Validating Animal Disease Models in Pharmacology: Strategies to Enhance Predictive Power and Translation
This article provides a comprehensive guide for researchers and drug development professionals on the critical process of validating animal disease models.
Validating Animal Disease Models in Pharmacology: Strategies to Enhance Predictive Power and Translation
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the critical process of validating animal disease models. It explores the foundational principles of why validation is essential for improving clinical translation, details established and emerging methodological frameworks for model assessment, addresses common challenges and optimization strategies, and compares validation approaches across different disease areas. By synthesizing current tools and evidence, this resource aims to equip scientists with the knowledge to select and justify animal models more effectively, thereby enhancing the efficiency and success of preclinical drug development.
The Critical Need for Model Validation: Foundations for Successful Translation
The Quantitative Landscape of Drug Development Attrition
The path of a new drug from discovery to market is a marathon of attrition, characterized by staggering failure rates and immense financial investment. Industry analyses consistently show that the average development timeline spans 10 to 15 years, with capitalized costs averaging $2.6 billion per approved drug [1]. The primary driver of this cost is the high failure rate during clinical development, where the likelihood of approval (LOA) for a drug candidate entering Phase I trials is a mere 7.9% [1]. This means more than nine out of every ten drugs that begin human testing will fail [1].
Recent dynamic analysis of clinical trial success rates (ClinSR) indicates that after a period of decline since the early 21st century, success rates have recently hit a plateau and are beginning to show signs of increase [2]. However, significant challenges persist. As of 2024, the success rate for Phase 1 drugs has plummeted to just 6.7%, compared to 10% a decade ago [3]. This contributes to a falling internal rate of return for R&D investment, which has dropped to 4.1%—well below the cost of capital [3].
Table 1: Drug Development Lifecycle by the Numbers
| Development Stage | Average Duration | Probability of Transition to Next Stage | Primary Reason for Failure |
|---|---|---|---|
| Discovery & Preclinical | 2-4 years | ~0.01% (to approval) | Toxicity, lack of effectiveness in models [1] |
| Phase I | 2.3 years | 52% - 70% | Unmanageable toxicity/safety [1] |
| Phase II | 3.6 years | 29% - 40% | Lack of clinical efficacy [1] |
| Phase III | 3.3 years | 58% - 65% | Insufficient efficacy, safety in larger populations [1] |
| FDA Review | 1.3 years | ~91% | Safety/efficacy concerns in submitted data [1] |
The failure rates vary substantially by therapeutic area. An analysis of phase-transition probabilities reveals that drugs for hematological disorders have the highest likelihood of approval from Phase I at 23.9%, while urology drugs have the lowest at just 3.6% [1]. The Phase II stage represents the single largest hurdle in drug development, where between 40% and 50% of all clinical failures occur due to a lack of clinical efficacy [1].
Table 2: Clinical Trial Success Rates by Therapeutic Area (2025 Analysis)
| Therapeutic Area | Phase I to Approval Success Rate | Notable Challenges |
|---|---|---|
| Oncology | Tracked slightly behind 2024 approvals in H1 2025 [4] | High biological complexity, tumor heterogeneity |
| Hematology | 23.9% (Highest) [1] | - |
| Urology | 3.6% (Lowest) [1] | - |
| Anti-COVID-19 Drugs | Extremely low ClinSR [2] | Compressed development timelines, novel mechanisms |
| Drug Repurposing | Unexpectedly lower than new drugs [2] | May involve off-target effects or novel biology |
Animal Models in Preclinical Validation: Benefits and Limitations
Validation Criteria for Animal Models
The value of an animal model in predicting human outcomes depends on how well it meets three established validation criteria first proposed by Willner in 1984 and now widely accepted across biomedical research [5].
Predictive Validity: This is considered the most crucial criterion, especially in preclinical drug discovery [5]. It measures how well results from the model correlate with human therapeutic outcomes. An example is the 6-OHDA rodent model for Parkinson's disease, which has been valuable for predicting treatment response [5].
Face Validity: This assesses how closely the model replicates the phenotypic manifestations of the human disease. The MPTP non-human primate model for Parkinson's Disease, for instance, effectively reproduces many of the motor symptoms seen in humans [5].
Construct Validity: This examines how well the method used to induce the disease in animals reflects the currently understood etiology and biological mechanisms of the human disease. Transgenic mouse models for Spinal Muscular Atrophy, which incorporate human SMN genes, exemplify strong construct validity [5].
Limitations in Translational Predictivity
Despite these validation frameworks, no single animal model perfectly replicates clinical conditions or shows validity in all three criteria [5]. A model might have strong predictive validity but completely lack face validity, or vice versa [5]. This inherent limitation contributes to what is known as the "translation crisis."
Significant physiological differences between animals and humans lead to problematic disparities in drug metabolism, target interactions, and disease pathophysiology [6]. These differences help explain why over 90% of clinical drug development efforts fail [7], with approximately 60% of trials failing due to lack of efficacy and 30% due to toxicity—issues that animal models frequently fail to predict [6].
The field of neurodegenerative disease research has particularly struggled with translatability, whereas areas like oncology have seen improvements through the use of more sophisticated models like patient-derived xenografts (PDX) and humanized models [5] [4].
Emerging Solutions: Advanced Models and Technologies
Integrated Preclinical Model Systems
No single model can fully recapitulate human disease, making a multifactorial approach using complementary models essential for improving translational accuracy [5] [4]. The most effective preclinical screening employs a sequential, integrated strategy that leverages the unique advantages of each model system.
Table 3: Comparison of Preclinical Screening Models in Oncology Research
| Model Type | Key Applications | Advantages | Limitations |
|---|---|---|---|
| 2D Cell Lines [4] | - Initial high-throughput screening- Drug efficacy testing- Combination studies | - Reproducible & standardized- Low-cost & versatile- Large established collections | - Limited tumor heterogeneity- Does not reflect tumor microenvironment |
| Organoids [4] | - Investigate drug responses- Personalized medicine- Predictive biomarker identification | - Preserves patient tumor genetics- Better clinical predictivity than cell lines- More cost-effective than animal models | - More complex/time-consuming to create- Cannot fully represent complete tumor microenvironment |
| Patient-Derived Xenografts (PDX) [4] | - Biomarker discovery/validation- Clinical stratification- Drug combination strategies | - Preserves original tumor architecture- Most clinically relevant preclinical model- Mirrors patient tumor responses | - Expensive & resource-intensive- Low-throughput- Ethical considerations of animal use |
The Role of AI and Data-Driven Approaches
Artificial intelligence and machine learning are transforming drug development by enabling more predictive analysis of complex biological data. AI-driven platforms can identify drug characteristics, patient profiles, and sponsor factors to design trials that are more likely to succeed [3]. Pharmaceutical companies are increasingly leveraging these technologies to:
- Optimize clinical trial designs by identifying clear success/failure criteria and commercially meaningful comparator arms [3]
- Use real-world data to identify and match patients more efficiently to clinical trials [3]
- Build predictive models that assess product consistency and reduce quality control time [7]
- Create digital twins of patients to test new drug candidates before human trials [7]
The FDA has recognized the potential of these approaches, releasing guidance in 2025 on "Considerations for the Use of Artificial Intelligence to Support Regulatory Decision Making for Drug and Biological Products" [6].
Human-Relevant Model Systems
A tidal shift is underway toward more human-relevant models that can substantially reduce the cost and timeline of early-stage drug development [6]. These include:
Organs-on-Chips: Microfluidic devices lined with living human cells that mimic human organ functionality. For example, Liver Chip models have been found to outperform conventional models in predicting drug-induced liver injury [6].
Human Induced Pluripotent Stem Cells (iPSCs): These enable the study of disease mechanisms and drug responses in human cells with specific genetic backgrounds.
Quantitative Computational Models: In silico tools that predict drug metabolism, toxicities, and off-target effects before any physical testing [6].
Regulatory changes are supporting this shift. The FDA Modernization Act 2.0, signed into law in 2022, specifically states the intent to utilize alternatives to animal testing for Investigational New Drug applications [6]. In September 2024, the FDA's CDER accepted its first letter of intent for an organ-on-a-chip technology as a drug development tool [6].
Experimental Protocols for Model Validation
Integrated Biomarker Discovery Workflow
The early identification and validation of biomarkers is crucial to modern drug development. The following protocol outlines a holistic, multi-stage approach for biomarker hypothesis generation and validation:
Stage 1: Hypothesis Generation (PDX-Derived Cell Lines)
- Method: Utilize PDX-derived cell lines for large-scale screening across diverse genetic backgrounds [4].
- Application: Identify potential correlations between genetic mutations and drug responses through targeted screening [4].
- Output: Generate initial sensitivity or resistance biomarker hypotheses for further validation.
Stage 2: Hypothesis Refinement (Organoid Testing)
- Method: Employ patient-derived organoids to validate biomarker hypotheses in more complex 3D tumor models [4].
- Multiomics Analysis: Integrate genomics, transcriptomics, and proteomics data to identify robust biomarker signatures [4].
- Output: Refined biomarker hypotheses with better clinical relevance.
Stage 3: Preclinical Validation (PDX Models)
- Method: Implement PDX models representing diverse tumor types to validate biomarker hypotheses before clinical trials [4].
- Application: Leverage the preserved tumor architecture and microenvironment of PDX models to understand biomarker distribution within heterogeneous tumors [4].
- Output: Clinically translatable biomarker signatures ready for patient stratification in clinical trials.
Research Reagent Solutions for Preclinical Validation
Table 4: Essential Research Reagents for Preclinical Oncology Studies
| Reagent / Model System | Function in Research | Example Applications |
|---|---|---|
| PDX-Derived Cell Lines [4] | Initial high-throughput screening platform | - Drug efficacy testing- Correlation of mutation status with drug response |
| Patient-Derived Organoids [4] | 3D culture preserving tumor characteristics | - Immunotherapy evaluation- Predictive biomarker identification- Safety studies |
| PDX Model Collections [4] | Gold standard for in vivo preclinical studies | - Biomarker discovery/validation- Clinical stratification- Drug combination strategies |
| Organ-on-Chip Devices [6] | Microfluidic devices mimicking human organs | - Prediction of drug-induced liver injury- Disease modeling- Personalized medicine |
| Multiomics Analysis Tools [4] | Integrated genomic, transcriptomic, proteomic analysis | - Biomarker signature refinement- Mechanism of action studies |
The translation crisis in drug development, characterized by persistently high attrition rates, remains a formidable challenge for the pharmaceutical industry. While animal models provide a necessary foundation for preclinical validation, their limitations in predictive validity contribute significantly to clinical failure. The path forward requires a multipronged approach: adopting integrated model systems that leverage the strengths of both traditional and emerging technologies, implementing AI-driven analytical tools to enhance decision-making, and embracing human-relevant models that better recapitulate human disease biology. Through these strategies, researchers can systematically address the validation gaps in preclinical research, ultimately improving the predictability of drug development and accelerating the delivery of effective therapies to patients.
In pharmacology research, the development of new therapeutics relies heavily on preclinical animal models. The validity of these models is paramount, as it determines how well experimental results can predict human outcomes. For researchers and drug development professionals, a rigorous understanding of validity types is not just academic—it is crucial for designing robust studies, interpreting data accurately, and making costly go/no-go decisions in the drug development pipeline. This guide provides a comparative analysis of three core validity principles—face, construct, and predictive validity—within the context of validating animal disease models for pharmacological research.
Defining the Core Validity Types
Validity refers to how accurately a method measures what it claims to measure [8]. In the specific context of animal models, it assesses how well the model represents the human disease and its response to therapeutic intervention.
| Validity Type | Core Question | Level of Formality | Primary Assessment Method |
|---|---|---|---|
| Face Validity | Does the model appear to measure the intended phenomenon? [8] [9] | Informal, subjective, superficial [10] [11] | Superficial judgment by non-experts or researchers [9] [11] |
| Construct Validity | Does the model accurately measure the underlying theoretical construct? [8] [11] | Formal, theoretical, comprehensive [8] | Convergent and discriminant validity testing [10] [11] |
| Predictive Validity | Does performance on the model predict a concrete future outcome? [8] [11] | Formal, empirical, practical | Correlation with a future "gold standard" criterion [8] [9] |
Face Validity
Face validity is the least scientific measure of validity, as it is a subjective assessment of whether a test or model appears to be suitable for its aims on the surface [8] [9]. For example, an animal model of depression might be considered to have face validity if the animals exhibit behaviors such as lethargy or reduced appetite, which are surface-level symptoms of human depression [11]. While its simplicity makes it useful for initial assessments, it is considered weak evidence for a model's quality because it does not ensure that the model is actually measuring the underlying disease construct [8] [10].
Construct Validity
Construct validity evaluates whether a model truly represents the theoretical concept it is intended to measure [8]. A "construct" is an abstract concept that cannot be directly observed, such as depression, anxiety, or cancer progression [8]. Establishing construct validity requires demonstrating that the model behaves in a manner consistent with the scientific theory of the construct. This is often assessed through two subtypes:
- Convergent Validity: The model shows correlation with other tests or models that measure the same or similar construct [10] [11].
- Discriminant Validity: The model can be differentiated from tests or models that measure different constructs [10].
Predictive Validity
Predictive validity assesses how well the results from a model can forecast a concrete outcome in the future [8] [11]. In pharmacology, this is the gold standard for evaluating an animal model's utility: its ability to predict a drug's efficacy or toxicity in humans [11]. A model has high predictive validity if treatments that are effective in humans also show effectiveness in the animal model, and vice-versa. This is a key focus in the validation of models intended to de-risk clinical trials.
Comparative Analysis in Animal Model Validation
The following table summarizes how each validity type is applied and assessed in the specific context of developing and validating animal disease models for pharmacology.
| Aspect | Face Validity | Construct Validity | Predictive Validity |
|---|---|---|---|
| Role in Pharmacology | Initial, rapid screening of model phenotypes. | Ensuring the model recapitulates the human disease's underlying biology. | Determining the model's utility for forecasting human clinical outcomes. |
| Key Application | Selecting models that exhibit obvious, surface-level symptoms analogous to human disease (e.g., motor deficits in a Parkinson's model). | Demonstrating that the model shares key genetic, molecular, and pathway dysregulations with the human disease. | Using the model for lead compound optimization and toxicology studies to prioritize candidates for clinical trials. |
| Data Type | Qualitative, observational | Multimodal (genomic, proteomic, behavioral, physiological) | Quantitative, empirical (correlation with clinical trial results) |
| Experimental Evidence | - Behavioral tests (e.g., forced swim test for depression) [11]- Pathological inspection (e.g., tumor size) | - Genetic similarity (e.g., transgenic models) [8]- Biomarker profiling (e.g., inflammatory cytokines)- Response to known therapeutics | - Correlation between animal model efficacy and human clinical trial outcomes [11]- Retrospective analysis of successful and failed drugs |
| Limitations | - Does not guarantee accuracy.- Vulnerable to anthropomorphism.- Cannot stand alone as evidence. | - Complex and costly to establish.- Requires a deep, well-defined theoretical understanding of the disease. | - Can be context-dependent (e.g., a model may predict efficacy for one drug class but not another).- Ultimate validation requires years of clinical data. |
Experimental Protocols for Assessment
Protocol for Establishing Face Validity
This protocol outlines the steps for a systematic assessment of a new animal model's face validity for major depressive disorder.
- Objective: To determine if the model exhibits observable symptoms analogous to core human depression symptoms.
- Materials: Animal model cohort, control cohort, standard behavioral testing equipment (e.g., open field, sucrose preference apparatus, forced swim test tank).
- Procedure:
- Define Symptom Domains: Based on clinical criteria (e.g., DSM-5), define the key symptom domains to be modeled (e.g., anhedonia, psychomotor retardation, despair).
- Select Behavioral Assays: Map each domain to a standardized behavioral test (e.g., Sucrose Preference Test for anhedonia, Open Field Test for locomotor activity, Forced Swim Test for behavioral despair).
- Blinded Scoring: Conduct experiments with researchers blinded to the animal groups. Record quantitative and qualitative data.
- Expert/Stakeholder Review: Have pharmacologists and behavioral neuroscientists review the data and rate the apparent relevance of the model to human depression on a Likert scale [11].
- Output: A qualitative profile of the model's surface-level resemblance to the human condition.
Protocol for Establishing Construct Validity
This protocol describes a multimodal approach to assess whether a model accurately reflects the theoretical construct of a specific cancer type.
- Objective: To evaluate the model's alignment with the known human disease biology at multiple levels.
- Materials: Animal model tissues, equipment for omics analyses (RNA-seq, mass spectrometry), histological equipment, validated biomarkers.
- Procedure:
- Convergent Validity Testing:
- Genomics: Compare tumor transcriptome from the model to human tumor databases (e.g., The Cancer Genome Atlas) for pathway enrichment similarity [10].
- Proteomics: Identify key protein biomarkers known to be dysregulated in the human cancer and confirm their presence and activity in the model.
- Pharmacology: Test if the model responds to standard-of-care drugs in a manner consistent with human patient responses.
- Discriminant Validity Testing:
- Demonstrate that the model's molecular profile is distinct from other, related cancer types.
- Show that therapies ineffective in the human disease are also ineffective in the model.
- Convergent Validity Testing:
- Output: A network of evidence showing the model's convergence with the human construct and divergence from unrelated constructs.
Protocol for Establishing Predictive Validity
This protocol uses a retrospective analysis to quantify an animal model's ability to predict human clinical efficacy.
- Objective: To calculate the model's predictive power for drug efficacy.
- Materials: Historical data on a set of drug compounds that have been tested in both the animal model and in human clinical trials.
- Procedure:
- Compound Selection: Assemble a blinded set of compounds, including both known clinically effective drugs and those that failed due to lack of efficacy.
- Model Testing: Review or run the compounds through the animal model to generate efficacy data (e.g., tumor growth inhibition, reduction in pathological score).
- Correlation Analysis: Compare the animal model results with the human clinical outcomes. Calculate metrics such as:
- Sensitivity: Proportion of effective drugs in humans that were positive in the model.
- Specificity: Proportion of ineffective drugs in humans that were negative in the model.
- Overall Predictive Accuracy: Proportion of all compounds correctly classified by the model [11].
- Output: Quantitative measures (sensitivity, specificity, accuracy) of the model's forecasting reliability.
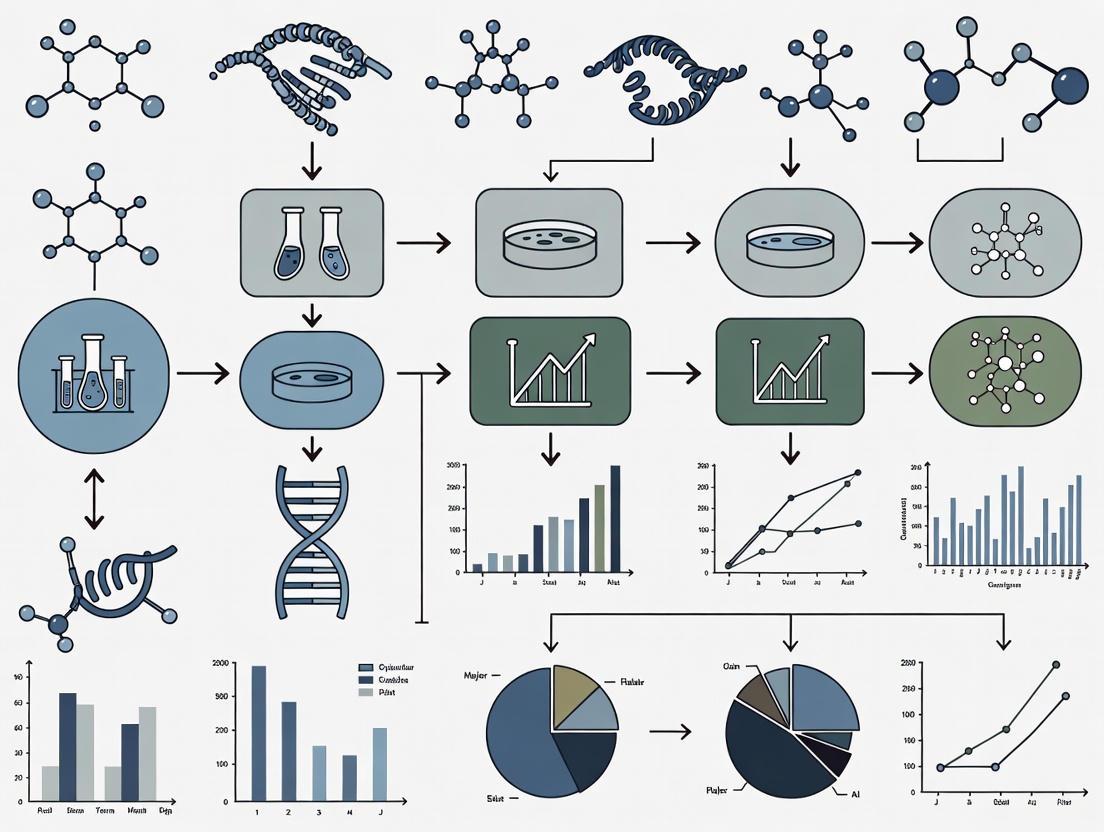
Visualizing the Validation Workflow
The following diagram illustrates the logical sequence and relationships between the different validity assessments in a typical model development pipeline.
