DOE) or machine learning approaches [25]. |
| Failure to induce resistance in continuous culture models | Inconsistent or sub-inhibitory drug pressure, allowing unrestricted growth of non-resistant cells. | Use automated continuous-culture devices like a morbidostat, which dynamically adjusts drug concentration to maintain a constant selection pressure [26]. |
| Poor predictive value of ex vivo drug testing | Assays relying on a single metabolic readout (e.g., ATP-based viability) may miss complex phenotypes like therapy-induced senescence [23]. | Complement metabolic assays with high-content imaging to capture multi-parameter data, including morphology, apoptosis, and specific biomarker levels (e.g., c-Met) [27] [23]. |
Table 2: Interpreting Unexpected Results in Antimicrobial Susceptibility Testing
| Scenario | Investigation | Corrective Action |
|---|---|---|
| A known susceptible strain falls in the resistant category. | Check quality control (QC) ranges for the antibiotic and method. Verify that the latest CLSI M100 breakpoints are being used [21]. | Repeat the test with fresh QC strains. Confirm the drug concentration in the assay medium. Consult the current year's CLSI M100 standard for interpretive criteria [20] [21]. |
| No zone of inhibition is observed in disk diffusion. | Confirm the organism's identity and typical susceptibility profile. Check for contamination. Verify the drug is not expired. | Test for intrinsic resistance. Use an alternative, CLSI-recommended method (e.g., broth dilution) to determine the Minimum Inhibitory Concentration (MIC) [26]. |
| Discrepancy between genotypic and phenotypic resistance results. | The resistance gene may be present but not expressed, or resistance may be mediated by an unknown or novel mechanism [24]. | Use phenotypic results (MIC) to guide clinical interpretation. Further investigate with transcriptional analysis or enzymatic functional assays [28]. |
Key Experimental Protocols
Protocol 1: Broth Dilution for Minimum Inhibitory Concentration (MIC) Determination
The MIC is the lowest concentration of an antimicrobial agent that prevents visible growth of a microorganism [26].
Materials:
- Cation-adjusted Mueller-Hinton Broth (for most aerobic bacteria)
- Sterile 96-well microtiter plates
- Antibiotic stock solution of known concentration
- Bacterial inoculum, adjusted to ~5 x 10^5 CFU/mL
Method:
- Prepare Drug Dilutions: Serially dilute the antibiotic (typically two-fold dilutions) in broth across the microtiter plate.
- Inoculate: Add an equal volume of the standardized bacterial inoculum to each well. Include growth control (bacteria, no drug) and sterility control (broth only) wells.
- Incubate: Incubate the plate under appropriate conditions (e.g., 35±2°C for 16-20 hours for most bacteria).
- Read Results: The MIC is the lowest drug concentration that completely inhibits visible growth. Compare this value to the interpretive criteria in the CLSI M100 standard to categorize the isolate as Susceptible, Intermediate, or Resistant [26].
Protocol 2: High-Content Analysis for Ex Vivo Drug Sensitivity
This protocol is used for detailed phenotypic profiling of patient-derived cells in response to drug treatment [27] [23].
Materials:
- Patient-derived cells or relevant cell line
- Laminin-coated 384-well CellCarrier plates
- Drug library
- Fixative (e.g., 4% paraformaldehyde)
- Permeabilization buffer (e.g., 0.3% Triton X-100)
- Primary and fluorescently-labeled secondary antibodies
- Nuclear stain (e.g., Hoechst 33342)
- Automated fluorescence microscope (e.g., PerkinElmer Operetta CLS) and analysis software (e.g., Harmony)
Method:
- Cell Seeding: Seed cells onto the coated plate and allow to adhere.
- Drug Treatment: Treat cells with the drug library after 24 hours. Include DMSO vehicle controls.
- Staining and Fixation: After the desired incubation period, fix cells, permeabilize, and block. Incubate with primary antibodies (e.g., anti-c-Met, anti-phospho-c-Met) overnight, followed by fluorescent secondary antibodies and nuclear stain [27].
- Image Acquisition and Analysis: Acquire images using the high-content imaging system. Use the software to automatically quantify multi-parameter readouts such as specific biomarker levels, cell viability (nuclei count), apoptosis (caspase 3/7 activation), and cell motility [27] [23].
Visualizing Pathways and Workflows
Antibiotic Resistance Mechanisms
HCS Drug Sensitivity Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Advanced Drug Sensitivity Research
| Item | Function/Application | Example from Literature |
|---|---|---|
| CLSI M100 Standard | Provides the current, evidence-based breakpoints for interpreting susceptibility test results (MIC values) for aerobic bacteria [21]. | Used as the primary reference for determining if a bacterial isolate is Susceptible, Intermediate, or Resistant to an antibiotic [20] [21]. |
| c-Met Inhibitors (e.g., Cabozantinib, Crizotinib) | Small molecule inhibitors targeting the c-Met receptor tyrosine kinase, used in cancer drug sensitivity studies [27]. | Applied in high-content analysis to identify glioblastoma patients with elevated c-Met levels who may respond to targeted therapy [27]. |
| CDK4/6 Inhibitors (e.g., Abemaciclib) | Inhibitors of cyclin-dependent kinases 4 and 6, used to induce cell cycle arrest in cancer cells. | A drug repurposing screen identified Abemaciclib as having a distinct c-Met-inhibitory function, revealing a new potential application [27]. |
| Lysomotropic Agents & Senolytics (e.g., Fluoxetine, BCL2 inhibitors) | Agents that accumulate in and disrupt lysosomal function, or drugs that selectively eliminate senescent cells [23]. | Used to target cancer stress adaptation pathways, such as therapy-induced senescence, particularly in treatment-resistant mesenchymal neuroblastoma cells [23]. |
| Morbidostat Device | An automated continuous-culture device that dynamically adjusts antibiotic concentration to maintain constant selection pressure [26]. | Enables real-time study of bacterial evolution and the development of drug resistance under controlled, sustained inhibition [26]. |
| Glycerides, C14-26 | 1-Heptadecanoyl-rac-glycerol|MG(17:0)|CAS 5638-14-2 | Research-grade 1-Heptadecanoyl-rac-glycerol, a bioactive monoacylglycerol with demonstrated antimicrobial properties. For Research Use Only. Not for human use. |
| Hordenine | Hordenine, CAS:62493-39-4, MF:C10H15NO, MW:165.23 g/mol | Chemical Reagent |
Advanced Models and Protocols for Enhanced Physiological Relevance
The transition from two-dimensional (2D) to three-dimensional (3D) cell culture represents a paradigm shift in biomedical research. While 2D culture has been a fundamental method for decades, it fails to replicate the complex architecture and cellular interactions of human tissues [29]. In contrast, 3D models like spheroids and organoids mimic the in vivo microenvironment more accurately, leading to more physiologically relevant data for drug discovery and disease modeling [30] [31]. This technical resource center provides essential troubleshooting guidance and protocols to help researchers successfully implement 3D culture technologies.
Troubleshooting Guides & FAQs
Spheroid Formation Issues
Problem: My spheroids are irregularly shaped and lack compactness.
- Solution A: Ensure you are using an appropriate surface treatment. Ultra-low attachment (ULA) plates or poly-HEMA coated plates prevent cell adhesion and promote self-aggregation. Research shows ULA plates typically produce larger, more cohesive spheroids compared to poly-HEMA coatings [32].
- Solution B: Optimize seeding density. Too few cells may not form spheroids, while too many can cause necrotic cores. Test a range from 500-10,000 cells/well in 96- or 384-well formats.
- Solution C: For difficult-to-aggregate cell lines, add low concentrations of extracellular matrix (ECM) components. For instance, adding 2.5% Matrigel to PANC-1 pancreatic cancer cells promotes formation of denser, more uniform spheroids [31].
- Solution D: Centrifuge plates after seeding (300-500 × g for 5-10 minutes) to force cell-cell contact and initiate spheroid formation [31].
Problem: My spheroids show high variability in size and shape between wells.
- Solution A: Use standardized, commercially available U-bottom spheroid microplates rather than homemade coating methods to ensure well-to-well consistency [33].
- Solution B: Prepare single-cell suspensions thoroughly before seeding to avoid clumping.
- Solution C: Maintain consistent medium volume across all wells and minimize evaporation. For hanging drop methods, use humidification chambers with DI water in surrounding wells [34].
Drug Sensitivity Testing Challenges
Problem: Drug responses in my 3D models don't match published in vivo data.
- Solution A: Extend treatment duration. Drugs may require more time to penetrate the 3D structure. Standard 72-hour treatments are common, but some models may need 5-10 days [35] [31].
- Solution B: Account for penetration barriers. The compact architecture of spheroids creates diffusion gradients that limit drug penetration to the core. Consider testing nanocarrier-based delivery systems designed to improve penetration [31].
- Solution C: Verify that your model recapitulates key TME features. Incorporation of stromal cells (e.g., cancer-associated fibroblasts) can significantly alter drug responses, making them more physiologically relevant [31].
Problem: My 3D cultures show unexpectedly high drug resistance compared to 2D.
- Solution A: This may reflect biological reality rather than a technical issue. 3D models naturally develop chemoresistance due to:
- Presence of quiescent cells in the core
- Activation of cell adhesion-mediated drug resistance (CAM-DR)
- Development of hypoxia and acidity gradients
- Solution B: Characterize your model's proliferation gradients using markers like Ki-67, which typically shows higher proliferation in outer layers and quiescence in the core [31].
- Solution C: For cytotoxicity assays, use 3D-optimized ATP-based viability assays that include steps to disrupt spheroids for accurate quantitation [32] [34].
Imaging and Analysis Difficulties
Problem: I can't get clear images of my spheroid interiors.
- Solution A: Use tissue clearing reagents specifically designed for 3D cultures, such as Corning 3D Clear Tissue Clearing Reagent, which improves light penetration without altering morphology [33].
- Solution B: Select appropriate imaging modalities. Avoid standard confocal microscopy for thick samples; instead use light sheet microscopy which provides better penetration for spheroids >200-300μm [31].
- Solution C: Always include a nuclear stain (e.g., DAPI) to assess penetration quality and spheroid architecture [33].
- Solution D: For high-content screening, use U-bottom plates that position spheroids consistently in each well for automated imaging [33].
Problem: Quantitative analysis of 3D cultures is challenging.
- Solution A: Utilize automated image analysis systems (e.g., Incucyte) that can track spheroid growth and morphology over time [31].
- Solution B: For invasion assays, establish consistent quantification methods such as measuring the area of matrix degradation or counting invasive protrusions [32].
- Solution C: When using fluorescence, always subtract background signal from cell-free regions and maintain identical acquisition settings across conditions [32].
Culture Contamination and Viability Problems
Problem: My patient-derived organoids fail to establish or grow slowly.
- Solution A: Optimize matrix composition. Different cell types require specific ECM environments. Systematic testing of Matrigel concentrations (ranging from 50-100%) may be necessary [35] [30].
- Solution B: Use specialized medium formulations containing appropriate niche factors. Patient-derived cancer cells often require customized formulations different from standard cell lines [35] [30].
- Solution C: Process samples quickly after clinical collection—ideally within 1-3 weeks depending on tissue amount and growth rate [35].
Problem: My cultures become contaminated during handling.
- Solution A: For hanging drop platforms, implement thorough sterilization protocols including sonication, 0.1% Pluronic acid treatment for 24 hours, and UV sterilization [34].
- Solution B: Maintain strict humidification to prevent medium evaporation in hanging drops, which can concentrate toxins and stress cells [34].
Essential Methodologies
Workflow Overview:
Detailed Steps:
- Sample Processing: Obtain cancer tissue from surgery or biopsy and process into single-cell suspension using enzymatic digestion.
- Plating: Plate cells in 384-well plates containing Matrigel using automation-compatible methods. Cell density should be optimized for each cell type (typically 500-5,000 cells/well).
- Spheroid Formation: Culture for 3-10 days until compact spheroids form. Monitor growth using live-cell imaging systems.
- Drug Treatment: Add compounds of interest using automated dispensers. Include controls (DMSO vehicle) and reference drugs.
- Viability Assessment: After 72 hours of treatment, measure cell viability directly using luminescence-based assays (e.g., CellTiter-Glo 3D).
- Optional Imaging: Before viability measurement, perform high-content brightfield or fluorescence imaging for morphological analysis.
- Data Analysis: Normalize data to controls, calculate IC50 values, and perform quality control checks.
Timeline: The complete 3D-DSRT protocol typically takes 1-3 weeks from clinical sampling to results, depending on tissue amount, growth rate, and drug numbers.
Workflow Overview:
Detailed Steps:
- Plate Preparation:
- Sonicate hanging drop plates in sterile DI water for 20 minutes
- Wash with running DI water
- Soak in 0.1% Pluronic acid for 24 hours to prevent protein adsorption
- Rinse thoroughly and sterilize with UV light (30-60 minutes per side)
Humidification System:
- Fill 6-well plates with 4-5mL sterile DI water
- Sandwich hanging drop plate between lid and bottom
- Add 800-1000μL sterile DI water around the rim to minimize evaporation
Cell Seeding:
- Prepare single-cell suspensions in serum-free medium
- Seed appropriate cell numbers (typically 1,000-5,000 cells in 40-50μL drops)
- For patient-derived cells, use small cell numbers (as few as 100-500 cells/drop)
Spheroid Formation and Drug Testing:
- Culture for 3-5 days until compact spheroids form
- Add drugs directly to hanging drops
- Monitor morphology and viability over time
Research Reagent Solutions
Table: Essential Materials for 3D Cell Culture Applications
| Product Category | Specific Examples | Key Applications | Technical Notes |
|---|---|---|---|
| Extracellular Matrices | Corning Matrigel Matrix, Collagen I, BME | Organoid culture, Spheroid compaction | Matrigel (∼60% laminin, ∼30% collagen IV) doesn't fully replicate patient tumor ECM (∼90% collagen) [31] |
| Scaffold-Free Platforms | Ultra-Low Attachment (ULA) plates, Poly-HEMA coatings, Hanging drop plates | Simple spheroid formation, High-throughput screening | ULA plates produce larger, more cohesive spheroids than Poly-HEMA [32]; Hanging drops offer high compaction [34] |
| Specialized Media | Defined organoid media, Serum-free formulations | Patient-derived organoids, Cancer stem cell maintenance | Require specific growth factor cocktails; Often need customization for different cell types [30] |
| Analysis Reagents | Corning 3D Clear Tissue Clearing Reagent, ATP-based viability assays, Live-cell stains | 3D imaging, Viability assessment, Long-term monitoring | Tissue clearing enables imaging of spheroid interiors without sectioning [33]; ATP assays require spheroid disruption [32] |
| Cell Culture Supplements | Growth factors (EGF, FGF, Wnt-3A), Noggin, R-spondin | Organoid establishment and maintenance | Essential for stem cell maintenance and differentiation; Concentrations require optimization [30] |
Quantitative Comparison of 3D Culture Platforms
Table: Performance Characteristics of Different 3D Culture Methods
| Platform | Throughput | Cost | Reproducibility | Key Advantages | Documented Limitations |
|---|---|---|---|---|---|
| Hanging Drop | High (384-well) | Low | Moderate | Minimal ECM interference, Easy imaging | Evaporation issues, Manual handling challenging [34] |
| ULA Plates | High (96-/384-well) | Moderate | High | Standardized workflow, Automation compatible | Spheroid size varies by cell line [32] |
| Poly-HEMA | Moderate | Low | Moderate | Cost-effective alternative to ULA | Produces smaller, less cohesive spheroids [32] |
| Matrigel Embedding | Moderate | High | Moderate | Supports complex organoid growth | Batch variability, Complex drug diffusion [35] [31] |
| Hydrogel Systems | Low-Moderate | High | Variable | Tunable mechanical properties | Specialized equipment often needed [29] |
Advanced Applications and Future Directions
Patient-Derived Models for Personalized Medicine
The pharmaceutical industry is increasingly adopting patient-derived organoids (PDOs) for drug screening and personalized treatment selection [5]. These models maintain the genetic and pathological features of original diseased tissues, enabling:
- Patient-specific drug sensitivity testing: PDOs can be established from patient biopsies and used to identify effective treatments before clinical administration [35] [5].
- Biobanking for drug discovery: Collections of PDOs representing different disease subtypes support the development of targeted therapies [30].
- Clinical trial optimization: PDO platforms can help select patient populations most likely to respond to investigational drugs [5].
Integration with Advanced Technologies
Current research focuses on enhancing 3D models through technological integration:
- Microfluidic systems create more physiologically relevant nutrient and waste gradients while enabling real-time monitoring [29].
- Automated imaging and AI-based analysis platforms enable high-content screening of complex 3D structures [5] [33].
- CRISPR-based gene editing allows precise manipulation of organoids to study disease mechanisms and identify therapeutic targets [30] [5].
The successful transition from 2D to 3D cell culture requires careful consideration of platform selection, protocol optimization, and analytical method adaptation. By addressing the common challenges outlined in this technical resource center, researchers can leverage the full potential of spheroids and organoids to generate more physiologically relevant data for drug discovery and disease modeling. The field continues to evolve rapidly, with ongoing improvements in standardization, automation, and analytical capabilities promising to further enhance the utility of 3D models in biomedical research.
Implementing Patient-Derived Cancer Cells (PDCCs) for Personalized Therapeutic Screening
Frequently Asked Questions (FAQs)
FAQ 1: What are the most common reasons for low PDCC culture initiation success, and how can they be mitigated? Low culture initiation success is a major challenge. This can be due to an extremely low number of obtainable cancer cells, sample quality issues (e.g., low cellularity or massive necrosis), or spontaneous cell death in culture [36] [37]. Mitigation strategies include:
- Rigorous Sample Quality Control: Assess patient tissue for cellularity and necrosis before culture initiation; excluding poor-quality samples can increase success rates [37].
- Optimized Culture Conditions: Use of 3T3-J2 fibroblast feeder layers can support the efficient establishment and long-term stability of 2D PDCC lines from colorectal cancer [37]. For primary hematologic cancer cells, provide essential microenvironmental stimuli (e.g., feeder cells for CLL, or IL-2 and T-cell expansion cocktails for Multiple Myeloma) to prevent spontaneous apoptosis [38].
- Advanced 3D Culture Systems: Employing 3D culture methods like Gelfoam histoculture can facilitate cancer cell migration and growth, providing a more physiologically relevant environment that may improve initiation success [39].
FAQ 2: How can I prevent fibroblast overgrowth in my PDCC cultures? Fibroblast overgrowth is a common problem in standard 2D cultures on plastic or glass. A demonstrated solution is to use a 3D Gelfoam histoculture method. In this system, fragments of patient-derived xenograft (PDX) tumors are placed on Gelfoam, leading to cultures that are essentially all cancer cells without fibroblast contamination [39]. This method has proven effective for establishing PDCCs from colon cancer liver metastases.
FAQ 3: How well do PDCC models retain the original tumor's characteristics? When established with optimized methods, PDCCs can faithfully recapitulate the original tumor. 2D PDCC models have been shown to maintain the genomic landscape of parental tumors with high efficiency [37]. Furthermore, 3D models derived from these cells, such as Air-Liquid Interface (ALI) organotypic cultures, can retain the histological architecture and transcriptomic profiles of the original patient tumor [37]. This preservation of key characteristics is crucial for ensuring the clinical relevance of drug sensitivity testing.
FAQ 4: My drug sensitivity data is highly variable. How can I improve the reliability of my screening results? Variability can arise from technical and biological factors, including heterogeneity in organoid size and shape, or inconsistencies in cell viability [37].
- Standardize Protocols: Follow optimized, standardized drug sensitivity and resistance testing (DSRT) protocols tailored to your cancer type. This includes controlling for seeding density, drug exposure time (typically 72 hours), and using appropriate positive and negative controls on each plate to calculate a Z-prime factor for quality control [38].
