Validating Analytical Methods for Drug Stability: A Guide to ICH Q2(R2) and the 2025 Q1 Framework
This article provides a comprehensive guide for researchers and drug development professionals on validating analytical methods for drug stability testing within the modern ICH regulatory landscape.
Validating Analytical Methods for Drug Stability: A Guide to ICH Q2(R2) and the 2025 Q1 Framework
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on validating analytical methods for drug stability testing within the modern ICH regulatory landscape. It covers the foundational principles of the newly consolidated ICH Q1 (2025 Draft) guideline and the updated ICH Q2(R2) on analytical method validation. The scope extends from core concepts and methodological applications to troubleshooting common challenges and implementing a lifecycle approach for robust, compliant stability programs, including advanced therapy medicinal products (ATMPs) and complex biologics.
The New Foundation: Understanding the 2025 ICH Q1 Consolidation and Its Impact on Analytical Validation
The International Council for Harmonisation (ICH) has undertaken a monumental step to modernize and consolidate the foundational guidelines governing the stability testing of pharmaceuticals. The new ICH Q1 Draft Guideline, which reached Step 2b of the ICH process in April 2025, represents a comprehensive revision that unifies the previously fragmented ICH Q1A-F and Q5C guidelines into a single, cohesive document [1] [2] [3]. This consolidation marks a significant shift from a series of documents developed incrementally since 1993 to a modernized, unified framework that reflects current scientific and regulatory practices [3]. The draft guideline outlines stability data expectations for drug substances and drug products, providing evidence on how their quality varies over time under the influence of environmental factors like temperature, humidity, and light [1].
The revision aims to address the evolving landscape of pharmaceutical development, which now includes complex biological products and advanced therapies that were not adequately covered in the original guidelines [4]. By promoting a more consistent, science- and risk-based approach to stability testing, the ICH seeks to harmonize regulatory expectations across global markets and provide a clearer, more adaptable framework that supports efficient drug development and robust product quality throughout the lifecycle [2] [3]. This article examines how the 2025 draft replaces the previous collection of guidelines, the implications for analytical method validation, and the new opportunities it presents for researchers and drug development professionals.
From Multiple Documents to One: The Scope of unification
The 2025 ICH Q1 draft guideline represents a significant consolidation of seven previously separate stability guidelines into a single comprehensive document. This unification simplifies the regulatory landscape for pharmaceutical scientists and establishes a coherent framework for stability testing across diverse product types.
The Pre-2025 Fragmented Landscape
Before this consolidation, stability testing requirements were spread across multiple documents, each addressing specific aspects:
- ICH Q1A(R2): Provided the core stability data package for new drug substances and products [5] [4].
- ICH Q1B: Focused specifically on photostability testing requirements [4].
- ICH Q1C: Addressed stability testing for new dosage forms [4].
- ICH Q1D: Covered bracketing and matrixing designs to reduce stability testing burden [4].
- ICH Q1E: Offered guidance on evaluation of stability data [4].
- ICH Q1F: Provided stability data requirements for new regions (now withdrawn) [2].
- ICH Q5C: Covered stability testing of biotechnological/biological products [4] [3].
This fragmented approach often led to challenges in interpretation and implementation, particularly for complex products that fell under multiple guidelines simultaneously [3].
The Unified 2025 Framework
The new draft guideline supersedes all aforementioned documents, creating a single source for stability testing requirements [1] [4]. The consolidated structure comprises 18 main sections and 3 annexes, organized to address both foundational stability principles and specialized needs of emerging product types [3]. This modular approach allows for more consistent application across synthetic molecules, biologics, and advanced therapy medicinal products (ATMPs) [2] [6].
Table: Direct Replacement Mapping of ICH Guidelines
| Previous Guideline | Primary Focus | Status in 2025 Draft |
|---|---|---|
| ICH Q1A(R2) | Stability testing of new drug substances & products | Fully incorporated and expanded |
| ICH Q1B | Photostability testing | Integrated into main document |
| ICH Q1C | Stability testing for new dosage forms | Incorporated with expanded scope |
| ICH Q1D | Bracketing and matrixing designs | Enhanced and included as Annex 1 |
| ICH Q1E | Evaluation of stability data | Integrated with new statistical guidance |
| ICH Q1F | Stability data for new regions | Withdrawn; global zones now included |
| ICH Q5C | Stability of biotechnological products | Fully integrated into main framework |
The unification specifically extends the scope to include synthetic and biological drug substances and products, including vaccines, gene therapies, and combination products that were not comprehensively covered under the existing stability guidances [4] [6]. This is particularly significant for developers of advanced therapies, who previously had to navigate multiple documents with potential gaps for their innovative products [3].
Key Changes and Implications for Analytical Method Validation
The 2025 ICH Q1 draft introduces substantial changes that directly impact how analytical methods for stability testing are developed, validated, and implemented throughout the product lifecycle. These changes reflect a modernized scientific approach that emphasizes risk-based principles and methodological robustness.
Expanded Scope and Lifecycle Management
The draft guideline significantly broadens its applicability to include product categories such as advanced therapy medicinal products (ATMPs), vaccines, and other complex biological products including combination products [4] [2]. This expansion necessitates development of novel analytical methods capable of addressing the unique stability challenges presented by these advanced modalities, which may include cell viability assays for ATMPs or specialized potency assays for gene therapies [3].
Furthermore, the guideline introduces lifecycle stability management aligned with ICH Q12, encouraging a more proactive, ongoing stability planning throughout the product lifecycle [2] [3]. This represents a shift from stability as a box-ticking exercise for regulatory submission to an integrated component of pharmaceutical quality systems [3]. For analytical method validation, this means methods must be robust and adaptable enough to support continued verification throughout the product's market life, including post-approval changes.
Enhanced Statistical Modeling and Data Analysis
The draft provides clearer instructions on using statistical models for stability testing, replacing previous standards that were often perceived as vague and complicated [3]. This includes enhanced guidance on stability modeling and more precise requirements for statistical data analysis and extrapolation when establishing re-test periods or shelf life [2].
For analytical scientists, this emphasizes the need for statistically sound method validation approaches that generate data suitable for sophisticated stability modeling. The methods must produce reliable, precise data that can support the statistical models used to predict product stability under various conditions [3]. The draft also formally acknowledges the role of reduced stability studies using tools like bracketing, matrixing, and modeling, provided they are supported by adequate scientific justification and robust analytical data [3].
Risk-Based and Science-Driven Approaches
The new guideline strongly emphasizes the application of science- and risk-based principles throughout stability testing programs [1] [2]. This aligns with modern Quality-by-Design and lifecycle management principles, offering greater flexibility while maintaining regulatory confidence [3].
This approach requires analytical methods to be developed with a comprehensive understanding of critical quality attributes and their potential variation under stability testing conditions. Method validation should demonstrate the method's ability to detect meaningful changes in these attributes, with validation parameters tailored based on risk assessment [3]. The draft encourages leaner stability study designs but increases the burden for scientific justification, requiring more comprehensive data and documentation to support any reduced testing protocols [3].
Practical Implementation: Protocols, Materials, and Workflows
Implementing the new ICH Q1 guideline requires understanding updated experimental approaches and their implications for daily laboratory practice. This section provides practical guidance on methodologies, essential materials, and analytical workflows aligned with the new framework.
Research Reagent Solutions for Stability Testing
Stability testing according to ICH Q1 requires specific reagents and materials to ensure accurate, reproducible results. The following table details essential solutions and their functions in stability studies.
Table: Essential Research Reagent Solutions for Stability Testing
| Reagent/Material | Primary Function in Stability Testing | Key Considerations |
|---|---|---|
| Reference Standards | Quantification of active ingredient and degradation products; system suitability [3] | Must be well-characterized and stored under validated conditions |
| Forced Degradation Solutions | Elucidating degradation pathways and validating stability-indicating methods [7] | Include acid, base, oxidative, thermal, and photolytic stress conditions |
| Mobile Phase Components | Chromatographic separation of analytes and degradation products [7] | pH, buffer concentration, and organic modifier must be robust |
| Microbiological Media | Microbial limit testing and sterility testing for parenteral products [7] | Growth promotion testing must meet pharmacopeial requirements |
| Preservative Efficacy Testing Materials | Evaluating antimicrobial effectiveness in multidose products [7] | Challenge organisms must represent likely contaminants |
Updated Stability Testing Workflow
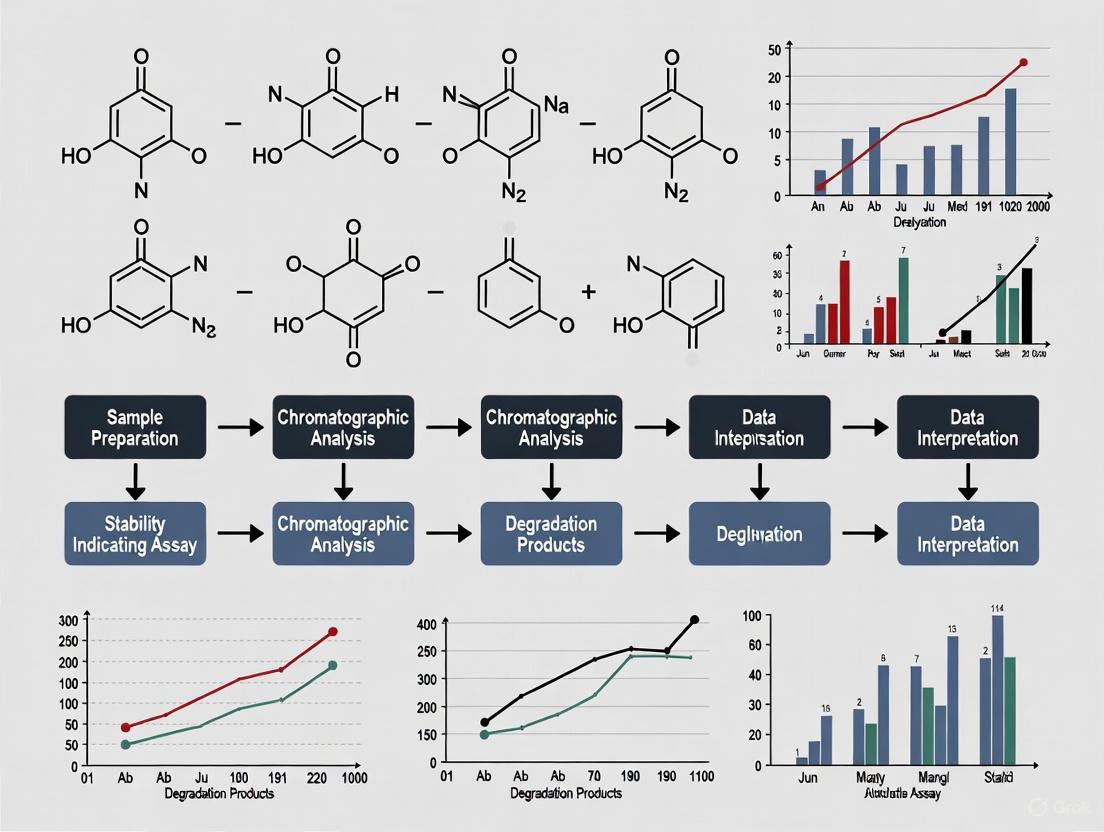
The new ICH Q1 guideline formalizes a comprehensive approach to stability testing that integrates quality by design and risk management principles. The following workflow diagram illustrates the key stages in designing and conducting stability studies under the updated framework.
Experimental Protocols for Key Stability Studies
The experimental methodologies for stability testing have been refined in the new guideline, with particular emphasis on scientific justification and risk-based approaches.
Long-Term Stability Testing Protocol
Long-term testing remains the cornerstone of stability programs, with the draft guideline reinforcing its importance while allowing for more flexible, risk-based designs [7].
- Objective: Evaluate drug substance/product quality under recommended storage conditions to establish shelf life or re-test period [7].
- Storage Conditions: 25°C ± 2°C / 60% RH ± 5% RH or 30°C ± 2°C / 65% RH ± 5% RH, depending on climatic zone [7].
- Testing Frequency: Every 3 months during first year, every 6 months during second year, and annually thereafter for drugs with proposed shelf life of at least 12 months [7].
- Key Analytical Parameters: Appearance, assay, degradation products, dissolution (for solids), moisture content, and microbiological testing where applicable [7].
- Statistical Analysis: Employment of stability modeling and statistical analysis for shelf life estimation, with clearer guidance provided in the new draft [2] [3].
Accelerated Stability Testing Protocol
Accelerated studies continue to play a crucial role in predicting long-term stability and identifying potential stability issues [7].
- Objective: Predict long-term stability over a shorter period and identify potential stability issues that may occur during storage and transport [7].
- Storage Conditions: 40°C ± 2°C / 75% RH ± 5% RH for minimum of 6 months [7].
- Testing Frequency: Typically at 0, 1, 2, 3, and 6-month timepoints [7].
- Key Analytical Parameters: Same as long-term testing, with particular attention to degradation products that may form more rapidly under stress conditions [7].
- Data Interpretation: Results from accelerated studies inform the design of long-term studies and may support extrapolation of shelf life when supported by statistical analysis [3].
Stability Testing for Advanced Therapy Medicinal Products (ATMPs)
The new guideline includes specific, though limited, guidance for ATMPs, addressing a significant gap in the previous guidelines [3].
- Special Considerations: Account for unique stability challenges of cell and gene therapies, including viability, potency, and unique degradation pathways [3].
- Storage Conditions: Often require cryogenic conditions or specific temperature ranges not covered by standard climatic zones [3].
- Testing Parameters: Include product-specific quality attributes such as cell viability, identity, purity, and potency markers [3].
- In-Use Stability: Critical for products requiring thawing, dilution, or other manipulation before administration [3].
Comparative Analysis: Previous vs. New Framework
The transition from the previous collection of guidelines to the unified 2025 draft represents a fundamental shift in stability testing philosophy and practice. This section provides a detailed comparison of key aspects across both frameworks.
Table: Comprehensive Comparison of Previous vs. New ICH Q1 Framework
| Aspect | Previous Framework (Q1A-F + Q5C) | New 2025 Draft Framework | Impact on Analytical Validation |
|---|---|---|---|
| Document Structure | 7 separate guidelines with some overlapping and gaps [3] | Single unified document with 18 sections + 3 annexes [3] | Simplified reference; clearer requirements |
| Product Scope | Primarily synthetic drugs & some biologics [4] | Includes ATMPs, vaccines, combination products [4] [2] | New methods needed for novel modalities |
| Statistical Guidance | Vague and complicated standards [3] | Clear instructions on modeling and data analysis [2] [3] | More robust method validation required |
| Study Design Approach | Largely fixed designs with limited flexibility [3] | Science- and risk-based with reduced studies allowed [1] [3] | Higher burden for scientific justification |
| Lifecycle Management | Focused on registration requirements [5] | Integrated with ICH Q12 for full lifecycle [2] [6] | Methods must support post-approval changes |
| Climatic Zones Coverage | Limited to specific ICH regions [7] | Includes all zones for global harmonization [6] | Broader environmental validation needed |
| Reference Standards | Limited specific guidance [3] | Clearer instructions on testing and storage [3] | Improved standardization across methods |
Regulatory and Implementation Timeline
Understanding the implementation status of the new guideline is crucial for planning stability programs. The following diagram illustrates the development timeline and future milestones for the ICH Q1 draft guideline.
The 2025 ICH Q1 draft guideline represents a transformative shift from a fragmented collection of stability guidelines to a unified, modern framework that addresses the current and future needs of the pharmaceutical industry. By consolidating Q1A-F and Q5C into a single document, the draft provides a more coherent approach to stability testing while expanding coverage to include advanced therapies, implementing enhanced statistical guidance, and promoting science- and risk-based principles [1] [2] [3].
For researchers and drug development professionals, this consolidation means simplified referencing and more consistent expectations across different product types. However, it also brings new responsibilities in justifying stability strategies through robust scientific data and comprehensive risk assessment [3]. The emphasis on lifecycle management aligns stability testing with broader quality systems, requiring analytical methods to be validated for long-term use across the product's commercial life [2] [6].
As the guideline progresses toward final implementation, stakeholders should proactively prepare by reviewing the draft document, assessing its impact on current programs, updating training curricula, and exploring digital tools that support the enhanced modeling and statistical analysis requirements [3]. While the full implementation timeline remains ahead, early engagement with the new framework will position organizations to successfully navigate this significant evolution in stability testing requirements, ultimately supporting the development of safe, effective, and high-quality medicines for global markets.
The stability testing landscape for pharmaceuticals is undergoing its most significant transformation in over two decades. The International Council for Harmonisation (ICH) has consolidated its previously fragmented stability guidances (Q1A-F and Q5C) into a single, comprehensive document—the draft ICH Q1 guideline released in 2025 [8] [9] [4]. This overhaul represents more than mere administrative consolidation; it fundamentally modernizes stability requirements to accommodate advanced therapeutic modalities that did not exist when the original guidances were written. For researchers and drug development professionals, this expansion explicitly brings Advanced Therapy Medicinal Products (ATMPs), complex biologics, and combination products under a harmonized stability framework for the first time, addressing critical gaps that have long challenged developers of innovative therapies [8] [9].
This guide compares the new stability testing paradigm against previous requirements, with particular focus on product categories that previously lacked clear ICH direction. We examine the experimental approaches and analytical method validation strategies needed to comply with the modernized, science-driven framework that emphasizes risk-based principles and lifecycle management [9].
Comparative Analysis of Old vs. New Stability Guidance
Table: Comparison of Key Changes in ICH Stability Guidance
| Aspect | Previous Approach (ICH Q1A-F, Q5C) | New Consolidated Approach (ICH Q1 2025 Draft) |
|---|---|---|
| Document Structure | Fragmented across multiple documents (Q1A-R2, Q1B, Q1C, Q1D, Q1E, Q5C) [8] | Single comprehensive guideline (18 sections + 3 annexes) [9] |
| Product Scope | Primarily small molecules; some biologics under Q5C [8] | Explicit inclusion of ATMPs, vaccines, oligonucleotides, peptides, combination products [8] [9] |
| Philosophical Basis | Standardized, "one-size-fits-all" protocols [8] | Science- and risk-based approaches with "alternative, scientifically justified approaches" [9] |
| Stability Strategy | Fixed study designs | Encourages bracketing, matrixing, predictive modeling with justification [8] |
| Lifecycle Perspective | Focused primarily on pre-approval data [8] | Formalized stability lifecycle management continuing post-approval [8] [9] |
| Statistical Guidance | Limited statistical evaluation guidance [8] | New annex dedicated to stability modeling and statistical evaluations [9] |
Experimental Protocols for New Product Categories
Stability Study Design for Advanced Therapy Medicinal Products (ATMPs)
ATMPs present unique stability challenges due to their living cellular components, complex biological activities, and frequently cryopreserved storage requirements [10]. The new ICH Q1 draft includes Annex 3, which provides specific stability guidance for these products [9].
Critical Methodology Considerations:
- Potency Assay Validation: Employ orthogonal methods using different scientific principles to measure the same critical quality attribute (CQA). For cell-based therapies, this includes both functional assays and viability measurements [11].
- Real-Time Stability Protocols: Design studies that monitor critical quality attributes throughout the proposed shelf life. For cryopreserved products, this includes stability through multiple freeze-thaw cycles [10].
- Container Closure System Testing: Verify compatibility with final container systems, including potential interactions with cryopreservatives and storage bags [9].
- In-Use Stability Assessments: Evaluate stability under conditions of actual clinical use, including post-thaw hold times and administration periods [9].
Stability Testing for Complex Biological Products
The expanded guidance explicitly addresses stability considerations for vaccines, oligonucleotides, peptides, and plasma-derived products [9].
Key Experimental Approaches:
- Forced Degradation Studies: Conduct under more severe conditions than accelerated testing to identify potential degradation pathways and develop stability-indicating methods [9].
- Multi-Parameter Stability Assessment: Monitor biological activity, conformational integrity, and particulate formation in addition to traditional chemical and physical parameters [9].
- Adjuvant and Excipient Stability: For vaccines and formulated biologics, include novel excipients and adjuvants in stability protocols due to their potential impact on product quality [9].
Combination Product Stability Considerations
For drug-device combination products, the guidance requires integrated stability approaches that account for both pharmaceutical and device components [9].
Essential Protocol Elements:
- Functionality Testing: Include device performance metrics throughout stability studies to ensure proper operation at expiry [9].
- Interface Assessment: Evaluate chemical and physical interactions between drug and device components over time [9].
- Simulated-Use Testing: Incorporate testing that mimics patient use conditions at various timepoints throughout the shelf life [9].
Analytical Method Validation in Stability Testing
Phase-Appropriate Validation Requirements
The regulatory approach to analytical method validation has evolved to reflect a phase-appropriate framework while maintaining scientific rigor [11].
Table: Analytical Method Expectations Across Development Phases
| Development Phase | Method Validation Expectation | Stability Testing Application |
|---|---|---|
| Phase 1 | Assay qualification (reliable, reproducible, sensitive enough for safety decisions) [11] | Monitoring of critical safety attributes (sterility, purity, identity) |
| Phase 2 | Refinement of critical process parameters; beginning of phase-appropriate validation [11] | Expanded stability testing with tighter specifications |
| Phase 3 to Commercial | Full validation per ICH Q2(R2) [12] [11] | Comprehensive stability-indicating methods for shelf-life determination |
Orthogonal Method Implementation
Regulators increasingly expect orthogonal methods—employing different scientific principles to measure the same attribute—particularly for critical quality attributes of complex products [11].
Implementation Framework:
- Justification Strategy: Provide scientific rationale for each orthogonal method selected, explaining how different measurement principles collectively ensure result reliability [11].
- Method Comparison Protocols: Establish correlation between different methods during development phase to demonstrate complementary value [11].
- Phase-Appropriate Implementation: Introduce orthogonal methods early in development, with increasing rigor through commercialization [11].
Visualization: Modern Stability Strategy Development
Modern Stability Strategy Development Flow
This workflow illustrates the science- and risk-based approach endorsed by the modernized ICH Q1 guideline. The process begins with thorough product understanding, proceeds through risk assessment, and implements flexible, justified stability strategies with ongoing lifecycle management [9].
Essential Research Reagent Solutions
Table: Key Reagents for Advanced Stability Programs
| Reagent/Category | Function in Stability Testing | Application Notes |
|---|---|---|
| Reference Standards | Quantification and method qualification | Must be fully qualified; characterized for CQAs [11] |
| Cell-Based Assay Systems | Potency determination for biologics and ATMPs | Functional, biologically relevant assays required by regulators [11] |
| GMP-Grade Culture Media | ATMP manufacturing and stability assessment | Essential for maintaining cell viability and function [10] [11] |
| Molecular Characterization Tools | Genetic stability assessment for ATMPs | Karyotype analysis to detect genetic instability [10] |
| Orthogonal Detection Reagents | Multiple method implementation for CQAs | Different scientific principles for same attribute [11] |
The consolidated ICH Q1 guideline represents a paradigm shift in stability testing, moving from rigid, standardized protocols to flexible, science-driven strategies. This expansion to include ATMPs, complex biologics, and combination products addresses longstanding gaps in regulatory guidance while creating new considerations for drug developers [8] [9].
Successful implementation requires:
- Early engagement with regulatory agencies through INTERACT or pre-IND meetings for complex products [11]
- Development of orthogonal analytical methods for critical quality attributes [11]
- Comprehensive risk assessment to justify reduced designs or modeling approaches [9]
- Lifecycle planning for stability monitoring beyond initial approval [8]
The modernized stability framework offers opportunities for more efficient, scientifically grounded stability programs while demanding greater expertise and justification from sponsors. For researchers and drug development professionals, understanding these expanded requirements is essential for successfully navigating the approval pathway for advanced therapies.
The recent publication of the draft ICH Q1 guideline, a consolidated revision superseding the ICH Q1A-F and Q5C series, marks a significant evolution in global stability testing requirements for pharmaceuticals [1] [13]. This updated framework expands its scope to encompass a broader range of product types, including advanced therapy medicinal products (ATMPs), vaccines, and other complex biologicals, while emphasizing science- and risk-based principles [14] [2]. Within this modernized context, the role of thoroughly validated analytical methods becomes more critical than ever. They form the foundational backbone that generates the reliable, reproducible stability data upon which all subsequent decisions—from shelf-life estimation to regulatory approval—depend.
This guide examines the integral connection between the new ICH Q1 framework and validated stability-indicating methods, providing a direct comparison of traditional versus modernized approaches. We will explore the experimental protocols that underpin method validation and demonstrate how these methodologies ensure data integrity throughout the product lifecycle.
The New ICH Q1 Framework: A Consolidated Foundation for Modern Products
The ICH Q1 draft guideline, reaching Step 2 of the ICH process in April 2025, represents a comprehensive effort to harmonize and modernize global stability testing practices [14] [2]. Its core objective is to provide harmonized requirements for generating stability data that supports regulatory submissions and post-approval changes across a diverse spectrum of drug substances and products [13].
Key Updates and Expanded Scope
The revised guideline is structured into 18 sections and three annexes, covering everything from development stability studies to lifecycle considerations [14]. A primary update is the expansion of product coverage, moving beyond traditional synthetic chemicals to include:
- Synthetic chemical entities, including oligonucleotides and semi-synthetics
- Biologicals, such as therapeutic proteins and plasma-derived products
- Advanced Therapy Medicinal Products (ATMPs) like cell and gene therapies (e.g., CAR-T cells)
- Vaccines and adjuvants
- Combination drug-device products [14] [2]
This consolidation also introduces new content on in-use studies, short-term stability, stability modeling, and guidance for product lifecycle management aligned with ICH Q12 [14] [2]. The guideline emphasizes that stability studies must provide evidence on how the quality of a drug substance or product varies over time under the influence of environmental factors like temperature, humidity, and light [1].
Stability Testing Conditions in the New Framework
The following table summarizes the core storage conditions for stability testing as outlined in the ICH guidelines, which are designed to simulate the climatic zones where products will be marketed.
Table 1: Standard ICH Stability Testing Conditions for Climatic Zones I and II
| Study Type | Storage Conditions | Minimum Time Period | Primary Purpose |
|---|---|---|---|
| Long-Term | 25°C ± 2°C / 60% RH ± 5% RH or 30°C ± 2°C / 65% RH ± 5% RH | 12 months | Primary data source for re-test period/shelf life [15] |
| Intermediate | 30°C ± 2°C / 65% RH ± 5% RH | 6 months | Bridges long-term and accelerated data [15] |
| Accelerated | 40°C ± 2°C / 75% RH ± 5% RH | 6 months | Evaluates short-term, extreme condition effects [15] |
The Indispensable Role of Validated Analytical Methods
Within the structure of ICH Q1, validated analytical methods are not merely a technical requirement but the critical component that ensures the integrity of the entire stability assessment. As defined by regulatory requirements, "The accuracy, sensitivity, specificity, and reproducibility of test methods employed by the firm shall be established and documented" [16]. Method validation is the process of demonstrating that an analytical procedure is suitable for its intended purpose, confirming it can execute reliably and reproducibly to generate accurate data for monitoring drug substance and product quality [16].