Research Reagent Solutions for Validation Studies
The following table details key reagents and tools essential for conducting the experiments described in the validation protocols.
| Reagent/Tool | Function in Validation | Example Application |
|---|---|---|
| Behavioral Test Equipment | Quantifies face validity by measuring disease-relevant behaviors. | Assessing locomotor activity in neurodegenerative disease models; measuring anhedonia via sucrose preference test for depression models. |
| Omics Profiling Kits (e.g., RNA-seq, Proteomics) | Provides molecular data to establish construct validity. | Comparing gene expression profiles between animal tumors and human cancer databases to confirm pathway alignment. |
| Validated Biomarker Assays | Serves as a bridge for convergent validity between animal and human biology. | Measuring circulating inflammatory cytokines in a model of rheumatoid arthritis; assessing cardiac troponin in a cardiotoxicity model. |
| Reference Compounds (Clinical standards & failed drugs) | Critical for assessing both construct and predictive validity. | Establishing that a model responds to known effective drugs (positive control) and does not respond to known ineffective ones (negative control). |
| Microphysiological Systems (Organs-on-a-Chip) | Emerging human-relevant tools used as a comparative standard for animal model validation [12]. | Comparing drug toxicity or efficacy data from an animal model with data from a human liver-on-a-chip to assess translational relevance. |
Face, construct, and predictive validity form a hierarchical framework for validating animal models in pharmacology. While face validity offers an accessible starting point and construct validity ensures biological fidelity, predictive validity remains the ultimate benchmark for a model's utility in drug development. A model strong in all three areas provides the highest confidence for translating preclinical findings to clinical success. As the field evolves with new technologies like AI and human-based microphysiological systems [13] [12] [14], the principles of validity will continue to be the cornerstone for evaluating not only animal models but also these next-generation tools, ensuring rigorous and reliable pharmacology research.
In pharmaceutical research, the selection of a preclinical animal model is a critical determinant of a drug's eventual clinical success. High rates of drug development attrition, often due to insufficient efficacy or unexpected safety issues not predicted by animal studies, have prompted a reevaluation of traditional model validation approaches [15] [16]. While the standard three validity criteria (face, construct, and predictive validity) provide a foundational framework, they often fall short in ensuring translational relevance for complex human diseases. A more rigorous, multidisciplinary assessment that incorporates etiology (disease cause), pathogenesis (disease progression), and histology (tissue pathology) is emerging as essential for optimizing model selection and improving the predictive power of preclinical research [15] [17]. This guide compares animal models across these refined criteria, providing researchers with a structured framework for model selection in pharmacology research.
Comparative Analysis of Animal Disease Models
The following tables provide a quantitative and qualitative comparison of common animal models across key diseases, focusing on their fidelity to human disease characteristics.
Table 1: Comparison of Inflammatory and Metabolic Disease Models
| Disease & Model | Etiological Fidelity | Pathogenetic Fidelity | Histological Concordance | Key Pharmacological Utility | Translatability Score |
|---|---|---|---|---|---|
| Adoptive T-cell Transfer Colitis (Mouse) | Induced (Transfer of T-cells) | Recapitulates immune dysregulation & inflammation | Transmural inflammation, epithelial hyperplasia | Target validation for immune-modulators [15] | High for specific immune mechanisms |
| Chemically-Induced Colitis (e.g., DSS in Mice) | Induced (Chemical damage) | Epithelial barrier disruption → inflammation | Mucosal ulceration, leukocyte infiltration | Screening anti-inflammatory compounds [15] | Moderate (acute injury vs. chronic disease) |
| Zebrafish Diabetes Model | Induced (Chemical/Genetic) | Beta-cell dysfunction, hyperglycemia | Islet morphology changes, not full human pathology | High-throughput screening of metabolic drugs [17] | Moderate for pathways, limited for systemic complications |
| Diet-Induced Obesity (Rodents) | Induced (High-fat diet) | Mirrors human metabolic syndrome: insulin resistance, dyslipidemia | Hepatic steatosis, adipose tissue inflammation | Evaluating weight-loss drugs and insulin sensitizers [17] | High for metabolic syndrome phenotype |
Table 2: Comparison of Infectious Disease and Oncology Models
| Disease & Model | Etiological Fidelity | Pathogenetic Fidelity | Histological Concordance | Key Pharmacological Utility | Translatability Score |
|---|---|---|---|---|---|
| Syrian Hamster COVID-19 | High (SARS-CoV-2 infection) | Viral replication in respiratory tract → lung inflammation [18] | Mirrors human-like lung pathology and viral load | Vaccine and antiviral efficacy testing [18] | High for respiratory disease progression |
| Humanized Mouse (Oncology) | Variable (Patient-derived xenografts/PDX) | Human tumor in mouse microenvironment | Retains original tumor histoarchitecture | Personalized therapy screening, immunotherapy development [18] [19] | Very High for human-specific drug target interaction |
| Genetically Engineered Mouse (GEMM) for Cancer | High (Specific genetic alterations) | Spontaneous tumor development in immune-competent host | Tumor histology and stroma interaction similar to human | Studying oncogenesis and targeted therapies [19] [17] | High for mechanism-driven drug discovery |
Experimental Protocols for Enhanced Model Validation
Protocol 1: Comprehensive Validation of an Inflammatory Bowel Disease (IBD) Model
This protocol utilizes the Animal Model Quality Assessment (AMQA) tool to ensure translational relevance [15].
- Model Induction and Justification: Justify the selected model (e.g., adoptive T-cell transfer vs. DSS-induced) based on the specific research question (e.g., testing an immunomodulator vs. a barrier-enhancing agent) [15].
- Etiological Assessment: Document how the model's induction method (e.g., specific immune cell population) aligns with known or hypothesized human disease triggers.
- Pathogenetic Profiling:
- Temporal Analysis: Conduct weekly measures of disease activity (e.g., weight, stool consistency, occult blood).
- Cytokine & Immune Phenotyping: Use flow cytometry and multiplex ELISA to profile inflammatory mediators (e.g., TNF-α, IL-6, IL-12/23, IFN-γ) in colonic tissue and serum, comparing to human IBD profiles.
- Microbiome Analysis (Optional): Sequence 16S rRNA from fecal samples to assess dysbiosis, a key pathogenic factor in human IBD.
- Histopathological Evaluation:
- Collect and fix colon segments in 10% neutral buffered formalin.
- Process, embed in paraffin, section at 5µm, and stain with Hematoxylin and Eosin (H&E).
- Score blinded sections using a validated system (e.g., scoring for inflammation severity, crypt loss, architectural distortion, and immune cell infiltration).
- Pharmacological Challenge: Administer a reference therapeutic (e.g., anti-TNF-α antibody) to confirm the model's responsiveness and predictive value for drug classes under investigation.
Protocol 2: Validation of a "Humanized" Mouse Model for Immuno-Oncology
This protocol is critical for evaluating models used to test human-specific immunotherapies [18] [19].
- Model Generation and Characterization:
- Employ NSG or similar immunodeficient mice.
- Engraft with human hematopoietic stem cells (CD34+) or a patient-derived xenograft (PDX).
- Confirm engraftment level (>25% human CD45+ cells in peripheral blood) via flow cytometry at 12-16 weeks post-transplant.
- Etiological and Histological Concordance:
- For PDX models, perform genomic and transcriptomic analysis to verify retention of the original human tumor's key drivers.
- Upon study termination, compare tumor histology from the mouse to the original patient biopsy using H&E and immunohistochemistry for relevant markers (e.g., PD-L1, tumor-specific antigens).
- Functional Pathogenetic Validation:
- Drug Exposure: Treat mice with a human-specific immunotherapy (e.g., anti-PD-1 antibody).
- Endpoint Analysis: Measure tumor volume regression. Harvest tumors for flow cytometric analysis of tumor-infiltrating human lymphocytes (CD8+/CD4+ T-cell ratios, activation markers) to confirm the drug's mechanism of action on the human immune system within the model.
Visualization of Model Validation Workflows
The following diagrams outline the logical workflows for implementing the enhanced validation criteria discussed in this guide.
Diagram 1: A workflow for selecting and validating an animal model for a specific Context of Use (COU), based on the AMQA framework. It emphasizes the sequential evaluation of etiology, pathogenesis, and histology before making a final model selection [15].
Diagram 2: The role of a thoroughly validated animal model within a modern, integrated drug development workflow that also leverages New Approach Methodologies (NAMs) like in silico and in vitro tools [18] [16] [20].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Advanced Model Validation
| Reagent/Material | Function in Validation | Example Application |
|---|---|---|
| Species-Specific Cytokine ELISA/Multiplex Kits | Quantifies key inflammatory mediators to profile pathogenesis and drug response. | Measuring TNF-α, IL-6, IL-1β in mouse colitis models to compare to human cytokine profiles [15]. |
| Flow Cytometry Antibody Panels | Characterizes immune cell populations in tissues (infiltration, activation state). | Profiling human T-cell subsets (CD4, CD8, Treg) in "humanized" mouse models for immuno-oncology [18] [19]. |
| CRISPR-Cas9 Gene Editing Systems | Creates genetically engineered models (GEMs) with precise etiological mutations. | Generating knockout mice with loss-of-function mutations to mimic human genetic diseases [18] [19]. |
| Patient-Derived Xenograft (PDX) | Provides a histologically accurate and genetically stable tumor for oncology studies. | Transplanting human tumor tissue into immunodeficient mice to test personalized therapy regimens [19]. |
| Organ-on-a-Chip Microfluidic Devices | Serves as a human-relevant complementary tool to de-risk in vivo studies. | Using a human lung-on-a-chip to study SARS-CoV-2 infection pathophysiology before animal testing [18] [16]. |
| IHC/IF Antibodies for Tissue Markers | Enables histological evaluation and scoring of disease-specific pathology. | Staining for collagen deposition in fibrosis models or specific neuronal proteins in neurodegenerative models [15] [17]. |
| 2-Oxoglutaric Acid | 2-Oxoglutaric Acid, CAS:34410-46-3, MF:C5H6O5, MW:146.10 g/mol | Chemical Reagent |
| Afzelin | Afzelin (Kaempferol 3-Rhamnoside) |
The evolving landscape of drug development, marked by both scientific advancement and regulatory shifts toward human-relevant methods [21] [16] [20], demands a more sophisticated approach to animal model validation. Moving beyond the three classic validity criteria to a deeper, evidence-based assessment of etiology, pathogenesis, and histology provides a powerful framework for researchers. This rigorous multi-parameter comparison, supported by the structured tools and protocols outlined in this guide, enables more informed model selection. Ultimately, this enhances the translational predictive value of preclinical pharmacology research, de-risks drug development pipelines, and accelerates the delivery of effective new therapies to patients.
Ethical Imperatives and the 3Rs (Replacement, Reduction, Refinement) in Model Selection
The validation of animal disease models represents a cornerstone of pharmacology research, ensuring the translational relevance of therapeutic discoveries. This process is intrinsically guided by the ethical framework of the 3Rs—Replacement, Reduction, and Refinement—first articulated by William Russell and Rex Burch in 1959 [22]. Today, regulatory and scientific evolution is accelerating the integration of these principles into mainstream research practice. The recent FDA Modernization Act 2.0, signed into US law in 2022, has abolished the mandatory requirement for animal testing before advancing to human clinical trials, permitting the use of scientifically valid non-animal methods [23] [12] [24]. This paradigm shift, coupled with initiatives from regulatory bodies like the FDA and EMA to actively phase out animal testing for specific products like monoclonal antibodies, underscores the growing imperative for a more ethical and human-relevant approach to disease modeling [20] [21]. This article objectively compares traditional animal models with emerging 3R-aligned alternatives, evaluating their performance, validation, and application within modern pharmacological research.
The 3Rs Framework: From Principle to Practice
The 3Rs provide a systematic ethical framework for governing the use of animals in science [25] [22].
- Replacement: The use of non-sentient material to replace conscious living higher animals. This can be full replacement (e.g., computer models, human organoids) or partial replacement (e.g., using invertebrates like Drosophila or zebrafish embryos, which are not protected by animal welfare legislation in its entirety) [25] [24].
- Reduction: Employing methods to obtain comparable levels of information from fewer animals, primarily through sophisticated experimental design and statistical analysis [25] [22].
- Refinement: Modifying husbandry or experimental procedures to minimize pain and distress and improve animal welfare [25].
Regulatory agencies worldwide are now working to incorporate this framework. The European Medicines Agency (EMA) has published guidelines on the regulatory acceptance of 3R testing approaches [26], while the FDA has detailed specific contexts—from safety pharmacology to chronic toxicity studies—where streamlined nonclinical programs and reduced animal use are acceptable [20].
Comparative Analysis of Model Systems: Performance and Validation
The selection of a model requires a careful balance of ethical considerations, biological relevance, and predictive validity. The following sections and tables provide a comparative analysis of various models.
Traditional Animal Models: Utility and Limitations in Pharmacology
Animal models, from rodents to non-human primates, have been invaluable for understanding whole-body physiology, complex immune responses, and long-term safety profiles [27] [12]. Their use is rooted in the phylogenetic and physiological resemblance to humans, especially in mammals [27]. However, their predictive validity for human outcomes is not guaranteed, as illustrated by the stark contrast between high success rates in animal models and the >99% clinical trial failure rate in Alzheimer's disease [28].
Table 1: Advantages and Limitations of Selected Traditional Animal Models
| Animal Model | Significances and Common Uses | Key Limitations and Ethical Considerations |
|---|---|---|
| Mice/Rats | Easy breeding, low cost, well-established genome, many transgenic strains; used in cancer, cardiovascular, and genetic studies [27]. | High inbreeding limits genetic diversity; not ideal for all human disease responses (e.g., inflammation); findings not always translatable [27]. |
| Non-Human Primates | Close genetic and physiological similarity to humans; critical for AIDS, Parkinson's, and vaccine research [27]. | Highest ethical constraints; expensive; long maturity period; specialized housing required [27]. |
| Zebrafish | Vertebrate with high genetic similarity; transparent embryos for developmental biology and toxicology; high regenerative capacity [27] [24]. | Less resemblance to human anatomy and physiology than mammals; not ideal for all disease studies [27]. |
| Guinea Pigs | Outbred model suitable for asthma, tuberculosis, and vaccine research [27]. | High phenotypic variation; limited use for some pathogens (e.g., Ebola) [27]. |
New Approach Methodologies (NAMs) as Replacements and Refinements
NAMs encompass a suite of non-animal technologies designed to provide more human-relevant safety and efficacy data [20] [23]. Their adoption is a key component of the FDA's plan to reduce animal testing [21].
Table 2: Performance and Validation of New Approach Methodologies (NAMs)
| Methodology | Description and Experimental Protocol | Performance Data and Regulatory Context |
|---|---|---|
| In Silico Modelling | Uses computational tools, AI, and machine learning to simulate drug pharmacokinetics (e.g., PBPK models) and predict toxicity [12] [24]. | A computer model for cardiac arrhythmia risk prediction demonstrated ~90% accuracy, compared to ~75% from traditional animal-based hERG testing [24]. |
| Organ-on-a-Chip (OoC) | Microfluidic devices with human cells that mimic the structure and function of human organs (e.g., lung, gut, liver) [12] [24]. | Roche has developed a commercial colon-on-a-chip using a patient's own cells to replicate the gastrointestinal tract for personalized therapy testing [24]. |
| Organoids | 3D cell cultures from human stem cells that model complex tissue interactions and disease mechanisms [12]. | Used for high-throughput compound screening and studying disease pathways in a human-relevant context [12]. |
| In Vitro Assays | Use of cultured human cells combined with high-content imaging and 'omics' technologies to study mechanisms of action and toxicology [12]. | In vitro liver models are accepted by the FDA to predict hepatotoxicity and drug-induced liver injury by assessing biomarker changes [20]. |
Experimental Validation and Workflow in 3R-Compliant Research
Adopting 3R-aligned models requires a rigorous and structured approach to validation. The following workflow diagrams and reagent toolkit outline the key components of this process.
Decision Workflow for 3R-Compliant Model Selection
This diagram illustrates the logical process a researcher should follow to select the most appropriate and ethical model for a pharmacological study, in line with the 3Rs hierarchy.
Integrated Strategy for Model Validation
This diagram outlines an integrated testing strategy (IATA) that combines multiple NAMs to build a robust, non-animal safety assessment, as encouraged by organizations like the OECD [23].
Research Reagent Solutions for 3R-Aligned Pharmacology
This table details key reagents and platforms essential for implementing advanced, non-animal research methodologies.
Table 3: Essential Research Reagents and Platforms for 3R-Compliant Research
| Reagent/Platform | Function in Experimental Protocol |
|---|---|
| Recombinant Antibodies | Non-animal-derived antibodies (e.g., from the PETA/ARDF Recombinant Antibody Challenge) that replace animal-derived monoclonal or polyclonal antibodies in research and testing [25]. |
| Stem Cells (Human) | Source material for generating organoids and populating organ-on-a-chip systems to create human-relevant disease and toxicity models [12] [24]. |
| Microfluidic Chips | The physical platform for organ-on-a-chip devices, enabling precise control of cell microenvironments and fluid flow to mimic human organ physiology [12] [24]. |
| QSAR Models & AOPs | Quantitative Structure-Activity Relationship (QSAR) models and Adverse Outcome Pathways (AOPs) are computational tools used as part of Integrated Approaches to Testing and Assessment (IATA) to predict chemical toxicity without animal tests [23]. |
| GastroPlus/Simcyp | Established software platforms that utilise PBPK modelling and simulation to predict oral bioavailability and inform formulation strategies, replacing certain animal pharmacokinetic studies [24]. |
The validation of animal disease models is undergoing a profound transformation, driven by the ethical imperatives of the 3Rs and supported by rapid technological advancement. Regulatory changes, such as the FDA Modernization Act 2.0, have provided the necessary impetus for the scientific community to embrace NAMs not merely as alternatives, but as superior, more human-predictive tools [21] [23] [12]. While traditional animal models continue to provide value in understanding whole-body systems, their role is becoming more targeted and judicious. The future of pharmacology research lies in integrated testing strategies that synergistically combine in silico, in vitro, and human-centric data [12]. This paradigm shift promises to enhance the predictive power of preclinical research, accelerate the development of safer therapeutics, and firmly align scientific progress with the highest ethical standards.
Frameworks in Action: Methodologies for Systematic Model Assessment
In pharmaceutical drug discovery, animal studies are a regulatory expectation for preclinical compound evaluation before progression into human clinical trials [29] [15]. However, the field faces a significant challenge: high rates of drug development attrition have prompted serious concerns regarding the predictive translatability of animal models to the clinic [29] [30] [15]. For instance, in acute ischaemic stroke research, only 3 out of 494 interventions showing positive effects in animal models demonstrated convincing effects in patients [30]. This translation gap represents not just scientific but also ethical and economic challenges, driving the need for systematic approaches to evaluate animal model relevance.
The Animal Model Quality Assessment (AMQA) emerges as a direct response to these challenges. Developed at GlaxoSmithKline (GSK), this structured tool provides a consistent framework for evaluating animal models to optimize their selection and application throughout the drug development continuum [15]. Unlike informal assessment approaches, AMQA offers a transparent, multidisciplinary methodology to reflect key model features and establish a clear connection between preclinical models and clinical intent, thereby rationalizing a model's usefulness for specific contexts of use [15].
Understanding AMQA: Development and Core Components
The Genesis of a Quality Assessment Tool
The AMQA tool originated from an internal after-action review at GSK that analyzed both successful and unsuccessful clinical assets to identify key points of misalignment between preclinical animal pharmacology studies and their corresponding clinical trials [15]. This investigation revealed several critical features that contribute to translational weaknesses, including fundamental understanding of the human disease, biological context of affected organ systems, historical experiences with pharmacologic responses, how well the model reflects human disease etiology and pathogenesis, and model replicability [15].
The tool evolved through three rounds of pilots and iterative design with input from various disciplines including in vivo scientists, pathologists, comparative medicine experts, and non-animal modelers [15]. This collaborative development ensured applicability across a broad portfolio of models, appropriateness for both well-characterized and novel models, and practical utility for researchers. The resulting framework addresses a recognized need in pharmacological research for more standardized approaches to model evaluation [15].
Key Assessment Domains and Workflow
The AMQA employs a question-based template that guides investigators through critical considerations for evaluating and justifying an animal model for a specific human disease interest [15]. This approach makes implicit assessments explicit, focusing on the relevant questions being asked in drug development. While the full questionnaire is detailed in the original publication, key assessment domains include:
- Human Disease Understanding: Evaluating the fundamental knowledge of human disease pathology and mechanisms.
- Biological/Physiological Context: Assessing the relevance of organ systems and physiological processes affected.
- Pharmacological Responsiveness: Reviewing historical experiences with drug responses in the model compared to humans.
- Etiological and Pathogenetic Alignment: Examining how well the model disease reflects human disease causes and progression.
- Replicability and Consistency: Determining the model's reliability across experiments and research settings.
The typical workflow for applying AMQA in pharmacological research involves multiple stages, as illustrated below:
The assessment culminates in a practical output that clearly identifies strengths and weaknesses of a model, providing insights that can guide model selection, highlight knowledge gaps requiring additional investigation, or suggest when alternative platforms might be more appropriate [15].