- Incorporate Machine Learning: Machine learning (ML) approaches, particularly conformal prediction, can be applied to drug sensitivity prediction. This framework provides a mathematical guarantee of reliability, outputting prediction intervals that contain the true drug response value with a user-specified certainty, thus improving trust in the results for clinical decision-making [40].
FAQ 5: Which culture method (2D vs. 3D) is best for my personalized therapeutic screening? The choice depends on your specific research goals and the trade-offs between physiological relevance and practicality. The table below compares the primary methods:
Table 1: Comparison of Primary PDCC Culture Methods [36]
| Method | Key Advantages | Key Limitations | Best Use Cases |
|---|---|---|---|
| 2D Monolayers | - Simple, easy to manipulate and observe [36] [37]- High proliferation rate [37]- Suitable for large-scale drug screens [36] | - Lacks tumor microenvironment [36]- Loss of tumor heterogeneity and phenotype [36] [37]- Extremely inefficient to establish new lines with traditional methods [37] | - Initial high-throughput drug screening where throughput and cost are primary concerns. |
| 3D Tumor Spheroids | - Better recapitulates 3D architecture and cell-cell interactions than 2D [36] | - Heterogeneous in size and shape [37]- Can lack the complexity of the full tumor microenvironment [36] | - Studying basic tumor biology and drug penetration. |
| 3D Organoids | - Retains genetic and phenotypic heterogeneity of the tumor [36] [37]- Can model patient-specific histology [37] | - Culture success rate can be variable [36]- Rigid matrix (e.g., Matrigel) may limit drug penetration [37]- Heterogeneity in organoid viability [37] | - High-fidelity drug testing and personalized therapy prediction when culture can be established. |
| Gelfoam 3D Histoculture | - Effectively eliminates fibroblast overgrowth [39]- Allows for indefinite passaging potential [39] | - Requires prior establishment of a Patient-Derived Xenograft (PDX) model [39] | - Generating pure cancer cell cultures for specific tumor types where PDX models are available. |
Troubleshooting Guides
Issue 1: Poor Cell Viability in Primary Cultures
Problem: Primary cancer cells die shortly after being placed in culture. Solutions:
- For Hematologic Cancers:
- CLL: Transiently co-culture primary CLL cells with feeder cells prior to drug exposure to prevent spontaneous apoptosis [38].
- Multiple Myeloma: Isolate CD138+ cells and activate them with autologous bone marrow T helper cells in the presence of IL-2 and a T-cell expansion cocktail (anti-CD3/CD28 beads) prior to drug screening [38].
- General Best Practices:
- Use High-Quality Samples: Process fresh tissues quickly or use properly biobanked samples. Note that biobanked samples may have lower baseline viability [38].
- Control Culture Environment: Always include positive (e.g., 100 µM benzethonium chloride) and negative (e.g., 0.1% DMSO) controls on every drug plate to monitor for non-drug induced cell death [38].
Issue 2: Inconsistent Drug Response Readings in Screening Assays
Problem: High variability between replicates in drug sensitivity screens. Solutions:
- Standardize Cell Preparation:
- Use a single-cell suspension by filtering the cells through a 40µm strainer [38].
- For cell lines, screen cells directly after thawing (if viability permits) to reduce variability from long-term culture adaptations. Alternatively, ensure cells are in a consistent growth phase [38].
- Carefully optimize the cell seeding density for each well format to avoid over-confluence or overly sparse wells at the experimental endpoint [38].
- Assay Protocol Rigor:
- Equilibrate assay plates and reagents (e.g., CellTiter-Glo) to room temperature before adding to cells to ensure consistent signal development [38].
- Use a liquid dispenser for uniform cell seeding and reagent addition. Sonicate the dispenser's valves before use to prevent clogging and ensure accuracy [38].
- Cover plates with gas-permeable membranes to limit evaporation during incubation [38].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for PDCC Culture and Screening
| Item | Function / Application | Example / Notes |
|---|---|---|
| 3T3-J2 Fibroblasts | Acts as a feeder layer to support the establishment and growth of 2D PDCC lines from certain cancer types, like colorectal cancer [37]. | Irradiated before use to prevent proliferation [37]. |
| Gelfoam | A scaffold for 3D histoculture that promotes cancer cell growth and migration while suppressing fibroblast overgrowth [39]. | Used for culturing PDX-derived tumor fragments [39]. |
| Matrigel / BME | Basement membrane extract used as a scaffold for 3D organoid culture, providing a more in vivo-like environment [36] [37]. | The relatively rigid matrix may sometimes limit drug penetration in screens [37]. |
| CellTiter-Glo Assay | A luminescent assay to quantify cell viability based on ATP content; commonly used as an endpoint in drug sensitivity screens [38]. | Used for 384-well plate formats; requires luminescence-compatible plates [38]. |
| Air-Liquid Interface (ALI) System | A transwell-based culture system that allows 2D-expanded PDCCs to form 3D organotypic structures that recapitulate original tumor histology [37]. | Useful for creating more physiologically relevant models for validation. |
| Drug Libraries | Collections of compounds used for high-throughput screening to identify patient-specific sensitivities [38]. | Design should be tailored to the cancer type and research question (e.g., targeted therapies, chemotherapies). |
| Nonanoic Acid | Nonanoic Acid, CAS:68937-75-7, MF:C9H18O2, MW:158.24 g/mol | Chemical Reagent |
| Senna | Senna, CAS:85085-71-8, MF:C42H38O20, MW:862.7 g/mol | Chemical Reagent |
Experimental Workflows and Data Reliability
The following diagram illustrates a complete workflow for establishing PDCCs and performing reliable drug sensitivity prediction, incorporating machine learning to enhance result trustworthiness.
The diagram below outlines the critical steps for processing different types of hematologic cancer samples to ensure their survival and accurate representation in drug sensitivity assays.
Step-by-Step Protocol for Reliable Drug Dose-Response Measurements
Accurate dose-response measurements are fundamental to drug discovery and development, providing critical parameters such as EC50 and IC50 that quantify compound potency. Within the broader context of optimizing cell culture conditions for drug sensitivity research, the reliability of these results is heavily dependent on a robust experimental protocol, proper data normalization, and systematic troubleshooting. This guide provides detailed methodologies and solutions for common issues encountered during dose-response experiments.
Experimental Protocol and Workflow
A standardized workflow is essential for generating reliable and reproducible dose-response data. The following steps outline the key phases of the experiment.
Step 1: Experimental Design and Dose Preparation
- Number and Range of Concentrations: It is recommended to use 5-10 concentrations distributed over a broad range to adequately define the bottom plateau, top plateau, and central linear portion of the curve [41]. Using too few concentrations may result in an incomplete curve and poor parameter estimation.
- Dose Spacing: Apply logarithmic spacing (e.g., 1, 10, 100, 1000 nM) rather than linear spacing. This provides better visualization of the sigmoidal curve shape and equal data point distribution on a log axis [41].
- Controls are Critical: Each experiment must include both positive controls (e.g., maximum effect or full inhibition) and negative controls (e.g., baseline or no inhibition) for subsequent data normalization [42].
Step 2: Cell Seeding and Compound Treatment
- Cell Seeding Density: Adhere to the recommended initial seeding density for your specific cell line. Tumor lines are often initiated at 2-4 x 10ⶠviable cells per 25 cm², while contact-inhibited lines may require lower densities around 5 x 10³ viable cells/cm² [43]. Conduct a growth curve to determine the optimal density if this information is not available.
- Cell Health and Passage Number: Use low-passage cells, as high passage numbers can lead to phenotypic and genotypic changes (genetic drift) that alter transfection efficiency and other biological responses, potentially compromising data reproducibility [43].
- Treatment Application: Apply compounds to cells after allowing for cell attachment. Ensure consistent incubation conditions (temperature, COâ‚‚, humidity) throughout the experiment.
Step 3: Data Collection and Normalization
- Response Measurement: Measure the endpoint response (e.g., cell viability, fluorescence, enzymatic activity) according to your assay protocol.
- Data Normalization: Normalize raw data to controls to account for plate-to-plate variation and express results in a standardized form [42].
- % Inhibition = [(Negative Control - Test Value) / (Negative Control - Positive Control)] × 100
- % Activation = [(Test Value - Negative Control) / (Positive Control - Negative Control)] × 100
- Normalization transforms the Y-values to a range between 0% and 100%, which facilitates comparison of results (EC50/IC50) across different experiments [41].
Step 4: Curve Fitting and Data Analysis
Four-Parameter Logistic (4PL) Model: Fit the normalized data (log(concentration) vs. response) using the 4PL model, also known as the Hill Equation [41] [42]. The model is defined as:
Y = Bottom + (Top - Bottom) / (1 + 10^((LogEC50 - X) * HillSlope))
Where:
- X is the log of concentration.
- Y is the response.
- Bottom is the minimum response asymptote (baseline).
- Top is the maximum response asymptote (maximum effect).
- HillSlope describes the steepness of the curve.
- LogEC50/LogIC50 is the log of the concentration that gives a response halfway between Bottom and Top.
Potency Metrics:
- EC50: The concentration that produces 50% of the maximal stimulatory response.
- IC50: The concentration that produces 50% inhibition.
- Relative vs. Absolute IC50: The relative IC50 is derived from the 4PL model fit and is the standard for dose-response analysis. The absolute IC50 is the point where the response is 50% inhibited, ignoring plateaus, and is less commonly used [41].
Troubleshooting Common Dose-Response Issues
FAQ 1: Why is there no assay window (no difference between positive and negative controls)?
- Instrument Setup: The most common reason for a complete lack of assay window is an improperly configured instrument. For TR-FRET assays, using incorrect emission filters will prevent signal detection. Always consult instrument setup guides and verify the setup with control reagents before running your assay [44].
- Reagent and Development Check: In enzymatic assays (e.g., Z'-LYTE), test the development reaction by ensuring the 100% phosphopeptide control is not exposed to development reagents (giving the lowest ratio) and the 0% phosphopeptide (substrate) is over-exposed to development reagents (giving the highest ratio). A properly functioning assay should show a significant difference (e.g., 10-fold) in the ratio between these controls [44].
- Cell Viability: If using a cell-based assay, confirm that your cells are healthy and have been seeded at the correct density. Poor cell health or incorrect density can obliterate the expected signal range [43].
FAQ 2: Why is the EC50/IC50 value inconsistent between experiments or labs?
- Compound Stock Solutions: The primary reason for differing EC50/IC50 values between labs is often variations in the preparation of stock solutions. Ensure accurate weighing, complete solubilization, and proper storage of compounds. Use standardized protocols for stock solution preparation across all experiments [44].
- Cell Culture Conditions: Phenotypic changes in cells due to high passage number ("genetic drift") can alter their response to compounds [43]. Use low-passage cells and maintain consistent culture conditions (medium, serum, passage procedure) to improve reproducibility.
- Assay Performance: Always monitor the Z'-factor, a key metric that assesses assay robustness by considering both the assay window and the data variation (standard deviation). An assay with a Z'-factor > 0.5 is considered suitable for screening. A large window with high noise can be less reliable than a smaller window with low noise [44].
FAQ 3: Why is the dose-response curve not sigmoidal, or why is the fit poor?
- Insufficient Data Points: The curve may be incomplete if you have too few concentrations defining the upper and lower plateaus. Ensure you have at least 2-3 data points defining each plateau [41].
- Incorrect Parameter Constraints: During curve fitting, the software may be over- or under-estimating the Top or Bottom plateaus. Visually inspect the fit. If the plateaus are unreasonable, consider constraining the Top and Bottom parameters based on the control values to improve the fit [41] [42].
- Outliers: Do not exclude outliers without investigation. If a data point is genuinely anomalous due to a pipetting error or bubble, it may be excluded. However, systematic outliers might indicate a problem with a specific concentration [41].
- Hill Slope: A very steep or shallow slope can sometimes be stabilized by constraining the Hill Slope to a reasonable value (e.g., 1.0) if you have a low number of observations [41].
FAQ 4: Why is the data too noisy or highly variable?
- Liquid Handling: Inconsistent pipetting during serial dilution or cell seeding is a major source of variation. Check pipette calibration and technique. Using an electronic multichannel pipette for critical steps can improve reproducibility.
- Cell Seeding Density: Inconsistent cell seeding leads to variable responses. Ensure cells are in a single-cell suspension and seeded uniformly across the plate. Using an automated cell counter can improve accuracy [43].
- Edge Effects: Evaporation in outer wells of a microplate can cause uneven results. Consider using a skirted or sealed plate, or incubating in a humidified chamber to minimize evaporation.
Key Reagents and Materials for Dose-Response Experiments
Table: Essential research reagent solutions for dose-response assays.
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Cell Lines | Biological system for testing compound effect | Use low-passage stocks; authenticate regularly; choose 2D vs. 3D models based on research goals [43] [45]. |
| Cell Culture Medium | Provides nutrients for cell growth and maintenance | Use consistent formulation and serum batches; pre-warm before use to maintain cell health [43] [45]. |
| Test Compound | The drug or molecule being tested | Ensure stock solution accuracy and stability; use high-purity DMSO if needed, keeping final concentration low (<0.1-1%). |
| Assay Detection Kit | Measures cellular response (viability, apoptosis, etc.) | Choose a validated, robust kit with a high Z'-factor; protect light-sensitive reagents [44]. |
| Positive/Negative Controls | Reference points for data normalization | Crucial for defining assay window and normalizing data (e.g., no compound vs. saturating compound) [42]. |
| Microplates | Vessel for cell culture and treatment | Choose surface treatment (e.g., TC-treated) for adherent cells; use plates suited to readout (e.g., white for luminescence). |
Advanced Considerations for Data Quality
Assessing Assay Quality with Z'-Factor: The Z'-factor is a critical metric for evaluating the quality and robustness of a screening assay [44]. It is calculated as follows:
Z' = 1 - [ (3σpositive + 3σnegative) / |μpositive - μnegative| ]
- σpositive, σnegative = standard deviations of the positive and negative controls.
- μpositive, μnegative = means of the positive and negative controls.
- A Z'-factor > 0.5 indicates an excellent assay suitable for screening. A lower Z'-factor suggests high variability or a small assay window, which will lead to less reliable IC50/EC50 values [44].
Optimizing Experimental Design (D-Optimality): For advanced screening, statistical optimal design theory can be applied to minimize the number of required measurements. A D-optimal design for a 4-parameter dose-response model often requires only the control plus three optimally chosen dose levels, which maximizes the precision of the parameter estimates for a given total number of data points [46]. This is particularly useful for resource-intensive experiments.
High-Throughput Screening (HTS) is a foundational methodology in modern drug discovery, enabling researchers to rapidly test thousands of chemical compounds or biological agents for activity against therapeutic targets. When optimized for drug sensitivity testing, particularly in cancer research, HTS provides invaluable insights into tumor biology and potential treatment options. This technical support center addresses the most common challenges researchers face when implementing HTS workflows, with particular emphasis on automation strategies that enhance reproducibility, reduce variability, and improve data quality in cell culture-based screening. The following troubleshooting guides and FAQs draw upon current best practices and technological advancements to support your research objectives.
FAQ: Workflow Design and Automation
What are the primary sources of variability in HTS workflows, and how can they be minimized?
Manual processes in HTS are significant sources of inter- and intra-user variability, which can lead to dramatic discrepancies in results. One study found over 70% of researchers reported being unable to reproduce others' work, largely due to this lack of standardization [47]. Human error in manual pipetting and reagent handling further compounds these inconsistencies, often going undocumented and complicating troubleshooting. Automation addresses these challenges through standardized workflows, with advanced systems offering verification features like DropDetection technology that confirms correct liquid dispensing volumes, allowing errors to be identified and corrected systematically [47].
How does automation specifically enhance HTS data quality and reproducibility?
Automated systems significantly improve assay performance by standardizing workflows across users, assays, and laboratory sites [47]. This standardization directly enhances data quality and reproducibility. Beyond consistency, automation delivers substantial practical benefits: it enables comprehensive screening of large compound libraries at multiple concentrations, generates richer datasets, increases throughput for troubleshooting scenarios where many conditions must be tested, and provides flexibility to adapt protocols as project needs evolve [47]. Additionally, automation facilitates miniaturization, reducing reagent consumption and overall costs by up to 90%, making comprehensive analyses feasible even with limited samples [47].
What considerations are most important when implementing automation in existing HTS workflows?
Successful automation integration requires careful planning. Begin by assessing current workflows to identify bottlenecks and labor-intensive tasks that would benefit most from automation, such as liquid handling, compound dilutions, and data analysis [47]. When selecting equipment, consider your lab's specific requirements for scale and workflow flexibility. For example, non-contact dispensers excel at high precision with low volumes, while robotic arms and integrated systems better handle larger-scale screening with multiple plates [47]. Also evaluate technical support availability, ease of use, and software integration capabilities to ensure a smooth transition. The overarching goal is to free researchers from repetitive tasks to focus on analysis and experimental design [48].
How do 2D and 3D cell culture systems differ in HTS applications, and when should each be used?
The choice between 2D and 3D culture systems depends on your research objectives and the biological questions being addressed. Two-dimensional systems (using multiwell microplates, microarrays, or microfluidics) enable cells to interact with their environment on a single plane, making them ideal for situations requiring precise control of multifactorial culture conditions to systematically determine the specific contributions of individual factors [49]. These systems are particularly valuable for toxicity and compound screening where many conditions need comparison with low variability [49].
In contrast, three-dimensional systems (including multiwell microplates, micromolds, microwells, and cell-encapsulated microgels) provide spatial complexity that better replicates the three-dimensional nature of tissue in vivo [49]. These models more accurately recapitulate the tissue microenvironment, including structural support, biochemical and biophysical cues, and cell-cell interactions relevant to disease states [49]. The industry is increasingly adopting automated 3D culture platforms that standardize processes like organoid seeding, media exchange, and quality control to improve reproducibility while reducing reliance on animal models [48].
Table 1: Comparison of 2D vs. 3D Cell Culture Systems for HTS
| Feature | 2D Systems | 3D Systems |
|---|---|---|
| Complexity | Single-plane cell environment | Spatial complexity mimicking in vivo conditions |
| Throughput | Very high (96- to 1536-well plates) | High (6- to 96-well formats with automation) |
| Physiological Relevance | Limited | Higher, better recapitulates tissue microenvironment |
| Primary Applications | Toxicity screening, compound screening | Disease modeling, predictive toxicology, personalized medicine |
| Automation Compatibility | Excellent, well-established | Improving with specialized platforms (e.g., MO:BOT) |
What are the critical steps for validating HTS assays to ensure reliable results?
HTS assay validation is essential for generating biologically and pharmacologically relevant data. The validation requirements depend on the assay's history and context [50]. For new assays, full validation includes stability studies and a 3-day plate uniformity assessment. When transferring previously validated assays to new laboratories, a 2-day plate uniformity study plus a replicate-experiment study are required [50]. Stability studies should determine reagent stability under both storage and assay conditions, establish DMSO compatibility (typically keeping final concentration under 1% for cell-based assays), and define reaction stability over the projected assay time [50]. Plate uniformity assessments use "Max," "Min," and "Mid" signals in an interleaved format across multiple days to establish adequate signal separation and consistent performance [50].
Troubleshooting Common HTS Challenges
Problem: High Variability Between Experimental Replicates
Potential Causes and Solutions:
- Liquid handling inconsistency: Implement automated liquid handling systems with verification features. Non-contact dispensers can improve precision, especially at low volumes [47].
- Unstable reagent conditions: Conduct thorough reagent stability studies under both storage and assay conditions. Determine stability after multiple freeze-thaw cycles if applicable, and establish appropriate storage aliquots [50].
- Inadequate environmental control: Use plate membranes that limit evaporation while allowing gas exchange, particularly for longer incubations [38].
- Cell culture inconsistencies: For primary cells, optimize culture conditions to maintain viability. For example, primary CLL cells may require transient co-culture with feeder cells, while multiple myeloma cells benefit from activation with autologous BM T helper cells prior to drug screening [38].
