Pharmacogenomics in Personalized Medicine: Integrating Genomic Data to Revolutionize Drug Development and Clinical Practice
This article examines the transformative role of pharmacogenomics in advancing personalized medicine for researchers, scientists, and drug development professionals.
Pharmacogenomics in Personalized Medicine: Integrating Genomic Data to Revolutionize Drug Development and Clinical Practice
Abstract
This article examines the transformative role of pharmacogenomics in advancing personalized medicine for researchers, scientists, and drug development professionals. It explores the foundational principles connecting genetic variation to individual drug responses, methodologies for clinical implementation across therapeutic areas, strategies to overcome economic and technological barriers, and validation through global regulatory frameworks and cost-effectiveness analyses. The synthesis provides a comprehensive roadmap for integrating pharmacogenomics into drug development pipelines and clinical care to enhance therapeutic efficacy and patient safety.
Genetic Foundations of Variable Drug Response: From Historical Observations to Genomic Mechanisms
Defining Pharmacogenomics within the Precision Medicine Paradigm
Pharmacogenomics (PGx) is a foundational component of precision medicine, dedicated to understanding how an individual's genetic makeup influences their response to medications [1]. The field moves clinical practice away from a "one-size-fits-all" model toward a personalized approach, optimizing drug selection and dosing to maximize efficacy and minimize adverse effects [2]. This paradigm shift is driven by the recognition that genetic polymorphisms in genes encoding drug-metabolizing enzymes, transporters, and targets are a major source of interindividual variability in drug response [3] [4]. The ultimate goal of pharmacogenomics is to replace the traditional trial-and-error method of prescribing with genetically informed, precision prescribing, thereby improving therapeutic outcomes and enhancing patient safety [2].
The clinical significance of pharmacogenomics is profound. For instance, an analysis of the 100,000 Genomes Project revealed that 62.7% of individuals carried an actionable pharmacogenetic variant, suggesting that 6% to 10% of people could benefit from genotype-guided dose adjustments or alternative drug regimens to achieve safer and more effective therapy [3]. Furthermore, real-world implementation studies have demonstrated that genotype-guided treatment can reduce the incidence of adverse drug events by up to 30% [5]. As genomic sequencing technologies continue to evolve, the integration of pharmacogenomic data into routine medical practice represents a significant advancement toward more personalized and effective treatment strategies across a wide range of therapeutic areas [3].
Core Principles and Genetic Architecture
Fundamental Terminology and Concepts
A standardized set of terms is essential for interpreting pharmacogenomic test results and clinical guidelines. Key concepts and nomenclature are defined below.
- Allele: One of two or more versions of a gene. An individual inherits two alleles for each gene, one from each parent [6].
- Diplotype: The combination of the two alleles (maternal and paternal) inherited by an individual for a particular gene. The diplotype is used to predict the drug-metabolizing phenotype [6] [5].
- Genotype: An individual's complete collection of genetic variants [6].
- Phenotype: The observable characteristic of an individual's ability to metabolize a drug, determined by their genotype (e.g., poor metabolizer, normal metabolizer) [6].
- Star (*) Allele Nomenclature: A standardized system for naming pharmacogenomic alleles. Alleles are designated by a gene symbol followed by an asterisk and a number (e.g.,
CYP2C19*2). This system accounts for all variants within a single haplotype, simplifying the reporting of complex genetic variation [6] [5].
From Genetic Variation to Clinical Presentation
The pathway from genetic variation to clinical outcome involves a structured translation process, illustrated below and detailed in the subsequent sections.
1. Genotype to Phenotype Translation The diplotype is translated into a predicted phenotype, which categorizes an individual's metabolic capacity [6] [5]. The major phenotypic categories are defined in Table 1.
Table 1: Standardized Pharmacogenomic Phenotype Definitions and Clinical Implications
| Metabolizer Status (Phenotype) | Functional Definition | Example Genotype (CYP2D6) | Example Clinical Recommendation (for Codeine) |
|---|---|---|---|
| Ultrarapid Metabolizer | Increased enzyme activity | *1/*1x2 (duplication of normal function allele) |
Avoid use due to potential for serious toxicity (increased conversion to morphine) [6]. |
| Normal Metabolizer | Fully functional enzyme activity | *1/*1 (two normal function alleles) |
Use label-recommended dosing [6]. |
| Intermediate Metabolizer | Decreased enzyme activity | *1/*5 (one normal, one no function allele) |
Use label-recommended dosing [6]. |
| Poor Metabolizer | Little to no enzyme activity | *4/*5 (two no function alleles) |
Avoid use due to possibility of diminished analgesia (lack of conversion to morphine) [6]. |
2. Phenotype to Clinical Action The predicted phenotype is used to generate specific clinical recommendations for drug selection and dosing, as outlined in guidelines from consortia like the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the Dutch Pharmacogenetics Working Group (DPWG) [1] [5]. For example, the CPIC guideline for the opioid codeine, which is a prodrug activated by CYP2D6, recommends avoiding its use in both ultrarapid metabolizers (risk of toxicity) and poor metabolizers (lack of efficacy) [6] [3].
Key Molecular Players and Clinical Applications
Major Pharmacogenes and Drug Metabolism Pathways
The most critical genes in pharmacogenomics include those encoding cytochrome P450 (CYP) enzymes, which are involved in the phase I metabolism of an estimated 70-80% of all commonly prescribed drugs [3] [4]. Polymorphisms in these genes lead to distinct metabolic phenotypes with direct clinical consequences, as shown in Table 2.
Table 2: Major Pharmacogenes, Their Drug Substrates, and Clinical Consequences of Variation
| Gene | Example Drugs | Clinical Impact of Genetic Variation |
|---|---|---|
| CYP2C19 | Clopidogrel, proton pump inhibitors (e.g., omeprazole), antidepressants [3] | Poor metabolizers show reduced efficacy of clopidogrel, increasing risk of stent thrombosis and major adverse cardiac events [7] [2]. |
| CYP2D6 | Codeine, tramadol, tamoxifen, antidepressants, antipsychotics [3] | Ultrarapid metabolizers of codeine produce toxic morphine levels, risking fatal respiratory depression, especially in children [6] [3]. |
| CYP2C9 | Warfarin, siponimod, NSAIDs [3] [8] | Variants increase bleeding risk with warfarin; require genotype-guided dosing [9] [8]. |
| TPMT, NUDT15 | Thiopurines (mercaptopurine, thioguanine) [3] [8] | Poor metabolizers at high risk for severe, life-threatening myelosuppression; require drastic dose reduction or alternative agents [8]. |
| DPYD | Fluoropyrimidines (5-fluorouracil, capecitabine) [3] | Deficiency in the encoded enzyme predicts severe and potentially fatal toxicity; requires dose adjustment or alternative therapy [3] [10]. |
| HLA-B | Carbamazepine, allopurinol, abacavir [1] [8] | Specific alleles (e.g., HLA-B*15:02 for carbamazepine) confer high risk for life-threatening cutaneous adverse reactions like Stevens-Johnson Syndrome [1]. |
Analytical Methods and Experimental Protocols
Standard Genotyping and Star Allele Calling
The standard methodology for determining an individual's pharmacogenotype involves targeted genotyping or next-generation sequencing (NGS), followed by computational star allele calling.
Detailed Experimental Protocol:
- Sample Preparation & Sequencing: Extract genomic DNA from a patient specimen (e.g., blood, saliva). For NGS, prepare a sequencing library, which may involve enrichment for a panel of pharmacogenes. Sequence the DNA using a high-throughput platform [5].
- Data Pre-processing: Align the resulting sequencing reads (in FASTQ format) to a reference genome (e.g., GRCh38) using alignment algorithms like BWA-MEM. Process the aligned data (BAM files) by sorting, indexing, and marking duplicates using tools like Samtools and Picard [5].
- Star Allele Calling: Analyze the pre-processed BAM files using specialized computational tools to determine the star allele diplotype. Commonly used tools include:
- Aldy: A versatile tool that can handle complex structural variations and copy number variants [5].
- PyPGx: A Python-based toolkit that supports a wide range of pharmacogenes and provides phenotype prediction [5].
- StellarPGx: Another robust caller designed for accurate diplotype assignment [5]. It is considered best practice to use at least two callers for cross-validation due to the complexity of some pharmacogenes [5].
- Phenotype and Recommendation Assignment: Translate the consensus diplotype into a phenotype using standardized tables (see Table 1). Apply evidence-based clinical guidelines (e.g., from CPIC) to generate a therapeutic recommendation [5].
Addressing the Dynamic Nature of Nomenclature
A critical consideration in PGx research and testing is the dynamic nature of the star allele nomenclature. The Pharmacogene Variation Consortium (PharmVar) serves as the central repository for allele definitions, which are continuously updated as new alleles are discovered and characterized [6] [5]. Between early version 1.1.9 and version 6.2, the PharmVar database added 471 core alleles and redefined or removed 49 others [5]. This evolution means that an individual's diplotype call can change over time if different database versions are used, which can, in rare cases, alter clinical recommendations. Researchers must document the PharmVar version used and implement cross-tool validation to ensure the reliability of their results [5].
A successful PGx research program relies on a suite of key databases, software tools, and biological reagents, detailed in Table 3.
Table 3: The Scientist's Toolkit: Key Resources for Pharmacogenomics Research
| Resource Name | Type | Primary Function and Utility |
|---|---|---|
| PharmVar (Pharmacogene Variation Consortium) | Database | The authoritative repository for the definitive star (*) allele nomenclature sequences and functional annotations for major pharmacogenes [6] [5]. |
| PharmGKB (Pharmacogenomics Knowledgebase) | Database | Curates knowledge about the impact of genetic variation on drug response, including clinical guidelines (CPIC, DPWG), drug labels, and variant annotations [1] [9]. |
| CPIC (Clinical Pharmacogenetics Implementation Consortium) | Guideline Body | Provides freely available, evidence-based, peer-reviewed guidelines for translating genetic test results into actionable prescribing decisions [1] [9] [8]. |
| GeT-RM (Genetic Testing Reference Materials) | Biological Reagents | Provides robust, characterized reference materials and cell lines for benchmarking and validating pharmacogenomic genotyping assays [5]. |
| Aldy, PyPGx, StellarPGx | Software Tool | Computational tools for determining star allele diplotypes from next-generation sequencing data (BAM/FASTQ files) [5]. |
| UK Biobank, All of Us | Biobank / Data Resource | Large-scale, EHR-linked biobanks with genomic data that enable discovery of novel drug-gene associations and investigation of PGx in real-world populations [9] [10]. |
Current Challenges and Future Directions
Despite its potential, the widespread clinical implementation of pharmacogenomics faces several significant barriers. Key challenges, as identified in recent literature, are summarized in Table 4 alongside proposed solutions.
Table 4: Barriers to Clinical Implementation of Pharmacogenomics and Potential Solutions
| Domain | Cited Barrier | Proposed Solution |
|---|---|---|
| Equity and Inclusion | Underrepresentation of diverse populations in PGx research and implementation; can introduce healthcare disparities and weaken evidence [9]. | Increase genetic diversity in research cohorts (e.g., All of Us); implement pan-ethnic testing panels that include alleles common in all populations [9]. |
| Evidence and Guidelines | Insufficient evidence for some drug-gene pairs; genetic exceptionalism demanding RCTs for every use case [9] [7]. | Incorporate different forms of evidence (e.g., mechanistic, pharmacokinetic); disseminate guidelines to frontline clinicians [9]. |
| Clinical Integration | Lack of EHR integration and clinical decision support (CDS); clinician resistance and knowledge gaps [9] [4]. | Develop and adopt data standards for genomic information in EHRs; expand competency-based education for healthcare professionals [9] [2]. |
| Payer Coverage & Reimbursement | Sparse, inconsistent, or absent insurance coverage for multigene panels and preemptive testing [9] [7] [4]. | Establish uniform evidence thresholds for coverage; demonstrate cost-effectiveness through robust health economics studies [9] [7]. |
Emerging technologies are poised to address some of these challenges. Long-read sequencing provides contiguous reads that span tens of kilobases, enabling comprehensive mapping of highly polymorphic and complex genes like CYP2D6, which is prone to gene duplications and hybrid alleles that are difficult to detect with short-read technologies [10]. Artificial intelligence and machine learning are being deployed to analyze complex, multi-dimensional datasets, predict the functional impact of genetic variants from sequence data alone, and even forecast individual drug response based on integrated multi-omics profiles [10]. The integration of polygenic risk scores (PGS), which aggregate the effects of many variants across the genome, represents a move beyond single gene-drug interactions to predict more complex treatment outcomes for conditions like type 2 diabetes and schizophrenia [10].
Pharmacogenomics stands as a critical and rapidly advancing pillar of precision medicine. By deciphering the genetic determinants of drug response, it provides a powerful framework for replacing empirical prescribing with a more predictive, personalized approach. The field has established a robust foundation of key genes and alleles, standardized nomenclature, and evidence-based guidelines for an growing number of drug-gene pairs. While challenges related to diversity, clinical implementation, and reimbursement remain active areas of work, technological innovations in sequencing, data integration, and analytics are accelerating the field's progress. The continued collaboration between researchers, clinicians, and policymakers is essential to overcome these hurdles, ensuring that the promise of pharmacogenomics—to deliver the right drug at the right dose to every patient—becomes a ubiquitous and equitable reality in healthcare.
Pharmacogenomics is the study of how an individual's entire genome influences their response to drugs, playing a pivotal role in the development of personalized medicine [11]. The foundation of drug response rests on two core principles: pharmacokinetics and pharmacodynamics.
- Pharmacokinetics describes what the body does to a drug, encompassing the processes of Absorption, Distribution, Metabolism, and Excretion (ADME) [12].
- Pharmacodynamics describes what the drug does to the body, involving the drug's biological effects on its target, such as a receptor or enzyme [12].
Genetic variations can alter both of these processes, accounting for 20% to 95% of inter-individual variability in drug metabolism and response [11]. Understanding these genetic influences is essential for tailoring therapies to maximize efficacy and minimize adverse effects, thereby fulfilling the promise of personalized medicine.
Genetic Influences on Pharmacokinetics (ADME)
Pharmacokinetic interactions determine how a drug is processed by the body. Genetic polymorphisms, particularly in genes encoding drug-metabolizing enzymes and transporters, can significantly alter this processing, leading to variable drug concentrations and, consequently, variable therapeutic outcomes [12].
Key Enzymes and Genetic Variants in Drug Metabolism
The cytochrome P450 (CYP450) enzyme family is responsible for metabolizing the majority of drugs [11]. Polymorphisms in the genes coding for these enzymes can profoundly influence drug response, causing it to be normal, increased, reduced, or completely neutralized [11]. These genetic variations give rise to distinct metabolic phenotypes.
Table: Pharmacogenomic Biomarkers in Drug Metabolism
| Gene | Metabolism Phenotype | Clinical Implication | Example Drugs |
|---|---|---|---|
| CYP2D6 | Ultra-rapid Metabolizer (UM) | Reduced drug efficacy; for prodrugs, risk of toxicity | Codeine, Tamoxifen, Tricyclic antidepressants [12] [11] |
| Poor Metabolizer (PM) | Increased risk of side effects | ||
| CYP2C19 | Poor Metabolizer (PM) | Reduced activation of prodrug, risk of therapeutic failure | Clopidogrel, Proton pump inhibitors [11] [13] |
| CYP2C9 | Poor Metabolizer (PM) | Reduced metabolism, risk of toxicity and dosing variability | Warfarin, Phenytoin [11] |
| DPYD | Poor Metabolizer (PM) | Severe toxicity due to drug accumulation | Capecitabine, Fluorouracil [13] |
The clinical impact of being a slow metabolizer depends on the drug's properties. For active drugs, slow metabolism leads to accumulation and increased risk of toxicity. For prodrugs (inactive compounds that require metabolic activation), slow metabolism can result in therapeutic failure due to insufficient formation of the active compound [13]. A prime example is clopidogrel, where patients with CYP2C19 poor metabolizer status produce low levels of the active metabolite, leading to a higher risk of cardiovascular events [11] [13].
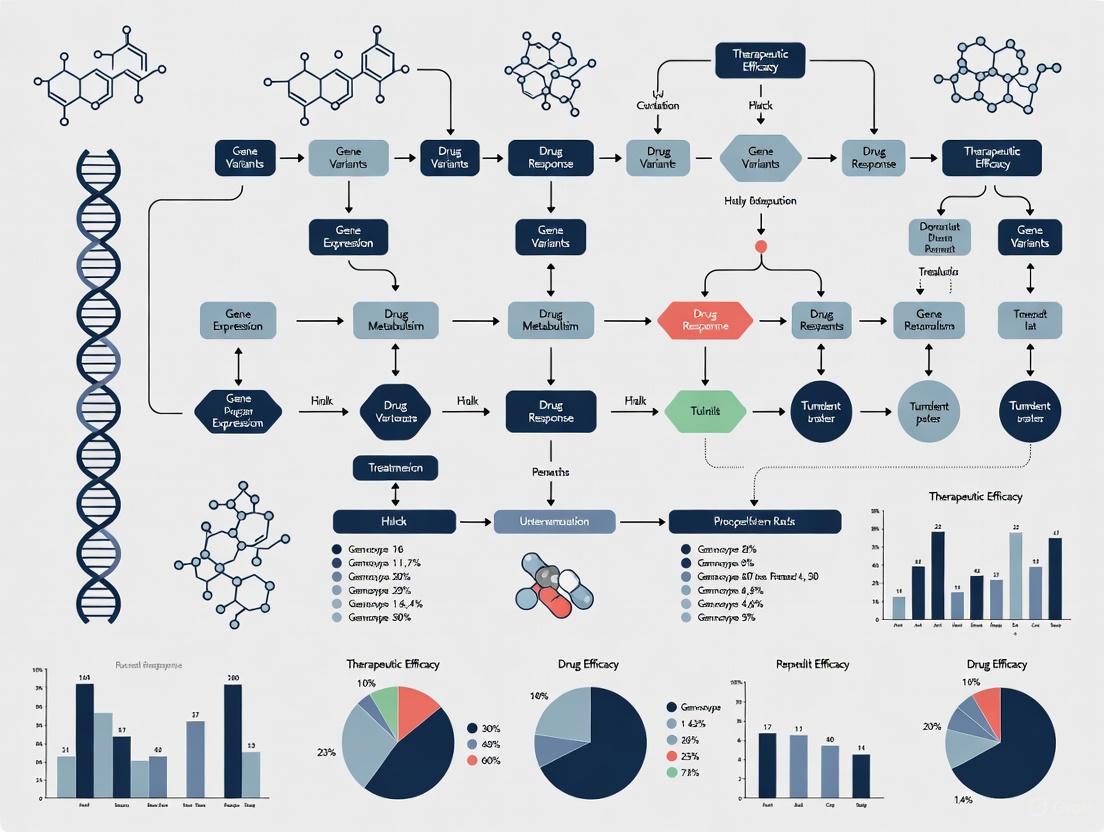
Diagram 1: The pathway from genetic variant to altered drug response via pharmacokinetics.
Genetic Influences on Pharmacodynamics
While pharmacokinetics deals with drug exposure, pharmacodynamics concerns the drug's effect on the body, including its therapeutic action and the risk of adverse reactions [12]. Genetic variants can alter the structure or function of a drug's target (e.g., a receptor or enzyme), changing the body's sensitivity to the drug irrespective of its concentration.
A key example involves the drug warfarin. Variants in the VKORC1 gene, which encodes the drug's target enzyme (vitamin K epoxide reductase), affect the drug's pharmacodynamics. These variants influence the enzyme's sensitivity to warfarin, directly impacting the required dosage [12] [11]. Another critical pharmacodynamic mechanism involves the human leukocyte antigen (HLA) genes. Specific variants, such as HLA-B1502, are strongly associated with an increased risk of severe hypersensitivity reactions like Stevens-Johnson syndrome in patients taking carbamazepine [11].
Table: Pharmacogenomic Biomarkers in Drug Targets and Safety
| Gene | Drug | Effect of Variant | Mechanism |
|---|---|---|---|
| VKORC1 | Warfarin | Altered dosing requirement | Pharmacodynamic: Alters sensitivity of drug target [12] [11] |
| HLA-B | Carbamazepine | Increased risk of severe skin reactions (SJS/TEN) | Pharmacodynamic: Alters immune-mediated drug reaction [11] |
| ERBB2 (HER2) | Trastuzumab | Determines drug eligibility and efficacy | Pharmacodynamic: Target overexpression drives drug efficacy [14] |
Integrating PK and PD: The Combined Genetic Influence
For many drugs, the overall response is a complex interplay of multiple genetic factors affecting both pharmacokinetics and pharmacodynamics. Warfarin provides a classic example of this dual influence, where dosing is affected by:
- Pharmacokinetic Gene: CYP2C9 variants affect the rate of warfarin metabolism [12] [11].
- Pharmacodynamic Gene: VKORC1 variants affect the sensitivity of the drug target [12] [11].
This multi-gene influence underscores the necessity of a comprehensive pharmacogenomic approach to accurately predict drug behavior, moving beyond single-gene tests to multi-gene panels for complex medications.
Diagram 2: The combined pharmacokinetic and pharmacodynamic genetic influences on warfarin dosing.
Experimental and Methodological Approaches
Research and clinical implementation in pharmacogenomics rely on robust methodologies to connect genetic variation to drug response phenotypes.
Genotyping and Sequencing Methodologies
The foundation of pharmacogenomic testing is identifying relevant genetic variants. These include:
- Single Nucleotide Polymorphisms (SNPs): Single base-pair substitutions that account for 90% of all human genetic variation [11]. The location of an SNP determines its functional impact.
- Structural Variations (SVs): Less frequent than SNPs but with greater functional consequences, SVs include insertions/deletions ("indels") and copy number variations (CNVs), which can lead to nonfunctional proteins [11].
Modern approaches often utilize multigene pharmacogenetic tests that simultaneously interrogate a panel of key genes (e.g., CYP2C9, CYP2C19, CYP2D6, VKORC1, DPYD) to provide a comprehensive profile. Adhering to recommendations from bodies like the Association for Molecular Pathology (AMP) ensures tests cover clinically relevant variants [9].
Phenotyping and Clinical Correlation
Linking genotype to a predicted phenotype is a critical step. For metabolic enzymes, this involves classifying individuals into one of four primary phenotypes:
- Poor Metabolizer (PM): Greatly reduced or absent enzyme activity.
- Intermediate Metabolizer (IM): Reduced enzyme activity.
- Normal/Extensive Metabolizer (EM): Standard enzyme activity.
- Ultra-rapid Metabolizer (UM): Increased enzyme activity [11].
The clinical interpretation of these phenotypes is standardized and disseminated through guidelines from consortia like the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the Dutch Pharmacogenetics Working Group (DPWG). These guidelines translate genetic test results into actionable clinical recommendations, such as "use an alternative drug" or "increase dose by 50%" [9].
Table: Essential Research Reagents and Resources
| Reagent / Resource | Function in PGx Research | Example / Specification |
|---|---|---|
| DNA Sequencing Kits | Extract DNA and identify genetic variants from patient samples (blood/saliva) [13] | Whole genome sequencing, Targeted SNP panels |
| CPIC Guidelines | Translate genotype into actionable phenotype and prescribing guidance [9] | CPIC Guideline for Codeine (CYP2D6) |
| FDA Table of Biomarkers | Identify clinically recognized drug-gene pairs with regulatory backing [14] | FDA Biomarker Table (e.g., HLA-B*1502 & Carbamazepine) |
| PharmGKB | Curated knowledgebase of drug-gene relationships, evidence levels, and clinical guidelines [9] | PharmGKB.org |
| Phenotyping Assays | Functional validation of metabolic activity (e.g., via probe drugs) | CYP activity measured in hepatocytes or via metabolite ratio |
Implementation in Personalized Medicine and Current Challenges
The integration of pharmacogenomics into routine clinical practice is a central goal of personalized medicine. Its implementation allows clinicians to:
- Select the most effective drug for an individual.
- Optimize drug dosage from the outset.
- Avoid drugs with a high risk of severe adverse reactions for particular patients [13].
Significant progress has been made, with the FDA including pharmacogenomic biomarkers in the labeling for over 100 drugs, providing official recognition of their clinical importance [14]. However, several barriers to widespread adoption remain, including:
- Evidence and Guidelines: Insufficient evidence for some drug-gene pairs and the need for incorporation into broader medical society guidelines [9].
- Education: A lack of knowledge and confidence in using pharmacogenetic information among healthcare providers [9].
- Equity and Inclusion: The underrepresentation of diverse populations in pharmacogenetics research, which can lead to disparities in clinical utility and healthcare outcomes [9].
The genetic influences on the core principles of pharmacokinetics and pharmacodynamics are a fundamental determinant of inter-individual drug response. The integration of this knowledge into drug development and clinical practice, through genotyping, phenotyping, and the application of clinical guidelines, is transforming the paradigm from a "one-size-fits-all" approach to a more effective and safer model of personalized medicine. Overcoming the remaining implementation challenges, particularly those related to evidence generation and health equity, is critical to fully realizing the potential of pharmacogenomics to improve patient outcomes.
In the field of personalized medicine, pharmacogenomics stands as a cornerstone, providing the scientific foundation for understanding how individual genetic makeup influences drug response. This technical guide examines the key genetic polymorphisms within the cytochrome P450 (CYP) superfamily and membrane transporter genes, which collectively govern the pharmacokinetics and pharmacodynamics of a substantial proportion of clinically used drugs. Research demonstrates that genetic variants in these proteins explain 20-30% of interindividual differences in drug response, contributing significantly to both adverse drug reactions and therapeutic failures [15]. The clinical implementation of this knowledge is evidenced by the inclusion of pharmacogenomic information in over 390 drug labels by the U.S. Food and Drug Administration [14]. This whitepaper provides researchers and drug development professionals with a comprehensive technical resource on these critical pharmacogenomic elements, framing them within the broader context of advancing personalized treatment strategies.
The Cytochrome P450 (CYP) Superfamily
Clinical Significance and Genetic Architecture
The CYP superfamily comprises 57 functional enzymes in humans that metabolize more than 80% of all clinically used medications [15]. These hemoprotein enzymes catalyze the oxidation of numerous drugs, facilitating their elimination from the body. Among these, CYP2D6 and CYP2C19 are of paramount clinical importance due to their extensive polymorphism, broad substrate specificity, and significant impact on drug disposition and response.
CYP2D6 metabolizes approximately 25% of commonly prescribed drugs, including numerous antidepressants (paroxetine, fluvoxamine, amitriptyline), antipsychotics (haloperidol, risperidone), beta-blockers, antiemetics, and opioids [16] [15]. The CYP2C19 enzyme metabolizes drugs including the antiplatelet agent clopidogrel, tricyclic antidepressants (amitriptyline, clomipramine), selective serotonin reuptake inhibitors (citalopram, sertraline), and the antifungal voriconazole [16] [15].
These genes are highly polymorphic, with the Pharmacogene Variation Consortium categorizing 129 known allelic variants for CYP2D6 and 35 clinically relevant variants for CYP2C19 [16]. These polymorphisms result in distinct metabolic phenotypes, classified for CYP2C19 as ultrarapid metabolizers (UM), rapid metabolizers (RM), normal metabolizers (NM), intermediate metabolizers (IM), and poor metabolizers (PM); and for CYP2D6 as UM, NM, IM, and PM [16].
Key Polymorphisms and Functional Consequences
The most clinically significant polymorphisms and their functional impacts are summarized in the table below.
Table 1: Key CYP Gene Polymorphisms and Functional Consequences
| Gene | Key Variant(s) | Functional Effect | Molecular Consequence | Clinical Impact |
|---|---|---|---|---|
| CYP2C19 | *2 (rs4244285) | Loss-of-function | Aberrant splicing, premature stop codon [15] | Reduced activation of clopidogrel; altered antidepressant exposure |
| *17 (rs12248560) | Increased function | Regulatory polymorphism increasing transcriptional activity [15] | Potential therapeutic failure due to rapid metabolism; requires dose adjustment | |
| CYP2D6 | *3 (rs35742686), *4 (rs3892097), *5 (gene deletion), *6 (rs5030655) | Loss-of-function | Frameshift, splicing defect, gene deletion, base change [16] | Increased drug exposure and toxicity risk for substrates including tricyclic antidepressants and codeine |
| *41 (rs28371725) | Reduced function | Splicing defect [16] | Intermediate metabolizer phenotype | |
| *1xN, *2xN (gene duplication) | Increased function | Multiple functional gene copies [15] | Ultrarapid metabolism; potential therapeutic failure |
The following diagram illustrates the metabolic pathway implications of these polymorphisms:
Figure 1: Impact of Genetic Polymorphisms on Drug Metabolism Pathways. Genetic variants in CYP genes determine metabolic capacity, influencing metabolite exposure levels and clinical outcomes.
Population Distribution and Geographical Gradients
The prevalence of important CYP alleles demonstrates significant geographical gradients across Europe, reflective of the continent's migratory history [15].
Table 2: Population Frequencies of Key CYP Alleles Across European Populations
| Population Region | CYP2C19*2 (%) | CYP2C19*17 (%) | CYP2D6*4 (%) | CYP2D6*5 (%) | CYP2D6 Duplications (%) |
|---|---|---|---|---|---|
| Northern Europe (Sweden, Denmark, Norway) | 13-15% | 19-22% | 19-25% | 4-6% | 0.5-1% |
| Central Europe (Czech Republic, Poland, Slovakia) | 8-12% | 29-33% | 20-25% | ~3% | 1-2% |
| Southern Europe (Italy, Spain, Greece) | 12-17% | 11-18% | 16-18% | 1-2% | 3-6% |
| Finland (distinct pattern) | 17.5% | ~20% | 10% | 2.2% | 4.3% |
These geographical gradients have profound implications for multinational drug development and clinical trial design, as the proportion of patients with atypical metabolic phenotypes varies significantly between regions [15].
Membrane Drug Transporters
Membrane transporters are integral membrane proteins that actively or passively control the influx and efflux of drugs and other molecules across biological membranes [17]. They play crucial roles in drug absorption, distribution, and elimination, significantly impacting both drug pharmacokinetics and pharmacodynamics. Two major superfamilies dominate this field: the ATP-binding cassette (ABC) transporters, which are primarily efflux transporters that utilize ATP hydrolysis to pump substrates out of cells, and the Solute Carrier (SLC) transporters, which include both influx and efflux transporters [18] [17].
The International Transporter Consortium (ITC) and regulatory authorities have identified specific transporters as clinically important determinants of drug disposition and drug-drug interactions [19]. According to the ITC, polymorphisms in ABCG2 (BCRP), SLCO1B1 (OATP1B1), and the emerging transporter SLC22A1 (OCT1) should be considered during drug development due to substantial evidence linking them to interindividual differences in drug levels, toxicities, and responses [19].
Key Transporter Polymorphisms
Table 3: Clinically Important Drug Transporter Polymorphisms
| Transporter | Gene | Key Polymorphism | Functional Effect | Clinical Impact |
|---|---|---|---|---|
| BCRP | ABCG2 | rs2231142 (Q141K) | Reduced protein expression and transport activity [19] | Altered pharmacokinetics of sulfasalazine, rosuvastatin; increased uric acid levels and gout risk [19] [20] |
| OATP1B1 | SLCO1B1 | rs4149056 (Val174Ala) | Reduced transport activity to hepatocytes [19] [18] | Increased systemic exposure to statins; higher risk of statin-induced myopathy [19] [18] |
| OCT1 | SLC22A1 | Multiple reduced function variants (e.g., R61C, M420del, G465R) | Decreased uptake activity into hepatocytes [19] | Altered metformin disposition and response; potential impact on several prescription drugs [19] |
| P-glycoprotein | ABCB1 | C3435T (synonymous) | Altered protein conformation and substrate specificity [21] | Controversial impact on digoxin, HIV protease inhibitors, and chemotherapy drug pharmacokinetics [21] |
The protein structures and cellular localization of these critical transporters are visualized below:
Figure 2: Key Drug Transporters in Hepatocyte Drug Handling. Uptake and efflux transporters work in concert to determine drug disposition, with polymorphisms impacting function at multiple sites.
Genome-Wide Association Study (GWAS) Validation
The clinical importance of transporter polymorphisms is underscored by GWAS findings. To date, a total of eight GWAS have reported genome-wide significant associations (p<5×10â»â¸) between polymorphisms in ABCG2 and SLCO1B1 and drug disposition or response [19]. These associations have been described for drugs used in the treatment of lipid disorders (statins), gout (allopurinol), cancer (methotrexate), and cardiovascular disorders (ticagrelor) [19]. Among these eight GWAS, four are related to drug disposition and four are related to therapeutic or adverse drug response.
For SLCO1B1, the nonsynonymous polymorphism rs4149056 (Val174Ala) has been either directly associated with pharmacologic traits or is in linkage disequilibrium with another variant that has been associated with the trait [19]. For ABCG2, multiple polymorphisms have been associated with various traits, though typically the missense polymorphism rs2231142 (Q141K) is in linkage disequilibrium with the associated polymorphisms [19].
Experimental Approaches and Methodologies
Genotyping Techniques and Functional Characterization
Robust experimental protocols are essential for reliable pharmacogenomic research. The following methodologies represent current best practices for investigating CYP and transporter polymorphisms.
Genotyping Methods:
- qPCR with TaqMan Probes: Standard and custom TaqMan reagents provide specific allele discrimination for known variants. This method was successfully employed in a study of 742 Bulgarian psychiatric patients for CYP2D6 and CYP2C19 genotyping [16].
- Copy Number Variation (CNV) Analysis: Specific PCR primers are used to detect gene deletions (e.g., CYP2D65) and duplications (e.g., CYP2D61xN, *2xN) [16].
- Massively Parallel Sequencing: Next-generation sequencing approaches allow for comprehensive variant discovery across pharmacogenes, identifying both common and rare variants [19].