The Stability-Indicating Method: A Core Concept
A stability-indicating method is an analytical procedure that can accurately and reliably measure the active pharmaceutical ingredient (API) and its degradation products without interference [16]. The core requirement is that the method must physically separate (baseline-resolve) the API, process impurities, and degradation products above the reporting thresholds [16]. This is typically achieved through forced degradation studies during method development, which investigate the main degradative pathways of the drug substance and product. These studies provide samples with sufficient degradation products to evaluate the method's ability to separate and quantify all relevant analytes, thereby demonstrating its specificity [16].
Comparative Analysis: The Impact of Method Validation on Stability Data Quality
The quality of stability data generated under ICH Q1 is directly contingent upon the rigor of the analytical method validation. The table below contrasts the outcomes of stability studies supported by poorly characterized methods versus those backed by fully validated, stability-indicating methods.
Table 2: Comparison of Stability Study Outcomes Based on Analytical Method Robustness
| Aspect | Poorly Characterized Methods | Validated Stability-Indicating Methods |
|---|---|---|
| Data Reliability | Questionable; potential for inaccurate potency and impurity results [16] | High; results are accurate, reproducible, and reliable for decision-making [16] |
| Degradation Detection | May miss critical degradants or misidentify peaks [16] | Comprehensively identifies and quantifies degradants through forced degradation studies [16] |
| Shelf-Life Estimation | Risky; based on potentially incomplete data, risking patient safety and product quality [15] | Scientifically sound; supports justified and accurate shelf-life claims using statistical evaluation [14] |
| Regulatory Compliance | Low; fails to meet ICH Q2, USP <1225>, and GMP requirements [16] | High; meets all regulatory validation requirements for submissions like NDAs [16] |
| Lifecycle Management | Difficult to manage post-approval changes due to unreliable baseline [16] | Enables effective lifecycle management and support for post-approval changes (per ICH Q12) [2] |
Core Validation Parameters and Experimental Protocols
The validation of a stability-indicating HPLC method is a systematic process governed by protocols with pre-defined acceptance criteria. The following section details the key parameters and methodologies involved.
Method Validation Parameters and Their Definitions
The validation of a stability-indicating method involves assessing multiple inter-related parameters to ensure its overall suitability.
Figure 1: The core parameters required for validating a stability-indicating analytical method, demonstrating their relationship to the overall method's purpose [16].
Detailed Experimental Protocols for Key Parameters
Specificity
- Objective: To demonstrate the method's ability to unequivocally assess the analyte in the presence of components that may be expected to be present, such as impurities, degradants, or excipients [16].
- Protocol:
- Forced Degradation Studies: Expose the drug substance and product to stress conditions (e.g., acid, base, oxidation, heat, and light) to generate degradation products [16].
- Chromatographic Separation: Inject stressed samples and demonstrate that the analyte peak is free from interference and that all degradation products are baseline-resolved [16].
- Peak Purity Assessment: Use a photodiode array (PDA) detector or mass spectrometry (MS) to confirm the homogeneity of the API peak, proving that no co-eluting impurities are present [16].
Accuracy
- Objective: To establish the closeness of agreement between the value found and the value accepted as a true or reference value [16].
- Protocol:
- Spiked Recovery Experiments: For a drug product, prepare a placebo blank and spike it with known quantities of the API (and available impurities) at multiple concentration levels, typically 80%, 100%, and 120% of the target assay concentration [16].
- Replication: Perform a minimum of nine determinations over the three concentration levels (e.g., three preparations at each level) [16].
- Calculation: Calculate the percent recovery of the analyte. Acceptance criteria are often set, for example, at 98.0–102.0% recovery for the API at the 100% level [16].
Precision
- Objective: To demonstrate the degree of scatter between a series of measurements obtained from multiple sampling of the same homogeneous sample [16].
- Protocol:
- Repeatability: Inject a minimum of five replicates of a homogeneous standard or sample preparation by one analyst on the same day. System precision (injection repeatability) is often required to have an RSD < 2.0% for peak areas [16].
- Intermediate Precision: Have a second analyst on a different day using different equipment repeat the assay of a homogeneous sample batch. The combined data from both analysts should meet pre-set criteria (e.g., overall RSD < 2.0%) [16].
Table 3: The Scientist's Toolkit: Essential Reagents and Materials for Method Validation
| Reagent / Material | Critical Function in Validation |
|---|---|
| Drug Substance (API) Reference Standard | Serves as the primary benchmark for identity, potency, and purity assessments [16]. |
| Known Impurity & Degradation Standards | Used to confirm method specificity, establish relative response factors, and validate accuracy for impurities [16]. |
| Placebo Formulation (for Drug Product) | A mock drug product without API; critical for demonstrating specificity and accuracy free from excipient interference [16]. |
| Forced Degradation Reagents | Acids, bases, oxidants, etc., used to intentionally degrade the product and challenge the method's stability-indicating properties [16]. |
| Mass Spectrometry-Compatible Solvents | Enable the use of MS as an orthogonal detection technique for peak identification and purity confirmation during method development [16]. |
The updated ICH Q1 guideline provides a modernized, harmonized framework for stability testing, but its effectiveness is entirely dependent on the quality of the analytical data fed into it. Validated, stability-indicating methods are not a peripheral compliance activity; they are the critical backbone that ensures the reliability of stability data for shelf-life prediction, supports regulatory submissions across a widening array of complex products, and ultimately safeguards patient safety. As the industry moves toward greater adoption of risk-based approaches, stability modeling, and lifecycle management, the demand for robust, well-understood analytical procedures will only intensify. The successful implementation of the new Q1 framework, therefore, hinges on a continued commitment to rigorous analytical method validation.
In the landscape of global pharmaceutical development, the International Council for Harmonisation (ICH) guidelines Q8, Q9, and Q10 represent a fundamental shift from traditional, quality-by-testing approaches toward a modern, integrated framework built on science-based and risk-based principles [17]. These guidelines form a synergistic system that guides the entire product lifecycle, from initial development through commercial manufacturing, with the ultimate goal of robustly ensuring product quality, safety, and efficacy [18] [19]. The European Medicines Agency (EMA) emphasizes that these guidelines should be viewed as an integrated system, with each providing specific details to support product realization and a lifecycle that remains in a state of control [20].
This triad of guidelines can be visualized as a three-legged stool, where each leg is essential for stability [21]. ICH Q8 (Pharmaceutical Development) introduces the systematic methodology of Quality by Design (QbD), ensuring that quality is built into the product from the outset. ICH Q9 (Quality Risk Management) provides the tools and principles for a proactive approach to identifying and controlling potential risks to quality. ICH Q10 (Pharmaceutical Quality System) establishes a comprehensive management framework that enshrines these concepts and drives continual improvement [17] [18]. Together, they enable the industry to achieve a more "maximally efficient, agile, [and] flexible pharmaceutical manufacturing sector that reliably produces high quality drug products" [21].
Comparative Analysis of ICH Q8, Q9, and Q10 Guidelines
While functionally interdependent, each ICH guideline possesses a distinct scope, primary objective, and set of core elements. Their complementary roles form the backbone of a modern pharmaceutical quality system.
Table 1: Core Components and Functions of the ICH Q8-Q10 Guidelines
| Guideline | Primary Focus & Objective | Key Concepts & Elements | Contribution to the Integrated System |
|---|---|---|---|
| ICH Q8 (R2): Pharmaceutical Development [17] [22] [21] | Focus: Pharmaceutical development process.Objective: To ensure systematic design and development of drug products and processes to consistently deliver intended performance. | • Quality by Design (QbD)• Quality Target Product Profile (QTPP)• Critical Quality Attributes (CQAs)• Critical Process Parameters (CPPs)• Design Space• Control Strategy | Provides the scientific foundation and road map (QTPP, CQAs) for development. Establishes a proactive framework (QbD) for building in quality, rather than testing it in. |
| ICH Q9 (R1): Quality Risk Management [17] [22] | Focus: Risk management principles and tools.Objective: To provide a proactive framework for identifying, assessing, controlling, communicating, and reviewing risks to quality. | • Risk Assessment (Identification, Analysis, Evaluation)• Risk Control (Reduction, Acceptance)• Risk Communication & Review• Risk Management Tools (e.g., FMEA, HACCP) | Provides the decision-making framework. Enables science-based decisions by ensuring the level of effort and control is commensurate with the level of risk to the patient. |
| ICH Q10: Pharmaceutical Quality System [17] [18] | Focus: Comprehensive quality management system.Objective: To establish a robust system for managing quality across the product lifecycle, enabling continual improvement. | • Process Performance & Product Quality Monitoring• Corrective and Preventive Action (CAPA) System• Change Management System• Management Review• Knowledge Management | Provides the operational infrastructure and culture. Ensures QbD and QRM principles are effectively implemented, monitored, and improved upon throughout the product's life. |
The Integrated Workflow: From Concept to Commercial Product
The power of ICH Q8, Q9, and Q10 is fully realized when their principles are woven into a single, seamless workflow from product conception to commercial manufacturing and beyond. The following diagram illustrates this integrated, lifecycle approach.
The workflow begins with ICH Q8, where the Quality Target Product Profile (QTPP) is defined as a prospective summary of the drug's desired quality characteristics [21]. This leads to the identification of Critical Quality Attributes (CQAs)—the physical, chemical, biological, or microbiological properties that must be controlled to ensure product quality [22] [21].
ICH Q9's risk management principles are then applied to link Critical Material Attributes (CMAs) and Critical Process Parameters (CPPs) to the CQAs [19]. This risk assessment is foundational for developing a control strategy to ensure that CQAs are consistently met [20]. The knowledge gained feeds back into Q8 to establish the manufacturing process and its associated design space—the multidimensional combination of variables demonstrated to assure quality [22].
Finally, ICH Q10 ensures this developed product and process are effectively managed throughout the commercial lifecycle. Its four key components—process performance monitoring, CAPA, change management, and management review—work together to maintain a state of control and facilitate continuous improvement [17] [18].
Experimental Protocols for Implementing QbD and QRM
Protocol 1: Establishing a QbD-Based Control Strategy for a Solid Dosage Form
The application of QbD is a systematic process that moves from high-level goals to a defined and well-understood control strategy.
- Define the Quality Target Product Profile (QTPP): The first step is to create a prospective list of the drug's target quality characteristics. For a solid oral tablet, this typically includes elements such as dosage form, strength, dissolution criteria, stability requirements, and container closure system [21].
- Identify Critical Quality Attributes (CQAs): Using the QTPP as a guide, determine which physicochemical or biological properties are critical to ensuring quality. For a tablet, common CQAs include assay/potency, content uniformity, dissolution rate, impurity profile, and moisture content [21]. A risk assessment is often used to screen and rank potential attributes based on their impact on safety and efficacy.
- Link Raw Materials and Process Parameters to CQAs: This stage employs Design of Experiments (DoE) and risk assessment tools (e.g., Failure Mode and Effects Analysis, FMEA) to understand the relationship between input variables and the CQAs [20]. The goal is to determine which Critical Material Attributes (CMAs) of the ingredients (e.g., API particle size distribution, excipient grade) and which Critical Process Parameters (CPPs) of the unit operations (e.g., blender speed, compression force, granulation endpoint) significantly impact the CQAs.
- Develop and Refine the Design Space: Based on the experimental data, a design space is developed for the CPPs to define their proven acceptable ranges that consistently yield product meeting all CQAs [22]. Operating within this space is not considered a change, providing operational flexibility.
- Implement and Validate the Control Strategy: The control strategy is a comprehensive plan that combines controls for CMAs, CPPs, and in-process tests, along with final product specifications, to ensure the process performs as expected and the product meets its QTPP [20]. This strategy is confirmed during process validation.
Protocol 2: Conducting a Risk Assessment for a Sterile Filling Operation
A practical application of ICH Q9 in a high-risk manufacturing environment involves a structured risk assessment to identify and control critical hazards [22].
- Risk Identification: Assemble a cross-functional team to systematically identify potential hazards (e.g., microbial contamination, endotoxin, incorrect fill volume) using tools like process mapping and historical data analysis [18].
- Risk Analysis: For each identified hazard, evaluate the severity of the impact on the patient and the probability of occurrence. A risk matrix is commonly used, often with a "traffic light" principle (Red/Amber/Green) to visualize priority levels [22] [20].
- Risk Evaluation: Rank the risks based on their analysis. A case study on a sterile-fill operation used this method to identify hazards with a risk priority number (RPN) of ≥105 as critical, requiring immediate and targeted controls [22].
- Risk Control: Implement measures to mitigate high-priority risks. This could include design modifications (e.g., isolator technology), process adjustments (e.g., defined environmental monitoring), and enhanced quality controls (e.g., 100% fill weight checks) [22] [18].
- Risk Review and Communication: Document the entire assessment and communicate the findings to all relevant stakeholders. The risk assessment should be a living document, reviewed periodically and when changes occur to the process or equipment [17].
Essential Research Reagent Solutions for Analytical Lifecycle Management
The implementation of a science- and risk-based approach to analytical methods, in alignment with the ICH Q8-Q10 framework, relies on specific tools and reagents. The USP has advocated for a lifecycle model for analytical procedures, mirroring the concepts used for process validation [23].
Table 2: Key Reagents and Materials for Robust Analytical Methods
| Research Reagent / Material | Critical Function & Rationale |
|---|---|
| System Suitability Reference Standards | Verifies that the analytical instrument and procedure are performing as intended at the time of the test. Essential for demonstrating method reproducibility and reliability as per ICH Q2. |
| Pharmaceutical Grade Reference Standards | Provides the definitive, highly characterized substance for identifying and quantifying the Active Pharmaceutical Ingredient (API) and its impurities. Critical for accurate method development and validation. |
| Process-Related Impurity Standards | Used to qualify and validate methods for specific impurities identified during risk assessment (ICH Q9). Enables accurate tracking and control of impurities as outlined in ICH Q3. |
| Stable Isotope-Labeled Internal Standards | Improves the accuracy and precision of mass spectrometry-based methods (e.g., LC-MS/MS) by correcting for variability in sample preparation and ionization. Key for robust bioanalytical methods. |
| Chromatography Columns & Consumables | Specific columns (e.g., UPLC, HPLC) and high-purity solvents/mobile phases are critical material attributes (CMAs) for chromatographic methods. Their consistent performance is vital for method robustness. |
The ICH Q8, Q9, and Q10 guidelines collectively provide a powerful, integrated framework for achieving a modern, robust pharmaceutical quality system. By moving from a reactive, quality-by-testing paradigm to a proactive, science- and risk-based approach, the industry can achieve significant benefits: enhanced product quality and patient safety, improved regulatory compliance, and increased operational efficiency through more strategic resource allocation [18]. The successful integration of these guidelines—where Q8 provides the scientific roadmap, Q9 enables risk-informed decision-making, and Q10 ensures effective lifecycle management—is the cornerstone of a maximally efficient and agile pharmaceutical manufacturing sector capable of reliably delivering high-quality medicines to patients [21] [19].
From Theory to Practice: Implementing ICH Q2(R2) Parameters in Stability Studies
Defining the Analytical Target Profile (ATP) for Stability-Indicating Methods
In the pharmaceutical industry, ensuring the quality, safety, and efficacy of drug substances and products over their shelf life is paramount. Stability-indicating methods (SIMs) are analytical procedures specifically designed and validated to measure the quality attributes of drug substances and products while reliably discriminating between the active pharmaceutical ingredient (API) and its potential degradation products [24]. Within the framework of International Council for Harmonisation (ICH) guidelines and the Quality by Design (QbD) paradigm, the Analytical Target Profile (ATP) has emerged as a foundational concept for the lifecycle management of these critical methods [25]. The ATP is defined as a prospective summary of the performance requirements for an analytical procedure, outlining the quality criteria that a reportable result must meet to ensure confidence in the decisions made about a product's quality and stability [25] [26]. This guide provides a comprehensive comparison of the ATP-centric approach against traditional method development, detailing the experimental protocols and data requirements for defining the ATP for stability-indicating methods in compliance with ICH guidelines.
Core Concepts: ATP, QbD, and ICH Stability Guidelines
The Analytical Target Profile (ATP) Defined
The ATP serves as the cornerstone for analytical method development and validation, much like the Quality Target Product Profile (QTPP) does for drug product development. In essence, the ATP specifies the required quality of the reportable result generated by the analytical method. It defines the maximum allowable uncertainty associated with a measurement, ensuring the result is fit for its intended purpose in making quality decisions [25]. For a stability-indicating method, the primary purpose is to accurately monitor the potency of the API and quantify the appearance of degradation products over time, thereby supporting the assignment of a scientifically justified shelf life.
The QbD Paradigm in Analytical Development
The implementation of QbD principles in analytical development, as mandated by ICH Q8, shifts the focus from merely testing quality into building it into the method from the outset [26]. This systematic approach involves:
- Defining the ATP: Clearly stating the method's purpose and required performance.
- Identifying Critical Method Attributes (CMAs): These are the performance characteristics of the method, such as specificity, accuracy, and precision, that must be controlled to ensure the ATP is met.
- Identifying Critical Method Parameters (CMPs): These are the variables in the analytical procedure (e.g., mobile phase composition, column temperature, flow rate) that can impact the CMAs.
- Establishing a Method Operable Design Region (MODR): The multidimensional combination of CMPs within which variations do not adversely affect the method's ability to meet the ATP, ensuring robustness [26].
The Regulatory Landscape: ICH Guidelines for Stability
Stability testing is rigorously defined by a suite of ICH guidelines. ICH Q1A(R2) provides the core protocol for stability testing, defining the storage conditions (e.g., 25°C ± 2°C/60% RH ± 5% RH for long-term studies) and minimum timeframes (e.g., 12 months for long-term data) required for registration applications [15] [27]. ICH Q1B addresses photostability testing, while ICH Q2(R1) outlines the validation of analytical procedures. The development of ICH Q14 and the revision of ICH Q2(R1) aim to formally harmonize and integrate modern, QbD-based concepts like the ATP into the analytical lifecycle [25].
The following workflow illustrates how the ATP drives the analytical method lifecycle within the QbD framework and its connection to product stability studies:
Comparative Analysis: ATP-Driven vs. Traditional Method Development
The adoption of an ATP-driven, QbD-based approach represents a significant evolution from traditional method development practices. The table below summarizes the key differences between these two paradigms.
Table 1: Comparison of ATP-Driven (QbD) and Traditional Analytical Method Development
| Aspect | ATP-Driven / QbD Approach | Traditional Approach |
|---|---|---|
| Philosophy | Quality is built into the method design from the start [26]. | Quality is tested into the method at the end of development. |
| Focus | Fitness for purpose; quality of the reportable result [25]. | Adherence to a fixed set of operational conditions. |
| Development Process | Systematic, using structured risk assessment and Design of Experiments (DoE) [26]. | Often sequential, one-factor-at-a-time (OFAT). |
| Robustness | Formally assessed and understood through a defined Method Operable Design Region (MODR) [26]. | Typically tested at the end of development with limited scope. |
| Regulatory Flexibility | Higher potential for flexibility via established performance-based conditions (ICH Q12) [25]. | Less flexible; changes often require regulatory notification. |
| Lifecycle Management | Continuous improvement guided by the ATP [25]. | Changes may require a new validation. |
The ATP-driven approach offers several distinct advantages. It provides a clear and unambiguous target for method development and validation, which enhances communication between development teams and regulatory agencies. By focusing on the performance of the reportable result rather than a specific technique, it can facilitate technological advancements and method improvements without necessitating major regulatory submissions, as long as the ATP continues to be met [25]. This is particularly valuable for long-term stability studies, where a method might need to be transferred or updated over its lifespan.
Defining the ATP for a Stability-Indicating Method
Key Components of the ATP
For a stability-indicating method, the ATP must explicitly define the criteria that ensure accurate quantification of the API and its degradation products. The core components include:
- Analyte and Matrix: Clearly define the analyte (e.g., specific API) and the matrix (e.g., drug product formulation including all excipients).
- Reportable Result: Specify the type of result needed (e.g., % assay of label claim, % of specific degradation product).
- Acceptable Uncertainty: Define the maximum combined uncertainty for the reportable result, which integrates specificity, accuracy, and precision [25].
- Range: Define the expected concentration range over which the method must perform, from the low level of degradation impurities to the high level of the API in the drug product [25].
Experimental Protocols for ATP Verification
The verification of an ATP for a stability-indicating method relies on a set of rigorously designed experiments, primarily centered on forced degradation studies and method validation.
Forced Degradation Studies (Stress Testing)
Forced degradation studies are critical for demonstrating the stability-indicating power of the method. These studies involve intentionally degrading the drug substance or product under various stress conditions to generate degradation products [24]. The experimental protocol generally includes:
- Acidic and Basic Hydrolysis: Treatment with acids (e.g., 0.75 N HCl) or bases (e.g., 0.03 N NaOH) at elevated temperatures (e.g., 25-75°C) for a defined period [26].
- Oxidative Degradation: Treatment with oxidizing agents like hydrogen peroxide (e.g., 10% H₂O₂) under reflux at elevated temperatures (e.g., 50°C) [26].
- Thermal and Photolytic Degradation: Exposure to dry heat and controlled light as per ICH Q1B.
The method must be able to separate and resolve the API from all generated degradation products, proving its specificity. The use of hyphenated techniques like HPLC-DAD and LC-MS is highly recommended for this purpose, as they allow for parallel quantitative analysis and qualitative identification of impurities [24].
Validation of Critical Method Performance Characteristics
The following table outlines the key performance characteristics defined in the ATP and their corresponding experimental protocols for validation.
Table 2: Key ATP Requirements and Corresponding Experimental Validation Protocols
| ATP Requirement | Experimental Validation Protocol | Typical Acceptance Criteria |
|---|---|---|
| Specificity/Selectivity | Inject samples from forced degradation studies. The method should resolve the API from all known and unknown degradation products [24]. | Peak purity index for the API peak passes; resolution from closest eluting peak > 2.0 [24] [26]. |
| Accuracy | Spike the API into the placebo or sample matrix at multiple concentration levels (e.g., 50%, 100%, 150%). Calculate recovery of the known amount [24]. | Mean recovery between 98.0% - 102.0% for the API. |
| Precision | - Repeatability: Multiple injections of a homogeneous sample (e.g., n=6) at 100% concentration.- Intermediate Precision: Repeat the analysis on a different day, with a different analyst, or different instrument [24]. | Relative Standard Deviation (RSD) ≤ 2.0% for the API assay. |
| Linearity & Range | Prepare and analyze standard solutions at a minimum of 5 concentration levels across a specified range (e.g., 50-150% of target concentration) [26]. | Correlation coefficient (r) > 0.999. |
| Robustness | Deliberately vary critical method parameters (CMPs) such as mobile phase pH (±0.1), temperature (±2°C), and flow rate (±10%) using a structured DoE (e.g., fractional factorial design) [26]. | All samples meet system suitability criteria despite variations. |
Case Study: Application of the ATP for a Green HPLC Method
A 2023 study on developing a green stability-indicating method for the concomitant analysis of fluorescein sodium and benoxinate hydrochloride provides an excellent example of the ATP and QbD in practice [26].
- ATP Definition: The goal was a "green, robust and fast stability indicating chromatographic method" for analyzing both drugs in the presence of degradation products within four minutes, replacing toxic solvents with eco-friendly alternatives [26].
- CMPs and CMAs: Critical Method Parameters screened via Fractional Factorial Design (FFD) included buffer pH, % of organic modifier, and column temperature. The Critical Method Attributes included resolution between peaks, analysis time, and greenness scores (Ecoscale, EAT) [26].
- Optimization: A Box-Behnken Design (BBD) was then used to model the relationship between CMPs and CMAs and to find the optimal MODR [26].
- Outcome: The optimized method used an isopropanol/phosphate buffer mobile phase, achieved analysis in under 4 minutes, and was validated for specificity across forced degradation studies (acidic, basic, oxidative), demonstrating successful ATP attainment [26].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Stability-Indicating Method Development
| Item | Function/Explanation |
|---|---|
| Chromatography System (HPLC/UHPLC) | Equipped with a DAD or PDA detector for peak purity assessment and hyphenation with Mass Spectrometry (LC-MS) for impurity identification [24] [26]. |
| C18 Chromatography Column | The most common stationary phase for reverse-phase separation of APIs and their degradation products [26]. |
| Buffers & Mobile Phases | e.g., Potassium dihydrogen phosphate for pH control; green solvents like Isopropanol or Ethanol as organic modifiers to replace acetonitrile [26]. |
| Forced Degradation Reagents | e.g., Hydrochloric Acid (HCl), Sodium Hydroxide (NaOH), Hydrogen Peroxide (Hâ‚‚Oâ‚‚) for generating degradation products under stress conditions [26]. |
| Design of Experiments (DoE) Software | Essential for systematic screening (e.g., FFD) and optimization (e.g., BBD) of method parameters, ensuring a robust MODR [26]. |
| EN106 | EN106, CAS:757192-67-9, MF:C13H13ClN2O3, MW:280.70 g/mol |
| EGFR-IN-146 | 2-phenyl-N-(pyridin-3-ylmethyl)quinazolin-4-amine |
The Analytical Target Profile is a powerful tool that aligns analytical method development with the core principles of Quality by Design and the rigorous requirements of ICH stability guidelines. By prospectively defining the required quality of the reportable result, the ATP ensures that stability-indicating methods are fit for their purpose of reliably monitoring drug quality throughout its shelf life. The comparative data and experimental protocols detailed in this guide demonstrate that an ATP-driven approach provides a more systematic, robust, and scientifically justified framework for method development compared to traditional practices. As the regulatory landscape evolves with ICH Q14, adopting the ATP concept will be crucial for pharmaceutical scientists and drug development professionals to achieve regulatory flexibility, enhance product quality, and ensure patient safety.
Within the pharmaceutical industry, demonstrating the stability of a drug substance or product is a regulatory imperative. This process relies heavily on analytical methods that can accurately and reliably quantify the active ingredient and monitor the formation of impurities over time. The validity of any stability conclusion is therefore intrinsically tied to the validity of the analytical procedure used. Analytical method validation provides the documented evidence that a method is fit-for-purpose, ensuring that the data generated for stability studies are trustworthy and scientifically sound [28] [29].
The International Council for Harmonisation (ICH) provides the harmonized framework for this validation, primarily through the Q2(R2) guideline on the validation of analytical procedures and the complementary Q14 guideline on analytical procedure development [28]. For professionals engaged in drug development, adherence to these guidelines is not merely a regulatory formality but a critical component of quality by design. It ensures that methods are capable of detecting changes in product quality attributes, such as a decrease in assay value or an increase in degradation products, which are essential for establishing a product's shelf life and storage conditions. This guide focuses on the five core parameters—Specificity, Accuracy, Precision, Linearity, and Range—that form the foundation of any validation protocol for drug stability testing.
Core Validation Parameters: Definitions and Experimental Protocols
The following sections detail each of the five core validation parameters, defining their significance and outlining the standard experimental protocols as per ICH guidelines.