Problem: Poor Data Quality in Screening Results
Potential Causes and Solutions:
- Insufficient assay validation: Implement comprehensive plate uniformity studies over multiple days using Max, Min, and Mid signals to ensure adequate signal window for detecting active compounds [50].
- Inadequate quality controls: Include positive controls (e.g., 100 µM benzethonium chloride) and negative controls (e.g., 0.1% DMSO) on each drug plate to calculate Z-prime factors and validate assay performance [38].
- Edge effects in microplates: Use plate membranes to minimize evaporation, and validate thermal uniformity across the entire plate incubator [38].
- Cell seeding density issues: Pre-establish optimal cell densities by studying growth curves over time using live-cell imaging platforms to select confluency that supports optimal growth without inhibition at the experimental endpoint [38].
Problem: Inefficient Workflow Integration
Potential Causes and Solutions:
- Poor technology interoperability: Select automation tools with integration capabilities. Some liquid handlers are specifically designed for incorporation into automated work cells, maximizing efficiency and reproducibility [47].
- Fragmented data management: Implement unified data platforms that connect instruments and processes. Structured metadata and traceability are essential for AI applications, requiring capture of every condition and state rather than just results [48].
- Resistance to technology adoption: Choose systems designed with ergonomics and usability in mind. Features like lighter frames, shorter travel distances, and intuitive controls encourage adoption and reduce operator strain [48].
Table 2: HTS Automation Benefits and Implementation Considerations
| Benefit | Impact Level | Key Implementation Factors |
|---|---|---|
| Enhanced Reproducibility | High | Standardized workflows reduce user variability |
| Increased Throughput | High | Enables screening of large compound libraries at multiple concentrations |
| Cost Reduction | Medium-High | Miniaturization reduces reagent consumption by up to 90% |
| Data Quality Improvement | High | Integrated verification features (e.g., drop detection) |
| Scalability | Medium | Flexible platforms adapt to changing project needs |
Essential Protocols for Drug Sensitivity Testing
Protocol 1: Drug Sensitivity and Resistance Testing (DSRT) for Cell Lines
This protocol is adapted from established methods for hematologic cancer cell lines but can be adapted for other cell types [38].
Day 1: Preparation of Cells
- For adherent cells, bring into suspension via trypsinization. Collect cells in a 50 mL tube and centrifuge at 300 g for 5 minutes at room temperature.
- Discard supernatant and resuspend in fresh, pre-warmed medium.
- Filter cell suspension using a 40 µm cell strainer to ensure single-cell suspension.
- Count cells using preferred method (hemocytometer or automated cell counter).
- Resuspend cells in medium at optimal density determined from prior growth curve analysis.
Day 1: Drug Sensitivity Testing
- Transfer cell suspension to pre-printed drug plates at appropriate volume (25 µL/well for 384-well plates) using a liquid dispenser.
- Optional: Cover plates with membranes that allow gas exchange but limit evaporation.
- Incubate plates at 5% CO₂, 37°C for predetermined time (typically 72 hours).
Day 4: Viability Measurement with CellTiter-Glo
- Equilibrate CellTiter-Glo reagent and assay plates at room temperature for 15-30 minutes.
- Add 25 µL pre-filtered CellTiter-Glo to each well in 384-well plates.
- Measure luminescence with a luminometer.
Protocol 2: Plate Uniformity Assessment for HTS Assay Validation
This protocol is essential for validating new HTS assays or transferring established assays to new laboratories [50].
Procedure:
- Prepare plates using an interleaved-signal format with "Max," "Min," and "Mid" signals distributed across each plate according to a standardized pattern.
- Use the same plate formats on all days of the test, maintaining consistent concentrations for midpoint signals throughout.
- Use independently prepared reagents for each trial, preferably running on separate days.
- For "Max" signal: Use maximum signal determined by assay design (e.g., untreated control for inhibition assays).
- For "Min" signal: Use background signal (e.g., fully inhibited reaction for inhibition assays).
- For "Mid" signal: Use intermediate signal (e.g., IC50 concentration of a standard inhibitor for inhibition assays).
- Analyze data using appropriate statistical templates for 96- or 384-well plates to determine Z-prime factors and signal variability.
Research Reagent Solutions
Table 3: Essential Materials for HTS Drug Sensitivity Testing
| Reagent/Material | Function | Application Notes |
|---|---|---|
| CellTiter-Glo | Measures cell viability via ATP quantification | Luminescent readout; compatible with 384-well formats [38] |
| DMSO | Solvent for test compounds | Final concentration should typically be kept below 1% for cell-based assays [50] |
| Pre-printed drug plates | Pre-formatted compound libraries | Enable standardized screening across experiments |
| 40 µm cell strainer | Ensures single-cell suspension | Critical for uniform cell seeding and reproducible results [38] |
| Plate membranes | Limit evaporation while allowing gas exchange | Particularly important for longer incubations [38] |
| Liquid handling verification tools | Confirm dispensing accuracy | Technologies like DropDetection identify and document dispensing errors [47] |
Workflow Visualization
HTS Experimental Workflow
Automation Implementation Strategy
Integrating Microfluidic Platforms and Co-Culture Systems for Complex Microenvironments
Troubleshooting Guide: Common Experimental Issues and Solutions
This guide addresses frequent challenges encountered when integrating microfluidic platforms with co-culture systems for drug sensitivity testing.
Troubleshooting Table
| Problem Category | Specific Symptom | Possible Cause | Recommended Solution |
|---|---|---|---|
| Cell Viability | Rapid cell death in specific chamber zones | Nutrient/waste gradient formation; excessive shear stress | Optimize flow rate to ensure uniform perfusion; validate shear stress parameters for specific cell types [51] |
| Generalized poor viability across device | Material cytotoxicity; evaporation from reservoirs | Test material biocompatibility; use humidified chambers or oil overlays to minimize evaporation [52] | |
| Device Operation | Droplet actuation failure in DMF | Biofouling on electrodes; insufficient actuation voltage | Incorporate anti-fouling coatings; verify voltage settings and hydrophobic layer integrity [52] |
| Unintended sedimentation of suspended cells | Low flow rates; gravitational settling in chambers | Implement gravity-driven tilting (±85°) for continuous resuspension [51] | |
| Bubble formation and trapping | Priming issues; outgassing from media | Degas media before use; design channel geometries with venting features [53] | |
| Biological Fidelity | Lack of expected cell-cell interactions | Physical barriers prevent paracrine signaling; incorrect cell ratio | Use porous membranes or micro-patterned hydrogels to allow soluble factor exchange; optimize seeding densities [51] [54] |
| Loss of tissue-specific function in 3D models | Inadequate ECM support; suboptimal dynamic conditioning | Utilize decellularized ECM hydrogels; apply physiologically relevant mechanical stimuli (e.g., cyclic strain, flow) [54] | |
| Analysis & Sensing | High background noise in on-chip sensors | Protein adsorption; non-specific binding | Implement surface passivation (e.g., BSA, Pluronic); include appropriate controls [55] |
| Inconsistent results between technical replicates | Device-to-device fabrication variance; manual handling errors | Adopt mass fabrication (hot embossing, injection molding); automate fluid handling where possible [56] [53] |
Frequently Asked Questions (FAQs)
Q1: What are the fundamental advantages of using microfluidics for co-culture and drug screening over traditional well plates?
Microfluidic co-culture systems provide superior control over the cellular microenvironment. They enable the generation of stable biochemical gradients, application of physiological fluid shear stress, and precise spatial patterning of different cell types. This allows for the creation of more physiologically relevant tissue-tissue interfaces and the study of directed cell migration, which is impossible in static well-plate cultures [51] [57]. Furthermore, they facilitate high-throughput, automated screening with minimal reagent consumption, making them ideal for lengthy drug testing campaigns [53].
Q2: How many cells are typically required for seeding in a droplet-based digital microfluidic (DMF) system, and what are the limits?
In Digital Microfluidics (DMF), cell handling is typically done using sub-microliter volume droplets. A common constraint is that each droplet can usually accommodate a maximum of approximately 500 to 1000 cells [52]. This limited capacity can be a challenge for assays that require pooling cells for downstream analysis, such as qPCR or ELISA. Experimental planning must ensure that cell numbers remain within this functional range for the specific DMF platform being used.
Q3: Our team is new to microfluidics. What is the best way to start prototyping without a cleanroom?
Multiple accessible options exist for cleanroom-free prototyping. You can use commercial prototyping kits like the POC Kit. For device design, free online platforms such as FLUI'DEVICE allow you to design and simulate chips without needing CAD expertise. Furthermore, 3D printing has become a widely used method for rapidly creating custom device geometries [56].
Q4: What key factors should we consider when selecting a material for our microfluidic chip?
Material choice is critical and depends on your application:
- PDMS: Excellent for prototyping, gas-permeable (good for cells), and optically clear. However, it can absorb small hydrophobic molecules and drugs, potentially skewing assay results.
- Thermoplastics (e.g., Flexdym, PMMA): Ideal for mass production, offer better chemical resistance, and reduce small molecule absorption. Their fabrication often requires specialized industrial equipment [56].
- Glass: Provides the best optical clarity and is chemically inert, but is more brittle and can be more difficult to fabricate. Always prioritize biocompatibility and chemical resistance to your assay reagents [56] [52].
Experimental Protocol: Establishing a Gravity-Driven Co-culture Platform
This protocol is adapted from the "human immune flow (hiFlow) chip" platform for co-culturing suspended cells with 3D microtissues [51].
Objectives and Applications
This method establishes a long-term (up to 6+ days), perfused co-culture of suspension cells (e.g., immune cells, circulating tumor cells) with 3D microtissues (e.g., tumor spheroids, organoids). It prevents unwanted sedimentation of suspended cells and enables real-time, high-resolution monitoring of cell-tissue interactions, making it highly suitable for pre-clinical evaluation of immunotherapies [51].
Materials and Reagents
- hiFlow Chip: A microscope-slide-sized chip featuring two independent microfluidic networks, each with medium reservoirs, a hexagonal cell-microtissue interaction chamber, and meandering channels [51].
- Programmable Tilting Module: A device capable of tilting the chip through a large angle (e.g., ±85°) at a defined frequency.
- Cell Culture Medium: Appropriate for the specific cells and tissues used.
- Suspension Cells: e.g., Primary Peripheral Blood Mononuclear Cells (PBMCs).
- 3D Microtissues (MTs): Pre-formed spheroids or organoids.
- Pipettes and Sterile Tips.
Step-by-Step Procedure
Device Preparation and Priming
- Place the sterile hiFlow chip on the stage of the tilting module inside a biosafety cabinet.
- Slowly pipette the complete cell culture medium into the inlet reservoirs of the microfluidic network, ensuring that the medium flows through and fills all channels and the central interaction chamber without introducing air bubbles.
- Confirm that the medium reaches the outlet reservoir, indicating a fully primed network.
Loading of Microtissues
- Using a pipette with a wide-bore tip to prevent shear damage, carefully aspirate the pre-formed microtissues in a small volume of medium (e.g., 10-20 µL).
- Gently dispense the microtissues directly into the hexagonal interaction chamber of the primed device. The design of the chamber includes seven specific compartments to hold the microtissues in place.
- Allow the microtissues to settle into their compartments for a few minutes.
Introducing Suspension Cells
- Prepare a concentrated suspension of your cells (e.g., PBMCs) at the desired density in culture medium.
- Add the cell suspension to one of the medium reservoirs. The total volume in the reservoir should be approximately 250 µL [51].
- Ensure the final cell-to-medium ratio is appropriate for your assay to enable effective cell-tissue communication.
System Operation and Monitoring
- Initiate the tilting program on the module. A typical operation involves tilting the chip back and forth by ±85° with a cycle time tailored to achieve the desired flow rate and resuspension efficiency.
- Place the entire setup (tilting module with chip) into a cell culture incubator (37°C, 5% CO₂) for long-term culture.
- Monitor the co-culture daily using an inverted microscope. The chip's design provides unhindered optical access for high-resolution, real-time imaging of cell-tissue interactions.
Data Analysis and Interpretation
- In-situ Analysis: Use time-lapse microscopy to quantify dynamic processes such as immune cell attachment to microtissues, tumor cell invasion, or changes in microtissue morphology over time.
- Endpoint Analysis: After the experiment, the open design of the hiFlow chip allows you to easily retrieve microtissues and suspension cells from the device for off-chip analysis, such as flow cytometry, RNA sequencing, or immunohistochemistry [51].
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function in the Experiment | Specific Example / Note |
|---|---|---|
| Extracellular Matrix (ECM) Hydrogel | Provides a 3D scaffold to support organoid and spheroid growth, mimicking the native tissue microenvironment. | Matrigel is common; synthetic or decellularized tissue-derived hydrogels (e.g., from brain or intestine) offer more defined composition [54] [53]. |
| Primary Cells & Organoids | Biologically relevant models for drug sensitivity testing, preserving patient-specific genetics and tumor heterogeneity. | Patient-derived pancreatic tumor organoids [53]. |
| Digital Microfluidic (DMF) Chip | Enables automated, pump-less manipulation of picoliter to microliter droplet volumes for assay automation. | Comprises glass with electrode arrays, a dielectric layer (e.g., Parylene C), and a hydrophobic coating (e.g., Teflon AF) [52]. |
| Programmable Tilting Module | Generates gravity-driven, bi-directional flow by creating hydrostatic pressure differences, preventing cell sedimentation. | Allows for tilting angles up to ±85° to keep suspension cells in circulation [51]. |
| Anti-biofouling Coatings | Prevents non-specific adhesion of proteins and cells to microchannel surfaces, maintaining consistent flow and reducing background. | Teflon AF, Cytop, or FluoroPel are used as hydrophobic coatings in DMF [52]. |
| Curcumin | Curcumin | High-purity Curcumin for research applications. Explore its multi-target mechanisms in inflammation, cancer, and oxidative stress studies. For Research Use Only. |
Experimental Workflow Diagram
Solving Common Problems: A Practical Guide to Assay Optimization
Strategic Optimization of Cell Seeding Density for Uniform Growth
Frequently Asked Questions
What are the consequences of seeding cells at an incorrect density? Incorrect seeding density can significantly impact your experimental outcomes. If the density is too high, it can lead to rapid nutrient depletion, accumulation of waste products (like lactic acid), and contact inhibition in adherent cultures, causing cells to stop growing or deteriorate [58] [59]. If the density is too low, cells may experience insufficient cell-to-cell interactions, slowed growth, and poor viability, which can skew results from assays measuring cell growth or drug response [59].
How can I improve the uniformity of cell seeding in multi-well plates? Non-uniform seeding, often observed as higher density at the edges of a plate (the "edge effect"), is a common source of variability [2] [60]. To improve uniformity:
- Use Automated Liquid Handlers: Robotic systems can dispense cells with high precision and consistency, reducing human error and variability between wells [59].
- Monitor with Imaging: Employ image cytometers to perform whole-well imaging immediately after seeding to check and ensure confluence is consistent across the entire plate [60].
- Ensure Proper Technique: When pipetting manually, ensure the cell suspension is mixed thoroughly and consistently while seeding.
My cells are not growing as expected after seeding. What should I check? Poor cell growth after seeding can stem from several issues. First, verify the viability of your initial cell suspension, which should be at least 90% [58]. Next, check the age and quality of your culture medium and supplements; old or improperly formulated media can lack essential nutrients [61]. Also, confirm that your incubator conditions (temperature, COâ‚‚, and humidity) are stable and optimal for your specific cell line [58] [59]. Finally, ensure you are not passaging cells while they are still in the lag phase or after they have reached confluency and entered the stationary phase [58].
Why is it important to subculture cells at the log phase? Subculturing, or passaging, cells during their logarithmic (log) phase of growth is crucial because this is when cells are proliferating most actively and uniformly [58]. Passaging at this point helps to maintain cells at an optimal density for continued growth, prevents contact inhibition and nutrient exhaustion, and ensures a consistent and healthy cell population for reproducible experiments [58]. Allowing cells to become over-confluent and enter the stationary phase can lead to metabolic stress, genomic instability, and it takes longer for them to recover when reseeded [58].
Troubleshooting Guides
Problem: Rapid pH Shift and Poor Cell Health
| Possible Cause | Recommended Solution |
|---|---|
| Incorrect COâ‚‚ tension [58] | Adjust the COâ‚‚ percentage in your incubator to match the sodium bicarbonate concentration in your medium (e.g., 5-10% COâ‚‚ for 2.0-3.7 g/L sodium bicarbonate) [58]. |
| Overcrowding / High Cell Concentration [58] | Subculture cells before they reach full confluency. A high cell concentration can rapidly exhaust the medium and cause a toxic buildup of metabolic by-products [58]. |
| Low-quality or old culture medium [61] | Use fresh, properly formulated medium and ensure supplements like serum are of high quality and application-suitable [61]. |
Problem: High Variability in Drug Sensitivity Assays
| Possible Cause | Recommended Solution |
|---|---|
| Non-uniform cell seeding [60] | Implement automated cell seeding or use image-based cytometers to verify seeding uniformity across all wells [60] [59]. |
| Evaporation from drug plates [2] | Avoid storing diluted drugs in culture plates for long periods. Use sealed PCR plates or ensure plates are properly sealed with parafilm or tape to prevent evaporation and drug concentration [2]. |
| Cytotoxic effects of the solvent (e.g., DMSO) [2] | Use the lowest possible concentration of solvent and include matched vehicle controls (e.g., DMSO) for each drug dose to account for solvent effects on viability [2]. |
| Suboptimal seeding density [2] | Perform an initial optimization experiment to determine the ideal seeding density for your specific cell line and assay duration to ensure cells do not overgrow or remain too sparse [2]. |
Experimental Protocol: Optimizing Seeding Density for Drug Screens
This protocol provides a detailed methodology for determining the optimal cell seeding density for robust and reproducible drug sensitivity assays, based on current best practices [2] [19].
Key Research Reagent Solutions
| Item | Function in the Protocol |
|---|---|
| Hemocytometer or Automated Cell Counter | To determine precise cell concentration and viability before seeding [58]. |
| Cell Culture Vessel (e.g., 96-well plate) | The platform for cell growth and drug treatment [58]. |
| Complete Growth Medium | Provides essential nutrients; its composition should be optimized and consistent [58] [62]. |
| Resazurin Reduction Assay | A cost-effective and sensitive method for quantifying cell viability after drug treatment [2] [19]. |
| Dimethyl Sulfoxide (DMSO) | A common solvent for reconstituting water-insoluble drugs; must be used at minimal, non-toxic concentrations [2]. |
Step-by-Step Methodology
Prepare a Single-Cell Suspension: Start with an actively growing culture of your chosen cell line (e.g., MCF7 for breast cancer research). Harvest and dissociate the cells to create a single-cell suspension, and resuspend them in fresh, pre-warmed complete growth medium [58] [19].
Count and Calculate Dilutions: Count the cells using a hemocytometer or automated cell counter to determine the concentration (in cells/mL). Calculate the volumes needed to seed a range of densities (e.g., from 5.0 × 10³ to 1.5 × 10ⴠcells per well in a 96-well plate) [58] [2].
Seed the Cells: Plate the cells in your culture vessel according to the calculated densities. Ensure the final volume is consistent across all wells. Gently shake the plate in a cross-shake pattern to distribute the cells evenly and prevent clumping in the center [58] [59].
Incubate and Treat: Place the culture vessel in a 37°C incubator with 5% CO₂ and the appropriate humidity. Allow cells to adhere and grow for 24 hours. Then, treat the cells with your pharmaceutical drugs of interest. Include matched DMSO vehicle controls for each drug concentration to correct for any solvent effects on viability [2].
Measure Viability and Analyze: After the desired drug exposure period (e.g., 72 hours), measure cell viability using your chosen assay, such as the resazurin reduction assay [2] [19]. Calculate key drug response metrics like ICâ‚…â‚€ (half-maximal inhibitory concentration) or the more robust GRâ‚…â‚€ (concentration for half-maximal growth rate inhibition) [2].