Functional Characterization Workflow: The following diagram outlines a standardized approach for functional characterization of polymorphisms:
Figure 3: Experimental Workflow for Characterizing Pharmacogenetic Variants. A multidisciplinary approach integrates in vitro and clinical studies to establish functional impact.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Pharmacogenomic Studies
| Reagent/Cell Line | Application | Function/Significance |
|---|---|---|
| MDR1-MDCK | Transcellular transport assays | Madin-Darby canine kidney cells overexpressing human P-glycoprotein (ABCB1) to study efflux transport |
| HEK293 Transfectants | Functional characterization of variants | Human embryonic kidney cells transfected with wild-type or polymorphic transporter genes for uptake assays |
| Ko143 | Specific BCRP inhibition | Potent and selective ABCG2 inhibitor used to confirm BCRP-specific transport in vitro [20] |
| TaqMan Genotyping Assays | Allelic discrimination | Fluorogenic 5'-nuclease chemistry for specific SNP detection and quantitation |
| Human Hepatocytes | Integrated transport and metabolism studies | Primary cells maintaining native expression of drug transporters and metabolizing enzymes |
| Vesicular Transport Assays | ABC transporter characterization | Membrane vesicles prepared from transporter-overexpressing cells to study ATP-dependent transport |
| AJM 290 | AJM 290, MF:C20H14FNO4S, MW:383.4 g/mol | Chemical Reagent |
| BRITE-338733 | 2-(4-(5-Ethylfuran-2-yl)-6-(2,2,6,6-tetramethylpiperidin-4-ylamino)pyridin-2-yl)-4-methylphenol | High-purity 2-(4-(5-Ethylfuran-2-yl)-6-(2,2,6,6-tetramethylpiperidin-4-ylamino)pyridin-2-yl)-4-methylphenol for research applications. This product is For Research Use Only. Not for human or veterinary use. |
The comprehensive characterization of genetic polymorphisms in CYP enzymes and drug transporters represents a fundamental component of personalized medicine research. The clinical pharmacogenetics of CYP2D6, CYP2C19, ABCG2, SLCO1B1, and SLC22A1 have matured sufficiently to warrant consideration in drug development programs and, in many cases, clinical practice. The geographical gradients in allele frequencies emphasize the importance of population-specific considerations in both research and clinical implementation. As pharmacogenomic strategies continue to evolve, supported by initiatives such as the European Partnership for Personalised Medicine's JTC2025 call on "Pharmacogenomic Strategies for Personalised Medicine" [22], the integration of this knowledge into drug development and clinical practice will be essential for advancing the precision medicine paradigm, ultimately enabling tailored therapeutic strategies that optimize efficacy while minimizing adverse drug reactions.
The journey to understand the blueprint of life represents one of science's most profound evolutions, transitioning from philosophical speculation to precise molecular intervention. This historical progression, originating with ancient Greek philosophers like Pythagoras and culminating in today's genomic era, established the fundamental principles that enable modern pharmacogenomics. Personalized medicine, which aims to tailor medical treatment to an individual's genetic makeup, is the direct descendant of centuries of research into the laws of heredity and biological information [23]. The field of pharmacogenomics (PGx) now applies this knowledge to study how interindividual variations in DNA sequence relate to drug response, thereby improving therapeutic outcomes by optimizing drug selection and dosing, reducing adverse drug reactions, and increasing overall treatment efficacy [24]. This whitepaper traces these critical historical milestones, detailing their technical foundations and their collective role in forging the tools for contemporary personalized drug therapy.
Historical Foundations: From Speculation to Mendel's Laws
The human understanding of heredity began not with experimentation, but with observation and philosophical reasoning.
Ancient and Classical Theories
In approximately 500 BC, Greek philosophers such as Hippocrates and Pythagoras proposed early theories of heredity. Pythagoras believed that semen collected a physical essence, or "pangens," from all parts of the father's body, which then condensed into a new individual in the womb. This theory suggested that characteristics acquired by a parent during their lifetime could be passed to offspring [25]. Later, in around 300 BC, Aristotle challenged this view, noting that children could inherit traits from their mothers and grandparents. He introduced the concept of information being transmitted via a non-physical "form-giving principle" rather than a physical template, although he still believed this information was carried in semen and menstrual blood [26] [25].
The Birth of Experimental Genetics
The pivotal breakthrough came from the meticulous work of Gregor Mendel, an Augustinian friar. Between 1856 and 1865, he conducted systematic breeding experiments using pea plants (Pisum sativum). His quantitative approach allowed him to deduce the fundamental principles of inheritance [26].
- Experimental Methodology: Mendel hand-pollinated thousands of pea plants, carefully tracking seven distinct characteristics across generations. For each trait, he crossed pure-bred parent plants and statistically analyzed the patterns appearing in their hybrid offspring [25].
- Key Findings: His experiments revealed that traits are passed on in discrete units (later termed "genes") that do not blend but remain distinct across generations. He formulated the laws of segregation (each individual has two alleles for a trait, which separate during gamete formation) and independent assortment (genes for different traits are inherited independently of one another) [26]. Mendel himself referred to the "material creating" the character as "factors" [26].
Table 1: Key Historical Milestones in Genetics (c. 500 BC - 2003)
| Date | Figure(s) | Key Contribution | Experimental Method |
|---|---|---|---|
| ~500 BC | Pythagoras & Hippocrates | Theory of "pangens" - hereditary material collected from all body parts [25]. | Philosophical reasoning and observation. |
| ~300 BC | Aristotle | Proposed information ("form-giving principle") as the basis of heredity [26] [25]. | Observation of family traits and embryo development (e.g., chicken eggs) [25]. |
| 1865 | Gregor Mendel | Established laws of inheritance (segregation and independent assortment) [26]. | Statistical analysis of trait inheritance in thousands of hand-pollinated pea plants [26] [25]. |
| 1900 | Hugo de Vries, Carl Correns, Erich von Tschermak | Independently rediscovered and confirmed Mendel's work [26]. | Repetition of plant hybridisation experiments. |
| 1910 | Thomas Hunt Morgan | Established that genes reside on chromosomes, using fruit flies (D. melanogaster) [26]. | Cross-breeding experiments tracking eye color mutations in fruit flies [25]. |
| 1944 | Oswald Avery, Colin MacLeod, Maclyn McCarty | Identified DNA as the molecule carrying genetic information [27]. | In vitro transformation of bacteria. |
| 1953 | James Watson, Francis Crick, Rosalind Franklin, Maurice Wilkins | Determined the double-helical structure of DNA [27]. | X-ray crystallography (Franklin) and model building. |
| 2003 | International Human Genome Project | Completed the sequencing of the human genome, confirming ~20,000-25,000 genes [27] [28]. | Large-scale capillary sequencing (Sanger method) of DNA fragments. |
The Rise of Modern Genomics and Pharmacogenomics
The 20th century witnessed the transition from classical genetics to molecular biology and genomics, setting the stage for pharmacogenomics.
From DNA to the Genome
The period between the 1950s and the early 2000s was marked by a series of transformative discoveries. In 1953, the double-helix structure of DNA, proposed by James Watson and Francis Crick with critical contributions from Rosalind Franklin, revealed the molecular basis for genetic storage and replication [27]. The following decades saw the development of foundational tools like the polymerase chain reaction (PCR) in 1983, which allowed for the amplification of specific DNA sequences, and DNA profiling in 1984 [27]. The apex of this era was the Human Genome Project (HGP), launched in 1990 and declared complete in 2003. The HGP provided the first reference sequence of the entire human genome, confirming an estimated 20,000 to 25,000 genes and revolutionizing all aspects of biomedical research [27] [28].
The Emergence of Pharmacogenomics
With the human genome sequenced, researchers could systematically investigate the genetic basis for variable drug responses. Pharmacogenomics emerged as a discipline focused on how interindividual variations in DNA sequence impact drug efficacy and toxicity [24]. Key initiatives, such as the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the Dutch Pharmacogenetics Working Group (DPWG), were formed to curate evidence and create clinical guidelines for gene-based drug prescribing [24] [29]. For example, the FDA-approved label for the antiplatelet drug clopidogrel now includes a warning that patients who are CYP2C19 poor metabolizers may experience diminished drug effectiveness, advising clinicians to consider alternative treatments [29].
Table 2: Modern Genomic and Pharmacogenomic Milestones (1978 - Present)
| Date | Initiative/Discovery | Significance | Impact on Personalized Medicine |
|---|---|---|---|
| 1978 | WHO Uppsala Monitoring Centre Established | Launched international pharmacovigilance collaboration, creating the Vigibase for adverse drug reaction (ADR) reports [29]. | Laid groundwork for post-marketing drug safety surveillance, a precursor to genetic ADR investigation. |
| 1990 | Human Genome Project Launched | International effort to sequence the entire human genome [27] [28]. | Provided the fundamental reference map for identifying genetic variants linked to disease and drug response. |
| 2003 | Human Genome Sequence Completed | Completed >92% of the human genome sequence, confirming ~20,000-25,000 genes [27]. | Enabled genome-wide association studies (GWAS) to find variants associated with drug metabolism and efficacy. |
| 2005-2010 | Early PGx Implementations | FDA adds PGx data to drug labels (e.g., warfarin); CPIC forms to create clinical guidelines [24] [29]. | Began translating genetic research into actionable clinical prescribing recommendations. |
| 2012 | CRISPR-Cas9 Gene Editing Discovered | A versatile and precise method for editing genes [27]. | Opened possibilities for correcting genetic mutations that cause disease or alter drug response. |
| 2020 | FDA Table of Pharmacogenetic Associations | Listed 22 distinct drug-gene pairs with potential impact on safety or response [29]. | Consolidated and highlighted key PGx relationships for clinicians and regulators. |
| 2023 (Example) | Iran PGx Initiative | Population-specific study of 37 pharmacogenes to guide treatment in oncology, cardiology, and psychiatry [23]. | Demonstrates global adoption of PGx, highlighting need for population-specific data to guide prescribing. |
| 2025 (Future) | AI/ML in Pharmacovigilance | Advanced AI models to analyze complex genetic data for ADR risk prediction [29]. | Promises more proactive and individualized drug safety monitoring through pattern recognition in large datasets. |
Technical Frameworks for Clinical PGx Implementation
Translating PGx research into routine clinical practice requires a structured, multi-stakeholder approach.
Stakeholders and Implementation Pathways
The successful integration of PGx into a hospital setting involves a coordinated effort among at least eight key stakeholder groups [24]. Regulatory bodies like the FDA and EMA authorize tests and provide drug labeling guidance. Hospital leadership secures funds and infrastructure, while the Pharmacy & Therapeutics Committee evaluates evidence and identifies the most actionable drug-gene pairs. The laboratory performs genotyping, Information Technology integrates results into electronic health records and clinical decision support systems, and healthcare providers ultimately order tests, interpret results, and make therapeutic decisions. Patients and payers (insurance) complete this ecosystem [24].
The following workflow diagram illustrates the multi-step process for implementing clinical pharmacogenomics:
Analytical and Computational Methods
A significant technical challenge in PGx is the functional interpretation of rare genetic variants. Genes involved in drug absorption, distribution, metabolism, and excretion (ADME) are highly variable, with tens of thousands of different single nucleotide variants (SNVs) and indels, over 98% of which are rare [30]. Characterizing these requires advanced methods:
- Next-Generation Sequencing (NGS): Facilitates comprehensive profiling of pharmacogenes. Specialized technologies like single-molecule real-time sequencing are needed for complex loci (e.g., CYP2D6, HLA) [30].
- Computational Prediction Tools: Tools like SIFT, PolyPhen2, and CADD use machine learning to predict the functional consequences of uncharacterized variants. However, their training on pathogenic datasets can limit accuracy for non-pathogenic pharmacogenomic variants [30].
- Experimental High-Throughput Characterization: Novel multiplexed assays allow for the simultaneous functional assessment of thousands of variants in vitro, generating crucial data to validate computational predictions [30].
The diagram below outlines the core process for interpreting genetic variants to guide drug therapy:
The Scientist's Toolkit: Essential Research Reagents and Materials
The advancement of pharmacogenomics relies on a suite of sophisticated reagents and analytical tools.
Table 3: Key Research Reagent Solutions in Pharmacogenomics
| Reagent/Material | Function in PGx Research |
|---|---|
| PCR Reagents | Amplifies specific DNA sequences for downstream analysis like sequencing or variant detection [27]. |
| Next-Generation Sequencing (NGS) Libraries | Prepared genomic libraries allow for the massive parallel sequencing of entire genomes or targeted gene panels (e.g., ADME core panels) [30]. |
| Sanger Sequencing Reagents | Provides gold-standard validation for specific genetic variants discovered via NGS or other screening methods [27]. |
| TaqMan Assays & Genotyping Arrays | Enables high-throughput, targeted genotyping of known, common single nucleotide polymorphisms (SNPs) [30]. |
| Nanopore Sequencing Kits | Facilitates long-read sequencing, which is critical for resolving complex genomic regions like CYP2D6 and HLA [30]. |
| Heterologous Expression Systems (e.g., Mammalian cells, Yeast) | Used for in vitro functional characterization of novel genetic variants in drug-metabolizing enzymes and transporters [30]. |
| Therapeutic Drug Monitoring (TDM) Assays | Measures drug and metabolite concentrations in patient plasma, providing phenotypic data to correlate with genotype [30]. |
| CRISPR-Cas9 Components | Allows for precise gene editing in cell lines or model organisms to validate the functional impact of genetic variants [27]. |
| Mirificin | Mirificin, CAS:103654-50-8; 1228105-51-8, MF:C26H28O13, MW:548.497 |
| Acetyl Perisesaccharide C | Acetyl Perisesaccharide C|For Research |
The historical journey from Pythagoras's philosophical speculations to the modern genomic era underscores a fundamental shift in understanding life's instructions. The convergence of Mendelian genetics, molecular biology, and large-scale genome sequencing has given rise to the disciplined science of pharmacogenomics. Today, PGx is poised to transform clinical practice by moving from a reactive, one-size-fits-all treatment model to a preemptive, personalized approach. Future progress hinges on overcoming current challenges, including the need for broader education for healthcare providers, clearer reimbursement pathways for PGx testing, and the development of more robust, population-specific clinical guidelines. Furthermore, the integration of artificial intelligence and machine learning with large-scale biobank data promises to unlock deeper insights into the genetic underpinnings of drug response, ultimately fulfilling the promise of personalized medicine that is rooted in a history of scientific discovery spanning millennia [29] [30].
Evolutionary Perspectives on ADME Gene Polymorphism Development
The genetic variation in genes governing drug Absorption, Distribution, Metabolism, and Excretion (ADME) represents a crucial interface between human evolutionary history and modern pharmaceutical science. This technical review examines the evolutionary forces—including natural selection, genetic drift, and population-specific adaptations—that have shaped the remarkable polymorphism observed in pharmacogenes. We synthesize evidence from population genetics, functional genomics, and clinical pharmacogenomics to demonstrate how evolutionary processes have created structured variation in ADME genes across human populations. This analysis provides a framework for understanding interindividual and interethnic variability in drug response, with significant implications for personalized medicine strategies in globally diverse populations. The integration of evolutionary perspectives into pharmacogenomic research promises to enhance drug safety and efficacy by enabling more precise targeting of therapeutic interventions.
The ADME gene family comprises a specialized set of genes encoding proteins responsible for the absorption, distribution, metabolism, and excretion of both exogenous compounds (including pharmaceuticals) and endogenous molecules. These genes include drug-metabolizing enzymes (DMEs) such as cytochrome P450 enzymes (CYPs), conjugating enzymes, and transporter proteins from the SLC and ABC families [31]. The evolutionary history of these genes reveals a complex interplay between environmental pressures, dietary changes, and pathogen exposures that have shaped their polymorphic landscape across human populations.
From an evolutionary perspective, ADME genes exhibit unusual characteristics that make them particularly susceptible to polymorphic variation. Unlike genes encoding critical structural or metabolic pathway components, many ADME genes show relaxed evolutionary constraints, allowing accumulation of functional variants without catastrophic fitness consequences [32]. This tolerance for variation has created a genetic architecture ideal for rapid adaptation to changing environments, especially as human populations dispersed globally and encountered novel chemical environments, dietary components, and disease pressures.
The Remote Sensing and Signaling Hypothesis provides a theoretical framework for understanding the broader physiological roles of ADME genes beyond drug processing [31]. This hypothesis posits that ADME genes form an interactive network regulating inter-organ communication via metabolites, signaling molecules, antioxidants, gut microbiome products, and uremic toxins. This broader physiological function helps explain why these genes have been subject to such varied selective pressures throughout human evolution.
Evolutionary Mechanisms Shaping ADME Polymorphisms
Natural Selection and Adaptive Evolution
Natural selection has operated on ADME genes through multiple mechanisms, with positive selection acting on standing variation as a prominent force. Genomic analyses have revealed that positive selection from standing variation has exerted moderate but persistent pressure on ADME genes in Eurasian populations, driving adaptive alleles to high frequencies over prolonged evolutionary history [33]. The timing of these selective events often coincides with major human migrations and ecological transitions, suggesting environmental factors as key drivers.
Specific examples of adaptation illustrate these mechanisms:
CYP2D6 gene duplication: In Northeast Africa approximately 10,000-5,000 years ago, strong positive selection favored survival of individuals carrying multiple copies of the CYP2D6 gene, potentially enhancing detoxification capabilities for plant alkaloids during periods of dietary diversification and starvation [34]. These duplication alleles subsequently spread through migration into Mediterranean regions but not to Asia or West Africa, creating distinct geographic patterns of variation.
ADH1B*48His (rs1229984): This well-documented polymorphism shows striking differentiation between Tibetan and other populations (FST = 0.646 between Tibetan and Lic populations) [33]. The adaptation to subsistence lifestyle following Neolithic agriculture has been proposed as the evolutionary driver, demonstrating how cultural innovations can reshape genetic variation.
PPARD locus: Analysis of contrastive sequence signatures between both sides of a recombination spot provides evidence for a selective sweep at the PPARD locus through genetic hitchhiking effect [33]. The onset of this adaptation coincided with early out-of-Africa migration of modern humans and persisted throughout their evolutionary history, suggesting prolonged selective pressure.
Population Dynamics and Genetic Drift
Human demographic history has profoundly influenced the distribution of ADME variants across populations. Founder effects, population bottlenecks, and migration patterns have all contributed to the structured variation observed in modern populations. The accumulation of rare variants—which account for over 90% of the overall genetic variability in pharmacogenes—has been particularly influenced by population-specific genetic drift [32].
Population genetic studies demonstrate that Amerindian populations show the most distinct ADME genetic profile compared to other continental groups (mean FST = 0.09917) [35]. This distinctiveness reflects both the founder effects during the peopling of the Americas and subsequent genetic isolation. Similarly, studies of African populations reveal substantial population structuring at CYP450 genes, associated with intra-African differences in responses to drugs used for infectious disease treatment [36].
The persistence of rare variants in population isolates represents a particularly important phenomenon for pharmacogenomics. Each individual harbors on average 40.6 putatively functional variants in ADME genes, with rare variants accounting for 10.8% of these [32]. These rare variants collectively contribute to the "missing heritability" in drug response traits not explained by common polymorphisms.
Table 1: Evolutionary Mechanisms and Their Impact on ADME Gene Variation
| Evolutionary Mechanism | Impact on ADME Genes | Representative Examples |
|---|---|---|
| Positive Selection | Increases frequency of adaptive alleles; creates geographic variation | CYP2D6 duplication in Northeast Africa; ADH1B in East Asians |
| Genetic Drift | Causes random fluctuations in allele frequency; prominent in small populations | Rare variant accumulation in population isolates; Amerindian distinctiveness |
| Population Bottlenecks | Reduces genetic diversity; increases frequency of founder variants | Reduced diversity in non-African populations; distinctive Amerindian profile |
| Migration and Admixture | Creates clinal variation and novel combinations of variants | East-West stratification in Eurasian populations; admixed population variability |
Population-Specific Variation in ADME Genes
Continental Patterns of Variation
ADME genes exhibit striking differences in allele frequencies across major population groups, reflecting their distinct evolutionary histories. These patterns have profound implications for global drug development and implementation of pharmacogenomic testing across diverse populations.
African populations display exceptional diversity in CYP450 genes, with numerous population-specific variants affecting drug metabolism. For example, CYP2C95 and CYP2C911 are predominantly found in African populations (1-3% and 1-23% frequency respectively) and are associated with excessive anticoagulation risk in African-American patients [36]. The CYP3A4*1B variant shows particularly high frequency in African populations (66-86%) compared to Europeans (2-4%) or East Asians (0%), contributing to population-specific metabolism of numerous pharmaceuticals [36].
Amazonian Amerindian populations demonstrate a unique ADME genetic profile characterized by significantly different allelic frequencies and genotype distributions in multiple markers compared to African, European, American, and Asian populations [35]. This distinctiveness highlights the importance of including under-represented populations in pharmacogenomic studies to ensure equitable application of precision medicine approaches.
East Asian populations show characteristic patterns of variation, including higher frequencies of CYP2C19 poor metabolizer alleles (*2 and *3) compared to other populations [36]. The extensive genetic architecture studies in Chinese populations reveal a north-south cline in ADME variation, with three major groups—northern minorities (Uygur, Mongolian, Tibetan), Han Chinese, and southern minorities—primarily reflecting geographical and historical relationships [33].
Functional Consequences of Population Variation
The population-specific variation in ADME genes has direct consequences for drug metabolism phenotypes and clinical outcomes:
CYP2D6 variation: Polymorphisms and haplotypes in CYP2D6 contribute to variable metabolism of approximately 25% of clinically administered drugs [36]. The gene is subject to copy number variations (CNVs), with individuals carrying multiple functional copies exhibiting ultrarapid metabolism that prevents achievement of therapeutic drug concentrations at standard dosages.
CYP2C19 variation: The CYP2C19*2 allele (no detectable enzyme levels) shows substantial frequency variation across populations (11-21% in Africans, 13-14% in American populations, 32-36% in Asians, and 7-22% in Europeans) [36]. This variation influences response to numerous drugs including clopidogrel, proton pump inhibitors, and antidepressants.
CYP3A5 variation: The CYP3A5*3 allele (reduced/undetectable expression) shows dramatic frequency differences, occurring in 93-96% of Europeans but only 4-81% of Africans [36]. This variation affects metabolism of tacrolimus and other important medications.
Table 2: Population Frequencies of Clinically Important ADME Variants
| Gene | Variant | Effect | African Frequency | European Frequency | East Asian Frequency |
|---|---|---|---|---|---|
| CYP2C9 | *2 | Reduced function | 7% | 9-16% | 1% |
| CYP2C9 | *3 | Reduced function | 2-3% | 5-11% | 2-6% |
| CYP2C9 | *5 | Reduced function | 1-3% | 0% | 0% |
| CYP2C19 | *2 | No function | 11-21% | 7-22% | 32-36% |
| CYP2C19 | *3 | No function | 1% | 0% | 5-6% |
| CYP2D6 | *17 | Reduced function | 20-35% | 1-3% | 0-1% |
| CYP3A4 | *1B | Increased function | 66-86% | 2-4% | 0% |
| CYP3A5 | *3 | Reduced function | 4-81% | 93-96% | 69-74% |
| TPMT | *3A | Reduced function | 1-3% | 3-5% | 1-2% |
Experimental Approaches and Methodologies
Population Genetics and Genotyping Methods
The dissection of evolutionary patterns in ADME genes relies on sophisticated genotyping and analytical approaches. High-throughput genotyping technologies have enabled comprehensive characterization of ADME variation across diverse populations. The DMET (Drug Metabolism Enzymes and Transporters) platform represents one such approach, allowing simultaneous assessment of multiple polymorphisms in ADME genes [37].
Standardized protocols for ADME genotyping typically involve:
- DNA extraction from peripheral blood using commercial kits (e.g., Biopur Mini Spin Plus) with quality assessment via spectrophotometry (e.g., NanoDrop 1000) [35]
- Genotyping using technologies such as TaqMan OpenArray customized assays run on platforms like QuantStudio 12K Flex Real-Time PCR systems [35]
- Quality control including Hardy-Weinberg equilibrium testing and exclusion of markers deviating from expected distributions [35]
For population genetics analyses, key methodologies include:
- FST (fixation index) calculations to measure population differentiation at each locus [35] [33]
- Multidimensional scaling (MDS) analysis to visualize genetic relationships between populations [35]
- STRUCTURE analysis to identify ancestral components and admixture patterns [33]
- Linkage disequilibrium (LD) analysis to identify regions with evidence of selective sweeps [33]
Detecting Natural Selection in ADME Genes
Several specialized approaches have been developed to identify signatures of natural selection in ADME genes:
Contrastive sequence signature analysis: Examining differences in genetic variation patterns between both sides of recombination spots can reveal selective sweeps through genetic hitchhiking effects [33]
Haplotype-based tests: Extended haplotype homozygosity and related approaches detect unusually long haplotypes indicative of recent positive selection
Integration with functional genomic data: Combining population genetic data with gene expression quantitative trait loci (eQTL) analyses helps connect adaptive variants to their functional consequences [33]
Cross-tissue co-expression network analysis: Identifying coordinated expression patterns of ADME genes across tissues (e.g., gut-liver-kidney axis) provides insights into their functional integration and evolutionary constraints [31]
Diagram 1: Experimental Workflow for Evolutionary Analysis of ADME Genes. This workflow outlines the key steps in characterizing evolutionary patterns in ADME genes, from sample collection through functional validation.
Table 3: Essential Research Resources for ADME Evolutionary Studies
| Resource Category | Specific Tools/Reagents | Application/Function |
|---|---|---|
| Genotyping Platforms | DMET (Drug Metabolism Enzymes and Transporters) microarray [37] | Simultaneous interrogation of multiple ADME polymorphisms |
| TaqMan OpenArray Genotyping Technology [35] | Customized SNP genotyping with high throughput capability | |
| Bioinformatic Tools | ADME-optimized prediction framework [32] | Computational functionality prediction for pharmacogenetic variants |
| STRUCTURE software [33] | Population structure analysis and ancestry estimation | |
| Arlequin v.3.5 [35] | Population genetics analyses including FST calculations | |
| Reference Databases | 1000 Genomes Project [35] [33] | Global genetic variation reference for population comparisons |
| Exome Aggregation Consortium (ExAC) [32] | Database of exonic variants from large-scale sequencing projects | |
| PharmGKB [38] [35] | Curated knowledge resource for pharmacogenomic associations | |
| Analytical Approaches | Multi-dimensional Scaling (MDS) [35] [33] | Visualization of population relationships based on genetic distances |
| Cross-tissue co-expression network analysis [31] | Identification of functionally connected ADME gene networks | |
| Loss-of-function intolerance scoring [32] | Assessment of evolutionary constraints on pharmacogenes |
Implications for Personalized Medicine and Drug Development
Clinical Translation of Evolutionary Insights
Understanding the evolutionary forces that shaped ADME variation provides a crucial foundation for implementing pharmacogenomics in clinical practice. The differential distribution of pharmacogenetic variants across populations has direct implications for drug safety and efficacy across diverse patient groups. Regulatory agencies have recognized this importance, with the FDA maintaining a table of pharmacogenomic biomarkers in drug labeling that includes numerous ADME-related genes [14].
Clinical implementation frameworks must account for evolutionary insights in several ways:
Population-specific dosing guidelines: For drugs like warfarin, clinical pharmacogenetics implementation consortium (CPIC) guidelines incorporate genetic factors that show population variation, including CYP2C9 and VKORC1 variants [38]
Rare variant consideration: Next-generation sequencing approaches capture rare variants that contribute substantially to functional variability in many pharmacogenes [32]
Admixed population strategies: Populations with recent admixture, such as African Americans and Latin Americans, require special consideration due to the complex interplay of genetic variants from different ancestral backgrounds [33]
Regulatory and Implementation Considerations
The integration of evolutionary perspectives into drug development and clinical practice requires addressing several challenges:
Database representation: Current pharmacogenetic databases remain skewed toward European-ancestry populations, limiting understanding of variation in other groups [35]
Biomarker validation: Biomarkers must be validated across diverse populations to ensure generalizability, considering the high population specificity of many ADME variants [37]
Clinical decision support: Electronic health record integration of pharmacogenetic data must account for population-specific allele effects and interpretation [38]
The overlap between FDA pharmacogenomic labeling and CPIC guidelines provides a framework for implementation. Analysis reveals that among ADME gene-drug pairs, 74% are classified as "actionable," 15% as "informative," 9% as "testing recommended," and 2% as "testing required" [38]. CYP2D6 represents the most prevalent ADME gene in FDA labeling, reflecting its importance in numerous drug metabolism pathways.
Diagram 2: Evolutionary Pathways from Environmental Pressures to Clinical Implications. This diagram illustrates the conceptual pathway linking environmental selective pressures through evolutionary mechanisms to genetic outcomes in ADME genes and their subsequent clinical implications for personalized medicine.
The evolutionary perspective on ADME gene polymorphisms provides a foundational framework for understanding the genetic architecture of drug response variability. The interplay between natural selection, genetic drift, and human demographic history has created a structured landscape of variation that differs substantially across populations. This evolutionary legacy has direct consequences for drug development, clinical trial design, and implementation of personalized medicine across diverse global populations.
Future research directions should include:
Expanded diversity in genomic studies: Deliberate inclusion of under-represented populations in pharmacogenomic studies to capture the full spectrum of ADME variation [35]
Integration of rare variants: Development of computational frameworks that incorporate both common and rare variants into drug response predictions [32]
Functional characterization: Systematic functional assessment of population-specific variants to determine their clinical relevance [37]
Evolutionary-aware clinical guidelines: Development of prescribing guidelines that incorporate population genetic principles while avoiding oversimplified racial categorization
The growing understanding of ADME gene evolution promises to enhance drug safety and efficacy by enabling more precise targeting of therapeutic interventions. By acknowledging the evolutionary forces that shaped pharmacogenetic variation, researchers and clinicians can better navigate the complex interplay between human genetic diversity and pharmaceutical interventions in an increasingly globalized healthcare environment.
Clinical Implementation and Therapeutic Applications: From Biomarker Discovery to Treatment Personalization
The efficacy and toxicity of cancer therapeutics are governed by a complex interplay of two distinct genetic systems: the germline genome, an individual's inherited genetic blueprint present in every cell, and the somatic genome, comprising acquired mutations found exclusively within tumor cells [39]. Germline variants influence drug metabolism, transport, and mechanism of action in all tissues, representing a systemic determinant of therapeutic response [40] [1]. In contrast, somatic mutations drive oncogenesis and can create tumor-specific dependencies that determine susceptibility to targeted therapies [39] [41]. The emerging paradigm in precision oncology recognizes that comprehensive drug response prediction requires integrated analysis of both genetic systems, as their contributions to treatment outcomes can be complementary and sometimes of comparable magnitude [40]. This whitepaper examines the distinct characteristics, detection methodologies, and predictive values of germline and somatic biomarkers, framing their integration as an essential component of pharmacogenomics-driven personalized medicine.
Fundamental Distinctions Between Germline and Somatic Variants
Biological Origin and Transmission
Germline and somatic variants differ fundamentally in their origin, distribution throughout the body, and implications for cancer risk and treatment.
Germline variants originate in reproductive cells (sperm or egg) and are incorporated into every cell of the offspring's body following conception [39]. These variants are heritable and can be passed to subsequent generations, following Mendelian inheritance patterns. When pathogenic, germline variants in cancer predisposition genes such as BRCA1, BRCA2, and Lynch syndrome-associated genes (MLH1, MSH2, MSH6, PMS2) confer increased lifetime cancer risk [39] [42].
Somatic variants, in contrast, are acquired throughout an individual's lifetime due to environmental exposures (tobacco, ultraviolet radiation, chemicals), replication errors, or other cellular insults [39]. These mutations are confined to specific cell populations and their progeny, are not present in all body cells, and cannot be transmitted to offspring. Somatic mutations drive carcinogenesis by activating oncogenes or inactivating tumor suppressor genes within specific tissues.
Table 1: Fundamental Characteristics of Germline versus Somatic Variants
| Characteristic | Germline Variants | Somatic Variants |
|---|---|---|
| Origin | Inherited from parents | Acquired during lifetime |
| Transmission | Heritable across generations | Not heritable |
| Cell Distribution | Present in every nucleated body cell | Confined to specific cell populations/tumors |
| Contribution to Cancer | ~5-10% of all cancers [39] | Majority of cancers (sporadic) |
| Temporal Stability | Constant throughout life | Evolve over time (temporal heterogeneity) |
| Detection Method | Blood, saliva, or buccal samples [39] | Tumor tissue or liquid biopsy [39] |
Clinical Indicators for Genetic Testing
Specific clinical and familial patterns should raise suspicion for germline versus somatic origins of cancer susceptibility:
Indicators of potential germline predisposition include [39]:
- Early-onset cancer (e.g., breast, colorectal, or endometrial cancer diagnosed before age 50)
- Multiple primary cancers in one individual or bilateral cancer in paired organs
- Rare cancers (e.g., male breast cancer, ovarian cancer, pancreatic cancer)
- Strong family history with evidence of autosomal dominant inheritance
- Specific tumor characteristics (e.g., triple-negative breast cancer, microsatellite instability)
- Presence of premalignant conditions (e.g., ≥20 colorectal adenomatous polyps)
Somatic mutations are suspected in sporadic cancers without the above patterns, particularly when associated with known environmental risk factors or advancing age [39].
Predictive Contributions to Drug Response
Germline Biomarkers: Systemic Determinants of Drug Metabolism and Toxicity
Germline variants influence drug response through multiple mechanisms, primarily affecting drug metabolism, transport, and targets. These systemic genetic factors can produce therapeutic outcomes ranging from lack of efficacy to severe adverse reactions.
Table 2: Germline Biomarkers with Clinical Utility in Oncology and Beyond
| Biomarker/Gene | Drug/Therapeutic Class | Effect/Mechanism | Clinical Utility |
|---|---|---|---|
| CYP2C19 | Clopidogrel [29] | Reduced activation in poor metabolizers | FDA label warning; consider alternative antiplatelets |
| CYP2D6 | Tamoxifen [43] | Reduced activation in poor metabolizers | Consider alternative endocrine therapy |
| DPYD | 5-Fluorouracil [40] | Increased toxicity due to reduced clearance | Dose adjustment or drug avoidance |
| HLA-B*15:02 | Carbamazepine [1] | Increased risk of severe cutaneous adverse reactions (SCARs) | Pre-treatment screening in high-risk populations |
| BRCA1/BRCA2 | PARP inhibitors [40] [42] | Synthetic lethality in homologous repair-deficient cells | Predictive biomarker for PARP inhibitor efficacy |
Recent evidence demonstrates that germline variants contribute substantially to variation in drug susceptibility. A systematic analysis of 993 cancer cell lines and 265 drugs revealed that germline contributions to drug susceptibility can be as large or larger than effects from somatic mutations [40]. For the HSP90 inhibitor 17-AAG, germline variants explained 5.1% of response variance, while somatic mutations showed no predictive power [40].
Somatic Biomarkers: Tumor-Specific Therapeutic Targets
Somatic mutations create therapeutic vulnerabilities that can be exploited with targeted therapies. These biomarkers typically inform on-target drug effects rather than systemic metabolism.