AMQA in Practice: Experimental Application and Protocol
Implementation Methodology
Implementing AMQA requires a systematic, collaborative approach with clearly defined protocols. The experimental application of AMQA involves several key phases:
Phase 1: Team Assembly and Scope Definition
- Convene a multidisciplinary team including in vivo scientists, laboratory animal veterinarians, pathologists, and clinical pharmacologists [15]
- Clearly define the context of use for the animal model within the drug development pipeline (e.g., target validation, efficacy testing, safety assessment) [31]
- Establish the specific human clinical condition of interest and key clinical endpoints to be modeled
Phase 2: Evidence Collection and Assessment
- Gather existing literature and historical data on the animal model's performance characteristics
- Collect internal experimental data from previous studies using the model
- Complete the AMQA question-based template through structured discussion and evidence review
Phase 3: Scoring and Interpretation
- Apply the high-level scoring system to evaluate predictive translatability
- Identify critical weaknesses that might limit clinical translation
- Develop mitigation strategies for identified weaknesses through model refinement or complementary approaches
A specific example documented in the literature demonstrates the application of AMQA to the adoptive T-cell transfer model of colitis as a mouse model to mimic inflammatory bowel disease in humans [15]. This published example provides researchers with a template for implementing the assessment in their own pharmacological research contexts.
Research Reagent Solutions for AMQA Implementation
The following table details essential materials and resources required for effective AMQA implementation in pharmacological research:
| Research Reagent Solution | Function in AMQA Implementation |
|---|---|
| Multidisciplinary Expert Team | Provides diverse perspectives on model relevance across scientific disciplines [15] |
| Historical Model Performance Data | Offers evidence-based insights into model consistency and pharmacological responsiveness [15] |
| Clinical Disease Characterization | Serves as reference standard for evaluating model alignment with human condition [15] |
| Pharmacological Response Database | Enables comparison of drug effects between model and human patients [15] |
| Standardized Assessment Template | Guides consistent evaluation process across different models and research teams [15] |
| Pathological Validation Tools | Provides objective measures of disease recapitulation at tissue and cellular levels [15] |
Comparative Analysis: AMQA Versus Alternative Assessment Approaches
Established Model Assessment Frameworks
While AMQA represents a comprehensive approach developed within the pharmaceutical industry, other frameworks exist for evaluating animal models in pharmacological research. The Framework to Identify Models of Disease (FIMD) includes factors to help interpret model similarity and evidence uncertainty [15]. Other approaches have suggested disease-specific functional deficit assessments [15] or incorporated various scoring systems to quantify model relevance [15].
What distinguishes AMQA is its specific development within a global pharmaceutical context and its direct focus on optimizing decision-making throughout the drug development pipeline. Unlike frameworks primarily designed for basic research, AMQA explicitly connects model assessment to clinical translation success, addressing the specific evidence needs for advancing compounds through preclinical development toward human trials [15].
Emerging Non-Animal Technologies (NAMs)
The landscape of preclinical assessment is rapidly evolving with the emergence of New Approach Methodologies (NAMs) that offer complementary or alternative approaches to traditional animal models. The following table compares AMQA with leading alternative assessment frameworks:
| Assessment Approach | Primary Focus | Key Strengths | Limitations in Pharmacology |
|---|---|---|---|
| Animal Model Quality Assessment (AMQA) | Evaluation of in vivo animal models for translational relevance [15] | • Industry-developed for drug development context• Structured, question-based approach• Multidisciplinary perspective• Direct line of sight to clinical intent | • Limited application to non-mammalian models• Requires significant expertise across disciplines• Less familiar in academic settings |
| Framework to Identify Models of Disease (FIMD) | Interpretation of model similarity and evidence uncertainty [15] | • Systematic evaluation of disease recapitulation• Considers multiple dimensions of model relevance | • Less specific to pharmacological context• Limited guidance on predictive translatability for drug response |
| New Approach Methodologies (NAMs) | Replacement, reduction, and refinement of animal use [31] [32] | • Human-relevant biology (organoids, organs-on-chips)• High-throughput capability• Reduced ethical concerns• Potential for human genetic diversity integration | • Limited regulatory acceptance for standalone use• Challenges with systemic disease modeling• Variable reproducibility between platforms• Often requires defined context of use [31] |
| Functional Deficit Assessment | Disease-specific functional outcomes [15] | • Focus on clinically relevant endpoints• Quantitative outcome measures | • Narrow scope limited to functional measures• May overlook pathological mechanisms |
The relationship between these assessment approaches and their applications across the drug development pipeline reveals distinct but complementary roles:
Quantitative Assessment: Performance Data and Validation Metrics
Impact on Decision-Making and Translation
While specific numerical outcomes of AMQA implementation are proprietary, the tool's value is demonstrated through its systematic approach to addressing key sources of translational failure in pharmacology. Quantitative analysis of historical translational challenges highlights the critical importance of rigorous model assessment:
| Translational Challenge Domain | Impact on Drug Development Success | AMQA Mitigation Approach |
|---|---|---|
| Biological Relevance | Species-specific differences in drug target homology limit predictive value for 100+ human-specific targets [31] | Structured assessment of target conservation and pharmacological responsiveness [15] |
| Disease Recapitulation | Fewer than 50% of animal studies sufficiently predict human outcomes in systematic reviews [30] | Evaluation of etiological and pathogenetic alignment with human disease [15] |
| Study Design Limitations | Underpowered animal studies (often with small group sizes) reduce reliability and reproducibility [30] | Consideration of model replicability and consistency in assessment [15] |
| Environmental Standardization | Overly strict standardization increases false-positive rates by 15-20% in some models [30] | Evaluation of model performance across varied experimental conditions [15] |
Integration with Complementary Assessment Methodologies
The most forward-looking application of AMQA involves its integration with emerging computational and AI-driven approaches. The AnimalGAN initiative developed by the FDA represents a complementary approach that uses generative AI to simulate animal study results and reduce reliance on animal testing [33]. In a pilot study, synthetic data from AnimalGAN for toxicogenomics, hematology, and clinical chemistry showed potential for use in toxicity assessments, mechanistic studies, and biomarker development similar to actual experimental data [33].
Furthermore, artificial intelligence and machine learning (AI/ML) approaches are increasingly being applied to enhance the assessment of model relevance and translation. AI/ML can help distinguish signal from noise in biological data, reduce data dimensionality, and automate the comparison of alternative mechanistic models [31]. The integration of these computational approaches with structured assessment tools like AMQA represents the future of model evaluation in pharmacology.
Future Directions: AMQA in the Evolving Preclinical Landscape
Integration with NAMs and Computational Approaches
The future of animal model assessment lies in integrated approaches that combine tools like AMQA with New Approach Methodologies and computational modeling. As recognized by regulatory agencies including the FDA, opportunities now exist to waive certain animal testing requirements, particularly for therapeutics targeting human-specific pathways, using NAMs that provide human-relevant data [31]. In this evolving landscape, AMQA can play a valuable role in determining when traditional animal models remain essential and when alternative approaches may provide superior predictive value.
Clinical pharmacologists are increasingly positioned to lead the integration of mechanistic models with AMQA assessments. Physiologically based pharmacokinetic (PBPK) models and quantitative systems pharmacology (QSP) approaches can translate in vitro NAM efficacy or toxicity data into predictions of clinical exposures, thereby informing first-in-human dose selection strategies [31]. These integrated approaches enable more robust decision-making in early drug development by combining human-relevant data from NAMs with structured assessment of traditional models through frameworks like AMQA.
Expanding Applications Beyond Model Selection
While initially developed to guide animal model selection, AMQA's potential applications continue to expand. The tool provides quality context for evidence derived from models to inform decision-makers at critical development milestones [15]. Additionally, AMQA can support harm-benefit analysis by institutional ethical review committees by providing a more rigorous assessment of potential scientific benefit than traditional justifications based primarily on citations of previous work [15].
As pharmacological research evolves toward more complex disease modeling and personalized medicine approaches, structured assessment tools like AMQA will become increasingly valuable for evaluating model fit-for-purpose across diverse therapeutic contexts. The transparency provided by such assessments helps research teams acknowledge and mitigate model limitations while maximizing the translational value of preclinical evidence in support of innovative medicines for patients.
In pharmacological research, selecting a disease model with high predictive validity for human responses is a critical, high-stakes decision. For decades, animal models have been the cornerstone of preclinical testing, yet they often fall short in predicting human safety and efficacy, contributing to the high failure rates of drugs in clinical trials [34]. The recent regulatory shift, exemplified by the U.S. Food and Drug Administration's (FDA) 2025 roadmap to phase out animal testing requirements for monoclonal antibodies, underscores the urgent need for robust, human-relevant models [12] [16]. This transition is fueled by the recognition that traditional animal-based data have been poor predictors of drug success, particularly for complex conditions like cancer, Alzheimer's, and inflammatory diseases [16].
In this evolving landscape, the Framework to Identify Models of Disease (FIMD) emerges as a vital standardized scoring system. FIMD is designed to provide researchers with a quantitative, transparent methodology to evaluate and compare the utility of various disease models—from traditional animal systems to advanced New Approach Methodologies (NAMs) like organ-on-chip, in silico modeling, and complex in vitro models [31]. By establishing a common metric for model assessment, FIMD aims to enhance the reliability of preclinical data, streamline regulatory submissions, and accelerate the development of safer, more effective therapies.
FIMD Core Architecture: Components and Scoring Methodology
The FIMD scoring system is built on a multi-axis architecture that quantifies the strengths and limitations of each model across dimensions critical for pharmacological research. The framework generates a composite FIMD Score on a 100-point scale, enabling direct, objective comparison between disparate models.
Table 1: The Core Components of the FIMD Scoring System
| Component | Max Score | Description | Key Metrics |
|---|---|---|---|
| Physiological Relevance | 30 | Assesses how well the model recapitulates key aspects of human disease biology and pathophysiology. | Target homology, disease phenotype recapitulation, multicellular interactions. |
| Predictive Validity | 25 | Measures the model's historical accuracy in predicting clinical efficacy and safety outcomes in humans. | Concordance with clinical trial results, safety liability identification. |
| Technical Robustness | 20 | Evaluates the model's reliability, reproducibility, and scalability. | Inter-laboratory variability, assay standardization, throughput. |
| Context-of-Use (CoU) Alignment | 15 | Scores the model's suitability for a specific research application (e.g., target validation, toxicity screening). | Defined CoU, regulatory acceptance for the intended purpose. |
| Operational Practicality | 10 | Assesses feasibility of implementation, including cost, timeline, and ethical considerations. | Cost-effectiveness, timeline, ethical compliance (3Rs). |
The FIMD Calculation Formula
The composite FIMD Score is a weighted sum of its components:
FIMD Score = (Physiological Relevance × 0.30) + (Predictive Validity × 0.25) + (Technical Robustness × 0.20) + (CoU Alignment × 0.15) + (Operational Practicality × 0.10)
Scores are categorized as: Excellent (85-100), Good (70-84), Moderate (55-69), and Poor (<55). This standardized score allows researchers to quickly gauge a model's overall utility and suitability for their specific project.
Quantitative Comparison of Disease Models Using FIMD
Applying the FIMD framework to common models used in drug development reveals their relative strengths and weaknesses. The following comparison highlights why a one-size-fits-all approach is often inadequate and how FIMD guides model selection based on the specific research context.
Table 2: FIMD Quantitative Comparison of Different Disease Models
| Model Type | Example Systems | FIMD Score | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Non-Human Primate (NHP) | Cynomolgus monkey | 78 (Good) | Whole-body physiology; complex immune system [31]. | High cost, ethical concerns, poor predictor for some immunotherapies (e.g., TGN1412) [31]. |
| Rodent Models | Transgenic mice, rat disease models | 65 (Moderate) | Genetic manipulability, established historical data, low cost. | Significant species-specific differences in pathophysiology and drug targets [31]. |
| Organ-on-a-Chip | Lung-on-a-chip, gut-on-a-chip | 82 (Good) | Human cells; replicates tissue-level function and mechanical forces; high human relevance [12]. | Limited multi-organ integration; model complexity can lead to variability [31]. |
| In Silico / QSP Models | PBPK, Quantitative Systems Pharmacology | 85 (Excellent) | High throughput; can simulate human populations and virtual trials; integrates diverse data sets [35]. | Dependent on quality of input data; can be a "black box"; requires computational expertise [35]. |
| Human Organoids | iPSC-derived brain, liver organoids | 80 (Good) | Human genetics; 3D structure captures some tissue complexity; patient-specific [12]. | Immaturity of cells; lack of vascularization and full immune component; reproducibility challenges [35]. |
The data shows that advanced NAMs like in silico and organ-on-a-chip models are achieving FIMD scores comparable to, and in some cases exceeding, traditional animal models. This quantitative justification underpins the regulatory and scientific shift towards these human-relevant approaches. However, the scores also clearly indicate that no single model is superior in all categories, emphasizing the need for a fit-for-purpose selection based on the defined Context-of-Use.
Experimental Protocols for FIMD Validation and Application
Protocol 1: Establishing Predictive Validity for Safety
This protocol is designed to quantify a model's accuracy in predicting human-relevant safety outcomes, a critical aspect of the Predictive Validity component in FIMD.
- Compound Selection: Curate a reference set of 20-30 compounds with well-characterized clinical safety profiles, including known safe drugs, drugs withdrawn for toxicity (e.g., liver toxicity), and benchmark biologics.
- Model Dosing & Exposure: Treat the model (e.g., liver-organoid, organ-on-chip) with the compounds at concentrations covering therapeutic and supra-therapeutic ranges. Include appropriate positive and negative controls.
- Endpoint Analysis: Measure a panel of high-content endpoints at multiple time points. These include:
- Cell Viability: ATP-based assays.
- Cellular Stress: High-content imaging for oxidative stress (ROS), mitochondrial membrane potential, and DNA damage markers.
- Secretory Profile: Multiplexed cytokine/chemokine release assay.
- Tissue Integrity: Transepithelial electrical resistance (TEER) for barrier models.
- Data Integration & Score Calculation: Use the resulting data to calculate a prediction model. The concordance between the model's prediction and the known human outcome is used to generate the Predictive Validity sub-score within FIMD.
Protocol 2: Benchmarking Physiological Relevance for Monoclonal Antibodies
This methodology supports the scoring of the Physiological Relevance component, particularly for models used to test mAbs, a primary focus of recent FDA guidance [12] [16].
- System Setup: Establish the model system, which could be a humanized mouse model (expressing the human drug target) or a NAM such as a PBMC-loaded organ-on-chip system or a 3D co-culture of human immune and target cells.
- Challenge with Reference mAbs: Treat the model with a panel of reference therapeutic mAbs. This panel should include:
- mAbs with known on-target, off-tissue toxicity in humans.
- mAbs with known cytokine release syndrome risk.
- mAbs with a clean clinical safety profile.
- Phenotypic Readouts: Quantify key pharmacological and toxicological responses:
- Efficacy: Target cell depletion (e.g., via flow cytometry) or modulation of a functional endpoint.
- Safety: Measure cytokine storm markers (e.g., IL-6, TNF-α, IFN-γ) and histological evidence of tissue damage.
- PK/PD Relationship: Model the exposure-response relationship if possible.
- FIMD Scoring: The model's ability to recapitulate the human-specific efficacy and safety phenotypes of the reference mAbs directly contributes to its Physiological Relevance score. A model that correctly identifies the risky and safe mAbs scores highly.
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful implementation of FIMD and the execution of the described protocols rely on a set of key reagents and platforms. The selection of high-quality, well-characterized materials is fundamental to ensuring the reproducibility and reliability of the model validation data.
Table 3: Essential Research Reagents and Platforms for Disease Model Validation
| Reagent/Platform | Function | Application in FIMD Context |
|---|---|---|
| Reference Compound Sets | A curated library of drugs with definitively known human efficacy and safety profiles. | Serves as the gold standard for experimentally determining a model's Predictive Validity score. |
| Human Primary Cells/iPSCs | Non-immortalized cells or induced pluripotent stem cells derived from human donors. | Forms the biological basis for human-relevant NAMs; critical for scoring Physiological Relevance. |
| High-Content Imaging Systems | Automated microscopy platforms for multiparametric analysis of cell morphology and function. | Quantifies complex phenotypic endpoints (e.g., cytotoxicity, oxidative stress) for Technical Robustness. |
| Multiplex Cytokine Assays | Bead- or ELISA-based kits to simultaneously quantify dozens of secreted proteins. | Measures critical immune and toxicity responses (e.g., cytokine release) for Safety Pharmacological Assessment. |
| AI/ML Analytics Platforms | Software utilizing artificial intelligence and machine learning to analyze complex datasets. | Integrates high-dimensional data from NAMs to generate predictive readouts and support Context-of-Use Alignment [31]. |
| Cianidanol | Cianidanol, CAS:8001-48-7, MF:C15H14O6, MW:290.27 g/mol | Chemical Reagent |
| Allocryptopine | Allocryptopine | Allocryptopine, a natural isoquinoline alkaloid. Key research applications include neuroprotection and anti-inflammation. For Research Use Only. Not for human use. |
The Framework to Identify Models of Disease (FIMD) provides the pharmacological research community with a critically needed tool for the systematic, quantitative evaluation of disease models. By moving beyond subjective preference and tradition, the standardized FIMD score brings objectivity to the model selection process. As the industry undergoes a foundational shift—driven by both regulatory push [16] and the scientific pull of more predictive human-based NAMs [12] [31]—the adoption of frameworks like FIMD will be essential. It empowers scientists to make informed, defensible decisions, ultimately enhancing the translational success of new drugs and ensuring that resources are invested in the most promising, human-relevant research avenues.
The transition of therapeutic interventions from controlled laboratory settings to effective clinical applications remains a significant challenge in biomedical research. External validity, defined as the extent to which research findings from one setting, population, or species can be reliably applied to others, stands as a critical determinant of successful translation [36]. In pharmacology research, this concept is particularly crucial when evaluating animal disease models, which must bridge the gap between experimental findings and human therapeutic applications. High rates of drug development attrition—with many programs discontinuing even in clinical Phase III—highlight the persistent difficulties in predicting human responses based on preclinical data [37] [38]. This guide provides a comprehensive comparison of frameworks and methodologies for assessing external validity, offering researchers structured approaches to evaluate the translational potential of their experimental models.
Fundamental Concepts: Defining Validity in Animal Models
The assessment of animal models for biomedical research has traditionally centered on three established validity criteria, originally proposed by Willner in 1984 and now widely accepted across research domains [5] [39]. These criteria provide a multidimensional framework for evaluating how effectively a model recapitulates critical aspects of human disease.
Table 1: Core Validity Criteria for Animal Model Assessment
| Validity Type | Definition | Research Question | Example Assessment Method |
|---|---|---|---|
| Predictive Validity | How well the model predicts unknown aspects of human disease or response to therapeutics [5] | Does response to known therapeutics in the model correlate with human clinical responses? | Testing established treatments in the model and comparing outcomes to human clinical data |
| Face Validity | How closely the model replicates the phenotypic manifestations and symptoms of the human disease [5] [39] | Does the model display key observable characteristics of the human condition? | Comparative analysis of behavioral, physiological, or biochemical markers against human disease presentation |
| Construct Validity | How accurately the model reflects the underlying biological mechanisms and etiology of the human disease [5] [39] | Does the disease in the model share the same fundamental biological basis as the human condition? | Genetic, molecular, and pathway analysis to compare disease mechanisms between model and human |
These three criteria are not mutually exclusive, and a comprehensive validation strategy should address all dimensions. However, it is important to recognize that no single animal model perfectly fulfills all validity criteria, necessitating careful model selection based on research objectives and often requiring complementary approaches using multiple models [5] [15].
Figure 1: Multidimensional Framework for Assessing Animal Model Validity
Quantitative Assessment Frameworks: Structured Tools for Validity Evaluation
The Animal Model Quality Assessment (AMQA) Tool
Developed by GlaxoSmithKline to address translational challenges in drug development, the AMQA tool provides a structured question-based framework for evaluating animal models [15]. This approach emphasizes multidisciplinary collaboration between researchers, veterinarians, and pathologists to transparently assess a model's strengths and weaknesses. The assessment covers multiple dimensions, including: the fundamental understanding of the human disease; biological and physiological context; historical data on pharmacological responses in the model; how well the model reflects human disease etiology and progression; and the model's replicability and consistency [15]. The output facilitates informed decision-making about model selection and helps identify potential translational weaknesses before committing significant resources.
Framework to Identify Models of Disease (FIMD)
The FIMD represents a more recent approach designed to systematically evaluate various aspects of external validity in an integrated manner [38]. This framework was developed through a scoping review that identified eight key domains critical for model validation: etiology and pathogenesis, genetic basis, symptoms and clinical presentation, histopathology and morphology, biomarkers, comorbidities, disease progression, and response to treatment [38]. Unlike earlier approaches that relied heavily on researcher interpretation, FIMD provides a standardized scoring system that enables scientifically relevant comparisons between different models. This systematic approach helps researchers select the most appropriate model for demonstrating drug efficacy based on specific mechanisms of action and indications.