Specificity
Definition and Significance: Specificity is the ability of an analytical procedure to assess the analyte unequivocally in the presence of components that may be expected to be present, such as impurities, degradants, or excipients [30] [28]. For stability-indicating methods, this is the most critical parameter. The method must be able to distinguish and quantify the analyte from its degradation products to provide an accurate stability profile.
Experimental Protocol: To demonstrate specificity, samples of the drug substance or product are subjected to stress conditions (e.g., acid, base, oxidation, thermal, and photolytic degradation) to generate degradants. The chromatogram of the degraded sample is then compared to that of a pure reference standard.
- Peak Purity Assessment: This is a crucial test, performed using a photodiode array (PDA) detector or mass spectrometry (MS). The software assesses the spectra across the entire analyte peak to confirm the absence of co-eluting impurities [29].
- Resolution: The resolution between the analyte peak and the closest eluting potential interferent must meet predefined acceptance criteria (e.g., Resolution > 1.5) [29].
Accuracy
Definition and Significance: Accuracy expresses the closeness of agreement between the value found and the value accepted as a true or reference value [30] [28]. It is a measure of trueness and is often reported as percent recovery. In the context of a stability test, an accurate method ensures that the reported potency or impurity level is a true reflection of the sample's quality.
Experimental Protocol: Accuracy is typically established by spiking the drug product with known quantities of the analyte.
- Sample Preparation: A minimum of nine determinations over a minimum of three concentration levels (e.g., 80%, 100%, 120% of the target concentration) covering the specified range should be performed [30] [29].
- Calculation: The recovery for each level is calculated as (Measured Concentration / Spiked Concentration) × 100%. The mean recovery across all levels should fall within predefined acceptance criteria, often 98–102% for the assay of an active ingredient [28].
Precision
Definition and Significance: Precision expresses the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions [30]. It is a measure of method variability and is subdivided into three levels:
- Repeatability (Intra-assay Precision): Precision under the same operating conditions over a short interval of time [29].
- Intermediate Precision: Precision within the same laboratory, incorporating variations like different days, different analysts, or different equipment [29].
- Reproducibility: Precision between different laboratories (assessed during method transfer) [29].
Experimental Protocol:
- Repeatability: Analyze a minimum of six determinations at 100% of the test concentration or nine determinations covering the specified range (e.g., three concentrations with three replicates each) [29].
- Intermediate Precision: A second analyst performs the same procedure on a different day, often using a different HPLC system. The results from both analysts are compared, and the % relative standard deviation (%RSD) is calculated for the combined data set [29].
- Data Reporting: Precision results are reported as the %RSD. For an assay method, an %RSD of ≤ 1.5% is often acceptable for repeatability [28].
Linearity and Range
Definition and Significance:
- Linearity is the ability of the method to obtain test results that are directly proportional to the concentration of the analyte within a given range [30] [31].
- Range is the interval between the upper and lower concentrations of analyte for which it has been demonstrated that the method has a suitable level of precision, accuracy, and linearity [30].
Experimental Protocol:
- Linearity: A series of standard solutions (a minimum of five) are prepared across the anticipated range (e.g., 50-150% of the target concentration). The responses are plotted against concentrations, and a linear regression model is applied. The correlation coefficient (r), y-intercept, and slope are reported. A correlation coefficient of >0.999 is typically expected for assay methods [28] [29].
- Range: The range is validated by demonstrating that the method meets the acceptance criteria for accuracy, precision, and linearity at the extremes and within the interval.
Table 1: Summary of Core Validation Parameters and Protocols
| Parameter | Experimental Methodology | Key Acceptance Criteria |
|---|---|---|
| Specificity | Analyze stressed samples; check peak purity via PDA or MS; measure resolution from closest eluting peak. | No co-elution; peak purity passes; resolution >1.5 [29]. |
| Accuracy | Analyze replicate samples (n≥9) at three concentration levels; calculate % recovery. | Mean recovery of 98-102% (for assay) [28] [29]. |
| Precision | Analyze homogeneous samples multiple times for repeatability; involve different analysts/days for intermediate precision. | %RSD ≤ 1.5% (for repeatability of assay) [28] [29]. |
| Linearity | Analyze a minimum of 5 concentrations across the specified range; perform linear regression. | Correlation coefficient (r) > 0.999 [28] [29]. |
| Range | Demonstrate that accuracy, precision, and linearity are acceptable across the entire range (e.g., 80-120% of target). | Meets all criteria for accuracy, precision, and linearity at the range limits [30]. |
Experimental Protocols for Key Validation Activities
This section provides detailed workflows for two fundamental validation experiments.
Protocol for a Method Comparison Study
When validating a new method (test method), it is often compared against an established one. This is critical for assessing systematic error or bias [32] [33].
- Selection of Comparative Method: Ideally, a well-characterized reference method should be used. If using a routine method, any large discrepancies must be interpreted with caution [32].
- Sample Selection: A minimum of 40 different patient specimens is recommended. These should be carefully selected to cover the entire working range of the method [32].
- Experimental Execution: Each specimen is analyzed by both the test and comparative methods. Analysis should be performed over a minimum of 5 different days to account for run-to-run variability. Specimens should be analyzed by both methods within a short time frame (e.g., two hours) to ensure stability [32].
- Data Analysis:
- Graphical Analysis: Use a Bland-Altman plot, where the x-axis is the average of the two methods and the y-axis is the difference between them (test minus comparative). This helps visualize bias and its consistency across the concentration range [33].
- Statistical Analysis: Calculate the average difference (bias) and the standard deviation of the differences. The limits of agreement are defined as Bias ± 1.96 × SD [33]. For data covering a wide range, linear regression (Y = a + bX) is used to estimate proportional and constant error [32].
The diagram below illustrates the logical workflow for this experiment.
Figure 1: Workflow for a Method Comparison Experiment
Protocol for a Robustness Evaluation
Robustness is the capacity of a method to remain unaffected by small, deliberate variations in method parameters [30] [29].
- Identify Key Parameters: Determine critical method variables (e.g., mobile phase pH, composition, column temperature, flow rate, different columns).
- Experimental Design: A bracketing approach is used, where each parameter is varied slightly around the specified optimum value while keeping others constant.
- Execution: A standard sample (often at 100% concentration) is analyzed under each varied condition.
- Assessment: Monitor the impact on critical performance attributes, such as resolution from a critical pair, tailing factor, and theoretical plates. The method is considered robust if these attributes remain within acceptance criteria despite the variations [30].
Comparative Analysis: A Case Study on Metoprolol Tartrate Assay
A 2024 study provides an excellent comparative analysis of two analytical techniques for quantifying Metoprolol Tartrate (MET) in pharmaceuticals: Ultra-Fast Liquid Chromatography with DAD detection (UFLC-DAD) and UV-Spectrophotometry [34]. This case study highlights the practical trade-offs between different analytical approaches.
Experimental Overview: Both methods were optimized and fully validated according to ICH guidelines. The UFLC-DAD method involved chromatographic separation, while the spectrophotometric method measured absorbance directly at 223 nm. The methods were compared based on their validation results and an assessment of their environmental impact using the Analytical GREEnness (AGREE) metric [34].
Table 2: Comparison of UFLC-DAD and UV-Spectrophotometry for Drug Assay
| Validation Parameter | UFLC-DAD Method | UV-Spectrophotometry Method |
|---|---|---|
| Specificity | High (Separation of analyte from excipients) [34] | Lower (Potential interference from excipients; cannot resolve mixtures) [34] |
| Linearity Range | Wider dynamic range [34] | Limited to a narrower range of concentrations [34] |
| Sensitivity (LOD/LOQ) | Higher sensitivity (Lower LOD and LOQ) [34] | Lower sensitivity (Higher LOD and LOQ) [34] |
| Operation & Cost | Complex operation, higher cost, longer analysis time [34] | Simple operation, low cost, rapid analysis [34] |
| Sample Consumption | Lower sample volume required [34] | Larger sample volume needed for analysis [34] |
| Environmental Impact | Lower greenness score [34] | Higher greenness score [34] |
Conclusion of the Case Study: The study concluded that the UFLC-DAD method was superior for specificity, sensitivity, and application across different dosage strengths. However, for the routine quality control of a single dosage form where specificity was not a primary concern, the UV-spectrophotometric method offered a valid, cost-effective, and greener alternative [34]. This demonstrates that the "best" method depends on the intended application and available resources.
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key materials and reagents essential for conducting robust analytical method validation, particularly for chromatographic assays.
Table 3: Essential Research Reagent Solutions for Analytical Validation
| Item | Function / Purpose |
|---|---|
| High-Purity Reference Standard | Serves as the benchmark for accuracy and linearity testing; its accepted concentration is the "true value" [29]. |
| Placebo/Excipient Blend | Used in specificity and accuracy experiments to confirm the absence of interference from non-active components [29]. |
| Forced Degradation Samples | Stressed samples (acid, base, oxidative, thermal, photolytic) used to demonstrate the specificity of a stability-indicating method [29]. |
| Mobile Phase Components | High-purity solvents and buffers are critical for achieving robust and reproducible chromatographic separation. |
| System Suitability Test Solutions | A reference preparation used to verify that the chromatographic system is performing adequately before and during validation runs [28] [29]. |
| Bergamottin | Bergamottin, MF:C21H22O4, MW:338.4 g/mol |
| Valone | Valone, CAS:145470-90-2, MF:C14H14O3, MW:230.26 g/mol |
In the realm of pharmaceutical development, controlling impurities is a fundamental aspect of ensuring drug safety and efficacy. The International Council for Harmonisation (ICH) guidelines Q2(R2) and Q14 emphasize that analytical procedures should be validated for their intended use, particularly for the detection and quantification of very low levels of impurities and degradation products [35]. Within this framework, the Limit of Detection (LOD) and Limit of Quantitation (LOQ) are two pivotal performance characteristics that define the lowest concentrations at which an analyte can be reliably detected or quantified, respectively [36] [37]. Establishing these limits is not merely a regulatory checkbox; it is a critical exercise that defines the capability and limitations of an analytical method, ensuring it is "fit for purpose" for drug stability testing and impurity profiling [36] [38]. This guide provides a practical comparison of the methodologies for determining LOD and LOQ, underpinned by experimental protocols and data relevant to researchers and drug development professionals.
Fundamental Concepts and Definitions
Understanding the distinct meanings of LOD and LOQ is essential for their correct application.
Limit of Detection (LOD): The LOD is the lowest concentration of an analyte that can be detected—but not necessarily quantified as an exact value—by the analytical procedure [39]. At this level, the analyte's signal can be distinguished from the background noise with a stated confidence level, typically 99% [39]. It is the point of decision, answering the question: "Is the analyte present or not?"
Limit of Quantitation (LOQ): The LOQ is the lowest concentration of an analyte that can be quantitatively determined with acceptable precision (repeatability) and accuracy (trueness) under stated experimental conditions [36] [37]. While the LOD confirms presence, the LOQ ensures that the numerical value generated is reliable enough for making informed decisions.
A third related term, the Limit of Blank (LoB), is often used as a statistical foundation. The LoB is the highest apparent analyte concentration expected to be found when replicates of a blank sample (containing no analyte) are tested [36]. The relationships and evolution from blank to detection to quantitation are visually summarized in the following workflow.
Methodological Comparison: How to Determine LOD and LOQ
There are several established approaches for determining LOD and LOQ, each with its own advantages and typical applications. The choice of method depends on factors such as the nature of the analytical technique, regulatory requirements, and the stage of method development.
Standard Deviation-Based Approaches
This approach leverages the statistical properties of the blank or the calibration curve and is widely recognized by IUPAC and other regulatory bodies [39] [40].
Table 1: Standard Deviation and Slope Methods for LOD/LOQ Calculation
| Method | Formula | Key Requirements | Typical Application |
|---|---|---|---|
| Based on Blank SD | LOD = Meanblank + 3(SDblank) [41]LOQ = Meanblank + 10(SDblank) [41] | Replicate measurements (n=10-20) of a blank sample [41]. | General use, especially when a suitable blank matrix is available. |
| Based on Calibration Curve | LOD = 3.3 * σ / S [37]LOQ = 10 * σ / S [37] | σ = Standard deviation of the responseS = Slope of the calibration curve. | Instrumental methods where a calibration curve is constructed. Recommended by ICH Q2(R1) [37]. |
| CLSI EP17 Protocol | LOD = LoB + 1.645(SD_low concentration sample) [36] | Requires data from both blank samples and a low-concentration sample. | Clinical and biological assays; provides a high degree of statistical confidence [36]. |
Signal-to-Noise Ratio and Visual Assessment
For many instrumental techniques, particularly chromatography, simpler, more empirical methods are often employed.
- Signal-to-Noise Ratio (S/N): This is a practical, widely used approach, especially in chromatography. The LOD is generally accepted as a S/N of 3:1, while the LOQ is defined as a S/N of 10:1 [37]. The "noise" is the baseline signal in the absence of the analyte, and the "signal" is the measured response of the analyte at low concentration.
- Visual Examination: This non-instrumental method involves analyzing samples with known concentrations of the analyte and establishing the minimum level at which the analyte can be detected (for LOD) or quantified (for LOQ) through visual inspection. Examples include estimating the minimum concentration of an antibiotic that inhibits bacterial growth or the endpoint of a titration [37].
Experimental Protocols and Workflow
A robust, step-by-step workflow is crucial for generating reliable LOD and LOQ values. The following protocol synthesizes recommendations from multiple guidelines, with a focus on complex samples [40].
Protocol for LOD/LOQ Determination via Calibration Curve
Step 1: Preparation of Solutions
- Prepare a blank sample, which contains all components of the sample matrix except the analyte of interest.
- Prepare a minimum of 5-8 calibration standards at low concentrations, ideally spanning a range that brackets the expected LOD and LOQ. Using multiple calibration curves is recommended for higher robustness [37] [40].
Step 2: Data Acquisition and Curve Construction
- Analyze the calibration standards in replicate (e.g., J=3-5 replicates per concentration).
- Construct a calibration curve by plotting the analyte response (y) against the nominal concentration (x). Perform ordinary least-squares (OLS) regression to obtain the slope (S) and the residual standard deviation (sy/x) or the standard deviation of the y-intercept [37] [40].
Step 3: Calculation
- Calculate the LOD and LOQ using the formulas from Table 1:
- LOD = 3.3 * sy/x / S
- LOQ = 10 * sy/x / S
Step 4: Verification
- Prepare and analyze independent samples at the calculated LOD and LOQ concentrations.
- For LOD, the detection should be reliable in approximately 95% of the tests (≤5% false negative rate) [36].
- For LOQ, the results should demonstrate a precision (expressed as %RSD) of ≤20% and an accuracy (expressed as % bias) of ±20% (or other pre-defined criteria based on method requirements) [36].
Table 2: The Scientist's Toolkit: Essential Reagents and Materials
| Item | Function / Explanation |
|---|---|
| Analyte-Free Blank Matrix | A critical reagent that mimics the sample matrix without the analyte. Used to estimate baseline noise and the Limit of Blank (LoB) [36] [40]. |
| Certified Reference Standard | A high-purity material with a known concentration of the analyte. Essential for preparing accurate calibration standards [38]. |
| Calibration Standards | A series of solutions with known analyte concentrations, used to establish the relationship between instrument response and analyte amount [40]. |
| Quality Control (QC) Samples | Independent samples prepared at concentrations near the LOD and LOQ. Used to verify the performance of the established limits [36]. |
| HPLC/UPLC System with Detector | Common instrumental platforms for impurity analysis. The detector's inherent noise level is key for S/N determinations [37] [42]. |
The determination of LOD and LOQ is a cornerstone of the Analytical Procedure Lifecycle (APL), as outlined in USP general chapter <1220> and the emerging ICH Q2(R2) and Q14 guidelines [35]. The overarching principle is that methods must be validated for their intended purpose, a requirement enshrined in GMP regulations (e.g., 21 CFR 211.194(a)(2)) [35]. For impurity methods, this means having a clearly defined Analytical Target Profile (ATP) that specifies the required detection and quantification capabilities.
In conclusion, there is no single "correct" method for establishing LOD and LOQ. The most appropriate strategy depends on the analytical technique, the nature of the sample matrix, and the specific regulatory context. Whether using the statistical rigor of the standard deviation approach, the practical convenience of the signal-to-noise ratio, or the comprehensive protocol of CLSI EP17, the ultimate goal remains the same: to ensure your analytical method is capable of reliably detecting and quantifying impurities, thereby safeguarding patient safety and ensuring product quality. By systematically comparing and applying these methodologies, scientists can generate defensible data that meets the stringent demands of modern pharmaceutical development.
In the pharmaceutical industry, demonstrating the reliability of analytical methods is a fundamental requirement for drug approval and quality control. Method validation provides assurance that an analytical procedure is suitable for its intended purpose and can generate reliable, reproducible results over the entire lifespan of a pharmaceutical product. Within this framework, robustness testing and system suitability testing (SST) serve as complementary pillars supporting data integrity, particularly for long-term stability studies mandated by ICH guidelines.
Robustness evaluates the method's capacity to remain unaffected by small, deliberate variations in method parameters, establishing a method's inherent reliability under normal operational fluctuations. System suitability testing serves as the ongoing verification that the analytical system—comprising instrument, reagents, column, and analyst—is functioning correctly each time the method is executed. For long-term studies spanning months or years, where methods must detect subtle changes in product quality attributes, both elements are indispensable for ensuring that observed changes truly reflect product stability rather than analytical variability.
This guide examines the experimental approaches, acceptance criteria, and practical implementation of these critical validation components, providing a structured comparison for scientists designing robust stability-indicating methods.
System Suitability Testing: The Daily Performance Check
Core Principles and Purpose
System suitability testing (SST) is a formal, prescribed test of an entire analytical system's performance conducted prior to sample analysis. It verifies that the specific instrument, on a specific day, is capable of generating high-quality data according to the validated method's requirements [43]. Think of SST not as a redundant check, but as the final gatekeeper of data quality—a proactive quality assurance measure that confirms fitness-for-purpose immediately before a batch of samples is analyzed [43]. According to regulatory perspectives, if SST results fall outside acceptance criteria, the analytical run may be invalidated, emphasizing its critical role in decision-making [44].
Key SST Parameters and Acceptance Criteria
SST evaluates chromatographic performance through several key parameters, each with defined acceptance criteria established during method validation. The table below summarizes the most critical parameters and their typical acceptance criteria for HPLC methods in pharmaceutical analysis.
Table 1: Key System Suitability Test Parameters and Acceptance Criteria
| Parameter | Definition | Typical Acceptance Criteria | Purpose in Stability Testing |
|---|---|---|---|
| Resolution (Rs) | Measure of separation between two adjacent peaks [44] | Minimum resolution between API and nearest impurity/degredant [44] | Ensures degradant peaks are separated from API for accurate quantification |
| Tailing Factor (Tf) | Measure of peak symmetry [44] | Typically ≤ 2.0 [44] | Prevents integration errors that could misrepresent degradation levels |
| Theoretical Plates (N) | Measure of column efficiency [43] | Method-specific minimum | Confirms column performance has not deteriorated significantly |
| Relative Standard Deviation (%RSD) | Measure of injection precision/repeatability [44] | Typically < 1.0-2.0% for replicate injections [44] [43] | Ensures system precision for detecting small changes over time |
| Signal-to-Noise Ratio (S/N) | Measure of detector sensitivity and system noise [43] | Typically ≥ 10 for quantification (LOQ) [45] | Verifies system can detect and quantify low-level degradants |
Regulatory Framework and Recent Updates
SST requirements are codified in various pharmacopeial standards. The United States Pharmacopeia (USP) General Chapter <621> provides comprehensive guidance on chromatography system suitability, with an updated version effective May 1, 2025, that includes refined definitions for system sensitivity and peak symmetry [45]. The European Pharmacopoeia (Chapter 2.2.46) similarly outlines requirements, with recent clarifications that SST criteria from related substances tests must be applied even when cross-referenced in assay procedures [46].
A crucial regulatory distinction is that SST is not a substitute for Analytical Instrument Qualification (AIQ). While AIQ ensures instruments are fundamentally fit-for-purpose, SST confirms the entire system works correctly for a specific method on the day of analysis [44]. Understanding this hierarchy—where General Notices override general chapters, and monographs override both—is essential for proper implementation [45].
Robustness Testing: Establishing Method Resilience
Objectives and Experimental Design
Robustness testing systematically evaluates a method's reliability when subjected to small, deliberate variations in operational parameters. The objective is to identify critical parameters that must be carefully controlled and to establish the method's operable range before it is transferred to quality control laboratories or deployed in long-term studies. A robust method should be insensitive to minor fluctuations that normally occur between instruments, analysts, laboratories, or across time.
The experimental design for robustness testing typically involves varying one parameter at a time while keeping others constant, allowing isolation of individual effects. For chromatographic methods, common variations include mobile phase pH (±0.2 units), organic composition (±2-3%), flow rate (±10%), column temperature (±5°C), and different columns (same type but different batches or brands). The recently introduced Stability Toolkit for the Appraisal of Bio/Pharmaceuticals' Level of Endurance (STABLE) provides a standardized framework for assessing drug stability under various stress conditions, employing a color-coded scoring system to quantify and compare stability across different APIs [47].
Experimental Protocol for HPLC Robustness Testing
The following workflow illustrates a systematic approach to robustness testing for stability-indicating HPLC methods:
Data Interpretation and Acceptance Criteria
In robustness testing, method performance is evaluated against the same system suitability parameters used in daily testing (resolution, tailing, precision, etc.). The method is considered robust if all critical peak pairs maintain resolution above the minimum requirement, tailing factors remain within specification, and precision meets acceptance criteria across all tested variations.
Experimental data from a validated RP-HPLC method for mesalamine quantification demonstrates this principle. The method maintained excellent precision (intra-day and inter-day %RSD < 1.0%) and accuracy (recoveries between 99.05% and 99.25%) despite intentional variations in method parameters, with all robustness variations showing %RSD below 2% [48]. This confirms the method's resilience to normal operational fluctuations, a critical attribute for long-term studies where consistency is paramount.
Comparative Analysis: Complementary Roles in Long-Term Studies
Functional Relationships and Implementation Timing
While both robustness testing and system suitability testing ensure method reliability, they serve distinct purposes and are implemented at different stages of the method lifecycle. The following diagram illustrates their complementary relationship and position within the overall method validation framework:
Direct Comparison of Characteristics
The table below provides a structured comparison of robustness testing and system suitability testing, highlighting their distinct characteristics and complementary roles in ensuring method reliability for long-term stability studies.
Table 2: Comparative Analysis: Robustness Testing vs. System Suitability Testing
| Characteristic | Robustness Testing | System Suitability Testing |
|---|---|---|
| Primary Objective | Establish method resilience to parameter variations [48] | Verify analytical system performance on day of use [43] |
| Implementation Timing | Once, during method validation | Before each analytical run [43] [49] |
| Varied Parameters | Multiple method parameters (pH, temperature, flow rate, etc.) [48] | Fixed method parameters |
| Measured Output | Method performance under varied conditions | System performance under standardized conditions |
| Regulatory Reference | ICH Q2(R2) [48] | USP <621> [44], Ph. Eur. 2.2.46 [46] |
| Impact on Study | Defines method control strategy | Determines if run can proceed [43] |
| Key Acceptance Criteria | Consistent performance across variations | Resolution > minimum, %RSD < limit, tailing factor ≤ 2.0 [44] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of robustness and system suitability testing requires specific high-quality materials and reagents. The following table details essential solutions and their functions in experimental protocols for method validation.
Table 3: Essential Research Reagent Solutions for Validation Studies
| Reagent/Material | Function in Experiments | Specific Application Example |
|---|---|---|
| Pharmaceutical Reference Standards | System suitability testing and calibration [43] | USP compendial standards for SST verification [44] |
| HPLC Grade Solvents | Mobile phase preparation for consistent chromatography [48] | Methanol and water for reverse-phase HPLC (60:40 v/v) [48] |
| Buffer Solutions | Control of mobile phase pH for robustness testing [48] | Variation of pH ±0.2 units in robustness studies |
| Certified HPLC Columns | Column performance verification during AIQ and SST [44] | C18 column (150 mm × 4.6 mm, 5 μm) for separation [48] |
| Forced Degradation Reagents | Generation of degradation products for specificity validation [48] | 0.1N HCl, 0.1N NaOH, 3% Hâ‚‚Oâ‚‚ for stress testing [48] |
| System Suitability Test Mixtures | Verification of chromatographic system performance [49] | Resolution solutions containing API and key impurities |
| (+-)-Methionine | (+-)-Methionine, CAS:26062-47-5, MF:C5H11NO2S, MW:149.21 g/mol | Chemical Reagent |
| Sterigmatocystine | Sterigmatocystine, MF:C18H12O6, MW:324.3 g/mol | Chemical Reagent |
Robustness testing and system suitability testing form an indispensable partnership in ensuring the reliability of analytical data generated throughout pharmaceutical product lifecycles. While robustness testing establishes a method's inherent resilience to normal operational variations during validation, system suitability testing provides ongoing verification of proper system performance with each use. For long-term stability studies—where methods must distinguish subtle product changes from analytical variability over extended periods—this dual approach provides the foundation for defensible shelf-life determinations and regulatory compliance. By implementing both elements with scientific rigor, drug development professionals can generate high-quality stability data that accurately reflects product performance and ensures patient safety.
In the realm of pharmaceutical development, robust analytical methods are indispensable for ensuring drug safety, efficacy, and quality. High-performance liquid chromatography (HPLC) and enzyme-linked immunosorbent assay (ELISA) represent two pillars of analytical science, serving distinct but equally crucial roles in the characterization and monitoring of pharmaceutical compounds. HPLC stands as the gold standard for analyzing and purifying molecular components in solutions, particularly for small molecule drugs [50]. In contrast, ELISA remains widely regarded as the gold standard for biomarker validation and clinical diagnostics owing to its exceptional specificity, sensitivity, and ability to quantify proteins in biological samples, making it particularly valuable for biological drugs [51].
The International Council for Harmonisation (ICH) Q2(R2) guideline provides the foundational framework for validating analytical procedures, offering guidance on deriving and evaluating various validation tests for each analytical procedure [12]. This guideline applies to new or revised analytical procedures used for release and stability testing of commercial drug substances and products, both chemical and biological/biotechnological [12]. As the landscape of analytical science evolves with technological advancements, the rigorous application of these validation principles becomes increasingly critical for maintaining regulatory compliance and ensuring patient safety.
This comparison guide examines the application of validation principles to HPLC for small molecules and ELISA for biologics through recent case studies, providing drug development professionals with objective performance comparisons and detailed methodological approaches to inform their analytical strategies.
Analytical Method Validation: Principles and Regulatory Framework
The ICH Q2(R2) guideline presents a comprehensive discussion of elements for consideration during the validation of analytical procedures included as part of registration applications submitted within ICH member regulatory authorities [12]. The guideline provides a collection of terms and their definitions, along with recommendations on how to derive and evaluate the various validation tests for each analytical procedure [12]. This guidance is directed to the most common purposes of analytical procedures, such as assay/potency, purity, impurities, identity, and other quantitative or qualitative measurements [12].