Table 3: Somatic Biomarkers with Clinical Utility in Oncology
| Biomarker | Drug/Therapeutic Class | Effect/Mechanism | Clinical Context |
|---|---|---|---|
| BRAF V600E | Vemurafenib, Dabrafenib [44] | Direct inhibition of mutated BRAF kinase | Melanoma, colorectal cancer |
| EGFR mutations | Gefitinib, Erlotinib, Osimertinib | Inhibition of mutated EGFR kinase | Non-small cell lung cancer |
| BRCA1/2 somatic | PARP inhibitors [42] | Synthetic lethality | Ovarian, breast, pancreatic cancer |
| Microsatellite Instability (MSI-H) | Immune checkpoint inhibitors [42] | Enhanced neoantigen presentation | Multiple solid tumors |
| HER2 amplification | Trastuzumab, HER2-targeted therapies | Antibody-mediated inhibition of HER2 signaling | Breast, gastric cancers |
Notably, some therapeutic biomarkers can originate from either germline or somatic alterations. For example, PARP inhibitor sensitivity occurs with both germline and somatic BRCA1/2 mutations, though approximately 35% of germline variants are not detected by somatic testing alone [45], highlighting the importance of comprehensive genetic assessment.
Methodological Approaches for Biomarker Discovery and Validation
Experimental Designs for Dissecting Germline and Somatic Contributions
Systematic approaches have been developed to quantify the relative contributions of germline and somatic variants to drug response:
Joint Modeling of Germline and Somatic Variants: Researchers applied elastic net regularized linear regression to predict drug susceptibility in 993 cancer cell lines screened against 265 compounds [40]. This approach modeled germline and somatic variants both separately and jointly, allowing direct comparison of their predictive contributions.
Quantitative Trait Locus (QTL) Mapping: Genome-wide association studies identified specific germline variants (drug response QTLs) significantly associated with sensitivity to individual drugs [40]. Nine drugs showed significant germline QTLs at family-wise error rate <5%, with eight being targeted therapies and one a DNA crosslinker.
Visible Neural Network (VNN) Integration: The DrugCell system models the hierarchical organization of cellular biological processes while simultaneously integrating germline genotype and drug structural information [41]. This approach couples drug response predictions with identifiable biological mechanisms by mapping neural network components to known molecular subsystems.
Diagram 1: DrugCell predictive architecture. This visible neural network integrates drug chemical structure with cellular genotype through separate branches that merge to predict drug response.
Technical Considerations for Genetic Testing
Discrepancies between germline and somatic testing results necessitate careful methodological considerations:
Sequencing Coverage and Depth: Germline testing typically employs whole-gene sequencing with high read depth, while somatic panels often target specific exons or variant hotspots with lower coverage, potentially missing some variants [45].
Variant Filtering and Classification: Germline analysis compares to reference genomes to identify inherited variants, while somatic calling identifies tumor-specific changes by comparing tumor to matched normal tissue [45].
Tumor-Normal Sequencing: The optimal approach for distinguishing germline from somatic variants involves sequencing matched tumor-normal pairs, enabling precise identification of somatic mutations while controlling for germline background [45].
Diagram 2: Complementary testing workflows. Germline and somatic testing follow distinct laboratory pathways with different sample requirements, sequencing approaches, and analytical methods before integration for clinical decision-making.
Clinical Integration and Therapeutic Applications
Timing and Considerations for Testing Implementation
The optimal integration of germline and somatic testing in clinical practice requires attention to testing timing and interpretation:
Germline Testing: Should ideally occur at cancer diagnosis or in preventive settings for at-risk individuals, as it informs both treatment decisions and cancer risk management for patients and relatives [45]. Current data show suboptimal implementation, with only 35% of eligible patients undergoing germline evaluation before molecular tumor board review, and 43% never receiving germline consultation [45].
Somatic Testing: Typically performed on tumor tissue after cancer diagnosis to guide therapeutic selection, with particular importance in advanced or metastatic disease [39] [45].
Discrepancy Resolution: Approximately 35% of germline pathogenic variants are not detected by somatic testing alone due to technical and analytical differences [45]. This underscores the importance of reflexive germline confirmation for clinically relevant somatic findings, particularly in genes with both germline and somatic implications (e.g., BRCA1/2, TP53, PTEN).
Clinical Decision-Making Based on Biomarker Type
The clinical implications of germline versus somatic findings differ substantially:
Germline Positive Results:
- Guide therapeutic choices (e.g., PARP inhibitors for BRCA1/2 carriers)
- Influence surgical decisions (e.g., risk-reducing contralateral mastectomy)
- Inform cancer surveillance and risk reduction strategies
- Prompt cascade testing of at-risk relatives
- May have implications for non-cancer drug prescribing (e.g., CYP2D6 status and tamoxifen)
Somatic Positive Results:
- Primarily direct targeted therapy selection
- Inform prognosis based on tumor molecular profile
- May identify eligibility for clinical trials
- Can reveal therapeutic resistance mechanisms
- Guide treatment based on tumor evolution at recurrence
Research Reagent Solutions and Experimental Tools
Table 4: Essential Research Resources for Germline and Somatic Biomarker Discovery
| Resource/Tool | Function/Application | Key Features | Representative Examples |
|---|---|---|---|
| Cancer Cell Line Repositories | Preclinical models for drug screening | Genetically characterized, high-throughput capability | GDSC [40] [44], CCLE [40], CTRP [41] |
| Drug Sensitivity Databases | Correlation of genomic features with drug response | Large-scale screening data, multiple compounds | GDSC (265 drugs) [40], CTRP (481 compounds) [41] |
| Visible Neural Networks (VNNs) | Interpretable AI for drug response prediction | Biologically structured models, mechanism insight | DrugCell [41] |
| Pharmacogenomic Knowledgebases | Curated drug-gene interactions | Evidence-based annotations, clinical guidelines | PharmGKB [1], CPIC [29] [1] |
| Tissue Transcriptome Databases | Prediction of drug sensitivity in normal and tumor tissues | Gene expression data from diverse tissues | TCGA, GTEx [44] |
| Genetic Analysis Tools | QTL mapping, association testing | Identification of germline variants affecting drug response | GWAS, eQTL mapping [40] |
Germline and somatic biomarkers offer complementary insights into drug response mechanisms, with germline variants informing systemic drug processing and somatic mutations revealing tumor-specific vulnerabilities. The integration of both biomarker types provides a more comprehensive foundation for precision oncology than either approach alone. Research methodologies have evolved from simple association studies to sophisticated integrated models that simultaneously leverage both genetic systems, with visible neural networks representing a promising approach for balancing predictive accuracy with biological interpretability. Clinical implementation requires understanding the technical limitations of different testing modalities and appropriate timing for test utilization. As pharmacogenomics continues to advance, the strategic integration of germline and somatic biomarkers will remain essential for optimizing therapeutic outcomes and advancing personalized cancer medicine.
Oncology precision medicine represents a paradigm shift from histology-based to molecularly-informed cancer care. This whitepaper examines the integral role of gene expression profiling and targeted therapies within this framework, contextualized within the broader pharmacogenomics landscape driving personalized medicine research. We detail the modern diagnostic toolkit—including whole transcriptome sequencing (RNA-Seq) and comprehensive genomic profiling—that enables detection of therapeutically actionable biomarkers. The discussion extends to computational frameworks like knowledge graphs that integrate multimodal data to illuminate drug-disease relationships and optimize therapeutic selection. Finally, we address implementation challenges and future directions, underscoring how pharmacogenomic principles are revolutionizing oncology drug development and clinical practice.
Pharmacogenomics, which analyzes how genetic makeup affects drug response, serves as the cornerstone of precision oncology by providing the mechanistic basis for personalized treatment strategies [46]. This field has evolved from early pharmacogenetic studies of single gene-drug pairs into a comprehensive “-omics†discipline that encompasses proteomics, transcriptomics, and metabolomics to better predict interindividual variability in drug efficacy and toxicity [46]. In oncology, this approach is particularly impactful because it addresses the profound molecular heterogeneity of tumors, even within the same histopathological classification.
The clinical implementation of pharmacogenomics enables a transition from empirical therapy selection to biomarker-driven approaches. By identifying genetic variants that influence drug metabolism, transport, and target engagement, researchers and clinicians can optimize treatment regimens for improved efficacy and reduced adverse drug reactions (ADRs) [46]. This is especially critical in oncology, where narrow therapeutic indices and significant toxicity risks necessitate careful patient stratification. Modern precision oncology leverages comprehensive molecular profiling to match patients with targeted therapies based on the specific genetic alterations driving their disease, thereby improving outcomes across multiple cancer types [47].
Molecular Profiling Technologies in Precision Oncology
Sequencing Approaches for Tumor Molecular Characterization
Comprehensive molecular profiling forms the foundation of precision oncology, enabling systematic identification of clinically actionable genomic and transcriptomic alterations [47]. Next-generation sequencing (NGS) technologies have revolutionized tumor characterization through several complementary approaches:
Whole-Genome Sequencing (WGS) interrogates the entire ~3.2 billion base pairs of the human genome, permitting unbiased detection of single nucleotide variants (SNVs), insertions and deletions (indels), copy number variations (CNVs), structural rearrangements, and mutational signatures across both coding and non-coding regions [47]. WGS is considered the gold standard for detecting germline mutations associated with hereditary cancer predisposition syndromes (e.g., Lynch syndrome, Li-Fraumeni syndrome) and complex structural variants that may elude targeted approaches [47].
Whole-Exome Sequencing (WES) targets the approximately 1-2% of the genome that encodes proteins, enriching for regions most likely to harbor driver mutations while reducing sequencing costs and computational complexity compared to WGS [47]. This method is particularly valuable for identifying somatic driver mutations in genes such as EGFR, BRAF, PIK3CA, KRAS, and BRCA1/2 that directly inform targeted therapy selection [47].
Whole-Transcriptome Sequencing (RNA-Seq) provides a dynamic representation of gene expression within the tumor and its microenvironment, capturing functional and regulatory dimensions of tumor biology that complement DNA-based analyses [47]. RNA-Seq enables identification of oncogenic gene fusions (e.g., ALK, ROS1, NTRK), alternative splicing events, allele-specific expression patterns, and quantitative transcript levels [47].
Table 1: Comparative Analysis of Sequencing Technologies in Precision Oncology
| Technology | Genomic Coverage | Primary Applications | Key Advantages | Clinical Utility |
|---|---|---|---|---|
| Whole-Genome Sequencing (WGS) | Complete genome (~3.2 billion base pairs) | Hereditary cancer predisposition, complex structural variants, non-coding alterations | Unbiased comprehensive detection, identifies variants outside coding regions | Germline mutation detection, structural variant analysis |
| Whole-Exome Sequencing (WES) | Protein-coding regions (~1-2% of genome) | Somatic driver mutation identification, tumor heterogeneity assessment | Cost-effective for coding regions, high coverage of exonic mutations | Guides targeted therapy selection, identifies clinical trial eligibility |
| Whole-Transcriptome Sequencing (RNA-Seq) | Expressed transcriptome | Gene fusions, expression profiling, pathway activation, tumor microenvironment | Detects functional consequences, identifies expressed fusions | Diagnostic clarification, fusion detection, resistance mechanism elucidation |
Complementary Molecular Diagnostic Techniques
Despite advances in NGS, traditional molecular techniques retain important roles in oncology diagnostics:
Fluorescence In Situ Hybridization (FISH) enables precise detection of gene amplifications, deletions, and rearrangements and remains the reference standard for identifying HER2 amplifications in breast and gastric cancers and ALK, ROS1, or RET fusions in non-small cell lung cancer (NSCLC) [47].
Immunohistochemistry (IHC) assesses protein expression and serves as the cornerstone for evaluating hormone receptor (ER, PR) and HER2 status in breast cancer, PD-L1 expression for immunotherapy selection, and mismatch repair (MMR) protein deficiency for identifying microsatellite instability (MSI) [47].
Experimental Workflow for Comprehensive Genomic Profiling
The following diagram illustrates the integrated workflow for tumor molecular profiling using multiple sequencing technologies:
Therapeutic Applications: From Biomarker Discovery to Targeted Treatments
Biomarkers Guiding Targeted Therapy Selection
Comprehensive genomic profiling identifies predictive biomarkers that directly inform treatment selection. Key biomarkers include:
Gene Fusions: Oncogenic fusions detected via RNA-Seq provide targets for specific inhibitors. For example, ALK fusions in NSCLC respond to alectinib, ROS1 fusions to entrectinib, and NTRK fusions across tumor types to larotrectinib [47].
Homologous Recombination Deficiency (HRD): Genomic scars indicating impaired DNA repair mechanisms predict sensitivity to PARP inhibitors in ovarian, breast, pancreatic, and prostate cancers [48] [47].
Tumor Mutational Burden (TMB): A high number of mutations per megabase of DNA correlates with improved response to immune checkpoint inhibitors across multiple cancer types [48].
Microsatellite Instability (MSI): Deficiency in DNA mismatch repair systems, detectable via NGS or IHC, predicts dramatic responses to PD-1 blockade regardless of tumor origin [47].
Integration of Molecular Data into Clinical Decision-Making
The following diagram illustrates how molecular profiling data informs therapeutic decision-making in precision oncology:
FDA-Approved Targeted Therapies in Oncology
Table 2: Selected FDA-Approved Targeted Therapies and Associated Biomarkers
| Therapeutic Agent | Cancer Type | Biomarker | Technology for Detection | Clinical Response Metrics |
|---|---|---|---|---|
| Alectinib | NSCLC | ALK fusions | RNA-Seq, FISH | Median PFS: 34.8 months |
| Trastuzumab | Breast/Gastric | HER2 amplification | FISH, IHC | 41% reduction in recurrence |
| Olaparib | Ovarian/Breast | BRCA1/2 mutations, HRD | WES, Genomic Scarring | 65% objective response rate |
| Larotrectinib | Pan-Cancer | NTRK fusions | RNA-Seq | 79% objective response rate |
| Pembrolizumab | Pan-Cancer | MSI-H/dMMR | IHC, NGS | 39.6% objective response rate |
| Dabrafenib + Trametinib | NSCLC/Melanoma | BRAF V600E mutation | WES, WGS | 63% overall response rate |
Computational and Data Science Approaches
Knowledge Graphs for Precision Medicine
Knowledge graphs have emerged as powerful computational frameworks for integrating heterogeneous biomedical data and generating clinically actionable insights. These structured representations connect entities—such as diseases, drugs, genes, proteins, and phenotypes—through semantically defined relationships, enabling sophisticated queries and inference [49] [50].
PrimeKG, a prominent precision medicine knowledge graph, integrates 20 high-quality resources to describe 17,080 diseases with over 4 million relationships across ten biological scales, including disease-associated protein perturbations, biological processes, pathways, anatomical and phenotypic scales, and approved drugs with their therapeutic actions [50]. This resource specifically incorporates 'indications', 'contradictions', and 'off-label use' drug-disease relationships that are typically sparse in other knowledge graphs, thereby supporting artificial intelligence analyses of how drugs affect disease-associated networks [50].
Artificial Intelligence in Biomarker Discovery and Drug Development
AI and machine learning algorithms are increasingly applied to multidimensional omics data to identify novel biomarkers, predict drug responses, and elucidate resistance mechanisms [46] [47]. These approaches include:
- Network-based analyses that model how therapeutic interventions perturb disease-associated molecular networks [50].
- Predictive modeling using transcriptomic data to forecast sensitivity or resistance to targeted therapies [47].
- Pattern recognition in complex datasets to identify molecular subtypes with distinct therapeutic vulnerabilities [49].
Implementation Challenges and Future Directions
Barriers to Clinical Adoption
Despite compelling scientific advances, multiple implementation challenges impede the widespread adoption of precision oncology:
- Reimbursement Structures: Current healthcare payment systems are poorly aligned with the one-time, high-cost nature of cell and gene therapies, particularly when benefits accrue over many years rather than within a single calendar year [51].
- Geographic Access Disparities: Treatment "deserts" persist where patients in rural areas have limited access to advanced molecular testing and specialized cancer centers offering targeted therapies [51].
- Infrastructure Requirements: Delivering complex therapies requires specialized facilities, trained personnel, and sophisticated supply chains that remain concentrated at major academic medical centers [51].
- Evidence Generation: Payers increasingly demand long-term durability data, which is challenging for novel therapies with limited follow-up periods [51].
Research Reagent Solutions for Precision Oncology
Table 3: Essential Research Tools and Technologies in Precision Oncology
| Research Tool | Provider/Example | Primary Function | Application in Precision Oncology |
|---|---|---|---|
| FoundationOneCDx | Foundation Medicine | Comprehensive genomic profiling (324 genes) | Detection of substitutions, indels, CNAs, rearrangements, MSI, TMB |
| FoundationOneRNA | Foundation Medicine | RNA sequencing (318 genes) | Gene fusion detection, complement to DNA sequencing |
| FoundationOneMonitor | Foundation Medicine | Circulating tumor DNA monitoring | Molecular response assessment, therapy resistance monitoring |
| PrimeKG Knowledge Graph | Precision Medicine KG | Multimodal data integration | Drug-disease relationship analysis, network medicine |
| Bgee Gene Expression | Bgee Database | Gene expression patterns | Anatomy-protein associations, expression quantification |
Emerging Trends and Future Perspectives
The field of precision oncology continues to evolve along several promising trajectories:
- Expansion Beyond Oncology: Cell and gene therapy approaches initially developed for cancer are now being investigated for autoimmune diseases, diabetes, and cardiovascular conditions [51].
- Earlier Intervention: Targeted therapies are increasingly moving into earlier lines of treatment as evidence of their efficacy grows, with the average number of patients treated per oncologist rising from 17 to 25 annually [51].
- Multimodal Data Integration: Combining genomic, transcriptomic, proteomic, and clinical data through unified computational frameworks will enable more holistic patient characterization and treatment selection [49] [47].
- Ethical and Equity Considerations: As precision medicine advances, ensuring equitable access across diverse populations and addressing potential biases in genomic databases remain critical priorities [46].
Gene expression profiling and targeted therapies represent transformative elements within the broader pharmacogenomics revolution that is fundamentally reshaping oncology research and clinical practice. The integration of comprehensive molecular diagnostics—including WGS, WES, and RNA-Seq—with sophisticated computational approaches enables increasingly precise matching of patients with optimal treatments based on the unique molecular characteristics of their tumors. While implementation challenges surrounding reimbursement, access, and infrastructure persist, the continued evolution of precision oncology promises to further refine cancer classification and therapeutic intervention, ultimately delivering on the paradigm of personalized medicine that is both predictive and preventive in its approach.
Pharmacogenomics represents a cornerstone of personalized medicine, enabling drug therapy to be tailored to an individual's genetic makeup to maximize efficacy and minimize adverse effects. This field has evolved from theoretical concept to clinical application, with robust evidence now supporting the implementation of pharmacogenomic testing for numerous medications across diverse therapeutic areas [52]. The fundamental premise is that genetic variations influence drug response through multiple mechanisms—altering drug metabolism, transport, or target interactions—which can be characterized and predicted through genetic testing. This technical review examines three well-established case studies—warfarin, thiopurines, and codeine—that exemplify the successful translation of pharmacogenomic principles into clinically actionable dosing strategies, providing valuable frameworks for researchers and drug development professionals working to advance personalized therapeutics.
The clinical implementation of pharmacogenomics follows several testing approaches: pre-emptive (conducted prior to prescribing), concurrent (performed at the time of prescribing in acute scenarios), reactive (conducted after an unexpected drug-related problem occurs), and incidental (when patients present with existing test results) [53]. For the drugs discussed in this review, pre-emptive or concurrent testing strategies are generally recommended to optimize initial dosing and prevent serious adverse events. The evidence base supporting these applications has grown substantially, with international consortia such as the Clinical Pharmacogenetics Implementation Consortium (CPIC) developing detailed guidelines to standardize the translation of genetic test results into clinical practice [53] [52].
Warfarin: Integrating Genetic and Clinical Factors for Anticoagulation Optimization
Genetic Determinants and Mechanism of Action
Warfarin, a widely used oral anticoagulant, exhibits substantial interindividual variability in dosing requirements, with daily doses ranging from 1–40 mg or more in different patients [54]. This variability stems from both genetic and environmental factors, with genes encoding the cytochrome P450 2C9 enzyme (CYP2C9) and vitamin K epoxide reductase complex subunit 1 (VKORC1) playing particularly significant roles. The CYP2C9 gene encodes the primary enzyme responsible for metabolizing the more potent S-enantiomer of warfarin to inactive metabolites [54]. Multiple polymorphisms of CYP2C9 have been identified that significantly influence enzyme activity, with the 2 and *3 variants demonstrating only 12% and 5% of the enzyme activity of the wild-type allele (1), respectively [54]. Patients carrying these variant alleles require significantly lower warfarin doses and experience an increased risk of bleeding complications, particularly during treatment initiation [54].
The VKORC1 gene encodes the molecular target of warfarin, which is responsible for recycling vitamin K epoxide to reduced vitamin K—an essential cofactor for activating coagulation factors II, VII, IX, and X [54]. Missense mutations in this gene explain inherited warfarin resistance in humans, while common polymorphisms significantly impact warfarin sensitivity in the general population [54]. The integration of genetic information for both CYP2C9 and VKORC1 with clinical factors provides a sophisticated approach to predicting individual warfarin requirements before commencing treatment.
Clinical Evidence and Dosing Algorithms
Research indicates that CYP2C9 genotype alone accounts for approximately 10–20% of the variability in warfarin maintenance dose, while the combination of genetic and clinical factors (including age, body surface area, sex, and concomitant drug use) explains between 29–39% of dose variability [54]. This evidence has led to the development of pharmacogenomic-guided dosing algorithms and nomograms designed to estimate warfarin requirements before treatment initiation, with the potential to reduce bleeding risk during the critical induction phase [54].
Clinical trials evaluating pharmacogenomic-guided warfarin dosing have demonstrated mixed but generally promising results. The European Pharmacogenetics of Anticoagulant Therapy (EU-PACT) trial, a multicenter, single-blinded randomized controlled trial, found that pharmacogenomic-guided dosing during the first 5 days of therapy resulted in significantly greater percentage of time in therapeutic range (67% vs. 60%), fewer patients with INR ≥4, and less time to achieve therapeutic INR levels compared to fixed dosing [55]. However, the Clarification of Optimal Anticoagulation Through Genetics (COAG) trial, which compared pharmacogenomic-guided dosing to clinical algorithm dosing, detected no significant differences in time in therapeutic range [55]. A key finding from COAG was a significant interaction between dosing strategy and race, with Black patients experiencing worse outcomes in the pharmacogenomic-guided group—highlighting the importance of including population-specific variants in dosing algorithms [55].
Figure 1: Warfarin Pharmacogenomic Pathways. This diagram illustrates the metabolic and pharmacodynamic pathways of warfarin, highlighting the key proteins influenced by genetic variations. CYP2C9 metabolizes warfarin to inactive compounds, while VKORC1 serves as drug target.
Quantitative Genetic Influences on Warfarin Dosing
Table 1: Key Genetic Variants Affecting Warfarin Response
| Gene | Variant | Functional Effect | Impact on Dose | Population Frequency |
|---|---|---|---|---|
| CYP2C9 | *2 (rs1799853) | 12% enzyme activity | ↓ 30-50% | 35% of Caucasians [54] |
| CYP2C9 | *3 (rs1057910) | 5% enzyme activity | ↓ 50-70% | 35% of Caucasians [54] |
| VKORC1 | c.-1639G>A | Reduced enzyme expression | ↓ 30-50% | High in Asians, variable in other populations [54] |
Table 2: Clinical Trial Outcomes of Pharmacogenomic-Guided Warfarin Dosing
| Trial | Participants | Intervention | Control | Primary Outcome | Result |
|---|---|---|---|---|---|
| EU-PACT [55] | 455 | PGx-guided dosing (first 5 days) | Fixed dosing | PTTR (12 weeks) | 67% vs. 60% (p<0.001) |
| COAG [55] | 1,015 | PGx-guided dosing (first 5 days) | Clinical algorithm | PTTR (4 weeks) | No significant difference |
| CoumaGen-II [55] | 504 vs. 1,866 | PGx-guided dosing | Standard dosing | Out-of-range INRs | Significant reduction with PGx |
Thiopurines: Precision Dosing in Oncology and Autoimmune Diseases
Metabolic Pathways and Genetic Determinants
Thiopurine drugs—including mercaptopurine, thioguanine, and the prodrug azathioprine—represent a classic example of pharmacogenomic implementation, particularly in the treatment of pediatric acute lymphoblastic leukemia (ALL) and inflammatory bowel diseases [56] [57]. These drugs undergo complex metabolic processes involving both catabolic and anabolic pathways that determine their therapeutic efficacy and toxicity profile. The anabolic pathway produces active thioguanine nucleotides (TGNs) that incorporate into DNA and RNA, impairing synthesis and leading to cell apoptosis [56] [57]. The catabolic pathway is mediated by thiopurine methyltransferase (TPMT), which converts thiopurines to inactive methylated metabolites [56].
The TPMT gene exhibits significant genetic polymorphism, with variant alleles associated with reduced enzyme activity. The 2, *3A, *3B, and *3C variants account for over 95% of inactivating mutations and show varying prevalence across ethnic populations [56] [57]. Approximately 0.3% of the general population has low TPMT activity, while 10% has intermediate activity, both conferring increased risk of severe myelosuppression with standard thiopurine dosing [57]. More recently, variations in the *NUDT15 gene have also been identified as important determinants of thiopurine intolerance, particularly in Asian populations [56]. The NUDT15 gene encodes a diphosphatase that catalyzes the hydrolysis of nucleoside triphosphates, including active thiopurine metabolites [56].
Clinical Implementation and Monitoring
Clinical guidelines now recommend TPMT and NUDT15 testing before initiating thiopurine therapy to guide initial dosing [56] [53]. Patients with intermediate enzyme activity typically require 30-50% dose reductions, while those with complete deficiency should receive 10-fold lower doses or alternative medications [56]. Therapeutic drug monitoring of metabolite levels—specifically erythrocyte levels of 6-thioguanine nucleotides (6-TGN) and 6-methylmercaptopurine (6-MMP)—provides an additional tool for optimizing therapy [56] [57]. In inflammatory bowel disease, 6-TGN concentrations between 230-450 pmol/8×10⸠red blood cells are associated with therapeutic efficacy, while levels above this range correlate with myelosuppression [56]. 6-MMP concentrations above 5,700 pmol/8×10⸠red blood cells are associated with hepatotoxicity [56].
The implementation of thiopurine pharmacogenetics has been particularly successful in pediatric oncology, where treatment protocols routinely incorporate TPMT genotyping to personalize mercaptopurine dosing during maintenance therapy for ALL [56]. This approach has contributed to the outstanding 5-year survival rates exceeding 90% now achieved in developed countries, while reducing the incidence of severe hematological toxicity [56].
Figure 2: Thiopurine Metabolic Pathways. This diagram illustrates the metabolic activation and inactivation pathways of thiopurine drugs, highlighting the roles of TPMT and NUDT15 enzymes. Genetic variations in these enzymes significantly influence drug toxicity and efficacy.
Genetic Variants and Clinical Management
Table 3: Key Genetic Variants Affecting Thiopurine Response
| Gene | Variant | Functional Effect | Clinical Impact | Dosing Recommendation |
|---|---|---|---|---|
| TPMT | *2 (rs1800462) | Reduced enzyme activity | Severe leukopenia, hematological toxicity | Reduce dose by 30-50% for intermediate activity, 90% for low activity [56] |
| TPMT | *3A (rs1800460) | Reduced enzyme activity | Severe leukopenia, hematological toxicity | Reduce dose by 30-50% for intermediate activity, 90% for low activity [56] |
| TPMT | *3C (rs1142345) | Reduced enzyme activity | Severe leukopenia, hematological toxicity | Reduce dose by 30-50% for intermediate activity, 90% for low activity [56] |
| NUDT15 | rs116855232 (p.Arg139Cys) | Loss of function | Thiopurine intolerance, leukopenia | Reduce dose substantially; consider alternative therapy [56] |
Table 4: Therapeutic Ranges for Thiopurine Metabolite Monitoring
| Metabolite | Therapeutic Range | Subtherapeutic | Toxic Range | Clinical Correlation |
|---|---|---|---|---|
| 6-TGN | 230-450 pmol/8×10⸠RBC (IBD) [56] | <235 pmol/8×10⸠RBC | >450-1000 pmol/8×10⸠RBC (variable by protocol) | Efficacy; higher levels associated with myelosuppression [56] [57] |
| 6-MMP | Not applicable | Not applicable | >5700 pmol/8×10⸠RBC | Hepatotoxicity [56] |
Codeine: Pharmacogenomics of Opioid Analgesia and Toxicity
CYP2D6 Metabolism and Clinical Consequences
Codeine represents a compelling case study in pharmacogenomics, demonstrating how genetic variation can dramatically alter the safety profile of a widely prescribed medication. Codeine is a prodrug that must be bioactivated via the cytochrome P450 2D6 (CYP2D6) enzyme to morphine to exert its analgesic effects [58] [52]. The CYP2D6 gene is highly polymorphic, with over 100 variants that create a continuum of metabolic activity categorized into four primary phenotypes: poor metabolizers (PMs), intermediate metabolizers (IMs), normal metabolizers (NMs), and ultrarapid metabolizers (UMs) [58] [52].
This genetic variation has profound clinical implications. Ultrarapid metabolizers experience rapid and extensive conversion of codeine to morphine, resulting in potentially toxic morphine levels even at standard codeine doses [58] [52]. This has led to fatal outcomes in several documented cases, particularly in children undergoing tonsillectomy or adenoidectomy, and in breastfed infants of mothers who were UMs taking codeine for postpartum pain [52]. In response to these safety concerns, the U.S. Food and Drug Administration (FDA) has contraindicated codeine use in all children younger than 12 years old and in patients under 18 after tonsillectomy or adenoidectomy [58] [52]. Conversely, poor metabolizers experience inadequate conversion of codeine to morphine, resulting in subtherapeutic analgesic response [58].
Clinical Implementation and Alternative Opioids
The pharmacogenomics of codeine presents a challenging risk-benefit calculus for clinicians. While the FDA contraindication provides a blanket protection strategy, some experts have advocated for a more nuanced approach utilizing CYP2D6 genotyping to identify patients who could safely benefit from codeine [58]. This approach would involve testing patients prior to prescribing and restricting codeine use to those with normal or intermediate metabolizer status, while avoiding it in both poor and ultrarapid metabolizers [58]. This strategy has been successfully implemented in specific patient populations, such as children with sickle cell disease who experience vaso-occlusive crises and may benefit from having acetaminophen with codeine—the only Schedule III opioid—as a therapeutic option [58].
It is important to note that the pharmacogenomic considerations extend beyond codeine to other opioids that are CYP2D6 substrates, including tramadol, hydrocodone, and oxycodone [59] [52]. Tramadol carries the same FDA boxed warning as codeine, contraindicating its use in children, and should not be considered as an automatic alternative to codeine without genotyping [52]. Research has demonstrated that genotype-guided prescribing of CYP2D6-metabolized opioids can lead to improved pain control, with one pragmatic study showing that in over 75% of CYP2D6 intermediate or poor metabolizers, opioids were appropriately replaced with non-opioid alternatives for pain management [52].
Figure 3: Codeine Pharmacogenomics and Clinical Consequences. This diagram illustrates the bioactivation of codeine to morphine via CYP2D6 and the clinical consequences of genetic variation in this enzyme. Ultrarapid metabolizers are at risk for toxicity, while poor metabolizers may experience reduced analgesia.
CYP2D6 Phenotypes and Clinical Recommendations
Table 5: CYP2D6 Phenotypes and Clinical Implications for Codeine
| Phenotype | Enzyme Activity | Codeine to Morphine Conversion | Clinical Risk | Prescribing Recommendation |
|---|---|---|---|---|
| Ultrarapid Metabolizer (UM) | Increased | Rapid and extensive | Respiratory depression, toxicity | Contraindicated; use alternative analgesic [58] [52] |
| Normal Metabolizer (NM) | Normal | Standard | Standard therapeutic response | Appropriate candidate for therapy [58] |
| Intermediate Metabolizer (IM) | Reduced | Diminished | Reduced efficacy | May require higher doses; consider alternatives [58] |
| Poor Metabolizer (PM) | Deficient | Minimal | Therapeutic failure | Contraindicated; use alternative analgesic [58] [52] |
Table 6: Clinical Evidence for Codeine Pharmacogenomic Implementation
| Study | Population | Intervention | Outcomes | Implications |
|---|---|---|---|---|
| Gammal et al. [58] | 830 patients with sickle cell disease | CYP2D6-guided codeine prescribing | Codeine avoided in 100% of UM and PM patients | Demonstrated feasibility of genotype-guided approach |
| FDA Adverse Event Reports [58] | Pediatric patients (<18 years) | Case reviews | 64 cases of severe respiratory depression; 10 deaths | Led to boxed warning and contraindications |
| Smith et al. [52] | Patients prescribed CYP2D6-metabolized opioids | Genotype-guided prescribing | Improved pain control; opioids replaced in >75% of IM/PM patients | Supports utility of preemptive testing |
Research Reagent Solutions: Essential Methodologies and Tools
Advancing research in pharmacogenomics requires specialized reagents and methodologies tailored to genetic analysis and clinical implementation. The following toolkit outlines essential resources for investigators working in this field.
Table 7: Essential Research Reagents and Methodologies for Pharmacogenomic Studies
| Category | Specific Tools/Assays | Research Application | Technical Considerations |
|---|---|---|---|
| Genotyping Technologies | PCR-RFLP, TaqMan assays, RT-PCR, microarray, next-generation sequencing | Variant detection and allele frequency determination | Platform choice depends on throughput needs, number of targets, and budget constraints [56] [57] |
| Metabolite Monitoring | HPLC, LC-MS/MS | Quantification of drug metabolites (e.g., 6-TGN, 6-MMP for thiopurines) | Essential for correlating genotype with phenotype; requires specialized instrumentation [56] [57] |
| Clinical Databases | PharmGKB, CPIC Guidelines, FDA Table of Pharmacogenomic Biomarkers | Evidence-based clinical implementation | Curated databases provide clinically actionable recommendations [59] [52] |
| Functional Assay Systems | Recombinant enzyme systems, cell-based assays (e.g., insect cells for VKORC1) [54] | Characterization of novel variants and mechanism studies | Determine functional impact of genetic variants; establish genotype-phenotype correlations |
The case studies of warfarin, thiopurines, and codeine exemplify the progressive maturation of pharmacogenomics from basic discovery to clinical application. Each drug demonstrates distinct aspects of implementation: warfarin illustrates the complexity of integrating multiple genetic and clinical factors into dosing algorithms; thiopurines represent the successful incorporation of pharmacogenetics into treatment protocols for life-threatening conditions; and codeine highlights the critical importance of pharmacogenomics in drug safety and regulatory decision-making. Together, they provide powerful evidence for the role of pharmacogenomic testing in personalized medicine.