Table 2: Comparison of Structured Assessment Frameworks for External Validity
| Framework | Primary Focus | Key Features | Output | Applications |
|---|---|---|---|---|
| AMQA Tool [15] | Translational relevance for drug development | Question-based template, multidisciplinary input, transparent weakness identification | Qualitative assessment with identified gaps | Model selection, ethical review support, decision-making context |
| FIMD [38] | Efficacy model validation for specific indications | Eight-domain structure, standardized scoring, integrated validation | Quantitative scores enabling model comparison | Optimal model identification for specific drug mechanisms |
| Three Criteria Framework [5] [39] | General model evaluation | Established validity concepts (predictive, face, construct) | Categorical validation assessment | Initial model screening, educational contexts |
Experimental Protocols for Assessing External Validity
A Priori vs. A Posteriori Generalizability Assessment
In clinical trial design and translation, generalizability assessment methods can be categorized based on when the evaluation occurs relative to trial completion [40]. A priori generalizability (also called eligibility-driven) evaluates the representativeness of the eligible study population to the target population before a trial begins, using data from study eligibility criteria and observational cohorts [40]. This approach provides investigators the opportunity to adjust study design before trial initiation, potentially improving future generalizability. In contrast, a posteriori generalizability (or sample-driven) assesses the representativeness of enrolled participants to the target population after trial completion [40]. Despite the advantages of a priori assessment, fewer than 40% of published studies utilize this approach, representing a significant missed opportunity for improving translational research [40].
Benchmarking Against Simple Models
In quantitative systems pharmacology (QSP), where complex mechanistic models integrate knowledge of physiology, disease, and drug effects, assessing predictive performance against simpler models provides a valuable validation approach [41]. This methodology involves developing simplified versions of complex models through techniques such as focusing on steady states, lumping compartments, and using approximations. The QSP model's predictions are then systematically compared against those generated by the simpler models. This benchmarking approach helps identify when added complexity genuinely improves predictive capability versus when it merely leads to overfitting of noise in the data [41]. Examples where this approach has proven valuable include cardiotoxicity prediction, where simple models of ion channel block sometimes outperformed complex biophysical models, and oncology drug combinations, where simple probabilistic models have successfully predicted combination responses [41].
Figure 2: Workflow for Benchmarking Complex Models Against Simpler Alternatives
Table 3: Key Research Reagent Solutions for Validity Assessment
| Reagent/Resource | Function in Validity Assessment | Application Context |
|---|---|---|
| Genetically Engineered Models [5] [15] | Recapitulate specific genetic aspects of human diseases | Construct validity assessment for diseases with known genetic components |
| Disease Induction Compounds (e.g., MPTP, 6-OHDA) [5] | Create disease phenotypes in animal models | Face validity establishment for neurological disorders |
| Humanized Mouse Models [5] | Incorporate human biological components (cells, genes, tissues) | Improved predictive validity for immunology and infectious disease research |
| Validated Behavioral Assays [39] [38] | Quantify disease-relevant phenotypes and treatment responses | Face and predictive validity assessment for neurological and psychiatric disorders |
| Biomarker Panels [38] | Provide objective measures of disease state and treatment response | Bridging face and predictive validity across species |
| Electronic Health Record Databases [40] [42] | Provide real-world patient data for generalizability assessment | A priori and a posteriori generalizability assessment in clinical translation |
Advanced Approaches: Machine Learning and Cross-Site Generalizability
With the increasing application of artificial intelligence in biomedical research, new methodologies have emerged for assessing generalizability across healthcare settings. Transfer learning approaches enable the adaptation of models developed in one clinical context to new settings with different patient populations and data characteristics [42]. In a multi-site COVID-19 screening case study, three methods for implementing ready-made models in new healthcare settings were compared: applying a model "as-is" without modification; readjusting decision thresholds using site-specific data; and finetuning models via transfer learning [42]. The results demonstrated that site-specific customization consistently improved predictive performance, with transfer learning achieving the best results (mean AUROCs between 0.870 and 0.925) [42]. These approaches are particularly valuable when data sharing between institutions is limited by privacy concerns, technical barriers, or regulatory constraints.
Assessing external validity requires a multifaceted approach that integrates established validity criteria with structured assessment frameworks and rigorous experimental design. The evolving landscape of validity assessment emphasizes transparent evaluation of model strengths and limitations, systematic comparison of alternative approaches, and strategic selection of models based on specific research contexts. By implementing these methodologies, researchers can make more informed decisions about model selection and interpretation, potentially improving the translation of preclinical findings to clinical applications. Future directions in the field include increased integration of real-world data for generalizability assessment, development of more sophisticated benchmarking approaches for complex models, and application of machine learning techniques to predict translational success across diverse biological contexts and experimental systems.
Integrating Biomarkers and Clinically-Relevant Endpoints for Enhanced Predictivity
In the complex landscape of drug development, biomarkers and endpoints serve as essential navigational tools, guiding researchers from early discovery through clinical validation. Biomarkers, defined as "characteristics that are objectively measured and evaluated as indicators of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention" [43], provide critical insights into disease mechanisms and treatment effects. However, their true value emerges only when properly validated and connected to clinically meaningful endpoints—outcomes that measure directly how a patient feels, functions, or survives [44]. The integration of these elements within animal models represents a crucial strategy for enhancing the predictivity of preclinical research and reducing the high failure rates that plague drug development programs.
The validation of animal models for pharmacology research hinges on establishing robust links between measurable biomarkers and endpoints that truly matter to patients. This connection forms the foundation for translational success, enabling researchers to extrapolate findings from animal studies to human clinical outcomes with greater confidence. As this guide will demonstrate through comparative data and experimental protocols, the strategic alignment of biomarker assessment with clinically-relevant endpoints significantly strengthens the evidence chain supporting drug efficacy and safety, ultimately accelerating the development of more effective therapies.
Biomarkers and Endpoints: Definitions and Hierarchical Relationships
Classification and Hierarchy of Endpoints
Biomarkers and endpoints exist within a structured hierarchy that reflects their relationship to clinical benefit. This hierarchy, essential for interpreting their predictive value, ranges from direct measures of patient experience to indirect biological markers with unproven clinical relevance [44]:
- Level 1: True Clinical Efficacy Measures: Endpoints that directly capture how patients feel, function, or survive. Examples include death, symptomatic bone fractures, pain intensity, and progression to wheelchair bound status in multiple sclerosis.
- Level 2: Validated Surrogate Endpoints: Biomarkers that reliably predict clinical benefit for specific disease settings and intervention classes. Examples include HbA1c for microvascular complications in diabetes and blood pressure for cardiovascular outcomes with antihypertensives.
- Level 3: Biomarkers "Reasonably Likely to Predict Clinical Benefit": Non-validated surrogates with strong biological rationale and preliminary evidence. Examples include durable complete responses in hematologic cancers and large effects on progression-free survival in some solid tumors.
- Level 4: Correlates of Biological Activity: Measures of biological activity not established to predict clinical benefit. Examples include CD-4 counts in HIV, antibody levels in vaccine development, and PSA levels in prostate cancer prevention.
The following diagram illustrates the hierarchical relationship between different endpoint types and the validation pathway connecting them to clinical benefit:
Biomarker Types and Their Clinical Applications
Biomarkers serve distinct purposes throughout the drug development continuum, with each type requiring specific validation approaches [43]:
- Surrogate Endpoint Biomarkers: Measured after randomization but before the true clinical endpoint to draw conclusions about treatment effects on clinically meaningful outcomes. For example, prostate-specific antigen (PSA) has been studied as a surrogate for symptomatic prostate cancer.
- Prognostic Biomarkers: Predict the natural history of disease regardless of treatment, identifying patients at higher risk of disease development or progression. An example includes single nucleotide polymorphisms (SNPs) added to traditional risk factors for invasive breast cancer prediction.
- Predictive Biomarkers: Identify patients more likely to respond to a specific treatment, enabling targeted therapeutic approaches and personalized medicine strategies.
- Cancer Screening Biomarkers: Detect cancer in asymptomatic individuals, often requiring specialized methodology to reduce sample size requirements using stored specimens.
Table 1: Biomarker Types and Their Applications in Drug Development
| Biomarker Type | Primary Function | Validation Challenges | Examples |
|---|---|---|---|
| Surrogate Endpoint | Substitute for clinical endpoints to shorten trial duration | Requires rigorous statistical and biological validation; high risk of misleading conclusions | PSA for prostate cancer; HbA1c for diabetes complications |
| Prognostic | Predict disease risk or natural history | Must demonstrate added value beyond standard predictors; cost-benefit analysis needed | SNPs in breast cancer risk models |
| Predictive | Identify treatment responders | Requires demonstration of differential treatment effect across biomarker subgroups | Genetic markers for targeted cancer therapies |
| Screening | Detect disease in asymptomatic populations | Must balance sensitivity, specificity, and predictive values in low-prevalence settings | Various cancer early detection biomarkers |
Validation Frameworks for Biomarkers and Animal Models
Statistical and Biological Criteria for Surrogate Endpoint Validation
The validation of surrogate endpoints requires both statistical evidence and biological plausibility. A comprehensive approach involves five key criteria that create a appropriately high bar for acceptance [43]:
Statistical Criteria:
- Criterion 1: Acceptable Sample Size Multiplier: The ratio of sample size needed for predicted versus directly observed treatment effects. Investigators must determine if the larger sample size required with a surrogate endpoint justifies the benefit of shorter trial duration.
- Criterion 2: Prediction Separation Score >1: Indicates that prediction bands at extreme values of surrogate endpoints show no overlap, strongly suggesting the surrogate is informative for the true endpoint.
Biological and Clinical Criteria:
- Criterion 3: Similar Biological Mechanism: Treatments in new trials should share biological mechanisms with those in historical validation trials.
- Criterion 4: Similar Secondary Treatments: Post-surrogate endpoint management should not differ substantially from validation trials.
- Criterion 5: Low Risk of Late Harmful Effects: Potential for harmful side effects occurring after surrogate endpoint measurement should be minimal.
Animal Model Validation: Beyond the Traditional Criteria
Animal model validation has evolved beyond traditional criteria to more systematic frameworks that assess translational predictivity. The well-established validities provide a foundation for evaluation [5]:
- Predictive Validity: The measure of how well a model predicts currently unknown aspects of human disease or therapeutic outcomes.
- Face Validity: How closely a model replicates the human disease phenotype, including symptoms and signs.
- Construct Validity: How well the biological mechanisms inducing the disease phenotype reflect currently understood human disease etiology.
The Framework to Identify Models of Disease (FIMD) addresses limitations of traditional approaches by systematically evaluating eight domains critical to model validity [38]. This standardized framework enables more scientifically relevant comparisons between models and helps researchers select the most appropriate model based on a drug's mechanism of action and indication.
Table 2: Comparison of Animal Model Validation Frameworks
| Validation Approach | Key Components | Advantages | Limitations |
|---|---|---|---|
| Traditional Three Validities [5] | Predictive, face, and construct validity | Well-established; widely recognized; applicable across research fields | Subjective interpretation; lack of standardization; insufficient alone for efficacy prediction |
| FIMD Framework [38] | Eight domains including etiology, pathophysiology, symptoms, treatment response, biomarkers, natural history, ecology, and negative symptoms | Systematic and transparent; enables direct model comparison; mechanism-focused | More complex implementation; requires extensive model characterization |
| Sams-Dodd/Denayer Tool [38] | Five categories (species, disease simulation, face validity, complexity, predictivity) scored 1-4 | Simple scoring system; quick assessment | Lacks nuance for specific efficacy parameters; limited comprehensiveness |
Experimental Design and Methodological Considerations
Integrating the "Number Needed to Treat" in Biomarker Validation
A novel approach to biomarker validation incorporates the "Number Needed to Treat" (NNT) concept to establish clinically meaningful performance criteria [45]. This methodology structures communication within trial design teams to elicit value-based outcome tradeoffs:
- NNT Discomfort Range: The interval between NNTLower and NNTUpper where treatment decisions become ethically challenging—treating all patients entails excessive overtreatment, while withholding treatment misses too many beneficial opportunities.
- Application to Biomarker Validation: A useful biomarker test should separate patients into subgroups with NNT values outside the discomfort range, enabling clear treatment decisions for both positive and negative test groups.
- Study Design Implications: By defining the NNT discomfort range and desired NNT values for test-positive and test-negative subgroups, researchers can establish target predictive values to guide validation study design with explicit clinical utility goals.
The experimental workflow below illustrates how the NNT concept is integrated into biomarker validation study design:
Practical Considerations in Biomarker Assessment
Successful biomarker implementation requires careful attention to methodological factors that significantly impact apparent performance [46]:
- Cut-off Selection: The choice of biomarker threshold always represents a trade-off between sensitivity and specificity. Different patient subgroups (e.g., medical versus surgical) may require different cut-offs due to confounding factors.
- Study Population Composition: Biomarkers should be validated in the intended-use population, not just healthy controls versus severe cases. The spectrum of disease in the validation population significantly impacts performance measures.
- Prevalence Considerations: Positive and negative predictive values are highly dependent on disease prevalence, making it essential to validate biomarkers in populations with prevalence similar to intended use settings.
- Analytical Validation: Rigorous assessment of analytical performance, including precision, accuracy, and reproducibility, must precede clinical validation.
Table 3: Common Biomarker Study Limitations and Solutions
| Common Limitation | Impact on Results | Recommended Solution |
|---|---|---|
| Inappropriate cut-off | Suboptimal sensitivity or specificity for intended use | Establish separate cut-offs for relevant patient subgroups; validate in independent population |
| Spectrum bias | Overestimation of diagnostic performance | Include appropriate spectrum of disease severity in validation population |
| Inadequate sample size | Wide confidence intervals; unreliable performance estimates | Conduct power analysis based on clinical utility targets |
| Population prevalence mismatch | Misleading predictive values | Validate in population with prevalence similar to intended use setting |
| Ignoring comorbidities | Reduced performance in real-world settings | Stratify analysis by common comorbidities; adjust cut-offs accordingly |
The Scientist's Toolkit: Essential Reagents and Models
Table 4: Essential Research Tools for Biomarker and Endpoint Integration
| Tool Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| In Vitro Models | Patient-derived organoids; Microfluidic organ-on-a-chip systems; High-throughput screening assays | Preclinical biomarker identification; Drug response prediction; Toxicity assessment | Patient-derived organoids replicate human tissue biology more accurately than traditional 2D cell lines [47] |
| In Vivo Models | Patient-derived xenografts (PDX); Genetically engineered mouse models (GEMMs); Humanized mouse models | Cancer biomarker validation; Immunotherapy response assessment; Therapeutic efficacy testing | PDX models maintain tumor heterogeneity and drug response patterns from original patients [47] |
| Analytical Platforms | Single-cell RNA sequencing; CRISPR-based functional genomics; Multi-omics integration | Biomarker discovery; Mechanism of action studies; Patient stratification strategy development | Single-cell RNA sequencing reveals heterogeneity within cell populations and identifies biomarker signatures [47] |
| Imaging Technologies | PET/MRI; Advanced CT; Molecular imaging | Tracking real-time biomarker activity; Treatment response monitoring; Disease progression assessment | Advanced imaging helps track real-time biomarker activity in live animal models, enhancing translational research [47] |
| Glutaric acid | Glutaric acid, CAS:68937-69-9, MF:C5H8O4, MW:132.11 g/mol | Chemical Reagent | Bench Chemicals |
| Tecnazene | Tecnazene, CAS:28804-67-3, MF:C6HCl4NO2, MW:260.9 g/mol | Chemical Reagent | Bench Chemicals |
The integration of biomarkers with clinically-relevant endpoints represents a fundamental strategy for enhancing the predictivity of animal models in pharmacology research. This comparative guide demonstrates that successful integration requires: (1) adherence to hierarchical endpoint relationships with understanding that not all biomarkers qualify as surrogate endpoints; (2) application of rigorous validation frameworks that incorporate both statistical evidence and biological plausibility; (3) implementation of innovative methodologies like NNT-based clinical utility assessment; and (4) careful attention to practical considerations including cut-off selection and population characteristics.
The strategic alignment of biomarker assessment with clinically meaningful endpoints strengthens the entire drug development pipeline, from early target identification through late-stage clinical trials. By applying the principles and methodologies outlined in this guide, researchers can make more informed decisions about which animal models and biomarkers offer the greatest potential for translational success, ultimately contributing to more efficient development of effective therapies for patients in need.
Navigating Pitfalls: Troubleshooting Common Validation Challenges
In preclinical pharmacology, the scientific validity of findings from animal studies is the cornerstone for developing new therapeutic drugs. Internal validity, which refers to the extent to which a causal relationship between experimental treatment and outcome is warranted, critically depends on rigorous experimental design and conduct that minimize systematic bias [48]. Accumulating evidence indicates that poor internal validity poses a substantial threat to the reproducibility and translational value of animal research, potentially misleading drug development pathways and squandering research resources [49] [50] [51].
This guide objectively examines the current limitations in internal validity within animal disease models, focusing specifically on the critical roles of randomization and blinding as methodological safeguards against bias. By comparing suboptimal practices with robust experimental designs and providing actionable protocols, we aim to equip researchers with the tools necessary to enhance the scientific rigor of their preclinical studies, thereby strengthening the foundation for pharmacological discovery and development.
The Current Landscape: Widespread Flaws in Experimental Design
A stratified, random sample of comparative laboratory animal experiments published in 2022 revealed a startling prevalence of design flaws. The analysis found that only 0–2.5% of studies utilized valid, unbiased experimental designs [50]. The majority employed Cage-Confounded Designs (CCD), where treatments are assigned to entire cages and the statistical analysis erroneously uses the individual animal as the unit of analysis. This flaw violates the fundamental assumption of data independence required for valid statistical tests like ANOVA, leading to spuriously inflated sample sizes through data pseudoreplication, reduced variances, narrowed confidence limits, and an increased probability of false positive results [50].
Furthermore, systematic assessments of both animal study applications submitted to ethical review boards and the resulting scientific publications show dismally low rates of describing or reporting basic measures against bias. In Swiss applications, descriptions of measures ranged from just 2.4% for a statistical analysis plan to 19% for a primary outcome variable. Reporting in the subsequent publications was similarly low, ranging from 0% for sample size calculation to 34% for a statistical analysis plan [48]. These deficiencies undermine the reliability of the harm-benefit analysis used in the ethical licensing of animal experiments and, ultimately, the credibility of the research findings [48].
Table 1: Prevalence of Measures Against Bias in Animal Research Protocols and Publications
| Measure Against Bias | Description in Applications (n=1,277) | Reporting in Publications (n=50) |
|---|---|---|
| Primary Outcome Variable | 19.0% | 22.0% |
| Statistical Analysis Plan | 2.4% | 34.0% |
| Inclusion/Exclusion Criteria | 11.3% | 18.0% |
| Randomization | 11.9% | 16.0% |
| Blinded Outcome Assessment | 6.8% | 12.0% |
| Allocation Concealment | 3.6% | 8.0% |
| Sample Size Calculation | 7.4% | 0.0% |
Critical Analysis of Key Limitations and Their Impact
The Confounding Cage Effect and Unit of Analysis Error
A fundamental and frequently overlooked source of bias in animal research is the cage effect. No cage of animals responds to a treatment in precisely the same way as another due to unique cage environments and individual phenotypic plasticity [50]. When each treatment group is assigned to a single cage, treatment effects become completely confounded by cage effects. In this scenario, any observed differences may stem from either treatment effects, cage effects, or some combination of the two, making it impossible to isolate the variance attributable to the treatment [50].
- Impact of the Error: In a completely confounded design with one cage per treatment, the effective sample size for ANOVA is one (n = 1), and the within-treatment (denominator) degrees of freedom equals zero, rendering a valid statistical analysis impossible [50].
- Recommended Designs: To control for cage effect, researchers should employ variations of Completely Randomized Designs (CRD) or, preferably, Randomized Block Designs (RBD) [50].
- In a simple CRD, animals are randomly assigned to cages, with all animals in a cage receiving the same treatment. The correct unit of analysis is the cage, and the sample size is the number of cages per treatment [50].
- In a Randomized Complete Block Design (RCBD), one animal from each treatment group is assigned to each cage, making each cage a "block." This design controls for cage effect and correctly uses the individual animal as the unit of analysis [50].
Inadequate Randomization and Allocation Concealment
Randomization ensures that each experimental unit has an equal probability of receiving a particular treatment, thereby distributing known and unknown covariates randomly across experimental groups [52] [53]. This process is a prerequisite for valid inferential statistics [53]. However, "selecting an animal 'at random' (i.e., haphazardly or arbitrarily) from a cage is not statistically random," as it involves human judgement and can introduce selection bias [53].
- Impact of Inadequate Randomization: Studies that do not report randomisation are more likely to report exaggerated effects that meet conventional measures of statistical significance [53]. Without proper randomization, systematic differences in animal characteristics or experimental conditions between groups can confound results, leading to biased outcome measures [50].
- Solutions and Protocols:
- Generation of Sequence: Use validated methods such as online random number generators (e.g., GraphPad QuickCalcs) or functions like
Rand()in spreadsheet software [53]. - Allocation Concealment: The generated sequence should be concealed from the researchers allocating animals to groups until the moment of assignment to prevent conscious or subconscious manipulation. The Experimental Design Assistant (EDA) offers a dedicated feature for this purpose [53].
- Advanced Strategies: For small sample sizes, simple randomization may lead to unbalanced groups. Blocking (randomising within smaller sub-experiments to account for nuisance variables like cage location or day of procedure) or minimisation (allocating to minimize imbalance across multiple factors like body weight) are encouraged strategies [53].