A recent gap analysis toolkit identified 56 specific omissions, expansions, and additions between the previous Q2(R1) and the current Q2(R2) guidelines, highlighting the evolving nature of analytical method validation standards [52]. Regulatory bodies increasingly advocate for a tailored approach to biomarker validation, emphasizing that it should be aligned with the specific intended use of the biomarker rather than relying on a one-size-fits-all method [51]. This principle extends to all analytical methods, whether for small molecules or biologics.
The close relationship between analytical method development and validation is formally recognized in the ICH framework, with Q14 introducing comprehensive guidance on the development of analytical methods, while Q2(R2) focuses on validation [52]. This integrated approach ensures that validation considerations are incorporated from the earliest stages of method development, leading to more robust and reliable analytical procedures.
Case Study 1: HPLC Method Validation for Small Molecules
In Silico HPLC Method Development and Validation
Traditional HPLC method development is notoriously material- and time-consuming, often relying on trial-and-error experimental campaigns [50]. A groundbreaking 2025 study demonstrated a data-driven methodology to predict molecule retention factors as a function of mobile phase composition without the need for any new experiments, solely relying on molecular descriptors obtained via simplified molecular input line entry system (SMILES) string representations of molecules [50].
This innovative approach combines quantitative structure-property relationships (QSPR) using molecular descriptors to predict solute-dependent parameters in linear solvation energy relationships (LSER) and linear solvent strength (LSS) theory [50]. The research demonstrated the potential of this computational methodology using experimental data for retention factors of small molecules made available by the research community [50]. This method can be adopted directly to predict elution times of molecular components; however, in combination with first-principle-based mechanistic transport models, the method can also be employed to optimize HPLC methods in-silico [50].
Table 1: Key Validation Parameters for the In Silico HPLC Prediction Model
| Validation Parameter | Approach | Result |
|---|---|---|
| Predictive Accuracy | Comparison of predicted vs. experimental retention factors | High correlation for small molecules |
| Model Robustness | Application across diverse molecular structures | Maintained predictive power |
| Application Scope | Testing with various mobile phase compositions | Effective across different conditions |
| Methodology | QSPR with molecular descriptors via SMILES strings | Successfully predicted solute-dependent parameters |
Experimental HPLC Validation with Advanced Column Technologies
Recent innovations in HPLC column technology have significantly enhanced method validation capabilities. The 2025 review of HPLC innovations highlighted several advancements supporting more robust method validation [53]:
Advanced Materials Technology introduced the Halo Inert, an RPLC column that integrates passivated hardware to create a metal-free barrier between the sample and the stainless-steel components [53]. This feature is particularly advantageous for phosphorylated compounds and metal-sensitive analytes because it helps to prevent adsorption to metal surfaces [53]. The main benefits include enhanced peak shape and improved analyte recovery, making it especially useful in applications requiring minimal metal interaction [53].
Fortis Technologies Ltd. manufactures the Evosphere Max chromatography columns, which use inert hardware to enhance peptide recovery and sensitivity [53]. These columns are made with monodisperse porous silica particles and come in three different particle sizes (1.7 μm, 3 μm, and 5 μm) with a 100-Å pore size [53]. They are designed for use in various chromatography applications, providing improved performance over traditional products, particularly for metal-chelating compounds [53].
Restek Corporation launched the Restek Inert HPLC Columns, which are designed for RPLC and built on totally porous, conventional silica particles with polar-embedded alkyl and modified C18 stationary phases [53]. These products are particularly suited for the analysis of chelating PFAS and pesticide compounds, offering improved response for metal-sensitive analytes [53]. A key feature is the use of inert hardware, enhancing performance by minimizing unwanted interactions [53].
Machine Learning for Automated HPLC Anomaly Detection
A 2025 study presented a novel machine learning framework for automated anomaly detection in HPLC experiments conducted in a cloud lab, specifically targeting air bubble contamination—a common yet challenging issue that typically requires expert analytical chemists to detect and resolve [54]. By leveraging active learning combined with human-in-the-loop annotation, the researchers trained a binary classifier on approximately 25,000 HPLC traces [54]. Prospective validation demonstrated robust performance, with an accuracy of 0.96 and an F1 score of 0.92, suitable for real-world applications [54].
The workflow comprised three major steps: (1) Initialization of Training Data, (2) ML Model Building via Human-in-the-Loop Approach, and (3) Deployment and Performance measurement of the final ML Model [54]. Beyond anomaly detection, the system can serve as a sensitive indicator of instrument health, outperforming traditional periodic qualification tests in identifying systematic issues [54]. The framework is protocol-agnostic, instrument-agnostic, and vendor-neutral, making it adaptable to various laboratory settings [54].
Diagram 1: Comprehensive HPLC Method Validation Workflow. This workflow integrates in silico prediction, advanced column selection, experimental validation, machine learning anomaly detection, and regulatory compliance checkpoints.
Case Study 2: ELISA Method Validation for Biologics
Comparative Validation of ELISA with Advanced Immunoassays
A 2024 unicentric prospective observational study compared the infliximab, adalimumab, vedolizumab, and ustekinumab trough levels and anti-adalimumab and anti-infliximab antibodies concentrations obtained when using a chemiluminescent instrument (i-TRACK) and an ELISA instrument (TRITURUS) [55]. Linear regression, Pearson or Spearman tests, Bland–Altman plots, and the Cohen kappa test were applied for every sample [55]. The correlation was excellent for both assays in the measurement of all drug concentrations [55]. However, values were generally lower when measured using i-TRACK than when using TRITURUS, especially when the values were high [55]. Both techniques proved valuable in clinical practice for monitoring adalimumab and infliximab drug concentration, but the results were modest for ustekinumab and vedolizumab, indicating that caution is recommended and further research is needed [55].
A 2025 study compared the measurement of anti-TNF biologics in serum samples of pediatric patients using ELISA versus a rapid and automated fluorescence-based lateral flow immunoassay (AFIAS) [56]. Spearman's correlation coefficients (rho) were 0.98 for IFX and 0.83 for ADL [56]. The calculated % bias was −14.09 for IFX and 15.79 for ADL [56]. The inter-rater agreement showed a "substantial" and a "moderate" agreement for IFX and ADL, respectively [56]. The authors concluded that the AFIAS assay has an accuracy and analytical performance comparable to that of the ELISA method used for therapeutic drug monitoring of IFX and ADL [56].
Table 2: Comparison of Immunoassay Platforms for Biologics Monitoring
| Platform | Analysis Time | Throughput | Correlation with ELISA | Key Advantages |
|---|---|---|---|---|
| Traditional ELISA | 3-5 hours [56] | Batch processing required | Reference method | Established gold standard, wide validation |
| Chemiluminescence (i-TRACK) | ~30 minutes [55] | Single samples | Excellent for IFX, ADA; modest for VED, UST [55] | Automated, standardized, no sample pooling needed [55] |
| Lateral Flow (AFIAS) | 20 minutes [56] | Single samples | 0.98 for IFX; 0.83 for ADL [56] | Rapid results, minimal processing steps [56] |
| Electrochemiluminescence (MSD) | Varies | Multiplexed | Up to 100x greater sensitivity than ELISA [51] | Broad dynamic range, multiplexing capability [51] |
Validation of Rapid ELISA Technologies
Innovations in ELISA technology have addressed several limitations of traditional methods. Traditional ELISAs take more than three hours and require multiple wash steps, but newer kits can generate data in just 90 minutes with only a single wash step [57]. These improvements significantly enhance workflow efficiency, particularly for researchers processing large sample volumes [57].
The performance of these rapid assays depends heavily on the quality of recombinant antibodies, which undergo rigorous validation using biophysical quality control to confirm their identity at the molecular level [57]. In sandwich ELISA formats, substantial effort is dedicated to selecting optimal antibody pairs for each assay to ensure robustness, reproducibility, and guaranteed batch-to-batch consistency [57]. Each assay is fully validated in complex biological samples, giving researchers confidence that their target will be accurately detected in real-world experiments [57].
Emerging Technologies Beyond Traditional ELISA
While ELISA remains the gold standard for biomarker validation, advanced technologies like liquid chromatography tandem mass spectrometry (LC-MS/MS) and Meso Scale Discovery (MSD) offer enhanced precision and sensitivity for biomarker analysis [51]. MSD, utilizing electrochemiluminescence (ECL) detection, provides up to 100 times greater sensitivity than traditional ELISA, enabling the detection of lower abundance proteins and a broader dynamic range [51]. LC-MS/MS also surpasses ELISA in sensitivity, making it a useful technique for detecting low-abundance species [51].
MSD's U-PLEX multiplexed immunoassay platform allows researchers to design custom biomarker panels and measure multiple analytes simultaneously within a single sample [51]. By enabling the simultaneous analysis of multiple biomarkers in small sample volumes, MSD's assays enhance efficiency in biomarker research, especially when dealing with complex diseases or therapeutic responses [51]. LC-MS/MS goes even further, allowing the analysis of hundreds to thousands of proteins in a single run [51].
Diagram 2: Comprehensive Immunoassay Method Validation Workflow. This workflow outlines the key stages in developing and validating immunoassays for biological drugs, from initial format selection through regulatory compliance.
Comparative Analysis: HPLC vs. ELISA Validation Approaches
Method Development and Optimization Strategies
The approaches to method development and optimization differ significantly between HPLC for small molecules and ELISA for biologics, reflecting their distinct technological foundations and application domains.
HPLC method development has traditionally relied on experimental campaigns driven by experience and one-variable-at-a-time strategies [50]. However, computational approaches are increasingly being adopted to minimize costly and time-consuming experiments [50]. The linear solvent strength (LSS) theory offers a simple way to describe how the mobile phase composition alters the solute adsorption and retention times [50]. As machine learning and artificial intelligence become more powerful and integrated into daily workflows, in-silico HPLC approaches will only become more important [50].
In contrast, ELISA development focuses heavily on antibody selection and validation. The success of sandwich ELISA formats depends on identifying optimal antibody pairs that bind to different sites on the target protein without interfering with each other [57]. Rigorous validation using biophysical quality control confirms antibody identity at the molecular level, ensuring robustness, reproducibility, and batch-to-batch consistency [57].
Validation Parameters and Acceptance Criteria
While both HPLC and ELISA methods must comply with ICH Q2(R2) guidelines, the specific validation parameters and acceptance criteria vary based on their respective applications and technological characteristics.
For HPLC methods, key validation parameters include peak shape, retention time reproducibility, column efficiency, and resolution between analytes [53] [50]. The development of new columns for separating small molecules consistently focuses on enhancing peak shapes for difficult molecules, improving column efficiency, extending the usable pH range, and providing improved and alternative selectivity [53].
For ELISA methods, validation parameters include specificity, sensitivity, dynamic range, and reproducibility across different sample matrices [57] [51]. The narrow dynamic range of traditional ELISA compared to some multiplexed immunoassays represents a significant limitation that advanced technologies aim to address [51]. Reproducibility is particularly crucial for applications requiring comparison of data across numerous samples or experimental conditions [57].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for HPLC and ELISA Validation
| Category | Product/Technology | Key Features | Application in Validation |
|---|---|---|---|
| HPLC Columns | Halo Inert [53] | Passivated hardware, metal-free barrier | Enhanced peak shape, improved recovery for metal-sensitive analytes |
| HPLC Columns | Evosphere Max [53] | Inert hardware, monodisperse porous particles | Enhanced peptide recovery and sensitivity |
| HPLC Guard Columns | Raptor Inert [53] | Superficially porous particles, inert hardware | Protection of analytical columns, improved response for metal-sensitive compounds |
| ELISA Platforms | SimpleStep ELISA [57] | Single wash step, 90-minute protocol | Rapid validation with maintained specificity and sensitivity |
| ELISA Antibodies | Validated antibody pairs [57] | Biophysical QC, batch-to-batch consistency | Ensured robustness and reproducibility across experiments |
| Alternative Immunoassays | MSD U-PLEX [51] | Multiplexing capability, electrochemiluminescence | Simultaneous validation of multiple biomarkers, enhanced sensitivity |
| Reference Materials | Certified reference standards | Documented purity and traceability | Method calibration and accuracy verification |
| Cynaroside | Cynaroside | High-purity Cynaroside, a bioactive flavonoid for research use only (RUO). Explore its applications in oncology, neurology, and metabolic disease studies. Inhibits key signaling pathways. | Bench Chemicals |
| Aphidicolin | Aphidicolin, CAS:69926-98-3, MF:C20H34O4, MW:338.5 g/mol | Chemical Reagent | Bench Chemicals |
The case studies presented demonstrate that both HPLC for small molecules and ELISA for biologics continue to evolve with significant advancements in validation methodologies. For HPLC, the integration of in silico prediction models, advanced column technologies, and machine learning for anomaly detection represents a transformative approach to method development and validation [54] [50]. For ELISA and related immunoassays, the emergence of rapid platforms with performance comparable to traditional methods offers opportunities for enhanced efficiency in therapeutic drug monitoring and biomarker validation [55] [56].
The selection of an appropriate analytical platform must consider the specific requirements of the intended application, including necessary sensitivity, dynamic range, throughput, and regulatory compliance needs. While advanced technologies like CLIA, MSD, and LC-MS/MS offer compelling advantages in specific scenarios, traditional ELISA and HPLC remain robust and well-validated choices for many applications [55] [51].
As regulatory standards continue to evolve under frameworks like ICH Q2(R2), the implementation of rigorously validated analytical methods that are tailored to their intended use becomes increasingly critical [12] [51]. By understanding the comparative performance characteristics and validation requirements of different analytical platforms, researchers and drug development professionals can make informed decisions that optimize both scientific rigor and operational efficiency in pharmaceutical development.
Navigating Challenges: Troubleshooting and Optimizing Methods for Complex Modalities
Common Pitfalls in Validating Methods for Biologics and Complex Products
Validating analytical methods is a cornerstone of ensuring the quality, safety, and efficacy of biologics and other complex products, such as advanced therapy medicinal products (ATMPs). Unlike small-molecule drugs, these products are characterized by inherent complexity and heterogeneity, which pose unique challenges for analytical scientists [58]. Method validation demonstrates that a procedure is suitable for its intended use and provides reliable data to support drug development and stability testing, in line with ICH guidelines [59]. However, navigating this process successfully requires an understanding of common pitfalls. This guide objectively compares validation challenges across different product types and provides detailed experimental protocols to help researchers avoid critical errors.
Understanding the Validation Landscape for Complex Products
The validation of analytical methods for biologics must account for their structural complexity, which arises from factors like large molecular size, intricate higher-order structures, and post-translational modifications [58]. This heterogeneity necessitates a panel of orthogonal analytical methods to fully characterize the product [58]. A key pitfall is attempting to apply a one-size-fits-all validation approach, particularly for novel modalities.
The Challenge of Product Complexity and Evolving Modalities
Biologics and ATMPs require methods that can evolve throughout the product lifecycle. For monoclonal antibodies (mAbs), some platform analytical technologies exist, lowering uncertainty [59]. In contrast, new molecule types, such as patient-specific cancer vaccines or antibody-drug conjugates, present greater hurdles because they may lack direct potency tests and require surrogate methods [59].
For ATMPs, including gene therapies, methods can be categorized by maturity, which directly impacts validation strategy [60] [61]:
- Fully Mature Assays: Examples include host cell protein (HCP) and host cell DNA testing. These are often kit-based and easier to validate.
- Assays Needing Development: Techniques like peptide mapping for post-translational modifications (PTMs) or size-exclusion chromatography (SEC) for aggregates require adaptation and special validation considerations for large molecules like AAV vectors [60] [61].
- Immature Assays: Techniques for assessing attributes like empty/full capsid ratio (e.g., analytical ultracentrifugation (AUC), cryo-electron microscopy) or potency are often not routine in GMP settings. They lack compliant software and require significant development, making validation a major challenge close to commercialization [60] [61].
Common Pitfalls and Comparative Analysis
A systematic analysis of common pitfalls reveals specific vulnerabilities across different product classes. The table below summarizes these challenges, providing a direct comparison to aid in risk assessment and planning.
Table 1: Common Pitfalls in Method Validation for Different Product Types
| Pitfall | Traditional Biologics (e.g., mAbs) | Advanced Therapies (ATMPs, e.g., AAV vectors) | Combination Products |
|---|---|---|---|
| Insufficient Method Robustness Testing | Modifying a mobile phase by 2% without understanding true method boundaries [59]. | High susceptibility to variability from complex biological starting materials and small batch sizes [60] [61]. | Must satisfy cGMP for both drug and device constituents (21 CFR Part 4); robustness includes device functionality [62]. |
| Inadequate Potency Assay Strategy | Relying on a single, non-mechanistic potency assay [59]. | Developing a potency assay that quantifies the complex mechanism of action (MoA) is a major obstacle; requires a phase-appropriate approach [60]. | Potency must be linked to the drug's primary mode of action within the combined product [62]. |
| Poor Sample & Reference Standard Management | Using uncharacterized or non-representative reference standards. | Extreme sample scarcity; lack of available reference materials making it difficult to prove method suitability [60] [61]. | Reference standards must be qualified for both the drug and its interaction with the delivery device. |
| Misjudged Validation Timeline & Resources | Compressed development timelines with insufficient consideration for method validation [59]. | Methods are often immature and require significant development, leading to re-validation and comparability studies [60]. | Regulatory pathway (PMA, 510(k), De Novo) impacts validation scope and timeline; misclassification causes delays [62]. |
| Overlooking Regulatory Communication | Assuming ICH Q2(R1) is solely sufficient without consulting biopharma-specific guidances like FDA's draft guidance or PDA TR57 [59]. | Lack of frequent dialogue with regulators on analytical strategy, especially given novel techniques and limited sample data [60] [61]. | Requires early engagement with FDA's Office of Combination Products (OCP) to determine lead center and pathway [62]. |
Experimental Data: The Impact of Incomplete Robustness Testing
Protocol for a Systematic Robustness Study: A robust method should withstand small, deliberate variations in method parameters. A common pitfall is verifying a narrow, pre-established parameter set rather than stress-testing to find true failure boundaries [59]. A systematic approach using Design of Experiments (DoE) is recommended.
- Identify Critical Parameters: Select method parameters that may influence results (e.g., pH of mobile phase, buffer concentration, column temperature, gradient time).
- Design the Experiment: Use a fractional factorial design to efficiently study the main effects and interactions of these parameters. For example, a study might investigate 6 factors at 2 levels each.
- Define Response Variables: Select critical performance characteristics as outputs (e.g., retention time, peak area, resolution).
- Execution: Perform the chromatographic runs as per the experimental design.
- Statistical Analysis: Analyze data using multiple linear regression to identify which parameters and interactions have a statistically significant effect on the responses.
Supporting Data: A hypothetical study on a SEC-HPLC method for protein aggregate analysis might yield the following results for the critical resolution factor:
Table 2: DoE Analysis of SEC-HPLC Method Robustness
| Factor | Effect on Resolution | P-Value | Conclusion |
|---|---|---|---|
| Buffer Concentration (+/- 5%) | 0.05 | 0.45 | Not Significant |
| Flow Rate (+/- 0.1 mL/min) | 0.12 | 0.08 | Not Significant |
| Column Temperature (+/- 2°C) | 0.45 | <0.01 | Significant |
| pH (+/- 0.1 units) | 0.08 | 0.15 | Not Significant |
This data reveals that column temperature is a critical method parameter that must be tightly controlled in the method procedure, whereas the other factors tested are less influential. Without a DoE approach, this key sensitivity might be missed, leading to method failure during transfer or routine use.
Detailed Experimental Protocols for Addressing Key Challenges
Protocol 1: Phase-Appropriate Potency Assay Validation for an ATMP
Potency assays for ATMPs with complex MoAs are a recognized hurdle. A phase-appropriate strategy is essential [60].
Objective: To validate a cell-based potency assay for a gene therapy vector that reflects its biological activity (e.g., transgene expression).
Materials:
- Test Articles: AAV vector samples (full, empty, partially filled capsids).
- Cell Line: A permissive cell line expressing the necessary receptor.
- Reference Standard: A well-characterized internal reference standard.
- Detection Reagents: Antibodies or dyes for detecting the transgene product (e.g., GFP, a specific protein).
Workflow:
- Cell Seeding: Plate cells in multi-well plates and culture until 70-80% confluent.
- Infection: Infect cells with a dilution series of the AAV vector and appropriate controls (e.g., negative control, reference standard).
- Incubation: Incubate for a defined period to allow for transgene expression.
- Detection: Quantify the transgene product using a suitable method (e.g., fluorescence for GFP, ELISA for a protein).
- Data Analysis: Generate a dose-response curve. Calculate relative potency by comparing the sample's EC50 to that of the reference standard.
Validation Parameters (Phase 3 Validation):
- Accuracy/Recovery: Spike known amounts of vector into a complex matrix; recovery should be 80-120%.
- Precision: Repeat the assay multiple times (inter-day, inter-analyst) to determine %RSD. For complex bioassays, an RSD of ≤25% may be acceptable.
- Specificity: Demonstrate that the signal is specific to the intended transgene product and that empty capsids do not produce a response.
- Linearity & Range: Establish the range over which the dose-response is linear and the potency can be calculated.
Diagram 1: Potency Assay Workflow
Protocol 2: Analytical Method Comparability Bridging Study
A major pitfall is failing to plan for method changes, which are common as products move from development to commercialization. When a method is improved or replaced, a comparability or bridging study is required [59] [60].
Objective: To demonstrate that a new, improved analytical method (e.g., a higher-resolution LC method) provides comparable results to the original method.
Materials:
- A set of representative samples (at least 6-10) that cover the expected range of product quality (e.g., different purity levels, stored under various conditions).
- Both the old and new analytical methods, fully operational.
- Statistical software for data analysis.
Workflow:
- Sample Selection: Select samples that are representative of the product and its variants.
- Blinded Analysis: Analyze all samples using both the old and new methods in a blinded and randomized order to avoid bias.
- Data Collection: Record the quantitative results for the key attribute(s) from both methods.
- Statistical Comparison: Use appropriate statistical tests to compare the data sets.
Validation Parameters & Data Analysis:
- Correlation Analysis: Perform simple linear regression (SLR) between the results from the two methods. A correlation coefficient (R²) > 0.95 is typically expected.
- SLR Equation: Y (New Method) = a * X (Old Method) + b
- Bland-Altman Plot: This is used to assess the agreement between two methods by plotting the differences between the two measurements against their averages. It helps identify any bias.
- Calculation: Difference = (New Method Result - Old Method Result); Average = (New Method Result + Old Method Result)/2
- Hypothesis Testing: Use a paired t-test to determine if there is a statistically significant difference between the mean values obtained by the two methods. A p-value > 0.05 indicates no significant difference.
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful development and validation of methods for complex products depend on critical reagents and materials. Proper management of these components is vital for data integrity.
Table 3: Key Research Reagent Solutions for Method Validation
| Reagent / Material | Function | Critical Management Consideration |
|---|---|---|
| Reference Standard | Serves as the primary benchmark for quantifying the analyte and calibrating the method. | Implement a two-tiered system (primary and working standards) with full characterization. Stability must be monitored over time [59]. |
| Critical Assay Reagents | Components essential for the method's function (e.g., enzymes, antibodies, cell lines, unique buffers). | Rigorous qualification is required. For cell-based assays, monitor passage number and stability. For antibodies, define specificity and titer. |
| Interim Reference | Used when a formal reference standard is unavailable, common in early-stage ATMP development [61]. | Provides continuity and confidence; requires bridging studies when replaced with a formal standard later [60] [61]. |
| System Suitability Standards | Used to verify that the total analytical system is functioning correctly on a given day. | Must be stable and provide a predictable response. Failure of system suitability invalidates the analytical run. |
| Schisandrin A | Schisandrin A, CAS:69176-53-0, MF:C24H32O6, MW:416.5 g/mol | Chemical Reagent |
| (-)-Arctigenin | (-)-Arctigenin, CAS:144901-91-7, MF:C21H24O6, MW:372.4 g/mol | Chemical Reagent |
Validating methods for biologics and complex products is fraught with pitfalls that stem from product complexity, immature technologies, and evolving regulatory expectations. Key failures include inadequate robustness testing, poorly designed potency assays, and insufficient planning for method lifecycle management. Success hinges on adopting a science- and risk-based approach, leveraging tools like DoE for robustness, implementing phase-appropriate validation strategies, and maintaining proactive communication with regulatory agencies. By understanding these common challenges and implementing the detailed experimental protocols provided, researchers can develop more reliable and defensible analytical methods, ultimately ensuring the quality of these innovative therapies.
Leveraging ICH Q14 for Enhanced Analytical Procedure Development and Control Strategies
The ICH Q14 guideline, titled "Analytical Procedure Development," represents a significant advancement in the pharmaceutical industry's approach to ensuring drug quality. Finalized in March 2024 by regulatory bodies including the FDA and EMA, this guideline provides science and risk-based approaches for developing and maintaining analytical procedures suitable for assessing the quality of drug substances and products [63] [64]. ICH Q14 applies to both new and revised analytical procedures used for release and stability testing of commercial chemical and biological drug substances and products, establishing a harmonized framework that facilitates more efficient, science-based, and risk-based post-approval change management [63] [64].
This guideline works in synergy with the revised ICH Q2(R2) on "Validation of Analytical Procedures," with both documents becoming effective around the same timeframe to create a comprehensive framework for the entire analytical procedure lifecycle [65]. The primary objective of ICH Q14 is to enhance the robustness and reliability of analytical methods while providing a structured approach to their development, validation, and ongoing management. By promoting a more systematic understanding of analytical procedures, ICH Q14 enables greater regulatory flexibility for post-approval changes when scientifically justified, ultimately supporting more efficient quality control strategies throughout a product's lifecycle [63].
Comparative Analysis: Traditional vs. Enhanced Approaches Under ICH Q14
Fundamental Paradigm Shifts in Analytical Development
ICH Q14 delineates two distinct approaches to analytical procedure development: the Traditional Approach and the Enhanced Approach. The Traditional Approach represents the conventional methodology that has been widely used in the industry, focusing primarily on univariate experimentation and established technologies. In contrast, the Enhanced Approach incorporates Quality by Design (QbD) principles and comprehensive risk management throughout the analytical procedure lifecycle [65]. This represents a significant paradigm shift from simply verifying method performance to building quality directly into the analytical method through systematic understanding and control.
The Enhanced Approach aligns with the concept of "quality built into the product," a principle pioneered by Dr. Joseph M. Juran in the early 1990s and later adopted by the FDA [65]. This philosophy recognizes that increased testing alone does not improve product quality; rather, quality must be designed into the product and processes from the beginning. ICH Q14 operationalizes this principle for analytical methods by encouraging a comprehensive understanding of how method parameters impact performance, thereby facilitating more flexible and science-based regulatory oversight.