Future advances in pharmacogenomics will require addressing several key challenges, including the development of ethnically diverse reference databases [55] [23], the creation of clinical decision support systems integrated into electronic health records [52], and the establishment of cost-effective implementation models [53] [52]. Additionally, as sequencing technologies continue to advance and costs decline, pre-emptive pharmacogenomic testing using multi-gene panels is likely to become more widespread, enabling the generation of genetic data that can inform prescribing decisions across multiple drugs throughout a patient's lifetime [53] [52]. The ongoing translation of pharmacogenomic discoveries into clinically actionable guidelines will continue to advance the field of personalized medicine, ultimately enabling more precise, safe, and effective drug therapy tailored to individual genetic profiles.
Preemptive Genotyping Strategies and Clinical Decision Support Systems
Preemptive pharmacogenomic (PGx) testing represents a paradigm shift in personalized medicine, moving from reactive, single-gene testing to a proactive model where a patient's genetic makeup is characterized before drug prescriptions are written. This approach aims to optimize medication efficacy and safety by guiding drug selection and dosing at the point of care [60] [61]. The clinical imperative for this strategy is underscored by the significant public health burden of adverse drug reactions (ADRs), which are a leading cause of hospitalization and mortality worldwide [60]. It is estimated that 3–6% of hospital admissions in the United States and 2.5–10.6% in Europe are due to ADRs [60]. Furthermore, carrying a genetic variant that alters the efficacy or safety of a drug is not rare; four out of five patients are likely to carry such a variant affecting commonly prescribed medications [60]. Preemptive genotyping ensures that this genetic information is available within the electronic health record (EHR), enabling Clinical Decision Support (CDS) systems to deliver genetically-guided prescribing recommendations when needed, thus preventing avoidable harm and improving therapeutic outcomes [60] [61] [62].
Implementation Strategies and Workflows
Successful implementation of preemptive PGx requires a structured, institution-wide approach that integrates sequencing, bioinformatics, data storage, and clinical decision support. The overarching workflow moves from patient identification and testing to the integration of results and the activation of CDS tools.
Core Preemptive Genotyping Workflow
The following diagram illustrates the end-to-end process for implementing a preemptive genotyping strategy, from patient identification to the point of clinical prescribing.
Key Strategic Considerations
Preemptive vs. Reactive Testing: Unlike reactive testing, which occurs in response to a specific drug prescription or an adverse event, preemptive testing involves screening patients for multiple pharmacogenetic variants prior to any drug therapy indication. This model allows genetic data to be available "on-demand" throughout a patient's lifetime, maximizing its utility for future prescriptions [61] [62].
Genotyping versus Sequencing: While targeted genotyping panels (e.g., Thermo Fisher's Axiom PharmacoScan Assay) are commonly used for cost-effectiveness, DNA sequencing (as in the Mayo-Baylor RIGHT 10K study) offers a more comprehensive approach. Sequencing can identify rare and novel variants that genotyping might miss. The RIGHT 10K study found that DNA sequencing identified an average of 3.3 additional conservatively predicted deleterious variants per patient compared to what genotyping would have revealed [63].
Defining the Gene Panel: The selection of genes and variants is critical. Panels are typically designed around genes with strong clinical evidence, often curated from resources like the Pharmacogenomics Knowledgebase (PharmGKB) and guidelines from the Clinical Pharmacogenetics Implementation Consortium (CPIC) or the Dutch Pharmacogenetics Working Group (DPWG) [60] [64]. A key finding from implementation studies is the high prevalence of actionable pharmacogenetic variation. The PREPARE study found that 93.5% of patients had at least one actionable gene variant [60], while the RIGHT 10K study showed that 99% of subjects carried an actionable variant in at least one of five key genes (SLCO1B1, CYP2C19, CYP2C9, VKORC1, CYP2D6) [60].
Quantitative Evidence and Clinical Impact
Robust evidence from large-scale studies demonstrates the clinical and economic benefits of preemptive pharmacogenomics. The data below summarize key outcomes from major implementation projects.
Table 1: Clinical Outcomes from Major Preemptive PGx Implementation Studies
| Study/Program | Study Design & Scale | Key Genes Tested | Primary Clinical Outcomes |
|---|---|---|---|
| PREPARE Study [60] | Randomized controlled trial (n=6,944) across Europe | CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP3A5, DPYD, F5, HLA-B, SLCO1B1, TPMT, UGT1A1, VKORC1 | 33% reduction in the incidence of clinically relevant adverse drug reactions (ADRs) in the genotyped group (21.5% vs. 28.6% in control). |
| Elliott et al. [60] | Prospective, open-label, randomized controlled trial | 6 genes (specific genes not listed in excerpt) | 52% reduction in ADRs; 52% fewer rehospitalizations and 42% fewer emergency department visits at 60-day follow-up. |
| Brixner et al. [60] | Cohort study in elderly patients | Cytochrome P450 (CYP) genes | Lower hospitalization rates (9.8% vs. 16.1%) and ED visit rates (4.4% vs. 15.4%) in the PGx-tested group. Mean cost savings of $218 per patient. |
| PREDICT Program [60] | Preemptive implementation (first 10,000 patients) | 34-gene VeraCode ADME core panel | 91% of patients had at least one variant in the tested drug-gene pairs, demonstrating high prevalence of actionable findings. |
| PGEN4Kids (St. Jude's) [60] | Preemptive testing in pediatric population (n=1,559) | ~300 genes | 78% of pediatric patients had at least one actionable pharmacogenetic variant. |
Table 2: Economic and Health System Impact of PGx CDS
| Aspect | Quantitative Finding | Source/Context |
|---|---|---|
| Cost-Effectiveness | Incremental cost-effectiveness ratio (ICER) of $39,477 per QALY gained for a PGx CDS alert program for clopidogrel and warfarin. | Cost-utility analysis from a health system perspective [65]. |
| Adverse Event Prevention | The CDS alert program helped avoid 16 major clinical events and 6 deaths for ACS (clopidogrel) and 2 clinical events and 0.9 deaths for AF (warfarin). | Model based on a 500,000-member health system [65]. |
| ADR-Related Hospitalization Costs | Estimated cost of treating an ADR ranges from $13,994 (non-ICU) to $19,685 (ICU). | Review of real-world evidence [60]. |
| Actionable Prescriptions | In 2013, 18% of all U.S. prescriptions (738 million) were for drugs with CPIC level A or B evidence for a pharmacogenetic interaction. | Analysis of prescription data [61]. |
Clinical Decision Support System Architecture
The CDS is the critical link that transforms static genetic data in the EHR into dynamic, actionable guidance for clinicians. Effective CDS integration is a cornerstone of successful preemptive genotyping programs [66] [62].
The "Five Rights" of CDS Design
To be effective, PGx CDS must adhere to the "five rights" framework: delivering the right information, to the right person, in the right intervention format, through the right channel, at the right time in the workflow [66].
- Right Information: The CDS should provide an actionable recommendation, not just raw genetic data. Where possible, it should include therapeutic alternatives to the drug being prescribed [66]. The most common level of detail used is the phenotype (e.g., "poor metabolizer"), as this is what clinical guidelines like CPIC and DPWG use for their recommendations [66].
- Right Person: Alerts should primarily target the prescribing clinician, but may also be valuable to clinical pharmacists involved in medication therapy management [66].
- Right Intervention Format & Channel: CDS tools can be active (interruptive alerts) or passive (integrated summary reports, banners in the EHR). User research indicates that PGx data must be incorporated within existing EHRs and displayed within the prescribing workflow, rather than in a static, standalone portal [62].
- Right Time: The ideal moment for an alert is when the prescriber is ordering a medication for which the patient has a clinically actionable PGx result [66] [62].
Technical Implementation and CDS Workflow
The logical process of a PGx CDS system, from data input to user interaction, is detailed in the following diagram.
The Scientist's Toolkit: Research Reagent Solutions
The transition of preemptive PGx from research to clinical application relies on a suite of robust technological platforms and reagents. The following table catalogues key solutions utilized in the field.
Table 3: Essential Research Reagents and Platforms for Preemptive PGx
| Tool / Reagent Solution | Function / Description | Example Use Case / Product |
|---|---|---|
| Targeted Genotyping Microarrays | High-throughput, cost-effective profiling of predefined sets of high-evidence PGx variants. Ideal for population-scale screening. | Thermo Fisher Axiom PharmacoFocus Assay (configurable, up to 2,000 variants in 150 genes) [64]. |
| Comprehensive PGx Microarrays | Broader profiling that includes both high-evidence and putative PGx variants, enabling translational research. | Thermo Fisher Axiom PharmacoScan Assay (4,627 variants in 1,191 genes) [64]. |
| Next-Generation Sequencing (NGS) | Provides a complete view of pharmacogenes by identifying novel, rare, and structural variants beyond the scope of genotyping arrays. | Targeted capture sequencing of 77 pharmacogenes (Mayo-Baylor RIGHT 10K study) [63]. |
| Bioinformatic Analysis Suites | Software that translates raw genotype data into functional star alleles and predicted phenotype assignments (e.g., "rapid metabolizer"). | Applied Biosystems Axiom Analysis Suite; third-party tools from Coriell Life Sciences & Translational Software [64]. |
| Clinical Decision Support (CDS) Software | Platforms that integrate PGx results into the EHR and provide the logic for triggering alerts and recommendations based on clinical guidelines. | Custom institutional builds informed by user-centered design [62]; systems implementing CPIC/DPWG rules [66]. |
| ZXH-3-26 | ZXH-3-26, CAS:2243076-67-5, MF:C38H37ClN8O7S, MW:785.27 | Chemical Reagent |
| SARS-CoV-2-IN-15 | SARS-CoV-2-IN-15, MF:C14H9ClF3NO2, MW:315.67 g/mol | Chemical Reagent |
Detailed Experimental Protocol: Preemptive PGx Implementation
The following protocol is synthesized from large-scale studies like the Ubiquitous Pharmacogenomics (U-PGx) Consortium's PREPARE study and the Mayo-Baylor RIGHT 10K study [60] [63].
Stage 1: Patient Identification and Sample Acquisition
- Participant Recruitment: Identify a target population within a healthcare system (e.g., primary care patients, biobank participants). Obtain informed consent for preemptive genotyping and storage of genetic data in the EHR for clinical use.
- Sample Collection: Collect DNA from participants via blood draw or saliva kit. For the RIGHT 10K study, DNA was sourced from consented Mayo Clinic Biobank volunteers [63].
Stage 2: Genotyping and Sequencing
- Method Selection: Choose a genotyping or sequencing platform based on the project's goals (e.g., breadth of variant coverage, cost, throughput).
- Genotyping Protocol: Use a targeted microarray (e.g., Axiom PharmacoScan) following the manufacturer's instructions. Briefly, this involves whole-genome amplification, fragmentation, precipitation, resuspension, hybridization to the array, staining, and imaging on a gene chip scanner [64].
- Sequencing Protocol: For a more comprehensive approach, use targeted oligonucleotide-capture sequencing. Design probes to capture the exonic and important intronic regions of a defined set of pharmacogenes (e.g., 77 genes). Perform library preparation, hybridize with the capture panel, sequence on a high-throughput platform (e.g., Illumina), and align sequences to a reference genome (e.g., GRCh38) [63].
Stage 3: Bioinformatic Analysis and Phenotype Calling
- Variant Calling: From sequencing data, identify single nucleotide variants (SNVs), insertions/deletions (indels), and copy number variations (CNVs) using a bioinformatics pipeline (e.g., GATK best practices).
- Diplotype Assignment: Translate the identified variants into star alleles (haplotypes) for each gene (e.g.,
*1/*2for CYP2C19). This requires specialized software and curated databases like the Pharmacogene Variation (PharmVar) Consortium. - Phenotype Prediction: Assign a predicted phenotype based on the diplotype combination according to standard consensus definitions (e.g., CPIC). The possible phenotypes are:
- Poor Metabolizer (PM)
- Intermediate Metabolizer (IM)
- Normal Metabolizer (NM)
- Rapid Metabolizer (RM)
- Ultrarapid Metabolizer (UM)
Stage 4: Clinical Integration and CDS Activation
- Data Integration: Securely deposit the predicted phenotypes (e.g., "CYP2C19: IM") into the EHR, typically in a dedicated genomic results section or a structured clinical repository.
- CDS Rule Creation: Develop and implement a set of drug-gene interaction rules within the EHR's CDS system. These rules should be based on current clinical guidelines (e.g., CPIC Level A). For example:
IF patient.phenotype.CYP2C19 = 'PM' OR 'IM' AND drug.order = clopidogrel THEN trigger alert[66] [62]. - CDS Tool Deployment: Configure the type of alert (active vs. passive) based on the severity of the interaction and feedback from clinician stakeholders to minimize alert fatigue [66] [62].
Pharmacogenomics has emerged as a cornerstone of precision medicine, addressing the fundamental principle that "one drug does not fit all" [1]. The field has experienced rapid advancement, particularly in understanding and preventing severe cutaneous adverse reactions (SCARs) – rare but life-threatening T-cell-mediated drug hypersensitivity reactions with significant morbidity and mortality [67] [68]. These reactions, including Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) and drug reaction with eosinophilia and systemic symptoms (DRESS), represent a major challenge in drug development and clinical therapy [67] [69].
The human leukocyte antigen (HLA) system, encoded by the most polymorphic region of the human genome on chromosome 6p21.3, plays a pivotal role in immune-mediated drug reactions [68] [1]. HLA molecules present peptide antigens to T-cells, and specific HLA polymorphisms can alter the peptide-binding groove, enabling certain drugs or their metabolites to be recognized as foreign, thereby triggering a destructive immune response [68]. The co-dominant expression of HLA genes means that susceptibility to drug hypersensitivity depends on the presence or absence of specific risk alleles [68].
This technical guide examines the critical role of HLA pharmacogenomics in predicting and preventing SCARs, framing this specialized field within the broader context of personalized medicine research aimed at optimizing drug safety through genetic stratification.
HLA System Fundamentals and SCAR Pathogenesis
HLA Molecular Biology and Nomenclature
The HLA complex comprises two major classes of molecules with distinct functions and tissue distributions. HLA class I molecules (HLA-A, -B, and -C) are expressed on virtually all nucleated cells and present intracellularly derived peptides to CD8+ cytotoxic T-cells. These molecules consist of a polymorphic α chain noncovalently associated with β2-microglobulin [68]. In contrast, HLA class II molecules (HLA-DR, -DQ, and -DP) are primarily expressed on professional antigen-presenting cells and present exogenous antigens to CD4+ T-helper cells, consisting of both α and β chains [68].
The WHO Nomenclature Committee standardizes HLA allele names using a specific system: the asterisk () signifies molecular typing, followed by numbers separated by colons denoting the allele group (first field), specific protein (second field), synonymous mutations (third field), and non-coding variations (fourth field) [68]. For example, HLA-B58:01:01:01L represents a specific allele with all four fields defined.
Mechanistic Basis of HLA-Associated SCARs
The pathogenesis of HLA-associated SCARs involves drug-specific interactions with HLA molecules that trigger aberrant T-cell responses. Several mechanistic models have been proposed, including:
- The hapten/prohapten model: Drugs or metabolites bind covalently to peptides or HLA molecules, creating novel antigenic determinants.
- The pharmacological interaction (p-i) model: Drugs bind reversibly but directly to HLA molecules or T-cell receptors, stimulating T-cells without conventional processing.
- The altered peptide repertoire model: Drugs alter the repertoire of self-peptides presented by HLA molecules, inducing autoimmunity.
For allopurinol, the metabolite oxypurinol binds non-covalently to the peptide-binding groove of HLA-B58:01, altering the presented peptide repertoire and activating CD8+ T-cells [70]. Similarly, carbamazepine directly interacts with HLA-B15:02, activating T-cells in patients with Stevens-Johnson syndrome [69].
The following diagram illustrates the mechanistic basis of HLA-associated SCARs:
Established HLA-Drug Associations for SCARs
Key HLA Allele-Drug Combinations
Substantial evidence has established strong associations between specific HLA alleles and drug-induced SCARs across diverse populations. These associations demonstrate considerable ethnic variation in allele frequencies and risk magnitudes, underscoring the importance of population-specific screening strategies [68] [1] [70].
Table 1: Established HLA Allele Associations with Drug-Induced SCARs
| Drug | HLA Allele | Adverse Reaction | Odds Ratio (Range) | Ethnic Populations at Highest Risk |
|---|---|---|---|---|
| Allopurinol | HLA-B*58:01 | SJS/TEN, DRESS | 117.6 (70.3-196.8) [70] | Han Chinese, Korean, Thai [70] [69] |
| Allopurinol | HLA-A*34:02 | SCARs | 20.6 (3.3-131.1) [67] | US populations (particularly Black individuals) [67] |
| Carbamazepine | HLA-B*15:02 | SJS/TEN | Strong association (ethnic-specific) [1] [69] | Han Chinese, Malaysian, Thai [1] |
| Carbamazepine | HLA-A*31:01 | Hypersensitivity, SCARs | Moderate association [1] | Japanese, Native American, Southern Indian [1] |
| Abacavir | HLA-B*57:01 | Hypersensitivity syndrome | Strong association [69] | European, African populations [69] |
Population-Specific Allele Prevalence and Risk Stratification
The prevalence of risk alleles varies significantly across ethnic groups, influencing screening recommendations and risk stratification approaches. For HLA-B*58:01, the prevalence ranges from 7.7% in Asian populations to 2.3% in White European populations [70]. Within Asian subgroups, South and Southeast Asian populations show particularly high prevalence (12.9%) compared to East and Central Asian populations (5.5%) [70].
A 2025 genetic association study revealed that HLA-B58:01 was absent in more than one-third of US patients with allopurinol-induced SCARs, indicating incomplete risk prediction with single-allele screening in ethnically diverse populations [67]. This study identified HLA-A34:02 as a second independent genetic risk factor in US populations, particularly significant for Black individuals who demonstrate both increased SCAR risk and higher HLA-B*58:01 carriage rates [67].
Methodological Approaches for HLA Screening in Research and Clinical Practice
HLA Genotyping Technologies
Multiple molecular techniques are available for HLA genotyping, offering varying levels of resolution appropriate for different research and clinical applications:
- Sequence-Specific Oligonucleotide PCR (SSO-PCR): Medium-resolution method using probe hybridization patterns; suitable for initial screening.
- Sequence-Specific Primer PCR (SSP-PCR): Medium-resolution method using allele-specific primers; provides rapid results.
- Sanger sequencing: Historically the gold standard for high-resolution typing; labor-intensive but comprehensive.
- Next-generation sequencing (NGS): Current high-resolution gold standard; enables complete sequencing of HLA genes across all polymorphic regions [67] [71].
- SNP-based imputation: Computational approach inferring HLA types from genome-wide SNP data; cost-effective for large cohorts but with reduced accuracy [67].
The choice of methodology depends on the required resolution, throughput, cost constraints, and application (research vs. clinical). For clinical screening, regulatory standards such as Clinical Laboratory Improvement Amendments (CLIA) certification ensure test quality and reliability [1].
Experimental Design and Protocol Considerations
Well-designed studies investigating HLA-SCAR associations require careful methodological planning:
Case Definition and Ascertainment:
- Cases should be specialist-adjudicated using standardized diagnostic criteria (e.g., international consensus criteria for SJS/TEN, DRESS) [67].
- Phenotypic heterogeneity necessitates precise clinical classification and documentation of reaction patterns.
- Multicenter collaboration is often essential to accrue sufficient cases for adequately powered analyses.
Control Group Selection:
- Drug-tolerant controls (patients exposed to the drug for ≥90 days without adverse effects) provide the most relevant comparison [67].
- Population controls help assess allele frequency in the general population but cannot assess drug-specific risks.
- Matching for ethnicity, age, and sex minimizes confounding in genetic association studies.
Statistical Analysis:
- Logistic regression models (additive genetic models typically preferred) test allele-phenotype associations [67] [71].
- Multiple testing corrections (e.g., Bonferroni, false discovery rate) are essential given the numerous HLA alleles tested.
- For novel associations, replication in independent cohorts strengthens validity.
- Sample size considerations should account for allele frequency, effect size, and statistical power.
The following diagram illustrates a representative experimental workflow for HLA-SCAR association studies:
Table 2: Essential Research Reagents and Resources for HLA-SCAR Studies
| Resource Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| Bioinformatics Databases | PharmGKB (https://www.pharmgkb.org/) [72] | Curated knowledge base of drug-gene relationships | Clinical guidelines, drug labels, variant annotations |
| ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) [72] | Archive of human genetic variants and phenotypes | Clinical assertions, evidence summaries | |
| PGRN Hub (http://www.pgrn.org/) [72] | Pharmacogenomics research network portal | Research collaboration, data sharing | |
| Analytical Tools | MiDAS R package [67] | Statistical analysis of HLA data | Case-control association testing, omnibus tests |
| PyHLA [71] | HLA association analysis | Logistic regression implementation for HLA data | |
| SNP2HLA [67] | HLA imputation from SNP data | Reference panel-based genotype inference | |
| Laboratory Reagents | NGS HLA typing panels [67] [71] | High-resolution HLA genotyping | Comprehensive coverage of classical HLA loci |
| HLA allele-specific antibodies | Serological confirmation | Traditional typing method validation | |
| Quality control biomarkers [67] | Sample quality assessment | DNA quantification, contamination checks | |
| Clinical Resources | CPIC Guidelines (https://cpicpgx.org/) [1] | Clinical implementation guidelines | Gene-drug clinical practice recommendations |
| FDA Table of Pharmacogenomic Biomarkers [72] | Regulatory guidance | Drug labeling information, safety data |
Global Regulatory Landscape and Clinical Implementation
The integration of HLA pharmacogenomics into clinical practice and drug development requires navigating a complex global regulatory environment. The United States has established a comprehensive pharmacogenomics framework, with the FDA issuing guidance documents, maintaining a table of pharmacogenomic biomarkers in drug labeling, and regulating genetic tests [1]. Internationally, the Clinical Pharmacogenetics Implementation Consortium (CPIC) develops globally recognized guidelines to facilitate the translation of genetic test results into therapeutic recommendations [1].
Significant variability exists in national policies regarding HLA screening. For example, HLA-B*15:02 screening prior to carbamazepine therapy is standard in many Asian countries with high allele prevalence but less consistently implemented in Western populations where the allele is rare [1]. The World Health Organization has established a Technical Advisory Group on Genomics to promote equitable implementation and address ethical, legal, and social implications [1].
Economic analyses demonstrate that HLA screening for high-risk drugs can be cost-effective, particularly in populations with elevated allele frequencies [70]. Successful implementation requires multidisciplinary collaboration across clinical pharmacology, dermatology, immunology, and laboratory medicine, supported by clinical decision support systems integrated into electronic health records.
Future Directions and Research Opportunities
Despite significant advances, important challenges and opportunities remain in HLA pharmacogenomics for SCAR prediction:
Beyond HLA: While HLA alleles represent the strongest known genetic risk factors, they demonstrate incomplete penetrance, suggesting additional genetic, environmental, or immunological modifiers. Genome-wide association studies may identify novel non-HLA loci contributing to SCAR susceptibility.
Functional Validation: Establishing mechanistic links between HLA alleles and SCAR pathogenesis through structural biology, immunology, and T-cell receptor repertoire studies remains a priority for validating association findings.
Multi-allele Risk Prediction: As evidenced by the discovery of HLA-A*34:02 in allopurinol-induced SCARs, multi-allele risk models may improve prediction across diverse populations [67]. Developing polygenic risk scores incorporating both HLA and non-HLA variants represents a promising direction.
Standardization and Harmonization: International efforts to standardize phenotyping, genotyping methodologies, and data reporting will facilitate meta-analyses and clinical translation.
Global Health Equity: Ensuring equitable access to pharmacogenomic testing across healthcare systems and ethnic groups remains a critical challenge requiring innovative implementation strategies and resource-appropriate technologies.
The continued integration of HLA pharmacogenomics into drug development and clinical practice promises to enhance patient safety while optimizing therapeutic efficacy, embodying the core principles of personalized medicine. As evidence accumulates and technologies advance, pre-prescription genetic screening for high-risk drugs is likely to expand, reducing the burden of severe adverse drug reactions through proactive risk stratification.
Overcoming Implementation Challenges: Technical, Economic and Infrastructure Barriers
Pharmacogenomics (PGx) represents a cornerstone of precision medicine, enabling healthcare providers to optimize drug selection and dosing based on an individual's genetic makeup. This whitepaper synthesizes current evidence on the cost-effectiveness of PGx testing across diverse healthcare economies. Economic evaluations demonstrate that approximately 71% of PGx-guided treatment strategies for drugs with Clinical Pharmacogenetics Implementation Consortium (CPIC) Level A evidence are cost-effective or cost-saving in developed healthcare systems [73]. Key drivers of value include reduced adverse drug reactions (ADRs), improved drug efficacy, and decreased hospitalizations. However, significant disparities exist in implementation capabilities and economic evidence between developed and developing nations, with the latter facing unique challenges related to infrastructure, funding, and genetic diversity. This analysis provides researchers, scientists, and drug development professionals with comprehensive methodological frameworks, current evidence synthesis, and future directions to advance the economically sustainable integration of PGx into global healthcare systems.
Pharmacogenomics studies how inherited genetic variation affects an individual's response to drugs, enabling more precise, effective, and safer therapeutic interventions [74]. The clinical relevance of PGx is substantiated by the U.S. Food and Drug Administration (FDA) listing of pharmacogenomic biomarkers in over 500 drug labels and CPIC guidelines that translate genetic data into actionable prescribing recommendations for approximately 70 drugs [1] [75]. PGx has demonstrated particular utility in mitigating adverse drug reactions, which account for 5-7% of hospital admissions globally and represent a leading cause of morbidity and mortality [76].
The economic evaluation of PGx interventions is crucial for their widespread adoption, particularly as healthcare systems worldwide face increasing pressure to maximize value from finite resources. Economic analyses of PGx testing must account for not only the direct costs of genetic testing but also downstream healthcare utilization, medication changes, and long-term health outcomes. Understanding these economic dimensions is essential for researchers and drug development professionals working to integrate PGx into the paradigm of personalized medicine across diverse global contexts.
Global Market Landscape and Adoption Trends
The pharmacogenomics market reflects accelerating clinical adoption and significant economic potential. Current valuations and projections illustrate robust growth driven by technological advancements, increasing demand for personalized medicine, and expanding clinical applications.
Table 1: Global Pharmacogenomics Market Overview
| Metric | 2024 Valuation | 2030/2034 Projection | Compound Annual Growth Rate (CAGR) |
|---|---|---|---|
| Market Size (2024) | USD 7.63-18.35 billion [76] [77] | USD 12.38 billion by 2030 [76] | 8.1% (2025-2030) [76] |
| Market Size (2034) | - | USD 44.2 billion by 2034 [77] | 9.19% (2025-2034) [77] |
Regional adoption patterns demonstrate significant variation in market penetration and growth trajectories:
- North America: Dominated the market with 36.8% share in 2024, driven by advanced infrastructure, strong regulatory support, and high pharmaceutical company concentration [76]
- Europe: Accounted for 28.6% of 2024 revenue, with countries like the UK and Germany investing heavily in genomic initiatives [76]
- Asia Pacific: The fastest-growing region (CAGR 9.7%), fueled by high chronic disease burden, genetic diversity ideal for research, and expanding government initiatives [76]
- Latin America and MEA: Emerging markets presenting significant opportunities despite challenges with funding and infrastructure [76]
Therapeutic area segmentation reveals oncology as the dominant application (39.8% market share in 2024), while cardiology is projected to be the fastest-growing segment due to the global burden of cardiovascular disease and evidence supporting PGx-guided antiplatelet and anticoagulant therapies [76].
Comprehensive Cost-Effectiveness Evidence
Systematic Review Findings
Recent systematic reviews provide robust evidence regarding the economic value of PGx testing across multiple therapeutic areas:
Table 2: Cost-Effectiveness Evidence for PGx-Guided Treatment
| Therapeutic Area | Drug-Gene Pair | Number of Studies | Studies Favoring PGx (Cost-Effective or Cost-Saving) | Key Findings |
|---|---|---|---|---|
| Cardiovascular | Clopidogrel-CYP2C19 | 23 | 22 (96%) | PGx-guided antiplatelet therapy significantly cost-effective in ACS/PCI patients [73] |
| Cardiovascular | Warfarin-CYP2C9/VKORC1 | 16 | 7 (44%) | Mixed evidence, with some studies showing cost-effectiveness [73] [78] |
| HIV | Abacavir-HLA-B*5701 | 8 | 8 (100%) | Universal screening prevents hypersensitivity reactions; highly cost-effective [73] |
| Neurology | Carbamazepine-HLA alleles | 8 | Part of 15/26 (58%) for HLA testing | Screening for SCARs risk highly cost-effective in high-prevalence populations [73] [1] |
| Psychiatry | Antidepressants-CYP2D6/CYP2C19 | 11 | 9 (82%) | Genotype-guided prescribing reduces trial-and-error, improves outcomes [73] [77] |
| Multiple | All CPIC Level A drugs | 108 | 77 (71%) | Comprehensive review showing majority of evidence supports cost-effectiveness [73] |
A landmark systematic review from 2022 analyzing 108 studies across 39 drugs with CPIC guidelines found that 71% demonstrated PGx testing to be either cost-effective (48 studies) or cost-saving (29 studies) [73]. The median quality score of these studies was 91 (range 48-100) on the Quality of Health Economic Studies (QHES) instrument, indicating generally high methodological rigor [73].
Real-World Economic Outcomes
Beyond modeling studies, real-world implementations provide compelling evidence of PGx's economic impact:
- A 2024 study of a PGx-enriched comprehensive medication management (PGx+CMM) program in a self-insured U.S. employee population demonstrated significant reductions in healthcare utilization, with 39% fewer inpatient admissions and 39% fewer emergency department visits among participants compared to matched controls [75]
- The same study reported an increase in outpatient visits (21%), indicating appropriate care shifting to lower-cost settings [75]
- The economic value proposition strengthens when genetic information is readily available in clinical records; one analysis estimated that 75% of PGx-guided treatments would be cost-effective or cost-saving if genetic testing costs were eliminated, compared to 57% with testing costs included [79]
Methodological Framework for PGx Economic Evaluations
Core Economic Evaluation Designs
Robust economic evaluation of PGx interventions requires appropriate methodological approaches:
- Cost-Effectiveness Analysis (CEA): Compares alternative interventions based on costs and clinical outcomes expressed in natural units (e.g., adverse drug reactions avoided, life-years gained) [79]
- Cost-Utility Analysis (CUA): A specialized form of CEA that measures health outcomes in quality-adjusted life years (QALYs), allowing comparisons across different therapeutic areas [79]
- Cost-Benefit Analysis (CBA): Quantifies both costs and benefits in monetary terms, enabling calculation of net monetary benefit [79]
- Budget Impact Analysis (BIA): Assesses the financial consequences of adopting a new intervention within a specific healthcare budget context
The incremental cost-effectiveness ratio (ICER) is a key metric in CEA and CUA, calculated as:
ICER values below established willingness-to-pay thresholds (typically $50,000-$150,000 per QALY in high-income countries) indicate cost-effectiveness [79].
Critical Methodological Considerations
Several factors significantly influence the outcomes and interpretation of PGx economic evaluations:
- Perspective: Analyses can adopt healthcare system, payer, societal, or patient perspectives, each capturing different cost categories [78]
- Time Horizon: PGx interventions may require longer timeframes to capture full benefits, as genetic information remains relevant throughout a patient's lifetime [80]
- Testing Strategy: Preemptive testing (conducted before drug prescribing) versus reactive testing (conducted in response to a specific prescription) has substantial economic implications [80]
- Analytical Approach: Decision-analytic modeling (e.g., decision trees, Markov models) versus analyses based on real-world cohort data each have strengths and limitations [73]
Diagram: Framework for Pharmacogenomics Economic Evaluation
Experimental Protocols and Implementation Models
Protocol for PGx-Enriched Comprehensive Medication Management
A recent study demonstrates an effective protocol for implementing PGx in employer populations [75]:
1. Participant Identification and Risk Stratification
- Use pharmacy and medical claims data to identify high-risk individuals based on:
- Potential drug-drug interactions
- Anticholinergic burden
- Medication contraindications
- Medications impacted by genetics (derived from FDA labeling, CPIC guidelines)
2. Genetic Testing and Analysis
- Self-collected saliva samples shipped to CLIA/CAP-certified laboratory
- PGx test panel analysis for clinically relevant genes (CYP2C19, CYP2D6, CYP2C9, VKORC1, SLCO1B1, etc.)
- Genotype conversion to diplotypes using standard nomenclature
- Clinical annotation and interpretation via clinical decision support tools (e.g., GeneDose LIVE)
3. Medication Action Plan Development
- Clinical pharmacists evaluate genetic and non-genetic risk factors
- Alternative regimens with lower inefficacy and safety risks modeled
- Comprehensive Medication Action Plan (MAP) with clinical rationale created
4. Provider Communication and Implementation
- MAP communicated to prescribing physicians via secure email/fax
- Follow-up support for implementation questions
- Ongoing monitoring of medication changes and outcomes
5. Economic Outcome Assessment
- Healthcare resource utilization tracked via claims data
- Pre-post analysis with propensity score-matched controls
- Statistical analysis using doubly robust modeling to reduce confounding
Protocol for Cost-Effectiveness Analysis Using Modeling
For situations where real-world implementation data is unavailable, modeling approaches provide valuable economic insights:
1. Model Structure Development
- Create decision tree or state-transition model representing clinical pathways
- Define key health states relevant to the drug-disease context
- Specify transitions between health states based on clinical evidence
2. Parameter Estimation
- Clinical probabilities: ADR rates, efficacy probabilities, mortality rates
- Resource utilization: Medication use, hospitalizations, physician visits
- Cost inputs: Drug costs, genetic test costs, medical service costs
- Utility weights: Quality of life values for health states
3. Analysis Framework
- Calculate costs and outcomes for PGx-guided versus standard strategies
- Compute incremental cost-effectiveness ratios
- Perform deterministic and probabilistic sensitivity analyses
- Assess budget impact under different adoption scenarios
4. Validation and Reporting
- Internal validity checks (face validity, cross-validation)
- External validation against real-world data when available
- Adherence to CHEERS (Consolidated Health Economic Evaluation Reporting Standards) guidelines
Global Disparities: Developed vs. Developing Country Contexts
Significant disparities exist in PGx implementation and economic evidence between developed and developing regions, creating distinct challenges and opportunities.