- Generation of Sequence: Use validated methods such as online random number generators (e.g., GraphPad QuickCalcs) or functions like
Failure to Implement Blinding
Blinding (or masking) ensures that researchers are unaware of group allocation during the preparation, execution, data acquisition, and/or analysis phases of an experiment. This minimizes the risk of unintentional influences that can introduce performance and detection bias [52]. For instance, knowledge of treatment groups might subtly affect how an animal is handled, how a outcome is measured, or how data is interpreted.
- Impact of Unblinded Studies: Similar to a lack of randomization, failure to blind is associated with inflated effect sizes [49] [48]. Unblinded assessment can systematically alter measurements in favor of the hypothesized outcome.
- Solutions and Protocols:
- Practical Implementation: Blinding requires strong protocols and a team approach [52]. Treatments can be coded by a third party not involved in the experiment. For example, in a vaccination study, treatments (e.g., PBS control and different vaccine formulations) were randomly assigned, coded, and investigators were blinded to the identity of the groups until after statistical analysis was complete [50].
- Scope of Blinding: Whenever possible, blinding should be applied during the administration of treatments, the monitoring of outcomes, and the assessment of histological or behavioral end-points.
The following workflow visualizes the integration of these core safeguards into a robust experimental pipeline.
Diagram: Integrated workflow for robust experimental design, highlighting key bias-control measures.
Comparative Analysis of Experimental Designs
The choice of experimental design fundamentally determines a study's ability to yield unbiased, interpretable results. The table below compares common designs, highlighting their relative merits and limitations.
Table 2: Comparison of Common Experimental Designs in Animal Research
| Experimental Design | Key Principle | Unit of Analysis | Advantages | Limitations |
|---|---|---|---|---|
| Cage-Confounded Design (CCD) | Treatments assigned to entire cages; animal used as unit. | Individual Animal (Incorrect) | Logistically simple. | Fatally flawed. Complete confounding of treatment and cage effects. Invalid statistics, high false-positive rate [50]. |
| Completely Randomized Design (CRD) | Animals randomly assigned to cages; all in cage get same treatment. | Cage | Controls for cage effect. Straightforward design and analysis [50]. | Increased variability. Requires more cages, potentially raising costs and ethical concerns [50]. |
| Randomized Complete Block Design (RCBD) | One animal from each treatment group placed in each cage (block). | Individual Animal | Excellent control for cage effect. Increases homogeneity, reduces data variance [50]. | Limits treatments per cage to cage capacity. Analysis requires two-way ANOVA [50]. |
Implementing rigorous designs requires not only methodological knowledge but also the appropriate tools and resources. The following table details key solutions for enhancing internal validity.
Table 3: Research Reagent and Resource Solutions for Robust Experimentation
| Tool / Resource | Category | Primary Function | Example / Note |
|---|---|---|---|
| Computerized Random Number Generator | Software Tool | Generates truly random allocation sequences to prevent selection bias. | GraphPad QuickCalcs, Rand() in Excel/Sheets [53]. |
| Experimental Design Assistant (EDA) | Software Platform | Aids in designing robust experiments, including randomization and allocation concealment [53]. | Online tool from the NC3Rs. |
| Code-Labelling System | Laboratory Practice | Enables blinding by masking treatment group identities from researchers and technicians. | Using coded syringes for injections; labeled treatment "A", "B", "C" [50]. |
| Statistical Software (Beyond Basic) | Software Tool | Enables analysis of complex designs like RCBD with two-way ANOVA or Mixed Models. | Required for RCBD and split-plot designs; not always in GraphPad Prism [50]. |
| ARRIVE Guidelines | Reporting Framework | Checklist to ensure comprehensive reporting of critical methodological details in publications [49]. | Endorsed by over 1,000 journals. |
The evidence is clear: overcoming limitations in internal validity is not a peripheral concern but a central prerequisite for generating reliable and translatable knowledge from animal disease models. Widespread failures in controlling for cage effects, implementing proper randomization, and applying blinding have created a credibility crisis in preclinical pharmacology, contributing to high attrition rates in drug development [50] [51]. The solutions, however, are attainable. By moving beyond cage-confounded designs to statistically sound frameworks like Randomized Block Designs, by replacing haphazard allocation with properly concealed randomization, and by integrating blinding throughout the experimental process, researchers can significantly bolster the internal validity of their work. Adopting these practices, supported by the tools and protocols outlined in this guide, will enhance the scientific rigor of animal research, ensure a more ethical use of resources and animal lives, and ultimately strengthen the pipeline of new pharmacological therapies.
Addressing Species Gaps and Biological Differences That Hinder Translation
Species differences between animal models and humans present a fundamental challenge in pharmacological research, leading to high failure rates for drugs that appear safe and effective in preclinical studies. This guide provides a comparative analysis of traditional animal models and emerging human-relevant approaches, detailing their methodologies, key performance data, and applications. As regulatory agencies like the FDA now actively promote a shift toward New Approach Methodologies (NAMs) [12] [54], understanding these tools and their validation is crucial for modern research and development.
The "species gap" refers to the fundamental biological differences between animal models and humans that hinder the accurate prediction of drug safety and efficacy. Despite long being a standard, animal testing has a dismal translational success rate of approximately 5% [55] [56]. This high failure rate is driven by disparities in genetics, metabolism, immune responses, and disease pathophysiology [57]. For instance, many human diseases do not occur naturally in animals and must be artificially induced, creating models that lack the true complexity of human conditions [57]. Consequently, over 90% of drugs that pass animal trials fail in human clinical studies due to safety concerns or a lack of efficacy [34] [57]. This critical bottleneck has accelerated the development and adoption of human-based NAMs, which aim to provide more predictive and ethically sound solutions for pharmacology research.
Comparative Analysis: Animal Models vs. Human-Based New Approach Methodologies (NAMs)
The following section provides a detailed, data-driven comparison of traditional animal models and the primary categories of human-relevant NAMs.
Performance Metrics and Key Differentiators
Table 1: Comparative Performance of Research Models
| Model Category | Key Characteristics | Predictive Accuracy for Human Response | Typical Applications | Major Limitations |
|---|---|---|---|---|
| Animal Models [12] [57] | Inbred species (e.g., mice, rats), whole-body physiology | ~8% (based on 92% clinical trial failure rate) [56] | Whole-body toxicity, complex physiology | Significant species differences, artificially induced diseases, high cost, ethical concerns |
| Organ-on-a-Chip (OoC) [55] [58] | Microfluidic device with human cells, mimics tissue-tissue interfaces | 80%+ (e.g., Liver-Chip: 87% sensitivity, 100% specificity for DILI) [55] [58] | Disease modeling, drug safety (e.g., DILI), nutrient transport | Modeling single organs in isolation, ongoing standardization |
| Organoids [55] [59] | 3D cell cultures from human stem cells, patient-specific | Higher human-relevance, captures patient diversity [56] | Disease mechanism studies, personalized medicine, drug screening | Variable maturity and size, lack standardized protocols |
| In Silico & AI Models [55] [54] | Computer simulations, AI/ML analysis of existing data | Improves with data quality and volume; used for prioritization [54] | Predicting PK/PD, toxicity, virtual screening, de novo drug design | Dependent on quality input data; can oversimplify biology [60] |
| Human-Based In Vitro Assays [55] | Uses primary human cells or cell lines in controlled environments | More predictive than animal models for human-specific effects [55] | High-throughput screening, mechanistic toxicology, efficacy testing | Often lacks the complexity of entire tissues or organs |
Quantitative Validation Data
Table 2: Experimental Validation Data for Key NAMs
| Technology | Validation Study Context | Reported Performance Metric | Comparative Animal Model Performance |
|---|---|---|---|
| Liver-Chip [58] | Prediction of Drug-Induced Liver Injury (DILI) | 87% Sensitivity, 100% Specificity [58] | Deemed safe in animals, but caused severe reactions in humans [56] |
| Immune Organoids [56] | Preclinical testing of Centi-Flu universal flu vaccine | Triggered production of B cells and activation of CD4+/CD8+ T cells, predicting broad immune response [56] | Previously validated in mice, rats, pigs, and ferrets, but human data was sought for de-risking [56] |
| AI-Driven Discovery [55] | General drug discovery and safety testing | Potential to reduce timelines and costs by at least half [55] | Traditional animal-based development is costly and time-intensive, with high failure rates [55] |
| Human Skin Models [55] | Testing injected drugs and implanted devices | Uses live immunocompetent ex vivo human skin, viable for up to 7 days; more predictive than animal/engineered models [55] | Animal skin differs significantly from human skin in structure and immune response. |
Experimental Protocols for Key NAMs
To ensure reproducibility and facilitate adoption, this section outlines detailed protocols for critical assays in human-relevant research.
Protocol: Drug-Induced Liver Injury (DILI) Assessment Using a Liver-Chip
This protocol is based on the Emulate Liver-Chip S1, the first Organ-Chip accepted into the FDA's ISTAND pilot program [58].
1. Principle: A microfluidic device containing a porous membrane is seeded with primary human hepatocytes on one side and human endothelial cells (e.g., liver sinusoid endothelial cells) on the other. The system is perfused with culture medium, creating a physiologically relevant microenvironment that can be exposed to test compounds to model human-specific toxic responses [58].
2. Reagents and Materials:
- Emulate Liver-Chip S1 or comparable MPS
- Primary human hepatocytes (cryopreserved)
- Primary human liver sinusoid endothelial cells
- Perfusion Base Medium and Supplements
- Test compound(s) and control articles (e.g., known hepatotoxicants like troglitazone vs. safe compounds)
- Cell culture reagents (trypsin-EDTA, PBS, etc.)
- Viability assay kits (e.g., for ATP content, LDH release)
- Immunofluorescence staining reagents (antibodies for albumin, CYP enzymes, BSEP)
3. Step-by-Step Workflow:
- Chip Priming: Activate the chip according to manufacturer's instructions and coat with appropriate extracellular matrix proteins.
- Cell Seeding: Seed primary human hepatocytes into the parenchymal channel and human endothelial cells into the vascular channel. Allow cells to adhere and form confluent layers.
- Tissue Maturation: Perfuse chips with culture medium for 5-7 days to allow for the formation of functional tissue barriers and the expression of key metabolic enzymes and transporters.
- Dosing: Introduce the test compound into the perfusion medium at clinically relevant concentrations. Include vehicle controls and benchmark compounds.
- Endpoint Analysis (After 7-14 days of exposure):
- Biomarker Analysis: Collect effluent medium daily to measure markers of injury (e.g., ALT, AST release).
- Viability Staining: Perform live/dead staining or measure intracellular ATP levels.
- Functional Assessment: Measure albumin and urea production, and cytochrome P450 activity.
- Histology: Fix and immunostain chips for tight junction proteins, bile acid transporters, and metabolic enzymes.
- Data Interpretation: Compare the response profile of the test article to that of known hepatotoxicants and safe compounds. A significant change in biomarkers and loss of function relative to controls indicates potential DILI risk.
Protocol: Immune Response Profiling Using 3D Immune Organoids
This protocol is adapted from platforms used to test immunotherapies and vaccines, such as the universal flu vaccine candidate Centi-Flu [56].
1. Principle: Immune organoids are generated from human peripheral blood mononuclear cells (PBMCs) or hematopoietic stem cells from diverse donors. These 3D structures recapitulate key aspects of the human immune system and can be "vaccinated" or exposed to therapeutics to measure antigen-specific B-cell and T-cell activation [56].
2. Reagents and Materials:
- Human PBMCs from multiple donors (reflecting genetic diversity)
- 3D bioreactor or low-attachment U-bottom plates
- Lymphocyte culture medium with necessary cytokines (e.g., IL-2, IL-7, IL-15)
- Vaccine antigen or therapeutic candidate (e.g., Centi-Flu)
- Antigens for challenge (e.g., various influenza strains)
- Flow cytometry antibodies (for CD3, CD4, CD8, CD19, CD38, CD27, activation markers)
- ELISpot kits for IFN-γ (T-cell) and antibody-secreting cell (B-cell) analysis
3. Step-by-Step Workflow:
- Organoid Generation: Isolate PBMCs from donor blood and culture them in 3D conditions with a cytokine cocktail that promotes the survival and differentiation of T cells, B cells, and antigen-presenting cells.
- Vaccination/Treatment: After 3-5 days of pre-culture, expose the immune organoids to the vaccine antigen or immunotherapeutic agent.
- Antigen Challenge: Several days post-treatment, challenge the organoids with specific antigens to assess the recall response.
- Immune Monitoring (7-14 days post-treatment):
- Humoral Immunity: Use ELISA to measure antigen-specific immunoglobulin (IgG, IgA) levels in the supernatant.
- B-Cell Analysis: Use flow cytometry to identify antigen-specific memory B cells and plasma cells.
- T-Cell Analysis: Use intracellular cytokine staining and ELISpot to quantify antigen-specific CD4+ and CD8+ T-cell responses.
- Data Interpretation: A successful response is indicated by a statistically significant increase in antigen-specific antibodies and T-cell activation in treated organoids compared to untreated controls.
Diagram 1: Experimental workflow for Liver-Chip-based DILI assessment.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of NAMs relies on a suite of specialized reagents and tools. The table below details key solutions for setting up and running advanced human-relevant assays.
Table 3: Key Research Reagent Solutions for Human-Relevant Assays
| Item | Function/Application | Key Features & Considerations |
|---|---|---|
| Primary Human Cells [55] | Provide species-relevant, donor-specific biological data for organoids, OoC, and assays. | Source from diverse donors (age, sex, ethnicity); cryopreserved for viability. |
| Specialized Culture Media | Support the growth and maintenance of complex human cell systems in 3D or perfused cultures. | Must be defined, serum-free, and contain necessary cytokines/growth factors. |
| Organ-on-a-Chip Kits [58] | Microphysiological systems (MPS) that mimic human organ structure and function. | Include microfluidic devices, membranes, and often cell-specific coating reagents. |
| Biomarker Assay Kits | Quantify functional outputs (e.g., albumin) and toxicity markers (e.g., ALT, LDH). | High-sensitivity, validated for use with cell culture supernatants. |
| Flow Cytometry Antibody Panels | Deeply phenotype and characterize immune cells in organoids or co-cultures. | Require pre-conjugated, validated antibodies for human surface and intracellular markers. |
| AI/Data Analysis Platforms [55] [54] | Analyze complex datasets from NAMs, predict outcomes, and model biological pathways. | Must integrate multi-omics data; require robust computational infrastructure. |
| Fumaric Acid | Fumaric Acid|High-Purity Reagent|RUO | High-purity Fumaric Acid for research. Key intermediate in the Krebs cycle. Used in biochemical, metabolic, and materials science. For Research Use Only. Not for human consumption. |
| Carnitine Chloride | DL-Carnitine Hydrochloride|RUO | DL-Carnitine hydrochloride (CAS 461-05-2) is a research compound for energy metabolism and antioxidant studies. For Research Use Only. Not for human consumption. |
Regulatory and Strategic Outlook
The regulatory landscape is rapidly evolving to embrace NAMs. The FDA Modernization Act 2.0 (2022) legally removed the animal-testing mandate, allowing the use of human-based alternatives in drug applications [58]. In April 2025, the FDA released a detailed roadmap outlining a plan to phase out routine animal testing, making it "the exception rather than the rule" within 3-5 years [12] [54] [58]. This is complemented by NIH initiatives that prioritize funding for research incorporating human-based technologies [59] [58]. For researchers, this shift means that integrating NAMs early in the R&D pipeline is no longer just a scientific preference but a strategic imperative to align with regulatory expectations, de-risk development, and accelerate the delivery of effective therapies to patients.
Diagram 2: Strategic rationale for transitioning to a NAM-based R&D paradigm.
A critical challenge in modern pharmacology is the prevalent use of animal models that fail to adequately represent the complex reality of human patients, particularly concerning age-related diseases and multi-morbidity conditions. While animal models remain indispensable for advancing translational research by identifying effective treatment targets and strategies for clinical application [61], their predictive value is often limited by oversimplified disease representations. The physiological processes of humans and mammals are complex in terms of circulatory factors, hormones, cellular structures, and tissue systems [27], yet many traditional models investigate single disease entities in young, genetically identical animals under highly controlled conditions. This approach creates a translational gap that becomes particularly evident when drugs that showed promise in animal studies fail in human clinical trials due to unanticipated interactions in elderly patients with multiple co-existing conditions [38]. This article objectively compares the capabilities and limitations of various animal model systems in replicating human co-morbidities and aging, providing researchers with experimental data and methodologies to enhance model selection for pharmacological research.
Current Animal Model Limitations in Mimicking Human Complexity
The Validity Framework for Disease Modeling
Researchers traditionally rely on three well-established criteria to assess animal model relevance: face validity (reproduction of clinical symptoms), construct validity (similarity in underlying biology), and predictive validity (response to clinically effective treatments) [38]. However, these criteria are often applied inconsistently and fail to systematically capture the multifaceted nature of human diseases, especially in complex aging populations. The Framework to Identify Models of Disease (FIMD) has been proposed to standardize model assessment across eight domains, integrating various aspects of external validity in a more systematic manner [38]. Despite these advances, significant limitations persist in modeling human complexity.
Specific Limitations in Co-morbidity and Aging Research
The ideal animal disease model does not exist [62], and this is particularly true for co-morbidity and aging research. Key limitations include:
Genetic Uniformity vs. Human Diversity: Most rodent models use inbred strains that do not have genetic variations like humans, limiting their translational relevance for complex disease interactions [27] [62]. For example, the C57BL/6J strain is used for studying multigenic factors in diet-induced obesity, but exhibits significant variability in weight gain across studies due to factors like gut microbiota and thermoregulation [62].
Compressed Lifespan Considerations: The relatively short lifespan of rodents complicates the study of slowly progressive, age-related diseases that develop over decades in humans [62]. This fundamental biological difference creates challenges in modeling the progressive accumulation of multiple pathological conditions.
Single-Disease Paradigm: Most models are designed to study single disease entities, failing to replicate the complex pathophysiological interactions that occur in patients with multiple chronic conditions [62] [38]. This oversimplification can lead to overestimation of drug efficacy and failure to detect adverse interactions.
Species-Specific Therapeutic Responses: There are notable species-specific differences in therapeutic responses. For instance, morphine, an effective but addictive painkiller in humans and C57BL/6J mice, is ineffective and non-addictive in DBA/2J mice [62], highlighting how genetic background can dramatically alter pharmacological responses.
Comparative Analysis of Model Systems for Complex Conditions
Quantitative Comparison of Animal Model Capabilities
Table 1: Comparison of Animal Model Capabilities for Co-morbidity and Aging Research
| Model Type | Strengths for Co-morbidity/Aging | Limitations for Co-morbidity/Aging | Human Relevance Score | Key Applications |
|---|---|---|---|---|
| Genetically Engineered Mice | Genetic tractability; customizable pathways; established protocols [27] | Typically study single pathways; limited genetic diversity; minimal age consideration [62] | Moderate-High (for specific pathways) | Monogenic diseases; targeted therapeutic testing [63] |
| Humanized Mice | Can express human genes/cells; better for human-specific pathophysiology [63] [18] | High cost; complex breeding; immune system limitations | High (for human-specific mechanisms) | Cancer, infectious diseases, autoimmune disorders [18] |
| Rats | Larger size for procedures; comprehensive physiological monitoring [27] | Fewer genetic tools than mice; limited co-morbidity models | Moderate | Cardiovascular diseases, metabolic studies, surgical models [27] [61] |
| Non-Human Primates | Close genetic/physiological similarity; complex cognitive assessment [27] [18] | Extreme ethical constraints; high cost; long maturation | Very High (for systemic interactions) | Neurodegenerative disorders, complex infectious diseases [27] [18] |
| Naturalized Mice | Diverse environmental exposures; more natural immune systems [63] | Recent development; standardization challenges | Moderate-High (for immune/environmental interactions) | Autoimmune diseases, inflammatory conditions [63] |
Table 2: Experimental Readouts and Validation Parameters for Complex Models
| Parameter Category | Specific Metrics | Data Type | Translation Potential | Technical Considerations |
|---|---|---|---|---|
| Multi-system Functional Assessment | Cardiac output, renal function, respiratory capacity, cognitive performance [62] | Quantitative physiological measurements | High (clinical relevance) | Requires specialized equipment; longitudinal monitoring |
| Molecular Biomarkers | Inflammation markers, oxidative stress indicators, metabolic hormones [61] | Biochemical/ molecular assays | Moderate-High (mechanistic insights) | Tissue-specific expression; dynamic changes |
| Histopathological Features | Multi-organ pathology, age-related changes, co-morbidity interactions [62] | Qualitative/ semi-quantitative scoring | Moderate (requires validation) | Expertise-dependent; standardized protocols essential |
| Therapeutic Response | Efficacy across conditions, adverse effect profile, drug-drug interactions [38] | Dose-response relationships | High (direct preclinical prediction) | Complex experimental design; polypharmacy simulations |
Emerging Solutions and Technological Advances
Several innovative approaches are being developed to address the challenge of modeling human co-morbidities and aging:
Humanized Mouse Models: These models are created by incorporating human genes, cells, or tissues into mice, making them better suited for studying diseases with specific human pathophysiological characteristics [63] [18]. For example, mice carrying human immune cells were used to uncover the causes of severe toxicities in CAR T-cell immunotherapy, leading to clinical trials to address these effects [63].