Structured Comparison of Development Approaches
Table 1: Comparative Analysis of Traditional vs. Enhanced Analytical Development Approaches
| Aspect | Traditional Approach | Enhanced Approach |
|---|---|---|
| Development Methodology | Univariate experimentation (one factor at a time) | Systematic multivariate experimentation (Design of Experiments) |
| Risk Management | Limited or informal risk assessment | Formal, systematic risk management throughout lifecycle |
| Knowledge Management | Limited documented knowledge | Comprehensive knowledge management establishing proven acceptable ranges |
| Control Strategy | Fixed operational parameters | Method operable design region (MODR) with defined controls |
| Regulatory Flexibility | Limited flexibility for changes | Greater flexibility for scientifically justified changes |
| Technology Scope | Primarily established technologies | Includes modern techniques (multivariate, RTRT, bio-analytical) |
The Enhanced Approach under ICH Q14 introduces several key concepts that differentiate it from traditional methods. The Analytical Target Profile (ATP) serves as the foundation, defining the intended purpose of the analytical procedure and the required performance criteria before method development begins [65] [66]. This proactive strategy ensures the method is designed to meet specific quality needs rather than simply validating whatever method emerges from development. The Enhanced Approach also establishes a Method Operable Design Region (MODR), which defines the multidimensional combination and interaction of analytical procedure parameters that have been demonstrated to provide assurance of suitable method performance [66]. Operating within the MODR provides flexibility while maintaining robustness, as changes within this region are not considered regulatory changes requiring prior approval.
Synergistic Relationship Between ICH Q14 and ICH Q2(R2)
Complementary Roles in Analytical Lifecycle Management
ICH Q14 and ICH Q2(R2) form a winning synergy that strengthens the entire analytical procedure lifecycle from development through validation and continuous improvement [65]. While ICH Q14 focuses on the development phase, providing guidance on scientific approaches for creating robust methods, ICH Q2(R2) addresses the validation phase, establishing principles for demonstrating that analytical procedures are fit for their intended purposes [67]. This complementary relationship ensures a seamless transition from method development to validation, with ICH Q14 establishing the scientific foundation that enables more effective validation under ICH Q2(R2).
The revision of ICH Q2(R2) was long overdue, as the previous version (ICH Q2(R1)) showed "signs of time" and was no longer adequately aligned with current analytical techniques and products, particularly for biotech products and advanced analytical methods [65]. The updated guideline incorporates principles from ICH Q8 (Pharmaceutical Development), ICH Q9 (Quality Risk Management), and ICH Q10 (Pharmaceutical Quality System), making it an exhaustive and modern guidance that aligns with the enhanced approaches described in ICH Q14 [65]. This alignment creates a harmonized framework that supports both traditional and enhanced approaches to analytical procedure development and validation.
Key Updates in ICH Q2(R2) Supporting ICH Q14 Principles
Table 2: Important New Elements in ICH Q2(R2) Supporting ICH Q14 Implementation
| Section/Element | Type | Description | Significance for ICH Q14 |
|---|---|---|---|
| Validation during lifecycle | New | Provides validation approaches for different stages of the analytical procedure lifecycle | Supports continuous improvement aligned with ICH Q14 lifecycle management |
| Considerations for multivariate procedures | New | Describes factors for calibrating and validating multivariate analytical procedures | Enables advanced analytical techniques promoted in ICH Q14 |
| Reportable Range | Updated | Offers expected reportable ranges for common uses of analytical procedures | Provides clearer linkage to ATP requirements |
| Demonstration of stability-indicating properties | New | Guidance on demonstrating specificity/selectivity of stability-indicating tests | Directly supports drug stability testing applications |
| Annexes with illustrative examples | New | Provides practical examples for common analytical techniques | Facilitates implementation of complex concepts |
The enhanced validation approach under ICH Q2(R2) encourages the use of more advanced analytical procedures, with an expected downstream benefit of more robust quality oversight by drug manufacturers [67]. Another anticipated benefit is improvement in the adequacy of validation data submitted, potentially resulting in fewer regulatory information requests and faster application approvals [67]. This aligns perfectly with ICH Q14's objective of facilitating more efficient regulatory evaluations and science-based post-approval change management.
Practical Implementation Framework and Experimental Protocols
Structured Workflow for ICH Q14 Implementation
Implementing ICH Q14 requires a systematic approach that translates theoretical concepts into practical applications. Research indicates that practical implementation remains challenging due to the lack of complete examples and training resources, making it difficult for organizations to bridge the gap between guideline expectations and real-world application [66]. Based on tested methodologies across various industrial settings, the following stepwise approach provides a robust framework for ICH Q14 implementation:
Method Request and ATP Definition: The process begins with formulating a clear analytical question, which drives the creation of an Analytical Target Profile (ATP). A comprehensive ATP should capture not only method performance requirements (accuracy, precision, specificity, range) but also business requirements and the needs of both method developers and end-users [66].
Knowledge and Risk Management: Using risk assessment tools (such as FMEA), method parameters that could impact performance are identified and prioritized for experimental investigation [66].
Systematic Experimentation: During method development, systematic experimentation, including Design of Experiments (DoE), is conducted to evaluate the influence of method parameters on performance and establish the method operable design region [66].
Control Strategy Implementation: A comprehensive control strategy is established, comprising suitable controls and system suitability tests (SSTs) to ensure the method consistently meets predefined criteria during routine use [66].
Method Validation: The method is validated according to ICH Q2(R2) principles, confirming it adheres to the ATP by evaluating parameters such as accuracy, precision, linearity, and robustness [66].
Lifecycle Management: Continuous monitoring and adjustment maintain method performance over time, ensuring effectiveness throughout the product lifecycle [66].
Experimental Design and Key Reagent Solutions
The implementation of ICH Q14 relies on specific experimental methodologies and reagent solutions that enable robust analytical development. The following table outlines essential research reagents and their functions in supporting ICH Q14-compliant analytical procedures:
Table 3: Key Research Reagent Solutions for ICH Q14 Implementation
| Reagent/Category | Function/Purpose | Application Context |
|---|---|---|
| Design of Experiments (DoE) | Systematic approach to evaluate multiple parameters and interactions | Method optimization and MODR establishment |
| Risk Assessment Tools (FMEA) | Identify and prioritize critical method parameters | Knowledge management and control strategy |
| Multivariate Calibration Standards | Enable calibration of complex analytical systems | Multivariate analytical procedures |
| System Suitability Test Materials | Verify method performance before routine use | Ongoing method performance verification |
| Stability-Indicating Components | Demonstrate method specificity for degradants | Stability testing methods |
| Reference Standards | Provide qualification basis for method performance | Method validation and transfer |
The experimental protocol for implementing ICH Q14 begins with ATP definition, where the analytical needs are translated into specific, measurable performance criteria. This is followed by a risk assessment phase using tools like Failure Mode Effects Analysis (FMEA) to identify potential critical method parameters (pCMPs) [66]. These pCMPs then undergo systematic investigation through structured experimentation, typically employing DoE methodologies rather than traditional one-factor-at-a-time (OFAT) approaches. The data generated from these studies enables the establishment of a method operable design region (MODR), which defines the multidimensional combination of analytical procedure parameters that have been demonstrated to provide suitable method performance [66].
Impact on Drug Stability Testing and Control Strategies
Enhanced Stability-Indicating Methods
ICH Q14 significantly strengthens the development and validation of stability-indicating analytical methods, which are crucial for drug stability testing programs. The guideline provides specific guidance on demonstrating stability-indicating properties, emphasizing the importance of showing method specificity or selectivity for both the active ingredient and potential degradants [67]. Under the enhanced approach, method development includes deliberate stress studies to demonstrate that the method can adequately detect and quantify degradation products while accurately measuring the active ingredient without interference.
The enhanced approach also supports the development of more robust stability testing protocols that can adapt to changes in degradation profiles over the product lifecycle. By establishing a thorough understanding of how method parameters affect the separation and detection of degradants, manufacturers can make scientifically justified adjustments to stability methods without requiring regulatory submissions for prior approval, provided changes remain within the established MODR [63]. This flexibility is particularly valuable for long-term stability programs where analytical technologies may evolve or where unexpected degradation pathways may emerge.
Advanced Control Strategies
ICH Q14 facilitates the implementation of more sophisticated analytical procedure control strategies that extend beyond traditional system suitability tests [66]. The enhanced control strategy may include a combination of controls applied during method execution (such as system suitability tests) and controls applied during the method lifecycle (such as periodic reviews and monitoring of method performance). This comprehensive approach to control strategy ensures that analytical procedures remain capable of detecting meaningful changes in product quality attributes throughout their operational lifetime.
For drug stability testing, the control strategy typically includes method performance monitoring across multiple timepoints and storage conditions. The data generated from stability studies can be used to continually verify that the analytical procedure remains fit for purpose, creating a feedback loop for continuous improvement. This lifecycle approach to analytical procedures aligns with the principles of ICH Q10 (Pharmaceutical Quality System) and supports a proactive rather than reactive approach to method performance management [65].
ICH Q14 represents a fundamental shift in how analytical procedures are developed, validated, and managed throughout their lifecycle. By promoting science-based and risk-based approaches, the guideline enables the development of more robust and reliable methods while providing greater flexibility for post-approval changes when scientifically justified [63]. The synergistic relationship between ICH Q14 and ICH Q2(R2) creates a comprehensive framework that supports both traditional and enhanced approaches to analytical procedure development and validation [65].
For drug stability testing programs, the implementation of ICH Q14 principles facilitates the development of more informative stability-indicating methods and more effective control strategies. The emphasis on Analytical Quality by Design (AQbD), systematic experimentation, and lifecycle management ultimately leads to higher quality analytical data, which supports better decision-making regarding product stability and shelf-life [66]. As the pharmaceutical industry continues to adopt ICH Q14, the benefits of more efficient regulatory evaluations, reduced submission questions, and more flexible post-approval change management are expected to accelerate, ultimately contributing to enhanced drug quality and patient safety.
Stability testing is a fundamental component of pharmaceutical development, serving to ensure that drug products maintain their quality, safety, and efficacy throughout their shelf life. The resource-intensive nature of these studies—which involve testing multiple batches under various conditions over several years—has driven the development of scientifically justified reduced testing protocols [68]. Within the framework of ICH guidelines, bracketing and matrixing have emerged as two formally recognized approaches for optimizing stability study designs without compromising data integrity [69]. These strategies are grounded in risk-based principles and require robust scientific justification to demonstrate that the reduced testing protocols still provide reliable stability assessments for all product configurations [69] [70].
The recent consolidation of ICH stability guidelines into a single comprehensive document underscores the continued relevance of these approaches while emphasizing science and risk-based principles aligned with Quality by Design (QbD) concepts [9]. This article provides a comparative analysis of bracketing and matrixing methodologies, supported by experimental data and regulatory frameworks, to guide researchers and drug development professionals in implementing justified reduced stability protocols.
Theoretical Foundations and Regulatory Framework
Definitions and Key Principles
Bracketing is defined as "the design of a stability schedule such that only samples on the extremes of certain design factors, e.g., strength, package size, are tested at all time points as in a full design" [69]. This approach operates on the principle that the stability of intermediate configurations can be reliably inferred from the performance of the extremes. For example, in a product range with multiple strengths, only the highest and lowest concentrations would undergo full testing, assuming the intermediate strengths exhibit stability characteristics within these boundaries [69] [71].
Matrixing involves "the design of a stability schedule such that a selected subset of the total number of possible samples for all factor combinations is tested at a specified time point" [69]. Unlike bracketing, matrixing reduces testing across multiple factors—such as batches, strengths, container sizes, and time points—by employing a statistical approach that ensures all combinations are tested at least once over the study duration [69] [71]. The fundamental assumption is that the stability of each subset tested adequately represents the stability of all samples at a given time point.
Regulatory Guidelines and Historical Context
The ICH Q1A(R2) guideline establishes the foundational definitions for both approaches, while ICH Q1D provides detailed guidance on their application, including sample table layouts and conditions under which reduced designs are acceptable [69] [70]. ICH Q1E offers further direction on the statistical evaluation of stability data derived from these designs [69].
A significant regulatory development occurred in April 2025, when ICH released an overhauled stability guideline that consolidates five previous guidelines into a single document. While this revision represents the most substantial update in over 20 years, it maintains the core principles of bracketing and matrixing, reaffirming their applicability under defined conditions [68] [9]. The updated guideline emphasizes science and risk-based approaches aligned with QbD principles and expands its scope to cover various product types, including biologics, oligonucleotides, and Advanced Therapy Medicinal Products (ATMPs) [9].
Table 1: Key ICH Guidelines Governing Reduced Stability Designs
| Guideline | Focus Area | Key Provisions |
|---|---|---|
| ICH Q1A(R2) | Stability Testing of New Drug Substances and Products | Provides foundational definitions for bracketing and matrixing |
| ICH Q1D | Bracketing and Matrixing Designs | Offers detailed guidance on application, including sample table layouts |
| ICH Q1E | Evaluation of Stability Data | Guides statistical evaluation of stability data from reduced designs |
| ICH Q1 (2025 Revision) | Consolidated Stability Guideline | Maintains core principles while emphasizing risk-based approaches |
Comparative Analysis: Bracketing vs. Matrixing
Fundamental Differences and Applications
While both approaches aim to reduce testing burden, they operate on distinct principles and are suited to different scenarios. Bracketing is particularly applicable when a product range includes multiple strengths or container sizes with identical or closely related compositions [69]. For instance, a tablet range manufactured using different compression weights of similar granulation or capsules filled with different weights of the same composition into various-sized shells are ideal candidates for bracketing [69].
Matrixing offers greater flexibility by allowing reduction across multiple factors simultaneously, including time points, batches, strengths, and container closure systems [69] [71]. This approach is particularly valuable for products with numerous variables where comprehensive testing would be prohibitively resource-intensive. The selection between these strategies depends on product-specific characteristics and the extent of available supporting data.
Table 2: Comparative Analysis of Bracketing and Matrixing Approaches
| Aspect | Bracketing | Matrixing |
|---|---|---|
| Basic Principle | Tests only extremes of a factor range | Tests subset of all possible factor combinations |
| Key Assumption | Stability of intermediates represented by tested extremes | Stability of subsets represents all samples at given time points |
| Best Application | Product ranges with multiple strengths or container sizes | Products with multiple variables (batches, strengths, container types) |
| Data Variability Consideration | Requires tested samples to truly represent extremes | Appropriate only when supporting data show small variability |
| Regulatory Preconditions | Must demonstrate selected extremes are truly worst-case | Requires statistical justification, especially with moderate variability |
| Impact on Study Cost | Reduces number of configurations to be tested | Reduces number of samples tested at each time point |
Implementation Considerations and Limitations
Successful implementation of either approach requires careful consideration of product-specific factors. For bracketing designs, the tested samples must unequivocally represent the extremes of the product range [69]. If the highest and lowest strengths do not truly represent the stability challenges of intermediate strengths, the approach becomes invalid. Similarly, for container sizes, factors such as wall thickness, surface area, headspace-to-volume ratio, and permeation rates must be considered when identifying extremes [71].
Matrixing implementations are particularly sensitive to data variability. As stated in ICH Q1D, "matrixing is appropriate when the supporting data exhibit only small variability. However, where the supporting data exhibit moderate variability, a matrixing design should be statistically justified. If the supportive data show large variability, a matrixing design should not be applied" [69]. This highlights the critical importance of understanding product stability behavior before implementing reduced designs.
The degree of reduction must also be carefully considered. As noted in industry case studies, "matrix study designs that utilized both time point and design factor reduction should be used for products with strong stability profiles" [71]. For products with known stability issues, more robust designs—including full testing, bracketing, or matrixing on time points only—are recommended.
Experimental Protocols and Case Studies
Factorial Design as an Alternative Approach
Recent research has explored factorial analysis as a complementary strategy for optimizing stability studies beyond traditional bracketing and matrixing. A 2025 study investigated this approach using three parenteral dosage forms: an iron complex, pemetrexed, and sugammadex [68]. The experimental protocol involved:
Accelerated Stability Testing: Products were subjected to accelerated conditions (40°C ± 2°C/75% RH ± 5% RH) for 6 months with testing at 0, 3, and 6 months [68].
Factorial Analysis: Accelerated stability data were analyzed to identify critical factors influencing stability, including batch, orientation, filling volume, and drug substance supplier [68].
Reduced Long-term Testing: Based on factorial analysis findings, long-term study designs were strategically reduced while maintaining reliability.
Validation: Regression analysis of long-term data confirmed the validity of the reduced designs [68].
This approach demonstrated that factorial analysis of accelerated stability data could reduce long-term stability testing by at least 50% for the studied parenteral products while maintaining assessment reliability [68].
Bracketing Implementation Case Study
A practical example of bracketing implementation involves Fentanyl Citrate compounded at three different strengths (2 mcg/mL, 10 mcg/mL, and 50 mcg/mL) and filled into three different container sizes (1 mL, 5 mL, and 10 mL) with the same material composition [71]. In this study:
- Only the extremes (2 mcg/mL and 50 mcg/mL strengths in 1 mL and 10 mL containers) were tested at all time points.
- Batch 1 of the 1 mL size for Fentanyl Citrate 2 mcg/mL passed at 60 days but failed at 90 days.
- Consequently, the beyond-use date (BUD) for all intermediate configurations (1 mL and 5 mL 10 mcg/mL; 5 mL 2 mcg/mL) could only be assigned 60 days, matching the least stable extreme condition [71].
This case illustrates both the efficiency gains and potential limitations of bracketing, as the stability of the intermediate configurations was constrained by the performance of the weakest extreme.
Matrixing Implementation Examples
Matrixing designs can vary in complexity based on the degree of reduction. A basic matrix design might involve three batches of two drug strengths tested over a two-year period, with all batches and strengths tested at 0, 12, and 24 months, but only a subset tested at intermediate time points (e.g., 3, 6, 9, 18 months) [71].
More complex designs can matrix both time points and design factors. For a product with three strengths, each in three container sizes with three batches each, a design might specify that at each time point, only one batch of each strength-container combination is tested, with the specific batch varying across time points [71]. The key principle is that "all batches and strengths are required to be tested at zero time, 12 months, and the final time point" if the study duration extends beyond 12 months [71].
Risk-Based Principles and Scientific Justification
Risk Assessment Framework
Implementing reduced stability designs requires systematic risk assessment. The ICH Q1D guideline emphasizes that "the use of any reduced design should be justified" based on product understanding and historical data [69]. Key risk considerations include:
- Product Complexity: Simple aqueous formulations generally present lower risk compared to biologics or complex formulations [72].
- Data Variability: Low variability in supportive stability data reduces risk for matrixing designs [69].
- Manufacturing Consistency: Processes with well-understood and controlled variability support reduced testing [72].
- Container Closure System Understanding: Comprehensive knowledge of drug-container interactions is essential for bracketing designs [71].
A risk-scoring framework can help determine the appropriate level of reduction. For low-risk scenarios, more extensive reductions may be justified, while high-risk products may require more conservative approaches [72].
Statistical Considerations and Data Evaluation
Statistical rigor is particularly crucial for matrixing designs. ICH Q1E provides guidance on evaluating stability data from reduced designs, including approaches for establishing shelf life [69]. Key statistical principles include:
- Sample Size Justification: The number of samples tested must provide sufficient statistical power to detect significant changes.
- Coverage Assurance: The sampling plan must ensure all factor combinations are tested adequately over the study duration.
- Stability Modeling: Regression analysis and analysis of covariance (ANCOVA) help model degradation trends and ensure consistency across batches [72].
Replication at specific time points, particularly at the beginning and end of studies, enhances the precision of slope estimates and mitigates the influence of outliers [72].
The Scientist's Toolkit: Essential Materials and Methods
Table 3: Key Research Reagent Solutions and Materials for Stability Studies
| Item | Function/Application | Examples/Standards |
|---|---|---|
| Stability Chambers | Provide controlled temperature and humidity conditions for long-term, intermediate, and accelerated studies | ICH Q1A(R2) specified conditions: 25°C/60% RH, 30°C/65% RH, 40°C/75% RH [68] |
| HPLC-UV Systems | Quantify drug substance concentration and detect degradation products | Used in accelerated stability testing for parenteral products [68] |
| Size Exclusion Chromatography (SEC) | Assess protein aggregation and purity for biologics | Critical for mAb therapeutics and protein-based products [72] |
| Ion-Exchange Chromatography (IEC) | Evaluate charge variants in biologics | Used in comprehensive stability assessments [72] |
| LC-MS Systems | Identify chemical modifications (oxidation, deamidation) | Employed in forced degradation studies [72] |
| Type I Glass Vials | Primary container for parenteral products | Used in parenteral stability studies with bromobutyl rubber stoppers [68] |
| Sorbic acid | Sorbic acid, CAS:161814-42-2, MF:C6H8O2, MW:112.13 g/mol | Chemical Reagent |
| Butylated Hydroxyanisole | Butylated Hydroxyanisole, CAS:921-00-6, MF:C11H16O2, MW:180.24 g/mol | Chemical Reagent |
Decision Framework for Protocol Selection
The following workflow illustrates the logical decision process for selecting and implementing reduced stability testing protocols:
Reduced Stability Protocol Decision Workflow
Bracketing and matrixing represent scientifically valid and regulatory-accepted approaches for optimizing stability study designs while maintaining data integrity. The selection between these strategies depends on product-specific characteristics, with bracketing suited to product ranges with identifiable extremes and matrixing applicable to products with multiple variables when supporting data exhibit low variability.
The 2025 ICH guideline revision reaffirms the place of these approaches within modern, risk-based pharmaceutical development frameworks. Emerging methodologies, such as factorial analysis, show promise for further optimizing stability protocols, particularly for complex dosage forms like parenteral products.
Successful implementation requires robust scientific justification, statistical rigor, and thorough documentation. When appropriately applied based on comprehensive product understanding and risk assessment, these reduced designs offer significant efficiency gains while ensuring product quality, safety, and efficacy throughout the shelf life.
Addressing Accelerated Timelines and Variability in Raw Materials
In the competitive and highly regulated pharmaceutical industry, the dual challenges of accelerating development timelines and managing raw material variability present a significant hurdle for scientists and drug development professionals. Variability in the physical and chemical properties of raw materials, including Active Pharmaceutical Ingredients (APIs) and complex media components, can profoundly impact process performance, final product quality, and stability profiles [73] [74]. Effectively controlling this variability is not just a technical objective but a core requirement of the Quality by Design (QbD) paradigm mandated by regulatory standards like the ICH guidelines [73].
This guide objectively compares two data-driven methodologies—multivariate material classification for oral solid dosage forms and FTIR-based predictive screening for biologics—that have demonstrated efficacy in mitigating these risks. By comparing experimental protocols and performance data, this analysis aims to equip scientists with the knowledge to select and validate robust analytical methods that ensure drug stability and process consistency amidst accelerated development schedules.
Comparative Analysis of Two Strategic Approaches
The following table summarizes the core attributes, applications, and outputs of the two principal strategies for addressing raw material variability, which will be examined in detail throughout this guide.
Table 1: Strategic Comparison for Managing Raw Material Variability
| Feature | Multivariate Material Classification for Solid Dosage Forms | FTIR-Based Predictive Screening for Biologics |
|---|---|---|
| Primary Goal | Accelerate formulation & process development via material classification [73] | Predict impact of complex media on cell culture productivity [74] |
| Target Materials | APIs & excipients for oral solid dosage forms [73] | Chemically-undefined raw materials (e.g., plant-derived hydrolysates) [74] |
| Key Analytical Technique | Bulk powder characterization (e.g., particle size, density) [73] | Fourier-Transform Infrared (FTIR) Spectroscopy [74] |
| Core Data Analysis Method | Principal Component Analysis (PCA) & Partial Least Squares Discriminant Analysis (PLS-DA) [73] | Principal Component Analysis (PCA) & Partial Least Squares (PLS) Regression [74] |
| Key Output | Classification of materials into processability categories [73] | Quantitative prediction of final productivity (e.g., antibody titer) [74] |
Experimental Protocols and Data Presentation
Protocol 1: Multivariate Classification of Powder Flowability
This protocol is designed for early-stage development of oral solid dosage forms, where material is scarce, and rapid assessment of manufacturability is critical [73].
3.1.1 Materials and Reagents
- 41 Powder Materials: The study utilizes a dataset of 34 APIs and 7 excipients, designated M1-M41, representing a wide range of particle morphologies from cohesive, micronized powders to free-flowing granules [73].
3.1.2 Methodology
- Material Characterization: Each material is characterized by a limited set of 8 physical properties relevant to powder flow:
- Particle Size Distribution (D10, D50, D90)
- Specific Surface Area (SSA)
- True Density
- Bulk Density (Loose and Tapped)
- Compressibility Index (CI)
- Permeability [73].
- Data Pre-processing: The dataset is organized into a matrix, and missing data is imputed. Variables are auto-scaled (mean-centered and divided by standard deviation) to give all properties equal weight [73].
- Multivariate Modeling:
- PCA: An unsupervised method is used to explore the data structure, reduce dimensionality, and identify potential outliers by visualizing the principal component scores [73].
- PLS-DA: A supervised classification model is developed to distinguish between categories of powder flowability. The model is validated using a cross-validation method [73].
3.1.3 Results and Performance Data The PLS-DA model successfully classified the 41 materials into three distinct categories—Excellent, Good, and Poor—based on their predicted performance in a continuous direct compression process [73]. The model's performance was validated, confirming its utility as a decision-making tool for material selection during early development.
Table 2: Classification of Example Materials Based on PLS-DA Model
| Material ID | Category | Key Differentiating Properties |
|---|---|---|
| M1, M2, M3 | Excellent | Larger particle size (D50), lower compressibility, higher permeability [73] |
| M4, M5, M6 | Good | Medium particle size, medium compressibility [73] |
| M7, M8, M9 | Poor | Smaller particle size (D50), higher compressibility, higher specific surface area [73] |
Protocol 2: FTIR-Based Predictive Modeling for Cell Culture
This protocol uses FTIR spectroscopy to predict the impact of chemically undefined raw materials on the productivity of mammalian cell cultures used in biologic drug manufacturing [74].
3.2.1 Materials and Reagents
- Complex Raw Material: A single, chemically-undefined media component (e.g., a plant-derived hydrolysate) identified as a major source of productivity variability [74].
- Cell Culture System: Industrial mammalian cell lines for the production of therapeutic antibodies (e.g., Products A and B) [74].
3.2.2 Methodology
- FTIR Spectral Acquisition:
- Multiple samples are taken from each lot of the raw material to account for intra-lot heterogeneity.
- Spectra are collected on FTIR spectrometers (e.g., Nicolet iS10 or Spectrum 3) with a harmonized protocol: 32 scans per sample, wavenumber range 4000–400 cmâ»Â¹ [74].
- Spectral Data Processing:
- Collected spectra are processed using a second-derivative transformation to resolve overlapping peaks and remove baseline offsets.
- The data is smoothed before analysis [74].
- Productivity Data Collection: Historical productivity data (e.g., final antibody titer) from commercial-scale batches using specific raw material lots is collected and averaged for each lot [74].
- Predictive Model Building:
- PCA: Used to review the spectral data and identify outliers.
- PLS Regression: The processed spectral data (X-matrix) is merged with the productivity data (Y-variable) to build a predictive model. The model is validated with seven-fold cross-validation, and its validity is confirmed through Y-randomization [74].