Developed Countries
Strengths:
- Well-established regulatory frameworks (FDA, EMA)
- Advanced laboratory infrastructure with CLIA/CAP certification
- Growing reimbursement pathways despite limitations
- Robust evidence base for many drug-gene pairs
- Integration with electronic health records
Implementation Barriers:
- Fragmented healthcare systems hamper data sharing [80]
- Inconsistent reimbursement policies across payers [80]
- Physician education gaps in PGx interpretation
- Privacy concerns regarding genetic data
Developing Countries
Unique Challenges:
- Healthcare Infrastructure: Limited laboratory capabilities, fewer trained personnel [74]
- Economic Constraints: High out-of-pocket expenditures, competing health priorities [74]
- Evidence Gaps: Underrepresentation in global genomic studies despite high genetic diversity [74]
- Regulatory Heterogeneity: Variable PGx guideline adoption and enforcement [1]
Unique Opportunities:
- Genetic Diversity: African populations display greatest genetic diversity worldwide, offering unique research opportunities [74]
- Public Health Applications: Potential for significant impact in infectious diseases (HIV, malaria, TB) [74]
- Leapfrogging Potential: Opportunity to implement preemptive testing before entrenched workflows develop
Table 3: Economic Considerations Across Healthcare Settings
| Factor | Developed Countries | Developing Countries |
|---|---|---|
| Testing Cost | $200-$500 per test [79] | Often prohibitive without external funding |
| Reimbursement | Variable coverage by private and public payers [80] | Limited to no coverage in most settings |
| Infrastructure | Advanced sequencing platforms widely available | Limited access to basic genotyping technologies |
| Evidence Base | Robust for major drug-gene pairs [73] | Limited population-specific data [74] |
| Implementation Models | Preemptive and reactive testing in integrated systems | Often pilot programs with external partners |
Research Reagents and Technological Solutions
The PGx research and implementation landscape relies on several critical technological components and research reagents:
Table 4: Essential Research Reagents and Technological Solutions
| Technology/Reagent | Primary Function | Key Applications | Representative Examples |
|---|---|---|---|
| PCR and Digital PCR | Amplification of specific genetic variants | Targeted genotyping of known PGx variants | CYP2C19*2, *3, *17; CYP2D6 poor metabolizer variants |
| Next-Generation Sequencing | Comprehensive genomic profiling | Discovery of novel variants, preemptive testing | Whole genome sequencing for multi-gene panels |
| Microarray Technology | High-throughput variant detection | Population screening, research studies | Pharmacogenomic arrays targeting CPIC genes |
| Bioinformatic Tools | Genotype calling, phenotype prediction | Clinical decision support, data interpretation | GeneDose LIVE, PharmCAT, PharmGKB |
| CLIA-Certified Reference Materials | Assay validation, quality control | Laboratory developed test verification | Coriell samples with known genotypes |
| Electronic Health Record Integration | Clinical decision support at point of care | Alerting systems, result storage | Epic PGx support, Cerner solutions |
Technological advancements are progressively reducing costs and expanding capabilities. Next-generation sequencing costs have decreased dramatically, enabling comprehensive preemptive testing approaches that may be more cost-effective than single-gene reactive tests [76]. Artificial intelligence is increasingly employed to enhance the speed and accuracy of genetic data analysis, identify novel gene-drug interactions, and integrate genomic data with electronic health records [77].
Diagram: Pharmacogenomics Testing Workflow
Future Directions and Strategic Recommendations
Based on current evidence and emerging trends, several strategic priorities emerge for advancing the cost-effective implementation of PGx globally:
Evidence Generation Priorities
- Develop Standardized Methodologies: Create consistent approaches for PGx economic evaluations to enhance comparability across studies and settings
- Expand Real-World Evidence: Conduct more prospective studies with real-world cohorts rather than hypothetical models, particularly in diverse populations [73]
- Address Evidence Gaps: Focus on understudied drug-gene pairs and therapeutic areas beyond oncology and cardiology
- Generate Context-Specific Data: Develop economic evidence relevant to specific healthcare systems, particularly in developing countries [74]
Implementation Strategies
- Preemptive Testing Approaches: Implement genetic testing before medication needs arise to maximize long-term value [80]
- Multi-Gene Panels: Transition from single-gene tests to comprehensive panels that support multiple prescribing decisions over a patient's lifetime [73]
- Digital Health Integration: Leverage AI and machine learning to interpret complex genetic data and support clinical decision-making [77]
- Workflow Integration: Seamlessly incorporate PGx into existing clinical workflows to minimize disruption and enhance adoption [81]
Policy and Infrastructure Development
- Harmonized Regulatory Frameworks: Develop consistent PGx guidelines and regulatory standards across regions to facilitate global implementation [1]
- Sustainable Financing Models: Create innovative reimbursement mechanisms that recognize both short-term costs and long-term benefits
- Capacity Building: Invest in laboratory infrastructure, healthcare professional training, and digital health systems in developing countries [74]
- Data Sharing Initiatives: Establish platforms for sharing PGx implementation experiences and economic outcomes across institutions and countries
Comprehensive economic analyses demonstrate that PGx testing represents a cost-effective approach for optimizing medication therapy across multiple therapeutic areas in developed countries. The evidence base is particularly robust for specific drug-gene pairs such as clopidogrel-CYP2C19, abacavir-HLA-B*5701, and many antidepressants. However, significant global disparities persist in implementation capabilities, economic evidence, and reimbursement frameworks.
For PGx to realize its full potential in personalized medicine, stakeholders must address several critical challenges: generating context-specific economic evidence, particularly for developing countries; developing sustainable financing models; building necessary infrastructure; and creating harmonized regulatory frameworks. Future research should focus on preemptive testing strategies, real-world implementation outcomes, and the economic value of PGx in diverse global contexts.
As the field evolves, PGx promises to transform medication therapy from a trial-and-error approach to a precision-based model, ultimately enhancing therapeutic outcomes while optimizing healthcare resource utilization across diverse global healthcare systems.
Genotype-phenotype discordance presents a significant challenge in the application of pharmacogenomics within personalized medicine. This phenomenon occurs when an individual's observed drug response (phenotype) does not align with the predicted response based on their genetic profile (genotype). The accurate prediction of drug efficacy and toxicity from genetic information is fundamental to precision medicine, yet discordant results can lead to suboptimal treatment decisions, adverse drug reactions, and therapeutic failures [82] [83].
Understanding and resolving these discrepancies is particularly crucial for drug development professionals and researchers working to implement robust pharmacogenomic strategies. As the field advances, with regulatory bodies like the FDA including pharmacogenomic biomarkers in an increasing number of drug labels and international consortia such as the Clinical Pharmacogenetics Implementation Consortium (CPIC) developing evidence-based guidelines, addressing the sources and solutions to discordance becomes increasingly important for the effective translation of pharmacogenomics into clinical practice and drug development pipelines [84] [1].
Biological Complexity
The relationship between genotype and phenotype is rarely straightforward, with numerous biological factors contributing to discordant observations.
- Polygenic and Multifactorial Influences: Many drug responses are influenced by multiple genes rather than single genetic variants. For example, warfarin dosing is affected by variants in CYP2C9, VKORC1, and CYP4F2 genes, among others [84]. The complex interplay between these genetic factors, along with non-genetic influences such as age, organ function, and drug-drug interactions, can lead to phenotypes that deviate from predictions based on single gene variants.
- Uncharacterized or Off-Target Mechanisms: Current pharmacogenomic testing panels are necessarily limited to known variants with established evidence. Resistance to antimicrobials in Gram-negative organisms, for instance, may arise from mechanisms not included on standard panels, such as porin loss, efflux pump activation, or novel resistance gene variants [82]. Similarly, in HIV treatment, transitional mutations or antagonistic interactions between mutations can result in apparently sensitive phenotypes despite the presence of resistance-associated genotypes [83].
- Gene Expression and Regulatory Variants: A fundamental limitation of genotypic assays is their focus on DNA sequence variations, which may not capture important regulatory influences on gene expression. Epigenetic modifications, transcriptional and translational regulation, and post-translational modifications can all affect the functional activity of drug-metabolizing enzymes and drug targets without altering the underlying DNA sequence [82].
Methodological Limitations
Technical aspects of testing methodologies contribute significantly to observed discordances.
- Assay Design Constraints: Commercial pharmacogenomic tests typically target specific, predefined variants with known functional impact. This targeted approach inevitably misses rare variants, novel mutations, or structural variations not included in the assay design. For example, the original lopinavir/ritonavir genotypic resistance scoring system misclassified some viruses as susceptible until the algorithm was updated to account for novel mutation patterns [83].
- Detection Thresholds and Mixed Populations: The ability to detect minor variant populations is limited by the sensitivity of the testing methodology. In microbial infections, mixed populations of wild-type and mutant viruses or bacteria can lead to discordance, as phenotypic tests may not show resistance if the proportion of mutant organisms is below the detection threshold or if the wild-type population dominates the overall response [83]. This is particularly challenging in HIV, where mutant/wild-type virus mixtures may not always be detected by phenotypic fold change measurements [83].
- Phenotypic Test Standardization: Phenotypic testing itself presents standardization challenges. For antimicrobial susceptibility testing, parameters such as inoculum size, growth medium, and incubation conditions can affect minimum inhibitory concentration (MIC) determinations [82]. In cellular drug response assays, factors like passage number, culture conditions, and endpoint measurements introduce variability that can contribute to discordant observations.
Table 1: Technical Sources of Genotype-Phenotype Discordance
| Category | Specific Source | Impact on Discordance | Example |
|---|---|---|---|
| Biological Complexity | Polygenic influences | Single gene tests may not capture complete pharmacogenomic profile | Warfarin dosing influenced by CYP2C9, VKORC1, and CYP4F2 [84] |
| Uncharacterized mechanisms | Resistance or altered metabolism despite "wild-type" genotype | Porin loss or efflux pumps in Gram-negative bacteria [82] | |
| Gene expression regulation | Protein function not predicted by DNA sequence | Epigenetic regulation of drug metabolizing enzymes | |
| Methodological Limitations | Assay design constraints | Failure to detect rare or novel variants | Original lopinavir/ritonavir algorithm missing novel mutations [83] |
| Detection thresholds | Inability to detect minor variant populations | HIV mutant/wild-type mixtures below detection threshold [83] | |
| Phenotypic test standardization | Variable phenotypic measurements | MIC variations due to inoculum size or growth medium [82] | |
| Analytical Challenges | Polymicrobial infections | Difficulty assigning resistance markers to specific organisms | Multiple Staphylococcus species with mecA detection [82] |
| Result interpretation algorithms | Over-simplified genotype-phenotype correlation rules | Arbitrary fold-change cutoffs for resistance classification [83] |
Resolution Methodologies and Experimental Approaches
Stepwise Discordance Resolution Protocols
Implementing systematic approaches to investigate discordant results is essential for both clinical management and research validation.
- Algorithm-Enhanced Genotype Interpretation: Advanced interpretation systems that incorporate weighted mutation scores, mutation patterns, and expert rules can significantly improve genotype-phenotype correlation. In HIV resistance testing, the development of refined genotypic algorithms for lopinavir/ritonavir through phenotype correlations reduced discordance by identifying novel mutation patterns and accounting for cross-resistance profiles [83]. These algorithms evolve as new correlation data become available, continually improving their predictive accuracy.
- Supplementary Phenotypic and Genotypic Characterization: When discordance is identified, additional testing can help elucidate the underlying mechanism. For antimicrobial resistance, this may include:
- Population Analysis: Examining for heteroresistance (subpopulations with different resistance profiles) through population analysis profiling [82].
- Extended Genotype Investigation: Performing expanded genetic testing to identify off-panel mechanisms, such as full gene sequencing rather than targeted variant detection [82].
- Gene Expression Analysis: Measuring transcript levels or enzyme activity to identify regulatory differences not apparent from genetic sequence alone [82].
- Orthogonal Method Validation: Confirming results using alternative methodologies strengthens discordance resolution. This may include:
- Alternative Phenotypic Assays: Using different phenotypic methods (e.g., both broth microdilution and disk diffusion for antibiotics) [82].
- Different Genotypic Platforms: Employing alternative genetic testing technologies (e.g., both PCR and sequencing-based approaches) [82].
- Functional Validation: Conducting in vitro functional studies to characterize the impact of genetic variants on protein function [1].
Advanced Integrated Testing Strategies
Sophisticated approaches that combine multiple technologies provide powerful solutions for dissecting complex discordance scenarios.
- Parallel Genotype-Phenotype Assessment: Implementing both genotypic and phenotypic testing simultaneously for critical decision points provides complementary data. In HIV management, some clinicians order both tests to optimize treatment decisions, though this approach requires careful interpretation when results appear discordant [83]. The phenotype test summarizes complex genotypic interactions into a single measurable result (fold-change in IC50), while the genotype helps explain the mechanistic basis and identify mixtures or transitional mutations that might affect future resistance development [83].
- Multi-Omics Integration: Combining genomic data with other molecular profiling techniques offers a more comprehensive view of drug response determinants. Transcriptomics, proteomics, and metabolomics can reveal functional consequences of genetic variants and identify non-genetic factors influencing phenotype. International research initiatives, such as the European Partnership for Personalised Medicine's JTC2025 call, are specifically promoting projects that use "(multi)-omics data in relation to drug or drug combination" to identify and validate pharmacogenomic markers [22].
- Longitudinal Monitoring and Dynamic Assessment: For chronic conditions or situations where resistance evolves over time, repeated testing can capture dynamic changes that explain apparent discordance. In HIV, transitional mutations may revert to wild-type in the absence of drug pressure, leading to sensitive phenotypes despite the presence of resistance-associated mutations in the genotype [83]. These transitional forms can quickly re-emerge as resistant mutations with appropriate drug exposure, explaining discrepancies between historical genotypes and current phenotypes.
Table 2: Experimental Approaches for Discordance Resolution
| Method Category | Specific Techniques | Key Applications | Technical Considerations |
|---|---|---|---|
| Stepwise Resolution Protocols | Algorithm-enhanced interpretation | HIV resistance testing, antimicrobial susceptibility | Requires continuous validation against phenotypic correlation data [83] |
| Supplementary phenotypic characterization | Heteroresistance detection, confirmatory testing | Population analysis profiling for minority variants [82] | |
| Orthogonal method validation | Result confirmation, method comparison | Use of different technological platforms for confirmation [82] | |
| Advanced Integrated Strategies | Parallel genotype-phenotype assessment | Complex resistance patterns, treatment optimization | Phenotype summarizes complexity; genotype explains mechanism [83] |
| Multi-omics integration | Comprehensive mechanism elucidation | Transcriptomics, proteomics, metabolomics with genomics [22] | |
| Longitudinal monitoring | Evolutionary resistance, dynamic changes | Tracking mutation reversion and emergence over time [83] | |
| Emerging Technologies | Next-generation sequencing | Comprehensive variant detection, novel gene discovery | Cost-effective for multiple pharmacogenomic loci [84] |
| Single-cell analysis | Cellular heterogeneity, minority populations | Technical complexity, higher cost [82] | |
| Digital PCR | Precise quantification of variant alleles | Excellent for detecting and quantifying minor variants [82] |
Implementation in Research and Clinical Practice
Analytical Framework and Quality Systems
Establishing robust analytical frameworks is essential for managing genotype-phenotype discordance in both research and clinical settings.
- Clinical Decision Support Systems: Integrating pharmacogenomic data with electronic health records (EHR) and implementing clinical decision support (CDS) tools enables systematic application of complex genotype-phenotype correlations. These systems can provide point-of-care alerts for potential discordance scenarios and suggest appropriate follow-up testing or alternative therapeutic approaches [85]. The emerging use of FHIR (Fast Healthcare Interoperability Resources)-based application programming interfaces (APIs) supports the development of pharmacogenomic-enhanced applications that can access existing pharmacogenomic knowledge platforms [85].
- Analytical Validation Protocols: Ensuring the reliability of both genotypic and phenotypic testing methods requires comprehensive validation. For pharmacogenomic tests, this includes establishing accuracy, precision, sensitivity, specificity, and reportable ranges for each genetic variant [86]. For phenotypic assays, standardization against reference methods and quality control using well-characterized reference strains is essential [82]. Laboratories should establish specific procedures for handling discordant results, including criteria for reflex testing and result reporting with interpretive comments [82] [86].
- Interdisciplinary Review Processes: Complex discordant cases benefit from review by multidisciplinary teams including clinical pharmacologists, geneticists, bioinformaticians, and treating specialists. This approach is particularly valuable for disorders of sexual differentiation, where phenotype-genotype discordance identified through noninvasive prenatal testing (NIPT) and ultrasound requires coordinated specialist interpretation [87]. Similarly, in pharmacogenomics, teams that include physicians, pharmacists, genetic counselors, and laboratory specialists can combine expertise to interpret challenging cases [84] [85].
Educational and Infrastructure Requirements
Addressing genotype-phenotype discordance effectively requires specialized knowledge and infrastructure.
- Professional Education and Genomic Literacy: Surveys indicate only approximately 10% of physicians feel confident in their knowledge of pharmacogenomics and its clinical application [84]. Enhancing genomic literacy through targeted education is essential for appropriate interpretation of discordant results. Educational initiatives should cover the limitations of testing methodologies, the complexity of genotype-phenotype relationships, and strategies for resolving discrepancies [84] [85]. Laboratories play a vital role by providing clear interpretive comments and clinical guidance along with test results [82] [86].
- Data Integration and Knowledge Systems: Managing discordance effectively requires systems that can integrate multiple types of data and access current knowledge resources. Third-party repositories that make pharmacogenomic data available through secure services represent one approach to maintaining accessible genotype information for lifetime medication management [85]. These systems must accommodate evolving knowledge, as new information may emerge that reinterprets previously generated genotypes in light of updated evidence [85].
- Regulatory and Reimbursement Frameworks: The implementation of approaches for managing discordance is influenced by regulatory and payment policies. In the United States, the FDA issues guidance on pharmacogenomics and genetic tests, while CMS regulates laboratory testing through CLIA certifications [1] [88]. Reimbursement policies vary significantly, with some payors requiring extensive evidence of clinical utility before covering comprehensive testing approaches that might help resolve discordance [85] [88]. These factors significantly impact the feasibility of implementing sophisticated discordance resolution strategies in practice.
Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Discordance Investigation
| Reagent Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Reference Materials | Characterized cell lines with known genotypes | Assay validation, quality control | Essential for establishing assay performance characteristics [82] |
| Well-characterized microbial strains | Phenotypic method standardization | Reference strains with defined resistance profiles [82] | |
| Certified genomic DNA standards | Genotypic assay calibration | Ensure consistency across testing platforms and laboratories [86] | |
| Analytical Reagents | Targeted PCR/PCR-array panels | Specific variant detection | Commercial panels for known pharmacogenetic variants [82] |
| Next-generation sequencing kits | Comprehensive variant discovery | Whole exome, whole genome, or targeted panels [84] | |
| Phenotypic assay reagents | Drug response measurement | Culture media, indicator compounds, growth detection systems [82] | |
| Software & Databases | Genotype interpretation algorithms | Result translation to predicted phenotype | Weighted rules-based systems, statistical models [83] |
| Pharmacogenomic knowledgebases | Evidence-based variant annotation | PharmGKB, CPIC guidelines [84] [1] | |
| Clinical decision support systems | Point-of-care guidance | EHR-integrated alert systems for potential discordance [85] |
Genotype-phenotype discordance represents a significant challenge in pharmacogenomics and personalized medicine, arising from both biological complexity and methodological limitations. Understanding the technical sources of these discrepancies—including polygenic influences, uncharacterized mechanisms, and assay design constraints—provides the foundation for developing effective resolution strategies.
The implementation of systematic, stepwise approaches to investigate discordant results, complemented by advanced integrated testing strategies that leverage multiple technological platforms, enables researchers and clinicians to navigate these challenges effectively. As the field progresses, enhanced bioinformatics tools, clinical decision support systems, and multidisciplinary collaboration frameworks will continue to improve our ability to interpret and act upon complex genotype-phenotype relationships.
Ultimately, addressing genotype-phenotype discordance requires not only technical solutions but also educational initiatives, infrastructure development, and supportive regulatory frameworks. By embracing these comprehensive approaches, the field of pharmacogenomics can advance toward more effective implementation of personalized medicine strategies that optimize therapeutic outcomes while minimizing adverse drug reactions.
Health Information Technology Requirements for Genomic Data Integration
The integration of genomic data into clinical and research workflows represents a cornerstone of modern personalized medicine. Pharmacogenomics (PGx), which studies how an individual's genetic makeup affects their response to drugs, is particularly reliant on robust health information technology (HIT) systems to translate genetic insights into actionable treatment strategies [11]. The ultimate goal of these efforts is to develop personalized, genetic-based strategies that will optimize therapeutic outcomes by maximizing drug efficacy and minimizing adverse reactions [11]. This technical guide outlines the core HIT requirements for successful genomic data integration within the broader context of personalized medicine research, addressing data standards, analytical tools, clinical implementation frameworks, and computational infrastructure.
Genomic Data Standards and Formats
Effective genomic data integration begins with strict adherence to community-established data standards, which ensure interoperability across research institutions and clinical systems. These standardized formats facilitate every stage of genomic analysis, from initial sequencing to clinical interpretation.
Table 1: Essential Genomic Data Standards and Formats
| Data Type | Standard Format | Primary Use | Common Tools |
|---|---|---|---|
| Raw Sequencing Reads | FASTQ | Stores raw nucleotide sequences and corresponding quality scores | FASTX-Toolkit [89] |
| Reference Genome | FASTA | Reference assembly for read alignment or BLAST | Aligners, BLAST [89] |
| Sequence Alignment | BAM/SAM | Binary/text format containing mapping and read quality information | SAMtools, IGV [89] |
| Genetic Variants | VCF (Variant Call Format) | Documents single nucleotide polymorphisms (SNPs) and genotype calls with quality metrics | vcftools, dbSNP repository [89] |
| Genomic Coordinates | BED | Defines start and end positions of genomic features | bedtools [89] |
The VCF format is particularly critical for PGx applications as it captures the single nucleotide polymorphisms (SNPs) that account for approximately 90% of all human genetic variations and significantly influence drug metabolism and response [11]. These SNPs can occur every 100 to 300 base pairs throughout the genome, and their location relative to a gene determines whether they affect its normal function [11]. For pharmacogenomic applications, identifying heterozygous versus homozygous SNPs is essential, as this determines the net effect on gene function and subsequent drug metabolism phenotypes [11].
Beyond SNPs, structural variations (SVs)—including small insertions or deletions (indels), copy number variations (CNVs), and inversions—occur less frequently but often have greater functional consequences because they encompass larger genomic regions [11]. The integration of both SNP and SV data requires HIT systems capable of handling these diverse data types while maintaining data integrity throughout the analytical pipeline.
Genomic Analysis Tools and Workflows
A robust genomic data integration pipeline requires specialized bioinformatics tools for sequence analysis, variant identification, and functional annotation. These tools enable researchers to transform raw sequencing data into biologically meaningful insights relevant to drug response.
Core Bioinformatics Tools
The National Center for Biotechnology Information (NCBI) provides fundamental tools for genomic analysis, with the Basic Local Alignment Search Tool (BLAST) serving as a cornerstone for comparing nucleotide or protein sequences to sequence databases to infer functional and evolutionary relationships [90]. For large-scale microbial genomic analysis, newer algorithms like LexicMap enable rapid searching across millions of bacterial and archaeal genomes, precisely locating mutations in minutes rather than days [91]. Additional specialized NCBI tools include:
- Primer-BLAST: Designs PCR primers and automatically checks their specificity against user-specified databases [90]
- Conserved Domain Search Service (CD Search): Identifies conserved protein domains using RPS-BLAST [90]
- Open Reading Frame Finder (ORF Finder): Graphical tool that identifies all open reading frames in nucleotide sequences [90]
- ProSplign: Computes alignment of proteins to genomic nucleotide sequence, specifically accounting for introns and splice signals [90]
- VecScreen: Identifies segments of nucleic acid sequence that may be of vector origin [90]
Pharmacogenomic Analysis Workflow
The following diagram illustrates the core bioinformatics workflow for converting raw genomic data into clinically actionable pharmacogenomic insights:
This workflow begins with quality control of FASTQ files, proceeds through alignment to a reference genome (typically in FASTA format) to produce BAM files, then performs variant calling to generate VCF files documenting genetic variations [89]. The final annotation step integrates pharmacogenomic knowledge bases to interpret the clinical significance of identified variants, particularly in genes known to influence drug metabolism and response.
Clinical Integration and Decision Support
Integrating genomic data into clinical workflows requires HIT systems that can store, process, and deliver genetically-informed recommendations at the point of care. This represents one of the most significant challenges in modern healthcare informatics.
Clinical Decision Support (CDS) Systems
AI-driven CDS tools are increasingly important for integrating PGx data into clinical workflows, providing clinicians with actionable recommendations about medication selection and dosing tailored to a patient's genetic profile [92]. These systems can alert providers to potential safety concerns such as allergies, contraindications, and optimal dosing based on genetic markers, thereby enhancing prescribing safety [92]. For example, CDS systems can incorporate known gene-drug associations such as:
- CYP2C19 and clopidogrel: The CYP2C19*2 allele is associated with reduced active clopidogrel metabolites, causing higher platelet aggregation and adverse clinical outcomes in cardiovascular patients [11]
- HLA-B and carbamazepine: The HLA-B*1502 allele is linked to increased risk of Stevens-Johnson syndrome/toxic epidermal necrolysis in Asian patients prescribed carbamazepine [11]
- CYP2D6 and psychotropic drugs: This gene influences metabolism of many psychiatric medications including atomoxetine, aripiprazole, and amitriptyline [14]
The U.S. Food and Drug Administration (FDA) has recognized the importance of PGx biomarkers by maintaining a Table of Pharmacogenomic Biomarkers in Drug Labeling, which includes information on genomic biomarkers related to drug exposure and clinical response variability, risk for adverse events, and genotype-specific dosing [14].
Multimodal Data Integration in Clinical Systems
Advanced clinical integration involves multimodal data fusion, combining genomic information with other clinical data sources such as medical imaging, electronic health records (EHRs), and wearable device outputs [93]. This approach provides a multidimensional perspective of patient health that enhances diagnosis, treatment, and management across various medical conditions. In oncology, for example, multimodal integration enables more precise tumor characterization and personalized treatment plans, with one model predicting anti-HER2 therapy response with an area under the curve (AUC) of 0.91 by combining radiology, pathology, and clinical information [93].
The following diagram illustrates the architecture for integrating multimodal data into clinical decision support:
Computational Infrastructure and Storage
Genomic data integration demands substantial computational resources and sophisticated storage solutions due to the enormous volume and complexity of genomic datasets. A single human genome sequence requires approximately 200 gigabytes of storage when including raw data, intermediate files, and analyzed results [93]. Infrastructure must therefore support:
- High-performance computing (HPC) clusters for parallel processing of alignment and variant calling
- Scalable cloud storage solutions with appropriate data governance frameworks
- Bioinformatics workflow management systems (e.g., Nextflow, Snakemake) for reproducible analyses
- Data compression technologies that maintain data integrity while reducing storage footprints
For large-scale genomic operations, such as those at Children's Hospital Colorado, enterprise-wide integration models leverage cutting-edge informatics technology to seamlessly utilize advanced genomic tests, securely manage data, and curate insights into clinical workflows [94].
Experimental Protocols and Methodologies
Protocol: Pharmacogenomic Variant Analysis for Drug Response Prediction
This protocol outlines a standardized approach for identifying and interpreting pharmacogenomic variants that influence drug response, particularly focusing on cytochrome P450 enzymes and drug transporters.
Materials and Reagents
Table 2: Essential Research Reagents for PGx Analysis
| Reagent/Resource | Function | Example/Format |
|---|---|---|
| Whole Blood or Saliva Sample | Source of genomic DNA | 3-5 mL whole blood in EDTA tubes or 2 mL saliva in collection kits |
| DNA Extraction Kit | Isolate high-quality genomic DNA | Qiagen DNeasy Blood & Tissue Kit or equivalent |
| Whole Genome Sequencing Kit | Library preparation and sequencing | Illumina DNA PCR-Free Prep or equivalent |
| Reference Genome | Alignment reference for variant calling | GRCh38 (hg38) in FASTA format [89] |
| Variant Annotation Database | Functional interpretation of variants | dbSNP, ClinVar, PharmGKB |
| Pharmacogene Panel | Targeted analysis of relevant genes | Custom panel including CYP450 family, VKORC1, TPMT, etc. |
Methodology
Sample Collection and DNA Extraction: Collect peripheral blood or saliva samples using appropriate consent procedures. Extract genomic DNA using standardized protocols, ensuring DNA concentration >50 ng/μL and A260/A280 ratio between 1.8-2.0.
Library Preparation and Sequencing: Prepare sequencing libraries using PCR-free methods to minimize bias. Sequence to minimum 30x coverage using Illumina, PacBio, or Oxford Nanopore platforms depending on research requirements.
Quality Control and Preprocessing: Assess raw read quality using FastQC. Trim adapters and low-quality bases using Trimmomatic or similar tools. Retain only reads with Q-score >30 for downstream analysis.
Sequence Alignment and Processing: Align cleaned reads to reference genome (GRCh38) using BWA-MEM or STAR aligner. Process resulting BAM files by marking duplicates, recalibrating base quality scores, and performing local realignment around indels using GATK best practices.
Variant Calling and Annotation: Call variants using GATK HaplotypeCaller or similar tools. Annotate variants using ANNOVAR or SnpEff with integrated pharmacogenomic databases including PharmGKB and CPIC guidelines. Focus particularly on:
- CYP450 family genes (CYP2D6, CYP2C19, CYP2C9, CYP3A4, CYP3A5)
- Drug transporter genes (SLCO1B1, ABCB1)
- Drug target genes (VKORC1, EGFR)
Phenotype Prediction: Translate genotypes into predicted phenotypes (e.g., poor metabolizer, intermediate metabolizer, extensive metabolizer, ultra-rapid metabolizer) using established allele function tables [11].
Clinical Correlation: Correlate predicted phenotypes with known drug response profiles from the FDA Table of Pharmacogenomic Biomarkers [14]. Generate clinical reports with specific dosing recommendations based on CPIC or professional guidelines.
Ethical, Legal, and Social Implications (ELSI)
The integration of genomic data into healthcare systems raises significant ethical, legal, and social implications that must be addressed through thoughtful policy and technical safeguards. The NHGRI ELSI Research Program specifically focuses on these challenges, including issues of privacy, data ownership, equitable access, and potential discrimination [95]. Key considerations include:
- Informed Consent Processes: Ensuring patients/research participants understand how their genomic data will be used, stored, and shared
- Data Privacy and Security: Implementing robust encryption, access controls, and audit trails to protect sensitive genetic information
- Health Disparities: Addressing potential inequities in access to pharmacogenomically-informed treatments across different populations [96]
- Regulatory Compliance: Adhering to HIPAA, GINA, and other relevant regulations governing genetic information
The integration of genomic data into healthcare and research environments demands sophisticated health information technology infrastructure spanning standardized data formats, specialized analytical tools, clinical decision support systems, and robust computational resources. As pharmacogenomics continues to advance our understanding of how genetic variations influence drug response, the HIT requirements outlined in this guide will become increasingly fundamental to realizing the promise of personalized medicine. Future developments in artificial intelligence and multimodal data fusion will further enhance our ability to translate genetic insights into optimized therapeutic strategies, ultimately improving drug efficacy and reducing adverse reactions for individual patients.
Integrating pharmacogenomics (PGx) into personalized medicine is fundamentally reshaping treatment paradigms by leveraging genetic information to maximize drug efficacy and minimize adverse drug events [97]. A critical and often overlooked aspect of this integration is the significant variation in pharmacogenomic allele frequencies across different biogeographic populations. These population-specific variations are a major contributor to health disparities, as a one-size-fits-all approach to drug therapy can lead to suboptimal outcomes for certain groups [98]. A deep understanding of these allele frequency differences is therefore essential for developing truly equitable and effective personalized medicine strategies, ensuring that the benefits of pharmacogenomics reach all patient populations [9].
Current research underscores that genetic ancestry is a pivotal factor in population pharmacogenomics [98]. Large-scale genomic analyses reveal that individuals from different ancestries possess distinct genetic profiles that influence their risk of experiencing drug-related adverse events. For instance, one study indicates that Admixed Americans and Europeans may demonstrate a higher risk proximity for drug toxicity, whereas individuals with East Asian ancestry exhibit a relatively protective genetic profile [98]. These differences highlight the danger of extrapolating therapeutic outcomes from one ethnic group to another and underscore the necessity for population-specific considerations in drug development and clinical care [99].
Quantitative Landscape of Population-Specific Allele Frequencies
Key Allele Frequency Variations
The quantitative evidence for population-specific allele frequencies is robust. Large-scale studies, such as an analysis of 200,000 individuals from the UK Biobank, have demonstrated distinct PGx allele, diplotype, and phenotype frequencies across five major biogeographic groups: European, Central/South Asian, East Asian, Afro-Caribbean, and Sub-Saharan African [97]. Notably, even when biogeographic groups exhibit similar proportions of phenotypes, these phenotypes are frequently driven by different sets of dominant PGx alleles [97].
Table 1: Representative Population-Specific Frequencies of Key PGx Alleles
| Gene | Variant (rsID or star allele) | Population | Frequency (%) | Clinical Significance |
|---|---|---|---|---|
| SLCO1B1 | ∗31 | Afro-Caribbean | 3.0 | Associated with simvastatin-induced myopathy [97] |
| SLCO1B1 | ∗31 | Sub-Saharan African | 3.9 | Associated with simvastatin-induced myopathy [97] |
| VKORC1 | rs9923231 | East Asian | ~90 (MAF) | Influences warfarin dosing requirements [99] |
| CYP2C9 | ∗2, ∗3 | European | ~35 (combined) | Reduces warfarin metabolism [9] |
| CYP2D6 | ∗17 | Sub-Saharan African | ~34 (MAF) | Alters metabolism of several antidepressants and antipsychotics [99] |
| DPYD | HapB3 | Various | Highly variable | Associated with severe fluoropyrimidine toxicity [99] |
Furthermore, research has identified specific "no-function" alleles that were previously under-detected. For example, the SLCO1B1 ∗31 allele, which is associated with an increased risk of simvastatin-induced myopathy, was found at frequencies of 3.0% in the Afro-Caribbean group and 3.9% in the Sub-Saharan African group, rates that are significant and had been seldom reported in earlier, smaller studies [97]. This finding highlights how a lack of diverse representation in research can directly impact clinical risk prediction for understudied populations.