Determine Optimal Density: The optimal seeding density is the one that produces stable dose-response curves with minimal variability between replicates, and where cells in the control wells are still in the log phase of growth at the end of the assay period, avoiding over-confluency [58] [2].
Workflow and Pathway Diagrams
Diagram 1: The process for optimizing cell seeding density for drug sensitivity screens.
Diagram 2: The impact of seeding density on the reliability of drug screening data.
Managing Evaporation and Edge Effects in Multi-Well Plates
What Are Evaporation and Edge Effects?
The edge effect is a phenomenon where the outer wells of a multi-well plate (such as a 96-well plate) experience higher rates of evaporation compared to the inner wells [63] [64]. This occurs because the edge wells are more exposed to environmental conditions within the incubator [63].
The primary consequence is evaporation, which leads to changes in the concentration of salts, nutrients, and test compounds in the culture medium or assay buffer [64]. This can result in:
- Increased osmolarity [64]
- Shifts in pH [65]
- Well-to-well variations in cell growth, gene expression, and assay results [65] [66]
This variability can significantly impact the reliability and reproducibility of your data, potentially leading to both false positive and false negative results (Type I and II errors) [66].
What Causes These Effects?
The core problem is the temperature gradient across the plate. Outer wells are less insulated and thus experience more evaporation, which concentrates the solution and alters the local environment [67]. This effect is not uniform; one study found that the edge effect can extend as far as three rows inward on a 96-well plate [66]. The table below summarizes the measurable impact on cell growth from one investigation.
Table: Impact of Edge Effect on Cell Metabolic Activity in 96-Well Plates [66]
| Plate Well Location | Reduction in Metabolic Activity (VWR Plates) | Reduction in Metabolic Activity (Greiner Plates) |
|---|---|---|
| Outer Wells | 35% lower | 16% lower |
| Second Row | 25% lower | 7% lower |
| Third Row | 10% lower | 1% lower |
| Central Wells | Baseline | Baseline |
Furthermore, the degree of edge effect can vary significantly depending on the manufacturer and design of the plate you use [66].
How Can You Prevent and Mitigate Edge Effects?
Here are proven strategies to conquer the edge effect, ranging from simple practices to specialized products.
Basic Practical Strategies
- Use a Low-Evaporation Lid or Sealing Tape: Always cover plates with their lids. For enhanced protection, use a low-evaporation lid or sealing films. For cell-based assays requiring gas exchange, use breathable sterile tape [64]. For biochemical assays, foil sealing tape or heat-sealing films are most effective [64].
- Fill Outer Wells with a Liquid Barrier: Fill the perimeter wells with sterile water, phosphate-buffered saline (PBS), or culture medium to create a humidified buffer zone [63]. This helps maintain humidity and reduce evaporation in the experimental outer wells.
- Optimize Your Incubation Practices:
- Thermal Equilibration: Equilibrate the entire plate to the incubation temperature (e.g., 37°C) before seeding cells to minimize thermal gradients [63].
- Room Temperature Pre-Incubation: After dispensing cells, let the plate sit at room temperature for a short period before placing it in the incubator. This promotes uniform cell settling and adhesion [63].
- Avoid Stacking Plates: If possible, avoid stacking plates in the incubator, as this can block airflow and create temperature gradients [65]. If stacking is necessary, ensure your incubator has good air circulation.
- Reduce Total Assay Time: Since evaporation is time-dependent, shortening the duration of the assay can directly reduce its impact [64].
Advanced Solutions
- Select Specialized Plate Designs: Some manufacturers produce plates designed specifically to minimize edge effects. For instance, some feature an advanced lid design that promotes better gas and temperature uniformity across all wells, significantly improving well-to-well consistency [65].
- Employ Robust Quality Control Metrics: For drug sensitivity screening, implement quality control measures beyond traditional controls. The Normalized Residual Fit Error (NRFE) metric can detect systematic spatial artifacts in drug-treated wells that traditional control-based metrics (like Z-prime) often miss [68]. Plates with high NRFE show significantly lower reproducibility [68].
Experimental Protocols for Mitigation
Protocol 1: Standard Mitigation for Cell Culture
This protocol integrates several basic strategies for robust cell culture experiments [63].
Diagram: Workflow for Standard Edge Effect Mitigation
Protocol 2: Quality Control for Drug Screening
This protocol uses the NRFE metric to identify and exclude unreliable data from high-throughput drug screens [68].
Diagram: QC Workflow for Drug Screening Data
The Scientist's Toolkit: Essential Materials
Table: Key Reagents and Materials for Managing Edge Effects
| Item | Function & Rationale |
|---|---|
| Sterile PBS or Water | An inert, cost-effective liquid used to fill perimeter wells, creating a humidified barrier that reduces evaporation in experimental edge wells [63]. |
| Breathable Sealing Tape | Allows for essential gas exchange (COâ‚‚ and Oâ‚‚) while limiting water vapor loss, making it ideal for long-term cell culture in multi-well plates [64]. |
| Foil Sealing Tape | Provides a nearly impermeable seal, offering the highest protection against evaporation for biochemical assays or short-term sample storage where gas exchange is not required [64]. |
| Specialized Plates (e.g., TPP) | Plates with unique lid and base designs that promote uniform air flow and temperature across all wells, inherently minimizing edge effects [65]. |
| Plate Heater / Water Bath | A uniform heat source (preferable to air incubators for some steps) for pre-warming plates to prevent thermal gradients during cell seeding or reagent addition [67]. |
Troubleshooting FAQs
Q1: My lab cannot afford specialized plates or large volumes of extra media. What is the most cost-effective way to reduce edge effect? The most budget-friendly approach is a combination of using a robust sealing film and the liquid barrier method with sterile water (instead of PBS or media). Ensure plates are properly pre-warmed before use and not stacked in the incubator to maximize the effectiveness of these simple measures [63] [65] [64].
Q2: I followed mitigation strategies, but my edge well data is still inconsistent. What could be wrong? Your plate seal might be compromised, or there could be an incubator-specific issue. Check that the incubator's humidity tray is filled and that air vents are not blocked. Furthermore, consider that your specific cell line or assay might be exceptionally sensitive. In this case, the most reliable solution is to avoid using the outer wells entirely for critical experimental data and use them only for liquid barriers or controls [63] [66].
Q3: Are edge effects only a problem for 96-well cell culture plates? No. While commonly discussed for 96-well cell culture, edge effects also significantly impact 384-well and 1536-well plates, where the smaller well volumes make evaporation an even more critical issue [64]. The problem also extends to other applications, including high-throughput proteomics sample preparation in multi-well plates [67].
Q4: How can I objectively check if my edge effect mitigation is working? You can perform a simple evaporation test. Fill a plate with a precise volume of water or PBS, use your standard mitigation techniques, and incubate it for the typical duration of your assay. Then, measure the remaining volume in edge versus center wells. A more advanced method for drug screening is to calculate the NRFE (Normalized Residual Fit Error) for your plates, which quantifies systematic spatial artifacts [68].
Controlling for Solvent Toxicity and DMSO Concentration Effects
Frequently Asked Questions (FAQs)
1. What are the primary safety concerns associated with using DMSO as a solvent in biological assays? The primary concern is that DMSO can induce significant cellular toxicity even at low concentrations previously considered safe. Studies have demonstrated that DMSO triggers apoptotic cell death in neuronal and retinal cells at concentrations as low as 1-4% (v/v). This toxicity occurs through caspase-3 independent pathways involving the translocation of Apoptosis-Inducing Factor (AIF) from mitochondria to the nucleus and activation of poly-(ADP-ribose)-polymerase (PARP) [69]. Furthermore, in antibiofilm studies, DMSO can significantly inhibit or, at intermediate concentrations (~6%), even promote biofilm formation, thereby confounding experimental results and leading to inaccurate conclusions about a test compound's efficacy [70].
2. At what concentration does DMSO typically start to exhibit toxicity? DMSO toxicity is concentration-dependent and can begin at low levels. In vitro studies using a retinal neuronal cell line confirmed toxicity at concentrations greater than 1% (v/v), with mechanisms elucidated at the 2-4% range [69]. In vivo rat models showed retinal apoptosis with intravitreal doses as low as 5 μl from stock concentrations of 1-8% (v/v) [69]. The effects can also be cell-type and assay-specific; for instance, in antibiofilm assays, DMSO concentrations between 0.03% and 25% significantly inhibited Pseudomonas aeruginosa biofilm formation [70].
3. What are the critical controls for experiments using DMSO as a solvent? Robust experimental design requires including appropriate controls to account for DMSO's effects. Key controls are:
- Untreated Control Group: A group that receives no treatment, not even the DMSO vehicle, to establish a baseline and check for solvent toxicity against the normal state [69].
- DMSO Vehicle Control Group: A group that receives the same final concentration of DMSO used to solubilize the test compound, ensuring any observed effects are not due to the solvent itself [69] [70].
- Media Control: To rule out effects from the culture medium alone [70]. It is critical that all control concentrations are explicitly stated in the experimental reporting [70].
4. How should I determine the maximum safe DMSO concentration for my experiment? The "safe" concentration is highly dependent on the specific cell type, assay duration, and endpoint measurement. You should:
- Consult literature on your specific cell line and assay type.
- Perform a dose-response curve for DMSO alone in your experimental system before testing any novel compounds. This preliminary testing will help you identify the threshold of toxicity in your specific setup [69].
- Use the lowest possible concentration that adequately solubilizes your test compound, ideally keeping the final concentration below 0.5-1% (v/v) unless your dose-response data confirms higher concentrations are harmless [69].
5. What is the recommended best practice for reporting DMSO usage in publications? To ensure scientific rigor and reproducibility:
- Always specify the final DMSO concentration to which cells or biofilms are exposed, expressed as % (v/v) [70].
- Report the data from all control groups, including the untreated control and DMSO vehicle control, and discuss these results in the context of the test compound's effects [69] [70].
- Avoid omitting control data or failing to specify control concentrations [70].
Troubleshooting Guides
Problem: Unexpected Cytotoxicity in Control Groups
Symptoms:
- Significant reduction in cell viability in DMSO vehicle control groups compared to untreated controls.
- Activation of cell death pathways (e.g., positive TUNEL staining, Annexin V binding) in the absence of the test compound.
- Inhibition of biofilm formation or, conversely, promotion of biofilm growth at intermediate DMSO concentrations.
Investigation and Resolution:
| Investigation Step | Action | Interpretation & Solution |
|---|---|---|
| Review DMSO Concentration | Calculate the final % (v/v) of DMSO in all experimental groups. | Concentrations >0.5% can be toxic for sensitive cell types. Solution: Re-prepare stock solutions to achieve a lower final concentration [69]. |
| Check Control Setup | Verify that both an untreated control (no DMSO) and a vehicle control (DMSO only) were included. | Without an untreated control, solvent toxicity cannot be detected. Solution: Always include both controls in the experimental design [69]. |
| Confirm Mechanism | Perform assays for caspase-independent apoptosis (e.g., AIF nuclear localization, PARP activation). | If positive, the observed toxicity is consistent with known low-dose DMSO effects. Solution: Consider alternative solvents or further reduce DMSO concentration [69]. |
| Assay-Specific Effects | In biofilm assays, test a range of DMSO concentrations alone. | DMSO may non-monotonically inhibit or promote biofilm growth. Solution: Ensure the chosen DMSO concentration has no significant effect on its own [70]. |
Problem: Inconsistent Results When Repeating Experiments with DMSO-Solubilized Compounds
Symptoms:
- High variability in viability or efficacy readouts between experimental replicates.
- Inability to reproduce dose-response curves.
Investigation and Resolution:
| Investigation Step | Action | Interpretation & Solution |
|---|---|---|
| Verify Solubility | Ensure the compound is fully soluble at the stock concentration in DMSO and does not precipitate upon dilution into the aqueous media. | Precipitation leads to inconsistent and inaccurate dosing. Solution: Perform a solubility test; use a lower stock concentration if needed [70]. |
| Standardize Handling | Use fresh, high-purity DMSO from a sealed, anhydrous bottle. Aliquot to prevent repeated freeze-thaw cycles and water absorption. | Water-contaminated DMSO can reduce solubility and may oxidize, forming harmful byproducts. Solution: Use fresh, dry DMSO aliquots [69]. |
| Control for Solvent Evaporation | In long-term cultures, check if the culture lid permits evaporation, potentially increasing DMSO concentration over time. | Evaporation can concentrate DMSO and test compounds, leading to increased toxicity. Solution: Use parafilm to seal culture plates or ensure humidified incubator conditions. |
Table 1: Documented Toxic Effects of DMSO Across Experimental Models
| Experimental System | DMSO Concentration Range | Observed Effect | Key Findings & Mechanism |
|---|---|---|---|
| Retinal Neuronal Cell Line (in vitro) [69] | >1% (v/v) | Significant cytotoxicity. | Confirmed via Annexin V, TUNEL, MTT, AlamarBlue assays. |
| Retinal Neuronal Cell Line (in vitro) [69] | 2% - 4% (v/v) | Caspase-3 independent apoptosis. | Mechanism: AIF translocation from mitochondria to nucleus; PARP activation. |
| Rat Retina (in vivo) [69] | 5μl of 1-8% stock (v/v) | Retinal apoptosis. | Toxicity confirmed in a live animal model. |
| Pseudomonas aeruginosa Biofilm [70] | 0.03% - 25% (v/v) | Significant inhibition of biofilm formation. | Acts synergistically with standard antibiotics at <1%. |
| Pseudomonas aeruginosa Biofilm [70] | ~6% (v/v) | Promoted biofilm growth. | Demonstrates a hormetic, non-monotonic effect. |
| Streptococcus pneumoniae Biofilm [70] | 0.03% - 25% (v/v) | No significant effect on biofilm formation. | Highlights organism-specific and model-specific DMSO effects. |
Table 2: Summary of Best Practices for DMSO Use in Biological Assays
| Practice Area | Common Error | Recommended Best Practice |
|---|---|---|
| Experimental Design | Using only a DMSO vehicle control, omitting an untreated control [70]. | Include both an untreated control (no treatment) and a DMSO vehicle control (matching the highest solvent concentration used) [69]. |
| Concentration Reporting | Failing to specify the final DMSO concentration in the assay [70]. | Always calculate and report the final % (v/v) DMSO to which cells/biofilms are exposed [69] [70]. |
| Data Interpretation | Attributing all effects solely to the test compound without considering solvent impact. | Compare test compound results against both the untreated and vehicle controls to isolate the solvent's contribution [69]. |
| Solvent Selection | Automatically using DMSO without exploring alternatives. | Use methods other than DMSO for solubilizing drugs where possible. If DMSO is essential, use the lowest feasible concentration [69]. |
Experimental Protocols
Protocol 1: Assessing DMSO Toxicity in Your Experimental System
Objective: To establish the maximum non-toxic concentration of DMSO for a specific cell line and assay duration.
Materials:
- High-purity, sterile DMSO
- Cell culture or bacterial model system
- Standard cell viability/assay kits (e.g., MTT, AlamarBlue, ATP assay)
Methodology:
- Prepare DMSO Dilutions: Prepare a series of culture media containing DMSO at final concentrations spanning 0.1%, 0.5%, 1%, 2%, and 4% (v/v). Include a media-only control with 0% DMSO.
- Expose Cells: Apply these media to your cells in replicates (n≥3) for the typical duration of your assay.
- Measure Viability: At the endpoint, perform your chosen viability or functionality assay according to the manufacturer's instructions.
- Analyze Data: Normalize all data to the 0% DMSO control (100% viability). Use statistical analysis (e.g., one-way ANOVA) to identify the highest DMSO concentration that does not cause a statistically significant reduction in viability/function.
Protocol 2: Designing a Controlled Experiment with a DMSO-Solubilized Compound
Objective: To test the effect of a novel compound solubilized in DMSO while rigorously controlling for solvent effects.
Materials:
- Test compound
- DMSO
- Assay reagents
Methodology:
- Define Groups: For each test compound concentration, plan the following experimental groups:
- Test Group: Culture + Target Concentration of Compound + Fixed [DMSO]
- Vehicle Control Group: Culture + Fixed [DMSO] (matching the concentration in the Test Group)
- Untreated Control Group: Culture + No Additives / Media Only
- Prepare Stocks: Dissolve the test compound in DMSO to create a high-concentration stock.
- Dilute for Assay: When adding to the assay, ensure that the volume of stock solution used results in the same final DMSO concentration across all relevant groups (Vehicle Control and all Test Groups). The Untreated Control should receive no DMSO.
- Run and Analyze: Conduct the experiment. The specific effect of the test compound is determined by comparing the Test Group to the Vehicle Control Group. The Vehicle Control Group compared to the Untreated Control reveals any toxicity from DMSO itself.
Visual Workflows and Pathways
DMSO-Induced Apoptosis Pathway
Experimental Design Workflow
The Scientist's Toolkit
Table 3: Essential Reagents and Materials for DMSO-Based Studies
| Item | Function/Description | Key Considerations |
|---|---|---|
| High-Purity DMSO | Aprotic solvent for solubilizing polar and non-polar compounds. | Use sterile, cell culture-tested grade. Store in sealed, anhydrous conditions in small aliquots to prevent water absorption and oxidation [69]. |
| Vehicle Control Solution | The DMSO solution without the active test compound, at the final concentration used in assays. | Critical control to isolate the biological effects of DMSO from those of the dissolved compound [69] [70]. |
| Viability Assay Kits | Reagents to quantify cell health (e.g., MTT, AlamarBlue, ATP-based luminescence). | Necessary for performing dose-response curves to establish DMSO toxicity thresholds in your specific model system [69]. |
| Apoptosis Detection Kits | Reagents to detect programmed cell death (e.g., Annexin V, TUNEL, caspase-3/7 activity assays). | Used to investigate the mechanism of DMSO-induced toxicity, confirming caspase-independent pathways [69]. |
| Culture Media | The nutrient medium for maintaining cells in vitro. | The composition can interact with DMSO. Media controls are essential to rule out confounding effects [70]. |
Optimizing Culture Media and Serum Conditions to Maintain Metabolic Stability
Troubleshooting Guides and FAQs
FAQ 1: What are the primary strategies for optimizing a complex, multi-component culture medium? Traditional optimization of culture media, which can contain dozens of components, is a resource-intensive process. Modern approaches use machine learning (ML) and Bayesian Optimization (BO) to drastically reduce the experimental burden.
- Biology-Aware Machine Learning: This approach integrates simplified experimental manipulation with error-aware data processing to build predictive models. It uses active learning to guide which experiments to run next, explicitly accounting for biological variability and experimental noise. This method has been used to successfully reformulate a 57-component serum-free medium for CHO-K1 cells, achieving a cell concentration approximately 60% higher than commercial alternatives [71].
- Bayesian Optimization-based Iterative Design: This framework is particularly effective for complex design spaces. It uses a probabilistic model to balance the exploration of new media formulations with the exploitation of promising ones identified from previous experiments. This method has been shown to identify improved media compositions using 3 to 30 times fewer experiments than standard Design of Experiments (DoE) methods [72].
FAQ 2: How can I effectively transition to a serum-free medium? The high cost and batch-to-batch variability of fetal bovine serum (FBS), alongside ethical concerns, drive the need for serum-free alternatives. A major hurdle is finding replacements for serum albumins, which stabilize the medium.
- Low-Cost Albumin Alternatives: Recent research has identified several low-cost, food-grade stabilizers that can effectively replace recombinant human serum albumin in serum-free media. In one study, these alternatives provided comparable or even superior stabilization for bovine muscle stem cells, enabling an overall medium price reduction of up to 73% for certain cell lines. The study also showed the approach was transferable to porcine, chicken, and CHO cells, though cell-line-specific differences were observed [73].