3.2.3 Results and Performance Data The PLS models demonstrated a strong ability to predict commercial-scale productivity based solely on the FTIR spectra of the raw material. For the models discussed, reported R² (goodness-of-fit) values were ≥ 0.8 and Q² (predictive ability) values were ≥ 0.7, indicating robust and predictive models [74]. This approach reduced the raw material evaluation time from approximately one month to just two days [74].
Table 3: Performance of FTIR-Based Predictive Models for Two Commercial Products
| Product | Number of RM Lots in Model | Model Key Metrics (R²/Q²) | Reported Outcome |
|---|---|---|---|
| Product A | 12 | R² ≥ 0.8, Q² ≥ 0.7 | Effectively predicted productivity, enabling rapid screening [74] |
| Product B | 18 | R² ≥ 0.8, Q² ≥ 0.7 | Effectively predicted productivity, enabling rapid screening [74] |
Integration with Drug Stability Testing and ICH Guidelines
The strategies described align perfectly with the science- and risk-based principles of the consolidated ICH Q1 guideline for stability testing [1] [4]. Controlling raw material variability is a foundational element of ensuring drug product stability.
- Supporting Shelf-Life Claims: ICH Q1 requires understanding how quality varies over time. By controlling raw material attributes, manufacturers ensure consistent product performance and stability, leading to more accurate and reliable shelf-life estimations [75].
- Stability-Indicating Methods: The multivariate and spectroscopic methods featured are modern embodiments of stability-indicating procedures. They provide a scientifically justified, data-rich foundation for understanding how raw material properties influence stability-critical quality attributes [73] [74].
- Lifecycle Management: ICH Q1 emphasizes stability considerations throughout the product lifecycle [75] [4]. The predictive tools allow for proactive management of raw material changes, such as supplier or synthesis route alterations, ensuring these changes do not adversely impact product stability without the need for extensive new stability studies [73].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table lists key reagents, materials, and software solutions essential for implementing the described experimental protocols.
Table 4: Key Research Reagent Solutions for Material Variability Studies
| Item Name | Function / Application | Relevant Protocol |
|---|---|---|
| Pharmaceutical Powders (APIs & Excipients) | Serve as test subjects for characterizing a wide range of flow properties and building a representative historical database [73]. | Multivariate Classification |
| Chemically-Undefined Media Components | Complex raw materials (e.g., hydrolysates) used to assess impact on cell culture productivity and build predictive spectral models [74]. | FTIR-Based Modeling |
| FTIR Spectrometer | Analytical instrument used to characterize the chemical composition and structure of raw materials via infrared spectroscopy [74]. | FTIR-Based Modeling |
| Multivariate Analysis Software | Software platform (e.g., SIMCA) used for performing PCA, PLS, and PLS-DA to build classification and regression models [73] [74]. | Both Protocols |
| Physical Property Testers | Instruments for measuring key powder properties like particle size, density, and surface area, which serve as inputs for the classification model [73]. | Multivariate Classification |
Workflow and Relationship Visualization
The following diagram illustrates the integrated logical workflow for applying these strategies within the context of drug development and stability validation.
Strategies for Method Transfer and Ensuring Data Integrity
In the pharmaceutical industry, the reliability of stability data for a drug product is paramount, serving as a critical component of regulatory submissions. The processes of analytical method transfer and rigorous data integrity management form the foundation of this reliability. These procedures ensure that quality control testing, a mandatory requirement of ICH guidelines, produces consistent and trustworthy results across different laboratories and throughout a product's lifecycle. This guide provides a comparative analysis of the formal strategies for transferring analytical methods, framed within the essential context of ensuring data integrity for drug stability testing.
A Comparative Guide to Analytical Method Transfer Strategies
The transfer of an analytical method from a transferring laboratory (sending unit) to a receiving laboratory is a documented process that qualifies the receiving site to use the analytical procedure reliably [76]. Selecting the correct transfer strategy is the first critical decision, with the choice hinging on the method's maturity, the receiving lab's familiarity with it, and the specific regulatory context [77] [78].
The following table compares the four primary approaches to method transfer.
| Transfer Approach | Core Principle | Best-Suited Context | Key Advantages & Considerations |
|---|---|---|---|
| Comparative Testing [77] [78] | Both laboratories analyze an identical set of predetermined samples; results are statistically compared. | Well-established, validated methods; laboratories with similar capabilities and equipment. [77] | Most common and straightforward approach. Relies on direct, side-by-side data comparison. [78] |
| Co-validation [77] [76] | The analytical method is validated simultaneously by both the transferring and receiving laboratories. | New methods being developed for multi-site use or before formal validation is complete. [77] | Builds equivalence into the method from the start. Requires intense collaboration and harmonized protocols. [78] |
| Revalidation / Partial Revalidation [77] [76] | The receiving laboratory performs a full or partial revalidation of the method. | Significant differences in lab conditions/equipment; substantial method changes; original validation non-compliant. [77] | Most rigorous approach. Demonstrates the method's suitability for the new environment. [78] |
| Transfer Waiver [77] [76] | The formal transfer process is waived based on strong scientific justification and documented evidence. | Highly experienced receiving lab; identical conditions; simple, robust methods (e.g., pharmacopoeial methods). [77] | Avoids redundant testing. Requires robust documentation and is subject to high regulatory scrutiny. [78] |
When is a Formal Method Transfer Not Required?
A formal method transfer may be waived in specific, justified situations. These include the use of compendial pharmacopoeia methods, which only require verification [77] [76], or when the product composition is comparable to an existing product and the receiving laboratory is already familiar with the method [77]. Transfers can also be waived for general methods like visual inspection or weighing, or if key personnel from the transferring unit move to the receiving unit [77].
Experimental Protocol for a Comparative Method Transfer
The comparative testing approach is frequently used. Its experimental design is critical for generating defensible data that proves equivalence between laboratories.
Protocol Development and Acceptance Criteria
A pre-approved, detailed transfer protocol is mandatory. This document must outline the objective, scope, responsibilities of each unit, materials and instruments to be used, the analytical procedure, experimental design, and, crucially, pre-defined acceptance criteria for each test [77] [78]. These criteria are typically based on the method's validation data, particularly reproducibility [77].
Typical Acceptance Criteria: The table below summarizes common acceptance criteria for key test types, which should be defined with respect to ICH requirements [77].
| Test Type | Typical Acceptance Criteria |
|---|---|
| Identification | Positive (or negative) identification must be obtained at the receiving site. [77] |
| Assay | The absolute difference between the mean results from the two sites should be not more than (NMT) 2-3%. [77] |
| Related Substances | Requirements vary by impurity level. For low levels, recovery of 80-120% for spiked impurities may be used. For higher levels (e.g., >0.5%), a defined absolute difference is typical. [77] |
| Dissolution | Absolute difference in mean results is NMT 10% at time points when <85% is dissolved, and NMT 5% when >85% is dissolved. [77] |
Execution and Data Analysis
The transfer involves both laboratories analyzing the same homogeneous and representative samples, which can include spiked samples or production batches [77] [78]. The resulting data from both sites is then compiled and subjected to statistical comparison as defined in the protocol. Common analyses include calculating standard deviation, relative standard deviation (RSD), confidence intervals, and the difference between the mean values of each laboratory [77]. Equivalence testing, t-tests, or F-tests may be employed [78].
Method Transfer Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The integrity of any analytical method transfer is contingent on the quality and consistency of the materials used. The following table details key reagent solutions and their critical functions in ensuring reliable results.
| Research Reagent / Material | Critical Function in Method Transfer & Stability Testing |
|---|---|
| Certified Reference Standards | Provide the benchmark for calibrating instruments and ensuring the accuracy and traceability of all quantitative results. [76] |
| Qualified Reagents & Solvents | The quality and consistency of reagents are vital for robust method performance, preventing interference and ensuring specificity. [77] |
| Spiked Samples | Artificially created samples with known amounts of analytes or impurities; used to challenge the method and demonstrate accuracy and recovery, especially in impurity testing. [77] |
| Stable Test Samples | Homogeneous, representative samples (e.g., from production batches) with confirmed stability for the duration of the transfer study are essential for a valid comparison. [77] [78] |
Ensuring Data Integrity Throughout the Process
Data integrity—the requirement for data to be complete, consistent, and accurate—is a cornerstone of regulatory compliance [79]. The FDA has issued warnings due to observed CGMP violations involving data integrity, making it a focal point during inspections [79].
A holistic approach is necessary to ensure data integrity from the outset of setting up a stability program and during a method transfer. This involves collaboration between R&D, Quality Control (QC), Quality Assurance (QA), and Regulatory Affairs to ensure compliance [79]. Key practices include using qualified and calibrated equipment, maintaining complete and traceable documentation (including raw data, chromatograms, and a final transfer report), and ensuring all personnel are thoroughly trained [77] [78].
Data Integrity Framework
A successful analytical method transfer is a meticulously planned and executed scientific exercise, underscored by an unwavering commitment to data integrity. The choice of transfer strategy—be it comparative testing, co-validation, revalidation, or a justified waiver—must be tailored to the specific method and context. Ultimately, thorough planning, open communication between laboratories, and a robust framework for ensuring data integrity are not just regulatory requirements but the fundamental practices that prevent laboratory errors and ensure the reliability of stability data for drug products, thereby protecting patient safety and product efficacy.
Ensuring Lifelong Compliance: Method Validation in Stability Lifecycle Management
This guide objectively compares the paradigm of traditional, discrete stability testing against the integrated, knowledge-driven approach facilitated by ICH Q12. The core thesis posits that managing stability through a continuous lifecycle model, supported by robust analytical method monitoring, leads to more predictable post-approval changes, enhanced product quality, and stronger regulatory agility. The following data and experimental protocols provide a framework for implementation, demonstrating the tangible performance benefits of this modernized system.
Performance Comparison: Traditional vs. ICH Q12 Lifecycle Approach
The integration of stability activities within the ICH Q12 framework fundamentally reshapes performance outcomes across the product lifecycle. The table below summarizes key comparative performance data.
Table 1: Performance Comparison of Stability Management Approaches
| Performance Metric | Traditional Discrete Approach | Integrated ICH Q12 Lifecycle Approach |
|---|---|---|
| Regulatory Predictability | Low; changes often require prior approval submissions, causing delays [80] [81] | High; defined Established Conditions (ECs) and PACMPs enable more predictable, efficient management [80] [82] [81] |
| Post-Approval Change Lead Time | Can be up to a year for review and approval [81] | Significantly reduced through agreed-upon protocols [81] |
| Resource Efficiency for Changes | High; costly, redundant testing for each change [83] | Optimized; science- and risk-based approaches reduce redundant testing [83] |
| Foundation for Decisions | Focused on regulatory approval [83] | Built on continuous product and process knowledge [83] |
| Impact on Continuous Improvement | Limited; cumbersome change processes disincentivize improvement [81] | Enhanced; flexible regulatory tools incentivize continual improvement [81] |
Experimental Protocols for Lifecycle Stability Verification
Adopting the ICH Q12 lifecycle model requires specific experimental strategies to build knowledge and verify stability. The following protocols are foundational.
Protocol for Establishing a Stability Operable Design Region (SODR)
- Objective: To define the multidimensional interaction between formulation, process parameters, packaging, and storage conditions that ensures product quality throughout the intended shelf-life [83].
- Methodology:
- Design of Experiments (DoE): Utilize a multi-factorial DoE to systematically vary critical material attributes (CMAs) and process parameters (CPPs). This is analogous to the efficient, multi-variable testing used in other fields to discover interactions [84].
- Stressing Conditions: Expose samples from different experimental batches to accelerated (e.g., 40°C/75% RH) and intermediate (e.g., 30°C/65% RH) conditions, as per ICH Q1A(R2), alongside long-term studies [83].
- Data Integration: Analyze the resulting stability data (assay, impurities, dissolution, etc.) to model the impact of CMA/CPP variations on Critical Stability Attributes (CSAs). The region where all CSAs remain within acceptance criteria defines the SODR [83].
- Data Interpretation: A robust SODR demonstrates that minor, well-understood variations in manufacturing or storage within the defined region will not adversely impact product shelf-life, providing a scientific basis for post-approval change management.
Protocol for a Post-Approval Change Management (PACMP)
- Objective: To pre-plan and gain regulatory agreement on the studies required to implement a future CMC change, enhancing predictability and efficiency [81].
- Methodology:
- Change Definition: Clearly describe the specific change (e.g., a minor equipment qualification or a site transfer within a qualified network).
- Risk Assessment & Justification: Conduct a risk assessment based on existing product and process knowledge to justify the reduced stability commitment.
- Stability Study Protocol:
- Batches: Typically one pilot-scale or production batch incorporating the change.
- Conditions: Long-term stability studies at 25°C/60% RH or 30°C/65% RH for the required duration (e.g., 3-6 months).
- Testing: A streamlined testing regimen focusing on CSAs most likely to be impacted by the change [83] [81].
- Data Interpretation: Successful completion of the agreed-upon stability data in the PACMP allows for the change to be implemented with a lower reporting category (e.g., annual report), avoiding a prior-approval supplement [81].
Visualizing the Stability Lifecycle Management Framework
The integrated stability lifecycle is a continuous process. The diagram below illustrates the four-stage framework and the flow of knowledge and activities.
Stability Lifecycle Management Framework
The relationship between the control strategy, analytical procedures, and stability studies is critical for maintaining quality. The following diagram details this interaction.
Control Strategy and Stability Verification
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of a stability lifecycle program relies on specific tools and materials. The table below catalogs key items and their functions.
Table 2: Essential Research Reagents and Materials for Stability Studies
| Item/Solution | Function in Stability Protocol |
|---|---|
| Reference Standards | Certified materials used to identify and quantify the active pharmaceutical ingredient (API) and its impurities during stability testing [83]. |
| Stability-Indicating Analytical Methods | Fully validated chromatographic (e.g., HPLC/UPLC) methods capable of detecting and quantifying degradation products distinct from the API [83]. |
| Forced Degradation Study Materials | Reagents for stress testing (e.g., acid, base, oxidant, light) to validate method specificity and elucidate degradation pathways [83]. |
| ICH Climatic Zone Storage Chambers | Environmental chambers that precisely control temperature and humidity (e.g., 25°C/60% RH, 30°C/65% RH, 40°C/75% RH) for long-term, intermediate, and accelerated studies [83]. |
| Validated Stability Data Management System | A computerized system for tracking stability samples, scheduling tests, and managing the large datasets generated, ensuring data integrity and facilitating trend analysis [83]. |
Forced degradation studies are a critical component of pharmaceutical development, serving as a controlled means to understand how a drug substance or product behaves under various stress conditions. These studies simulate harsh environments to accelerate degradation, helping scientists uncover potential vulnerabilities in a molecule’s structure and predict its long-term stability. While regulatory agencies require these studies to support stability-indicating methods and shelf-life claims, their value extends far beyond mere compliance. They provide a roadmap for formulation design, packaging decisions, and risk mitigation strategies, ultimately ensuring that pharmaceutical products maintain their quality, safety, and efficacy throughout their shelf life [85].
In the context of validating analytical methods for drug stability testing per ICH guidelines, forced degradation studies play a foundational role. They help demonstrate that analytical procedures are stability-indicating, meaning they can accurately detect and quantify changes in the product's quality attributes over time. The International Council for Harmonisation (ICH) provides guidance on analytical procedure validation through documents such as ICH Q2(R2), which outlines key validation elements including accuracy, precision, specificity, detection limit, quantitation limit, linearity, and range for procedures used in release and stability testing of commercial drug substances and products [12].
Methodological Framework for Forced Degradation Studies
Experimental Design and Stress Conditions
Forced degradation studies involve the systematic application of controlled stress conditions to drug substances and products, typically exceeding those used in standard stability studies conducted per ICH Q5C. The design of these studies requires careful consideration of multiple factors, including prior knowledge about the product or similar molecules, assessment of critical quality attributes (CQAs), and the specific degradation pathways likely to be encountered. While study designs may vary based on the specific molecule and development stage, the fundamental approach involves exposing the drug to a range of stress conditions that mimic potential real-world challenges [86].
The selection of appropriate stress conditions is guided by the nature of the drug molecule and its intended formulation. Common stress conditions include:
Acidic and basic hydrolysis: These conditions target functional groups such as esters, lactones, acetals, and some amides that are prone to acid or base-catalyzed hydrolysis. Acidic degradation typically involves exposing the drug to strong mineral acids like hydrochloric acid under controlled temperature and time conditions. At the molecular level, acidic hydrolysis breaks bonds through protonation of electrophilic centers, making them more susceptible to nucleophilic attack by water. Basic degradation involves treating the drug with strong bases such as sodium hydroxide, which can lead to bond cleavage, ring opening, and rearrangements through direct nucleophilic attack by hydroxide ions [85].
Oxidative stress: Oxidation represents one of the most common degradation pathways, particularly for molecules containing electron-rich groups like phenols, tertiary amines, sulfides, and unsaturated bonds. Oxidative stress can be induced using agents like hydrogen peroxide or radical initiators such as AIBN (azobisisobutyronitrile), each offering distinct degradation profiles. Peroxide-based oxidation generates reactive oxygen species that attack nucleophilic centers in the molecule, while AIBN-based oxidation produces carbon-centered radicals that initiate different chain reactions [85].
Thermal stress: Thermal degradation involves exposing the drug to elevated temperatures in both the presence and absence of moisture. Dry heat stress accelerates chemical reactions such as rearrangements, bond cleavage, and oxidation, particularly in thermally labile compounds. Thermal studies simulate long-term storage in hot climates and help determine the need for temperature-controlled packaging or labeling [85].
Humidity stress: Humidity stress combines heat and moisture to evaluate the impact of water vapor on the drug substance or product. This condition is especially important for hygroscopic materials and solid dosage forms, as moisture can facilitate hydrolysis, promote crystallinity changes, and cause phase transitions [85].
Photolytic stress: Photolytic degradation involves exposing the drug to both UV and visible light to simulate sunlight or artificial lighting. Light can induce various reactions, including bond cleavage, isomerization, and formation of reactive intermediates, particularly in molecules with conjugated systems, aromatic rings, and halogenated compounds [85].
The following diagram illustrates the experimental workflow for conducting forced degradation studies:
Experimental Workflow for Forced Degradation Studies
Analytical Techniques for Monitoring Degradation
The characterization of degradation products and the monitoring of degradation pathways require a comprehensive analytical strategy employing multiple orthogonal techniques. The selection of analytical methods is driven by the degradation pathways expected, the critical quality attributes of the product, and the stage of development [86]. Common analytical techniques used in forced degradation studies include:
Size-exclusion chromatography (SE-UPLC or SE-HPLC): This technique is used to separate and quantify protein aggregates (high molecular weight species) and fragments (low molecular weight species) from the monomeric drug product. It is particularly valuable for monitoring fragmentation and aggregation under various stress conditions [87].
Capillary electrophoresis (CE-SDS): This method provides high-resolution separation and quantification of product-related impurities, including aggregates and fragments. It offers complementary information to size-exclusion chromatography and is particularly useful for detecting subtle changes in protein size variants [87].
Isoelectric focusing (icIEF or IEF): This technique characterizes charge variants resulting from post-translational modifications or degradation-induced changes. It separates isoforms based on their isoelectric points and can detect acidic and basic variants that may arise from degradation [87].
Biological activity assays: These functional assays determine the potency of the drug product under specific stress conditions. For monoclonal antibodies, complement assays or other mechanism-based activity measurements can reveal whether stress conditions have affected the biological function of the molecule [87].
The following table summarizes the key analytical techniques employed in forced degradation studies and their specific applications:
Table 1: Analytical Techniques for Forced Degradation Studies
| Analytical Technique | Acronym | Primary Application | Measured Parameters |
|---|---|---|---|
| Size-exclusion chromatography | SE-UPLC/SE-HPLC | Separation by size | Monomer content, high molecular weight aggregates, low molecular weight fragments |
| Capillary electrophoresis | CE-SDS | Purity and impurity profiling | Product-related impurities, fragments, aggregates |
| Isoelectric focusing | icIEF/IEF | Separation by charge | Charge variants (acidic/basic isoforms), main peak |
| Biological activity assays | N/A | Functional assessment | Potency, efficacy, mechanism-based activity |
Comparative Assessment of Biosimilar and Originator Products
Case Study: Monoclonal Antibody Degradation Profiles
Forced degradation studies play a particularly important role in the comparative assessment of biosimilar and originator biological products. As required by regulatory agencies, biosimilar developers must demonstrate that their product is highly similar to the reference product in terms of quality attributes, safety, and efficacy. Forced degradation studies provide a powerful tool for this comparative assessment by revealing similarities and differences in degradation pathways under controlled stress conditions [87].
A recent study comprehensively characterized and compared biosimilar monoclonal antibodies with their originator counterparts under various forced degradation conditions. The products were exposed to different stress conditions including oxidative stress, pH stress, thermal stress, freeze/thaw cycles, and agitation. The products were then analyzed at defined time points using validated analytical methods to assess aggregation profiles, biological activity, and charge variant distribution [87].
The following table summarizes the quantitative results from this comparative forced degradation study, showing the changes in key quality attributes for both biosimilar and originator monoclonal antibodies under various stress conditions:
Table 2: Comparative Degradation Profiles of Biosimilar vs. Originator Monoclonal Antibodies
| Stress Condition | Product | Monomer Content (%) | HMW Aggregates (%) | Acidic Variants (%) | Basic Variants (%) |
|---|---|---|---|---|---|
| Control (Unstressed) | Biosimilar | 97.9 ± 0.01 | 1.2 ± 0.01 | 28.6 ± 0.30 | 11.8 ± 0.53 |
| Originator | 98.0 ± 0.02 | 1.1 ± 0.01 | 29.1 ± 0.25 | 11.5 ± 0.42 | |
| Thermal Stress (37°C, 14 days) | Biosimilar | 96.6 ± 0.01 | 2.4 ± 0.01 | 40.1 ± 0.03 | 10.1 ± 0.16 |
| Originator | 96.5 ± 0.02 | 2.5 ± 0.01 | 40.3 ± 0.05 | 10.2 ± 0.12 | |
| Thermal Stress (50°C, 14 days) | Biosimilar | 89.6 ± 0.02 | 9.0 ± 0.02 | 67.6 ± 0.28 | 7.4 ± 0.29 |
| Originator | 89.4 ± 0.03 | 9.2 ± 0.02 | 67.9 ± 0.31 | 7.3 ± 0.25 | |
| pH Stress (pH 4, 72 hours) | Biosimilar | 53.6 ± 0.02 | 45.6 ± 0.03 | 26.2 ± 0.04 | 22.2 ± 0.18 |
| Originator | 53.8 ± 0.03 | 45.4 ± 0.02 | 26.5 ± 0.06 | 22.0 ± 0.15 |
The data from this comparative study demonstrated that the biosimilar monoclonal antibody was analytically similar to the originator product in terms of critical parameters related to efficacy and safety under various stress conditions. Both products exhibited similar degradation profiles across all stress conditions tested, with no statistically significant differences in most parameters. This similarity in degradation behavior provides confidence that the biosimilar and originator products will behave similarly throughout their shelf life and under accidental stress conditions during manufacturing, storage, transportation, and administration [87].
Mechanisms of Degradation at the Molecular Level
Understanding the molecular mechanisms of degradation is essential for interpreting forced degradation results and designing stable formulations. Different stress conditions target specific molecular vulnerabilities, leading to distinct degradation pathways:
Acidic hydrolysis: This stress condition primarily affects acid-labile functional groups. At the molecular level, acidic hydrolysis breaks bonds through protonation of electrophilic centers, making them more susceptible to nucleophilic attack by water. For example, esters may cleave into their corresponding alcohol and acid, while amides may yield amines and acids. The rate and extent of degradation depend on the molecule's structure, acid concentration, and temperature [85].
Basic hydrolysis: Base-catalyzed reactions often proceed through direct nucleophilic attack by hydroxide ions. Basic hydrolysis can lead to bond cleavage, ring opening, and rearrangements. For instance, lactones may open to form hydroxy acids, and esters may convert to alcohols and carboxylic acids. Some molecules may undergo β-elimination or retro-aldol reactions under basic conditions [85].
Oxidative degradation: Oxidation pathways depend on the specific oxidant used. Peroxide-based oxidation generates reactive oxygen species such as hydroxyl radicals, which attack nucleophilic centers in the molecule, leading to N-oxide formation, sulfoxidation, cleavage of double bonds, and aromatic ring hydroxylation. In contrast, AIBN-based oxidation produces carbon-centered radicals that can abstract hydrogen atoms, initiate polymerization-like reactions, or cause fragmentation in sensitive molecules [85].
The following diagram illustrates the major degradation pathways and their molecular mechanisms:
Molecular Mechanisms of Major Degradation Pathways
Regulatory and Practical Applications
Role in Analytical Method Validation
Forced degradation studies provide the scientific foundation for validating stability-indicating analytical methods as required by ICH guidelines. According to ICH Q2(R2) on validation of analytical procedures, methods used for stability testing must demonstrate specificity for the analyte in the presence of potential degradants. Forced degradation studies generate these degradants, allowing demonstration that the analytical method can accurately detect and quantify the active ingredient while separating it from its degradation products [12].
The data generated from forced degradation studies helps establish that analytical methods are stability-indicating and suitable for their intended purpose throughout the product lifecycle. This is particularly important for biological products, where multiple quality attributes must be monitored and complex degradation pathways may be involved. The studies provide evidence that the methods can detect changes in critical quality attributes that may impact product safety and efficacy [86].
Applications in Comparability Assessments
Forced degradation studies play an essential role in comparability assessments following manufacturing process changes for biological products. As described in ICH Q5E, comparability exercises are necessary when changes are made to the manufacturing process of biological drugs to ensure that these changes have no adverse impact on the quality, safety, and efficacy of the drug product [86].
According to industry surveys, forced degradation studies are used by all companies to support comparability assessments, though the specific study designs may vary. The extent of manufacturing process changes is a key driver in deciding whether to implement forced degradation studies as part of the comparability assessment. Companies typically use a risk-based approach to determine the scope and depth of forced degradation studies needed, considering factors such as the nature of the process change, its potential impact on known quality attributes, and the phase of development [86].
The Scientist's Toolkit: Essential Reagents and Materials
The following table outlines key research reagent solutions and essential materials used in forced degradation studies, along with their specific functions:
Table 3: Essential Research Reagents and Materials for Forced Degradation Studies
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Hydrochloric Acid (HCl) | Acidic stress agent | Acidic hydrolysis studies at various concentrations (e.g., 0.1-1.0 M) |
| Sodium Hydroxide (NaOH) | Basic stress agent | Basic hydrolysis studies at various concentrations (e.g., 0.1-1.0 M) |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | Oxidative stress agent | Peroxide-based oxidation studies (typically 0.1-0.3%) |
| AIBN (Azobisisobutyronitrile) | Radical initiator | Radical-mediated oxidation studies |
| Buffer Systems (various pH) | pH control and maintenance | Creating specific pH environments for stability assessment |
| Reference Standards | Analytical calibration | Quantification of parent drug and degradation products |
| Enzymes (e.g., proteases) | Biocatalytic stress agents | Simulating enzymatic degradation pathways |
Forced degradation studies represent an indispensable tool in pharmaceutical development, particularly for validating analytical methods used in stability testing per ICH guidelines. These studies provide critical insights into the degradation behavior of drug substances and products, revealing vulnerabilities that might not be apparent under normal storage conditions. The comparative assessment of biosimilar and originator products under forced degradation conditions demonstrates the power of these studies in establishing analytical similarity and predicting long-term stability behavior.