Analysis of Population Differentiation in Pharmacogenes
The fixation index (Fst) is a key metric for quantifying population differentiation (PD) of genetic variants. Analyses of Very Important Pharmacogenes (VIPs) reveal that while most variants have low Fst values, a subset of common variants exhibits high differentiation [99]. For instance, the variant rs1229984 in the ADH1B gene, which affects alcohol metabolism, showed a very high Fst value of 0.55 between East Asian and other populations [99].
Table 2: Highly Differentiated PGx Variants (Fst > 0.25) from WES Data Analysis
| Gene | Variant | Highest Fst | Population with High Frequency | Phenotypic Association |
|---|---|---|---|---|
| ADH1B | rs1229984 | 0.55 | East Asian | Alcohol metabolism [99] |
| MTHFR | rs4846051 | 0.30 | Not Specified | Response to methotrexate in rheumatoid arthritis [99] |
| PTGIS | rs6012687 | 0.28 | Not Specified | Not Specified [99] |
| CYP2B6 | rs2279343 | High (exact value not provided) | Sub-Saharan African | Efavirenz pharmacokinetics [99] |
It is critical to note that 97.5% of variants in whole-exome sequencing data are rare (MAF < 3%), and Fst, being proportional to MAF, is generally low for these variants [99]. This underscores the limitation of relying solely on Fst and the need for specialized methods like the Population Differentiation of Rare and Common variants (PDRC) to detect PD driven by rare, functionally significant variants in pharmacogenes [99].
Methodologies for Studying Population-Specific Allele Frequencies
Leveraging Large-Scale Biobanks and Integrated Genetic Data
The UK Biobank serves as a paradigm for how modern genetic biobanks can be used as a robust resource for estimating PGx frequencies. The following workflow outlines the comprehensive process of generating a high-quality, integrated genetic dataset for analysis [97].
Diagram Title: UK Biobank Genetic Data Integration and QC Workflow
The methodology involves generating an integrated dataset from three primary genetic data sources: whole-exome sequencing (WES), microarray-based genotype calls, and imputed data [97]. A critical step is the rigorous, multi-stage quality control (QC) process applied to each data source independently before integration. For WES data, this includes thresholds for genotype quality (GQ ≥ 20), read depth (DP ≥ 7 for SNVs, ≥10 for indels), and allele balance, followed by variant-based missing rate and Hardy-Weinberg equilibrium (HWE) tests [97]. Microarray and imputed data undergo similar processes, including liftover to GRCh38 coordinates, removal of sample outliers, and variant-level filtering based on missingness and HWE [97]. The final integrated dataset is created by combining the QC-passed data, with WES data taking the highest precedence, followed by microarray calls, and then imputed data, based on their respective genotype concordance rates [97].
The PDRC Method for Analyzing Rare and Common Variants
To overcome the limitations of Fst in analyzing rare variants, the PDRC (Population Differentiation of Rare and Common variants) method was developed. Inspired by Generalized Cochran-Mantel-Haenszel (GCMH) statistics, PDRC efficiently summarizes both rare and common variants to identify pharmacogenes with high levels of population differentiation [99].
Diagram Title: PDRC Analysis Workflow for Pharmacogenes
The PDRC method is applied to real-world data, such as whole-exome sequencing datasets from the Type 2 Diabetes Genetic Exploration by Next-generation sequencing in multi-Ethnic Samples (T2D-GENES) initiative and the Go-T2D repository [99]. The analysis focuses on a curated set of 48 Very Important Pharmacogenes (VIPs) from the PharmGKB database. The method's advantage lies in its ability to capture PD from both rare and common variants simultaneously, summarizing the results at the gene level without being overly dependent on adjacent common variants or requiring phased haplotypes, which can be error-prone with rare variants [99]. This approach has successfully identified several candidate genes with high PD, including ACE, CYP2B6, DPYD, F5, MTHFR, and SCN5A [99].
Successful research in population-specific PGx requires a suite of key reagents, computational tools, and data resources.
Table 3: Essential Research Reagents and Resources for Population PGx Studies
| Resource/Tool | Type | Primary Function | Key Feature |
|---|---|---|---|
| PharmCAT | Software Tool | Translates genetic data into PGx annotations and phenotype calls. | Enables batch processing of large cohorts; integrates with CPIC guidelines [97]. |
| PharmGKB | Knowledgebase | Curates and disseminates PGx knowledge, including allele frequencies and clinical guidelines. | Provides Very Important Pharmacogene (VIP) summaries and downloadable frequency data [97] [99]. |
| CPIC Guidelines | Clinical Guidelines | Provide evidence-based, peer-reviewed recommendations for translating genetic test results into actionable prescribing decisions. | Uses standardized allele function and phenotype nomenclature (e.g., "poor metabolizer") [66]. |
| UK Biobank | Data Resource | Large-scale genetic and health data from ~500,000 participants. | Enables estimation of PGx frequencies across diverse biogeographic groups within the cohort [97]. |
| All of Us | Data Resource | NIH-funded program aiming to build a diverse health database from one million+ participants in the USA. | Specifically focuses on addressing diversity gaps in biomedical research [9]. |
| PDRC Method | Statistical Method | Identifies genes with significant population differentiation by combining rare and common variant signals. | Overcomes limitations of Fst for rare variant analysis [99]. |
Implications for Drug Development and Clinical Practice
Informing Clinical Trial Design and Global Drug Development
Understanding population-specific allele frequencies is critical for designing inclusive and globally relevant clinical trials. The genetic makeup of a trial population can significantly influence outcomes, and a lack of diversity can lead to misleading conclusions about a drug's safety and efficacy for certain groups [99]. For example, a drug that is primarily metabolized by the CYP2D6 enzyme may appear safe in a trial cohort predominantly composed of individuals with a "normal metabolizer" phenotype. However, if the drug is later prescribed to a population with a higher prevalence of "poor metabolizer" or "ultra-rapid metabolizer" phenotypes, the risk of adverse events or therapeutic failure could be substantially higher [98]. Therefore, pre-trial genetic screening and intentional recruitment strategies that account for global PGx diversity are necessary to ensure clinical trial results are generalizable and to support regulatory approval and clinical use across different regions and ancestries [99] [98].
Optimizing Clinical Decision Support (CDS) for Diverse Populations
For PGx to be effectively implemented at the point of care, it must be integrated into clinical workflows via sophisticated Clinical Decision Support (CDS) systems. The "five rights" framework is essential for designing effective PGx CDS: providing the right information, to the right person, in the right intervention format, through the right channel, at the right time in the workflow [66]. The "right information" is particularly crucial in the context of population diversity. CDS tools must be able to process complex genetic data (e.g., diplotype, activity score, phenotype) and deliver an actionable recommendation, often based on standardized phenotypes from guidelines like those from CPIC [66]. As research uncovers more population-specific alleles and diplotypes, CDS systems and the clinical tests that feed them must be updated to ensure they accurately interpret genetic results for patients from all biogeographic backgrounds, thereby preventing the perpetuation of health disparities through technological means [9].
The evidence is unequivocal: pharmacogenomic allele frequencies vary significantly across human populations, and these variations are a tangible, genetic contributor to health disparities in drug therapy outcomes. The continued underrepresentation of certain populations in PGx research remains a significant barrier to equitable implementation [9]. Future progress depends on concerted efforts to increase genetic diversity in research cohorts, such as through the "All of Us" program, and the implementation of pan-ethnic pharmacogenetic testing that deliberately assays for variants important across all populations, not just those common in European ancestry groups [9].
Furthermore, closing the implementation gap requires addressing challenges in electronic health record integration, developing standardized CDS tools, and expanding provider and patient education [9]. As these barriers are overcome, a deeper understanding of population-specific allele variations will empower drug development professionals and clinicians to tailor therapies more precisely, ultimately ensuring that the promise of personalized medicine is delivered equitably to every patient, regardless of their genetic ancestry.
Pharmacogenomics (PGx), the study of how genetic variation influences individual response to medications, serves as a cornerstone of personalized medicine. A critical decision in both clinical implementation and research study design is the selection of genetic testing strategy: single-gene tests ordered for a specific drug versus multigene panels that preemptively profile multiple pharmacogenes. This analysis provides a technical comparison of these approaches, evaluating their utility, economic impact, and implementation frameworks to guide researchers, scientists, and drug development professionals. The choice between these strategies directly influences the efficiency, cost-effectiveness, and ultimate success of personalized treatment programs.
Methodological Comparison: Testing Strategies and Workflows
Fundamental Characteristics and Operational Paradigms
The operational distinction between single-gene and multigene testing extends beyond the number of genes analyzed to encompass fundamental differences in timing, workflow integration, and clinical application.
Reactive Single-Gene Testing is characterized by its stimulus-response model. The test is initiated by a specific medication-prescribing decision—either pending or following an adverse event or therapeutic failure [100]. This approach aligns with conventional diagnostic workflows but presents significant limitations:
- Turnaround Time: Typically requires 5-7 business days, delaying critical prescribing decisions [100].
- Prescriber Knowledge Burden: Clinicians must possess specific knowledge about which pharmacogenetic test to order and when [100].
- Inefficiency: Multiple medications may necessitate repeated testing over a patient's lifetime, an inefficient process given that a single DNA sample suffices for comprehensive profiling [100].
- Point-of-Care Variant: A subset of reactive testing where rapid turnaround (hours) is achieved through devices deployed in clinical settings (e.g., CYP2C19 testing for clopidogrel prior to percutaneous coronary intervention) [100].
Preemptive Multigene Panel Testing adopts a proactive, preventive model where genetic data is generated once and stored in the electronic health record (EHR) for lifelong application [100]. This strategy offers distinct advantages:
- Immediate Availability: Results are accessible pre-prescription, eliminating delays in therapy modification [100].
- Clinical Decision Support (CDS): Alerts can proactively guide prescribers at the point of care, reducing the cognitive burden [100].
- Comprehensive Profiling: Analyzes all actionable pharmacogenes simultaneously, identifying the approximately 90-95% of individuals who carry an actionable genotype for at least one medication [100].
- Efficiency: Leverages a single DNA sample to guide countless future prescribing decisions across multiple medical specialties [100].
Table 1: Comparative Characteristics of Testing Approaches
| Feature | Reactive Single-Gene Testing | Preemptive Multigene Panel Testing |
|---|---|---|
| Timing of Ordering | Ordered as drug therapy is initiated or contemplated | Ordered independently of medication use |
| Turnaround Time | ~5-7 business days | Results already available in EHR at time of prescribing |
| Result Portability | Limited; may be repeated for future medications | High; results can be reused lifelong as other medications are prescribed |
| Prescriber Knowledge | Requires knowledge about which test to order | CDS alerts prompt prescriber for action |
| Testing Platform | Often single-gene | Often array-based or sequencing |
| Cost Structure | Cost per therapeutic decision | Approximately equivalent to 2 single-gene tests; provides cost savings over years of use [100] |
Implementation Workflow and Data Integration
The integration of either testing strategy into a research or clinical workflow requires careful consideration of data generation, interpretation, and application. The following diagram illustrates the logical flow and key decision points for each strategy.
Economic and Health Outcomes Analysis
Cost-Effectiveness of Pharmacogenomic-Guided Therapy
A systematic review of cost-effectiveness for drugs with Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines provides compelling evidence supporting PGx testing. The analysis of 108 studies evaluating 39 drugs revealed that 71% of studies (77/108) concluded that PGx testing was either cost-effective (48) or cost-saving (29) [73]. Only 20% (21/108) found testing not cost-effective, while 9% (10/108) were uncertain [73]. The median quality score of these studies was high (91/100 on the QHES scale), indicating robust methodologies [73].
The economic benefit varies by drug-gene pair:
- Clopidogrel/CYP2C19: Among 23 studies, 22 demonstrated cost-effectiveness or cost-saving [73].
- Warfarin/CYP2C9/VKORC1: Evidence was more mixed, with only 7 of 16 studies favoring testing [73].
- HLA Testing: For abacavir, allopurinol, and carbamazepine, 15 of 26 studies demonstrated cost-effectiveness or cost-saving [73].
- Antidepressants: 9 of 11 studies supported the cost-effectiveness of CYP2D6/CYP2C19 testing [73].
Economic Modeling of Multigene Panel Implementation
Simulation studies specifically analyzing multigene panel testing demonstrate significant economic advantages. A model evaluating an 11-gene panel for guiding antihypertensive therapy projected substantial savings over a 3-year horizon [101].
In a simulated insured panel of 10 million patients, multigene-guided therapy yielded:
- Savings of $6.26 billion for evaluation and management
- Savings of $908 million for medications
- Savings of $37.47 billion for adverse events averted [101]
After accounting for incremental genetic testing costs of $2.36 billion, the net savings totaled $42.28 billion over three years—a 47% reduction in total costs [101]. This translated to savings of $4,228 per covered patient over three years, or $1,409 annually [101]. Critically, 89% of these savings resulted from averting adverse events rather than drug cost reductions [101].
Table 2: Economic Outcomes of Multigene vs. Single-Gene Testing
| Economic Parameter | Single-Gene Testing | Multigene Panel Testing | Evidence Source |
|---|---|---|---|
| Overall Cost-Effectiveness | 71% of studies show CE/CS across 39 drugs [73] | Limited direct studies, but simulation shows dominance [101] | Systematic Review [73] |
| Cost per Test | ~$150-$400 (out-of-pocket) [102] | ~$300-$500 (out-of-pocket) [102] | Market Analysis [102] |
| Long-Term Economic Impact | Routinely cost-effective for specific drug decisions [100] | Projected 47% cost reduction in hypertension management [101] | Simulation Study [101] |
| Primary Savings Driver | Avoidance of specific adverse drug reactions | Averting adverse events (89% of savings) [101] | Simulation Study [101] |
| Testing Efficiency | Inefficient use of DNA sample; repeated tests likely [100] | Cost of panel ≈ two single-gene tests; covers lifetime [100] | Implementation Review [100] |
Real-World Utilization and Cost Structures
Despite evidence supporting cost-effectiveness, real-world uptake of PGx testing remains limited. A study of a US managed care population (2013-2017) found only 5,712 patients (0.12%) received single-gene testing through their insurance from a sample of 4.66 million enrollees [103]. The most common test was CYP2C19, and testing volume more than doubled from 2013 to 2015 before slightly decreasing in 2016 [103].
Current market pricing (2025) for pharmacogenomic tests shows:
- Basic single-gene tests: $150-$400 out-of-pocket [102]
- Multigene panels: $300-$500 out-of-pocket [102]
- Comprehensive whole-genome sequencing with PGx: $1,000-$2,000+ [102]
Insurance coverage remains variable, often requiring demonstration of medical necessity (e.g., treatment resistance or adverse drug reaction history) [102]. Medicare covers specific tests like CYP2C19 for clopidogrel or warfarin-related testing under narrow conditions, while private insurers increasingly cover testing for psychiatric medications [102].
Implementation Frameworks and Research Applications
Guidelines and Evidence Standards
Implementation of PGx testing relies on established guidelines, primarily from CPIC, which creates evidence-based, peer-reviewed guidelines for translating genetic results into prescribing actions [100]. CPIC assigns evidence levels from A-D, with levels A and B indicating that genetic information should or could be used to change prescribing [73]. As of 2022, the FDA recognizes 56 drugs with valid pharmacogenetic associations that support therapeutic management [73].
The evidence paradigm for pharmacogenomics continues to evolve. While randomized controlled trials (RCTs) remain the gold standard, many argue they are often impractical or unethical for PGx [100]. Regulatory agencies increasingly embrace real-world evidence, with the FDA's 21st Century Cures Act tasking the agency to incorporate real-world data into regulatory decisions [100].
Technological Advances and Research Directions
Emerging technologies are reshaping pharmacogenomics research and expanding clinical applications:
- Long-Read Sequencing: Enables comprehensive mapping of complex pharmacogenes like CYP2D6, accurately capturing structural variations, gene duplications, deletions, and hybrid alleles that confound short-read technologies [10].
- EHR-Linked Biobanks: Resources like UK Biobank, All of Us, and FinnGen integrate genomic data with longitudinal health records, enabling discovery of novel pharmacogenomic associations across diverse populations [10].
- Polygenic Risk Scores: Extend beyond single-gene interactions to capture the cumulative effect of multiple variants on drug response, showing promise for predicting efficacy of sulfonylureas, lurasidone, and beta-blockers [10].
- Machine Learning and AI: Deep learning models like Hubble.2D6 predict functional impacts of CYP2D6 haplotypes directly from DNA sequence data, while neural networks show potential for predicting drug metabolism phenotypes [10].
- Multiomics Integration: Combining genomics with transcriptomics, proteomics, and metabolomics provides comprehensive understanding of drug disposition and action, helping to explain heterogeneity in treatment response [10].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms for Pharmacogenomics Studies
| Tool/Reagent | Function/Application | Implementation Example |
|---|---|---|
| Long-Read Sequencers (PacBio, Oxford Nanopore) | Resolve complex pharmacogene loci (e.g., CYP2D6, CYP2A6) with structural variants; generate haplotype-resolved data [10]. | Comprehensive CYP2D6 star-allele calling including hybrid alleles and copy number variations [10]. |
| EHR-Linked Biobanks (UK Biobank, All of Us) | Provide genotype data linked to longitudinal medication records and clinical outcomes for pharmacoepidemiologic studies [10]. | Identification of novel genetic variants associated with warfarin maintenance dose in 200,000 participants [10]. |
| CLIA-Certified Laboratories | Ensure clinical-grade genotyping for validation studies and implementation projects; required for return of results to patients. | Processing of DNA samples for multigene panels like the RightMed test [102]. |
| Clinical Decision Support (CDS) Systems | Integrate PGx results into electronic health records to provide point-of-care alerts based on CPIC guidelines [100]. | Alert for CYP2C19 poor metabolizers when clopidogrel is prescribed, suggesting alternative antiplatelets [100]. |
| PharmGKB Database | Curated knowledge resource for drug-gene associations, variant annotations, and dosing guidelines [88]. | Reference for evidence levels and functional annotations of pharmacogenetic variants during analysis. |
| CPIC Guidelines | Evidence-based protocols for translating genotype results into prescribing actions for specific drug-gene pairs [100] [73]. | Standardized protocol for TPMT genotyping to guide thiopurine dosing in autoimmune diseases and oncology [100]. |
The strategic selection between multigene panels and single-gene tests represents a critical inflection point for pharmacogenomics research and implementation. While single-gene testing offers a straightforward reactive model for specific drug-gene pairs with proven cost-effectiveness, multigene panel testing provides a transformative, preemptive framework that aligns with the longitudinal nature of medication use across a patient's lifetime.
Economic evidence strongly supports both approaches, with 71% of cost-effectiveness studies favoring pharmacogenetic testing overall, and simulation models projecting substantial savings from multigene panel implementation—particularly through adverse event avoidance. The modest premium for multigene panels (approximately equivalent to two single-gene tests) delivers exponential value through lifelong application across multiple therapeutic areas.
For researchers and drug development professionals, multigene panels offer efficient comprehensive profiling that accelerates pharmacogenomic discovery and validation. Emerging technologies—including long-read sequencing, AI-driven prediction models, and multiomics integration—are rapidly enhancing our ability to detect and interpret clinically relevant variants. The ongoing development of EHR-linked biobanks provides unprecedented resources for validating pharmacogenomic associations across diverse populations.
Implementation success requires robust infrastructure including CLIA-certified laboratories, clinical decision support systems integrated into EHRs, and adherence to evidence-based guidelines like those from CPIC. As these elements mature, preemptive multigene panel testing is poised to become the foundational standard for precision medicine, enabling truly personalized, predictive, and preventive pharmacotherapy.
Evidence Validation and Global Policy Frameworks: Regulatory Science and Health Economics
Pharmacogenomics (PGx) has emerged as a vital component of precision medicine, transforming the fundamental paradigm from "one drug fits all" to tailored therapeutic strategies [1]. This field provides critical insights into how genetic variations influence individual responses to medications, enabling healthcare providers to optimize drug efficacy while minimizing adverse drug reactions (ADRs). The global implementation of PGx, however, faces significant challenges due to substantial variations in regulatory policies and guidelines across international jurisdictions [1]. These disparities create complexities for researchers, pharmaceutical developers, and healthcare systems attempting to integrate PGx into clinical practice and drug development on a global scale.
Regulatory agencies worldwide have developed different approaches to PGx implementation, reflecting varying scientific perspectives, healthcare infrastructures, and policy frameworks. Among these, the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) represent two of the most influential regulatory bodies whose guidelines significantly impact global drug development and clinical practice [104]. Understanding the similarities, differences, and harmonization efforts between these agencies is essential for advancing pharmacogenomics within personalized medicine research and ensuring the safe and effective implementation of PGx-guided therapies across diverse patient populations.
Global Regulatory Frameworks for Pharmacogenomics
Key Regulatory Bodies and Their Roles
Table 1: Major International PGx Guideline Issuing Bodies
| Organization | Region/Scope | Primary Function in PGx | Key Outputs |
|---|---|---|---|
| U.S. Food and Drug Administration (FDA) | United States | Regulatory oversight of drug safety and efficacy; issues PGx guidance for industry [1] | PGx biomarker tables; drug labeling requirements; data submission guidance |
| European Medicines Agency (EMA) | European Union | Scientific evaluation and supervision of medicines; provides PGx guidelines for medicine developers [105] | Summary of Product Characteristics (SmPC); scientific guidelines |
| Clinical Pharmacogenetics Implementation Consortium (CPIC) | Global | Creates evidence-based, peer-reviewed guidelines for translating genetic data into prescribing decisions [1] [106] | Gene/drug clinical practice guidelines |
| Dutch Pharmacogenetics Working Group (DPWG) | Netherlands/Europe | Develops guidelines to optimize drug therapy based on genetic polymorphisms [106] | Gene/drug interaction guidelines |
| World Health Organization (WHO) | Global | Provides global leadership on health; established Technical Advisory Group on Genomics [1] | Global recommendations on genomic implementation |
Foundational Regulatory Approaches
The FDA has established a comprehensive pharmacogenomics policy framework that extends to clinical, research, and industry settings [1]. The agency's approach includes issuing guidance documents on PGx and genetic tests for heritable markers, maintaining a Table of Pharmacogenomic Biomarkers in Drug Labeling, authorizing direct-to-consumer tests for medication metabolism variants, and issuing safety communications about genetic tests with unapproved claims [1]. The FDA's regulatory authority encompasses mandatory requirements for pharmacogenomic data submissions during drug development, with specific guidance documents outlining when and how sponsors should submit PGx data in investigational new drug applications (INDs), new drug applications (NDAs), and biologics license applications (BLAs) [107] [108].
In contrast, the EMA's regulatory structure differs fundamentally from the FDA's centralized model. While the FDA has direct authority to approve drug products, the EMA evaluates submissions and provides non-binding recommendations to the European Commission (EC), which issues the final marketing authorization [104]. The EMA provides scientific guidelines on pharmacogenomics to help medicine developers prepare marketing authorization applications for human medicines [105]. This process involves the Committee for Medicinal Products for Human Use (CHMP), which conducts scientific assessments, though in practice the EC nearly always follows the CHMP's recommendations [104].
Comparative Analysis of FDA and EMA PGx Guidelines
Methodological Framework for Regulatory Comparison
Experimental Protocol 1: Systematic Analysis of PGx Guideline Concordance
- Objective: To quantitatively evaluate the concordance between PGx guidelines issued by the FDA, EMA, and academic consortia (CPIC/DPWG).
- Data Sources: FDA's "Table of Pharmacogenomic Biomarkers in Drug Labeling" [14], EMA's Summary of Product Characteristics (SmPC) documents, CPIC and DPWG guidelines [106].
- Drug Selection Criteria: Include drugs with actionable gene-drug interactions in CPIC/DPWG guidelines and drugs with PGx information in FDA/EMA labeling [106].
- Categorization Framework:
- No information: No mention of gene-drug interaction
- PGx information: Mention of gene-drug interaction without specific actions
- Recommendation: Suggested action for gene-drug interaction
- Strong recommendation: Specific dose adjustments required
- Contraindication: Drug contraindicated in specific genetic backgrounds
- Mandatory: Required testing or adjustments based on genetics [106]
- Analysis Method: Independent categorization by multiple reviewers with consensus process for discrepant categorizations. Actionable labels defined as categories 3-6 above [106].
Figure 1: Workflow for systematic comparison of PGx guidelines across regulatory agencies and consortia.
Quantitative Analysis of Regulatory Concordance
Table 2: Comparative Analysis of Actionable PGx Labeling Between FDA and EMA
| Metric | FDA | EMA/FM* | Concordance | Reference |
|---|---|---|---|---|
| Drugs with actionable PGx labels | 126 drugs with actionable gene-drug labels by FDA and/or EMA/FM | 54% consensus in actionable PGx labeling between FDA and EMA/FM | [106] | |
| CPIC/DPWG guideline implementation | 50% of drugs with CPIC/DPWG actionable interactions had actionable PGx information in SmPCs | [106] | ||
| Agency agreement on CPIC/DPWG drugs | 18% of cases showed agreement between agencies on CPIC/DPWG drugs | [106] | ||
| PGx biomarker categories | Germline or somatic gene variants, functional deficiencies with genetic etiology, gene expression differences, chromosomal abnormalities, selected protein biomarkers [14] | Similar scope but different implementation emphasis |
*EMA/FM refers to European Medicines Agency plus national agencies (FIDMD+MEB) for drugs approved before EMA founding in 1995 [106]
Case Study: Carbamazepine Regulatory Approaches
Experimental Protocol 2: Analysis of HLA-B*15:02 Screening Requirements
- Background: Carbamazepine, an essential antiepileptic medication, is associated with increased risk of severe cutaneous adverse reactions (SCARs), including Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis (SJS/TEN) in patients carrying the HLA-B*15:02 allele [1].
- Prevalence Considerations: The HLA-B*15:02 allele prevalence varies significantly across populations (5-15% in Han Chinese, 8-27% in Thais, but low in European populations) [1].
- Regulatory Analysis Framework:
- Identify carbamazepine labeling requirements across agencies
- Compare screening recommendations for different populations
- Analyze consistency of cross-reactivity warnings for other aromatic antiepileptics
- Findings: All examined countries recognized genetic variation in carbamazepine response within their guidelines, showing notable consistency in this specific case [1].
Figure 2: Regulatory response to carbamazepine pharmacogenomics across agencies.
Implementation Frameworks and Research Methodologies
Pharmacogenomic Data Submission Standards
Table 3: Comparative PGx Data Submission Requirements
| Parameter | FDA Requirements | EMA Requirements |
|---|---|---|
| Submission Timing | During IND, NDA, and BLA processes; specific guidance on required vs. voluntary submissions [107] [108] | During marketing authorization application process |
| Data Types | Genomic biomarkers (germline or somatic variants, functional deficiencies, gene expression, chromosomal abnormalities) [14] | Similar scope with potential differences in emphasis and application |
| Technical Standards | Format and content specifications provided in guidance documents [108] | Scientific guidelines for medicine developers [105] |
| Regulatory Impact | Data used in regulatory decision-making for drug safety and efficacy | Considered in benefit-risk assessment during marketing authorization |
Clinical Implementation and Laboratory Standards
In the United States, the Centers for Medicare & Medicaid Services (CMS) regulates all non-research laboratory testing through the Clinical Laboratory Improvement Amendments (CLIA). While any laboratory can develop a PGx test, clinical use of test results requires CLIA certification [1]. This framework ensures analytical validity but does not directly assess clinical utility, creating a complex regulatory landscape where laboratories must navigate both FDA and CLIA requirements.
The FDA maintains the "Table of Pharmacogenetic Associations," which categorizes gene-drug interactions with sufficient scientific evidence to suggest altered drug metabolism or differential therapeutic effects [109]. This resource distinguishes between associations that support therapeutic management recommendations and those with more preliminary evidence, providing crucial guidance for researchers and clinicians navigating the rapidly evolving PGx landscape.
Research Reagents and Methodological Toolkit
Table 4: Essential Research Reagents and Resources for PGx Regulatory Science
| Resource Category | Specific Examples | Research Application | Regulatory Relevance |
|---|---|---|---|
| Genomic Databases | PharmGKB, dbSNP, 1000 Genomes | Variant frequency data, functional annotation | Population-specific biomarker validation |
| Clinical Guideline Repositories | CPIC, DPWG guidelines | Evidence-based prescribing recommendations | Informing regulatory labeling decisions |
| Biomarker Compendiums | FDA Table of Pharmacogenomic Biomarkers [14], FDA Table of Pharmacogenetic Associations [citation:5 | Reference for validated biomarkers | Direct regulatory guidance for drug development |
| Adverse Event Databases | FDA Adverse Event Reporting System (FAERS), EudraVigilance [29] | Post-market safety signal detection | Pharmacovigilance requirement for safety monitoring |
| Genetic Testing Standards | CDC GeT-RM program, CLIA standards | Test validation and quality control | Laboratory compliance requirements |
Future Directions and Global Harmonization
The field of pharmacogenomics continues to evolve rapidly, with several emerging trends shaping the future regulatory landscape. Advanced artificial intelligence (AI) and machine learning (ML) methods now facilitate analysis of complex genetic data, revealing insights not previously available from traditional analytical approaches [29]. These technologies enhance the capability to identify ADRs linked to specific genotypes, enabling more targeted risk management strategies and personalized therapeutic approaches.
Global harmonization of pharmacogenomics policies remains an essential but challenging goal. The current discrepancies between major regulatory agencies create inefficiencies for drug developers and uncertainties for healthcare providers implementing PGx testing [106]. As research demonstrates, there is "a huge discrepancy between information given by the CPIC and DPWG and the pharmacogenomic information in drugs labels in the corresponding SmPC," highlighting the need for greater alignment between academic consortia and regulatory bodies [106]. Furthermore, significant differences between U.S. and European regulatory approaches complicate global drug development and clinical implementation efforts.
The promising trend toward international cooperation between the EMA and FDA, including parallel scientific advice procedures, represents a positive step toward reducing regulatory divergence [104]. However, substantial work remains to achieve the level of harmonization needed for efficient global implementation of pharmacogenomics. Future efforts should focus on standardizing evidence requirements for PGx biomarkers, aligning clinical validity standards across jurisdictions, and developing mutually recognized regulatory pathways for pharmacogenomically-guided therapies.
The global regulatory landscape for pharmacogenomics is characterized by both significant progress and substantial challenges. While the FDA and EMA, along with international guideline developers, have established frameworks for implementing PGx in drug development and clinical care, important differences in approach, interpretation, and requirements persist. These disparities reflect legitimate differences in regulatory philosophy, healthcare systems, and population genetics, but they also create barriers to the global advancement of personalized medicine.
The comprehensive comparison presented in this analysis demonstrates that regulatory harmonization remains a critical unmet need in pharmacogenomics. Researchers and drug developers must navigate this complex landscape by understanding the specific requirements of different agencies, engaging early with regulatory bodies through consultation procedures, and designing development programs that can generate evidence meeting multiple regulatory standards. As the field continues to evolve, ongoing efforts toward global harmonization will be essential for realizing the full potential of pharmacogenomics to deliver on the promise of personalized medicine—ensuring that the right patient receives the right drug at the right dose, regardless of geographic location.
The integration of pharmacogenomics (PGx) into personalized medicine requires robust clinical evidence gathered through both traditional Randomized Controlled Trials (RCTs) and Real-World Implementation Studies. These complementary evidence-generation frameworks serve distinct yet interconnected roles in validating the clinical utility of genotype-guided therapy and translating these findings into routine care. RCTs provide controlled evidence of efficacy under ideal conditions, while implementation studies assess effectiveness and feasibility in real-world clinical settings, addressing practical barriers to adoption [110]. This methodological duality is essential for establishing a complete evidence chain from PGx discovery to widespread clinical application, ultimately fulfilling the promise of personalized medicine by ensuring the right drug and dose for each patient based on their genetic profile.
Randomized Controlled Trials in Pharmacogenomics
Fundamental Designs and Objectives
Randomized Controlled Trials represent the gold standard for establishing causal relationships between PGx-guided interventions and clinical outcomes. In pharmacogenomics, RCTs primarily aim to determine whether a subgroup of patients identified by genetic characteristics responds differently to treatment or to verify if a genotype-guided treatment strategy provides superior outcomes compared to standard care [111]. These trials are characterized by controlled conditions, strict inclusion/exclusion criteria, and rigorous protocol adherence to minimize variability and bias.
PGx RCTs employ several specific designs that differ in the timing of randomization and genotyping. The prospective genotype-stratified design randomizes all eligible patients but pre-stratifies by genotype, ensuring balanced allocation across treatment arms for key genetic subgroups. The genotype-guided design randomizes participants to either genotype-guided therapy or standard care, testing the utility of the genetic information itself in clinical decision-making. A third approach involves retrospective genotyping of participants from a completed RCT to identify genetic associations with drug response, though this method may be limited by sample availability and statistical power [111]. Each design addresses different research questions and has specific advantages depending on the known genetic associations and clinical context.
Quantitative Landscape of PGx Clinical Trials
An analysis of ClinicalTrials.gov through June 2023 revealed that of 350,728 registered interventional studies, only 619 (0.18%) contained pharmacogenetics-related terms, indicating that while growing, PGx-focused clinical research remains a specialized domain [112]. The distribution of these trials across medical specialties demonstrates particular concentration in certain therapeutic areas, and the most frequently studied genes reflect those with well-established roles in drug metabolism and response.
Table 1: Distribution of PGx Clinical Trials by Medical Specialty
| Medical Specialty | Percentage of PGx Trials | Key Genetic Focus Areas |
|---|---|---|
| Oncology | 28.43% | DPYD, UGT1A1, TPMT, CYP2D6 |
| Mental Health | 10.66% | CYP2D6, CYP2C19, HLA-B |
| Cardiology | 7.10% | CYP2C19, CYP2C9, VKORC1 |
| Pain Management | 5.80% | CYP2D6, OPRM1 |
| Transplantation | 4.70% | CYP3A5, ABCB1 |
| Hematology | 3.90% | CYP2C9, VKORC1 |
Table 2: Most Frequently Studied Genes in PGx Clinical Trials
| Gene | Number of Clinical Trials | Primary Therapeutic Areas |
|---|---|---|
| CYP2D6 | 46 | Mental Health (28.26%), Pain Management |
| CYP2C9 | 28 | Hematology, Cardiology |
| CYP2C19 | 35 | Cardiology, Mental Health |
| ABCB1 | 18 | Transplantation, Cardiology |
| CYP3A5 | 15 | Transplantation, Cardiology |
Trial phase distribution among PGx clinical trials shows a balanced approach across development stages: Phase 1 (105 trials), Phase 2 (137 trials), Phase 3 (68 trials), and Phase 4 (127 trials), with 142 trials classified as "Not Applicable" [112]. This distribution reflects both drug development applications and implementation-focused research of already approved medications.