Naturalized Mouse Models: These models expose mice to more diverse environmental factors to better capture effects on human physiology, metabolism, and immune system function [63]. With more natural immune systems, these mice enabled researchers to reproduce the negative effects of drugs for autoimmune and inflammatory conditions that had previously failed in human clinical trials [63].
Genetically Modified Large Animals: Genetically modified pig organs, in which harmful animal genes are removed and human ones are added, represent a promising step for modeling complex human conditions and addressing donor shortage for patients with end-stage diseases [63].
Framework to Identify Models of Disease (FIMD): This systematic approach assesses various aspects of the external validity of efficacy models in an integrated manner, helping researchers identify the most relevant model to demonstrate drug efficacy based on its mechanism of action and indication [38].
Experimental Designs and Methodological Considerations
Protocol for Developing Co-morbidity Models
Table 3: Stepwise Protocol for Developing Complex Co-morbidity Animal Models
| Step | Procedure | Parameters to Monitor | Timeline | Validation Checkpoints |
|---|---|---|---|---|
| 1. Baseline Characterization | Comprehensive phenotyping of all systems | Body weight, metabolic panel, organ function, behavioral assessment | 2-4 weeks | Establish reference ranges; exclude outliers |
| 2. Primary Disease Induction | Implement first disease component using validated method (e.g., high-fat diet for metabolic syndrome) | Disease-specific biomarkers, system-specific functional tests | 4-12 weeks | Confirm disease establishment before progression |
| 3. Secondary Condition Introduction | Introduce second pathological component (e.g., renal injury model in obese animals) | Interaction markers, systemic inflammation, compensatory mechanisms | 4-8 weeks | Monitor for unexpected interactions or mortality |
| 4. Therapeutic Intervention | Administer test compound with appropriate controls | Efficacy across conditions, adverse effects, pharmacokinetic interactions | 2-8 weeks | Compare to single-disease responses |
| 5. Comprehensive Endpoint Analysis | Multi-system histological, molecular, and functional assessment | Pathological scoring, molecular pathways, functional integration | 2-4 weeks | Correlate findings with human disease manifestations |
Workflow Diagram for Co-morbidity Model Development
(Diagram 1: Sequential workflow for developing complex co-morbidity animal models)
Pathway Diagram for Age-Related Multi-Morbidity
(Diagram 2: Interconnected pathways in age-related multi-morbidity)
Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Co-morbidity and Aging Studies
| Reagent Category | Specific Examples | Function/Application | Considerations for Co-morbidity Studies |
|---|---|---|---|
| Genetic Engineering Tools | CRISPR/Cas9 systems, Cre-lox vectors, transposon systems [61] | Introduction of specific mutations, conditional gene expression | Multiple gene targeting; temporal control of induction |
| Humanized System Components | CD34+ hematopoietic stem cells, human cytokine cocktails, PBMC transplants [63] | Creation of humanized immune systems in animal models | Compatibility with multiple disease systems; functional validation |
| Metabolic Inducers | High-fat diets, streptozotocin, fructose solutions [27] [62] | Induction of metabolic diseases like diabetes, obesity | Progressive disease development; combination approaches |
| Aging Biomarkers | p16INK4a antibodies, senescence-associated beta-galactosidase kits, telomere length assays [62] | Assessment of biological age and senescence | Multi-tissue analysis; correlation with functional decline |
| Multi-system Functional Probes | Microdialysis systems, metabolic cages, telemetry implants [62] | Simultaneous monitoring of multiple physiological systems | Data integration challenges; minimizing animal stress |
| Molecular Pathway Reagents | Phospho-specific antibodies, cytokine arrays, oxidative stress detection kits [61] [62] | Analysis of signaling pathways across disease states | Pathway crosstalk consideration; tissue-specific expression |
The challenge of creating animal models that faithfully replicate human co-morbidities and aging remains significant, yet advancements in genetic engineering, humanized systems, and systematic validation frameworks are steadily bridging this translational gap. No single model can fully capture the complexity of aged human patients with multiple conditions, but strategic combination of complementary approaches—such as integrating humanized mice with naturalized environments or utilizing multi-system phenotyping in genetically diverse populations—offers a path forward. The biomedical research community's commitment to refining model systems [18], while adhering to ethical principles of the 3Rs (Replacement, Reduction, and Refinement) [27], will accelerate the development of more predictive preclinical models. As researchers continue to address the problem of unrepresentative samples, the integration of animal models with emerging technologies like organs-on-chips and computational approaches [63] [18] presents a promising strategy to enhance the translational value of pharmacological research while ultimately reducing dependence on animal models where scientifically appropriate.
The high failure rate of clinical drug development, despite extensive preclinical testing, presents a critical decision-making challenge for researchers and drug development professionals. This analysis examines the role of after-action reviews in improving the validation of animal disease models for pharmacology research. By systematically evaluating discrepancies between animal and human outcomes, researchers can refine model selection, enhance experimental design, and accelerate the adoption of human-relevant New Approach Methodologies (NAMs), ultimately creating a more predictive and efficient drug development pipeline.
The Clinical Failure Landscape: Quantifying the Animal Model Translation Gap
Animal models serve as a fundamental tool in preclinical drug development, yet their predictive value for human outcomes remains limited. A comprehensive analysis of the drug development pipeline reveals a startling 90% failure rate for drug candidates that enter clinical trials, with 40-50% failing due to lack of clinical efficacy and 30% due to unmanageable toxicity [64]. This translation gap represents a substantial scientific and financial challenge that after-action reviews can help address through systematic analysis of failure patterns.
Table 1: Primary Causes of Clinical Trial Failures for Drugs Advancing from Preclinical Animal Studies
| Failure Category | Percentage of Failures | Relationship to Animal Model Limitations |
|---|---|---|
| Lack of Clinical Efficacy | 40-50% | Disease pathophysiology in animals does not adequately recapitulate human disease [64] [30] |
| Unmanageable Toxicity | 30% | Species-specific differences in drug metabolism, tissue exposure, and off-target effects [64] |
| Poor Drug-Like Properties | 10-15% | Inaccurate prediction of human pharmacokinetics and pharmacodynamics [64] |
| Commercial/Strategic Factors | ~10% | Less directly related to animal model limitations |
The predictive validity of animal models varies substantially across disease areas. In Alzheimer's disease research, for example, an analysis of 20 interventions tested in 208 animal studies across 63 different animal models found that clinical outcomes correlated with animal results in only 58% of cases [28]. Similarly, in acute ischemic stroke research, only 3 out of 494 interventions that showed positive effects in animal models demonstrated convincing effects in patients [30].
Experimental Protocols for Model Validation
Retrospective Correlation Analysis
Purpose: To systematically quantify the predictive value of specific animal models by comparing historical preclinical and clinical results [28].
Methodology:
- Identify drug candidates that advanced to human trials based on animal data
- Categorize models by species, induction method (genetic, surgical, chemical), and disease endpoint measurement
- Document translational success rates for each model category
- Analyze patterns in failed predictions to identify specific model limitations
Key Parameters: Species characteristics, method of disease induction, outcome measurement techniques, and pharmacological class of interventions [28].
Multivariate Severity Assessment in Animal Models
Purpose: To standardize the assessment of animal distress and model validity using composite scoring systems that improve reproducibility and translational relevance [65].
Methodology:
- Monitor multiple parameters simultaneously: body weight, burrowing behavior, nesting activity, and clinical distress scores
- Apply non-parametric bootstrapping to generate robust estimates and 95% confidence intervals
- Combine parameters into a Relative Severity Assessment (RELSA) score through multidimensional transformation and mapping against reference procedures
- Compare maximum achieved severity (RELSAmax) across different models and interventions [65]
Key Parameters: RELSAmax score, parameter robustness across experimental variations, and comparison to defined reference sets.
Structure-Tissue Exposure/Selectivity-Activity Relationship (STAR) Profiling
Purpose: To improve drug candidate selection by balancing potency/specificity with tissue exposure/selectivity – factors often overlooked in traditional drug optimization [64].
Methodology:
- Classify drug candidates into four categories based on potency/selectivity and tissue exposure/selectivity
- Measure tissue-specific drug accumulation in disease-relevant versus normal tissues
- Correlate tissue distribution patterns with efficacy and toxicity outcomes
- Use classification to predict required clinical dose and likelihood of success [64]
Key Parameters: Tissue exposure ratios, specificity/potency measurements, and dose-efficacy-toxicity correlations.
Decision Framework: Animal Model Selection and Integration with NAMs
Table 2: Animal Model Predictive Performance Across Disease Areas
| Disease Area | Number of Interventions Assessed | Correlation Between Animal and Human Outcomes | Key Limitations Identified |
|---|---|---|---|
| Alzheimer's Disease | 20 interventions across 208 animal studies | 58% | Divergent results across different models; no single model represents full human syndrome [28] |
| Acute Ischemic Stroke | 494 interventions with positive animal results | 3 interventions successful in humans | Young, healthy animals vs. elderly human patients with comorbidities; treatment timing differences [30] |
| Depression | Multiple novel mechanisms | Limited predictive success | Inappropriate modeling of human symptomatology; failure to target correct clinical populations [66] |
| Cancer (Angiogenesis Inhibition) | Sunitinib and similar agents | Paradoxical effects | Increased metastasis in animal models not initially predicted; short-term vs. sustained treatment effects [30] |
The U.S. Food and Drug Administration has initiated a transformative three to five-year roadmap to reduce reliance on animal testing, particularly for monoclonal antibody therapies and biologics [12]. This shift is accompanied by NIH's prioritization of human-based research technologies, including the establishment of the Office of Research Innovation, Validation and Application (ORIVA) to coordinate development and validation of non-animal approaches [59]. These regulatory changes highlight the growing importance of integrating NAMs with traditional animal studies.
Figure 1: After-Action Review Workflow for Animal Model Validation. This diagram illustrates the systematic process for analyzing clinical failures to improve preclinical model selection and design.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Animal Model Validation and NAMs Integration
| Tool Category | Specific Technologies | Research Application | Validation Role |
|---|---|---|---|
| In Silico Modeling Platforms | AI/machine learning predictive tools, PBPK modeling [12] [34] | Predicting human pharmacokinetics, toxicity, and drug interactions | Cross-validate predictions with animal data to build confidence in human relevance |
| Organ-on-a-Chip Systems | Microengineered devices with human cells [12] [59] | Replicating human organ-level physiology and disease responses | Compare compound effects in human cells versus animal tissues to identify species-specific responses |
| 3D Tissue Models | Organoids from human stem cells [12] | Modeling complex human tissue interactions and disease mechanisms | Bridge between 2D cell cultures and whole animal systems for better human predictivity |
| Transgenic Animal Models | CRISPR-Cas9 genome editing [67] | Introducing human disease-relevant genetic modifications | Create more clinically relevant phenotypes by incorporating human genetic factors |
| Behavioral Assessment Tools | Burrowing, nesting tests, multivariate composite scoring [65] | Quantifying disease phenotypes and treatment efficacy in neurological disorders | Standardize outcome measurements across laboratories to improve reproducibility |
| Biomarker Assays | Genomics, proteomics, transcriptomics platforms [64] | Identifying translational biomarkers that bridge animals and humans | Develop biomarkers measurable in both animal models and clinical trials for better translation |
Integrated Testing Strategies: The Path Forward
The FDA's Modernization Act 2.0 and recent FDA roadmap represent a regulatory shift toward integrated testing strategies that combine multiple New Approach Methodologies (NAMs) with targeted animal studies [12] [34]. This approach recognizes that no single method can fully replace the complex physiology of a whole living system, but that human-relevant data should be prioritized wherever possible.
Organ-on-a-chip technology and organoids now enable researchers to study disease mechanisms and drug effects in human-derived tissues that capture patient-specific characteristics [12] [59]. These systems are particularly valuable for assessing tissue-specific drug exposure and toxicity – key factors in the STAR classification system that aims to improve candidate drug selection [64].
The transition away from animal models faces significant challenges, including standardization and validation of alternative methods [12] [34]. However, the systematic implementation of after-action reviews following clinical failures provides a powerful mechanism to accelerate this transition by identifying precisely where and why animal models fail to predict human outcomes, thereby guiding more strategic investments in human-relevant NAMs.
Figure 2: Transition from Traditional to Integrated Testing Strategies. This diagram contrasts the current over-reliance on animal data with emerging approaches that prioritize human-relevant New Approach Methodologies (NAMs).
Systematic after-action reviews of clinical failures provide invaluable insights for improving animal model selection, validation, and integration with human-relevant technologies. By implementing standardized protocols for retrospective analysis, adopting multivariate assessment frameworks, and strategically combining animal models with advanced NAMs, researchers can significantly enhance the predictive validity of preclinical research. This disciplined approach to learning from failure addresses a critical need in pharmacological research, potentially reducing the staggering 90% clinical failure rate and accelerating the development of safer, more effective therapeutics for patients.
Comparative Analysis and Future Directions in Model Validation
The use of animal models is a cornerstone of preclinical pharmacology research, providing critical insights into disease mechanisms and therapeutic potential before human trials. The validation of these models determines their predictive power and translational relevance. According to established scientific criteria, animal model validation rests on three fundamental pillars: predictive validity (how well the model predicts therapeutic outcomes in humans), face validity (how closely the model resembles the human disease phenotype), and construct validity (how well the model reflects the known etiology and biological mechanisms of the human disease) [5].
Different biomedical fields face distinct challenges in fulfilling these validation criteria. Oncology, immunology, and neuroscience each confront unique biological complexities that influence how animal models are developed, validated, and utilized. This guide provides an objective comparison of validated animal models across these three fields, highlighting their performance characteristics, methodological approaches, and applications in drug development.
Field-Specific Comparison of Animal Models
Table 1: Comparative Overview of Animal Models Across Research Fields
| Aspect | Neuroscience | Immunology | Oncology |
|---|---|---|---|
| Primary Validation Challenge | Limited construct validity due to complex human-specific cognition and behavior [5]. | Translating immune responses across species; human immune system complexity [68]. | Tumor microenvironment (TME) heterogeneity and species-specific cancer biology [68]. |
| Common Model Organisms | Mice, Rats, Non-human primates [27]. | Mice (including syngeneic and humanized), Zebrafish [27] [68]. | Mice (syngeneic, xenograft, PDX, GEMM), Rats [27] [68]. |
| Key Model Types | Transgenic (e.g., for SMA, Alzheimer's), Neurotoxin-induced (e.g., MPTP, 6-OHDA) [5]. | Syngeneic, Humanized (immune system), Inbred strains for specific immune defects [68]. | Cell-derived xenografts (CDX), Patient-derived xenografts (PDX), Genetically engineered mouse models (GEMMs), Syngeneic [68]. |
| Strengths | Strong face validity in neurotoxin models (e.g., MPTP in primates); strong construct validity in genetic models (e.g., SMA mice) [5]. | Syngeneic models offer intact immunity for I-O studies; Humanized models enable study of human-specific immune components [68]. | PDX models recapitulate patient tumor heterogeneity; Syngeneic models have intact immunity for immunotherapy screening [68]. |
| Limitations | Poor predictive validity for neurodegenerative diseases; high failure rate in clinical translation [5] [51]. | Syngeneic models lack human TME fidelity; Humanized models are costly and can have incomplete immune reconstitution [68]. | CDX models lack human TME and intact mouse immunity; PDX models are costly and time-consuming [68]. |
Table 2: Quantitative Data from Preclinical Studies Using Different Models
| Field | Model Type | Typical Use Case | Reported Translational Concordance | Common Endpoints |
|---|---|---|---|---|
| Oncology | Syngeneic Mouse | Immune-oncology drug screening [68]. | Variable; highly dependent on model and agent [68]. | Tumor growth inhibition, Immune cell infiltration (flow cytometry). |
| Oncology | Patient-Derived Xenograft (PDX) | Co-clinical trials, biomarker identification [68]. | High for some tumor genotypes and drug responses [68]. | Tumor volume, Pharmacodynamic biomarkers. |
| Neuroscience | Neurotoxin (6-OHDA) Rodent | Predictive validity for Parkinson's therapies [5]. | Historically better for symptomatic than disease-modifying therapies [5]. | Motor behavior (e.g., rotational tests). |
| Neuroscience | Transgenic (SOD1) Mouse | Amyotrophic Lateral Sclerosis (ALS) drug testing [5]. | Poor; numerous failed clinical translations [5]. | Survival time, Motor function decline. |
| Immunology | Humanized Mouse (e.g., NSG) | Preclinical evaluation of human-specific immunotherapies [68]. | Improving, but limited by incomplete human immune system reconstitution [68]. | Human immune cell engraftment, Cytokine levels, Drug PK/PD. |
Detailed Methodologies and Experimental Protocols
Oncology: Patient-Derived Xenograft (PDX) Models
Protocol for PDX Generation and Therapeutic Testing
- Tumor Implantation: Fresh tumor tissue from a patient biopsy or surgical resection is collected under sterile conditions. The tissue is cut into small fragments (approx. 10-30 mm³) and surgically implanted into the corresponding organ (orthotopic) or subcutaneously (ectopic) in an immunodeficient mouse (e.g., NOD-scid gamma (NSG) mouse) [68].
- Engraftment and Expansion: The implanted mice are monitored for tumor engraftment, which can take several months. Upon successful engraftment, the tumor (designated P0) is harvested, divided, and serially passaged into new recipient mice to expand the cohort (P1, P2, etc.) for experiments [68].
- Therapeutic Intervention: Once tumors in the experimental cohort (typically P2-P5) reach a predetermined volume (e.g., 100-150 mm³), mice are randomized into treatment and control groups. The treatment group receives the investigational drug, while the control group receives a vehicle.
- Endpoint Analysis: Primary endpoints are tumor volume measurement and survival. Secondary analyses include:
Immunology: Humanized Mouse Models for Immune-Oncology (I-O)
Protocol for Human Immune System (HIS) Mouse Generation and I-O Testing
- Strain Selection: Select a highly immunodeficient host strain such as NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) or BRG (BALB/c-Rag2tm1Il2rgtm1).
- Human Cell Engraftment: Two common methods are used:
- CD34+ Model: newborn mice are irradiated and injected with human CD34+ hematopoietic stem cells (HSCs) isolated from umbilical cord blood or fetal liver.
- PBMC Model: adult mice are irradiated and injected with human peripheral blood mononuclear cells (PBMCs) from a donor [68].
- Immune Reconstitution Validation: 12-16 weeks post-engraftment, peripheral blood is sampled via retro-orbital bleed or tail vein to assess the level of human immune cell chimerism using flow cytometry. Key markers include CD45+ (total human leukocytes), CD3+ (T cells), CD19+ (B cells), and CD33+ (myeloid cells) [68].
- Tumor Challenge and Treatment: Validated HIS mice are engrafted with human tumor cells (either cell lines or patient-derived tissue) subcutaneously or orthotopically. After tumor establishment, mice are treated with a human-specific I-O therapy (e.g., anti-PD-1 antibody).
- Analysis of Immune Response: Tumor growth is monitored. At endpoint, tumors, spleen, and blood are harvested. The TME and peripheral organs are analyzed by flow cytometry and IHC for human immune cell infiltration (e.g., CD8+ T cells), activation markers (e.g., CD69, Granzyme B), and exhaustion markers (e.g., PD-1, TIM-3) [68].
Neuroscience: Transgenic Model for Spinal Muscular Atrophy (SMA)
Protocol for Testing Therapeutics in SMNΔ7 Mice
- Model Selection: The SMNΔ7 mouse (on an FVB background) is a standard model for severe SMA. It carries two transgenes: a mutant Smn1 gene and a human SMN2 transgene.
- Genotyping and Cohort Setup: Tail biopsies are taken from pups at postnatal day (P) 3-5 for genotyping to identify homozygous SMA pups and wild-type littermate controls. Treatment and control groups are balanced by gender and litter.
- Therapeutic Administration: For a gene therapy test, the investigational drug (e.g., an SMN-expressing AAV9 vector) is administered via systemic injection (intracerebroventricular or intraperitoneal) at P1-2. Vehicle is injected into the control SMA group.
- Phenotypic Monitoring: Mice are monitored daily for key survival and phenotypic milestones, including:
- Righting reflex: The time it takes for a pup to right itself onto all fours when placed on its back.
- Necropsy and Tissue Collection: Tissues like spinal cord, muscle, and brain are collected for molecular analysis to measure SMN protein levels and assess motor neuron survival [5].
Signaling Pathways and Experimental Workflows
Diagram 1: Neuro-Immune Signaling in Oncology TME. This diagram illustrates how stress-induced sympathetic nervous system (SNS) activation releases Norepinephrine (NE) in the Tumor Microenvironment (TME). NE binds to β2-Adrenergic Receptors (β2-AR) on immune cells, triggering immunosuppressive effects. These include increased immunosuppressive cells (MDSCs, Tregs), impaired function of cytotoxic CD8+ T and NK cells, and upregulation of PD-L1 on tumor cells. The β-blocker Propranolol can inhibit this pathway [69] [70].