FAQ 3: What factors are critical for ensuring reproducible drug sensitivity testing in cultured cells? The reliability of drug response data is paramount for preclinical research. Key confounders include cell plating density, culture conditions, and the inherent growth rate of the cell line.
- Control of Plating Density: Seeding cells at an optimal, uniform density is crucial. Density that is too high can lead to contact inhibition or nutrient depletion, while density that is too low can cause delayed proliferation. It is recommended to perform pilot experiments to determine a density that ensures uniform growth over the entire assay period [74].
- Use of Growth-Rate Corrected Metrics: Traditional metrics like IC50 can be confounded by the natural variation in cell division rates between cell lines. Using Growth Rate Inhibition (GR) metrics corrects for this by computing drug response on a per-division basis, leading to more reproducible and reliable potency measurements [74].
- Standardized Protocols for Specific Cell Types: Different primary cells require unique culture support. For instance, primary Chronic Lymphocytic Leukemia (CLL) and Multiple Myeloma (MM) cells require co-culture with feeder cells or activation with cytokines (e.g., IL-2) to survive in culture for drug screens, whereas this is less critical for Acute Myeloid Leukemia (AML) cells [38].
FAQ 4: My cells are not growing well despite using optimized media. What could be wrong? Poor cell growth in the absence of contamination can stem from several issues:
- Quality of Supplements and Reagents: The quality and application suitability of supplements like FBS can vary between batches [75].
- Cryopreservation and Thawing Conditions: Cell health can be compromised by suboptimal freezing or thawing protocols, or inaccurate cell counting during passaging [75].
- Microbial Contamination: Invisible contaminants like mycoplasma can affect up to 30% of cultures without causing turbidity, negatively impacting cell metabolism and growth. Regular testing using PCR-based methods is recommended [75].
- Cell Line Misidentification: Cross-contamination of cell lines is a widespread problem. It is critical to source cells from reputable cell banks and perform authentication to ensure you are working with the correct cell line [75].
Table 1: Advanced Media Optimization Approaches
| Optimization Method | Key Principle | Experimental Efficiency | Demonstrated Outcome |
|---|---|---|---|
| Biology-Aware Machine Learning [71] | Uses active learning to guide experiments, accounting for biological noise. | High; 364 media tested for a 57-component reformulation. | ~60% increase in cell concentration for CHO-K1 cells vs. commercial media. |
| Bayesian Optimization [72] | Iterative design balancing exploration and exploitation with probabilistic models. | 3x - 30x fewer experiments than Design of Experiments (DoE). | Improved media for PBMC viability and recombinant protein production in K. phaffii. |
Table 2: Troubleshooting Poor Cell Growth
| Symptom | Potential Cause | Recommended Action |
|---|---|---|
| Poor growth, low viability | Microbial contamination (e.g., mycoplasma) | Implement regular PCR-based testing for contaminants [75]. |
| Suboptimal culture conditions | Validate plating density and growth rate; use GR metrics for drug studies [74]. | |
| Inaccurate cell count / passaging | Standardize cell counting and passaging protocols [75]. | |
| Inconsistent drug response | Uncontrolled plating density | Perform pre-study to determine density for uniform growth [74]. |
| Uncorrected growth rate differences | Use GR metrics instead of traditional viability measures [74]. | |
| High cost & variability | Use of FBS/recombinant albumin | Evaluate low-cost, food-grade stabilizers as albumin alternatives [73]. |
Detailed Experimental Protocols
Protocol 1: Bayesian Optimization Workflow for Media Development
This protocol outlines the iterative process for optimizing media composition using Bayesian methods, adapted from a study that successfully improved media for peripheral blood mononuclear cells (PBMCs) and recombinant protein production [72].
- Define the Optimization Goal: Clearly state the primary objective (e.g., maximize cell viability, specific metabolite production, or recombinant protein titer).
- Establish the Design Space: Identify all media components to be optimized (e.g., concentrations of basal media, cytokines, nutrients). Define constraints (e.g., total must sum to 100%).
- Run Initial Experiment Set: Perform a small, initial set of experiments (e.g., 6-8 formulations) to build the first surrogate model.
- Model and Plan Next Experiments:
- A Gaussian Process (GP) model is trained on the collected data.
- The Bayesian optimizer uses the GP to suggest the next batch of experiments that best balance exploring the design space and exploiting promising regions.
- Iterate: Repeat the cycle of running experiments and updating the model until the performance goal is met or the experimental budget is exhausted.
The following workflow diagram illustrates this iterative, self-reinforcing process:
Protocol 2: Standardized Drug Sensitivity and Resistance Testing (DSRT) for Cell Lines
This protocol provides a robust method for measuring drug response, adapted from NIH LINCS program recommendations and current best practices [74] [38].
Day 1: Preparation of Cells
- For adherent cells, bring into suspension using trypsinization. Collect cells in a tube and centrifuge at 300 g for 5 minutes at room temperature (RT) [38].
- Resuspend the cell pellet in fresh, pre-warmed medium.
- Filter the cell suspension through a 40 µm cell strainer to ensure a single-cell suspension [38].
- Count cells and resuspend to the optimal density determined from prior growth curves.
Day 1: Drug Exposure
- Transfer the cell suspension to pre-printed drug plates (e.g., 25 µL/well for 384-well plates) using a liquid dispenser. Include positive (e.g., 100 µM benzethonium chloride) and negative (e.g., 0.1% DMSO) controls on each plate [38].
- Incubate plates at 37°C, 5% CO2 for the desired duration (e.g., 72 hours).
Day 4: Viability Measurement
- Equilibrate the assay plates and CellTiter-Glo reagent at RT for 15-30 minutes.
- Add an equal volume of CellTiter-Glo to each well (e.g., 25 µL for a 384-well plate) [38].
- Measure luminescence with a plate-reading luminometer.
The Scientist's Toolkit
Table 3: Essential Reagents for Media Optimization and Drug Testing
| Reagent / Material | Function | Application Notes |
|---|---|---|
| Recombinant Albumin / Food-Grade Stabilizers [73] | Stabilizes serum-free media, binds lipids and other compounds. | Low-cost food-grade alternatives can reduce medium cost by up to 73% for some cell lines. |
| CellTiter-Glo Assay [38] | Measures cell viability based on ATP content, providing a luminescent readout. | A standard endpoint assay for large-scale drug screens; use on cells equilibrated to room temperature. |
| Cytokines (e.g., IL-2, IL-6) [38] | Supports survival and proliferation of specific primary cells (e.g., PBMCs, MM cells) in culture. | Essential for maintaining the viability of primary hematologic cancer cells during drug screens. |
| Bayesian Optimization Software | Computational framework for designing iterative experiments. | Drastically reduces the number of experiments needed to optimize complex media [72]. |
| Anti-CD3/CD28 Beads [38] | Activates T-cells, providing necessary survival signals for co-cultured cells like in MM. | Used in pre-stimulation of primary Multiple Myeloma cells prior to drug screening. |
Addressing Temporal Changes in Nutrient Depletion and Waste Accumulation
Troubleshooting Guides
Guide 1: Diagnosing Causes of Reduced Cell Growth and Viability
Problem: A noticeable decrease in cell proliferation or an increase in cell death is observed in cultures, compromising drug sensitivity assays.
Solution: Investigate temporal nutrient depletion and waste accumulation as primary causes.
| Observation | Potential Cause | Investigation Method | Corrective Action |
|---|---|---|---|
| Rapid growth reduction within minutes to hours [76] | Depletion of a key nutrient (e.g., glucose, glutamine) triggering cooperative reduction in uptake of other nutrients [76] | Use suspended microchannel resonator (SMR) to measure real-time mass accumulation rate (MAR); test with fresh media [76] | Short-term: Increase frequency of media exchange. Long-term: Optimize initial nutrient concentration or cell seeding density [77]. |
| Reduced growth & increased stress markers after 24-48 hours [77] | Nutrient levels (glucose, amino acids) falling below physiological range [77] | Measure glucose/amino acid concentrations in spent media (e.g., via HPLC or commercial kits). | Transition to a daily media exchange protocol to maintain nutrients in a physiological range [77]. |
| Cell death following 48 hours of glucose starvation [78] | Severe energy depletion and loss of cellular adhesion to the extracellular matrix [78] | Microscopic observation for detached, rounded cells; Trypan blue staining for viability [78]. | Ensure adequate glucose concentration; do not extend culture periods beyond 48 hours without media refreshment in glucose-free conditions [78]. |
| Growth arrest without immediate cell death (e.g., after Gln deprivation) [78] | Nutrient-specific stress response leading to a reversible proliferative arrest [78] | Cell counting and viability assays over several days; MTS assay for metabolic activity [78]. | Re-feed cultures with complete media to test for recovery; for long experiments, plan media exchange schedules. |
| Activation of cellular stress and death pathways [77] | Cumulative effect of nutrient depletion and waste accumulation (e.g., lactate, ammonium) [25] | RNA sequencing to identify enrichment of ER stress, apoptotic signaling, and starvation pathways [77]. | Profiling of spent media to identify consumed nutrients and accumulated wastes; adjust media formulation accordingly. |
Guide 2: Addressing Inconsistent Results in Drug Sensitivity Assays
Problem: Replicate drug treatment experiments show high variability in IC50 values or cell response.
Solution: Standardize culture conditions to minimize pre-analytical variables related to metabolic environment.
| Observation | Potential Cause | Investigation Method | Corrective Action |
|---|---|---|---|
| Variable drug efficacy between experiments | Fluctuating basal metabolic state of cells due to inconsistent nutrient availability before/during assay [77] | Standardize a pre-assay media refreshment protocol (e.g., 24 hours before drug addition). | Ensure all cells in an experiment have identical media history and are in a similar metabolic state prior to drug treatment. |
| Differences between labs using same cell line | Use of non-physiological, nutrient-rich media (e.g., DMEM, RPMI) that re-wires cellular metabolism [77] [25] | Shift to physiological media formulations (e.g., Plasmax) [77]. | Adopt a physiological media for all experiments to better mimic the in vivo environment and improve reproducibility [77]. |
| Uncontrolled charge heterogeneity in produced mAbs affecting drug activity assessment [25] | Nutrient depletion and accumulation of metabolic by-products (e.g., ammonium) during bioreactor process influencing Post-Translational Modifications [25] | Monitor charge variants using cation-exchange chromatography (CEX) or capillary isoelectric focusing (cIEF) [25]. | Optimize culture parameters (pH, temperature, feed timing) and use machine learning to model their complex effects on product quality [25]. |
Frequently Asked Questions (FAQs)
Q1: How quickly can nutrient depletion impact my cell cultures? The impact is remarkably fast. Studies using precise mass sensors show that depletion of glucose or glutamine can cause a significant reduction in cellular mass accumulation rate within minutes. This response is larger than the mass contribution of the depleted nutrient itself, indicating that cells cooperatively reduce the uptake of other nutrients [76].
Q2: My cells are alive but not growing after glutamine deprivation. Should I discard the culture? Not necessarily. Research on transformed fibroblasts shows that glutamine deprivation can induce a prolonged reversible proliferative arrest. Cells may resume proliferation if returned to complete media, even after 96 hours of starvation. Always test viability and recovery potential before discarding a culture [78].
Q3: We use standard commercial media (DMEM/RPMI). Why is nutrient depletion still a problem? Traditional commercial media often contain non-physiological, excess levels of nutrients. While this prevents starvation in the short term, it creates an artificial metabolic state. Furthermore, when using newer, more physiological media like Plasmax, nutrients can be rapidly consumed to below physiological levels, necessitating more frequent feeding schedules to maintain metabolic homeostasis [77].
Q4: What are the critical nutrients I should monitor most closely? Glucose and glutamine are two of the most critical and rapidly consumed nutrients. They serve as primary sources of energy and building blocks for biosynthesis. However, non-essential amino acids can also have a significant impact; their depletion sometimes causes a larger short-term growth reduction than the depletion of essential amino acids [76] [78].
Q5: How does nutrient depletion affect the quality of biotherapeutics like monoclonal antibodies (mAbs)? Nutrient depletion and waste accumulation are key drivers of charge heterogeneity in mAbs. They can promote post-translational modifications like deamidation (increasing acidic variants) and hinder enzymatic processing (increasing basic variants). This heterogeneity is a critical quality attribute affecting stability, efficacy, and safety, and must be tightly controlled during process development [25].
The following table summarizes key quantitative findings on nutrient depletion from recent research to inform your experimental planning.
Table 1: Experimentally Observed Nutrient Depletion Timeframes and Consequences
| Cell Line / System | Nutrient Depleted | Time to Effect | Observed Consequence | Experimental Context |
|---|---|---|---|---|
| L1210, FL5.12 [76] | Glucose | Minutes | 37-52% reduction in Mass Accumulation Rate (MAR) [76] | Rapid media exchange in SMR |
| L1210, FL5.12 [76] | Glutamine | Minutes | 30-34% reduction in Mass Accumulation Rate (MAR) [76] | Rapid media exchange in SMR |
| L1210 [76] | Non-Essential Amino Acids (NEAAs) | Minutes | ~2x larger MAR reduction vs. Essential AA depletion [76] | Rapid media exchange in SMR |
| PC-3, LNCaP, MCF-7, SH-SY5Y [77] | Glucose in Plasmax media | 48 hours | Depletion to hypoglycemic levels (<2 mM) [77] | Batch culture, measurement from spent media |
| cen3tel fibroblasts [78] | Glucose | ~48 hours | Loss of cellular adhesion, followed by cell death [78] | Batch culture, microscopy and viability counts |
| cen3tel fibroblasts [78] | Glutamine | ~96 hours | Prolonged proliferation arrest, followed by cell death [78] | Batch culture, cell counting |
Experimental Protocols
Protocol 1: Monitoring Nutrient Depletion in Spent Media Using Targeted Analysis
Objective: To quantitatively track the consumption of key nutrients from the culture media over time to establish a feeding regimen.
Materials:
- Cells of interest and their appropriate culture medium.
- Sterile culture flasks/plates.
- Centrifuge tubes.
- Benchtop centrifuge.
- 0.22 µm syringe filters.
- Access to HPLC or LC-MS/MS system.
Method:
- Seed Cells: Seed cells at a density relevant for your assay (e.g., 2-2.5 x 10^5 cells per 3 cm dish [78]).
- Collect Spent Media: At predetermined time points (e.g., 0, 24, 48, 72 hours), carefully collect the culture supernatant from representative cultures.
- Process Samples:
- Centrifuge the collected media (e.g., 500 x g for 5 minutes) to pellet any floating cells or debris.
- Filter the supernatant through a 0.22 µm filter.
- Store filtered samples at -80°C until analysis to prevent further degradation.
- Analyze Metabolites: Use targeted analytical methods (e.g., LC-MS/MS) to quantify the concentrations of nutrients of interest (e.g., glucose, amino acids) in the spent media versus a sample of fresh, unused media [77].
- Data Analysis: Plot the concentration of each nutrient against time. The slope of the depletion curve informs the consumption rate.
Protocol 2: Assessing Acute Cellular Growth Response to Nutrient Change
Objective: To measure the immediate impact of nutrient depletion on single-cell mass accumulation.
Materials:
- Suspension cells (e.g., L1210, Jurkat) or trypsinized adherent cells.
- Standard and nutrient-deficient media.
- Suspended Microchannel Resonator (SMR) system [76].
Method:
- Establish Baseline: Load a single cell into the SMR and perfuse it with standard growth medium. Measure the oscillation period to calculate the buoyant mass and establish a baseline Mass Accumulation Rate (MAR) over ~20 minutes [76].
- Deplete Nutrient: Rapidly switch the perfusion fluid to an isosmotic medium lacking the nutrient of interest (e.g., no glucose, no glutamine).
- Monitor Response: Continuously track the cell's buoyant mass. A measurable reduction in MAR can be observed within minutes of the switch [76].
- Reversibility Test (Optional): Switch the medium back to the complete formulation to test if the growth reduction is reversible.
Signaling Pathway and Experimental Workflow Diagrams
Diagram 1: Cellular Response Pathway to Acute Nutrient Depletion
Diagram 2: Workflow for Spent Media Analysis
The Scientist's Toolkit
Table 2: Essential Reagents and Tools for Investigating Nutrient Depletion
| Item | Function / Description | Example Application |
|---|---|---|
| Physiological Culture Media | Media formulated to mimic the nutrient composition of human blood plasma (e.g., Plasmax). Reduces metabolic artifacts from standard rich media [77]. | Creating more in vivo-like conditions for drug sensitivity testing; studying realistic nutrient consumption rates. |
| Suspended Microchannel Resonator (SMR) | A device that measures the buoyant mass of single cells with high precision, allowing real-time monitoring of mass accumulation rates [76]. | Detecting acute (minute-scale) growth responses to nutrient depletion that are invisible in population-level assays. |
| LC-MS/MS Systems | Liquid Chromatography with Tandem Mass Spectrometry. The gold standard for targeted, quantitative analysis of specific metabolites (e.g., amino acids, glucose) in complex mixtures like spent media [77]. | Precisely measuring the concentration of nutrients in spent culture media to generate depletion curves. |
| Spent Media Analysis Kits | Commercial colorimetric or fluorometric assay kits for detecting specific metabolites (e.g., glucose, lactate, glutamine). | A more accessible alternative to LC-MS/MS for labs to monitor key metabolites and determine media exhaustion. |
| Machine Learning (ML) Platforms | Computational tools used to model the complex, non-linear relationships between culture parameters (nutrients, pH, temperature) and cell behavior or product quality [25]. | Optimizing culture conditions and feeding strategies in bioprocess development to control critical quality attributes like charge heterogeneity. |
Ensuring Data Integrity: Metrics, AI, and Cross-Platform Validation
In preclinical drug development and personalized oncology, accurately quantifying how cancer cells respond to therapeutic compounds is paramount. The choice of drug response metric can significantly influence the interpretation of a drug's potency and efficacy, impacting decisions on which drug candidates advance to clinical trials. For decades, the half-maximal inhibitory concentration (IC50) was the standard benchmark for this purpose. However, a fundamental limitation has been recognized: IC50 values are highly sensitive to the rate of cell division during the assay [79]. This means that for a drug with a specific mechanism of action, the calculated IC50 can vary dramatically simply due to differences in the natural growth speeds of different cell lines or variations in culture conditions, creating artefactual correlations and obscuring true biological insights [79] [80].
To address these confounders, next-generation metrics have been developed. The Normalized Growth Rate Inhibition (GR) method, which yields metrics like GR50, was introduced to correct for the effects of cell division rate [79] [80]. Subsequently, the Normalized Drug Response (NDR) metric was refined to incorporate both positive and negative control conditions, providing a more dynamic range, especially in detecting cytotoxic effects [81]. This technical support article provides a comparative analysis of these key metrics—IC50, GR50, and NDR—to guide researchers in selecting and implementing the most appropriate method for their drug sensitivity studies, directly within the context of optimizing cell culture conditions for robust and reproducible results.
Metric Definitions and Theoretical Foundations
IC50: The Conventional Metric
- Definition: The half-maximal inhibitory concentration (IC50) is the concentration of a drug that reduces cell viability (or a surrogate signal like ATP content) by 50% relative to an untreated control at the end of the assay period [82].
- Calculation: It is derived by fitting a sigmoidal curve to dose-response data where the y-axis represents the relative cell count or viability, typically normalized to a vehicle control (100%) and a positive control (0%). The point at which this curve crosses the 50% inhibition level is the IC50 [82].
- Key Limitation: Its value is intrinsically tied to the number of cell divisions that occur during the experiment. A faster-growing cell line will show a much lower (and seemingly more potent) IC50 for the same cytostatic drug than a slower-growing one, not due to different drug mechanisms but simply due to the differential accumulation of cells in the control well [79].
GR50: The Growth Rate-Corrected Metric
- Definition: The GR50 is the drug concentration at which the normalized growth rate inhibition (GR value) is 0.5. The GR value quantifies the drug-induced change in growth rate on a per-division basis [79] [80].