When properly designed and executed, forced degradation studies transcend mere regulatory compliance to become strategic assets in formulation development, packaging selection, and lifecycle management. They enable scientists to anticipate stability issues before they occur in the marketed product, thereby reducing risks to product quality and patient safety. As the pharmaceutical industry continues to evolve with increasingly complex molecules and therapeutic modalities, forced degradation studies will remain essential for ensuring that medicines remain safe, effective, and of high quality throughout their shelf life.
For researchers and drug development professionals, stability testing constitutes a fundamental pillar of pharmaceutical development, ensuring that drug substances and products maintain their quality, safety, and efficacy throughout their shelf life. The International Council for Harmonisation (ICH) has provided a set of guidelines (ICH Q1A-E, Q3A-B, Q5C, Q6A-B) intended to unify standards for the European Union, Japan, and the United States to facilitate mutual acceptance of stability data sufficient for registration by regulatory authorities in these jurisdictions [15]. Traditional ICH stability studies involve testing drug substances under specific storage conditions to assess thermal stability and sensitivity to moisture. These protocols mandate long-term testing over a minimum of 12 months at 25°C ± 2°C/60% RH ± 5% RH or at 30°C ± 2°C/65% RH ± 5% RH, with intermediate and accelerated testing covering a minimum of 6 months at 30°C ± 2°C/65% RH ± 5% RH and 40°C ± 2°C/75% RH ± 5% RH, respectively [15].
While this empirical, time-based approach remains the regulatory gold standard, it presents significant bottlenecks in fast-paced development environments. For virtual biotechs under pressure to reach Biologics License Application (BLA) quickly, or companies needing robust Chemistry, Manufacturing, and Controls (CMC) data for funding, waiting years for stability data constitutes a major constraint [88]. The industry is now witnessing a paradigm shift toward advanced modeling approaches that leverage predictive analytics, machine learning, and sophisticated kinetic models to forecast long-term stability with confidence much earlier in development timelines. These science and risk-based approaches can compensate for not having a complete real-time stability data set at the time of initial regulatory submission, thereby accelerating the availability of new medicines [89]. This guide provides a comprehensive comparison of these emerging methodologies against traditional approaches, offering experimental protocols and implementation frameworks for scientists navigating this evolving landscape.
Traditional Stability Assessment: ICH Guidelines and Limitations
The ICH Stability Framework
The traditional stability assessment paradigm, as defined by ICH guidelines, requires rigorous and tedious testing over extended periods to obtain preclinical stability data [15]. Stability studies were designed for monitoring and evaluating the quality of Active Pharmaceutical Ingredients (API) and Finished Pharmaceutical Products (FPP) under the influence of different factors such as environmental conditions (temperature, moisture, light), API-excipients interactions, packaging materials, shelf life, and container-closure systems during a certain period [15]. These studies are categorized into three types based on conditions applied: long-term, intermediate, and accelerated stability studies, with the stability-evaluation process often divided into three phases across the product life cycle [72].
The selection of batches for stability studies must follow specific requirements. Stability studies should include at least three batches of drug substance or drug product, with pilot-scale batches usable initially alongside a commitment to evaluate manufacturing-scale batches after product approval [72]. For products with a proposed shelf life longer than 12 months, material from long-term storage conditions should be tested every three months during the first year, every six months in the second year, and annually thereafter throughout the proposed shelf life [72]. This comprehensive approach ensures robust data collection but consumes considerable time and resources.
Limitations of Conventional Approaches
The conventional ICH approach presents several challenges in modern drug development contexts. The most significant limitation is the time required—at least 6 months of experimental laboratory work for accelerated studies alone to obtain preliminary stability data for regulatory dossiers [15]. For fast-moving biotechs with board-level pressure to reach key milestones quickly, or small companies needing robust CMC stories to secure funding, waiting years for stability data represents a major constraint where time is the currency of the entire project [88].
Additionally, traditional approaches consume precious material resources. For early-stage companies, drug substance is incredibly valuable, and using large quantities for long stability studies can be prohibitively costly [88]. These companies often operate with limited staff and resources, struggling with service providers who act more like academic labs than goal-oriented partners. The pressure to reach Investigational New Drug (IND) applications is immense, and every decision undergoes intense investor scrutiny [88]. For complex molecules and new modalities like viral vectors, antibody-drug conjugates (ADCs), and RNA therapies, these challenges are exacerbated as these molecules are often more sensitive to their environment, making formulation and stability a greater challenge with complicated degradation pathways difficult to predict with conventional methods [88].
Advanced Modeling Approaches: Methodologies and Comparative Advantages
Accelerated Predictive Stability (APS) Studies
Accelerated Predictive Stability studies have emerged as novel approaches to predict the long-term stability of pharmaceutical products more efficiently. APS studies are carried out over a 3-4 week period, combining extreme temperatures and RH conditions (40-90°C)/10-90% RH, in contrast to the 6-month minimum for ICH accelerated studies [15]. This approach provides a dataset in less than 1 month, saving time and reducing costs during preclinical development [15]. The fundamental principle involves subjecting products to stress conditions that accelerate degradation, then using mathematical models to extrapolate to standard storage conditions.
The implementation of APS studies during development of industrially fabricated medicines and extemporaneous compounding formulations offers significant advantages for rapid screening of formulation candidates. By predicting long-term stability from shorter-term, data-rich experiments, development programs can reach BLA or IND stages faster while conserving valuable material through efficient study designs that provide maximum information from minimum drug substance [88]. However, APS approaches require careful model validation and may have limitations for complex degradation pathways exhibiting non-linear behavior.
Advanced Kinetic Modeling (AKM)
Advanced Kinetic Modeling represents a more sophisticated approach to stability prediction, outperforming traditional ICH guidelines for biologic stability according to recent research [90]. AKM can accurately describe the complex behaviors of biologics, reducing risks from the developmental stage all the way through last-mile delivery [90]. The methodology involves generating a minimum of 20 to 30 data points from at least three different temperatures for modeling, with selection of kinetic models that adequately describe the evolution of considered quality attributes performed by screening Arrhenius-based equations of varying complexity and statistical analysis [90].
Research demonstrates dramatic differences between AKM and traditional approaches, particularly at elevated temperatures. At 25°C and 37°C, AKM proved notably more accurate for long-term stability predictions at recommended storage conditions than shelf-life estimation methods recommended by ICH guidelines [90]. This increased accuracy applies to any biopharmaceutical and stability studies of various critical quality attributes. Sanofi has successfully utilized AKM modeling for dose-saving of commercialized vaccines exposed to short temperature excursions during shipments and to accelerate technology transfers of well-known products or to extend their shelf-life without waiting for real long-term stability data [90]. Regulators are increasingly accepting these approaches, with the European Medicines Agency (EMA) accepting Sanofi's shelf-life estimation for its COVID-19 vaccine based on kinetic modeling and a few months of experimental stability data [90].
AI and Machine Learning Approaches
Artificial intelligence and machine learning represent the cutting edge of predictive stability, using computational modeling and scientific risk-based approaches to prospectively assess long-term stability and shelf-life of biotherapeutics and vaccines [91]. These approaches involve combining high-throughput analytical screening with AI-based stability prediction to map out formulation design spaces much faster than with traditional methods [88]. The technology is particularly valuable for complex modalities where predictive analytics can be most powerful in addressing unique instability issues not well-suited to standard screening protocols [88].
AI-driven predictive stability modeling encompasses various applications, including Bayesian statistics and machine learning applications with applicability to both synthetic and biological molecules [89]. For biologics, product-specific and platform prior knowledge can be used to overcome model limitations known for non-quantitative stability indicating attributes [89]. These approaches allow development teams to move into development with a much higher degree of confidence in their drug product's stability profile, transforming formulation development from a slow, step-by-step process into a dynamic, predictive science [88].
Table 1: Comparative Analysis of Stability Assessment Methodologies
| Methodology | Time Requirement | Data Points Required | Key Advantages | Regulatory Acceptance |
|---|---|---|---|---|
| ICH Guidelines | 6-12 months minimum | Standard testing intervals | Established gold standard, comprehensive data | Full acceptance for registration |
| APS Studies | 3-4 weeks | High-frequency sampling under stress conditions | Rapid screening, material efficiency | Emerging acceptance for development decisions |
| Advanced Kinetic Modeling | 1-3 months | 20-30 points across ≥3 temperatures | High accuracy for complex biologics | Case-by-case basis (e.g., EMA COVID-19 vaccine) |
| AI/ML Approaches | Variable (depends on data availability) | Large historical datasets | Handles complex modalities, pattern recognition | Early stage with encouraging regulatory signals |
Table 2: Application Scope Across Product Types
| Product Type | Traditional ICH | APS | AKM | AI/ML |
|---|---|---|---|---|
| Small Molecules | Excellent | Good | Good | Excellent |
| Monoclonal Antibodies | Good | Moderate | Excellent | Excellent |
| Vaccines | Good | Limited | Excellent [90] | Good |
| Advanced Therapies (Gene/Cell) | Challenging | Limited | Good | Excellent [88] |
| Conventional Dosage Forms | Excellent | Good | Good | Good |
Experimental Protocols and Implementation Frameworks
Protocol for Advanced Kinetic Modeling
Implementing Advanced Kinetic Modeling requires a systematic approach to generate robust, predictive data. Manufacturers should adopt good modeling practices and generate a minimum of 20 to 30 data points from at least three different temperatures for modeling [90]. The experimental workflow begins with study design, selecting appropriate stress conditions based on the molecule's characteristics. The selection of kinetic models that adequately describe the evolution of the considered quality attribute must be performed by screening Arrhenius-based equations of varying complexity and statistical analysis [90].
For protein therapeutics, a comprehensive stability assessment focuses on understanding degradation mechanisms—aggregation, oxidation, and chemical modifications—that can compromise product integrity [72]. Analytical testing includes quantification of drug-substance concentration using high-performance liquid chromatography with ultraviolet-light detection (HPLC-UV) and assessment of purity through size-exclusion chromatography (SEC) [72]. Additional tests include visual inspections for physical formulation changes such as color, clarity, and particulate formation, while advanced methods like liquid chromatography with mass spectrometry (LC-MS) can identify chemical modifications, such as oxidation, deamidation, and fragmentation [72]. Data from these analyses feed into kinetic models that project stability under recommended storage conditions.
AI and Predictive Analytics Implementation
The implementation framework for AI-driven predictive stability begins with data aggregation from diverse sources. Predictive analytics software requires specific capabilities: data preparation and management to process and clean large amounts of data from various sources; modeling and analysis using advanced statistical tools and machine learning models for precise predictions; and visualization and reporting to present complex data and analysis results in understandable formats [92]. For biopharma applications, the smart formulation platform approach combines high-throughput analytical screening with AI-based stability prediction to map out formulation design spaces much faster than with traditional methods [88].
A successful ongoing verification approach by comparing predicted data with real-time stability data represents an appropriate risk management strategy intended to address regulatory concerns and further build confidence in the robustness of these predictive modelling approaches with regulatory agencies [89]. This validation framework is essential for regulatory acceptance, as global regulatory acceptance of stability modeling could allow patients to receive potential life-saving medications faster without compromising quality, safety, or efficacy [89].
Diagram 1: Stability Assessment Pathways: Traditional vs Predictive. This workflow compares the sequential traditional ICH pathway with the iterative predictive modeling approach, highlighting significant time savings through parallel modeling and verification processes.
Essential Research Reagent Solutions for Stability Modeling
Implementing advanced stability modeling approaches requires specific analytical tools and computational resources. The selection of appropriate reagents and platforms is critical for generating robust data for predictive models. Below is a comprehensive table of essential research solutions for stability modeling experiments.
Table 3: Essential Research Reagent Solutions for Stability Modeling
| Category | Specific Tools/Platforms | Function in Stability Modeling | Application Context |
|---|---|---|---|
| Statistical Analysis | Regression analysis, ANCOVA | Modeling degradation trends, ensuring batch consistency | Precise determination of expiration dates [72] |
| Kinetic Modeling | Arrhenius-based equations | Long-term stability predictions using accelerated data | Predicting product behavior at standard storage conditions [72] |
| Predictive Analytics Software | SAS Viya, RapidMiner, Prophet | Automated forecasting, ML model development | Handling large datasets, generating stability projections [93] [92] |
| Chromatographic Systems | HPLC-UV, SEC, IEC, LC-MS | Drug substance quantification, purity assessment, charge variants | Monitoring chemical stability, detecting degradation [72] |
| Structural Analysis | DSC, CD spectroscopy | Protein thermal stability, secondary structure integrity | Confirming physical stability over time [72] |
| AI/ML Platforms | Custom Python scripts, One AI | Predictive model development, pattern recognition | Formulation optimization, stability forecasting [88] |
Regulatory Landscape and Implementation Strategy
Evolving Regulatory Perspectives
Regulatory bodies like the FDA and EMA are actively encouraging the use of innovative technologies, including AI and machine learning, in drug development [88]. They recognize the potential for these tools to accelerate timelines and increase understanding of product attributes [88]. Provided models are validated and data is robust, predictive stability data can be a valuable part of regulatory submissions, especially for programs on accelerated pathways [88]. The European Medicines Agency's acceptance of Sanofi's shelf-life estimation for its COVID-19 vaccine based on kinetic modeling and limited experimental stability data represents a significant milestone in regulatory flexibility [90].
Globally, Advanced Kinetic Modeling is being discussed by multiple stability working groups for integration into international guidelines [90]. This evolving regulatory landscape creates opportunities for sponsors to incorporate predictive approaches into their development strategies. A successful ongoing verification approach comparing predicted data with real-time stability data represents an appropriate risk management strategy to address regulatory concerns while building confidence in these innovative approaches [89].
Strategic Implementation Framework
Implementing predictive stability modeling requires a phased, scientifically justified approach. For early development phases, APS studies are ideal for rapid screening of formulation candidates and identifying potential degradation pathways [15]. As programs advance, AKM provides more accurate long-term predictions, particularly for complex biologics where traditional accelerated studies may be misleading [90]. For established products, predictive analytics can support shelf-life extensions and manufacturing site transfers without waiting for complete real-time data [90].
Material requirements for predictive approaches are significantly lower than traditional stability programs, making them particularly valuable for early-stage programs where drug substance is scarce and expensive [88]. The implementation should include commitments to ongoing verification through comparative analysis of predicted and real-time data as it becomes available [89]. This demonstrates a science-based approach to model validation while providing regulators with necessary assurance of product quality throughout the shelf life.
The evolution of stability assessment from purely empirical time-based studies to sophisticated predictive modeling represents a significant advancement in pharmaceutical development. While traditional ICH guidelines remain the gold standard for regulatory submissions, advanced approaches like Accelerated Predictive Stability studies, Advanced Kinetic Modeling, and AI-driven predictive analytics offer powerful complementary tools for accelerating development timelines and conserving resources. The comparative data presented in this guide demonstrates that these methodologies can provide equivalent or superior predictive accuracy compared to conventional approaches, particularly for complex biologics and advanced therapies.
For researchers and drug development professionals, the optimal strategy involves integrating traditional and predictive approaches throughout the product lifecycle. Early development benefits from rapid screening capabilities of APS and AI-driven platforms, while later stages gain from the accuracy of AKM for shelf-life determination. Regulatory acceptance continues to evolve positively, with agencies recognizing the value of these science-based approaches. As the industry continues adopting these methodologies, stability modeling will increasingly transform from a regulatory hurdle into a strategic advantage, accelerating patient access to novel therapies without compromising quality or safety.
In the dynamic landscape of pharmaceutical manufacturing, post-approval changes are inevitable. Companies implement process improvements, formulation updates, and scale-up activities to enhance efficiency, ensure supply, or improve product characteristics. However, these modifications can potentially alter the stability profile of a drug substance or product, necessitating a scientific evaluation of whether existing analytical methods remain capable of detecting these changes. Within the framework of ICH guidelines, analytical method re-validation becomes a critical bridge between product changes and continued quality assurance [12] [1].
The recent overhaul of ICH stability (Q1) and analytical validation (Q2(R2)) guidelines provides a more integrated, modern framework for this endeavor [4] [9] [94]. The new ICH Q1 guideline, a consolidated document five times longer than its predecessor, emphasizes a science- and risk-based approach aligned with Quality by Design principles and encourages considering stability throughout the product lifecycle [9] [95]. Simultaneously, the final ICH Q2(R2) guideline provides the general framework for the principles of analytical procedure validation [94]. For researchers and drug development professionals, understanding the interplay between these guidelines is essential for designing an efficient yet compliant re-validation strategy during post-approval changes. This guide objectively compares the scope, requirements, and strategic approaches to method re-validation under the current regulatory landscape.
Regulatory Framework: ICH Q1 and Q2(R2) in Context
The Evolution of ICH Stability Guidelines (Q1)
The ICH Q1 guideline has undergone its most significant update in over 20 years. The new draft, released for consultation in April 2025, consolidates the previous Q1A(R2), Q1B, Q1C, Q1D, Q1E, and Q5C guidelines into a single, comprehensive document [4] [9]. This 108-page guideline is structured into 18 sections and three annexes, designed to be considered in its entirety for a comprehensive approach to stability studies [9].
Key advancements in the new Q1 draft include:
- Broader Scope: Explicitly applies to a wider variety of products, including advanced therapy medicinal products (ATMPs), vaccines, oligonucleotides, proteins, and combination products with devices, which were not previously covered in detail [9] [95].
- Lifecycle Focus: Introduces a dedicated section on stability lifecycle management, aligning more closely with ICH Q12 [9] [95].
- Enhanced Risk-Based Approaches: Encourages more flexible, science-based study designs tailored to the product and its intended market [95].
- New Content Areas: Adds a new section (Section 12) addressing stability considerations for reference materials, novel excipients, and adjuvants due to their significant potential impact on drug product quality [9].
Analytical Procedure Validation and Development: ICH Q2(R2) and Q14
The ICH Q2(R2) guideline, finalized in March 2024, provides a general framework for the principles of analytical procedure validation [94]. It serves as a collection of terms and their definitions and discusses the elements for consideration during validation of analytical procedures used in registration applications [12]. It is complemented by ICH Q14 on Analytical Procedure Development, which facilitates more efficient, science-based, and risk-based post-approval change management [94].
The scope of ICH Q2(R2) covers validation tests for procedures used for release and stability testing of commercial drug substances and products, both chemical and biological/biotechnological. It can also be applied to other analytical procedures used as part of the control strategy following a risk-based approach [12].
Method Re-validation Triggers: A Comparative Analysis of Change Types
Not all post-approval changes carry the same risk to analytical method performance. The need for and extent of re-validation should be governed by a science- and risk-based assessment of the change. The following table summarizes common post-approval changes and their typical impact on analytical method re-validation requirements.
Table 1: Re-validation Requirements for Common Post-Approval Changes
| Change Category | Specific Examples | Potential Impact on Stability Profile | Recommended Re-validation Actions |
|---|---|---|---|
| Formulation Changes | Change in excipient grade/vendor; Minor qualitative/quantitative formula change | Altered potential for drug-excipient interactions; New degradation pathways | Specificity (for new impurities); Accuracy and Precision for assay in new matrix |
| Process Changes | Scale-up; Change in equipment principle; New synthesis pathway for drug substance | Potential for new impurity profiles; Changes in polymorphic form or particle size | Specificity (to resolve new impurities); Detection Limit/Quantitation Limit for new impurities |
| Container Closure System | Change in primary packaging material; New delivery device | Altered moisture/oxygen protection; Potential for new leachables | Specificity (to separate leachables); Forced degradation studies to confirm method stability-indicating nature |
| Manufacturing Site Transfer | Transfer to a new facility with similar equipment and controls | Typically low risk if process is well-controlled and scaled appropriately | Robustness testing to confirm method performance under new laboratory conditions; Comparative testing |
The foundation for this risk-based approach is underscored in the new ICH Q1 guideline, which emphasizes that the outcomes of development stability studies (Section 2) are essential for developing stability-indicating analytical methods and understanding degradation pathways [9]. When a process or formulation change occurs, this prior knowledge is critical for assessing which analytical methods may be affected.
Experimental Protocols for Re-validation
Protocol 1: Forced Degradation Studies for Specificity Assessment
Objective: To confirm that an analytical procedure can unequivocally quantify the analyte in the presence of new potential degradation products that may form due to a process or formulation change [9].
Methodology:
- Sample Preparation: Prepare samples of the drug substance (with new synthesis pathway) or drug product (with new formulation/process) along with appropriate blanks.
- Stress Conditions: Apply relevant stress conditions to deliberately degrade the samples [9]. These should be more severe than accelerated conditions and may include:
- Acidic/Basic Hydrolysis: Treat with 0.1-1M HCl or NaOH at elevated temperature (e.g., 40-70°C) for several hours.
- Oxidative Stress: Expose to 0.1-3% hydrogen peroxide at room temperature.
- Thermal Stress: Solid-state stress at 10-20°C above accelerated storage conditions.
- Photostability: Follow ICH Q1B options [9].
- Analysis: Inject stressed samples into the chromatographic system (e.g., HPLC/UPLC) and compare the chromatograms with those of unstressed samples.
- Data Evaluation: Assess peak purity (e.g., using a PDA detector) of the main analyte peak to ensure no co-elution with degradation products. The method should adequately resolve all degradation peaks from the main peak and from each other.
Protocol 2: Partial Validation for an Updated Assay Method
Objective: To demonstrate that a previously validated assay method remains accurate, precise, and linear for a drug product with a modified formulation.
Methodology:
- Accuracy (Recovery): Spike known amounts of the drug substance into the new placebo blend (representing the modified formulation) at three concentration levels (e.g., 80%, 100%, 120% of the target concentration). Analyze these samples and calculate the percentage recovery of the analyte.
- Precision:
- Repeatability: Analyze six independent sample preparations of the drug product (with the new formulation) at 100% of the test concentration. Calculate the relative standard deviation (RSD) of the results.
- Intermediate Precision: Perform the same analysis on a different day, with a different analyst, and/or using a different instrument. The combined RSD should meet predefined criteria.
- Linearity: Prepare standard solutions of the analyte at a minimum of five concentration levels, from below to above the expected range (e.g., 50-150%). Plot the instrument response versus concentration and determine the correlation coefficient, y-intercept, and slope of the regression line.
The principles for deriving and evaluating these validation tests are outlined in ICH Q2(R2) [12]. The extent of validation should be based on the nature of the change, as illustrated in Table 1.
The Scientist's Toolkit: Essential Reagent Solutions
Table 2: Key Research Reagents for Analytical Re-validation Studies
| Reagent/Material | Function in Re-validation | Critical Quality Attributes |
|---|---|---|
| Pharmaceutical Grade Active Pharmaceutical Ingredient (API) | Serves as the primary reference standard for accuracy, linearity, and specificity studies. | High purity (>98.5%), fully characterized identity, known impurity profile. |
| New Placebo/Excipient Blend | Represents the modified formulation matrix without the API for specificity and accuracy (recovery) studies. | Represents the new commercial-grade excipient composition and ratio. |
| Forced Degradation Reagents (e.g., HCl, NaOH, Hâ‚‚Oâ‚‚) | Used to generate degradation products for specificity assessment of the method towards new potential impurities. | ACS reagent grade or equivalent, with known concentration and stability. |
| HPLC/UPLC Grade Solvents and Buffers | Constitute the mobile phase for chromatographic separations; critical for robustness and transfer. | Low UV absorbance, specified purity, pH of buffers accurately prepared and documented. |
| Chromatographic Columns | Stationary phase for separation; a key parameter in method robustness and specificity. | Columns from the same manufacturer and with the same ligand chemistry as the validated method. |
Strategic Workflow for Planning Re-validation
Navigating the re-validation process for a post-approval change requires a systematic, risk-based workflow. The following diagram illustrates the logical sequence of decision points and actions, from the initial change trigger to the final regulatory submission, ensuring a compliant and scientifically sound approach.
Decision Workflow for Method Re-validation
This workflow emphasizes the critical role of risk assessment, which should be informed by prior knowledge from development stability studies as emphasized in the new ICH Q1 guideline [9], the nature of the change, and the Analytical Target Profile (ATP). The outcome of the data evaluation dictates the subsequent steps, ensuring that a failure to re-validate triggers a more fundamental method improvement or development activity.
The harmonized, modernized ICH Q1 and Q2(R2) guidelines provide a robust framework for managing analytical method performance in an evolving product lifecycle. The key to successful re-validation for post-approval changes lies in a proactive, science-driven strategy. This involves leveraging prior knowledge from development studies, implementing a risk-based approach to define the scope of re-validation, and understanding the specific implications of different change types on the analytical procedure. By integrating stability and analytical expertise, pharmaceutical professionals can ensure that their control strategies remain effective, compliant, and agile, thereby safeguarding product quality and patient safety while enabling continuous improvement throughout the product's commercial life.
The validation of analytical methods is a cornerstone of pharmaceutical development, ensuring that drug products are safe, efficacious, and of consistent quality throughout their shelf life. While foundational guidelines from the International Council for Harmonisation (ICH), such as the recently revised ICH Q2(R2) on analytical procedure validation, provide a harmonized framework, the application of these principles varies significantly across different product types. A comparative analysis reveals that the validation strategies for traditional small molecules, complex biologicals like vaccines, and innovative Advanced Therapy Medicinal Products (ATMPs) are shaped by their distinct molecular complexities, stability profiles, and manufacturing processes. Framed within the context of a broader thesis on validating analytical methods for drug stability testing, this guide objectively compares the analytical validation and stability requirements for these three categories, underscoring a critical industry shift from a one-size-fits-all checklist to a science- and risk-based lifecycle approach [96] [97].
The recent consolidation of stability guidelines into the new ICH Q1 draft and the modernization of validation principles in ICH Q2(R2) and ICH Q14 reflect a concerted effort to address the entire spectrum of modern medicines, from synthetic chemicals to cell and gene therapies [96] [3]. This evolving regulatory landscape demands that researchers and developers not only understand the core validation parameters but also how to adapt them for products with unique challenges, such as the short shelf-life of autologous cell therapies or the complex potency assays for vaccines. This analysis will dissect these differences through structured comparisons, detailed experimental protocols, and visualizations to serve as a practical resource for drug development professionals.
Regulatory Framework and Core Guidelines
The regulatory framework for analytical validation is built upon a hierarchy of ICH guidelines, which are subsequently adopted by regional authorities like the FDA and EMA. The following diagram illustrates the logical relationships between the core guidelines governing analytical procedure validation and stability testing for different product categories.