Diagram 2: PDX Model Generation Workflow. This workflow outlines the key steps in creating and utilizing Patient-Derived Xenograft (PDX) models. A patient tumor sample is processed and implanted into an immunodeficient mouse. After successful engraftment (P0), the tumor is serially passaged to expand the cohort. Mice from passages P2-P5 are used for therapeutic studies, analyzing tumor growth and biomarkers. Molecular characterization of the original patient sample and the final PDX tumor is crucial to confirm retention of key biological features [68].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Model Development and Analysis
| Reagent / Material | Field of Use | Function and Application |
|---|---|---|
| Immunodeficient Mice (e.g., NSG, BRG) | Oncology, Immunology | Serves as the in vivo host for engrafting human tumors (PDX) and/or human immune cells (HIS models), enabling the study of human-specific biology in a live organism [68]. |
| Human CD34+ Hematopoietic Stem Cells | Immunology | Used to create Humanized Immune System (HIS) mice. These cells reconstitute a human-like immune system in immunodeficient mice, allowing for preclinical testing of immunotherapies [68]. |
| ChEMBL Database | Multi-field | A large-scale, open-access database containing bioactivity data from in vivo assays. It allows researchers to investigate compound effects across different biological complexities and identify those tested in specific animal disease models [71]. |
| Anti-PD-1/PD-L1 Antibodies | Oncology, Immunology | Checkpoint inhibitors used as a standard immunotherapy control in both syngeneic and humanized mouse models to evaluate the efficacy of novel I-O agents or combinations [68] [72]. |
| Flow Cytometry Antibody Panels | Immunology, Oncology | Essential for immunophenotyping. Used to quantify and characterize immune cell populations (e.g., T cells, B cells, MDSCs) infiltrating the tumor microenvironment or in peripheral blood of HIS mice [68]. |
| Spatial Transcriptomics Platforms | Neuroscience, Oncology | Enables gene expression analysis within the context of tissue architecture. Crucial for understanding the tumor microenvironment and complex neural-immune cell interactions in their native spatial context [73] [72]. |
| β-Adrenergic Receptor Agonists/Antagonists | Neuroscience, Oncology | Pharmacological tools (e.g., agonist Isoproterenol, antagonist Propranolol) used to manipulate the neuro-immune axis in cancer models, specifically to study the impact of stress/β-AR signaling on anti-tumor immunity [70]. |
The validation and performance of animal models are critically dependent on the specific biological questions being asked in neuroscience, immunology, and oncology. While oncology has advanced with highly clinically relevant models like PDXs, and immunology has developed sophisticated humanized systems, neuroscience continues to grapple with the fundamental challenge of modeling complex human cognition and neurodegeneration.
The emerging field of cancer neuroscience highlights a growing recognition of the interconnectedness of these physiological systems and underscores the need for complex, integrated models [73] [69] [70]. Future directions will likely involve the development of more sophisticated humanized models that incorporate multiple systems (e.g., neural and immune components), increased use of AI and machine learning to analyze complex data from these models, and a stronger emphasis on multi-factorial validation approaches that combine several complementary models to improve translational predictability [5] [72]. The continued refinement of these tools is paramount for de-risking drug development and enhancing the success rate of translating preclinical findings into clinical benefits for patients.
The Role of Transgenic and CRISPR-Cas9 Models in Recapitulating Human Disease Genetics
The validity of preclinical animal models is a cornerstone of biomedical research, directly influencing the translation of pharmacological discoveries from the laboratory to the clinic. For decades, transgenic technologies enabled the introduction of foreign DNA into an organism's genome, allowing for the study of human disease genes in vivo. The subsequent advent of CRISPR-Cas9 genome editing has revolutionized the field by providing unprecedented precision and efficiency in creating genetic modifications. Within the context of a broader thesis on the validation of animal disease models for pharmacology research, this guide objectively compares the performance of these two foundational technologies. With regulatory agencies like the FDA actively publishing roadmaps to reduce reliance on traditional animal testing [12] [34] [58], the choice of a well-validated, genetically accurate model system is more critical than ever. This analysis summarizes quantitative data, details experimental protocols, and provides essential resource information to guide researchers in selecting the optimal model for their investigative needs.
Fundamental Principles
Transgenic Models: Traditional transgenic technology typically involves the random insertion of a DNA construct—often a cDNA sequence under the control of a promoter—into the mouse genome via pronuclear injection. This approach leads to overexpression of a foreign gene but does not modify the endogenous genomic locus. It is well-suited for studying gain-of-function mutations or expressing reporter genes [74].
CRISPR-Cas9 Models: The CRISPR-Cas9 system is a bacterial adaptive immune system repurposed for precise genome engineering. It utilizes a guide RNA (gRNA) to direct the Cas9 nuclease to a specific genomic location, where it creates a double-strand break (DSB). The cell repairs this break primarily through two pathways:
- Non-Homologous End Joining (NHEJ): An error-prone process that often results in small insertions or deletions (indels), leading to gene knockouts.
- Homology-Directed Repair (HDR): A precise repair mechanism that can be co-opted to introduce specific point mutations or insert new sequences (knock-ins) using a donor DNA template [75] [76] [77].
Comparative Workflow Visualization
The following diagram illustrates the key procedural differences and outcomes between traditional transgenic and CRISPR-Cas9 methods for generating animal models.
Performance Comparison: Quantitative Data and Experimental Evidence
Model Generation Efficiency
The table below summarizes key performance metrics for transgenic and CRISPR-Cas9 model generation, based on aggregated data from commercial service providers and published literature.
Table 1: Efficiency and Cost Comparison of Model Generation
| Performance Metric | Traditional Transgenic Models | CRISPR-Cas9 Models | Supporting Experimental Data |
|---|---|---|---|
| Typical Timeline | 9 - 12 months [74] | 6 - 8 months [74] | Reduced timeline cited as a key advantage of CRISPR [74]. |
| Targeting Efficiency | Low and variable; depends on random integration. | High; can achieve germline transmission in 20-80% of F0 founders [74]. | Commercial providers note ability to generate hundreds of different models due to high efficiency [74]. |
| Knock-in Capability | Limited to small inserts (<10 kb) via traditional methods. | Robust; techniques like Easi-CRISPR enable large knock-ins (e.g., reporter genes, human cDNA) [74]. | Easi-CRISPR uses long single-stranded DNA for efficient integration of large cassettes [74]. |
| Genetic Background Flexibility | Moderate; time-consuming to backcross. | High; can be directly applied to a broad range of backgrounds, including existing GE models [74]. | Cited as a key advantage for complex genetic studies and model customization [74]. |
| Cost (Relative) | Higher [74] | Lower [74] | Reduced cost compared to traditional methods is a documented advantage [74]. |
Accuracy in Recapitulating Human Disease Genetics
Different genetic manipulation techniques offer varying degrees of biological accuracy, which impacts their utility for modeling human disease.
Table 2: Model Accuracy and Pathological Recapitulation
| Aspect of Modeling | Traditional Transgenic Models | CRISPR-Cas9 Models | Application in Disease Research |
|---|---|---|---|
| Genetic Context | Random insertion; disrupted native regulatory elements. | Precise modification at the endogenous locus; preserves native gene regulation [77]. | Critical for diseases like ALS, where mutations in the SOD1 gene must be studied in their native context [78]. |
| Mutation Type | Primarily gain-of-function and overexpression. | Can model knockouts, point mutations, knock-ins, and epigenetic modifications [75] [76] [77]. | Used to correct disease-causing mutations in patient-derived cells for SCD and β-thalassemia [75] [79]. |
| Physiological Expression | Non-physiological, constitutive overexpression common. | Physiological expression levels and patterns from the native promoter. | Enables more accurate study of gene dosage effects, as seen in neurodegenerative disease modeling [77]. |
| Multigenic Diseases | Limited; difficult to stack multiple transgenes. | Efficient multiplexing; multiple gRNAs enable editing of several genes simultaneously [80]. | Powerful for cancer research, allowing disruption of multiple oncogenes/tumor suppressors in one model [80]. |
Experimental Protocols: Detailed Methodologies
Protocol for CRISPR-Cas9 Mediated Knock-in Model Generation
The following protocol, adapted from commercial service providers [74], outlines the steps for creating a precise knock-in model using advanced CRISPR techniques.
Step 1: Strategy and Reagent Design
- Target Selection: Identify the precise genomic locus for modification. Analyze the sequence for potential off-target sites using bioinformatics tools.
- gRNA Design: Design and synthesize a gRNA with high on-target efficiency and minimal off-target activity. The gRNA sequence should be adjacent to a Protospacer Adjacent Motif (PAM, e.g., NGG for SpCas9).
- Donor Template Construction: For knock-ins, design a single-stranded DNA (ssDNA) donor template (for Easi-CRISPR) or a double-stranded DNA donor. The template should contain the desired mutation or insert (e.g., reporter gene, epitope tag) flanked by homology arms (~800-1000 nt for ssDNA).
Step 2: Embryo Manipulation
- Preparation: Harvest fertilized zygotes from donor females.
- Microinjection/Electroporation: Introduce the CRISPR reagents—a complex of Cas9 protein (or mRNA) and gRNA, along with the donor DNA template—into the zygotes. Electroporation is increasingly used for its efficiency and throughput.
- Embryo Transfer: Surgically transfer the viable embryos into the oviducts of pseudopregnant surrogate females.
Step 3: Founder Animal Analysis
- Genotyping: Once offspring (F0 founders) are born, collect tissue samples (e.g., ear biopsies) for DNA extraction.
- Molecular Characterization: Use a combination of PCR-based genotyping and sequencing to identify animals carrying the intended genetic modification. For knock-ins, confirm precise junction sequences and ensure no random integration of the donor template.
- Off-Target Analysis: On a case-by-case basis, perform next-generation sequencing (NGS) of predicted off-target loci to confirm specificity, a service now offered by specialized providers [74].
Step 4: Colony Establishment
- Breeding: Cross confirmed F0 founder animals with wild-type mates to test for germline transmission and generate heterozygous F1 offspring.
- Expansion and Phenotyping: Establish a stable breeding colony from F1 animals. Commence detailed phenotypic and molecular analysis to validate the disease model.
Protocol for Transgenic Model Generation
This standard protocol highlights the key differences from the CRISPR-Cas9 approach, particularly the random integration event.
Step 1: DNA Construct Design and Preparation
- Assemble a linearized DNA construct containing a promoter element (e.g., a ubiquitous or tissue-specific promoter), the cDNA of the gene of interest, and a polyadenylation signal.
- Purify the construct to remove vector sequence and contaminants.
Step 2: Pronuclear Microinjection
- Harvest fertilized single-cell embryos.
- Using a fine glass needle, microinject the DNA construct directly into the larger male pronucleus of the embryo.
- Culture the injected embryos overnight to the two-cell stage.
Step 3: Embryo Transfer and Founder Identification
- Transfer the viable two-cell embryos into pseudopregnant surrogate females.
- Wean the resulting offspring (potential F0 founders) and screen them for integration of the transgene via Southern blotting or quantitative PCR to determine copy number and integration site number.
Step 4: Line Establishment
- Founders that successfully integrate the transgene are bred to establish independent lines. Each line must be characterized separately, as the site of integration can significantly affect transgene expression levels and patterns.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful model generation and validation rely on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for Genetic Model Generation
| Reagent / Solution | Function | Example Applications |
|---|---|---|
| Cas9 Nuclease Variants | Catalyzes double-strand DNA breaks at target sites. High-fidelity (HF) versions reduce off-target effects [79] [76]. | Standard SpCas9 for NGG PAM sites; other variants (e.g., SaCas9) for different PAMs and smaller size for viral delivery. |
| Guide RNA (gRNA) Libraries | Synthetic RNA molecules that direct Cas9 to specific genomic sequences. | For large-scale functional genomics screens to identify genes essential for cancer cell survival [79] [80]. |
| Homology-Directed Repair (HDR) Donors | DNA template (ssDNA or dsDNA) containing the desired edit, flanked by homology arms. | For precise point mutations (disease-associated SNPs) or insertion of reporter genes (e.g., EGFP, Luciferase) [74]. |
| dCas9 Effector Systems | Catalytically "dead" Cas9; can be fused to transcriptional activators/repressors or base-editing enzymes without cutting DNA [77]. | For epigenetic editing (CRISPRa/i) or single-base changes (Base Editing) without inducing DSBs, reducing indel artifacts. |
| Adeno-Associated Virus (AAV) Vectors | Viral delivery vehicle for CRISPR components in vivo. Limited packaging capacity (~4.7 kb) [76]. | Used in preclinical studies to deliver CRISPR systems to somatic tissues, e.g., silencing mutant SOD1 in an ALS mouse model [78]. |
| Lipid Nanoparticles (LNPs) | Non-viral delivery system for CRISPR ribonucleoproteins (RNPs) or mRNA in vivo [76] [80]. | Successfully used in clinical settings; e.g., delivering Cas9 mRNA to glioblastoma cells to target oncogenes like EGFRvIII [80]. |
The objective comparison presented in this guide demonstrates a clear paradigm shift in disease model generation. While traditional transgenic models retain utility for overexpression studies, CRISPR-Cas9 technology offers superior performance in efficiency, precision, and the ability to recapitulate human genetic diseases in their native physiological context. The selection of a model system must be guided by the specific research question: transgenic models for gain-of-function studies, and CRISPR-Cas9 for modeling precise genetic lesions, knockouts, and complex polygenic diseases. As the pharmacological research landscape evolves, with increasing regulatory emphasis on human-relevant data and the reduction of animal testing [12] [58], the precision and versatility of CRISPR-Cas9 models make them an indispensable tool for validating therapeutic targets and accelerating the development of novel drugs.
In the complex field of pharmacology research, particularly in the validation of animal disease models, researchers face a deluge of data from countless individual studies. Systematic reviews and meta-analyses have emerged as powerful methodologies to distill this vast amount of information into reliable, evidence-based conclusions. These formal processes provide a structured approach to identify, evaluate, and synthesize all available evidence on a specific research question, thereby minimizing bias and offering more robust insights than traditional narrative reviews [81] [82]. For researchers and drug development professionals working with animal models, these methodologies are invaluable for determining which models most accurately predict human responses to pharmacological interventions, ultimately guiding more efficient translation from preclinical research to clinical application [83] [84].
The distinction between these two methodologies is crucial: a systematic review is a comprehensive, objective process that collects and critically appraises all available studies on a formulated research question using explicit, systematic methods to minimize bias [82]. In contrast, a meta-analysis is a statistical technique used within a systematic review to quantitatively combine and analyze results from multiple independent studies, generating a more precise overall estimate of effect size [85] [86]. Understanding this relationship—that a meta-analysis may be conducted as a component of a systematic review but not all systematic reviews include meta-analysis—is fundamental to appropriately applying these tools in pharmacological research [87].
Key Concepts and Definitions: Systematic Reviews vs. Meta-Analyses
Comparative Analysis: Fundamental Differences and Relationships
The table below outlines the core distinctions and applications of systematic reviews versus meta-analyses in research:
| Feature | Systematic Review | Meta-Analysis |
|---|---|---|
| Primary Objective | To comprehensively identify, evaluate, and synthesize all relevant studies on a specific question [81] [82]. | To statistically combine results from multiple independent studies to produce a single, more precise estimate of effect [85] [82]. |
| Core Methodology | Uses explicit, pre-specified protocols for search, selection, appraisal, and synthesis of evidence [81] [85]. | Employs statistical models to pool quantitative data from included studies [82]. |
| Output | A qualitative or narrative synthesis of findings, often with tabulated study characteristics and quality assessments [87]. | A quantitative summary (e.g., pooled effect size, confidence intervals), typically visualized with forest plots [85] [87]. |
| When Used | Essential for answering focused research questions, mapping evidence, and identifying knowledge gaps [81]. | Appropriate when studies are sufficiently similar in design, population, intervention, and outcomes to allow meaningful statistical pooling [85] [86]. |
| Key Strength | Minimizes bias through comprehensive, reproducible methods; provides a full picture of the evidence landscape [85]. | Increases statistical power and precision; can resolve uncertainty when individual studies conflict or are underpowered [85] [82]. |
| Main Limitation | Can be time and resource-intensive; synthesis may be complex if studies are heterogeneous [81]. | Not always appropriate or possible; can be misleading if studies are clinically or methodologically too diverse ( "apples and oranges" problem) [85] [87]. |
The Integrated Workflow
Systematic reviews and meta-analyses typically follow a staged, integrated process. The workflow below illustrates how these two methodologies interrelate within a single research project.
Application to Animal Disease Model Validation
The Critical Role of Evidence Synthesis in Preclinical Research
In pharmacology, systematic reviews and meta-analyses of animal studies serve distinct but complementary purposes compared to their clinical counterparts. While clinical systematic reviews often aim to directly inform treatment decisions, preclinical systematic reviews are more exploratory. They are primarily used to evaluate the translational potential of animal models, generate new hypotheses, and inform the design of subsequent clinical trials [84]. By synthesizing evidence across multiple animal studies, researchers can determine if data supporting a new treatment is sufficiently robust to justify moving to human trials, thereby reducing research waste and unnecessary animal use [83] [84].
A key application is assessing the external validity of animal models—how well results from these models generalize to the human condition. Traditional criteria of face validity (similar symptoms), construct validity (similar underlying biology), and predictive validity (similar response to drugs) are often applied subjectively [38]. Systematic reviews provide a framework for objectively evaluating these validity parameters across the entire evidence base, helping to identify which animal species, genetic strains, and induction methods most accurately recapitulate human disease pathophysiology and drug responses [38] [84].
A Framework for Identifying Optimal Animal Models
The following diagram outlines a standardized framework for using systematic reviews to identify optimal animal models for efficacy assessment in drug development, incorporating key validation parameters.
Methodological Protocols for Conducting Systematic Reviews
Standardized Workflow for Evidence Synthesis
The conduct of a high-quality systematic review, whether focused on clinical or preclinical studies, follows a rigorous, pre-specified protocol to ensure transparency, reproducibility, and minimization of bias [81] [85]. The initial stage involves formulating a precise research question, typically structured using the PICO framework (Population, Intervention, Comparison, Outcomes) [81]. In the context of animal model validation, this translates to: Population (specific animal species and strain), Intervention (disease induction method or genetic modification), Comparison (control animals), and Outcomes (measured parameters validating the model).
A critical second step is registering the protocol with organizations like PROSPERO before beginning the review, which enhances transparency and reduces the risk of selective reporting bias [81] [83]. The subsequent literature search must be comprehensive, covering multiple bibliographic databases (e.g., Medline, Embase, Cochrane CENTRAL) and often including unpublished studies to mitigate publication bias [81]. At least two reviewers then independently screen studies for eligibility based on pre-defined inclusion/exclusion criteria, extract data, and assess the risk of bias in included studies using tools like the Cochrane Risk of Bias tool for clinical trials or the SYRCLE tool for animal studies [81] [83].
Statistical Methodology for Meta-Analysis
When studies are sufficiently homogeneous in design and outcomes, a meta-analysis can be performed. This involves statistical pooling of effect sizes from individual studies to generate a summary estimate with greater precision [82]. The choice of effect measure (e.g., odds ratio, risk ratio, mean difference) depends on the type of outcome data being analyzed [87]. A key consideration is assessing heterogeneity—the degree of variation in effects between studies—often quantified using the I² statistic [82]. High heterogeneity suggests that studies may not be estimating a single common effect and warrants exploration of potential sources through subgroup analysis or meta-regression [85] [87].
The results are typically visualized using forest plots, which display the effect size and confidence interval for each study alongside the pooled estimate [87]. Assessment of publication bias (the tendency for positive results to be published more than negative results) is also crucial, often performed through visual inspection of funnel plots or statistical tests [81] [84].
Essential Research Reagents and Tools for Evidence Synthesis
The following table details key resources and methodologies required for conducting rigorous systematic reviews and meta-analyses in pharmacological research.
| Tool / Reagent | Primary Function | Application in Evidence Synthesis |
|---|---|---|
| PICO Framework | Structures the research question into key components [81]. | Defines the scope for animal model validation: Patient/Problem (human disease), Intervention (animal model), Comparison (control), Outcome (validation parameters). |
| PRISMA Guidelines | A 27-item checklist for reporting systematic reviews and meta-analyses [83]. | Ensures complete and transparent reporting of the review process, from search strategy to synthesis. |
| PROSPERO Registry | International prospective register of systematic review protocols [81]. | Prevents duplication of effort, increases transparency, and reduces risk of reporting bias by registering the protocol before starting. |
| Cochrane Risk of Bias Tool | Assesses methodological quality of randomized controlled trials [81]. | Evaluates internal validity of clinical studies included in reviews assessing predictive validity of animal models. |
| SYRCLE Risk of Bias Tool | Assesses methodological quality of animal studies [83]. | Evaluates internal validity of primary animal studies, identifying potential biases in sequence generation, blinding, etc. |
| GRADE System | Grades the quality of evidence and strength of recommendations [81] [83]. | Rates confidence in estimates from animal studies, considering risk of bias, inconsistency, indirectness, and imprecision. |
| Statistical Software (R, Stata) | Performs complex statistical analyses for meta-analysis [82]. | Conducts data pooling, heterogeneity assessment, subgroup analysis, and generates forest and funnel plots. |
Systematic reviews and meta-analyses provide an indispensable framework for navigating the complex evidence landscape in pharmacology, particularly in the critical task of validating animal disease models. By applying rigorous, transparent, and reproducible methods, these methodologies enable researchers to objectively evaluate the collective strength of preclinical evidence, identify the most predictive animal models, and make informed decisions about translating findings to clinical trials. As the volume of preclinical research continues to grow, the disciplined application of evidence synthesis will become increasingly vital for reducing research waste, upholding the ethical use of animals, and ultimately improving the efficiency and success rate of drug development.