- Core Formula: The GR(c) value for a drug at concentration
cis calculated as:GR(c) = 2^(k(c) / k(0)) - 1, wherek(c)is the growth rate of the treated culture andk(0)is the growth rate of the untreated control [79]. - Interpretation of GR values:
- Key Advantage: GR metrics are designed to be largely independent of cell division rate and assay duration, providing a more consistent measure of a drug's biological effect [79].
NDR: The Metric for Cytotoxic Dynamic Range
- Definition: The Normalized Drug Response (NDR) is a further refinement that makes use of both negative (vehicle) and positive (full cell death) control conditions to normalize the response. It was developed to better capture cytotoxic effects in imaging-based assays [81].
- Context: The NDR metric was tested alongside GR metrics in live-cell imaging-based organoid drug screening, where it was found to outperform traditional relative viability (RV) and GR metrics in certain contexts [81]. The authors of one study subsequently developed the Normalized Organoid Growth Rate (NOGR) metric to more effectively capture both cytostatic and cytotoxic drug effects in brightfield imaging assays, building upon the principles of NDR and GR [81].
- Key Advantage: By incorporating a full cell death control, it expands the dynamic range for quantifying strong cytotoxic effects, which can be limited when using fluorescence cell death markers that may not fully penetrate 3D organoid structures [81].
Table 1: Core Definitions and Interpretations of Drug Response Metrics
| Metric | Full Name | Fundamental Principle | Key Interpretation |
|---|---|---|---|
| IC50 | Half-Maximal Inhibitory Concentration | Measures relative cell count/viability at endpoint. | Concentration that reduces cell count to 50% of the control. |
| GR50 | Half-Maximal Growth Rate Inhibition | Measures drug-induced change in growth rate per division. | Concentration that reduces the growth rate to 50% of the control's rate. |
| NDR | Normalized Drug Response | Normalizes growth response using both vehicle and cell death controls. | Designed to improve quantification of cytotoxic effects. |
A direct comparison of these metrics reveals critical differences in their performance and suitability for various experimental goals. The core advantage of GR and NDR metrics lies in their correction for confounding factors that severely impact IC50.
Table 2: Comparative Performance of Drug Response Metrics
| Characteristic | IC50 / Emax | GR50 / GRmax | NDR / NOGR |
|---|---|---|---|
| Sensitivity to Cell Division Rate | Highly sensitive; major confounder [79] | Largely insensitive; corrects for it [79] [80] | Designed to be insensitive [81] |
| Sensitivity to Assay Duration | Highly sensitive; values shift over time [79] | Stabilizes quickly (within ~1 division) [79] | Suitable for time-course live-cell imaging [81] |
| Ability to Distinguish Cytostatic vs. Cytotoxic | Poor, based on single endpoint [81] | Good; GR < 0 indicates cytotoxicity [79] | Enhanced; improved dynamic range for cell death [81] |
| Dependence on Seeding Density | Highly sensitive [81] [2] | Reduced sensitivity with live-cell imaging [81] | Reduced sensitivity with live-cell imaging [81] |
| Required Controls | Vehicle control (negative control) [82] | Vehicle control & initial cell count (or doubling time) [79] [74] | Vehicle control & full cell death control (positive control) [81] |
| Primary Application | Endpoint bulk viability assays (e.g., CellTiter-Glo) [81] | Endpoint or time-course assays (2D or 3D) [79] [74] | Live-cell imaging-based assays (especially 3D organoids) [81] |
The robustness of GR metrics was demonstrated in a study where the induction of a slow-growing phenotype (via BRAF
Experimental Protocols & Methodologies
Core Protocol for GR Metric Calculation
Implementing GR metrics requires modest changes to conventional dose-response experiments [79] [74].
Experimental Setup:
- Plate cells in a multi-well plate, ensuring uniform growth. Optimize seeding density to avoid contact inhibition or nutrient depletion during the assay [74] [2].
- Include an "time-zero" plate or wells to measure the initial cell count at the time of drug addition (
N_initial). This is crucial for endpoint calculations [79] [74]. - For each drug titration, include vehicle-treated control wells (
N_control) to measure untreated growth. - Expose cells to a range of drug concentrations for a defined period (e.g., 72 hours).
Cell Number Measurement:
GR Value Calculation:
Curve Fitting and GR50 Determination:
- Plot GR(c) values against the log of drug concentration.
- Fit a sigmoidal curve (e.g., a Hill curve) to the data.
- The GR50 is the concentration where the fitted curve crosses GR(c) = 0.5. Other parameters like GRmax (the minimum GR value) can also be extracted [79].
Advanced Protocol for NDR/NOGR in Imaging-Based Assays
For assays utilizing live-cell imaging, particularly with 3D patient-derived organoids, the workflow can be adapted to leverage the strengths of NDR and its derivatives like NOGR [81].
The key differentiator in this workflow is the use of label-free, image-based segmentation to track organoid growth and classify viability over time, which overcomes limitations of endpoint biochemical assays [81].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Advanced Drug Response Assays
| Item | Function / Description | Example Use Case |
|---|---|---|
| Cell Viability Assay Kits (e.g., CellTiter-Glo, Resazurin) | Measures ATP or metabolic activity as a surrogate for cell number. Requires careful optimization to avoid evaporation and DMSO effects [2]. | Endpoint viability measurement for GR calculation in 2D cultures. |
| Live-Cell Imaging System | Automated microscope for non-invasive, time-lapse imaging of cells in culture. Enables direct growth tracking. | Essential for the OrBITS method and direct growth rate calculation in 2D and 3D models [81]. |
| Image Analysis Software (e.g., OrBITS, deepOrganoid) | Label-free segmentation algorithms to identify and track organoids or cells in brightfield images. | Quantifying organoid growth and classifying dead organoids by their dark, granulated appearance [81]. |
| Extracellular Matrix (ECM) (e.g., Matrigel, Collagen) | Provides a 3D scaffold for culturing organoids, mimicking the in vivo tumor microenvironment [14]. | Establishing patient-derived tumor organoid (PDTO) cultures for drug screening. |
| DMSO (Cell Culture Grade) | Universal solvent for water-insoluble compounds. Must be used at low, non-toxic final concentrations (e.g., <0.1-1%) with matched vehicle controls for each dose [2]. | Preparing drug stock solutions and vehicle controls. |
Troubleshooting Guides & FAQs
FAQ 1: My dose-response curves look poor and IC50 values are highly variable. What could be the main issue?
- Primary Cause: The most common confounder is inconsistent cell growth between experiments, often due to variations in seeding density, culture conditions, or assay duration. These factors directly and artifactually impact IC50 values [79] [2].
- Solution:
- Optimize and Standardize: Systematically test a range of seeding densities to find one that ensures uniform, exponential growth throughout the assay without reaching confluence [74] [2].
- Switch to GR Metrics: Adopt GR metrics, which are designed to be robust against these variations. Ensure you measure an initial cell count (
N_initial) at the time of drug addition for accurate GR calculation [79] [80]. - Control Evaporation: Use properly sealed plates and include perimeter wells filled with PBS to minimize "edge effects" caused by evaporation, which can skew results [2].
FAQ 2: When should I use GR50 over IC50, and when is NDR more appropriate?
- Use IC50 with caution: Its use should be limited to situations where cell growth is minimal or highly consistent across all conditions and replicates, which is rare. It may be acceptable for rapid cytotoxicity assays where cells do not divide.
- Default to GR50: For any standard dose-response experiment with dividing cells, GR50 is the recommended metric. It provides a more biologically relevant measure of drug potency by correcting for division rate, leading to more reproducible results within and between laboratories [79] [2].
- Choose NDR/NOGR for advanced models: When working with 3D models like organoids in live-cell imaging assays, NDR or the newer NOGR metric is more appropriate. They are specifically designed to handle the complexity of these models and offer a superior dynamic range for detecting cytotoxic cell death label-free [81].
FAQ 3: How do I properly define 0% and 100% for these metrics, and why does it matter?
- For IC50: 100% is typically defined by the vehicle (e.g., DMSO) control, and 0% can be defined by a positive control (e.g., a high concentration of a cytotoxic drug) or the background of the assay. Ambiguity in these definitions leads to the problematic concept of "absolute IC50" versus "relative IC50" [82].
- For GR Metrics: 100% growth (GR=1) is defined by the untreated control's growth rate. 0% growth (GR=0) is defined as no net growth over the assay, a state of perfect cytostasis. Negative GR values indicate cell loss [79].
- For NDR/NOGR: 100% is defined by the vehicle control, and 0% is defined by a full cell death control (e.g., using a potent cytotoxic agent). This explicit use of a death control is key to its enhanced performance in detecting cytotoxicity [81].
- Why it matters: The entire dose-response curve and all derived metrics (IC50, GR50) depend entirely on how 0% and 100% are defined. Inconsistent definitions are a major source of non-reproducibility. Always report how your controls were set up [82].
FAQ 4: My drug shows a strong effect, but the curve doesn't reach a bottom plateau. Can I still report a GR50?
- Yes, but with care. If the data form a clear downward trend but the bottom plateau is not fully defined, the calculated GR50 can still be informative, provided you have a reliable positive control to define the minimum response (0% growth or full death) [81] [82].
- Best Practice: Constrain the bottom of the curve fit to the value defined by your positive control (for NDR) or to 0 (for GR, indicating cytostasis). This produces a more reliable and interpretable GR50 estimate than an unconstrained fit to incomplete data [82]. Report this constraint in your methods.
Implementing the Normalized Drug Response (NDR) Metric for Improved Accuracy
Understanding Normalized Drug Response (NDR)
The Normalized Drug Response (NDR) metric is an improved model for quantifying drug effects in cell-based screening. It was developed to address biases in existing methods that arise from varying cell growth rates and experimental artifacts, which are common sources of inconsistency in high-throughput drug screens [83].
Unlike conventional metrics that rely solely on a negative control (like untreated cells), NDR utilizes both positive controls (e.g., wells with completely dead cells) and negative controls to dynamically account for background noise and differences in cell growth. This allows NDR to accurately characterize a wider spectrum of drug-induced effects, from complete cell death (lethal effect) to growth inhibition and even growth stimulation [83] [84].
How NDR Compares to Other Drug Response Metrics
The table below summarizes how NDR addresses the limitations of traditional drug sensitivity metrics.
| Metric | Key Inputs | Pros | Cons |
|---|---|---|---|
| Normalized Drug Response (NDR) | Start-point & end-point readouts; Positive and negative controls [83] | Accounts for growth rates and background noise; Captures a wide spectrum of effects (lethal, inhibitory, stimulatory); Improved consistency across replicates and time points [83] | Requires careful experimental setup for all controls |
| Percent Inhibition (PI) | End-point readouts; Positive control [83] | Uses positive control to model background noise [83] | Sensitive to changes in negative control growth; Narrower spectrum of captured effects [83] |
| Growth Rate Inhibition (GR) | Start-point & end-point readouts; Negative control only [83] [2] | Accounts for varying cell division rates; More consistent than IC50 or Emax [2] | Does not account for variability in positive control; Can produce unstable values in slow-growing cells [83] |
| IC50 / Emax | End-point readouts; Negative control only [2] | Simple to calculate and interpret | Highly sensitive to cell growth rate and assay duration; Leads to biased estimates [2] |
A Step-by-Step Protocol for Implementing an NDR Assay
Here is a detailed methodology for a cell viability-based drug sensitivity assay designed for NDR calculation, incorporating best practices for robust results.
1. Experimental Design and Plate Layout
- Cell Seeding: Seed cells in a 96-well or 384-well microplate. Optimization of seeding density is critical for robust NDR calculation [2].
- Controls: Include the following control wells on every plate:
- Negative Control: Cells treated with the drug's solvent (e.g., DMSO).
- Positive Control: Cells treated with a cytotoxic agent to induce 100% cell death.
- Blank Control: Culture medium without cells to measure background signal.
- Drug Treatment: Treat cells with a titration range of the drug(s) of interest.
2. Key Reagents and Materials
| Research Reagent Solution | Function in the Assay |
|---|---|
| Cell Viability Assay Reagent | Measures metabolic activity or ATP content as a proxy for viable cell number (e.g., Resazurin, RealTime-Glo) [83] [2]. |
| Drug Dilution Series | A range of concentrations to establish a dose-response curve. |
| Positive Control Compound | A substance known to kill all cells (e.g., a high-concentration staurosporine or digitonin) to define the baseline for 100% effect [83]. |
| Vehicle Control (e.g., DMSO) | The solvent used to dissolve the drug; used to define the baseline for 0% effect. Must be matched in all control and drug-treated wells [2]. |
3. Data Acquisition and NDR Calculation
- Readout: Use a luminescence or fluorescence plate reader.
- Timing: Take measurements at two time points:
- Start-point (T0): Shortly after adding drugs (e.g., 4-6 hours post-seeding). This represents the initial cell population.
- End-point (T1): After the desired drug exposure period (e.g., 72 hours). This represents the final cell population after treatment [83].
- Calculation: The NDR metric is calculated using the following formula, which normalizes the drug-treated signal against the dynamic changes in both negative and positive controls [83]:
NDR = (ST1 - PT1) / (ST0 - PT0) / (NT1 - PT1) / (NT0 - PT0)Where:S= Signal in the drug-treated wellN= Signal in the negative control wellP= Signal in the positive control wellT0= Start-point measurementT1= End-point measurement
Troubleshooting Common Issues in NDR Implementation
FAQ 1: Our NDR values are inconsistent between experimental replicates. What could be the cause?
- Potential Cause 1: Inconsistent cell seeding density. Variations in the number of cells plated can lead to differing growth rates and viability readouts, directly impacting NDR consistency [2].
- Solution: Standardize the process for creating a single-cell suspension and optimize the seeding density for each cell line to ensure uniform plating. Using automated cell counters and liquid dispensers can improve reproducibility [2].
- Potential Cause 2: Evaporation from drug and control plates during storage or incubation. This can unintentionally concentrate compounds and solvents, altering the effective dose and DMSO concentration, which is toxic to cells [2].
- Solution: Avoid storing diluted drugs in culture plates for extended periods. If necessary, use sealed plates (e.g., with Parafilm or aluminum tape) and store at recommended temperatures. Include matched DMSO controls for each drug concentration to correct for solvent toxicity [2].
FAQ 2: The signal from our positive control is unstable, making the NDR metric unreliable. How can we fix this?
- Potential Cause: The chosen positive control agent or its concentration is not consistently achieving 100% cell death, or the background signal is too high.
- Solution: Titrate different cytotoxic agents (e.g., high-dose staurosporine, digitonin) to identify one that consistently and completely kills your specific cell lines. Ensure the blank control (medium alone) is used to correct for background luminescence or fluorescence.
FAQ 3: For very slow-growing cells, the NDR metric seems to perform poorly. Is there an alternative?
- Potential Cause: In cells with very slow division rates, the dynamic range between the start-point (T0) and end-point (T1) measurements becomes very small, which can reduce the accuracy of growth-rate based metrics.
- Solution: While NDR is more stable than GR in slow-growth conditions [83], consider extending the assay duration to allow for more measurable growth, if cell viability permits. Alternatively, in advanced models like patient-derived organoids, the recently developed Normalized Organoid Growth Rate (NOGR) metric may offer further improvements for capturing effects in slow-growing systems [81].
FAQ 4: Can NDR be used with imaging-based assays, not just viability readouts?
- Answer: Yes. The NDR principle has been successfully adapted for live-cell imaging. It can be applied to metrics derived from brightfield images, such as organoid growth area, and can be combined with label-free detection of cell death to enhance its dynamic range and accuracy [81].
NDR Calculation and Experimental Workflow
The following diagram illustrates the logical workflow for planning, executing, and analyzing a drug sensitivity experiment using the NDR metric.
Key Performance Indicators for NDR Validation
After implementing an NDR assay, monitor these quantitative indicators to validate its performance.
| Parameter to Measure | Target Value / Outcome | Purpose of the Check |
|---|---|---|
| Z'-factor | > 0.5 [83] | To confirm the assay is robust and has a sufficient dynamic range between positive and negative controls. |
| Replicate Consistency | Low absolute difference in NDR between replicates [83] | To ensure the technical reproducibility of the assay and the NDR metric. |
| Dose-Response Curve Fitting | High-quality sigmoidal curve fit | To verify that the data quality is sufficient for reliable extraction of summary metrics (e.g., IC50, GR50). |
| Positive Control Signal | Stable and significantly different from negative control | To validate that the positive control is consistently effective and that background noise is properly accounted for. |
Leveraging AI and Machine Learning for Predictive Drug Sensitivity Analysis
Artificial Intelligence (AI) and Machine Learning (ML) are transforming the field of predictive drug sensitivity analysis, offering powerful tools to address the global challenge of antimicrobial resistance (AMR) and optimize cancer therapies. These technologies can extract in-depth information from imaging and laboratory data, enabling the swift prediction of pathogen antibiotic resistance and providing reliable evidence for the judicious selection of antibiotics [85]. For researchers focused on optimizing cell culture conditions, AI/ML integration provides unprecedented capabilities to analyze high-dimensional data, identify complex patterns, and generate accurate predictions of drug response, ultimately enhancing the reproducibility and clinical relevance of preclinical drug sensitivity testing.
Foundational AI/ML Concepts for Drug Sensitivity Testing
Core Machine Learning Approaches
Several AI/ML approaches have been successfully applied to drug sensitivity prediction:
Classical Machine Learning: Traditional models including Support Vector Machines (SVM), Random Forests (RF), Logistic Regression (LR), and K-Nearest Neighbors (KNN) have been widely used for drug sensitivity prediction [86] [87]. These methods can effectively analyze relationships between cellular features and drug response but may struggle with extremely high-dimensional data.
Deep Learning Models: Deep neural networks (DNN) and variational autoencoders (VAE) have demonstrated significant performance improvements for different drugs and disease conditions [87]. These models can capture complex, non-linear relationships in high-dimensional genomic and proteomic data.
Interpretable AI Models: Newer approaches like DrugGene integrate biological knowledge into model architecture by mapping neural network components to specific biological subsystems and pathways [87]. This enhances model transparency and provides mechanistic insights alongside predictions.
Quantum Machine Learning (QML): Emerging QML frameworks like QProteoML leverage quantum algorithms to address challenges of high dimensionality, feature redundancy, and class imbalance in proteomic data [86]. These approaches use quantum phenomena (superposition and entanglement) to model complex biological relationships more efficiently.
Key Data Types for AI-Driven Predictive Modeling
| Data Category | Specific Data Types | AI Application Examples |
|---|---|---|
| Cell Line Data | Gene expression, Gene mutations, Copy number variations [87] | Visible Neural Networks (VNN) for interpreting subsystem states [87] |
| Drug Compound Data | Chemical structures, Molecular descriptors, Morgan fingerprints [87] | Artificial Neural Networks (ANN) for capturing structural features [87] |
| Experimental Results | IC50, AUC, GR metrics, Cell viability measurements [2] [19] | Model training and validation for sensitivity prediction [87] |
| Clinical Data | Patient-derived cancer cells, Treatment outcomes [35] | Translation of preclinical findings to clinical applications |
Frequently Asked Questions (FAQs)
Q1: How can AI/ML address the critical issue of experimental variability in cell-based drug screens?
Experimental variability in cell-based drug screens remains a significant challenge, with biological and technical factors substantially affecting data replicability and reproducibility [2]. AI/ML approaches can identify and correct for these sources of variability through several mechanisms: Variance component analysis can determine the relative contribution of different experimental parameters (e.g., pharmaceutical drug choice, cell line, growth medium, assay incubation time) to overall variability [2]. Furthermore, optimized AI models can integrate these confounding factors into predictive algorithms, effectively normalizing for experimental variability and generating more robust predictions across different laboratory conditions.
Q2: What are the key advantages of interpretable AI models over traditional "black box" approaches for drug sensitivity prediction?