Representative RCT Protocol: The GUIDED Trial
The Genomics Used to Improve DEpression Decisions (GUIDED) trial exemplifies a rigorously designed PGx RCT examining clinical utility in a challenging therapeutic area [113].
Objective: To determine whether pharmacogenomics-guided treatment improves outcomes for patients with major depressive disorder (MDD) who have previously had inadequate response to antidepressant therapy.
Methodology:
- Design: Rater- and patient-blind, randomized controlled trial.
- Participants: 1,167 outpatients diagnosed with MDD with patient- or clinician-reported inadequate response to at least one antidepressant.
- Intervention: Patients were randomized to treatment-as-usual (TAU) or a pharmacogenomics-guided intervention arm where clinicians had access to a pharmacogenomic test report to inform medication selection (guided-care).
- Genetic Assessment: The test categorized medications as 'use as directed,' 'use with caution,' or 'use with increased caution and with more frequent monitoring' based on the patient's genotype.
- Primary Outcome: Symptom improvement measured by change in 17-item Hamilton Depression Rating Scale (HAM-D17) at week 8.
- Secondary Outcomes: Response (≥50% decrease in HAM-D17) and remission (HAM-D17 ≤7) at week 8.
Key Findings: While symptom improvement between groups did not reach statistical significance (27.2% guided-care vs. 24.4% TAU, p=0.107), both response (26.0% vs. 19.9%, p=0.013) and remission (15.3% vs. 10.1%, p=0.007) rates showed statistically significant improvements in the guided-care group [113]. A particularly notable finding emerged from analyzing medication congruence: patients who switched from genetically incongruent medications at baseline to congruent medications by week 8 experienced substantially greater symptom improvement (33.5% vs. 21.1%, p=0.002), response (28.5% vs. 16.7%, p=0.036), and remission (21.5% vs. 8.5%, p=0.007) compared to those remaining on incongruent medications [113].
Diagram 1: GUIDED Trial Design Flow
Real-World Implementation Studies in Pharmacogenomics
Defining Characteristics and Methodological Considerations
Real-world implementation studies differ fundamentally from traditional RCTs in both objectives and design. While RCTs aim to establish evidence of causality under controlled conditions, implementation studies seek to establish evidence of clinical utility in real-world settings and assess process indicators of implementation feasibility [110]. These studies are characterized by "all-comer" populations that better represent clinical practice, limited exclusion criteria, and flexible protocols that can adapt to evolving clinical environments.
The Preemptive Pharmacogenomic Testing for Preventing Adverse Drug Reactions (PREPARE) study exemplifies a large-scale PGx implementation study, employing an open-label, multicenter, controlled, cluster-randomized, crossover design across 18 hospitals, nine community health centers, and 28 community pharmacies in seven European countries [110]. This pragmatic design prioritized ecological validity over strict experimental control, reflecting how PGx testing would actually function in diverse healthcare settings.
Key Implementation Study Protocol: The PREPARE Study
The PREPARE study protocol represents a sophisticated approach to assessing real-world implementation of panel-based pharmacogenetic testing [110] [60].
Objective: To investigate the clinical utility of a panel-based pharmacogenetic approach in preventing adverse drug reactions (ADRs) in real-world settings and to assess process indicators of implementation.
Methodology:
- Design: Open-label, multicenter, controlled, cluster-randomized, crossover implementation study.
- Participants: 6,944 patients from primary care, oncology, and general medicine units receiving a first prescription for one of 39 drugs with clinical recommendations in the Dutch Pharmacogenetics Working Group (DPWG) guidelines.
- Genetic Intervention: A 12-gene pharmacogenetic panel (CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP3A5, DPYD, F5, HLA-B, SLCO1B1, TPMT, UGT1A1, VKORC1) testing for 50 germline variants.
- Intervention Arm: Non-mandatory advice to adjust standard treatment according to DPWG recommendations based on genotype results.
- Control Arm: Standard treatment without genetic guidance.
- Primary Outcome: Occurrence of clinically relevant ADRs within 12-week follow-up period after starting the index drug.
- Analysis: Intention-to-treat using gatekeeping analysis, first comparing outcomes in patients with actionable drug-gene interactions in study vs. control groups, followed by analysis of all patients if significant.
Key Findings: The study demonstrated a statistically significant 33% reduction in the incidence of clinically relevant ADRs in the genetically guided arm compared to standard care (21.5% vs. 28.6%) [60]. An remarkable 93.5% of patients had at least one actionable gene variant, highlighting the potential breadth of PGx application [60]. This large-scale implementation provided robust evidence that preemptive PGx testing can prevent ADRs in routine clinical care across diverse healthcare settings.
Diagram 2: PREPARE Study Cluster Randomized Crossover Design
Comparative Analysis: RCTs versus Implementation Studies
The fundamental differences between RCTs and implementation studies extend across multiple methodological dimensions, each serving distinct but complementary roles in the evidence generation continuum.
Table 3: Key Methodological Differences Between RCTs and Implementation Studies
| Characteristic | Randomized Controlled Trials | PGx Implementation Studies |
|---|---|---|
| Primary Aim | Establish evidence of causality | Establish evidence of clinical utility & implementation feasibility |
| Study Population | Selected, strict in/exclusion criteria | "All-comer" population, minimal exclusions |
| Intervention | Placebo-controlled or active comparator | PGx-guided therapy vs. standard care |
| Primary Endpoints | Efficacy (e.g., survival, symptom reduction) | Clinical outcome + process indicators |
| Randomization | Mostly patient-level randomization | Typically cluster-level randomization |
| Blinding | Double-blinding standard | Open-label to assess implementation strategy |
| Protocol Adherence | Strict protocol adherence | Pragmatic design, adaptations allowed |
| Generalizability | May have limited generalizability | High real-world generalizability |
Evidence Assessment Frameworks and Clinical Annotation
Standardized Evidence Evaluation Systems
The translation of PGx associations into clinically actionable recommendations requires systematic evidence assessment frameworks. The Pharmacogenomics Knowledgebase (PharmGKB) has developed a quantitative scoring system to assign Levels of Evidence (LOE) to clinical annotations, increasing transparency, consistency, and reproducibility [114].
The PharmGKB clinical annotation scoring system incorporates multiple evidence attributes:
- Phenotype Category: Higher points for clinical outcomes (efficacy, toxicity) versus intermediate phenotypes (metabolism/PK)
- Statistical Significance: Tiered points based on P-values, with stricter thresholds for genome-wide association studies
- Study Size: Graduated scoring based on cohort size, with higher points for larger studies
- Effect Size: Additional points for strong associations (OR/HR/RR <0.5 or >2) with supportive confidence intervals
- Study Type: Highest points for clinical studies, with deductions for negative associations [114]
This systematic approach enables objective comparison of evidence strength across different drug-gene pairs and supports clinical implementation decision-making.
Regulatory Perspectives on PGx Evidence
Regulatory agencies have established frameworks for evaluating PGx evidence, with the FDA maintaining a "Table of Pharmacogenetic Associations" that categorizes gene-drug interactions based on supporting evidence strength [109]. This table distinguishes between associations that merely inform pharmacological mechanisms versus those with sufficient evidence to recommend specific therapeutic actions.
The FDA recognizes several categories of pharmacogenetic associations:
- Associations supporting therapeutic management recommendations (e.g., HLA-B*57:01 testing before abacavir initiation)
- Associations informing potential dosage adjustments (e.g., CYP2D6-guided aripiprazole dosing)
- Associations highlighting potential toxicity risks (e.g., CYP2C19 status and clopidogrel effectiveness)
- Pharmacokinetic associations without specific prescribing recommendations [109]
This graded regulatory approach acknowledges that different levels of evidence warrant distinct clinical actions, providing a framework for appropriate implementation based on evidence maturity.
Research Reagents and Methodological Tools
Table 4: Essential Research Reagents and Resources for PGx Studies
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Curated Knowledgebases | PharmGKB, CPIC Guidelines, DPWG Guidelines | Evidence synthesis, clinical interpretation, phenotype translation |
| Genotyping Technologies | Targeted arrays, Next-generation sequencing panels, CYP2D6 cascade | Variant detection, star allele calling, novel variant discovery |
| Clinical Implementation Tools | CDS hooks, EHR integration platforms, patient registries | Real-world implementation, workflow integration, outcome assessment |
| Analytical Frameworks | PharmGKB LOE scoring, CPIC level assignment, FDA biomarker table | Evidence assessment, clinical actionability determination |
| Study Design Resources | Cluster randomization protocols, crossover templates, pragmatic trial frameworks | Implementation study design, bias minimization, real-world generalization |
Current Challenges and Future Directions
Despite substantial progress, significant challenges remain in PGx evidence generation and implementation. Persistent barriers include the underrepresentation of diverse populations in pharmacogenetics research, disagreements on evidence thresholds for clinical utility, sparse or inconsistent insurance coverage, limited EHR integration capabilities, and knowledge gaps among healthcare providers [9]. Additionally, the field continues to grapple with methodological questions about the optimal study designs for demonstrating clinical utility and the appropriate balance between evidentiary rigor and practical implementation needs.
Future directions should prioritize inclusive research populations to ensure equitable benefit, develop multigene testing approaches that efficiently capture multiple clinically relevant variants simultaneously, establish standardized evidence thresholds across regulatory and payer organizations, and enhance educational resources for both providers and patients [9]. The ongoing European Partnership for Personalised Medicine (EP PerMed) JTC2025 call, focusing on "Pharmacogenomic Strategies for Personalised Medicine," represents a coordinated multinational effort to address these challenges through targeted research funding [22]. As the field evolves, the complementary roles of RCTs and implementation studies will continue to be essential for generating the comprehensive evidence base needed to realize the full potential of pharmacogenomics in personalized medicine.
CPIC Guidelines and Their Role in Standardizing Clinical Practice
The Clinical Pharmacogenetics Implementation Consortium (CPIC) is an international consortium established in 2009 as a shared project between PharmGKB and the Pharmacogenomics Research Network (PGRN) [115]. CPIC's primary mission is to facilitate the use of pharmacogenetic tests in patient care by overcoming a critical barrier: the difficulty in translating genetic laboratory test results into actionable prescribing decisions for affected drugs [115]. This non-profit organization, sustained by volunteers and a small dedicated staff, creates, curates, and disseminates freely available, peer-reviewed, evidence-based, updatable, and detailed gene/drug clinical practice guidelines [115].
CPIC functions as a pivotal component in the personalized medicine ecosystem by providing the necessary framework to operationalize pharmacogenomic knowledge. The consortium's guidelines have become the global standard for translating pharmacogenomic test results into clinical actionable recommendations, with demonstrated widespread adoption across healthcare institutions and electronic health record systems [116]. By establishing standardized processes for interpreting genetic test results and linking them to therapeutic recommendations, CPIC has evolved from a guideline development initiative into a global leader in pharmacogenomics implementation, fostering collaboration, standardization, and sustainable integration into diverse healthcare settings [116].
The CPIC Guideline Development Framework
Systematic Methodology and Evidence Grading
The CPIC guideline development process follows a rigorous, standardized methodology designed to ensure consistency, reliability, and evidence-based recommendations. Each CPIC guideline adheres to a standardized format that includes a systematic approach for grading levels of evidence linking genotypes to phenotypes, assigning phenotypes to clinical genotypes, developing prescribing recommendations based on genotype/phenotype relationships, and assigning strength to each prescribing recommendation [117]. This structured process is detailed in their Standard Operating Procedure published in Current Drug Metabolism, which outlines the comprehensive approach for incorporating pharmacogenomics into routine clinical practice [117].
A fundamental principle of CPIC guidelines is that they are designed to help clinicians understand HOW available genetic test results should be used to optimize drug therapy, rather than WHETHER tests should be ordered [117]. This approach aligns with the consortium's key assumption that clinical high-throughput and pre-emptive (pre-prescription) genotyping will become more widespread, meaning clinicians will increasingly have patients' genotypes available even without ordering a test for a specific drug [117]. The guidelines undergo rigorous peer review and are published in a leading journal (in partnership with Clinical Pharmacology and Therapeutics) with simultaneous posting to cpicpgx.org, where they are regularly updated [115].
Gene-Drug Pair Prioritization and Evidence Assessment
CPIC employs a systematic approach for prioritizing gene-drug pairs and assessing evidence levels. The consortium assigns CPIC levels to genes/drugs based on several criteria, including ClinPGx Summary Annotation Levels of Evidence of 1A, 1B, 2A, and 2B, or a ClinPGx PGx level for FDA-approved drug labels of "actionable pgx," "genetic testing recommended," or "genetic testing required" [118]. Gene-drug pairs may also be considered based on nomination to CPIC for guideline development [118].
The CPIC level assignments are categorized as follows [118]:
- CPIC Level A: Gene/drug pairs with sufficient evidence for recommending prescribing actions
- CPIC Level B: Gene/drug pairs with moderate evidence for recommending prescribing actions
- CPIC Level C: Gene/drug pairs with limited evidence that does not support prescribing recommendations
- CPIC Level D: Gene/drug pairs with inadequate evidence for any prescribing actions
Only CPIC Level A and B gene/drug pairs have sufficient evidence for at least one prescribing action to be recommended, making these the primary focus of guideline development [118]. To date, CPIC guidelines cover 34 genes and 164 drugs, demonstrating the substantial scope of their evidence-based recommendations [116].
Table 1: CPIC Guideline Development Framework Components
| Component | Description | Purpose |
|---|---|---|
| Evidence Grading | Systematic evaluation of literature linking genotypes to phenotypes | Ensure recommendations are based on robust evidence |
| Phenotype Assignment | Standardized method for translating diplotypes to phenotypes | Create consistent interpretation across institutions |
| Recommendation Strength | Categorization of prescribing recommendations (strong, moderate, optional) | Guide clinical decision-making with appropriate flexibility |
| Updatable Process | Regular review and revision of guidelines | Incorporate new evidence and maintain currency |
| Peer Review | Formal review process through journal partnership | Ensure quality and credibility through independent evaluation |
Term Standardization: A Foundational Element for Implementation
The Delphi Consensus Methodology for Term Development
CPIC recognized early that the lack of standardized terminology for reporting pharmacogenetic test results presented a significant barrier to clinical implementation. To address this challenge, CPIC led a comprehensive term standardization project using a modified Delphi method to develop consensus among pharmacogenetics experts [119]. This structured approach involved multiple iterative surveys designed to systematically refine expert opinion and reach consensus on uniform terms that could be applied across pharmacogenes to characterize allele functional status and inferred phenotypes based on diplotypes [119].
The Delphi process began with identifying terms currently used by genetic testing laboratories and in the scientific literature through an extensive review of laboratory reports and publications [119]. Experts with diverse involvement in pharmacogenetics (including clinicians, researchers, genetic testing laboratorians, pharmacogenetics implementers, and clinical informaticians) participated in the process [119]. After completion of five surveys, a consensus (>70%) was reached with 90% of experts agreeing to the final sets of pharmacogenetic terms [119]. The entire process emphasized semantic consistency and practical utility for clinical implementation.
Standardized Term Categories and Applications
The term standardization initiative focused on developing consistent terminology for two primary aspects of pharmacogenetic test results: (1) allele functional status (descriptive terms for individual alleles), and (2) inferred phenotypes (based on the combined impact of both alleles in a diplotype) [119]. The experts ultimately organized pharmacogenes into three categories for terminology purposes [119]:
- Drug-metabolizing enzymes (e.g., CYP enzymes, UGT1A1, DPYD, TPMT)
- Drug transporters and non-drug metabolizing enzymes (e.g., SLCO1B1, VKORC1)
- High-risk genotypes (e.g., HLA-B)
This categorization allowed for development of appropriate terminology sets for each group while maintaining consistency within categories. The standardized terms have proven essential for facilitating the exchange of structured interpretations between laboratories, electronic health records systems, and patients' personal health records, significantly improving interoperability and the portability of results throughout a patient's lifetime [119].
Expansion of Standardization Efforts
Building on the success of the initial terminology project, CPIC has initiated a second term standardization project to address additional genes not covered in the first effort [120]. This expansion includes genes such as VKORC1 (important for warfarin dosing), RYR1, CACNA1S, CFTR, G6PD, IFNL3, and mtRNR1, among others [120]. The ongoing effort demonstrates CPIC's commitment to comprehensive terminology standardization across the entire pharmacogenetics landscape.
The VKORC1 gene presented particular challenges for standardization because it is tested primarily in the context of predicting starting doses of warfarin, which also depends on CYP2C9 genotypes [120]. Consequently, many laboratories report a drug-centered phenotype such as "greatly increased sensitivity to warfarin" rather than using the standardized terminology formats applied to other genes [120]. These complex cases require specialized approaches to terminology development while maintaining alignment with the overall standardization framework.
Implementation Impact and Global Adoption
Quantitative Assessment of CPIC Utilization
The global impact of CPIC guidelines is demonstrated through comprehensive analysis of implementation metrics. Recent data highlights substantial growth and widespread adoption across diverse healthcare settings [116]. As of 2025, CPIC has developed 28 active guidelines with international authorship that have garnered over 10,000 citations and 1.4 million views, reflecting their substantial influence on the field [116]. Bibliometric analyses and internal tracking mechanisms reveal robust implementation, with 85% of PubMed-indexed pharmacogenomic implementation studies referencing CPIC guidelines [116].
The practical adoption of CPIC resources extends across the healthcare ecosystem, with 128 healthcare institutions and 40 commercial laboratories reporting use of CPIC content in their pharmacogenetics programs [116]. The technical integration of CPIC guidelines is facilitated through an API that supports over 80,000 monthly queries, increasingly embedded within electronic health record systems including Epic's foundational genomics module [116]. This level of integration demonstrates the real-world utility of CPIC guidelines in facilitating clinical decision support at the point of care.
Table 2: CPIC Guideline Impact Metrics (2019-2024)
| Metric Category | Specific Measure | Quantitative Impact |
|---|---|---|
| Guideline Output | Active Guidelines | 28 |
| Guideline Output | Genes Covered | 34 |
| Guideline Output | Drugs Covered | 164 |
| Academic Influence | Total Citations | >10,000 |
| Academic Influence | Guideline Views | 1.4 million |
| Academic Influence | Implementation Studies Referencing CPIC | 85% |
| Clinical Implementation | Healthcare Institutions Using CPIC | 128 |
| Clinical Implementation | Commercial Laboratories Using CPIC | 40 |
| Technical Integration | Monthly API Queries | 80,000+ |
| Professional Endorsement | Major Society Endorsements | ASHP, ASCPT, CAP, ClinGen, PharmGKB |
Evolution of Implementation Barriers
Longitudinal assessment of implementation challenges reveals a significant shift in the primary barriers to pharmacogenomics adoption. CPIC member surveys conducted in 2012 and 2024 demonstrate an evolution from concerns about the scientific evidence base to practical obstacles related to clinical workflow integration [116]. Earlier implementation efforts were predominantly hampered by questions about the robustness of evidence linking genetic variants to drug response outcomes. As the evidence base has matured through systematic curation and guideline development, the focus has shifted to operational challenges.
Contemporary barriers identified in recent surveys include clinician education, reimbursement structures, and EHR integration complexities [116]. This transition reflects the maturation of the field and the successful establishment of the evidence foundation through CPIC's rigorous guideline development process. The consortium has correspondingly expanded its focus to address these implementation challenges through supplementary resources, educational initiatives, and collaboration with EHR vendors to facilitate seamless integration of pharmacogenetic decision support.
CPIC provides a comprehensive suite of resources that serve as essential tools for researchers and clinicians implementing pharmacogenomics. These resources facilitate the translation of genetic data into clinically actionable recommendations and support standardization across institutions. The following table details key resources available through CPIC and partner organizations.
Table 3: Essential Research Reagents and Resources for Pharmacogenomics Implementation
| Resource Name | Type | Function | Access Platform |
|---|---|---|---|
| CPIC Guidelines | Evidence-based clinical guidelines | Translate genetic test results into actionable prescribing recommendations | cpicpgx.org & CPT Journal |
| PharmGKB | Knowledge resource | Curate pharmacogenetic variants, annotations, and drug-centered pathways | pharmgkb.org |
| CPIC API | Technical interface | Enable automated integration of CPIC recommendations into EHR systems | cpicpgx.org/api |
| Term Standardization Tables | Standardized nomenclature | Ensure consistent terminology for allele function and phenotype across laboratories | CPIC Guidelines Tables 1 & 2 |
| Phenotype Translator | Computational algorithm | Convert diplotype data into predicted phenotype categories | Incorporated in CPIC guidelines |
| Pharmacogene Curation Expert Panels (PCEPs) | Expert consensus groups | Assign clinical function to pharmacogene alleles through systematic evidence review | Multidisciplinary expert panels |
Methodological Protocols for Implementation
For researchers seeking to implement CPIC guidelines in clinical or research settings, CPIC provides detailed methodological frameworks that ensure consistent application of their recommendations. The Pharmacogene Curation Expert Panels (PCEPs) represent a critical methodological resource, comprising multidisciplinary experts who systematically review and evaluate evidence to assign functional status to pharmacogenetic haplotypes [121]. These panels employ rigorous evidence assessment protocols, standardized terminology, and consensus-driven functional assignments that form the foundation for CPIC guidelines.
The process for assigning clinical function to pharmacogene alleles follows a transparent framework that encourages global participation and feedback from the pharmacogenomics community [121]. This inclusive approach promotes adoption of CPIC guidelines in clinical practice while maintaining methodological rigor. For implementation scientists, CPIC provides explicit guidance on integrating these resources into clinical decision support systems, including standardized approaches for handling ambiguous genotypes, rare variants, and special populations.
The Clinical Pharmacogenetics Implementation Consortium has established itself as the global standard for translating pharmacogenomic knowledge into clinically actionable guidance. Through its systematic guideline development process, terminology standardization initiatives, and implementation resources, CPIC has addressed critical barriers to the clinical adoption of pharmacogenomics. The demonstrated impact—with widespread integration across healthcare institutions, commercial laboratories, and electronic health record systems—confirms the essential role CPIC plays in advancing personalized medicine.
As the field continues to evolve, CPIC's standardized frameworks and evidence-based approach provide the necessary foundation for scalable implementation of pharmacogenomics across diverse healthcare settings. The consortium's focus on addressing practical implementation barriers while maintaining scientific rigor positions it as a continuing driving force in the realization of personalized medicine, ensuring that pharmacogenetic discoveries are effectively translated into optimized drug therapy for individual patients.
Defining Biomarkers and Their Regulatory Significance
A biomarker is a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention, including therapeutic interventions [122]. Biomarkers encompass molecular, histologic, radiographic, or physiologic characteristics that provide a valuable window into the body's inner workings, offering objective data beyond how a patient feels, functions, or survives [122] [123]. The FDA Biomarker Qualification Program (BQP) mission focuses on working with external stakeholders to develop biomarkers as drug development tools, advancing public health by encouraging efficiencies and innovation in drug development [124].
Biomarkers serve critical functions across the drug development continuum, from diagnosing diseases (e.g., sweat chloride for cystic fibrosis), determining risk (e.g., BRCA mutations for breast cancer), monitoring disease status (e.g., PSA for prostate cancer), watching for treatment side effects, and measuring patient response to drugs [123]. In pharmacogenomics, biomarkers enable personalized medicine by identifying genetic variations that influence drug metabolism and response, as demonstrated by cytochrome P450 genes (CYP2D6, CYP2C19, CYP1A2) that significantly impact antidepressant efficacy and safety profiles [125].
The Role of Biomarker Validation in Personalized Medicine
Biomarker validation represents a cornerstone of precision medicine, providing the evidentiary foundation for translating pharmacogenomic research into clinical practice. Validated biomarkers allow researchers to stratify patient populations, predict treatment response, optimize dosing regimens, and minimize adverse drug reactions. The validation process ensures that biomarkers consistently produce reliable, interpretable results that can inform regulatory decisions and clinical care [122]. For pharmacogenomics to realize its potential in personalized medicine, robust biomarker validation frameworks are essential to establish scientific credibility and clinical utility across diverse patient populations [9].
FDA Regulatory Framework for Biomarker Evaluation
The FDA Biomarker Qualification Program provides a formal regulatory pathway for qualifying biomarkers for use in drug development programs. Once qualified, a biomarker can be used in any drug development program for the specified context of use without needing FDA to reconsider and reconfirm its suitability in each application [126]. This program addresses a critical market need, as Janet Woodcock, a former FDA official, explained: "One of the problems with biomarkers is there is really no one in charge of developing them. What we are seeking at FDA is public adoption of new biomarkers by the scientific community" [123].
The qualification process is collaborative, often involving multiple interested parties working together in working groups or consortia to develop a biomarker for qualification. This approach allows for shared resources and reduces the burden on individual collaborators, encouraging participation despite limited resources [122]. The 21st Century Cures Act formalized this process, establishing a structured, transparent pathway for biomarker qualification with specific submission stages and transparency provisions requiring public posting of qualification determinations [122].
The Three-Stage Qualification Process
The FDA's biomarker qualification process follows three distinct stages, each with specific objectives and requirements:
Stage 1: Letter of Intent (LOI)
A requestor submits an LOI providing initial information about the biomarker proposal, including the drug development need the biomarker addresses, biomarker information, context of use (COU), and information on how the biomarker will be measured. The FDA reviews the LOI to assess the biomarker's potential value and the proposal's overall feasibility based on current scientific understanding. If accepted, the requestor may submit a Qualification Plan [122]. The FDA aims to complete its review of LOIs within 3 months, though analyses indicate median review times often exceed these targets [123].
Stage 2: Qualification Plan (QP)
The QP is a detailed proposal describing the biomarker development plan to provide necessary information for qualifying the biomarker for the proposed COU. It summarizes existing supporting information, identifies knowledge gaps, and proposes approaches to address these gaps. The QP must include detailed information about the analytical method and performance characteristics [122]. FDA provides a revised Qualification Plan Content Element Outline (July 2025) with comprehensive instructions for preparing QP submissions [126]. The agency aims to review QPs within 6 months [123].
Stage 3: Full Qualification Package (FQP)
The FQP represents a comprehensive compilation of supporting evidence that informs the FDA's qualification decision. It contains all accumulated information, organized by topic area, and serves as the basis for the FDA's final determination about whether to qualify the biomarker [122]. The FDA aims to review FQPs within 10 months [123]. Upon successful qualification, the biomarker becomes publicly available for use in any CDER drug development program for the qualified context of use to support regulatory approval of new drugs [122].
Table 1: FDA Biomarker Qualification Process Stages and Requirements
| Stage | Submission Type | Purpose | FDA Review Timeline | Key Components |
|---|---|---|---|---|
| Stage 1 | Letter of Intent (LOI) | Initial proposal assessment | 3 months (target) | Drug development need, biomarker information, context of use, measurement approach |
| Stage 2 | Qualification Plan (QP) | Detailed development strategy | 6 months (target) | Evidence summary, knowledge gaps, analytical methods, performance characteristics |
| Stage 3 | Full Qualification Package (FQP) | Comprehensive evidence review | 10 months (target) | All accumulated supporting data organized by topic area |
Context of Use: The Foundation of Biomarker Qualification
A critical concept in FDA's biomarker evaluation is Context of Use (COU), defined as the manner and purpose of use for a drug development tool [126]. When FDA qualifies a biomarker, it is specifically qualified for a particular COU, which describes all elements characterizing the purpose and manner of use. The qualified COU defines the boundaries within which available data adequately justify use of the biomarker [126]. This specificity ensures that biomarkers are used appropriately based on their validated performance characteristics and intended application.
The COU statement should comprehensively describe how the biomarker will be applied in drug development, including the specific decisions it will inform, the patient population, the timing of measurement, and the analytical methods used. As additional data are obtained over time, requestors may submit new projects to expand a qualified COU [126].
Biomarker Validation Methodologies and Analytical Considerations
Bioanalytical Method Validation Requirements
The 2025 FDA Bioanalytical Method Validation for Biomarkers Guidance represents the agency's current thinking on biomarker assay validation. This guidance, finalized in January 2025, has generated significant discussion within the bioanalytical community despite its concise length of less than three pages [127]. A fundamental principle in this guidance is that "method validation for biomarker assays should address the same questions as method validation for drug assays" [128].
The guidance identifies several critical analytical parameters that must be validated for biomarker assays, reflecting a continuity from the 2018 BMV guidance while incorporating updated references to international standards. The European Bioanalysis Forum (EBF) has highlighted concerns about the guidance, particularly noting the absence of explicit reference to context of use and the direction to use ICH M10, which explicitly excludes biomarkers from its scope [127]. This creates tension because, while the validation parameters of interest are similar between drug concentration and biomarker assays, the technical approaches must be adapted to demonstrate suitability for measuring endogenous analytes [128].
Table 2: Essential Bioanalytical Validation Parameters for Biomarker Assays
| Validation Parameter | Definition | Considerations for Biomarker Assays |
|---|---|---|
| Accuracy | Closeness of measured value to true value | Challenging for endogenous analytes; may use surrogate matrices or standard addition |
| Precision | Agreement between repeated measurements | Includes within-run and between-run precision; criteria may vary by COU |
| Sensitivity | Lowest measurable concentration | Limit of detection (LOD) and lower limit of quantification (LLOQ) must be established |
| Selectivity | Ability to measure analyte despite interfering substances | Must demonstrate specificity in presence of similar endogenous molecules |
| Parallelism | Proportionality between diluted and undiluted sample | Critical for immunoassays; demonstrates matrix comparability |
| Range | Interval between upper and lower concentration | Must cover expected physiological and pathological levels |
| Reproducibility | Precision under varied conditions | Includes inter-laboratory variability for central labs |
| Stability | Integrity under storage and handling conditions | Includes freeze-thaw, short-term, and long-term stability |
Technical Approaches for Endogenous Biomarkers
A fundamental challenge in biomarker validation lies in the endogenous nature of most biomarkers, which distinguishes them from xenobiotic drugs. This distinction necessitates specialized technical approaches beyond traditional pharmacokinetic validation methods. The 2025 guidance acknowledges that ICH M10 should be a starting point, especially for chromatography and ligand-binding assays, but recognizes it may not be applicable to all biomarker analyses [127].
Four primary technical approaches have emerged for dealing with endogenous compounds in biomarker assays:
- Surrogate Matrix: Using an alternative matrix that lacks the endogenous analyte to prepare calibration standards
- Surrogate Analyte: Using a structurally similar analog that can be distinguished from the endogenous analyte
- Background Subtraction: Measuring baseline levels and subtracting them from post-intervention measurements
- Standard Addition: Adding known quantities of authentic standard to the actual study matrix [127]
These approaches address the fundamental challenge that "biomarker assays must demonstrate suitability for measuring endogenous analytes - a fundamentally different challenge from the spike-recovery approaches used in drug concentration assays" [128]. The guidance emphasizes that parallelism assessments are particularly important when using surrogate matrix and surrogate analyte approaches [127].
Fit-for-Purpose and Context of Use Considerations
A critical concept in biomarker validation is the fit-for-purpose approach, which aligns validation rigor with the intended context of use. While the 2025 guidance doesn't explicitly reference context of use, the bioanalytical community strongly advocates for COU-driven validation strategies [127]. The criteria for accuracy and precision should be closely tied to the specific objectives of biomarker measurement, including factors such as biomarker reference ranges and the magnitude of change relevant to decision-making [127].
This approach recognizes that fixed validation criteria, as applied in drug bioanalysis, may be inappropriate for biomarkers. Instead, validation should be tailored to the specific biomarker investigation and subsequent clinical interpretations. For example, a biomarker intended for diagnostic decisions would require more rigorous validation than one used for exploratory research purposes.
Implementation Challenges and Current Landscape
Program Performance and Qualification Statistics
Despite the established regulatory framework, the Biomarker Qualification Program has demonstrated limited output. Analysis reveals that the FDA has qualified only eight biomarkers through the BQP, with most qualified prior to the December 2016 enactment of the 21st Century Cures Act [123]. The most recent qualification occurred in 2018, indicating a significant slowdown in recent years [123].
Of the qualified biomarkers, four were designed to assess safety, two serve prognostic purposes, and the remaining two are validated for diagnosis and monitoring, respectively [123]. This distribution suggests the program has been comparatively more effective at encouraging development of safety biomarkers, with approximately one-third of accepted biomarker programs focusing on safety assessment [123].
Timeliness and Resource Challenges
Recent analyses characterize the BQP as slow-moving, with review timelines regularly exceeding the FDA's targets. Median times for FDA review of letters of intent and qualification plans are more than double the agency's respective three- and six-month guidance targets [123]. Sponsor development of qualification plans is also protracted, taking a median of more than two-and-a-half years among programs with analyzable timeline data [123].
The complexity of developing certain biomarker types presents additional challenges. Surrogate endpoint biomarkers, which hold significant promise for speeding drug reviews, demonstrate particularly lengthy development timelines. Of the four programs with available data, median development time was nearly four years - 16 months longer than the 31-month median for other programs [123]. This suggests the program may not be well-suited for advancing novel response biomarkers despite their potential significance [123].
Resource constraints represent a significant factor in these challenges. The BQP lacks dedicated funding, with suggestions that linking user fee act resources to FDA divisions participating in qualification plan reviews could address this shortcoming [123]. Additional resources could facilitate more frequent feedback between biomarker developers and the FDA, potentially streamlining the qualification process.
Alternative Pathways for Biomarker Adoption
Given the challenges with the formal qualification pathway, alternative approaches for biomarker adoption have gained prominence. As highlighted by Nicole Gormley, director of the FDA's Division of Hematologic Malignancies II, the FDA can also accept new biomarkers through "collaborative group interactions," citing minimal residual disease in multiple myeloma as an example [123]. This pathway may offer more flexibility and efficiency for certain biomarker types, particularly those with strong evidentiary support from clinical research networks.
Additionally, biomarkers can be validated through the agency's review and approval of specific drug or biological products, where sponsors develop sufficient data to justify use within the context of a particular application [123]. While this approach doesn't provide the broad qualification available through the BQP, it can establish precedent for biomarker use in specific contexts.