The core guidelines create an interconnected system. ICH Q2(R2) defines the validation parameters for analytical procedures, while its complementary guideline, ICH Q14, provides a framework for systematic, risk-based analytical procedure development, introducing concepts like the Analytical Target Profile (ATP) [98] [97]. The ICH Q1 Draft guideline consolidates previous stability guidelines (Q1A-R2, Q1B, Q5C, etc.) into a single document, establishing a modernized, unified framework for stability testing that explicitly includes advanced therapies [96] [3]. ICH Q9 (Quality Risk Management) underpins all these activities, promoting a proactive, risk-based approach that is particularly critical for complex products like ATMPs and vaccines [97].
Comparative Analysis of Validation Requirements
Analytical Method Validation Parameters
The core validation parameters defined in ICH Q2(R2)—such as accuracy, precision, and specificity—are universally applicable. However, their relative importance and the methodologies used to assess them differ markedly based on product complexity [12] [97].
Table 1: Comparison of Key Analytical Validation Parameters
| Validation Parameter | Small Molecules | Vaccines (Biologics) | ATMPs (Cell & Gene Therapies) |
|---|---|---|---|
| Potency Assay | Standardized chemical assay for strength. | Critical; requires a cell-based bioassay reflecting mechanism of action (e.g., immunogenicity). | Highly critical; complex functional assays measuring biological response (e.g., cell killing, gene expression) [11]. |
| Specificity/ Identity | Chromatographic methods (HPLC) to distinguish from impurities. | Techniques (e.g., PCR, MS) to identify antigenic components and vector identity (for viral vectored vaccines). | Multiple orthogonal methods (e.g., flow cytometry, NGS) to identify product and process-related impurities [11]. |
| Purity/ Impurities | Focus on process-related and degradation impurities. | Focus on product-related variants (aggregation, fragmentation) and process residuals (host cell DNA/protein). | Distinction between product and process-related impurities is complex; requires monitoring of ancillary materials [11]. |
| Accuracy & Precision | High, readily achievable with chemical standards. | More variable due to biological matrix interference; emphasis on assay robustness. | Variable; phase-appropriate expectations. High precision can be challenging for live cell-based systems [11] [99]. |
| Lifecycle Approach | Traditional validation often sufficient. | Benefits from enhanced approach with ATP for complex bioassays. | Essential; requires phase-appropriate validation and frequent updates based on product knowledge [11] [97]. |
For ATMPs, regulators explicitly encourage the use of orthogonal methods—employing different scientific principles to measure the same attribute—to build confidence in critical quality attributes like identity, potency, and purity [11]. For example, a gene therapy program might use both qPCR and next-generation sequencing (NGS) to assess vector genome integrity.
Stability Testing Considerations
The stability testing requirements for these product categories are undergoing significant modernization under the new ICH Q1 draft, which expands its scope beyond traditional molecules [96].
Table 2: Comparison of Stability Testing Strategies
| Stability Aspect | Small Molecules | Vaccines (Biologics) | ATMPs (Cell & Gene Therapies) |
|---|---|---|---|
| Primary Focus | Chemical degradation and potency over time. | Physical and biological stability (e.g., antigen aggregation, loss of immunogenicity). | Maintenance of biological function and viability; often a short shelf-life [96]. |
| Storage Conditions | Standard ICH conditions (e.g., 5°C ± 3°C, 25°C/60%RH). | Often refrigerated (2-8°C) or frozen (-20°C or lower) to maintain stability; cold chain is critical. | Often cryopreserved at ultra-low temperatures (e.g., -150°C to -196°C in vapor phase LN2) [99]. |
| Shelf-Life Definition | Based on long-term real-time data with statistical modeling. | Real-time data is essential; accelerated data may have limited predictive value. | Real-time data is critical due to complex degradation pathways; first ICH guidance provided in Annex 3 of new Q1 draft [96] [3]. |
| In-Use Stability | Standardized for reconstitution if needed. | Critical for lyophilized or multi-dose vials; must demonstrate stability after reconstitution/dilution. | Critical for products requiring thawing, washing, or transport to bedside; studies must mimic clinical handling [99]. |
| Stability-Indicating Methods | Well-established (e.g., HPLC for assay and related substances). | Require multiple methods to monitor different attributes (e.g., SE-HPLC, CIEF, bioassay). | Require a multivariate panel of assays (potency, viability, identity, sterility) to fully characterize stability [11] [96]. |
The new ICH Q1 draft formally integrates stability lifecycle management, reframing stability from a pre-approval activity to a continuous process throughout the product's commercial life, which is especially relevant for ATMPs whose profiles may be refined post-approval [96].
Manufacturing Process and Control Validation
The nature of the manufacturing process directly influences the control strategy and associated validation activities.
Table 3: Comparison of Manufacturing and Control Validation
| Manufacturing Aspect | Small Molecules | Vaccines (Biologics) | ATMPs (Cell & Gene Therapies) |
|---|---|---|---|
| Process Scale | Large, scalable batch processes. | Batch processes, though often multi-step and complex. | Often small-scale, patient-specific (autologous) or small-batch (allogeneic) [99]. |
| Process Validation | Focuses on demonstrating consistent, reproducible output at commercial scale (PPQ). | Similar to small molecules but with greater focus on controlling bioreactor conditions and aseptic processing. | For autologous therapies, validation focuses on the consistency and robustness of the process platform across numerous individual batches [99]. |
| Starting Materials | Well-defined chemical intermediates. | Well-defined cell banks and reagents; GMP-grade. | High-quality input materials are critical; research-grade materials are not acceptable. EMA requires genome editing machinery to be defined as starting materials [11]. |
| Capacity Expansion | Adding large-scale equipment or new production lines. | Complex but follows scalable unit operations. | Complex due to single-patient batches; options include adding manufacturing suites/sites, requiring re-validation (APS, PPQ, comparability) [99]. |
For autologous cell therapies, "capacity expansion" does not mean making a larger batch, but rather increasing the number of individual manufacturing suites or sites to serve more patients, each requiring rigorous validation such as Aseptic Process Simulation (APS) and Process Performance Qualification (PPQ) [99].
Detailed Experimental Protocols
Protocol for Potency Assay Validation for an ATMP
This protocol outlines the key experiments for validating a critical potency assay for a cell-based ATMP, such as a CAR-T product, based on expectations for functional, biologically relevant assays [11].
- Objective: To validate a cell-based cytotoxicity assay that measures the ability of CAR-T cells to lyse target tumor cells, ensuring it is accurate, precise, and specific for its intended use in stability testing and lot release.
- Materials:
- Research Reagent Solutions:
- CAR-T Cells: The investigational Advanced Therapy Medicinal Product (ATMP).
- Target Cells: Tumor cell line expressing the target antigen.
- Control Cells: Isogenic tumor cell line not expressing the target antigen (for specificity).
- Cytotoxicity Detection Reagent: Such as lactate dehydrogenase (LDH) or a fluorescent dye measuring membrane integrity.
- Cell Culture Medium: Appropriate media for maintaining target and effector cells.
- Reference Standard: A well-characterized cell sample for system suitability and assay control.
- Research Reagent Solutions:
- Methodology:
- Assay Design: Co-culture CAR-T cells with target cells at multiple Effector:Target (E:T) ratios in a 96-well plate. Include controls for spontaneous lysis (target cells alone) and maximum lysis (target cells with detergent).
- Specificity: Perform the assay using the control cells (antigen-negative) to demonstrate that measured cytotoxicity is antigen-specific.
- Accuracy & Precision:
- Accuracy: Spiking recovery experiments by adding a known number of CAR-T cells to a fixed number of target cells and comparing measured vs. expected lysis.
- Precision:
- Repeatability: Have one analyst perform the assay at least 6 times on the same day with the same cell preparations.
- Intermediate Precision: Have two analysts perform the assay on three different days using different reagent lots.
- Linearity & Range: Test a range of CAR-T cell concentrations (covering the proposed E:T ratios) to establish the linear dynamic range of the assay and the limits of quantitation.
- Robustness: Deliberately introduce small variations in critical parameters (e.g., incubation time ±30 minutes, reagent volume ±5%) to determine the assay's robustness.
- Data Analysis: Calculate percent cytotoxicity for each test condition. Use linear regression for the linearity assessment. Calculate mean, standard deviation, and percent coefficient of variation (%CV) for precision. A %CV of less than 20-25% is often considered acceptable for complex bioassays.
Protocol for a Comparative Stability Study Under the ICH Q1 Framework
This protocol applies the new ICH Q1 draft principles to design a stability study comparing the three product categories, emphasizing their unique stress factors [96] [3].
- Objective: To evaluate and compare the stability profiles of a small molecule drug, a subunit vaccine, and a cell-based ATMP under long-term and accelerated storage conditions.
- Materials:
- Research Reagent Solutions:
- Small Molecule: Drug substance and final drug product in its commercial packaging.
- Vaccine: Lyophilized or liquid antigen formulation in its final vial.
- ATMP: Cryopreserved bag or vial of the cell therapy product.
- Stability Chambers: Qualified chambers capable of maintaining specified temperature and humidity conditions.
- Analytical Instrumentation: HPLC (small molecule), SE-HPLC and ELISA (vaccine), Flow Cytometer and Cell Counter (ATMP).
- Research Reagent Solutions:
- Methodology:
- Study Design: A bracketing or matrixing design can be proposed, justified by a risk assessment as per ICH Q1, to reduce testing burden without compromising knowledge.
- Storage Conditions:
- Small Molecule: 25°C/60% RH (Long-Term) and 40°C/75% RH (Accelerated).
- Vaccine: 5°C ± 3°C (Long-Term) and 25°C/60% RH (Accelerated).
- ATMP: Stored in vapor phase liquid nitrogen (-150°C to -196°C) or as specified by the manufacturer. In-use stability: Thaw and hold at room temperature for a defined period (e.g., 1-4 hours) with sampling.
- Testing Timepoints: 0, 3, 6, 9, 12, 18, 24, 36 months for long-term; 0, 3, 6 months for accelerated.
- Testing Attributes:
- Small Molecule: Appearance, assay/potency, related substances, degradation products, water content.
- Vaccine: Appearance (color, clarity), potency (immunoassay or bioassay), purity (SE-HPLC), pH, sterility, endotoxin.
- ATMP: Viability (trypan blue exclusion), total cell count, potency (e.g., cytotoxicity assay), identity (flow cytometry for surface markers), sterility, and vector copy number (for gene therapies).
- Data Analysis: Use statistical modeling as encouraged in the new ICH Q1 Annex 2. For small molecules, linear regression is typically used to establish shelf-life. For biologics and ATMPs, where degradation may not follow linear kinetics, more complex models may be required. The data will be evaluated against pre-defined acceptance criteria for each product.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting the validation and stability studies described in this guide.
Table 4: Key Research Reagent Solutions for Validation & Stability Studies
| Reagent/Material | Function & Application |
|---|---|
| Qualified/Validated Assays | Pre-optimized and characterized test methods (e.g., ELISA kits, PCR assays) used for quantifying specific analytes like proteins or nucleic acids, reducing development time [11]. |
| Characterized Cell Banks | Well-documented Master and Working Cell Banks used in bioassays for vaccines and ATMPs, ensuring consistency and reproducibility in functional potency tests [11]. |
| Reference Standards | Highly characterized samples of the drug substance or product with a defined purity and potency, used as a benchmark for system suitability and quantifying test samples in assays [11] [3]. |
| GMP-Grade Starting Materials | Raw materials (e.g., cytokines, growth factors, viral vectors) manufactured under Good Manufacturing Practice standards, which are critical for ATMP production and are expected by regulators to ensure patient safety [11]. |
| Stability-Specific Analytical Tools | Instruments and associated reagents for key tests: HPLC/UPLC (small molecule purity), Cell Counters & Flow Cytometers (ATMP viability/identity), NGS Systems (orthogonal testing for gene therapy vector integrity) [11]. |
The comparative analysis underscores that a nuanced, product-specific approach is paramount for the successful validation of analytical methods and stability protocols. While small molecules adhere to well-established and highly predictable pathways, vaccines introduce a layer of biological complexity that demands a robust control strategy centered on functional potency. ATMPs reside in a distinct paradigm, where the living product itself necessitates a highly flexible, phase-appropriate, and orthogonal validation strategy, often under evolving regulatory guidance.
The ongoing modernization of ICH guidelines, particularly Q1, Q2(R2), and Q14, provides a framework that embraces this diversity through science- and risk-based principles and lifecycle management. For researchers and drug development professionals, mastering the application of these universal principles to the unique challenges of each product category is not just a regulatory requirement, but a critical enabler for efficiently bringing safe and effective medicines—from traditional chemicals to transformative cell and gene therapies—to patients in need.
Conclusion
The successful validation of analytical methods for stability testing is no longer a standalone activity but an integral part of a holistic, science- and risk-based product lifecycle strategy. The harmonized 2025 ICH Q1 guideline, together with ICH Q2(R2) and Q14, demands a proactive approach where deep product understanding and robust, validated methods are paramount. As the industry advances with complex modalities like ATMPs, the principles outlined here will be crucial. Future directions will increasingly rely on predictive stability modeling and enhanced real-time monitoring, pushing the boundaries of traditional stability science and ensuring that innovative therapies reach patients with guaranteed quality, safety, and efficacy throughout their shelf life.
References
- 1. ICH Q1 guideline on stability testing of drug substances and ... [https://www.ema.europa.eu/en/ich-q1-guideline-stability-testing-drug-substances-drug-products]
- 2. New ICH Q1 Draft Guideline - What's Changing in Stability ... [https://www.gmp-compliance.org/gmp-news/new-ich-q1-draft-guideline-whats-changing-in-stability-testing]
- 3. ICH Q1 Draft Guideline Marks a New Era for Stability Testing [https://stabilityhub.com/2025/09/07/ich-q1-draft-guideline-marks-a-new-era-for-stability-testing/]
- 4. Q1 Stability Testing of Drug Substances and Drug Products [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q1-stability-testing-drug-substances-and-drug-products]
- 5. ICH Q1A (R2) Stability testing of new drug substances and ... [https://www.ema.europa.eu/en/ich-q1a-r2-stability-testing-new-drug-substances-drug-products-scientific-guideline]
- 6. Drug Development – ICH Q1 Revision: A New Era for ... [https://rpngroup.com/insights/drug-development-ich-q1-revision-a-new-era-for-global-stability-testing/]
- 7. ICH Guidelines: Drug Stability Testing Essentials [https://amsbiopharma.com/ich-guidelines-drug-stability-testing/]
- 8. Stability Storm 2025: How ICH Q1's Overhaul is Shaking Up [https://www.linkedin.com/pulse/stability-storm-2025-how-ich-q1s-overhaul-shaking-up-small-biotech-5jtie]
- 9. The ICH Just Released Its Overhauled Stability Guideline ... [https://insider.thefdagroup.com/p/ich-q1]
- 10. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 11. Where the US and EU differ and overlap with CGTs/ATMPs [https://www.pharmalex.com/thought-leadership/blogs/qa-for-innovators-navigating-the-complex-regulatory-world-of-atmps-cgts/]
- 12. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 13. Federal Register :: Q1 Stability Testing of Drug Substances and Drug Products; International Council for Harmonisation; Draft Guidance for Industry; Availability [https://www.federalregister.gov/documents/2025/06/24/2025-11552/q1-stability-testing-of-drug-substances-and-drug-products-international-council-for-harmonisation]
- 14. ICH Guidance Q1: Stability Testing of Drug Substances and Drug Products (Step 2 Draft 2025)- Public Consultation [https://www.regulatoryaffairsnews.com/post/ich-guidance-q1-stability-testing-of-drug-substances-and-drug-products-step-2-draft-2025-public]
- 15. ICH versus Accelerated Predictive Stability Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC9693625/]
- 16. Validation of Stability-Indicating HPLC Methods for ... [https://www.chromatographyonline.com/view/validation-of-stability-indicating-hplc-methods-for-pharmaceuticals-overview-methodologies-and-case-studies]
- 17. Understanding ICH Q7, Q8, Q9 & Q10: Guide for pharma ... [https://www.ideagen.com/thought-leadership/blog/difference-between-ich-q7-ich-q8-ich-q9-ich-q10]
- 18. ICH Q8, Q9, and Q10: A Complete Guide to ... [https://www.dotcompliance.com/blog/pharmaceutical-manufacturing/ich-q8-q9-and-q10-a-complete-guide-to-pharmaceutical-quality/]
- 19. Building a Maturity Model for Pharmaceutical Change Control [https://investigationsquality.com/2025/03/30/building-a-maturity-model-for-pharmaceutical-change-control-integrating-ich-q8-q10/]
- 20. Update of Training Material for ICH Q8, Q9 and Q10 [https://www.gmp-compliance.org/gmp-news/update-of-training-material-for-ich-q8-q9-and-q10]
- 21. What you need to know about ICH Q8 [https://www.qualio.com/blog/ich-q8]
- 22. Guide to ICH Q7, Q8, & Q9: GMP, QbD, and QRM Standards [https://intuitionlabs.ai/articles/ich-q7-q8-q9-guide]
- 23. Analytical Methods - USP's Future Expectations [https://www.gmp-compliance.org/gmp-news/analytical-methods-usps-future-expectations]
- 24. Choices of chromatographic methods as stability indicating ... [https://www.sciencedirect.com/science/article/pii/S2405844021006563]
- 25. Using the Analytical to Drive the Target ... Profile Analytical Method [https://pubmed.ncbi.nlm.nih.gov/30624912/]
- 26. Quality by design paradigm for optimization of green stability ... [https://www.nature.com/articles/s41598-023-37548-5?error=cookies_not_supported&code=9c557a36-c568-4d72-8b09-458e450cda44]
- 27. ICH Q1A Storage Stability Testing [https://jordilabs.com/lab-testing/regulatory/ich-q1a-storage-stability-testing/]
- 28. ICH Guidelines for Analytical Method Validation Explained [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 29. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 30. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 31. Understanding the Four Types of Analytical Method ... [https://www.oxford-analytical.co.uk/understanding-the-four-types-of-analytical-method-validation/]
- 32. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 33. Design, Analysis and Interpretation of Method-Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 34. Comparative analysis and validation of analytical ... [https://www.sciencedirect.com/science/article/abs/pii/S0019452224000530]
- 35. Quo Vadis Analytical Procedure Development and ... [https://www.chromatographyonline.com/view/quo-vadis-analytical-procedure-development-and-validation-]
- 36. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 37. What is meant by the limit of detection and quantification (LOD ... [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/limit-of-detection-quantifcation]
- 38. Understanding the Importance of Analytical Method ... [https://www.linkedin.com/posts/brian-king-ori-112908249_analytical-method-validation-is-fundamental-activity-7364229783284498433-Y-Zk]
- 39. Detection limit [https://en.wikipedia.org/wiki/Detection_limit]
- 40. A tutorial for computing limits of detection and ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267021011685]
- 41. What is the difference between Limit of Detection (LOD) ... [https://lab-training.com/difference-limit-detection-lod-limit-quantification-loq/]
- 42. LOD / LOQ - visionCATS's documentation! - CAMAG [https://visioncats-doc.camag.com/302/RegularUserDocumentation/method_analysis_file/evaluation/lodloq.html]
- 43. System Suitability Testing: Ensuring Reliable Results [https://www.labmanager.com/system-suitability-testing-ensuring-reliable-results-34248]
- 44. System suitability Requirements for a USP HPLC Method [https://www.mtc-usa.com/kb-article/aa-03965]
- 45. Are You Sure You Understand USP ? [https://www.chromatographyonline.com/view/are-you-sure-you-understand-usp-621-]
- 46. System suitability test for LC and GC assays - EDQM FAQs [https://faq.edqm.eu/pages/viewpage.action?pageId=111247388]
- 47. Stability Toolkit for the Appraisal of Bio/Pharmaceuticals ... [https://www.mdpi.com/2673-4532/6/3/25]
- 48. Design and validation of a robust stability-indicating reversed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619242/]
- 49. System Suitability in HPLC Analysis [https://www.pharmaguideline.com/2017/09/system-suitability-in-hplc-analysis.html]
- 50. In Silico High-Performance Liquid Chromatography ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11983366/]
- 51. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 52. Navigating ICH Q2(R2) compliance in analytical method ... [https://pubmed.ncbi.nlm.nih.gov/40154788/]
- 53. Innovations in Liquid Chromatography: 2025 HPLC ... [https://www.chromatographyonline.com/view/innovations-in-liquid-chromatography-2025-hplc-column-and-accessories-review]
- 54. Machine learning anomaly detection of automated HPLC ... [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d5dd00253b]
- 55. Observational Study to Compare Biological Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11048504/]
- 56. Measurement of Anti-TNF Biologics in Serum Samples ... [https://www.mdpi.com/1999-4923/17/4/421]
- 57. ELISA testing gets faster and more reproducible [https://www.nature.com/articles/d42473-025-00230-7]
- 58. Biopharmaceutical analysis — current analytical ... [https://link.springer.com/article/10.1007/s00216-025-06036-2]
- 59. Challenges in Analytical Method Development and ... [https://www.biopharminternational.com/view/challenges-analytical-method-development-and-validation]
- 60. Validation Challenges for Advanced Therapies [https://www.bioprocessintl.com/cell-therapies/analytical-method-validation-challenges-for-advanced-therapies-using-gene-therapies-as-an-example]
- 61. Challenges of Analytical Method Validation for ATMPs [https://www.pda.org/pda-letter-portal/home/full-article/challenges-of-analytical-method-validation-for-atmps]
- 62. Navigating FDA Guidelines for Combination Products [https://redica.com/navigating-fda-guidelines-for-combination-products-a-comprehensive-guide/]
- 63. Q14 Analytical Procedure Development March 2024 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q14-analytical-procedure-development]
- 64. ICH Q14 Analytical procedure development - Scientific guideline [https://www.ema.europa.eu/en/ich-q14-analytical-procedure-development-scientific-guideline]
- 65. New ICH Q2 (R2) and ICH Q14: a Step Forward Towards the ... [https://blog.pqegroup.com/ra-phv/new-ich-q2-r2-and-ich-q14]
- 66. A Practical Approach to Implementing ICH Q14 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12449753/]
- 67. What You Need to Know About ICH Q14 and ICH Q2(R2) ... [https://premier-research.com/perspectives/what-you-need-to-know-about-ich-q14-and-ich-q2r2-part-2/]
- 68. Use of Factorial Designs to Reduce Stability Studies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389050/]
- 69. What is the Difference between Bracketing and Matrixing? [https://www.gmp-compliance.org/gmp-news/what-is-the-difference-between-bracketing-and-matrixing]
- 70. Q1D Bracketing and Matrixing Designs for Stability Testing ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q1d-bracketing-and-matrixing-designs-stability-testing-new-drug-substances-and-products]
- 71. Save Money By Using Bracketing and Matrixing [https://www.fairfieldlabs.com/knowledge/industry-news/lower-the-cost-of-your-stability-program-by-using-bracketing-and-matrixing/]
- 72. Statistical Tools for Biologics Stability Testing [https://www.bioprocessintl.com/qa-qc/comprehensive-stability-assessment-of-biotechnological-products-degradation-mechanisms-statistical-tools-and-regulatory-compliance-part-1]
- 73. Data analytics on raw material properties to accelerate ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517319302583]
- 74. Predicting raw material impact on cell culture parameters in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12354791/]
- 75. 《ICH Q1稳定性试验指å—》è‰æ¡ˆä¸æ–‡ç‰ˆå…¨æ–‡ [http://m.anytesting.com/news/1955553.html]
- 76. Analytical Method Validation, Verification and Transfer Right [https://www.complianceonline.com/resources/getting-the-analytical-method-validation-verification-and-transfer-right.html]
- 77. Best practices for analytical method transfers [https://medfilesgroup.com/best-practices-for-analytical-method-transfers/]
- 78. Analytical Method Transfer: Best Practices and Guidelines [https://www.labmanager.com/analytical-method-transfer-best-practices-and-guidelines-34130]
- 79. Data Integrity While Building Stability Testing Program [https://www.q1productions.com/data-integrity-building-stability-testing-program/]
- 80. ICH Q12 Technical and regulatory considerations for ... [https://www.ema.europa.eu/en/ich-q12-technical-regulatory-considerations-pharmaceutical-product-lifecycle-management-scientific-guideline]
- 81. Pharmaceutical Product Lifecycle Management & ICH Q12 ... [https://www.advarra.com/blog/pharmaceutical-product-lifecycle-management/]
- 82. ICH Q12: Implementation Considerations for ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/ich-q12-implementation-considerations-fda-regulated-products]
- 83. Stability Lifecycle: An Application of ICH Q12 to Manage ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/613529-Stability-Lifecycle-An-Application-of-ICH-Q12-to-Manage-the-Pharmaceutical-Stability-Program/]
- 84. Use Statistics to Experiment, Surface New Data and Boost ... [https://www.forbes.com/sites/rkoselka/2025/11/20/how-to-experiment-with-more-real-data-to-boost-performance/]
- 85. Forced degradation studies: A critical lens into ... [https://www.clinicaltrialsarena.com/sponsored/forced-degradation-studies-a-critical-lens-into-pharmaceutical-stability/]
- 86. An Industry Perspective on the use of Forced Degradation ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354923005373]
- 87. Comparative Forced Degradation Study of Anticomplement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030638/]
- 88. Predictive Analytics for Biopharma Shelf-Life Extension [https://www.leukocare.com/blog/predictive-analytics-for-biopharmaceutical-shelflife-extension]
- 89. Stability modeling methodologies to enable earlier patient ... [https://www.sciencedirect.com/science/article/pii/S0022354924004258]
- 90. Kinetic Model Outperforms ICH Guidelines for Biologic ... [https://www.genengnews.com/topics/bioprocessing/kinetic-model-outperforms-ich-guidelines-for-biologic-stability/]
- 91. Predictive stability in biopharmaceuticals and vaccines [https://www.sciencedirect.com/science/article/pii/S0022354925003259]
- 92. Comparing Predictive Analytics Software | OMR Reviews [https://omr.com/en/reviews/category/predictive-analytics]
- 93. The 7 best predictive analytics software options in 2025 [https://zapier.com/blog/predictive-analytics-software/]
- 94. Q2(R2) Validation of Analytical Procedures March 2024 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q2r2-validation-analytical-procedures]
- 95. New ICH Q1 guideline: key changes and updates [https://www.linkedin.com/posts/aditya-dev-shukla-3a5a7b236_the-draft-ich-q1-guideline-released-on-april-activity-7321707872600354816-D7gR]
- 96. Deep Dive in to ICH Q1 2025 Draft: Stability Testing ... [https://www.linkedin.com/pulse/deep-dive-ich-q1-2025-draft-stability-testing-drug-products-shetty-ye9yf]
- 97. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 98. ICH publishes Training Materials on Q2(R2) and Q14 [https://www.gmp-compliance.org/gmp-news/ich-publishes-training-materials-on-q2r2-and-q14]
- 99. Manufacturing Capacity Expansion and Validation for ... [https://www.pda.org/pda-letter-portal/home/full-article/manufacturing-capacity-expansion-and-validation-for-autologous-cell-therapies]