Interpretable AI models provide crucial advantages for drug sensitivity prediction by enhancing model transparency and providing biological insights. While traditional deep learning models often function as "black boxes," interpretable approaches like DrugGene incorporate biological pathways directly into the model architecture [87]. This allows researchers to not only predict drug sensitivity but also understand the underlying biological mechanisms driving these predictions. The model can identify which specific cellular subsystems and pathways are most influential in determining drug response, providing testable hypotheses for further experimental validation and potentially revealing new drug targets or resistance mechanisms.
Q3: How can researchers ensure their cell viability assays are optimized for AI-driven drug sensitivity analysis?
Optimizing cell viability assays requires careful attention to multiple experimental parameters that directly impact data quality and AI model performance. Key considerations include: selecting appropriate cell numbers to avoid over-confluence or sparse growth, controlling for evaporation effects in multi-well plates, using matched DMSO controls for each drug concentration to account for solvent toxicity, and implementing rigorous quality control metrics [2] [19]. Additionally, employing robust drug response metrics (GR metrics, AUC, IC50) that account for cellular division rates can significantly improve interlaboratory reproducibility and enhance AI model generalizability across different experimental conditions [2].
Q4: What role can quantum machine learning play in advancing drug sensitivity prediction?
Quantum Machine Learning (QML) represents a promising frontier for addressing particularly challenging aspects of drug sensitivity prediction. QML frameworks like QProteoML are specifically designed to handle high-dimensional, imbalanced datasets common in proteomic and genomic studies of drug response [86]. By leveraging quantum principles including superposition and entanglement, these approaches can perform complex computations more efficiently than classical systems, potentially identifying subtle patterns in data that might be missed by conventional algorithms. This is particularly valuable for predicting rare resistance patterns or analyzing datasets where the number of features far exceeds the number of samples.
Troubleshooting Guides
Poor Model Performance and Overfitting
Problem: AI/ML models for drug sensitivity prediction show excellent performance on training data but poor generalization to new data, indicating overfitting.
Potential Causes and Solutions:
- Cause: High-dimensional feature space with limited samples ("curse of dimensionality") [86]
- Solution: Implement dimensionality reduction techniques such as Quantum Principal Component Analysis (qPCA) [86] or feature selection methods to identify the most informative biomarkers
- Cause: Class imbalance with under-representation of resistant cases [86]
- Solution: Utilize data augmentation approaches including Quantum Generative Adversarial Networks (QGANs) to generate synthetic samples for underrepresented classes [86]
- Cause: Inadequate cross-validation strategies
- Solution: Employ nested cross-validation and external validation sets to ensure robust performance estimation
Experimental-AI Integration Challenges
Problem: Discrepancies between AI model predictions and experimental results in validation studies.
Potential Causes and Solutions:
- Cause: Suboptimal cell culture conditions introducing variability not accounted for in models [2]
- Solution: Systematically optimize and standardize cell culture parameters including cell seeding density, medium composition, and drug treatment duration [2]
- Cause: Improper drug storage and handling affecting actual drug concentrations [2]
- Solution: Implement controlled storage conditions for diluted drugs and account for solvent evaporation effects, particularly in DMSO-based solutions [2]
- Cause: Inappropriate viability assay endpoints or measurement techniques [19]
- Solution: Validate assay conditions for each cell line and ensure linear dynamic range for measurements
Interpretation and Biological Validation Difficulties
Problem: Challenges in interpreting AI model outputs and translating predictions to biologically meaningful insights.
Potential Causes and Solutions:
- Cause: Use of "black box" models without inherent interpretability [87]
- Solution: Implement interpretable AI approaches like DrugGene that map predictions to specific biological subsystems and pathways [87]
- Cause: Insufficient integration of prior biological knowledge
- Solution: Incorporate pathway databases and functional annotations into model architecture to provide biological context for predictions
- Cause: Lack of experimental validation strategies for model-derived hypotheses
- Solution: Design targeted experiments to test model-identified key pathways and biomarkers
Experimental Protocols and Workflows
AI-Enhanced 2D Drug Sensitivity Screening Protocol
This protocol outlines an optimized approach for 2D drug sensitivity screening that generates high-quality data for AI/ML model development and validation [2] [19].
Materials and Reagents:
- Cancer cell lines of interest
- Complete growth medium with appropriate serum supplementation
- Pharmaceutical compounds dissolved in appropriate solvents (typically DMSO)
- Resazurin solution or other validated viability assay reagents
- Tissue culture-treated 384-well plates
- Automated liquid handling systems (recommended)
Procedure:
Cell Preparation and Plating:
- Harvest exponentially growing cells using standard tissue culture techniques
- Determine cell count and viability using trypan blue exclusion or automated cell counters
- Prepare cell suspension at optimized density (e.g., 7.5 × 10³ cells/well for 96-well format) [2]
- Plate cells in 100 μL complete medium per well, using interior wells to minimize edge effects
- Incubate plates for 24 hours at 37°C, 5% CO₂ to allow cell attachment
Drug Preparation and Treatment:
- Prepare drug serial dilutions in appropriate solvent, using matched solvent controls for each concentration
- Add drug solutions to cells, ensuring consistent final solvent concentration across all wells
- Include vehicle controls and blank wells without cells for background subtraction
- Incubate drug-treated cells for predetermined time (typically 48-72 hours)
Viability Assessment:
- Add resazurin solution (10% final concentration) directly to cells without medium removal
- Incubate for 2-4 hours at 37°C to allow metabolic conversion
- Measure fluorescence (Ex560/Em590) or absorbance (570/600 nm) using plate reader
- Subtract background signals from cell-free wells
Data Analysis and AI Integration:
- Calculate normalized viability values for each drug concentration
- Generate dose-response curves and compute response metrics (IC50, AUC, GR50)
- Format data for AI/ML model training with appropriate feature representation
3D Drug Sensitivity and Resistance Testing (DSRT) Protocol
The 3D-DSRT protocol enables more physiologically relevant drug sensitivity testing using patient-derived cells (PDCs) in matrix-based culture systems [35].
Materials and Reagents:
- Patient-derived cancer cells or appropriate cell lines
- Growth factor-reduced Matrigel or other 3D culture matrices
- 384-well U-bottom plates for spheroid formation
- Automated dispensing systems for matrix handling
- Luminescence-based viability assay reagents
- High-content imaging systems (optional)
Procedure:
Cell-Matrix Preparation:
- Prepare single-cell suspensions from patient samples or cultured cells
- Mix cells with ice-cold Matrigel at appropriate density (e.g., 500-2000 cells/well)
- Dispense cell-matrix mixture into 384-well plates using chilled tips
- Centrifuge plates briefly to ensure proper well bottom coverage
- Incubate at 37°C for 20-30 minutes to allow matrix polymerization
Culture Maintenance and Drug Treatment:
- Overlay polymerized matrix with appropriate culture medium
- Culture cells for 3-5 days to allow spheroid formation
- Prepare drug dilutions in culture medium
- Carefully remove existing medium and add drug-containing medium
- Incubate for treatment period (typically 72 hours)
Endpoint Analysis:
- Measure cell viability using luminescence-based ATP detection assays
- For additional phenotyping, perform live/dead staining or fix for immunohistochemistry
- Acquire bright-field and fluorescence images using automated microscopy
- Quantify spheroid size, morphology, and viability parameters
Data Processing for AI Modeling:
- Extract multiparametric features from viability and imaging data
- Normalize data to appropriate controls
- Integrate with molecular profiling data (genomic, proteomic) for comprehensive AI analysis
Workflow Visualization
AI-Driven Drug Sensitivity Analysis Workflow
AI-Driven Drug Sensitivity Analysis Workflow - This diagram illustrates the iterative process of integrating experimental data with AI/ML approaches for drug sensitivity prediction, highlighting the continuous feedback loop between model generation and experimental validation.
Experimental Optimization for AI-Ready Data
Experimental Optimization for AI-Ready Data - This workflow details the critical experimental parameters that require optimization to generate high-quality, reproducible data suitable for AI/ML model development in drug sensitivity studies.
Research Reagent Solutions
Essential Materials for AI-Enhanced Drug Sensitivity Research
| Reagent/Material | Function/Application | Optimization Considerations |
|---|---|---|
| Cell Viability Assay Kits (e.g., resazurin, ATP luminescence) | Quantification of cellular response to drug treatment | Validate linear range for each cell line; prefer homogenous assays for high-throughput applications [19] |
| Extracellular Matrix (e.g., Matrigel, synthetic hydrogels) | 3D culture support for physiologically relevant models | Batch variability requires standardization; concentration optimization needed for each cell type [35] |
| Drug Compounds | Therapeutic agents for sensitivity testing | Solvent compatibility; storage stability; evaporation control during assays [2] |
| DMSO Solvent | Vehicle for compound dissolution | Cytotoxicity at high concentrations; use matched controls for each concentration [2] |
| Cell Culture Media | Cellular growth and maintenance | Serum lots can affect drug response; consider defined media for reproducibility [2] |
| Multi-well Plates (384-well, 96-well) | Platform for high-throughput screening | Plate geometry affects edge effects; use tissue culture-treated surfaces for optimal cell attachment [2] |
Regulatory and Validation Considerations
The integration of AI/ML technologies into drug sensitivity testing requires careful attention to regulatory standards and validation approaches. The U.S. Food and Drug Administration (FDA) has developed specific frameworks for AI/ML-based medical devices, emphasizing the importance of good machine learning practices throughout the development lifecycle [88]. For research applications, key considerations include:
- Model Transparency: Implement interpretable AI approaches that provide insight into prediction mechanisms [87]
- Robust Validation: Employ rigorous cross-validation strategies and external validation cohorts to ensure model generalizability
- Bias Mitigation: Address class imbalance and dataset limitations that could introduce prediction biases
- Regulatory Alignment: Consider FDA guidance on predetermined change control plans for AI-enabled devices when developing clinical applications [88]
As AI/ML technologies continue to evolve, their integration with optimized cell culture systems and experimental protocols will play an increasingly important role in advancing predictive drug sensitivity analysis and addressing the critical challenge of treatment resistance in cancer and infectious diseases.
Frequently Asked Questions (FAQs)
Q1: What is the difference between the Z-factor and the Z'-factor? The Z-factor (or Z value) and Z'-factor (Z-prime value) are both used to assess assay quality but are applied at different stages and use different data [89].
- Z'-factor: Used during assay development and validation before testing actual samples. It assesses the assay's inherent quality and signal dynamic range using only positive and negative control data [89].
- Z-factor: Used during or after screening when test samples are included. It evaluates the assay's actual performance with the test compound library, incorporating variation from both the samples and controls [89].
Q2: My Z'-factor is consistently below 0.5. Does this mean my cell-based assay is unusable? Not necessarily. While a Z'-factor > 0.5 is traditionally considered excellent for high-throughput screening (HTS), this strict threshold can be an unwanted barrier for essential but inherently more variable assays, such as cell-based phenotypicscreens [89]. For complex biological systems, a Z'-factor between 0 and 0.5 may still be acceptable. The decision should be made on a case-by-case basis, considering the specific assay context and unmet need [89].
Q3: What are common experimental confounders that can ruin my assay's robustness in drug sensitivity screens? Poor assay robustness often stems from suboptimal experimental design. Key confounders to control for include [2]:
- Evaporation: Significant evaporation from drug storage plates (even at 4°C or -20°C) can concentrate compounds, drastically altering dose-response curves.
- Edge Effect: Cells in perimeter wells of microplates can show elevated signal due to evaporation during incubation, creating a positional bias.
- DMSO Cytotoxicity: The DMSO solvent can itself be cytotoxic at concentrations as low as 1% (v/v), affecting cell viability. Using a single DMSO control for all drug doses can lead to inaccurate results; matched DMSO concentration controls are recommended.
- Drug Storage: Improper storage of diluted drugs can lead to degradation or concentration changes.
Q4: How is robustness testing different from standard assay validation? Robustness testing specifically evaluates how an assay performs under minor, deliberate variations in its parameters or in the presence of invalid inputs [90]. In software and engineering, this involves methods like fault injection, where errors are intentionally introduced to check the system's resilience [90]. For biological assays, it means testing how stable the results are when conditions like reagent concentration, incubation time, or cell passage number are slightly altered. A robust assay should produce consistent results despite these small changes [2].
Troubleshooting Guides
Problem: Low or Negative Z'-factor A low or negative Z'-factor indicates a small signal window (difference between positive and negative controls) and/or high data variability [89].
| Possible Cause | Troubleshooting Steps |
|---|---|
| High Signal Variability | • Check pipetting accuracy and instrument calibration.• Ensure cells are healthy, uniformly seeded, and at an optimal density [2].• Use a high-quality microplate reader with low noise and consistent performance across wells [89]. |
| Small Dynamic Range | • Optimize positive and negative control conditions to maximize the signal difference.• Review reagent concentrations, incubation times, and detection sensitivity.• For cell-based assays, confirm the control compounds are working as intended at the chosen concentration. |
| Assay Not Optimized | Systematically optimize reagents, procedures, and kinetics based on the Z'-factor before screening test compounds [89]. |
Problem: Poor Assay Robustness and Reproducibility Your assay works but gives inconsistent results within a single lab or across multiple laboratories.
| Possible Cause | Troubleshooting Steps |
|---|---|
| Unidentified Confounders | • Perform a variance component analysis to pinpoint major sources of variability (e.g., specific drugs, cell lines, operators) [2].• Implement strict protocols for drug storage (e.g., using sealed plates, avoiding repeated freeze-thaw cycles) to prevent evaporation and degradation [2]. |
| Suboptimal Cell Culture Conditions | • Avoid using serum-free medium if it increases variability; 10% FBS can improve stability without necessarily compromising drug effects [2].• Do not supplement growth medium with antibiotics during drug screening, as they can interact with compounds [2]. |
| Inappropriate Drug Response Metrics | Consider using growth rate inhibition metrics (GR50, GRmax) instead of conventional metrics (IC50, Emax), as they can produce more consistent interlaboratory results by accounting for differences in cellular division rates [2]. |
The table below summarizes common metrics used for assessing assay quality and drug response.
| Metric | Formula / Description | Interpretation and Ideal Range | ||
|---|---|---|---|---|
| Z'-factor [89] | ( Z' = 1 - \frac{3(\sigmap + \sigman)}{ | \mup - \mun | } )( \mu ): mean; ( \sigma ): standard deviation; ( p ): positive control; ( n ): negative control. | 1 > Z' ≥ 0.5: Excellent assay.0.5 > Z' > 0: May be acceptable for complex assays.Z' < 0: Assay is not usable. |
| Z-factor [89] | ( Z = 1 - \frac{3(\sigmas + \sigmac)}{ | \mus - \muc | } )( s ): sample; ( c ): control. | Same interpretation as Z'-factor, but applied during screening with test samples. |
| IC50 [2] | Half-maximal inhibitory concentration; the drug concentration that reduces cell viability by 50%. | A measure of drug potency. Lower IC50 indicates higher potency. Can be variable between labs. | ||
| GR50 [2] | The drug concentration at which the growth rate inhibition is 50%. | A normalized measure of potency that can be more reproducible than IC50. | ||
| AUC [2] | Area Under the dose-response Curve. | A measure of overall drug effect. A smaller AUC indicates greater sensitivity. |
Detailed Experimental Protocol: Z'-Factor Calculation and Assay Optimization
This protocol is adapted for optimizing a cell viability assay, such as the resazurin reduction assay, for drug sensitivity screening [2] [19].
1. Assay Setup and Plate Layout
- Cell Seeding: Plate cells (e.g., MCF7 breast cancer cell line) at an optimized density (e.g., 7.5 × 10³ cells per well in a 96-well plate) in 100 µL of growth medium supplemented with 10% FBS [2].
- Controls: Include positive controls (e.g., cells treated with a cytotoxic drug like 100 µM bortezomib) and negative controls (e.g., cells treated with vehicle only, such as 0.1% DMSO) on each plate. Use a minimum of 12 replicate wells for each control for a reliable Z'-factor calculation [89].
- Plate Handling: To minimize the "edge effect," use microplates designed to reduce evaporation and consider pre-warming plates before adding cells. Fill perimeter wells with PBS only to create a protective barrier [2].
2. Drug Treatment and Incubation
- Drug Preparation: Prepare drug dilutions in advance, but aliquot and store them at -20°C in tightly sealed PCR plates or plates sealed with Parafilm to prevent evaporation. Avoid storing diluted drugs for more than 48 hours [2].
- Vehicle Controls: Use matched DMSO controls. If your drug dilution series uses different final DMSO concentrations (e.g., from 0.001% to 0.1%), include a separate vehicle control for each concentration to account for any DMSO cytotoxicity [2].
- Incubation: Incubate cells with drugs for a predetermined time (e.g., 72 hours) in a humidified incubator at 37°C with 5% CO₂.
3. Viability Measurement (Resazurin Assay)
- Reagent Addition: After drug incubation, add 10-20 µL of a resazurin solution (0.15 mg/mL stock) directly to each well.
- Incubation and Detection: Incubate the plate for 2-4 hours at 37°C. Measure the fluorescence (Excitation ~560 nm, Emission ~590 nm) or absorbance (~570 nm) using a microplate reader. Both detection methods are comparable for the resazurin assay [2].
4. Data Analysis and Z'-Factor Calculation
- Calculate the mean (µ) and standard deviation (σ) of the signals from the positive control (µp, σp) and negative control (µn, σn) wells.
- Apply the values to the Z'-factor formula: Z' = 1 - [ 3(σp + σn) / |µp - µn| ]
- Interpret the result using the table in the "Summary of Key Quantitative Metrics" section above.
Workflow: Assay Development and Quality Control
This diagram outlines the key stages in developing and validating a robust assay, incorporating Z'-factor analysis and robustness testing.
Research Reagent Solutions
This table lists essential materials and their functions for setting up a robust cell viability assay for drug screening.
| Item | Function / Application |
|---|---|
| Resazurin Sodium Salt | A cell-permeable, blue-color redox indicator that is reduced to pink, fluorescent resorufin by metabolically active cells. Used as the readout in cell viability assays [2] [19]. |
| Dimethyl Sulfoxide (DMSO) | A universal solvent for reconstituting most water-insoluble pharmaceutical drugs. Final concentration in assays should be kept low (typically <0.5-1%) to avoid cytotoxicity [2]. |
| Optically Clear Microplates | Flat-bottom, tissue culture (TC)-treated plates are standard for cell-based assays. Use plates designed to minimize evaporation to reduce edge effects [2]. |
| Fetal Bovine Serum (FBS) | Provides essential nutrients, growth factors, and hormones for cell growth. Using medium with 10% FBS can improve assay robustness compared to serum-free medium for some cell lines [2]. |
| Positive Control Compound | A known cytotoxic agent (e.g., Bortezomib, Staurosporine) used to generate the minimum signal in the Z'-factor calculation [89] [2]. |
| Vehicle Control (e.g., PBS) | The solution without the active drug used to generate the maximum signal in the Z'-factor calculation. Also used to fill perimeter wells to minimize evaporation [89] [2]. |
Validating Results Across Platforms and Between Laboratories
Frequently Asked Questions (FAQs)
1. What is the difference between method transfer, cross-validation, and partial validation?
These are distinct but related activities in the method lifecycle:
- Method Transfer: A formal process to implement a fully validated analytical method in a new laboratory (the receiving lab). The goal is to demonstrate that the method performs equivalently in the new environment. The extent of testing can range from a full validation to a comparative side-by-side test, depending on the similarity of operating systems between the originating and receiving labs [91] [92].
- Cross-Validation: This is performed when two or more different methods (e.g., an old method and a new method, or methods from different vendors) are used to generate data for the same study. It ensures that the results from both methods are comparable [91].
- Partial Validation: This is conducted when a modification is made to an already-validated method. The extent of re-validation is based on the risk and significance of the change. Modifications can include changes to the sample preparation procedure, mobile phase composition (for chromatographic assays), or analysis range [91].