Integration with Pharmacogenomics and Personalized Medicine
Pharmacogenomic Biomarkers in Clinical Practice
The integration of pharmacogenomic biomarkers represents a cornerstone of personalized medicine, enabling tailored therapies based on individual genetic profiles. Clinical implementation has demonstrated significant benefits, particularly in psychiatry where a case report highlights the importance of pharmacogenomics in medication-resistant depression [125]. Analysis of cytochrome P450 genes (CYP2D6, CYP2C19, CYP1A2) in a patient with treatment-resistant depression revealed specific variations that explained poor medication response and adverse effects, leading to optimized treatment when the genetic information was applied [125].
Several international consortia and databases support the clinical implementation of pharmacogenomics, including:
- Clinical Pharmacogenetics Implementation Consortium (CPIC): Creates freely available, evidence-based pharmacogenetic prescribing guidelines
- Pharmacogenomics Knowledgebase (PharmGKB): Curates knowledge about the impact of genetic variation on drug response
- Dutch Pharmacogenetics Working Group (DPWG): Develops pharmacogenetics-based prescribing guidelines [125]
These resources have addressed initial implementation barriers by standardizing terminology, establishing processes for translating genotype to phenotype to therapeutic guidance, and reaching evidentiary thresholds for implementation [9].
Addressing Diversity and Equity in Biomarker Development
A significant challenge in pharmacogenomic biomarker development involves the lack of diversity, equity, and inclusion in biomedical research. Underrepresentation of diverse populations in pharmacogenetics research weakens the evidence for clinical validity and utility, potentially introducing healthcare disparities [9]. The case of warfarin pharmacogenomics illustrates this problem, where discrepant results between self-identified Black and non-Black participants in the Clarification of Optimal Anticoagulation through Genetics (COAG) trial were partly attributable to a dosing algorithm that didn't include alleles more common in individuals with sub-Saharan African ancestry [9].
Potential solutions to address these disparities include:
- Increasing genetic diversity among study populations in pharmacogenetics research
- Implementing pan-ethnic pharmacogenomic testing
- Establishing financing mechanisms to support testing in marginalized communities
- Better integrating patient views and values regarding pharmacogenetic testing into medical care [9]
Initiatives like the All of Us Research Program, which has enrolled nearly a million participants with majority representation from groups traditionally underrepresented in biomedical research, represent significant steps toward addressing these disparities [9].
Regulatory Considerations for Pharmacogenomic Biomarkers
The qualification of pharmacogenomic biomarkers presents unique regulatory considerations, particularly regarding evidence standards and clinical utility assessment. While CPIC guidelines have made substantial progress in standardizing clinical implementation approaches, regulatory acceptance for qualified context of use requires additional evidence generation [9]. The FDA's Table of Pharmacogenetic Associations provides one mechanism for recognizing pharmacogenetic relationships in drug labeling, though the evidence needed to modify this table continues to evolve [9].
The regulatory landscape for laboratory-developed tests (LDTs) performing pharmacogenomic testing also impacts implementation. Ensuring clear regulatory requirements and providing resources to navigate these requirements supports laboratories in implementing quality pharmacogenomic testing [9]. Consistency in regulatory oversight helps maintain test quality while encouraging innovation in this rapidly advancing field.
Experimental Protocols and Research Applications
Biomarker Validation Workflow
The validation of biomarkers follows a systematic workflow that progresses from assay development through full validation, with iterative refinement based on context of use requirements. The following diagram illustrates the key stages in this process:
Biomarker Validation Workflow
This workflow emphasizes the foundational importance of defining context of use before initiating assay development, as this determines the specific validation requirements and acceptance criteria. The process involves iterative refinement, with pilot validation informing necessary adjustments before committing to full method validation.
Biomarker Qualification Pathway
The formal FDA qualification process involves specific stages with defined objectives and decision points, as illustrated in the following diagram:
FDA Qualification Pathway
This pathway illustrates the sequential nature of the qualification process, with decision points at each stage determining whether development can proceed. The diagram highlights the target review timelines established by FDA, though actual review times often exceed these targets [123].
Essential Research Reagents and Tools
Table 3: Essential Research Reagent Solutions for Biomarker Validation
| Reagent/Tool Category | Specific Examples | Function in Biomarker Validation |
|---|---|---|
| Reference Standards | Certified reference materials, synthetic biomarkers | Establish calibration curves, determine accuracy, prepare quality controls |
| Assay Kits | Commercial ELISA kits, PCR assays, sequencing panels | Provide standardized components for specific biomarker measurements |
| Quality Controls | Pooled biological samples, commercial QC materials | Monitor assay performance over time, assess inter-day precision |
| Matrix Components | Charcoal-stripped serum, artificial cerebrospinal fluid | Serve as surrogate matrices for endogenous analyte quantification |
| Analytical Instruments | LC-MS/MS systems, plate readers, flow cytometers | Enable precise quantification of biomarker concentrations |
| Data Analysis Software | Method validation software, statistical packages | Support calculation of validation parameters, statistical analysis |
Evolving Regulatory Landscape
The regulatory landscape for biomarker validation continues to evolve, with the 2025 FDA Bioanalytical Method Validation guidance representing both continuity and change from previous approaches. While maintaining fundamental principles from the 2018 guidance, the 2025 update references ICH M10, representing harmonization with international standards despite M10's explicit exclusion of biomarkers from its scope [128] [127]. This evolution reflects ongoing efforts to balance scientific rigor with practical considerations for biomarker validation.
Stakeholders have advocated for greater recognition of context of use in validation approaches, with the European Bioanalysis Forum highlighting this as a critical consideration missing from the 2025 guidance [127]. Future revisions may incorporate more explicit COU-driven validation strategies that recognize the varying evidence needs for different biomarker applications.
Advancing Personalized Medicine Through Biomarker Qualification
Despite current challenges with the qualification program, biomarkers remain essential tools for advancing personalized medicine. The integration of pharmacogenomic biomarkers into clinical practice demonstrates the significant potential of validated biomarkers to improve treatment outcomes, particularly in complex conditions like medication-resistant depression [125]. As biomarker science advances, strengthening the qualification pathway through additional resources, streamlined processes, and greater stakeholder engagement will be essential for realizing the full potential of personalized medicine.
The future of biomarker development will likely involve greater emphasis on diverse population representation, novel analytical approaches for complex biomarkers, and integration of real-world evidence to support qualification. Addressing these priorities will enhance the regulatory framework's ability to support innovation while ensuring biomarkers used in drug development and clinical practice meet rigorous standards for reliability and clinical utility.
The European Partnership for Personalised Medicine (EP PerMed) is a pivotal transnational platform for joint programming of national and European regional research and innovation programmes, established to implement the "Strategic Research & Innovation Agenda (SRIA) for Personalised Medicine" through dedicated funding initiatives [129]. Supported by the European Union under Horizon Europe (Grant Agreement N° 101137129), EP PerMed represents a coordinated European response to advance personalized medicine (PM) by aligning strategies, pooling resources, and achieving investments of scale across national boundaries [22] [129]. This partnership is strategically designed to accelerate the implementation of personalized healthcare approaches into clinical practice for the benefit of patients and society, thereby enhancing Europe's competitiveness in this rapidly evolving field [130] [129].
EP PerMed defines personalized medicine as "a medical model using characterisation of individuals' phenotypes and genotypes (e.g. molecular profiling, medical imaging, lifestyle data) for tailoring the right therapeutic strategy for the right person at the right time, and/or to determine the predisposition to disease and/or to deliver timely and targeted prevention" [129]. This definition underscores the comprehensive nature of PM, moving beyond traditional "one-size-fits-all" approaches to optimize prevention, diagnosis, and treatment strategies based on each individual's unique characteristics [129]. Within this framework, pharmacogenomics (PGx) has emerged as a critical disciplinary pillar, investigating how genetic variations influence interindividual differences in drug metabolism, efficacy, and safety to enable more precise therapeutic interventions [131].
The JTC2025 Initiative: Scope, Objectives, and Specifications
The EP PerMed Joint Transnational Call 2025 (JTC2025) represents the partnership's second major funding initiative, specifically targeting "Pharmacogenomic strategies for personalised medicine approaches (PGxPM2025)" [132] [130]. This call mobilizes substantial resources with 35 funding organizations across 24 countries participating and an available budget exceeding €36.5 million to support multinational research consortia [132] [130]. The call operates through a two-stage application process with clearly defined deadlines and an expected project start date at the end of 2025 or beginning of 2026 [132].
The JTC2025 establishes three primary research objectives aimed at advancing pharmacogenomic strategies for personalized medicine. First, it supports projects focused on identifying novel pharmacogenomic markers or signatures using multi-omics data in relation to drugs or drug combinations. Second, it funds research validating pharmacogenomic markers or signatures for predicting drug outcomes. Third, it encourages projects utilizing pharmaco-omics strategies to determine optimal dosage, treatment efficacy, and risks of adverse drug responses or non-response to tailor personalized treatment pathways, including combined treatments [132] [133]. These objectives collectively address critical gaps in translating pharmacogenomic discoveries into clinically actionable strategies.
Table 1: Key Timeline and Structural Details of JTC2025
| Parameter | Specification |
|---|---|
| Call Title | Pharmacogenomic Strategies for Personalised Medicine Approaches (PGxPM2025) |
| Funding Organizations | 35 funding bodies across 24 countries and 10 European regions [132] |
| Total Budget | > €36.5 million [132] [130] |
| Application Process | Two-stage (pre-proposal and full-proposal) [132] |
| Pre-proposal Deadline | 18 February 2025 (14:00 CET) [132] |
| Full-proposal Deadline | 17 June 2025 (14:00 CEST) [132] |
| Project Start | End of 2025/beginning of 2026 [132] |
Research Scope and Eligibility Requirements
The JTC2025 welcomes research projects across all disease areas, emphasizing interdisciplinary and cross-sectoral collaborations [132] [22]. The call specifically encourages research that addresses pharmacogenomic strategies for personalized medicine through several approaches, including the identification of new pharmacogenomic markers or signatures using multi-omics data, validation of existing markers for predicting drug outcomes, and the application of pharmaco-omics to determine optimal dosage, efficacy, and adverse drug response risks [133]. A distinctive feature of this call is its strong emphasis on participatory research approaches, requiring the active involvement of patients or citizens as integral members of research teams [22].
Eligibility criteria for JTC2025 consortium composition follow specific rules to ensure transnational representation and balanced participation. Consortia must include at least three partners eligible for funding from three different EU Member States or Associated Countries whose funding organizations participate in the call [132]. The consortium composition rules limit the number of partners with own funding and per country, with specific allowances for patient/citizen representing organizations, which are excluded from these calculations and can be added as additional partners [132]. This structure ensures genuine multinational collaboration while maintaining manageable consortium sizes.
Table 2: Consortium Composition Rules for JTC2025 Applications
| Number of Partners in Proposal | 3 | 4 | 5 | 6 | 7 | +1 (Widening) |
|---|---|---|---|---|---|---|
| Maximum Partners with Own Funding | 0 | 1 | 1 | 1 | 1 | 1 |
| Maximum Partners per Country | 1 | 2 | 2 | 2 | 3 | 3 (for 8 partners) |
Methodological Frameworks for PGx Research
Experimental Design and Workflow Considerations
Robust pharmacogenomic research requires meticulously planned experimental designs that incorporate appropriate controls, validation steps, and statistical considerations. For JTC2025-related projects, researchers should develop workflows that integrate genomic discovery with functional validation and clinical translation. The African American Cardiovascular Pharmacogenetic Consortium (ACCOuNT) provides an exemplary model for PGx study design, particularly for addressing diversity gaps in pharmacogenomic research [134]. Their approach includes prospective cohort recruitment with precise inclusion/exclusion criteria, genome-wide genotyping, transcriptome analysis, and integration of social and demographic factors that may influence drug response independently of genetics [134].
For JTC2025 applications, research proposals should incorporate multi-omics data integration, combining genomic, transcriptomic, and other molecular profiling data to identify and validate pharmacogenomic markers [132] [133]. The experimental design should include appropriate sample size calculations with power considerations, especially for discovering novel variants in diverse populations. Additionally, protocols should address specific technical considerations such as correction for population substructure in genetic analyses, replication cohorts for validating discoveries, and functional validation experiments using in vitro or model systems to establish biological mechanisms [134].
Implementation Science and ELSA Components
Beyond basic discovery research, JTC2025 emphasizes the importance of implementation science and Ethical, Legal, and Social Aspects (ELSA) research integrated into pharmacogenomic studies [22]. Successful proposals should include plans for assessing barriers to clinical implementation, developing strategies for integrating pharmacogenomic testing into healthcare systems, and evaluating health economic implications. This translational focus aligns with CPIC's mission of facilitating the clinical implementation of pharmacogenetic tests by creating freely available, evidence-based clinical practice guidelines [115]. Research proposals should therefore consider not only discovery but also the pathway to clinical adoption, including the development of clinical decision support tools, provider education strategies, and assessment of patient perspectives on pharmacogenomic testing.
Core Pharmacogenomic Databases and Consortia
The pharmacogenomics research landscape is supported by several key resources that provide critical infrastructure for data analysis, interpretation, and clinical translation. These resources have become indispensable for researchers in the field, offering curated knowledge, standardized nomenclature, and implementation guidelines.
Table 3: Essential Resources for Pharmacogenomic Research
| Resource | Primary Function | Key Features | Relevance to JTC2025 |
|---|---|---|---|
| PharmGKB [135] | Knowledge Resource | Curates gene-drug-disease relationships; drug labels with PGx info; clinical guidelines | Literature evidence for proposals; annotation of variants |
| PharmVar [135] | Variation Repository | Central repository for pharmacogene variation; star allele nomenclature | Standardized variant definitions for research reporting |
| CPIC [115] | Clinical Implementation | Evidence-based guidelines; translating genetic test results to prescribing decisions | Supporting implementation research components |
| PGRN Oncology Database [135] | Collaboration Tool | Information on available cancer pharmacogenomics cohorts | Fostering collaborations; cohort discovery |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful pharmacogenomic research requires access to well-characterized biological samples, specialized reagents, and analytical tools. The following table outlines essential materials and their applications in PGx research, particularly relevant for JTC2025 proposals.
Table 4: Essential Research Reagents and Materials for PGx Studies
| Reagent/Material | Function/Application | Specifications | Example Use Cases |
|---|---|---|---|
| DNA/RNA Extraction Kits | Nucleic acid purification from whole blood, tissues, or cells | High-quality, PCR-ready materials; preservation of RNA integrity | Genotyping arrays; whole-genome sequencing; transcriptome analysis [134] |
| Genotyping Arrays | Genome-wide variant profiling | Population-inclusive content; imputation quality | Discovery of novel population-specific variants [134] |
| Whole Genome Sequencing Kits | Comprehensive variant discovery | Adequate coverage (>30x); structural variant detection | Identifying novel pharmacogenomic variants beyond array data [134] |
| RNA-Sequencing Library Prep Kits | Transcriptome analysis | Strand-specific; low input capability | Expression quantitative trait loci (eQTL) studies; splice variant analysis [134] |
| iPSC Generation Systems | Cellular model development | Reprogramming efficiency; differentiation protocols | Functional validation of variants in relevant cell types [134] |
| PCR Reagents & Probes | Targeted genotyping; validation | TaqMan assays; digital PCR for rare variants | Validation of discovered variants in replication cohorts |
| Clinical Phenotyping Forms | Standardized data collection | ISTH criteria for bleeding; standard toxicity grading | Consistent phenotype assessment across transnational cohorts [134] |
Participating Countries and Funding Structures
The JTC2025 call represents an extensive collaboration across European and international boundaries. The participating countries include 24 nations: Austria, Belgium, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Latvia, Lithuania, Luxembourg, Norway, Poland, Portugal, South Africa, Spain, Sweden, and Turkiye [132]. Additionally, 10 European regions are participating independently: Flanders (Belgium), Wallonia-Brussels Federation (Belgium), Saxony (Germany), Lombardy (Italy), Tuscany (Italy), Azores (Portugal), Centro Region (Portugal), Andalusia (Spain), Catalonia (Spain), and Navarre (Spain) [132]. This multi-layered participation structure enables research consortia to form diverse partnerships that leverage regional strengths and address specific population needs.
The funding mechanism for JTC2025 follows a distributed model where individual research groups are funded by their respective regional or national EP PerMed funding organization rather than through a central funding body [22]. This structure means that applications must satisfy both the transnational eligibility criteria and the specific requirements of each participating funding organization. Applicants are strongly advised to contact their national representatives early in the application process to confirm eligibility and understand any additional submission requirements [132]. Several countries, including Italy, Portugal, South Africa, and Israel, have specific pre-eligibility check procedures and additional documentation that must be completed before or in parallel with the main application submission [132].
The EP PerMed JTC2025 initiative represents a significant strategic investment in advancing pharmacogenomics as a cornerstone of personalized medicine in Europe and beyond. By funding transnational consortia that integrate academic, clinical, and private sector research teams, the call aims to accelerate the discovery and validation of pharmacogenomic markers and their translation into clinical practice. The emphasis on interdisciplinary approaches, including ELSA research, health economics, and implementation science, recognizes the multifaceted challenges inherent in adopting personalized medicine approaches in healthcare systems.
For researchers and drug development professionals, successful participation in this initiative requires not only scientific excellence but also careful attention to consortium building, alignment with national funding priorities, and integration of patient perspectives. The future of pharmacogenomics will increasingly depend on such collaborative models that leverage diverse expertise, populations, and resources to realize the promise of truly personalized therapeutic strategies. As these initiatives evolve, they will likely place greater emphasis on artificial intelligence approaches for analyzing complex multi-omics data, expanding diversity in pharmacogenomic research to include underrepresented populations, and developing more efficient implementation pathways to bridge the gap between discovery and clinical application [131].
Conclusion
Pharmacogenomics represents a paradigm shift in drug development and clinical practice, moving from population-based to genetically-guided individualized therapy. The integration of germline and somatic genomic data enables prediction of drug efficacy and toxicity, particularly in oncology and high-risk medications. However, widespread implementation requires addressing economic barriers, developing robust health information technologies, and establishing global regulatory harmonization. Future directions must focus on validating rare genetic variants, expanding diverse population representation in research, developing complex biomarker signatures, and creating sustainable implementation models. The ongoing multinational research initiatives and evolving regulatory frameworks provide a strong foundation for realizing the full potential of pharmacogenomics in creating safer, more effective personalized treatment paradigms across therapeutic areas.
References
- 1. Pharmacogenomics in drug therapy: global regulatory ... [https://www.nature.com/articles/s41431-025-01950-6]
- 2. AAN 2025: Precision Medicine and Pharmacogenomics in ... [https://www.pharmacytimes.com/view/aan-2025-precision-medicine-and-pharmacogenomics-in-neurological-care]
- 3. Pharmacogenomics Overview - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK617055/]
- 4. The Slow and Winding Path to Pharmacogenomic Test ... [https://www.insideprecisionmedicine.com/topics/precision-medicine/the-slow-and-winding-path-to-pharmacogenomic-test-adoption/]
- 5. Dynamic star allele definitions in Pharmacogenomics [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1584658/full]
- 6. Pharmacogenomic test report nomenclature & terminology [https://www.jax.org/education-and-learning/clinical-and-continuing-education/clinical-topics/genetic-testing/pgx-report]
- 7. Navigating Pharmacogenomic Testing in Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355021/]
- 8. Pharmacogenomic Testing 2025-07-26 [for Anthem BCBS ... [https://guidelines.carelonmedicalbenefitsmanagement.com/pharmacogenomic-testing-2025-07-26/]
- 9. Progress in Pharmacogenomics Implementation in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439016/]
- 10. Five Key Advances Shaping Pharmacogenomics [https://www.technologynetworks.com/tn/lists/five-key-advances-shaping-pharmacogenomics-405156]
- 11. Role of Pharmacogenomic Biomarkers In Predicting and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3828931/]
- 12. Pharmacogenomics: mechanisms of action [https://www.genomicseducation.hee.nhs.uk/blog/pharmacogenomics-mechanisms-of-action/]
- 13. Pharmacogenomics: How Genetics Can Optimize Your ... [https://www.veritasint.com/blog/en/pharmacogenomics-how-genetics-can-optimize-your-treatment/]
- 14. Table of Pharmacogenomic Biomarkers in Drug Labeling [https://www.fda.gov/drugs/science-and-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling]
- 15. Frequencies of clinically important CYP2C19 and CYP2D6 ... [https://www.nature.com/articles/s41431-019-0480-8]
- 16. CYP2C19 and CYP2D6 Genotypes and Metabolizer Status ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9321582/]
- 17. Transporter Genes - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/transporter-genes]
- 18. Pharmacogenetics of Membrane Transporters - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6388404/]
- 19. Influence of Transporter Polymorphisms on Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6348109/]
- 20. very important pharmacogene information for ABCG2 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5788016/]
- 21. Variation and evolution of the ABC transporter genes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7372709/]
- 22. EP PerMed JTC2025 Pre-announcement [https://www.eppermed.eu/news-events/news/ep-permed-jtc2025-pre-announcement-pharmacogenomic-strategies-for-personalised-medicine-pgxpm2025/]
- 23. The Role and Impact of Pharmacogenomics in Advancing ... [https://www.icpermed.eu/news/the-role-and-impact-of-pharmacogenomics-in-advancing-personalised-medicine-in-iran/]
- 24. Pharmacogenomics in practice: a review and implementation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10233068/]
- 25. History of The Gene Interactive | The Gene | Ken Burns [https://www.pbs.org/kenburns/the-gene/history-of-the-gene]
- 26. History of genetics [https://en.wikipedia.org/wiki/History_of_genetics]
- 27. History of genomics timeline from 1871 to present day [https://www.yourgenome.org/theme/timeline-history-of-genomics/]
- 28. NHGRI History and Timeline of Events [https://www.genome.gov/about-nhgri/Brief-History-Timeline]
- 29. Transforming Pharmacovigilance With Pharmacogenomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598900/]
- 30. Emerging strategies to bridge the gap between ... [https://www.nature.com/articles/s41525-020-0119-2]
- 31. A Network of SLC and ABC Transporter and DME Genes ... [https://www.nature.com/articles/s41598-019-47798-x]
- 32. Integrating rare genetic variants into pharmacogenetic drug response... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-018-0157-3]
- 33. Contrastive sequence signatures between the both sides of a ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11620-y]
- 34. Biomarkers for Improved Drug Therapy—Recent... Pharmacogenomic [https://link.springer.com/article/10.1208/s12248-017-0161-x]
- 35. Polymorphisms of ADME-related genes and their ... [https://www.nature.com/articles/s41598-019-43610-y]
- 36. African variation at Cytochrome P450 genes - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3868406/]
- 37. (PDF) Pharmacogenomic Profiling of ADME Variants: Current... Gene [https://www.academia.edu/52085823/Pharmacogenomic_Profiling_of_ADME_Gene_Variants_Current_Challenges_and_Validation_Perspectives]
- 38. ADME Gene-Related Pharmacogenomic Labeling of FDA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10972161/]
- 39. Germline and Somatic Variants: What Is the Difference? [https://www.ons.org/publications-research/voice/news-views/01-2020/germline-and-somatic-variants-what-difference]
- 40. The germline genetic component of drug sensitivity in ... [https://www.nature.com/articles/s41467-018-05811-3]
- 41. Predicting Drug Response and Synergy Using a Deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7737474/]
- 42. Germline vs Somatic Testing; Genomic vs Genetic Testing [https://ocrahope.org/news/germline-vs-somatic-testing-genomic-vs-genetic-testing/]
- 43. Pharmacogenomics: Driving Personalized Medicine [https://www.sciencedirect.com/science/article/abs/pii/S0031699724007798]
- 44. Predicting tumor response to drugs based on gene ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-021-07581-7]
- 45. Discrepancies Between Somatic and Germline Results in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12132614/]
- 46. Pharmacogenomics: Driving Personalized Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10289244/]
- 47. Advances in Precision Oncology: From Molecular Profiling to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607717/]
- 48. Foundation Medicine Spotlights Scientific Achievements ... [https://www.foundationmedicine.com/press-release/esmo-2025]
- 49. Toward a Unified Graph-Based Representation of Medical ... [https://arxiv.org/abs/2410.14739]
- 50. Building a knowledge graph to enable precision medicine [https://www.nature.com/articles/s41597-023-01960-3]
- 51. 2025 Cell and Gene Therapy Report Looks at Industry ... [https://www.targetedonc.com/view/2025-cell-and-gene-therapy-report-looks-at-industry-challenges-how-to-expand-nationally]
- 52. Pharmacogenomics: An evolving clinical tool for precision ... [https://www.ccjm.org/content/87/2/91]
- 53. Using pharmacogenomics to personalise drug therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12187479/]
- 54. Warfarin: a case history in pharmacogenetics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1768901/]
- 55. Warfarin pharmacogenetic trials: is there a future for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4110075/]
- 56. Pharmacogenetics of thiopurines - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8992634/]
- 57. The Role of Pharmacogenetics in the Therapeutic ... [https://www.mdpi.com/2077-0383/12/21/6742]
- 58. The case for pharmacogenetics-guided prescribing of codeine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8168366/]
- 59. The Role of Pharmacogenomics in Opioid Prescribing [https://link.springer.com/article/10.1007/s11864-022-01010-x]
- 60. a reality for future health care | The Pharmacogenomics ... [https://www.nature.com/articles/s41397-024-00326-1]
- 61. PREEMPTIVE PHARMACOGENETIC TESTING [https://pmc.ncbi.nlm.nih.gov/articles/PMC5920773/]
- 62. Pharmacogenetics Clinical Decision Support Systems for ... [https://www.jmir.org/2024/1/e49230/]
- 63. Implementation of preemptive DNA sequence–based ... [https://www.sciencedirect.com/science/article/pii/S1098360022000387]
- 64. Preemptive pharmacogenomics [https://www.thermofisher.com/us/en/home/products-and-services/promotions/pgx-how.html]
- 65. a cost-utility analysis | The Pharmacogenomics Journal [https://www.nature.com/articles/s41397-022-00275-7]
- 66. Pharmacogenomic Clinical Decision Support: A Review, How ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9291515/]
- 67. HLA-B*58:01 and Risk of Allopurinol-Induced Severe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12573116/]
- 68. A Comprehensive Review of HLA and Severe Cutaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8622011/]
- 69. Pharmacogenomics of severe cutaneous adverse ... [https://www.nature.com/articles/jhg201337]
- 70. HLA-B*58:01 genotyping prevalence and the association ... [https://www.nature.com/articles/s41598-025-16062-w]
- 71. Risk and Association of Specific HLA Alleles With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477543/]
- 72. Pharmacogenetics: An Important Part of Drug Development ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7255432/]
- 73. of Pharmacogenetic Cost for Drugs with... Effectiveness Testing [https://pmc.ncbi.nlm.nih.gov/articles/PMC9828439/]
- 74. Implementing health economics for pharmacogenomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181413/]
- 75. Clinical and economic outcomes of a pharmacogenomics ... [https://www.nature.com/articles/s41397-024-00350-1]
- 76. The Pharmacogenomics Technology Market [https://americanpharmacogenomicsassociation.com/business/the-pharmacogenomics-technology-market-trends-insights-and-opportunities/]
- 77. Pharmacogenomics Market Size and Growth 2025 to 2034 [https://www.novaoneadvisor.com/report/pharmacogenomics-market]
- 78. Systematic review of the evidence on the cost-effectiveness ... [https://www.sciencedirect.com/science/article/pii/S1098360021012387]
- 79. - Cost of pharmacogenetic-guided treatment: are we... effectiveness [https://www.nature.com/articles/tpj201721?error=cookies_not_supported&code=cccd0122-240c-4a13-9ae0-4d87723b9c33]
- 80. Cost-effectiveness of Pharmacogenomic Testing [https://blogs.cdc.gov/genomics/2023/05/08/cost-effectiveness/]
- 81. Frontiers | Implementing pharmacogenetic testing in community... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1659875/full]
- 82. The Genotype-to-Phenotype Dilemma: How Should ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8316082/]
- 83. the evolution in our understanding HIV-1 drug resistance [https://www.natap.org/2003/april/042203_1.htm]
- 84. Pharmacogenomic Testing: Clinical Evidence and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6789586/]
- 85. Implementing a Pharmacogenomics Program [https://clpmag.com/diagnostic-technologies/molecular-diagnostics/implementing-pharmacogenomics-program/]
- 86. Clinical pharmacogenomic testing and reporting [https://www.sciencedirect.com/science/article/pii/S109836002105468X]
- 87. Phenotype-genotype discordance and disorders of sexual ... [https://www.probiologists.com/article/phenotype-genotype-discordance-and-disorders-of-sexual-differentiation]
- 88. Barrier Erosion and Remaining Challenges [https://pubmed.ncbi.nlm.nih.gov/40468601/]
- 89. Genomic Data Standards [https://docs.terraref.org/technical-documentation/data-standards/genomic-data-standards]
- 90. Sequence Analysis - Site Guide - NCBI - NIH [https://www.ncbi.nlm.nih.gov/guide/sequence-analysis/]
- 91. New algorithm enables fast 'gold-standard' search of the ... [https://www.nature.com/articles/s41587-025-02939-8]
- 92. Artificial intelligence, medications, pharmacogenomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11703462/]
- 93. Multimodal Integration in Health Care: Development With ... [https://www.jmir.org/2025/1/e76557]
- 94. Genomics unleashed: Informatics integration at the heart of ... [https://www.illumina.com/content/illumina-marketing/amr/en_US/events/webinar/2025/genomics-unleashed-informatics-integration-heart-healthcare.html]
- 95. Ethical, Legal and Social Implications Research Program [https://www.genome.gov/Funded-Programs-Projects/ELSI-Research-Program-ethical-legal-social-implications]
- 96. Pharmacogenomic Testing (PGx) in Psychiatric Care: ... [https://elsihub.org/video/elsiconversations-pharmacogenomic-testing-pgx-psychiatric-care-exploring-ethical-and-0]
- 97. Frequencies of pharmacogenomic alleles across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10577080/]
- 98. Genetic ancestry in population pharmacogenomics ... [https://www.sciencedirect.com/science/article/pii/S2589004224021412]
- 99. Analysis of population-specific pharmacogenomic variants ... [https://www.nature.com/articles/s41598-017-08468-y]
- 100. Advancing Pharmacogenomics from Single-Gene to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9483991/]
- 101. Economic evaluation of a pharmacogenomic multi-gene ... [https://pubmed.ncbi.nlm.nih.gov/30280614/]
- 102. How Much Does a Pharmacogenomics Test Cost? What ... [https://americanpharmacogenomicsassociation.com/education/how-much-does-a-pharmacogenomics-test-cost-what-you-need-to-know-before-you-pay/]
- 103. The landscape of pharmacogenetic testing in a US ... [https://www.nature.com/articles/s41436-020-0788-3]
- 104. In-Depth Look at the Differences Between EMA and FDA [https://www.mabion.eu/science-hub/articles/similar-but-not-the-same-an-in-depth-look-at-the-differences-between-ema-and-fda/]
- 105. Multidisciplinary: pharmacogenomics [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/multidisciplinary-guidelines/multidisciplinary-pharmacogenomics]
- 106. Evaluation of Current Regulation and Guidelines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7232863/]
- 107. Pharmacogenomic Data Submissions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/pharmacogenomic-data-submissions]
- 108. Pharmacogenomic Data Submissions March 2023 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/pharmacogenomic-data-submissions-0]
- 109. Table of Pharmacogenetic Associations [https://www.fda.gov/medical-devices/precision-medicine/table-pharmacogenetic-associations]
- 110. Pharmacogenetic Implementation Studies—Lessons Learned ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439011/]
- 111. Pharmacogenetics in randomized controlled trials [https://pubmed.ncbi.nlm.nih.gov/22008051/]
- 112. Pharmacogenomics in clinical trials: an overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10625420/]
- 113. Impact of pharmacogenomics on clinical outcomes in major ... [https://www.sciencedirect.com/science/article/pii/S0022395618310069]
- 114. An Evidenceâ€Based Framework for Evaluating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8457105/]
- 115. CPIC [https://cpicpgx.org/]
- 116. Advancing Clinical Pharmacogenomics Worldwide Through ... [https://pubmed.ncbi.nlm.nih.gov/40678821/]
- 117. Guidelines [https://cpicpgx.org/guidelines/]
- 118. Genes-Drugs [https://cpicpgx.org/genes-drugs/]
- 119. Standardizing terms for clinical pharmacogenetic test results [https://pmc.ncbi.nlm.nih.gov/articles/PMC5253119/]
- 120. Term Standardization for Clinical Pharmacogenetic Test ... [https://cpicpgx.org/resources/term-standardization-for-clinical-pharmacogenetic-test-results-part-2/]
- 121. The Clinical Pharmacogenetics Implementation ... [https://www.sciencedirect.com/science/article/abs/pii/S0002929725003957]
- 122. About Biomarkers and Qualification [https://www.fda.gov/drugs/biomarker-qualification-program/about-biomarkers-and-qualification]
- 123. AgencyIQ – Sluggish biomarker program offers FDA ... [https://friendsofcancerresearch.org/news/agencyiq-sluggish-biomarker-program-offers-fda-opportunity-for-reform/]
- 124. Biomarker Qualification Program [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/biomarker-qualification-program]
- 125. Case Report: Pharmacogenomics in clinical practice [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1587875/full]
- 126. Drug Development Tool (DDT) Qualification Programs [https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tool-ddt-qualification-programs]
- 127. FDA Guidance for Industry on Bioanalytical Method ... [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 128. The 2025 FDA Biomarker Guidance: Understanding ... [https://www.linkedin.com/pulse/2025-fda-biomarker-guidance-understanding-lxoke]
- 129. EP PerMed Joint Transnational Call (JTC) 2025 [https://www.eppermed.eu/funding-projects/calls/joint-transnational-calls/]
- 130. Pharmacogenomic strategies for personalised medicine ... [https://www.researchireland.ie/funding/pharmacogenomic-strategies/]
- 131. The Role of Pharmacology, Genomics, and AI in Improving ... [https://pubmed.ncbi.nlm.nih.gov/40285487/]
- 132. EP PerMed Joint Transnational Call (JTC) 2025 [https://www.eppermed.eu/funding-projects/calls/jtc2025/]
- 133. EP PerMed: Pharmacogenomic Strategies for Personalised ... [https://www.innovationsfonden.dk/en/p/international-collaborations/ep-permed-pharmacogenomic]
- 134. The ACCOuNT Consortium: A Model for the Discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6510376/]
- 135. PGx Resources [https://www.pgrn.org/pgrn-resources]