The validation of animal disease models represents a cornerstone of pharmacology research, yet a persistent translational gap undermines drug development efficiency. With over 90% of drugs that appear safe and effective in animal studies failing in human trials, the limitations of traditional approaches have become unsustainable [88]. This crisis has catalyzed a paradigm shift toward human-relevant technologies that promise to enhance predictive accuracy. The contemporary research landscape is now characterized by the strategic integration of complex in vitro systems—including organ-chips, organoids, and microphysiological systems—within a revised framework for therapeutic development [6]. This transition is further supported by evolving regulatory perspectives, evidenced by the FDA Modernization Act 2.0 which explicitly enables alternatives to animal testing for drug applications [6]. This guide objectively compares the performance of emerging human-relevant technologies against established animal models, providing experimental data and methodologies to inform research decisions within the validation framework for pharmacological research.
Comparative Analysis of Research Models
Performance Metrics of Animal Models Versus AdvancedIn VitroSystems
The validation of animal models traditionally rests on three criteria: predictive validity (accuracy in forecasting therapeutic outcomes), face validity (phenotypic similarity to human disease), and construct validity (alignment with human disease mechanisms) [5]. No single model perfectly fulfills all criteria, necessitating a multifactorial approach. The following table summarizes key comparative metrics across model types.
Table 1: Performance Comparison of Research Models in Drug Development
| Model Characteristic | Traditional Animal Models | Advanced In Vitro Models (Organ-Chips, Organoids) |
|---|---|---|
| Human Biological Relevance | Moderate to Low (species differences in anatomy, physiology, drug metabolism) [27] [88] | High (utilizes human primary cells, stem cells; recapitulates human-specific pathways) [89] [90] |
| Predictive Accuracy for Human Efficacy | Low (contributing to ~60% of clinical trial failures due to lack of efficacy) [88] | Promising (e.g., Liver-Chip model correctly identified human-relevant drug-induced liver injury) [6] |
| Predictive Accuracy for Human Toxicity | Variable (e.g., well-predicted for cardiac effects; poor for some organs) [88] | High Potential (provides human-specific toxicological pathways; avoids species-specific metabolism issues) [90] [6] |
| Complexity of Environment | High (systemic, multi-organ context) [27] | Moderate (single-organ or limited multi-organ interaction; improving) [89] [90] |
| Throughput & Cost | Low throughput, high cost (lengthy husbandry, ethical oversight) [91] | Medium to High throughput, variable cost (scalable; lower cost per data point than animals) [92] |
| Regulatory Acceptance | Established, required for most INDs [71] | Growing (first organ-chip submitted for CDER qualification in 2024) [6] |
Quantitative Data on Model Predictive Value
Specific case studies highlight the quantitative performance differences between traditional and new approach methodologies (NAMs).
Table 2: Case Study Data on Model Predictive Performance
| Model / Technology | Application / Test Case | Reported Outcome / Performance |
|---|---|---|
| Mouse Ascites Method [91] | Production of monoclonal antibodies (mAb) | Produces high-concentration mAb, but can cause significant pain/distress in mice. mAb can be contaminated with mouse proteins. |
| In Vitro Methods (Semi-permeable membrane) [91] | Production of monoclonal antibodies (mAb) | mAb concentration can be as high as in ascites fluid and is free of mouse contaminants. Can be more expensive for small-scale production. |
| Animal Models [88] | General preclinical safety and efficacy prediction | >90% failure rate in human trials; ~30% due to unmanageable toxicity, ~60% due to lack of efficacy. |
| Emulate Liver-Chip [6] | Prediction of Drug-Induced Liver Injury (DILI) | Outperformed conventional animal models and hepatic spheroid models in predicting human-relevant DILI. |
| iPSC-derived Cardiomyocytes [90] | Modeling Doxorubicin-induced Cardiotoxicity | Recapitulated patient-specific predilection to toxicity, identifying multiple mechanisms (ROS, DNA damage). |
| Human Organ Perfusion Systems [88] | Pre-clinical drug testing on donated human organs | Provides a platform for real-time, high-resolution data collection in a near-physiological human organ context. |
Experimental Protocols for Key Human-Relevant Technologies
Organ-on-Chip Model Workflow
Organ-Chips are microfluidic devices lined with living human cells that recreate organ-level functions and responses [89] [92]. The following protocol details a standard workflow for establishing a barrier tissue model (e.g., gut, lung).
Protocol 1: Establishing a Dynamic Organ-Chip Culture
- Chip Fabrication: Manufacture a microfluidic device from a clear, flexible polymer (e.g., PDMS). The device typically contains parallel microchannels (e.g., top and bottom) separated by a porous membrane coated with extracellular matrix (e.g., collagen) to aid cellular attachment [89].
- Cell Seeding: Introduce relevant human primary or stem cell-derived cells into the respective channels. For instance, seed epithelial cells on the top channel and endothelial cells on the bottom channel to mimic a tissue-vascular interface [89].
- Perfusion Culture: Connect the biochip to a peristaltic pump system to initiate continuous flow of culture medium through the channels. This perfusion simulates biomechanical forces such as blood flow, peristalsis, or breathing motions [89].
- Model Maturation: Culture the chip under dynamic flow conditions for several days to weeks to allow the cells to form mature, functional tissue structures that exhibit in vivo-like phenotypes and barrier integrity.
- Experimental Intervention: Introduce test compounds (drug candidates, toxins), pathogens, or immune cells into the system via the fluidic streams to study pharmacological responses, disease mechanisms, or immune cell recruitment [89].
- Endpoint Analysis: Utilize real-time, high-resolution readouts including:
Induced Pluripotent Stem Cell (iPSC) Disease Modeling
iPSCs enable the creation of patient-specific disease models by reprogramming somatic cells into a pluripotent state [90].
Protocol 2: Validating a Disease Mutation Using iPSC-derived Cells
- iPSC Generation & Line Establishment:
- Disease Cohort Selection: Identify patients with the phenotype of interest (e.g., doxorubicin cardiotoxicity) and healthy controls. Perform genome-wide association studies (GWAS) to identify genetic variants associated with the phenotype [90].
- Genetic Validation via SNP Correction:
- Using CRISPR/Cas9 or similar gene-editing technology, correct the single nucleotide polymorphism (SNP) in the patient-derived iPSC line to create an isogenic control [90].
- Differentiate the corrected iPSC line and the original (diseased) iPSC line into the relevant cell type (e.g., cardiomyocytes).
- Phenotypic Screening: Challenge the differentiated cells with the relevant stimulus (e.g., doxorubicin). Measure functional endpoints (e.g., contractility, cell death), molecular markers (e.g., reactive oxygen species, DNA damage), and -omics profiles (transcriptomics, proteomics) [90].
- Rescue & Mechanism Elucidation: A successful reversal of the disease phenotype in the gene-corrected line validates the causal role of the genetic variant. This model can then be used for deeper mechanistic studies and drug screening [90].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of advanced in vitro models relies on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for Complex In Vitro Systems
| Item / Reagent | Function / Application | Key Considerations |
|---|---|---|
| Primary Human Cells [89] | Provide human-relevant, physiologically accurate responses in organ-chips and 3D cultures. | Sourcing, donor variability, limited lifespan in culture. Patient-derived cells capture genetic diversity. |
| Induced Pluripotent Stem Cells (iPSCs) [90] | Foundation for patient-specific disease modeling; can be differentiated into any cell type. | Requires robust differentiation protocols; potential for residual immature phenotype. |
| Microfluidic Biochips [89] [92] | Provide the 3D scaffold and microarchitecture for tissue formation and perfusion. | Material (e.g., PDMS) can absorb small molecules; design dictates functionality. |
| Extracellular Matrix (ECM) Hydrogels [89] | Mimic the native tissue microenvironment, supporting 3D cell growth and signaling. | Composition (e.g., Matrigel, collagen) influences cell behavior; batch-to-batch variability. |
| Chemically Defined Media [90] | Supports cell growth and function without the variability of serum-containing media. | Enables reproducible, controlled experiments; formulation is cell-type specific. |
| Perfusion Pump Systems [89] | Generate dynamic fluid flow and biomechanical forces in organ-chips. | Critical for applying shear stress, mechanical stretch, and nutrient/waste exchange. |
The future of pharmacology research lies not in the wholesale replacement of animal models, but in their strategic augmentation with human-relevant technologies. The data and protocols presented here demonstrate that advanced in vitro systems offer superior performance in key areas, particularly human biological relevance and the prediction of specific toxicities and efficacies that are poorly modeled in animals. The ongoing validation and qualification of these tools by regulatory bodies like the FDA and critical path institutes signal a permanent shift in the research landscape [93] [6]. For researchers, the imperative is to adopt a fit-for-purpose strategy, selecting models based on a clear understanding of their predictive, face, and construct validity for the specific research question. By integrating data from organ-chips, iPSC models, and human organ perfusion systems—and using computational models as an unifying layer—the field can build a more predictive, efficient, and human-relevant path to new medicines.
Conclusion
The rigorous validation of animal disease models is not merely a procedural step but a fundamental prerequisite for improving the dismal rates of translation from bench to bedside. By systematically applying structured frameworks like the AMQA and FIMD, researchers can transparently assess a model's strengths and weaknesses, leading to more informed model selection and better-informed go/no-go decisions in drug development. While significant challenges remain—particularly concerning species differences and external validity—the continued refinement of these tools, coupled with the strategic integration of emerging human-relevant technologies such as complex in vitro systems, paves the way for a more predictive, efficient, and ethical future in pharmacology research. Ultimately, a fit-for-purpose validation strategy is paramount for de-risking drug development and delivering safe, effective therapies to patients.
References
- 1. The Predictive Pipeline: Structuring Drug Development ... [https://www.drugpatentwatch.com/blog/the-predictive-pipeline-structuring-drug-development-timelines-with-ai-driven-patent-intelligence/?srsltid=AfmBOopUmP_sJf0YnQEE_laRBH6o66bkb7gQ0RwLM3QVHWi6jXAPf-fK]
- 2. Dynamic clinical trial success rates for drugs in the 21st ... [https://www.nature.com/articles/s41467-025-64552-2]
- 3. Biopharma RD Faces Productivity And Attrition Challenges ... [https://www.clinicalleader.com/doc/biopharma-r-d-faces-productivity-and-attrition-challenges-in-2025-0001]
- 4. Transforming Cancer Therapy: Insights from 2025 H1 FDA ... [https://blog.crownbio.com/transforming-cancer-therapy-insights-from-2025-h1-fda-approvals-and-preclinical-drug-discovery]
- 5. Understanding Validity in Animal Models for Drug Discovery [https://www.taconic.com/resources/validated-animal-models]
- 6. Beyond Animals: Revolutionizing Drug Discovery with Human ... [https://wyss.harvard.edu/news/beyond-animals-revolutionizing-drug-discovery-with-human-relevant-models/]
- 7. How pharma is speeding up drug R&D with data [https://www.aveva.com/en/perspectives/blog/how-pharma-is-speeding-up-drug-r-and-d-with-data/]
- 8. The 4 Types of Validity in Research | Definitions & Examples [https://www.scribbr.com/methodology/types-of-validity/]
- 9. The 4 Types of Validity in Research Design (+3 More to ... [https://www.activecampaign.com/blog/validity-in-research-design]
- 10. Types of Measurement Validity [https://conjointly.com/kb/measurement-validity-types/]
- 11. Validity In Psychology Research: Types & Examples [https://www.simplypsychology.org/validity.html]
- 12. FDA to phase out animal testing requirement [https://www.bps.ac.uk/Publishing/Pharmacology-Matters/August-2025/No-More-Lab-Animals-%E2%80%9D-FDA-to-Phase-Out-Animal-Test]
- 13. Best Patent Tools for Pharmaceutical R&D: Top 7 for 2025 [https://www.patsnap.com/resources/blog/articles/pharmaceutical-patent-tools-2025/]
- 14. Drug Discovery Platforms Market Size & Trends, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/drug-discovery-platforms-market]
- 15. A Structured Approach to Optimizing Animal Model Selection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9291347/]
- 16. FDA and NIH Announce Initiatives to Reduce Animal ... [https://www.lw.com/en/insights/fda-and-nih-announce-initiatives-to-reduce-animal-testing-and-encourage-alternative-methodologies]
- 17. The Importance of Animal Models in Biomedical Research [https://www.mdpi.com/2076-2615/13/7/1223]
- 18. The continued importance of animals in biomedical research [https://www.nature.com/articles/s41684-024-01458-4]
- 19. Animal Models Used in Tests 2025-2033 Overview [https://www.archivemarketresearch.com/reports/animal-models-used-in-tests-782819]
- 20. Replacing and Reducing Animal Testing at CDER [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/replacing-and-reducing-animal-testing-cder]
- 21. FDA Announces Plan to Phase Out Animal Testing ... [https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs]
- 22. The 3Rs and Humane Experimental Technique [https://pmc.ncbi.nlm.nih.gov/articles/PMC6826930/]
- 23. The new paradigm in animal testing – “3Rs alternatives†[https://www.sciencedirect.com/science/article/abs/pii/S0273230024001466]
- 24. Animal testing and the 3Rs: Replacement [https://www.bps.ac.uk/publishing/pharmacology-matters/may-2025/animal-testing-and-the-3rs-replacement]
- 25. Animal Use Alternatives (3Rs) | National Agricultural Library [https://www.nal.usda.gov/animal-health-and-welfare/animal-use-alternatives]
- 26. Regulatory acceptance of 3R (replacement, reduction ... [https://www.ema.europa.eu/en/regulatory-acceptance-3r-replacement-reduction-refinement-testing-approaches-scientific-guideline]
- 27. Role of animal models in biomedical research: a review [https://pmc.ncbi.nlm.nih.gov/articles/PMC9247923/]
- 28. Are some animal models more equal than others? A case ... [https://www.sciencedirect.com/science/article/pii/S0014299919304765]
- 29. The Animal Model Quality Assessment - PubMed [https://pubmed.ncbi.nlm.nih.gov/35421235/]
- 30. Can animal data predict human outcome? Problems and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3411287/]
- 31. New Approach Methodologies: What Clinical Pharmacologists ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404678/]
- 32. Alternatives to Animal Testing [https://www.niehs.nih.gov/health/topics/science/sya-iccvam]
- 33. AnimalGAN Initiative [https://www.fda.gov/about-fda/nctr-research-focus-areas/animalgan-initiative]
- 34. The end of animal testing? Transitioning to models is promising [https://www.statnews.com/2025/07/15/end-animal-testing-new-drug-development-in-vitro-assays-modeling-organ-on-chip/]
- 35. Advancing the frontier of rare disease modeling: a critical ... [https://www.nature.com/articles/s41746-025-02068-1]
- 36. Is it possible to overcome issues of external validity in ... [https://pubmed.ncbi.nlm.nih.gov/30404629/]
- 37. Concepts and Challenges in Quantitative Pharmacology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2628212/]
- 38. A standardised framework to identify optimal animal models ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0218014]
- 39. Criteria of validity for animal models of psychiatric disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC3384226/]
- 40. Clinical Trial Generalizability Assessment in the Big Data Era [https://pmc.ncbi.nlm.nih.gov/articles/PMC7359942/]
- 41. Benchmarking QSP Models Against Simple Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC6118293/]
- 42. Machine learning generalizability across healthcare settings [https://www.nature.com/articles/s41746-022-00614-9]
- 43. Simple Methods for Evaluating 4 Types of Biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412628/]
- 44. Biomarkers and Surrogate Endpoints In Clinical Trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3551627/]
- 45. Planning clinically relevant biomarker validation studies using ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-016-0862-4]
- 46. Biomarker assessment – what to be aware of [https://acutecaretesting.org/en/articles/biomarker-assessment--what-to-be-aware-of]
- 47. Preclinical vs. Clinical Biomarkers: Understanding Their ... [https://blog.crownbio.com/preclinical-vs-clinical-biomarkers-understanding-their-distinct-roles-in-drug-development]
- 48. Authorization of Animal Experiments Is Based on Confidence ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.2000598]
- 49. Systematic review of guidelines for internal validity in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647591/]
- 50. A call to action to address critical flaws and bias in ... [https://www.nature.com/articles/s41598-025-15935-4]
- 51. The (misleading) role of animal models in drug development [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2024.1355044/full]
- 52. Methods for applying blinding and randomisation in animal ... [https://pubmed.ncbi.nlm.nih.gov/39365005/]
- 53. 4a. Randomisation - Explanation [https://arriveguidelines.org/arrive-guidelines/randomisation/4a/explanation]
- 54. FDA Eliminates Animal Testing: Impact on Biotechs [https://premier-research.com/perspectives/fda-eliminates-animal-testing-impact-on-biotechs/]
- 55. Non-Animal & Human-Relevant Research News [https://riseforanimals.org/news/sci-news-sept-2025/]
- 56. Why a human-first approach is the future of drug discovery [https://www.drugdiscoverynews.com/why-a-human-first-approach-is-the-future-of-drug-discovery-16647]
- 57. The systemic flaws in status quo science [https://www.beyondanimalresearch.org.nz/post/the-systemic-flaws-in-status-quo-science]
- 58. A Recent Timeline of U.S. Actions to Reduce and Replace ... [https://emulatebio.com/alternatives-to-animal-testing-in-drug-development/]
- 59. NIH to Prioritize Human-Based Research Technologies [https://nihrecord.nih.gov/2025/07/04/nih-prioritize-human-based-research-technologies]
- 60. Gaps between medical biology and AI drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S1359644625002259]
- 61. Animal Models of Human Disease 2.0 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11679604/]
- 62. Animal Models of Human Pathology: Revision, Relevance ... [https://www.mdpi.com/2227-9059/12/11/2418]
- 63. Modern animal models for biomedical research ... - STAT News [https://www.statnews.com/2025/11/07/animal-research-mice-models-invaluable-biomedical-discovery/]
- 64. Why 90% of clinical drug development fails and how to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9293739/]
- 65. Robustness of a multivariate composite score when ... [https://www.nature.com/articles/s41598-023-29623-8]
- 66. Innovative Drugs to Treat Depression: Did Animal Models ... [https://www.nature.com/articles/npp2013342]
- 67. Role of animal models in biomedical research: a review [https://labanimres.biomedcentral.com/articles/10.1186/s42826-022-00128-1]
- 68. Preclinical models for development of immune–oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10150782/]
- 69. Neuro-immune crosstalk in cancer: mechanisms and ... [https://www.nature.com/articles/s41392-025-02241-8]
- 70. The neuro-immune axis in cancer: from mechanisms to ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01748-5]
- 71. A large-scale dataset of in vivo pharmacology assay results [https://www.nature.com/articles/sdata2018230]
- 72. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 73. Review Next-gen tools in cancer neuroscience [https://www.sciencedirect.com/science/article/pii/S2211124725010290]
- 74. CRISPR/Cas9-Mediated Genetic Engineering In Vivo [https://www.taconic.com/services/crispr-gene-editing]
- 75. CRISPR–Cas9 Gene Editing: Curing Genetic Diseases by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10980556/]
- 76. CRISPR/Cas9 therapeutics: progress and prospects [https://www.nature.com/articles/s41392-023-01309-7]
- 77. Application and perspective of CRISPR/Cas9 genome ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1364742/full]
- 78. CRISPR/Cas9 a genomic engineering technology for ... [https://www.sciencedirect.com/science/article/pii/S2352320425001634]
- 79. Application of CRISPR-Cas9 genome editing technology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10916045/]
- 80. CRISPR/Cas9 technology in tumor research and drug ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1552741/full]
- 81. Introduction to systematic review and meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5903119/]
- 82. The Differences Between a Systematic Review vs Meta ... [https://www.distillersr.com/resources/systematic-literature-reviews/understanding-the-differences-between-a-systematic-review-vs-meta-analysis]
- 83. Value of preclinical systematic reviews and meta-analyses ... [https://www.nature.com/articles/s41390-024-03197-1]
- 84. Importance of Systematic Reviews and Meta-analyses ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7479780/]
- 85. The difference between a systematic review and a meta- ... [https://www.covidence.org/blog/the-difference-between-a-systematic-review-and-a-meta-analysis/]
- 86. What's the difference between a systematic review and a meta ... [https://mdanderson.libanswers.com/faq/367768]
- 87. Systematic Review or Meta-Analysis? - HMSOM Library [https://library.hmsom.edu/SystematicReviews/SR_MA]
- 88. Beyond animal testing: How human data trials are ... [https://pharmaphorum.com/rd/beyond-animal-testing-how-human-data-trials-are-reshaping-drug-development]
- 89. In vitro vs in vivo - Organ-on-chip for biomedical research [https://dynamic42.com/in-vitro-vs-in-vivo/]
- 90. In Vitro Alternatives to Animal Models - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK507212/]
- 91. Summary of Advantages and Disadvantages of In Vitro ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK100200/]
- 92. In Vitro vs In Vivo: A History of Modern Cell Culture [https://emulatebio.com/in-vitro-vs-in-vivo-cell-culture/]
- 93. NIH to prioritize human-based research technologies [https://www.nih.gov/news-events/news-releases/nih-prioritize-human-based-research-technologies]