2. Why is cell authentication and quality control critical for inter-laboratory studies?
Failure to properly authenticate cell lines and check for contaminants can irreproducibly compromise research data.
- Misidentification & Cross-Contamination: An estimated 16.1% of published papers use problematic cell lines, and the ICLAC register lists over 576 misidentified lines. Cross-contamination by fast-growing cell lines like HeLa is a common problem [45] [93].
- Microbial Contamination: Up to 30% of cell cultures are estimated to be contaminated with mycoplasma, which can escape visual detection and alter cell behavior [45] [93].
- Best Practices: Always source cells from reputable cell banks, perform regular authentication (e.g., STR profiling), and conduct routine checks for mycoplasma and other contaminants [45].
3. What are the key considerations when transferring a cell-based drug sensitivity assay?
Successful transfer of a functional assay like Drug Sensitivity Testing (DST) requires careful planning of pre-analytical and analytical steps [38] [94] [92].
- Cell Source and Handling: Protocols must be optimized for the specific cell type (e.g., primary cells vs. cell lines). Primary cells from hematologic cancers often require specific microenvironmental stimuli (e.g., feeder cells, cytokines) to maintain viability during the assay, which can last up to 72 hours [38].
- Defined Acceptance Criteria: Establish quality controls for the assay itself. This includes setting a minimum viability for negative control wells (e.g., using DMSO) and calculating metrics like the Z-prime factor to ensure the assay's robustness before analyzing drug-treated samples [38].
- Standardized Protocols: Document all procedures in detail, including cell isolation methods, seeding density, drug exposure time, and viability readout method (e.g., CellTiter-Glo) [38] [94].
Troubleshooting Common Validation Issues
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Cell Culture & Pre-Analytics | Poor cell viability in control wells [38] | • Suboptimal culture conditions for primary cells.• Incorrect cell seeding density.• Extended processing time. | • Use specialized medium and essential supplements (e.g., IL-2, IL-6) [38] [95].• Optimize density via growth curve analysis [38].• Implement transient co-culture with feeder cells for primary CLL/MM [38]. |
| Low tumor cell purity from patient samples [94] | • High background of non-tumor cells (e.g., CD45+ immune cells) in samples like malignant pleural effusions. | • Employ negative selection (CD45+ immunomagnetic depletion) or positive selection (EpCAM+ enrichment) [94].• Use a cell strainer for size-based separation [94]. | |
| Assay Performance | High variability between replicates [38] [93] | • Inconsistent cell handling or pipetting.• Microbial contamination.• Edge effects in microplates. | • Standardize protocols and train personnel [96].• Work in laminar flow hoods; routinely screen for mycoplasma [45] [93].• Use plate seals to limit evaporation; calibrate pipettes and dispensers [38] [96]. |
| Assay fails robustness metrics (e.g., low Z-prime) [38] | • Weak signal-to-noise ratio.• Unstable reagent or control wells. | • Include positive (e.g., 100 µM benzethonium chloride) and negative (0.1% DMSO) controls on every plate [38].• Re-optimize cell seeding density and incubation time [38]. | |
| Method Transfer & Data Correlation | Poor correlation between original and receiving lab [91] | • Differences in critical reagent lots or equipment.• Minor but impactful protocol deviations. | • Share common critical reagents if possible, especially for ligand binding assays [91].• Perform a side-by-side comparative test using predefined acceptance criteria [92].• Document all procedures and equipment models in detail [91]. |
Experimental Protocols for Key Validation Activities
Protocol 1: Drug Sensitivity and Resistance Testing (DSRT) for Cell Lines
Adapted from a standardized protocol for hematologic cancer models [38]
Key Research Reagent Solutions:
| Reagent / Material | Function in the Protocol |
|---|---|
| Pre-printed Drug Library (in DMSO) | Provides the test compounds for the screen. |
| CellTiter-Glo Luminescent Assay | Measures cellular ATP as a proxy for cell viability at the endpoint. |
| CO₂ Incubator (5% CO₂, 37°C) | Maintains physiological pH and temperature for cell growth. |
| Liquid Dispenser (e.g., CERTUS Flex) | Ensures accurate and reproducible cell seeding in microplates. |
| 384-well Assay Plates | The standard format for high-throughput drug screening. |
Detailed Methodology:
- Day 1: Preparation of Cells
- For adherent cells, bring into suspension using a gentle detachment agent like Accutase to preserve surface proteins [45].
- Collect cells in a 50 mL tube and centrifuge at 300 g for 5 minutes at room temperature (RT).
- Discard the supernatant, resuspend the cell pellet in fresh, pre-warmed medium, and filter the suspension through a 40 µm cell strainer to ensure a single-cell suspension.
- Count cells and resuspend them in medium to the optimal density previously determined from a growth curve.
- Day 1: Drug Sensitivity and Resistance Testing (DSRT)
- Transfer the cell suspension to the pre-printed drug plates (e.g., 25 µL/well for 384-well plates) using a calibrated liquid dispenser.
- Include positive (e.g., 100 µM benzethonium chloride) and negative (0.1% DMSO) controls on each plate for quality control.
- Optionally, cover the plates with gas-permeable membranes to limit evaporation.
- Incubate the plates for the desired duration (e.g., 72 hours) in a humidified incubator at 5% CO₂ and 37°C.
- Day 4: Measurement of Cell Viability
- Equilibrate the assay plates and the CellTiter-Glo reagent at RT for 15-30 minutes.
- Add an equal volume of CellTiter-Glo reagent to each well (e.g., 25 µL for a 384-well plate).
- Shake the plate on an orbital shaker to induce cell lysis and mix the contents.
- Allow the plate to incubate at RT for 10 minutes to stabilize the luminescent signal.
- Read the luminescence using a plate-reading luminometer.
The workflow for this protocol is summarized in the following diagram:
Protocol 2: Tumor Cell Isolation from Malignant Pleural Effusions for DST
This protocol is tailored for samples with low tumor cell purity [94].
Detailed Methodology:
- Sample Collection and Initial Processing:
- Collect pleural fluid in sterile tubes containing EDTA (10 mM final concentration) to prevent clotting.
- Centrifuge the sample at 800 g for 20 minutes to separate cells from fluid.
- Lyse red blood cells using an appropriate lysis buffer, followed by centrifugation at 500 g for 5 minutes.
- Filter the cell suspension through a 70 µm mesh and either proceed immediately or freeze in 90% FBS/10% DMSO.
- Tumor Cell Identification and Isolation:
- Identify and quantify the tumor cell population using flow cytometry staining for EpCAM (an epithelial cell marker) and CD45 (a pan-hematopoietic marker) [94].
- For isolation, perform repeated rounds of CD45+ immunomagnetic depletion to negatively select for tumor cells. The number of depletion rounds can be adjusted based on the initial percentage of tumor cells in the sample [94].
- After isolation, the enriched tumor cell population is ready for seeding into drug assay plates, as described in Protocol 1.
Validation and Transfer Workflow Diagram
The following diagram outlines the logical relationship and workflow between the key activities in method validation and transfer, from initial setup to final implementation in a new laboratory.
Conclusion
Optimizing cell culture conditions is not merely a technical prerequisite but a fundamental requirement for generating biologically relevant and reproducible drug sensitivity data. This synthesis of foundational knowledge, methodological advancements, troubleshooting strategies, and robust validation metrics provides a comprehensive framework to address the critical issue of experimental reproducibility in preclinical research. The future of the field lies in the wider adoption of physiologically relevant models like 3D organoids, the implementation of improved data normalization methods like the NDR metric, and the integration of AI-driven analysis. These advancements, combined with a rigorous, optimized approach to cell culture, will significantly enhance the predictive power of in vitro drug screens, ultimately accelerating the development of more effective and personalized therapeutic strategies.
References
- 1. A Multi-center Study on the Reproducibility of Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6700527/]
- 2. Optimization of cell viability assays to improve replicability ... [https://www.nature.com/articles/s41598-020-62848-5]
- 3. Cell Culture Troubleshooting [https://www.sigmaaldrich.com/US/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting?srsltid=AfmBOorBtpuMbvTWNiRDDg-pUMJzBhNkXDId7ybTztHSYRDo03HUnutW]
- 4. What's Killing My Cell Cultures? Troubleshooting ... [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/what-is-killing-my-cell-cultures-troubleshooting-cell-growth-issues.html]
- 5. 3D Cell Culture Summit Roadshow 2025 [https://www.corning.com/worldwide/en/products/life-sciences/news-events/events/2025/09/3d-summit-2025.html]
- 6. Optimizing drug sensitivity assays in patient-derived tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11890276/]
- 7. WST-1 Assay: principles, protocol & best practices for cell ... [https://www.abcam.com/en-us/knowledge-center/cell-biology/wst-1-assay-principles-protocols-and-best-practices-for-cell-viability]
- 8. Standard Operating Procedure to Optimize Resazurin- ... [https://www.mdpi.com/2079-6374/14/4/156]
- 9. Cell Viability Assays - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK144065/]
- 10. How to Measure Cell Viability [https://www.promega.com/resources/guides/cell-biology/cell-viability/]
- 11. Optimizing resazurin-based viability assays for P-MSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12100786/]
- 12. The Resazurin Reduction Assay Can Distinguish Cytotoxic ... [https://www.sciencedirect.com/science/article/pii/S2472555222074111]
- 13. Protocol for Single and Combination Drug Screening Using ... [https://pubmed.ncbi.nlm.nih.gov/40106141/]
- 14. Bridging the gap: the role of 3D cell cultures in mimicking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12378905/]
- 15. Metabolism in the tumor microenvironment - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605492/]
- 16. Targeting metabolic pathways in the tumor ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X24000970]
- 17. Constraint based modeling of drug induced metabolic ... [https://www.nature.com/articles/s41540-025-00586-y]
- 18. Cellular interactions within the immune microenvironment ... [https://www.nature.com/articles/s41467-025-56279-x]
- 19. Optimization of Cell Viability Assays for Drug Sensitivity ... [https://pubmed.ncbi.nlm.nih.gov/37142929/]
- 20. Antibacterial Susceptibility Test Interpretive Criteria [https://www.fda.gov/drugs/development-resources/antibacterial-susceptibility-test-interpretive-criteria]
- 21. M100 | Performance Standards for Antimicrobial ... [https://clsi.org/shop/standards/m100/]
- 22. High-content screening [https://en.wikipedia.org/wiki/High-content_screening]
- 23. High content-imaging drug synergy screening identifies ... [https://www.nature.com/articles/s41419-025-07933-1]
- 24. Antibiotic Resistance - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK513277/]
- 25. Machine learning-driven optimization of culture conditions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355708/]
- 26. Protocols | Antimicrobial Resistance [https://www.nature.com/collections/tpqnsjkvhw/protocols]
- 27. High-Content Analysis-Based Sensitivity Prediction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7864197/]
- 28. Antibiotic Resistance Protocols [https://link.springer.com/book/10.1007/978-1-0716-3981-8]
- 29. Is It Time to Start Transitioning From 2D to 3D Cell Culture? [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2020.00033/full]
- 30. Trends and challenges in organoid modeling and expansion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11608026/]
- 31. A 3D spheroid model for assessing nanocarrier-based ... [https://www.nature.com/articles/s44385-025-00041-x]
- 32. Impact of different 3D culture environments on spheroid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570515/]
- 33. 3D Cell Imaging | Best Practices in 3D Cell Culture Imaging [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/the-cutting-edge/best-practices-for-3d-cell-imaging.html]
- 34. Physiologic Patient Derived 3D Spheroids for Anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9894675/]
- 35. Protocol for 3D drug sensitivity and resistance testing of ... [https://www.sciencedirect.com/science/article/pii/S2472555222137081]
- 36. Frontiers | Advancements and challenges in culturing patient - derived ... [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2025.1663420/full]
- 37. Colorectal Cancer Patientâ€Derived 2D and 3D Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9353492/]
- 38. Standardized assays to monitor drug sensitivity in ... [https://www.nature.com/articles/s41420-023-01722-5]
- 39. A Universal Gelfoam 3-D Histoculture Method to Establish... [https://pubmed.ncbi.nlm.nih.gov/33288569/]
- 40. Reliable anti-cancer drug sensitivity prediction and ... [https://www.nature.com/articles/s41598-024-62956-6]
- 41. How Do I Perform a Dose-Response Experiment? [https://www.graphpad.com/support/faq/how-do-i-perform-a-dose-response-experiment/]
- 42. Setting up a Dose Response Protocol - CDD Support [https://support.collaborativedrug.com/hc/en-us/articles/214359303-Setting-up-a-Dose-Response-Protocol]
- 43. Cell Culture FAQs [https://lifescience.invitro.com.au/l/cell-culture-faqs]
- 44. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 45. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 46. Optimal experimental designs for dose–response studies with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4655015/]
- 47. How Automation Overcomes Variability & Limitations in ... [https://dispendix.com/blog/how-automation-overcomes-variability-limitations-in-hts-troubleshooting]
- 48. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 49. Advances in high throughput cell culture technologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11135158/]
- 50. HTS Assay Validation - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK83783/]
- 51. A microfluidic platform for the co-culturing of microtissues with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12514218/]
- 52. Mammalian cell culture and analysis in digital microfluidic ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00250h]
- 53. Automated microfluidic platform for dynamic and ... [https://www.nature.com/articles/s41467-020-19058-4]
- 54. Microfluidic Platforms for Organ-on-a-Chip Models [https://www.sciencedirect.com/science/article/abs/pii/S2468451125000558]
- 55. Why can your cytometry results be wrong without you ... [https://immunostep.com/2025/05/02/why-can-your-cytometry-results-be-wrong-without-you-knowing-it/]
- 56. Microfluidics in 2025: Applications, Trends & How It Work [https://eden-microfluidics.com/news-events/microfluidics-overview/]
- 57. Recent Advances on Cell Culture Platforms for In Vitro Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11468737/]
- 58. Seeding, Subculturing, and Maintaining Cells [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/maintaining-cultured-cells.html]
- 59. Cell Seeding Essentials: Strategies for Lab Success [https://opentrons.com/applications/cell-seeding?srsltid=AfmBOopNXon2qnX1DjV9f-hO3ztbWFZ5xS3KyFr2d2i3F87BqtmkVtsn]
- 60. Monitor Uniform Cell Seeding Density in Plates and Wells [https://www.revvity.com/ask/monitor-uniform-cell-seeding-density-in-plates-and-wells]
- 61. Cell Culture Troubleshooting [https://www.merckmillipore.com/SB/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting]
- 62. A high-throughput media design approach for high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4169041/]
- 63. How to Conquer Edge Effect in TC Plates [https://gmpplastic.com/blogs/useful-articles-on-lab-supplies-faq-section/how-to-conquer-edge-effect-in-tc-plates?srsltid=AfmBOorlBmOCliKaTFYexfi0uwJW5NpFSdab2caiiUosnnPnqh1ZxgQd]
- 64. Three Ways To Reduce Microplate Edge Effect - WellPlate.com [https://www.wellplate.com/three-ways-reduce-microplate-edge-effect/]
- 65. Eliminating Edge Effect in Cell Culture Plates [https://midsci.com/resources/blog/eliminatingedgeeffect.tpp/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYwcjTwMgw0C3J29jQ0CXU2MDAzdnA0NTI30w8EKDHAARwP9KGL041EQhd94L0IWAH1gVOTr7JuuH1WQWJKhm5mXlq8fkZqTmZuZB_RlXnpqSnpqalpaanKJXklBAdBBUXiNNDSEKsDjqILc0Igqn7RgT0dFRQD-Q1RW/dz/d5/L2dJQSEvUUt3QS80TmxFL1o2XzIyQTJIMVMwUEdDSzMwUUU0MjAxRkMxMDUy/?srsltid=AfmBOooM8rPqZXvX7N5aJ6clAvsU8WEL-djsGqcJqKmlUE7fCZMKlMc0]
- 66. A global problem. The trouble with culturing cells in 96-well ... [https://www.sciencedirect.com/science/article/pii/S2405580821000819]
- 67. The Edge Effect in High-Throughput Proteomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC10251511/]
- 68. Spatial artifact detection improves the reproducibility of drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570324/]
- 69. Unexpected low-dose toxicity of the universal solvent DMSO [https://pubmed.ncbi.nlm.nih.gov/24327606/]
- 70. Out of control: The need for standardised solvent ... [https://www.sciencedirect.com/science/article/pii/S2590207522000156]
- 71. Biology-aware machine learning for culture medium ... [https://www.sciencedirect.com/science/article/pii/S1871678425000731]
- 72. Accelerating cell culture media development using ... [https://www.nature.com/articles/s41467-025-61113-5]
- 73. Low-cost food-grade alternatives for serum albumins ... [https://pubmed.ncbi.nlm.nih.gov/40312489/]
- 74. Measuring Cancer Drug Sensitivity and Resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5538315/]
- 75. Cell Culture Troubleshooting [https://www.sigmaaldrich.com/US/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting?srsltid=AfmBOopnQEqZHQ0G1htkGCR1KI3kZQUrJ73RDdmpR6C28wIP77c6yhGw]
- 76. Cooperative nutrient accumulation sustains growth of mammalian cells | Scientific Reports [https://www.nature.com/articles/srep17401]
- 77. Rapid nutrient depletion to below the physiological range by cancer cells cultured in Plasmax - PubMed [https://pubmed.ncbi.nlm.nih.gov/35876286/]
- 78. Spandidos Publications: Oncology Reports [https://www.spandidos-publications.com/10.3892/or.2019.7125]
- 79. Growth rate inhibition metrics correct for confounders in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4887336/]
- 80. Growth rate inhibition metrics correct for confounders in ... [https://lincs.hms.harvard.edu/hafner-natmethods-2016/]
- 81. Development and validation of the Normalized Organoid ... [https://www.nature.com/articles/s42003-024-07329-5]
- 82. 50% of what? How exactly are IC50 and EC50 defined? [https://www.graphpad.com/support/faq/50-of-what-how-exactly-are-ic50-and-ec50-defined/]
- 83. A normalized drug response metric improves accuracy and ... [https://www.nature.com/articles/s42003-020-0765-z]
- 84. A normalized drug response metric improves accuracy and ... [https://pubmed.ncbi.nlm.nih.gov/31974521/]
- 85. Advancements in AI-driven drug sensitivity testing research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081381/]
- 86. A quantum machine learning framework for predicting drug ... [https://www.nature.com/articles/s41598-025-06544-2]
- 87. Prediction of anticancer drug sensitivity using an interpretable ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-024-05669-x]
- 88. Artificial Intelligence in Software as a Medical Device [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-software-medical-device]
- 89. The Z prime value (Z´) [https://www.bmglabtech.com/en/blog/the-z-prime-value/]
- 90. Robustness testing [https://en.wikipedia.org/wiki/Robustness_testing]
- 91. Method Transfer, Partial Validation, and Cross Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC4389741/]
- 92. Points to Consider in Quality Control Method Validation ... [https://www.bioprocessintl.com/qa-qc/points-to-consider-in-quality-control-method-validation-and-transfer]
- 93. Cell Culture Troubleshooting [https://www.sigmaaldrich.com/US/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting?srsltid=AfmBOooQrbAdRu0NYQu4hTcWi3_iUl7SGebsrTmoOJO8iO5JZ4xZv2Di]
- 94. Evaluation and modification of tumor cell isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420342/]
- 95. How to Optimize Cell Culture Media for High-Yield ... [https://cellculturecompany.com/how-to-optimize-cell-culture-media-for-high-yield-recombinant-protein-production-in-mammalian-cells/]
- 96. How to Optimize Cell Culture [https://gmpplastic.com/blogs/useful-articles-on-lab-supplies-faq-section/how-to-optimize-cell-culture?srsltid=AfmBOopdSLkkdeNyJ6dCHbqaxL6lk87QR9gSm8qnVnGaG_v_8j0_f_uI]